Abstract
Sustainable digital transformation in healthcare is becoming increasingly urgent; there is limited empirical research on the organizational factors that contribute to success in emerging economies. This study addresses this gap by analyzing how leadership, knowledge management, and technology acceptance influence the development of smart hospitals, using Thailand as a case study. A mixed-methods approach was adopted, combining semi-structured interviews with senior administrators and a survey involving 370 respondents from 37 hospitals. The data were analyzed using exploratory factor analysis and multiple regression. The results indicate that institutional knowledge repositories and leaders’ reading comprehension skills significantly enhance the digital maturity of hospitals. Conversely, reliance on traditional communication methods and an excessive focus on ease of use negatively impact outcomes. These findings suggest that leadership-driven cognitive readiness and well-structured knowledge systems are more important than merely simplifying digital solutions. The originality of this research lies in integrating sustainability principles into digital transformation, connecting management competencies with the resilience of health systems. This study offers actionable insights for policymakers in low- and middle-income countries and presents a framework for the sustainable development of smart hospitals. Limitations and suggestions for future research are also discussed.
1. Introduction
The advancement of digital technologies has significantly influenced global healthcare systems by improving service delivery, operational efficiency, and patient engagement. In emerging economies, digital transformation plays a vital role in overcoming structural challenges such as workforce limitations, access inequities, and resource scarcity. One of the most transformative developments in this context is the emergence of smart hospitals, which leverage integrated digital infrastructure and intelligent systems to enhance both clinical and administrative functions [1,2,3,4].
Sustainability in healthcare encompasses more than environmental protection; it also involves economic viability, social equity, and institutional resilience [5]. A sustainable smart hospital not only deploys technology effectively but also minimizes environmental impact, supports equitable access to healthcare, ensures financial feasibility, and fosters long-term adaptability. Examples include reducing paper use through electronic health records, optimizing energy consumption via smart building systems, and extending services to rural areas through telemedicine platforms.
However, sustainable digital transformation requires more than just technical upgrades. Organizational factors such as leadership vision, knowledge management systems, and technology acceptance are essential to ensuring long-term success [2]. Despite increasing attention to smart healthcare, limited empirical research has examined how these strategic enablers influence both digital maturity and sustainability outcomes—particularly within public health systems in low- and middle-income countries (LMICs).
To bridge this gap, this study examines the strategic factors driving sustainable digital transformation in public hospitals within emerging economy contexts, using Thailand as a representative case. Sustainable digital transformation is understood here as the integration of advanced technologies into healthcare operations in ways that simultaneously improve efficiency, equity, resilience, and ecological responsibility. Specifically, the study investigates how leadership, knowledge sharing, and perceived technology ease of use contribute to the development and sustainability of smart hospitals. Despite the rapid global expansion of smart hospitals, limited research has critically examined how these organizational enablers interact to drive sustainable outcomes, particularly in resource-constrained settings. Prior studies have primarily emphasized technological deployment while overlooking the human and institutional dimensions that shape digital maturity. To address this gap, a mixed-methods design was employed, integrating qualitative data from expert interviews with quantitative data from healthcare professionals across public hospitals. This design enables triangulation of insights across institutional and individual levels, providing a robust basis for analyzing the organizational dynamics that underpin successful and sustainable transformation. This study aims to address the gap in understanding the strategic factors driving sustainable digital transformation in public hospitals within emerging economies, using Thailand as a case study. Sustainable digital transformation is defined as the integration of advanced technologies into healthcare operations in a manner that enhances efficiency, equity, resilience, and ecological responsibility.
Specifically, the research investigates the roles of leadership, knowledge sharing, and perceived ease of use of technology in the development and sustainability of smart hospitals. Despite the rapid global growth of smart hospitals, there has been limited research that critically examines how these organizational enablers interact to achieve sustainable outcomes, particularly in resource-constrained environments. Previous studies have focused mainly on technological deployment while often overlooking the human and institutional factors that influence digital maturity.
To fill this gap, a mixed-methods approach was employed, combining qualitative data from expert interviews with quantitative data collected from healthcare professionals in public hospitals. This design allows for the triangulation of insights at both the institutional and individual levels, providing a solid foundation for analyzing the organizational dynamics that support successful and sustainable transformation.
This research contributes to the literature by advancing an integrated framework that links digital maturity with sustainability in healthcare systems. The findings offer empirically grounded insights for policymakers, administrators, and digital health stakeholders in resource-constrained settings. By highlighting the strategic roles of leadership, institutional knowledge, and workforce competencies, this study informs the development of future-ready public health strategies that align digital transformation with broader sustainability goals, including those articulated in the United Nations Sustainable Development Goals (SDGs).
2. Literature Review
2.1. Smart Hospital Level and Sustainable Healthcare Systems
The concept of smart hospitals has gained significant attention in the healthcare industry, as it promises to improve patient outcomes, enhance operational efficiency, and reduce overall costs. The existing literature on smart hospital development highlights several key dimensions that characterize the maturity of a smart hospital, including resource management, patient care, and information management [6]. These dimensions are reflected in the maturity framework summarized in Table 1, which outlines the definitions and criteria of smart hospital levels. For instance, resource management in smart hospitals involves efficiently utilizing physical resources, such as inventory and transportation, and optimizing human resources through integrating digital technologies. Additionally, patient care in smart hospitals focuses on leveraging digital tools to enhance the quality and personalization of healthcare services, such as through electronic medical records, telemedicine, and data-driven decision-making [7].

Table 1.
Definitions and Criteria of Smart Hospital Maturity Levels.
By embedding sustainability into smart hospital development, institutions can simultaneously improve healthcare quality and contribute to the long-term ecological and economic performance of the health system [6].
The development of smart hospitals progresses through six distinct maturity levels, each contributing to the advancement of healthcare. Level 1 (Smart Place) focuses on creating a safe, clean, and modern environment that promotes the well-being of patients and staff. Level 2 (Smart Tools) introduces digital and automated devices designed to enhance service efficiency and improve diagnostic accuracy. Level 3 (Smart Services) integrates electronic medical records and digital government systems to streamline patient interactions and administrative processes. Level 4 (Smart Outcome) involves the adoption of enterprise resource planning and data-driven systems to facilitate benchmarking, performance improvement, and risk management. Level 5 (Smart Hospital) represents the achievement of full technological and organizational integration, ensuring operational efficiency, sustainability, and cost-effectiveness. Level 6 (Advanced Smart Hospital) is the highest stage, featuring cutting-edge innovations such as artificial intelligence, the Internet of Things (IoT), and renewable energy. This level enables personalized care and positions hospitals as interconnected nodes within a broader healthcare ecosystem.
2.2. Knowledge Management in Smart Hospital and Sustainable Hospital
Integrating digital technologies into healthcare settings also necessitates the effective management of knowledge, which is a critical success factor for smart hospital development. Knowledge management in the context of smart hospitals involves capturing, sharing, and applying knowledge to support decision-making, problem-solving, and continuous improvement [10]. The competencies and practices of knowledge management used in this study are summarized in Table 2.
2.2.1. Importance of Knowledge Management in Sustainable Digital Transformation
Knowledge management is essential for a hospital’s digital transformation, encouraging the integration of technologies to support smart hospital development. It helps identify digital solutions that align with strategic goals. Recent studies emphasize the significance of leadership, knowledge management, and technology acceptance in Thailand’s healthcare sector for successful technology integration [11].
Knowledge management enables healthcare organizations to retain institutional memory, reduce duplication, and facilitate evidence-based decisions—all essential for sustainable resource use. Hospitals that manage their knowledge assets effectively are better positioned to adapt to environmental challenges and policy shifts [12].
2.2.2. Practices and Systems of Knowledge Management in Healthcare
Knowledge management in the healthcare sector encompasses a range of practices and systems that facilitate the capture, storage, sharing, and application of knowledge. Collaborative platforms and tools for knowledge sharing among healthcare professionals and teams [13]. Knowledge repositories and databases are used to centralize and organize healthcare-related information [14], as well as best practices, data analytics, and visualization tools to derive insights from healthcare data and support evidence-based decision-making. Training and development programs to enhance the digital literacy and knowledge management skills of healthcare staff. Effective knowledge management in smart hospitals can lead to improved patient outcomes, enhanced operational efficiency, and better decision-making, ultimately contributing to the overall success of digital transformation initiatives.
2.2.3. Impact of Knowledge Management on Hospital Performance and Patient Outcomes
Knowledge Management (KM) enhances hospital performance and patient outcomes. KM practices empower healthcare organizations to streamline operations and make informed decisions by organizing, capturing, and sharing critical information. Research indicates that hospitals implementing robust KM systems, such as electronic health records (EHRs), optimize workflow efficiency and reduce errors [15,16]. The studies have shown that fostering a knowledge-sharing culture significantly correlates with improved service quality and patient care [17]. Furthermore, integrating advanced technologies like artificial intelligence enhances KM capabilities, allowing for better resource utilization and strategic decision-making [18]. Effective KM practices are vital for achieving better patient safety and satisfaction, underscoring healthcare institutions’ need to invest in comprehensive KM strategies [19].
The hypothesis suggests that effective hospital knowledge management enhances organizational effectiveness and patient care. Key practices involve using technology for knowledge storage, fostering a supportive culture, and building staff trust. Strong leadership and investments in training enhance knowledge creation, leading to better decision-making and service quality. Moreover, knowledge-sharing systems support hospital sustainability by improving operational efficiency and reducing clinical errors. Hospitals with strong KM frameworks are more likely to implement green practices and staff development programs aligned with sustainability goals [15].
Hypothesis 1:
Knowledge Management positively impacts upgrading the smart hospital level.

Table 2.
Measure of Knowledge Management.
Table 2.
Measure of Knowledge Management.
| Themes (Factors) | Codes | Competences (Items) | Description | Reference |
|---|---|---|---|---|
| Knowledge Management | Knowledge Management | Organizational Competency (KM1) | Fundamental to an organization’s achievement are its core competencies. These represent a unique blend of capabilities that define the organization’s strengths and attributes. Core competencies empower the organization to deliver value to its customers, competitively position itself within the market, and adapt to ever-changing environments. These competencies can be further categorized into two main types: core competencies and distinctive competencies. | [20,21] |
| Knowledge Repositories and Libraries (KM2) | The knowledge repository serves as a centralized hub for all forms of organizational knowledge. It encompasses a wide range of structured internal information, including research reports interpreting raw data, established techniques and methodologies, documented policies, internal memoranda, presentations, published articles, committee reports, and an inquiry-tracking database. | [22,23,24,25,26,27] | ||
| Knowledge Capture and Sharing (KM3) | Knowledge Capture and sharing encompass the strategic processes and systems that collect, store, and disseminate valuable organizational or community knowledge. This involves identifying critical insights, information, and expertise and making them readily accessible to those who can benefit. Examples include best practices, lessons learned, research findings, data, and methodologies, all documented in a structured and organized manner. Knowledge sharing leverages communication channels, platforms, and repositories to facilitate access, contribution, and collaboration around these knowledge resources. Effective knowledge capture and sharing ultimately foster a culture of learning, innovation, collaboration, and informed decision-making. | [28,29,30] | ||
| Culture of Knowledge Sharing (KM4) | Organizations that cultivate a knowledge-sharing culture unlock a strategic advantage by fostering innovation, agility, and resilience. This collaborative environment leverages the collective Intelligence and expertise of the workforce, enabling continuous learning, enhanced problem-solving, and sustained growth. | [31,32,33,34,35] | ||
| Strategic Knowledge Management in Talent Acquisition (KM5) | Leveraging knowledge management (KM) principles within the talent acquisition process optimizes efficiency and decision-making. By fostering knowledge sharing and best practices, organizations can streamline workflows, eliminate redundancy, and ultimately secure top talent. This strategic approach ensures a consistent and high-quality hiring experience. Training and support programs are designed with a learner-centric approach. These programs are tailored to address the specific needs of individual learners and are delivered through various engaging methods. Relevant resources are provided to further support learning objectives. A robust feedback and evaluation system ensures continuous improvement of both the programs and the learning experience. | [35,36,37] | ||
| Learner-Centric Development (KM6) | Training and support programs are designed with a learner-centric approach. These programs are tailored to address the specific needs of individual learners and are delivered through various engaging methods. Relevant resources are provided to further support learning objectives. A robust feedback and evaluation system ensures continuous improvement of both the programs and the learning experience. | [38,39,40,41] |
2.3. Leadership and Sustainable Smart Hospital
Effective leadership is crucial in the transition to smart hospitals, as it directly influences healthcare quality and operational success. Transformational leadership, recognized for inspiring and motivating staff, is vital in nurturing a culture prioritizing patient safety and innovation [42]. Leaders are expected to possess diverse skills, including cognitive abilities for strategic decision-making and interpersonal skills for fostering collaboration. This study emphasizes that consistent leadership with a clear vision is essential for navigating policy inconsistencies and staff resistance to change [43]. Additionally, strong communication skills enhance the leader’s capacity to effectively facilitate technological and organizational changes [44]. Leadership capabilities significantly impact the successful implementation of smart hospital initiatives, driving improvements in healthcare delivery and patient outcomes. The study operationalizes leadership competencies according to the framework presented in Table 3.
2.3.1. Role of Leadership in Facilitating Smart Hospital Development
Leadership is crucial for transforming hospitals into smart facilities by establishing a strategic vision and fostering innovation. Effective leaders overcome resistance to change, motivate staff, and align goals with technology. Transformational leadership improves employee motivation and patient satisfaction, significantly impacting organizational performance and efficiency amid digitalization complexities [45]. Sustainability-oriented leadership ensures digital strategies are aligned with long-term ecological, economic, and social goals. Leaders must champion policies that embed sustainability into the organizational culture and operational workflows [46].
2.3.2. Leadership Styles and Their Impact on Healthcare Quality
Different leadership styles significantly influence the quality of healthcare delivery. Transformational leadership is particularly impactful as it inspires and motivates healthcare employees, increasing patient satisfaction and improving clinical outcomes. This leadership approach fosters a culture of continuous improvement and innovation, which is essential in the rapidly evolving environment of smart hospitals. In contrast, authoritarian leadership can maintain service quality but may stifle creativity and adaptability, potentially hindering improvements and staff morale. Integrative leadership, which combines various leadership approaches, is also highlighted as effective in providing comprehensive and effective patient care. Transformational and green leadership styles are most effective in fostering innovation and sustainability. Such leadership emphasizes collaboration, long-term planning, and adaptive change management [47]. Therefore, the choice of leadership style is a critical factor in enhancing healthcare quality and ensuring positive patient experiences [48].
2.3.3. Example of Effective Leadership in Smart Hospital Projects
Effective leadership is pivotal for the successful implementation of smart hospital projects. Leaders in this context must demonstrate strategic vision and the ability to motivate teams toward shared goals. For instance, strong leaders facilitate innovation by fostering an environment of collaboration and open communication, allowing staff to voice concerns and share insights. Transformational leadership styles inspire and empower healthcare professionals, enhancing patient safety and care quality. Additionally, leaders play a crucial role in managing change, addressing resistance, and ensuring stakeholder engagement throughout the digital transformation process. Moreover, Hospitals led by visionary leaders often adopt energy-efficient technologies, reduce resource waste, and promote staff engagement in sustainability initiatives [47]. Examples from various smart hospital initiatives illustrate that decisive and visionary leadership correlates strongly with project outcomes, driving both technological adoption and the overall improvement in service delivery within healthcare settings [49,50,51].
Thus, Leadership skills are vital in smart hospitals, fostering innovation and collaboration. Influential leaders inspire patient-centered care, ensuring technology meets patient needs. With a clear vision and problem-solving abilities, they navigate integrating smart technologies, enhancing efficiency, accuracy, and accessibility in healthcare delivery, and steering the institution toward optimal care.
Hypothesis 2:
Leadership skills positively impact upgrading the smart hospital level.

Table 3.
Measure of Leadership Skills.
Table 3.
Measure of Leadership Skills.
| Themes (Factors) | Codes | Competences (Items) | Description | Reference |
|---|---|---|---|---|
| Leadership Skills | Cognitive Skills (CS) | Communication Skills (CS1) | Effective communication is a cornerstone of success in both personal and professional endeavors. Strong communication skills enable individuals to build trust and rapport, foster team collaboration, and adeptly resolve conflicts. By developing and honing these crucial abilities, individuals can significantly enhance their effectiveness as communicators, ultimately contributing to greater overall success and personal fulfillment. | [42,52,53,54,55] |
| Listening Skills (CS2) | Active listening is a vital communication skill that fosters a deeper understanding between speaker and listener. It requires the listener to fully engage with the speaker by attentively following verbal and nonverbal communication cues. This attentiveness lets the listener grasp the intended message, including underlying thoughts and emotions. Finally, active listening involves providing feedback, such as summarizing or paraphrasing key points, to confirm comprehension and encourage further dialog. | [55,56,57] | ||
| Writing Skills (CS3) | Writing Skills encompass the proficiency to articulate thoughts, ideas, information, and emotions through written language in a clear, concise, and impactful manner. This proficiency involves a strong command of grammar, vocabulary, and sentence structure, enabling the writer to communicate with the intended audience effectively. | [55] | ||
| Reading Comprehension Skills (CS4) | Reading Comprehension Skills encompass the ability to process written text effectively. This includes understanding the words’ literal meaning, interpreting the author’s underlying message and intent, and critically analyzing the information presented. Strong reading comprehension skills are foundational for successful learning and engagement with various written materials. | [58,59,60] | ||
| Business Skills (BS) | Operation Analysis (BS1) | Operational Analysis is a systematic approach to evaluating and improving an organization’s operational efficiency, effectiveness, and overall performance. | [61,62,63] | |
| Management of Personal Resources (BS2) | Personnel resource management involves overseeing and optimizing the utilization of human capital within an organization to achieve its goals and objectives. | [64,65] | ||
| Management of Financial Resources (BS3) | Financial resource management involves planning, organizing, directing, and controlling an organization’s financial activities to achieve its objectives while maximizing profitability and minimizing risk. | [66,67] | ||
| Management of Material Resources (BS4) | Management of Material Resources involves overseeing the acquisition, utilization, and optimization of physical assets and inventory within an organization to support its operations and achieve its goals. | [68,69] | ||
| Interpersonal Skills (IS) | Social Perceptiveness (IS1) | Social Perceptiveness refers to the ability to understand and accurately interpret the thoughts, feelings, motives, and intentions of others based on social cues, verbal and nonverbal communication, and situational context. | [70,71,72] | |
| Negotiation (IS2) | Negotiation Skills refer to communicating effectively, reaching agreements, and resolving conflicts through dialog and compromise. | [73,74] | ||
| Persuasion (IS3) | Persuasion influences someone’s beliefs, attitudes, opinions, or behaviors through communication and reasoning. | [75,76] | ||
| Strategic Skills (SS) | Vision (SS1) | Visioning in an organization refers to developing a shared vision or aspirational statement that outlines the organization’s desired future state. | [77,78,79] | |
| System Evaluation (SS2) | System Evaluation is a systematic process of assessing a system’s performance, effectiveness, efficiency, and overall quality. | [80,81,82] | ||
| Identification of Key Causes (SS3) | Identifying key causes involves identifying the underlying factors or root causes contributing to a particular problem, issue, or outcome. | [83,84] | ||
| Solution Appraisal (SS4) | Solution Appraisal involves evaluating and assessing potential solutions or interventions to address a problem or meet a need. | [85] |
2.4. Technology Acceptance and Digital Integration
The successful integration of digital technologies in the healthcare sector also heavily depends on healthcare professionals’ acceptance and adoption of these technologies. Factors that can influence technology acceptance include the following:
2.4.1. Factor Influencing Technology Acceptance Among Healthcare Staff
Technology acceptance among healthcare staff is significantly affected by several key factors. Perceived usefulness, which refers to the belief that technology enhances work efficiency and patient care, is crucial in fostering acceptance. Additionally, ease of use plays a vital role; technologies perceived as complex or burdensome can lead to resistance among staff. Trust in technology, driven by its reliability and data security, is another critical factor influencing acceptance. Furthermore, the perception of technology as a threat to professional autonomy may hinder adoption, as healthcare professionals fear it could undermine their clinical judgment. Models such as the Technology Acceptance Model (TAM) and the Unified Theory of Acceptance and Use of Technology (UTAUT) emphasize these aspects, underscoring how attitudes, perceived control, and social influences shape healthcare staff’s willingness to embrace new technologies in patient care [85,86]. Moreover, Healthcare professionals are more likely to adopt technologies perceived as environmentally responsible and efficiency-enhancing. Education on the ecological benefits of digital systems enhances adoption [86].
2.4.2. Model and Theories of Technology Acceptance in Healthcare
Several theoretical models have been developed to understand and predict the factors influencing technology acceptance in healthcare settings. The Technology Acceptance Model suggests that perceived usefulness and perceived ease of use are the primary determinants of an individual’s intention to use a technology [87]. The Unified Theory of Acceptance and Use of Technology incorporates additional factors, such as social influence and facilitating conditions, to explain technology acceptance. These models can provide valuable insights into the implementation of smart hospital initiatives by highlighting the critical role of addressing the needs and concerns of healthcare professionals, as well as the importance of strong organizational support and effective leadership in promoting the successful adoption of digital technologies within the healthcare sector. In addition, TAM and UTAUT models can be extended by incorporating sustainability-related perceived usefulness, such as reduced carbon footprint or lower material waste [88].
2.4.3. Case Studies and Examples of Technology Implementation in Smart Hospital
Case studies emphasize that addressing technology acceptance factors is vital for smart hospital success. Research in Canada identified effort expectancy, social influence, and organizational conditions as key influences, while a study in India highlighted trust and privacy concerns. A holistic approach is essential, integrating technology with organizational and leadership factors for effective digital transformation. Moreover, Hospitals that demonstrate how technology supports sustainability goals experience higher staff buy-in and stakeholder trust [89].
Thus, technology acceptance is a crucial driver of smart hospital development, as it impacts the adoption of innovative solutions, enhances operational efficiency, and ultimately improves patient care within the healthcare system. The dimensions of technology acceptance considered in this research are described in Table 4.

Table 4.
Measure of Technology Acceptance.
Hypothesis 3:
Technology acceptance positively impacts upgrading the smart hospital level.
2.5. Conceptual Model
The conceptual model integrates knowledge management, leadership skills, and technology acceptance as core enablers of both smart hospital maturity and healthcare sustainability. The integrated conceptual model is illustrated in Figure 1.
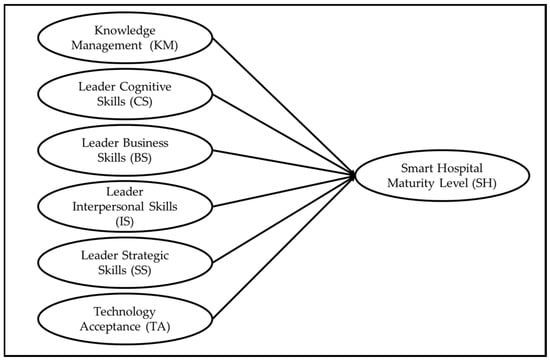
Figure 1.
Conceptual Model of Strategic Enablers for Sustainable Smart Hospital Development.
3. Research Methodology
This study used a mixed-methods approach to explore the strategic enablers of smart hospital development in Thailand’s public healthcare sector. By integrating qualitative and quantitative methods, the research aimed to capture both the contextual depth and the broader patterns needed to understand the digital transformation process within public hospitals.
A systematic literature search was conducted using the Scopus database, resulting in the identification of 1415 records. After removing duplicates, 1322 records remained for screening based on their titles and abstracts. Of these, 1102 records were excluded due to irrelevance to healthcare, a lack of focus on smart hospital development, or insufficient empirical evidence. Consequently, 220 full-text articles were evaluated for eligibility. Among these, 120 articles were excluded for reasons including lack of relevance to strategic enablers such as leadership, knowledge management, or technology acceptance, methodological limitations, or failure to meet inclusion criteria related to the setting or context. Ultimately, 100 articles were retained for the final synthesis. The entire selection process is summarized in Figure 2.
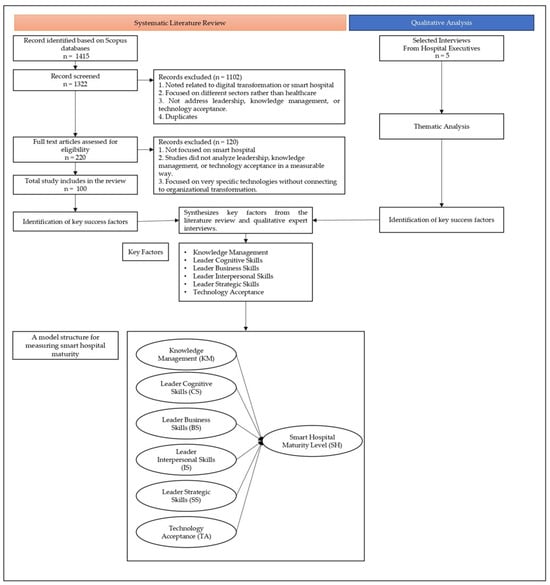
Figure 2.
Research Framework Integrating Literature Review and Thematic Analysis to Identify Strategic Enablers of Smart Hospital Maturity.
The empirical phase consisted of four key stages. First, semi-structured interviews were conducted with senior hospital administrators to explore themes such as institutional leadership, knowledge-sharing practices, and digital readiness. Next, the insights gained from the literature and the interviews were used to develop a structured survey instrument. This survey was then reviewed and validated by domain experts to ensure clarity and contextual relevance.
The validated questionnaire was distributed to 370 participants from 37 public hospitals throughout Thailand. The sample comprised hospitals of various sizes and administrative levels, ensuring diverse representation. The data were then analyzed using descriptive statistics, normality tests, outlier tests, exploratory factor analysis (EFA), and multiple regression analysis to assess the impact of strategic enablers on the maturity of smart hospitals.
This multi-stage approach offered both qualitative insights and quantitative strength. By integrating expert opinions and empirical validation, we were able to create a comprehensive framework that connects leadership competencies, knowledge management systems, and technology acceptance to the advancement of smart hospital models in resource-limited public healthcare environments.
3.1. Data Collection
This study employed a comprehensive data collection strategy grounded in a mixed-methods design to explore the strategic success factors influencing sustainable digital transformation toward smart hospitals in Thailand’s public healthcare sector. The research incorporated both qualitative and quantitative approaches to gain in-depth insights from expert informants and broader patterns from a statistically relevant sample.
The data collection process was divided into two main phases: qualitative and quantitative. Each phase was carefully structured to ensure methodological rigor, relevance, and alignment with the study’s objectives. The qualitative phase focused on collecting data through semi-structured interviews with selected experts in the smart hospital domain. These interviews aimed to capture nuanced experiences and insights from hospital executives who had firsthand involvement in digital transformation initiatives. The findings from this phase also informed the design of the survey instrument used in the quantitative phase.
In the quantitative phase, a structured questionnaire was distributed to a larger pool of participants representing various levels of public hospitals in Thailand. This phase was intended to validate the themes derived from the qualitative phase and to statistically examine the relationships among key constructs, including leadership competencies, knowledge management practices, technology acceptance, and smart hospital maturity.
This mixed-methods data collection framework allowed the researchers to triangulate findings, increase validity, and offer a comprehensive understanding of both individual and institutional factors driving the shift toward sustainable smart hospitals. The careful integration of qualitative and quantitative data enhanced the robustness of the study’s empirical foundation. It ensured that both micro-level insights and macro-level trends were adequately captured and analyzed.
3.1.1. Qualitative Data Collection
The qualitative data collection was carried out through semi-structured interviews with four key informants selected from hospitals actively engaged in smart hospital development. Participants were chosen using purposive sampling to ensure diverse representation from primary, secondary, and tertiary hospitals across various geographic regions in Thailand. All informants held senior management positions and were directly involved in the strategic planning and implementation of digital health technologies.
Each interview lasted approximately one hour and was conducted either face-to-face or via telephone, depending on logistical feasibility. Interviews were carried out in Thai to ensure comfort and clarity for participants and were audio-recorded with prior consent. The interview protocol was designed to explore themes such as institutional leadership, knowledge-sharing mechanisms, digital tool adoption, and challenges related to sustainability.
The interview questions were open-ended, allowing participants to elaborate freely on their experiences and opinions. This flexibility enabled the collection of rich, context-sensitive data. Interview recordings were transcribed verbatim and translated into English for thematic analysis. The research team ensured translation accuracy through independent reviews and validation by bilingual experts. To further increase reliability, member checking was conducted by sharing the summarized transcripts with participants for confirmation.
The qualitative phase provided essential foundational insights into how smart hospital initiatives were being conceptualized and executed within public hospitals. It revealed the importance of leadership continuity, interdepartmental communication, and staff engagement in achieving digital maturity. These insights were instrumental in informing the content and structure of the subsequent quantitative questionnaire.
3.1.2. Quantitative Data Collection
Following the qualitative phase, a structured questionnaire was developed to quantitatively assess the strategic factors that influence smart hospital development. The survey was informed by the themes and constructs that emerged from the interviews and was reviewed by subject-matter experts for clarity and relevance. It consisted of six main sections: demographic information, hospital digital maturity, leadership characteristics, knowledge management practices, technology acceptance, and perceptions of sustainability.
The questionnaire was developed based on constructs identified in the literature review (Section 2.2, Section 2.3 and Section 2.4) and themes emerging from the qualitative interviews. Items measured leadership competencies, knowledge management practices, technology acceptance, and hospital maturity using 4- or 5-point Likert scales. Content validity was established through review by three academic experts in healthcare management and two hospital administrators, ensuring clarity and relevance of items. A pilot test was conducted with 20 healthcare professionals, and minor adjustments were made to the wording to improve comprehension. The final instrument demonstrated strong internal consistency, with Cronbach’s alpha values for all constructs exceeding the recommended threshold of 0.70.
The target population included hospital administrators, department heads, and senior staff from 37 public hospitals in Thailand. Stratified purposive sampling was used to ensure that hospitals of various levels and locations were adequately represented.
Questionnaires were distributed both electronically and via postal mail to accommodate different preferences and ensure higher response rates. Respondents were given two weeks to complete the survey, with follow-up reminders sent to non-respondents. A total of 370 valid responses were collected, reflecting a strong response rate from a high-level administrative sample.
Upon collection, the data were entered into Statistical Package for the Social Sciences (SPSS) software for cleaning and preparation. The research team conducted a preliminary review to identify missing values, outliers, and inconsistencies. The cleaned dataset was then used to perform exploratory factor analysis and multiple regression analysis to examine the relationships among the identified strategic success factors and the smart hospital maturity outcomes.
This dual-phased data collection strategy allowed for comprehensive coverage of both exploratory and confirmatory aspects of the research. It provided a strong empirical basis for analyzing the interplay between strategic enablers and the development of smart, sustainable healthcare institutions in Thailand.
3.2. Data Analysis
The data analysis for this study was guided by a mixed-methods research design, tailored specifically to explore the strategic enablers of sustainable digital transformation in the public healthcare systems of emerging economies. Thailand was selected as a representative case due to its proactive government-led initiatives and structured smart hospital maturity framework under the Ministry of Public Health. This comprehensive approach enabled both the identification of contextual patterns and the empirical validation of critical factors influencing the success of digital transformation.
The analysis was conducted in two sequential phases. The first phase involved qualitative analysis using thematic exploration to extract key insights from expert interviews. This phase established the foundational understanding necessary for instrument development in the subsequent quantitative phase. The second phase utilized statistical methods to validate and generalize the insights obtained qualitatively, allowing for a comprehensive and triangulated interpretation.
Conceptually, both phases were rooted in the strategic domains of leadership, knowledge management, and technology acceptance, framed through the lens of sustainability. The qualitative phase employed Braun and Clarke’s six-step thematic analysis methodology to uncover patterns in narratives collected from hospital executives. Themes relating to digital strategy leadership, institutional knowledge-sharing mechanisms, and adaptive organizational behavior toward sustainable digital tools were identified.
Quantitative data analysis included the use of exploratory factor analysis (EFA) and multiple regression. These techniques were employed to validate the constructs and test hypotheses about the relationships between leadership, knowledge management, technology acceptance, and smart hospital maturity. The results offered statistical robustness and broader relevance to the findings, enabling greater insight into how emerging public healthcare systems can design scalable and sustainable smart hospital models.
This methodological structure not only strengthens the internal and external validity of the research but also aligns with the global discourse on sustainable digital healthcare transformation in developing regions. The integrated findings contribute to advancing both theoretical frameworks and practical policy interventions aimed at equitably transforming healthcare infrastructure through sustainable digital innovation.
3.2.1. Qualitative Methodology
The qualitative data, obtained from four semi-structured interviews with executive-level personnel from hospitals engaged in smart hospital development, were subjected to thematic analysis using [104] the six-phase approach. This framework provided a structured yet flexible methodology to extract meaningful themes from the transcribed data. The analysis began with data familiarization, during which transcripts were reviewed multiple times to immerse the researchers in the narratives. Initial codes were then generated manually, focusing on segments of text that reflected recurring concepts related to leadership vision, digital readiness, knowledge-sharing practices, and the perceived barriers to digital transformation.
These codes were subsequently categorized into potential themes and evaluated for internal coherence and distinctiveness. Thematic refinement involved collapsing overlapping themes and eliminating weak or inconsistent categories. Final themes were defined and labeled to accurately reflect their conceptual scope. To ensure trustworthiness, peer debriefing and member checking were employed. Bilingual experts assisted in verifying the accuracy of translations from Thai to English to maintain contextual meaning. Representative quotations from interviewees were used to support each theme and to illustrate the connection between empirical insights and the study’s theoretical framework.
3.2.2. Quantitative Methodology
The quantitative data were analyzed following data verification for completeness and consistency. Descriptive statistics were computed to summarize respondent demographics and to provide a contextual overview of hospital characteristics, digital maturity levels, and perceptions related to leadership, knowledge management, and technology acceptance. Subsequently, Exploratory Factor Analysis (EFA) was conducted to validate the dimensional structure of each construct. Principal component extraction with varimax rotation was applied, and variables with factor loadings below 0.5 or with significant cross-loadings were excluded to enhance construct clarity and measurement validity.
4. Results
This section presents the key findings of the study, derived from both qualitative and quantitative data sources. The results highlight the strategic factors that contribute to the successful digital transformation toward smart hospitals while integrating sustainability into their operations.
4.1. Qualitative Results
The implementation of smart hospital projects in Thailand represents a significant advancement in healthcare delivery, integrating cutting-edge technology to improve patient care and operational efficiency. The qualitative study was crucial in identifying the practical challenges and potential benefits from the perspectives of those directly involved. By engaging specialists through semi-structured interviews, summarized in Table 5, the study likely offers a detailed view of the interviewees’ backgrounds, providing context to their responses and ensuring a comprehensive understanding of the project’s impact from various professional angles.

Table 5.
Interviewee Profiles and Roles in Smart Hospital Implementation.
The triangulation method was employed to verify the authenticity and credibility of the data. Interviews were transcribed and analyzed through thematic analysis, uncovering two primary themes that impact the transition to smart hospitals: Leadership and Knowledge Management.
4.1.1. Leadership Insights
A significant challenge identified was the inconsistency in the Ministry of Health’s policies, which fluctuate based on the director’s position and rotation. This theme arose from interviews with the Deputy Director, Board of Directors, and Public Health Specialist, who highlighted the varying perspectives and approaches to the project among directors. Frequent policy changes undermine the project’s continuity and effectiveness. Consequently, strong leadership is essential for inspiring and motivating team members, articulating a clear vision, and executing the necessary actions to meet project objectives. Themes relating to leadership competencies identified through thematic analysis are summarized in Table 6.

Table 6.
Leadership Themes Identified from Thematic Analysis.
4.1.2. Knowledge Management Insights
Another important theme was the significance of knowledge transfer and updates in improving the quality of healthcare services. Interviewees stressed the need for supervisors to share their expertise and experiences with staff and the importance of annual training sessions to stay current with the latest medical knowledge and policies from the Ministry of Public Health. This theme was exemplified by the Deputy Director, Board of Directors, and Public Health Specialist, who pointed out that effective knowledge management enhances skills, boosts confidence, and improves performance in healthcare delivery. Knowledge management themes derived from the interviews are presented in Table 7.

Table 7.
Knowledge Management Themes Identified from Thematic Analysis.
4.2. Quantitative Results
The quantitative component of the research collected data through a structured survey administered to top management personnel across 37 public hospitals in Thailand, yielding 370 valid responses. The survey encompassed six sections that collected information on demographic characteristics, the current state of smart hospital development, leadership capabilities, knowledge management practices, and technology acceptance, utilizing a 4-point or 5-point Likert scale. The data collection was conducted over two months, employing both postal (200 surveys) and online methods (170 surveys) to ensure a broad reach.
Statistical analyses, including Exploratory Factor Analysis (EFA) and multiple regression analysis, were conducted to investigate the relationships among leadership, knowledge management, technology acceptance, and the development of smart hospitals. The results revealed significant correlations, highlighting that effective leadership, strong knowledge management practices, and high levels of technology acceptance are pivotal drivers of smart hospital development.
Interestingly, the analysis indicated that the perceived ease of technology usage had a negative impact on the progression of smart hospital initiatives, suggesting that mere user-friendliness does not guarantee development success. This finding points to the necessity for comprehensive training and strategic integration approaches to overcome implementation challenges. Overall, these quantitative insights underscore the importance of a multifaceted strategy that prioritizes leadership stability and robust knowledge management to ensure the effective adoption and maturation of smart hospital technologies within the Thai healthcare landscape
4.2.1. Descriptive Statistics
The data presented in Table 8 offers a comprehensive overview of the distribution of respondents across different hospital sizes. Medium-sized community hospitals have the highest representation among the respondents. This prevalence suggests that medium-sized hospitals are a standard healthcare setting, potentially reflecting a balance in capacity and accessibility that serves a significant portion of the population. On the other hand, small-sized community hospitals, while less represented, still account for a fifth of the respondents, hinting at a substantial number of healthcare facilities that operate on a smaller scale, possibly catering to local communities or offering more specialized services. The demographic characteristics of the respondents, as reflected in the data, are crucial for interpreting the survey results accurately and ensuring that the findings are representative of the broader healthcare environment.

Table 8.
Distribution of Sample Hospitals by Size and Bed Capacity.
The distribution of hospital sizes presented in Table 8 shows that medium-sized community hospitals make up the majority of the sample. This indicates that the findings primarily represent institutions that effectively balance accessibility with operational capacity, making them a pertinent reflection of Thailand’s healthcare system.
Table 9 shows the positions of the respondents, which were classified into twelve groups. Mostly, 63% are registered nurses. Nutritionists are the lowest percentage at 1%, while planners, policy analysts, and academic statisticians shared the percentage at 7%. Other positions included medical physicians, who represent 5%, in addition to physiotherapists, computer technical officers, and dentists (3% each). Lastly, medical technologists, radiological technologists, general administrators, and pharmacists (2% each).

Table 9.
Demographic Distribution of Respondent Roles Across Sample Hospitals.
As shown in Table 9, the majority of respondents were registered nurses (63%), followed by policy analysts and statisticians (14% combined). Physicians accounted for 5% of the sample, while other clinical and technical roles represented smaller proportions. This distribution highlights that leadership and managerial competencies in the sample were concentrated among nurses and senior administrators, reflecting their central role in hospital digital transformation initiatives.
The 37 hospitals’ Smart Hospital Maturity Level assessment, detailed in Table 10, provides a revealing snapshot of the current state of digital integration within the Thai healthcare system. Most hospitals are transitioning to more innovative operations, embracing Smart Services and Smart Tools. Adopting digital technologies for enhanced service delivery and integrated tool usage indicates a proactive approach toward modernization. However, the journey towards complete digital transformation is complex and multifaceted.

Table 10.
Smart Hospital Maturity Levels Across Participating Hospitals.
The fact that 45.95% of hospitals are at the Smart Services stage suggests a strong focus on patient-centric care, utilizing technology to streamline processes and improve patient outcomes. Similarly, the 32.43% of hospitals that have adopted Smart Tools are likely experiencing increased efficiency and accuracy in diagnostics and treatment, while the relatively small percentage (5.41%) of hospitals that have attained the Advanced Smart Hospital level points to the nascent nature of comprehensive digital transformation in the sector.
The Smart Hospital Maturity Assessment (Table 10) reveals that nearly 46% of hospitals are at Level 3 (Smart Services), while only 8% have achieved Levels 5 to 6. This indicates that most institutions are still in transitional stages; although digital adoption has begun, full integration and sustainability-oriented outcomes are not yet widespread. These findings highlight the necessity for organizational enablers—such as effective leadership and knowledge management—to facilitate progress toward higher maturity levels, which directly addresses the research objectives.
Assessment of the statistical appropriateness of the dataset for further analysis began with normality and outlier detection procedures, which were systematically conducted. Normality was examined by calculating the skewness and kurtosis values for all items. These values were found to fall within the commonly accepted threshold of ±2, as recommended in the literature, thereby confirming that the data exhibited a distribution suitable for parametric statistical techniques. Ensuring normality is particularly important when applying methods such as regression and factor analysis, as violations of this assumption can distort statistical inferences.
Exploratory Factor Analysis (EFA) was then applied to determine the underlying latent structure of the dataset and confirm construct validity. The analysis employed principal component extraction combined with varimax rotation to maximize interpretability of the factors. Items exhibiting factor loadings below 0.50 or significant cross-loadings on multiple components were removed to ensure construct clarity. The refined factor model revealed well-defined constructs aligned with the theoretical domains of leadership capabilities, knowledge management practices, and technology acceptance. These validated constructs formed the foundation for the multiple regression analysis that followed, strengthening the robustness and reliability of the research findings. The results of normality, outlier detection, and exploratory factor analysis are summarized in Table 11.

Table 11.
Normality, Outlier, and Exploratory Factor Analysis Test Results.
The values of skewness and kurtosis fell within the acceptable range of ±2, confirming the normal distribution of the data. This ensured the appropriateness of applying parametric techniques such as regression. Exploratory Factor Analysis validated the dimensional structure of the constructs, with all factor loadings exceeding 0.50 and aligning with the theoretical domains of leadership, knowledge management, and technology acceptance. No severe outliers were detected. These results confirm the robustness and construct validity of the dataset, providing a sound foundation for subsequent regression analysis.
4.2.2. Multiple Regression Analysis of Factors Influencing Smart Hospital Development
This section explores the relationships between various factors and the development of smart hospitals through multiple regression analysis. Prior studies have identified key elements that can significantly enhance the performance of healthcare facilities, thereby facilitating their evolution into smart hospitals. These factors include knowledge management, leadership skills, and technology acceptance.
Our analysis yielded an R-squared value of 0.703, indicating that these factors collectively explain approximately 70.3% of the variance in smart hospital development. This high explanatory power underscores the importance of these elements in the transformation process. The outcomes of the multiple regression analysis are presented in Table 12.

Table 12.
Multiple Regression Analysis of Factors Influencing Smart Hospital Maturity.
The results of the multiple regression analysis reveal that the strategic, cognitive, and managerial abilities of healthcare leaders significantly influence the maturity of smart hospitals. Among the measured leadership competencies, the ability to institutionalize and leverage knowledge repositories and libraries (KM2) emerged as a critical positive predictor of digital transformation progress (B = 2.239, p = 0.018). This finding reflects how healthcare leaders who prioritize structured knowledge systems contribute to enhancing organizational memory, promoting evidence-based decision-making, and enabling efficient resource allocation—factors essential to both operational sustainability and digital maturity. These repositories play a pivotal role in supporting clinical governance, reducing duplication, and fostering institutional resilience in response to dynamic healthcare challenges.
Conversely, communication skills (CS1) displayed a statistically significant negative association with smart hospital maturity (B = −3.567, p = 0.013). While effective communication is traditionally seen as a leadership strength, this result suggests that outdated or misaligned communication styles may create friction within digitally transforming institutions. Leaders relying heavily on conventional, non-digital communication channels may struggle to support real-time data exchange, cross-functional collaboration, and interoperability—all of which are essential for smart hospital development. These findings emphasize the necessity for leadership adaptation in communication strategies, such as integrating digital platforms, fostering transparent data flow, and encouraging agile communication structures that align with smart systems.
In contrast, reading comprehension skills (CS4)—a vital cognitive leadership attribute—were found to have a significant positive effect (B = 3.644, p = 0.002). This ability allows leaders to interpret and internalize complex documents, including digital health standards, policy frameworks, and sustainability protocols. Leaders with strong comprehension skills are better equipped to navigate regulatory requirements, evaluate technological options, and align organizational strategy with evolving national and global health agendas. As digital transformation requires continuous engagement with technical guidelines and sustainability indicators, this cognitive skill set is indispensable for healthcare executives striving to lead resilient, future-ready institutions.
An additional finding concerns technology ease of usage (TA1), which exhibited a negative relationship with hospital maturity (B = −2.252, p = 0.015). While user-friendliness is generally seen as beneficial, this result suggests that oversimplified digital tools may fail to support the complexity of healthcare operations. Leadership decisions that prioritize ease of use over strategic functionality could lead to fragmented systems or limited data integration, ultimately hindering progress toward sustainability. Therefore, effective leadership must strike a balance—selecting technologies that are not only accessible but also capable of supporting advanced analytics, interoperability, and long-term adaptability.
In comparison to studies conducted in other low- and middle-income countries (LMICs), the case of Thailand highlights the critical role of knowledge management in ensuring hospital sustainability. Research from India and Vietnam has also shown that structured digital repositories can reduce duplication and enhance adherence to policies. However, unlike in high-income countries, where user-friendly systems tend to promote adoption, this study found a negative relationship. This suggests that in resource-constrained environments, overly simplified systems may struggle to address complex operational needs. These findings underscore the necessity for technology strategies that are tailored to specific needs.
From a policy perspective, the results indicate that investing in leadership training programs, digital literacy, and sustainable knowledge systems is more effective than just focusing on acquiring user-friendly tools. By embedding these capabilities, organizations can ensure digital readiness while also aligning with sustainability priorities, such as resource efficiency, equitable access, and institutional resilience.
Overall, these results demonstrate that leadership abilities—particularly those involving strategic planning, knowledge management, and cognitive processing—are central to the success of digital transformation in public hospitals. Rather than viewing technology as the sole driver of smart hospital development, this study highlights that human leadership capabilities are equally, if not more, critical in achieving sustainable and scalable digital health systems. In this context, leadership serves as both an enabler and integrator of innovation, guiding institutions through the complex landscape of healthcare modernization.
These insights offer strong empirical support for the hypothesis that leadership abilities in healthcare are fundamental to smart hospital maturity and sustainable transformation. They also provide actionable guidance for policymakers: investing in leadership development programs that emphasize cognitive readiness, strategic foresight, and digital communication will be essential for accelerating smart healthcare initiatives in resource-constrained public health systems.
5. Discussion
The findings of this study provide important insights into the strategic success factors driving sustainable digital transformation toward smart hospitals in Thailand’s public healthcare sector. The integration of qualitative and quantitative data has revealed a complex interaction among leadership competencies, knowledge management systems, and technology acceptance in influencing the digital maturity of hospitals.
The qualitative results underscored the critical importance of leadership vision and stability. Hospital executives emphasized the need for sustained leadership commitment to navigate digital transformation effectively. This finding aligns with previous literature suggesting that transformational and sustainability-oriented leadership is essential in guiding institutional change and embedding environmental, social, and economic considerations into long-term strategic planning [46,105,106]. Leaders who support learning cultures and continuous innovation are better positioned to foster sustainable hospital environments.
Knowledge-sharing systems were also highlighted as fundamental to success. The interview data suggested that hospitals with robust training programs, digital knowledge repositories, and collaborative practices were more likely to develop mature digital capabilities. This finding is reinforced by the quantitative result showing that knowledge repositories had a strong positive effect on hospital maturity. These repositories serve not only as information banks but also as engines for operational efficiency, clinical safety, and resource conservation, contributing to the ecological and economic dimensions of sustainability [107,108,109].
Interestingly, the communication skills of the leader and the ease of use of technology were found to have a negative impact on the quantitative analysis. This counterintuitive result may suggest that the adoption of digital systems introduces communication complexity and requires deeper technological understanding than is often assumed. Simplistic tools that prioritize ease of use without accounting for integration depth or sustainability alignment may limit long-term benefits. Moreover, communication challenges could reflect institutional inertia or misalignment between technological and operational workflows. These findings point to the need for better digital literacy training and system-level alignment [110].
Reading comprehension skills of leaders, conversely, were shown to positively influence digital maturity. This reinforces the role of human capital in sustaining digital transformation. Staff who can accurately interpret digital guidelines and policy documentation are more likely to implement systems successfully and adapt to changing technological landscapes. In sustainability terms, this means that the cognitive readiness of healthcare professionals is a cornerstone for achieving efficient, environmentally conscious, and socially equitable service delivery [1,3].
Taken together, these findings emphasize that sustainability in digital healthcare is not simply about installing new technologies. It involves strategic alignment, knowledge infrastructure, leadership commitment, and human capacity. For Thailand’s public healthcare sector, this implies that efforts to advance smart hospitals must be holistic, engaging both systemic and behavioral change. Strengthening sustainability principles—such as long-term resource use, digital equity, and institutional adaptability—within digital transformation agendas is critical to achieving future-ready healthcare systems [2,5,111]
The qualitative results underscored the critical importance of leadership vision and stability. Hospital executives emphasized the need for sustained leadership commitment to navigate digital transformation effectively. This finding aligns with previous literature suggesting that transformational and sustainability-oriented leadership is essential in guiding institutional change and embedding environmental, social, and economic considerations into long-term strategic planning [6,108]. Leaders who support learning cultures and continuous innovation are better positioned to foster sustainable hospital environments.
Knowledge-sharing systems were also highlighted as fundamental to success. The interview data suggested that hospitals with robust training programs, digital knowledge repositories, and collaborative practices were more likely to develop mature digital capabilities. This finding is reinforced by the quantitative result showing that knowledge repositories had a strong positive effect on hospital maturity. These repositories serve not only as information banks but also as engines for operational efficiency, clinical safety, and resource conservation, contributing to the ecological and economic dimensions of sustainability [111].
Interestingly, communication skills and the ease of use of technology were found to have a negative impact on the quantitative analysis. This counterintuitive result may suggest that the adoption of digital systems introduces communication complexity and requires deeper technological understanding than is often assumed. Simplistic tools that prioritize ease of use without accounting for integration depth or sustainability alignment may limit long-term benefits. Moreover, communication challenges could reflect institutional inertia or misalignment between technological and operational workflows. These findings point to the need for better digital literacy training and system-level alignment.
Reading comprehension skills, conversely, were shown to positively influence digital maturity. This reinforces the role of human capital in sustaining digital transformation. Staff who can accurately interpret digital guidelines and policy documentation are more likely to implement systems successfully and adapt to changing technological landscapes. In sustainability terms, this means that the cognitive readiness of healthcare professionals is a cornerstone for achieving efficient, environmentally conscious, and socially equitable service delivery.
These findings underscore that achieving sustainability in digital healthcare extends beyond merely implementing new technologies. It necessitates deliberate strategic alignment, robust knowledge infrastructure, dedicated leadership, and a skilled, adaptable workforce. In the context of Thailand’s public healthcare sector, advancing smart hospitals requires a comprehensive approach that addresses both systemic reforms and behavioral adaptations. Embedding sustainability principles—such as efficient resource utilization, digital inclusion, and institutional flexibility—into digital transformation efforts is essential for establishing resilient and future-ready healthcare systems.
The quantitative phase produced statistically significant findings across the leadership, knowledge management, and technology acceptance constructs. Factor analysis confirmed the structure of key dimensions: strategic leadership, communication and vision, knowledge repositories, organizational learning, ease of technology use, and perceived sustainability value.
Multiple regression analysis revealed that several variables had a significant impact on the smart hospital maturity score. Knowledge repositories and reading comprehension skills were the strongest positive predictors, suggesting that institutions that prioritize internal knowledge systems and cognitive readiness are more likely to progress in their digital transformation journey. Conversely, communication overload and simplistic technological tools—designed for ease of use but lacking in robustness—were found to have a negative effect.
Overall, the regression model explained approximately 70% of the variance in hospital maturity. These findings support the hypothesis that strategic leadership, knowledge infrastructure, and user-centered digital policies are key enablers of sustainable smart hospital development in Thailand’s public healthcare sector.
6. Conclusions and Policy Implications
This study was motivated by the growing imperative to achieve sustainable and inclusive digital transformation in public healthcare systems, particularly within emerging economies facing structural constraints such as limited budgets, fragmented infrastructure, and uneven access to care. While previous efforts to promote smart hospital development have emphasized technological deployment, this research sought to investigate the strategic organizational enablers—specifically leadership competencies, knowledge management practices, and technology acceptance—that underpin successful and sustainable digital transformation. Using Thailand as a representative case, the study responds to a critical knowledge gap in the empirical literature concerning the human and institutional dimensions of digital healthcare sustainability.
The originality of this study lies in its integration of digital transformation, sustainability, and management competencies into a single analytical framework. It emphasizes that knowledge repositories and the cognitive abilities of leaders are more effective enablers than merely relying on basic digital tools. This approach enhances our theoretical understanding of the development of sustainable smart hospitals. The research makes a unique contribution by combining three interconnected domains—digital transformation, sustainability, and management competencies—into a cohesive framework for analyzing smart hospital development. This comprehensive perspective advances the existing literature by demonstrating that technological deployment alone is inadequate without strong leadership and organizational capacity.
This study primarily focuses on Thailand, but its findings are applicable to other emerging and developing economies that face similar structural challenges, such as limited budgets, uneven infrastructure, and workforce shortages. The strategic enablers identified—leadership competencies, robust knowledge repositories, and technology adoption aligned with the local context—can guide healthcare transformation strategies in low- and middle-income countries (LMICs). By incorporating sustainability principles into digital transformation efforts, public health systems can enhance their institutional resilience and align with global objectives, such as the United Nations Sustainable Development Goals (SDGs).
Employing a mixed-methods approach, the study integrated qualitative interviews with healthcare administrators and quantitative survey data from 370 professionals across 37 public hospitals in Thailand. Qualitative insights provided contextually rich perspectives on leadership stability and knowledge-sharing dynamics. At the same time, quantitative analysis—through exploratory factor analysis and multiple regression—validated the relationships among core constructs and their influence on smart hospital maturity. This design enabled triangulation across micro- and macro-level institutional settings, enhancing the robustness of the findings.
The results revealed several significant predictors of smart hospital maturity. Most notably, knowledge repositories of leadership and leader reading comprehension were positively associated with digital advancement, highlighting the critical importance of institutional memory and leader cognitive readiness skills in sustaining transformation. Conversely, perceived ease of technology use and leadership communication skills were negatively associated, suggesting that simplistic digital solutions and unstructured communication may hinder deeper institutional integration. These findings challenge conventional assumptions about usability and underscore the need for leaders to adopt more strategic, capability-driven approaches to digital healthcare reform.
The key policy implication is the necessity of moving beyond a technology-centric model toward one that prioritizes strategic leadership, robust knowledge systems, and human capital development. Policymakers should invest in leadership development programs that emphasize sustainability-oriented and transformational leadership styles capable of navigating policy shifts and staff resistance. In parallel, the establishment of centralized digital knowledge repositories and continuous professional development programs is essential to ensure that healthcare workers possess the competencies to interpret and adapt to evolving digital systems and sustainability standards.
Furthermore, digital health strategies must be aligned with broader national sustainability frameworks, such as the United Nations Sustainable Development Goals (SDGs). This includes promoting digital equity, reducing resource consumption through paperless and energy-efficient operations, and enhancing institutional resilience. Integrating these objectives into national digital health roadmaps will position public hospitals not only as sites of technological innovation but also as drivers of equitable and sustainable health system reform.
The study has several limitations. First, the data are self-reported, which may introduce response bias. Second, the analysis is limited to one country, which restricts generalizability. Finally, the study employs a cross-sectional design, limiting causal inferences. Future research should expand the scope of investigation to include longitudinal studies that track smart hospital implementation over time and assess long-term impacts on sustainability outcomes. Comparative studies between public and private healthcare institutions across various regional contexts would also help generalize findings and identify best practices for scalable implementation. Additionally, future work may examine the role of external partnerships—such as public–private collaborations and academic-industry linkages in accelerating sustainable digital transformation in healthcare.
Author Contributions
Conceptualization, S.C., N.R., Y.U. and C.J.; methodology, S.C., N.R. and C.J.; software, S.C.; validation, N.R.; formal analysis, investigation, S.C.; resources, data curation, S.C.; writing—original draft preparation, S.C.; writing—review and editing, S.C., N.R. and C.J.; visualization, and supervision, C.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institution Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Human Research Ethics Committee of Thammasat University (Science Branch) (HREC-TUSc), project code 103/2565, approved on 22 October 2022.
Informed Consent Statement
Informed Consent Statement from all subjects involved in the study.
Data Availability Statement
The data supporting the findings of this study are not publicly available due to ethical requirements and institutional confidentiality agreements. In accordance with research ethics protocols, all data are securely stored and access is strictly restricted to authorized personnel. Sharing or public dissemination of the data is not permitted in order to protect participant privacy.
Acknowledgments
This work was supported by the Center of Excellence in Logistics and Supply Chain Systems Engineering and Technology (LogEn) at Sirindhorn International Institute of Technology, Thammasat University. This article results from a research project entitled "Survey on the Digitalization and Human Resources of Thai Industries," supported by the Institute of Developing Economies.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Carini, C.; Piva, E. The sustainability potential of smart hospitals: Organizational and technological pathways. Sustainability 2022, 14, 3799. [Google Scholar] [CrossRef]
- Shahgholian, M.; Sadeghi, A.; Khani, M.M. Digital transformation in healthcare systems: The role of leadership and change management. Sustainability 2022, 14, 994. [Google Scholar] [CrossRef]
- Calzavara, A.; Mazzega, E.; Cillo, V. Designing resilient digital hospitals for a sustainable future. Sustainability 2023, 15, 379. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO Guideline: Recommendations on Digital Interventions for Health System Strengthening; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Zerbini, F.; Luzzini, D.; Brusoni, S. Sustainability-oriented innovation in public healthcare: A capabilities-based perspective. Sustainability 2021, 13, 8003. [Google Scholar] [CrossRef]
- Chiarini, A. Sustainable healthcare through digital technologies. Sustainability 2022, 14, 15. [Google Scholar] [CrossRef]
- Rasoulian-Kasrineh, M.; Sharifzadeh, N.; Tabatabaei, S.M. Smart Hospitals Around the World: A Systematic Review; Research Square: Durham, NC, USA, 2021. [Google Scholar] [CrossRef]
- Ministry of Public Health, Thailand. Smart Hospital Roadmap (2021–2027); Ministry of Public Health, Digital Health Division: Nonthaburi, Thailand. Available online: https://bdh.moph.go.th/site/main-smarthospital/ (accessed on 30 June 2023). (In Thai).
- Higazee, M.Z.A.; Gab Allah, A.R. The relationship between the political skills and negotiation behaviors of front-line nursing managers. Nurs. Forum 2022, 57, 1240–1248. [Google Scholar] [CrossRef] [PubMed]
- Kritchanchai, D.; Engelseth, P.; Srisakunwan, S. Implementing and Using New Information Technology in Hospital Logistics. In Proceedings of the 2018 IEEE International Conference on Industrial Engineering and Engineering Management (IEEM), Bangkok, Thailand, 16–19 December 2018; p. 1186. [Google Scholar] [CrossRef]
- Raimo, N.; Turi, I.D.; Albergo, F.; Vitolla, F. The drivers of the digital transformation in the healthcare industry: An empirical analysis in Italian hospitals. Technovation 2022, 121, 102558. [Google Scholar] [CrossRef]
- Lu, B.; Yue, S. Analysis of the Evolutionary Game of Three Parties in Environmental Information Disclosure in Sustainability Reports of Listed Forestry Companies in China. Sustainability 2022, 14, 2871. [Google Scholar] [CrossRef]
- Karamat, J.; Tong, S.; Ahmad, N.; Waheed, A.; Mahmood, K. Enablers Supporting the Implementation of Knowledge Management in the Healthcare of Pakistan. Int. J. Environ. Res. Public Health 2018, 15, 2816. [Google Scholar] [CrossRef]
- Morr, C.E.; Subercaze, J. Knowledge Management in Healthcare. In IGI Global eBooks; IGI Global: Hershey, PA, USA, 2010; p. 490. [Google Scholar] [CrossRef]
- Maramba, G.; Smuts, H. A Framework for Implementing a Computer-Based Knowledge Management System in Healthcare Organisations. Int. J. Knowl. Manag. 2022, 18, 1–30. [Google Scholar] [CrossRef]
- Ravikumar, R.; Kitana, A.; Taamneh, A.; Aburayya, A.; Shwedeh, F.; Salloum, S.; Shaalan, K. The Impact of Big Data Quality Analytics on Knowledge Management in Healthcare Institutions: Lessons Learned from Big Data’s Application within The Healthcare Sector. South East. Eur. J. Public Health 2023, 5, 1–17. [Google Scholar] [CrossRef]
- Ayatulloh, D.; Nursalam, N.; Kurniawati, N.D. The Effect of Knowledge Management in Healthcare Services: A Systematic Review. J. Pendidik. Keperawatan Indones. 2021, 7, 84–96. [Google Scholar] [CrossRef]
- Ljajić, S.; Randjelović, D.; Pirsl, D. Power of Knowledge, General Knowledge Management Strategies and Development of Relevant Managerial Competences. In Proceedings of the Tenth International Scientific Conference THE POWER OF KNOWLEDGE, Agia Triada, Greece, 7–9 October 2016; Available online: https://www.academia.edu/29093901/POWER_OF_KNOWLEDGE_GENERAL_KNOWLEDGE_MANAGEMENT_STRATEGIES_AND_DEVELOPMENT_OF_RELEVANT_MANAGERIAL_COMPETENCES (accessed on 30 June 2023).
- Solomon, L.; Gudi, R.B.; Asfandiyar, H.; Sneha, S.; Shahria, H. Knowledge Management in a Healthcare Enterprise: Creation of a Digital Knowledge Repository. In Proceedings of the 2022 IEEE International Conference on Digital Health (ICDH), Barcelona, Spain, 11–15 July 2022; pp. 215–217. [Google Scholar] [CrossRef]
- Kothari, A.; Hovanec, N.; Hastie, R.; Sibbald, S. Lessons from the business sector for successful knowledge management in health care: A systematic review. BMC Health Serv. Res. 2011, 11, 173. [Google Scholar] [CrossRef]
- Sittig, D.F.; Wright, A.; Meltzer, S.; Simonaitis, L.; Evans, R.S.; Nichol, W.P.; Ash, J.S.; Middleton, B. Comparison of clinical knowledge management capabilities of commercially-available and leading internally-developed electronic health records. BMC Med. Inform. Decis. Mak. 2011, 11, 13. [Google Scholar] [CrossRef] [PubMed]
- Grütter, R.; Steurer, J. Supporting Knowledge Management in an Online Community of Healthcare Professionals—The Evimed Project. Electron. Mark. 2000, 10, 282–286. [Google Scholar] [CrossRef]
- Dudas, V.; Bookwalter, T.; Kerr, K.M.; Pantilat, S.Z. The Impact of Follow-Up Telephone Calls to Patients After Hospitalization. Am. J. Med. 2001, 111, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Bose, R. Knowledge management-enabled health care management systems: Capabilities, infrastructure, and decision-support. Expert Syst. Appl. 2003, 24, 59–71. [Google Scholar] [CrossRef]
- Martinuzzi, A.; Carraro, E.; Petacchi, E.; Pasqualotti, S.; Costalunga, M.; Betto, S. Implementation of an ICF-based project/program in a pediatric Neuro-Rehabiltation hospital: Follow-up evaluation by stakeholders. Disabil. Rehabil. 2013, 35, 1059–1064. [Google Scholar] [CrossRef]
- Terzieva, M. Project Knowledge Management: How Organizations Learn from Experience. Procedia Technol. 2014, 16, 1086–1095. [Google Scholar] [CrossRef]
- Jacobs, E.J.; Roodt, G. The mediating effect of knowledge sharing between organisational culture and turnover intentions of professional nurses. S. Afr. J. Inf. Manag. 2011, 13, 6. [Google Scholar] [CrossRef]
- Assem, P.B.; Pabbi, K.A. Knowledge sharing among healthcare professionals in Ghana. VINE J. Inf. Knowl. Manag. Syst. 2016, 46, 479–491. [Google Scholar] [CrossRef]
- Ahsan, A.; Dewi, E.S.; Suharsono, T.; Setyoadi, S.; Soplanit, V.G.; Ekowati, S.I.; Syahniar, N.P.; Sirfefa, R.S.; Kartika, A.W.; Ningrum, E.H.; et al. Knowledge Management-Based Nursing Care Educational Training: A Key Strategy to Improve Healthcare Associated Infection Prevention Behavior. SAGE Open Nurs. 2021, 7, 23779608211044601. [Google Scholar] [CrossRef] [PubMed]
- Norris, A.; Brittain, J. Education, Training and the Development of Healthcare Informatics. Health Inform. J. 2000, 6, 189–195. [Google Scholar] [CrossRef]
- Brown, C.A.; Dickson, R. Healthcare students’e-literacy skills. J. Allied Health 2010, 39, 179–184. [Google Scholar]
- Adeleke, I.T.; Lawal, A.H.; Adio, R.A.; Adebisi, A.A. Information Technology Skills and Training Needs of Health Information Management Professionals in Nigeria: A Nationwide Study. Health Inf. Manag. J. 2015, 44, 30–38. [Google Scholar] [CrossRef]
- Karamitri, I.; Talias, M.A.; Bellali, T. Knowledge Management Practices in Healthcare Settings: A Systematic Review. Int. J. Health Plann. Manag. 2017, 32, 4–18. [Google Scholar] [CrossRef]
- Martinez-Gil, J. An Overview of Knowledge Management Techniques for e-Recruitment. J. Inf. Knowl. Manag. 2014, 13, 1450014. [Google Scholar] [CrossRef]
- Haesli, A.; Boxall, P. When knowledge management meets HR strategy: An exploration of personalization-retention and codification-recruitment configurations. Int. J. Hum. Resour. Manag. 2005, 16, 1955–1975. [Google Scholar] [CrossRef]
- Ruggles, R. The State of the Notion: Knowledge Management in Practice. Calif. Manag. Rev. 1998, 40, 80–89. [Google Scholar] [CrossRef]
- Haux, R. Strategic Information Management in Hospitals: An Introduction to Hospital Information Systems; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2004. [Google Scholar] [CrossRef]
- Nicolini, D.; Powell, J.; Conville, P.; Martinez-Solano, L. Managing Knowledge in the Healthcare Sector: A Review. Int. J. Manag. Rev. 2008, 10, 245–263. [Google Scholar] [CrossRef]
- Shahmoradi, L.; Safadari, R.; Jimma, W. Knowledge Management Implementation and the Tools Utilized in Healthcare for Evidence-Based Decision Making: A Systematic Review. Ethiop. J. Health Sci. 2017, 27, 541–558. [Google Scholar] [CrossRef] [PubMed]
- Ree, E.; Wiig, S. Linking transformational leadership, patient safety culture, and work engagement in home care services. Nurs. Open 2019, 7, 256–264. [Google Scholar] [CrossRef]
- Soesanto, R.; Efendy, H. Leadership Management of Military Hospital in Efforts to Improve the Patient Service (Case Study of RSAL Dr. Mintoarjo). Int. J. Hum. Resour. Stud. 2017, 8, 60. [Google Scholar] [CrossRef]
- Guzmán, V.E.; Muschard, B.; Gerolamo, M.; Kohl, H.; Rozenfeld, H. Characteristics and Skills of Leadership in the Context of Industry 4.0. Procedia Manuf. 2020, 43, 543–550. [Google Scholar] [CrossRef]
- Terzic-Supic, Z.; Bjegovic-Mikanovic, V.; Vukovic, D.; Santric-Milicevic, M.; Marinkovic, J.; Vasic, V.; Laaser, U. Training Hospital Managers for Strategic Planning and Management: A Prospective Study. BMC Med. Educ. 2015, 15, 25. [Google Scholar] [CrossRef]
- Afsar, B.; Umrani, W.A. Transformational leadership and sustainable performance: Mediating roles of responsible leadership and psychological empowerment. Sustainability 2020, 12, 3257. [Google Scholar] [CrossRef]
- Lapão, L.V. The nursing of the future: Combining digital health and the leadership of nurses. Rev. Lat. Am. De Enferm. 2020, 28, e3338. [Google Scholar] [CrossRef]
- Sfantou, D.F.; Laliotis, A.; Patelarou, A.E.; Sifaki-Pistolla, D.; Matalliotakis, M.; Patelarou, E. Importance of Leadership Style towards Quality of Care Measures in Healthcare Settings: A Systematic Review. Healthcare 2017, 5, 73. [Google Scholar] [CrossRef]
- Tanniru, M.; Khuntia, J.; Weiner, J. Hospital leadership in support of digital transformation. Pac. Asia J. Assoc. Inf. Syst. 2018, 10, 1. [Google Scholar] [CrossRef]
- Vogelsmeier, A.; Scott-Cawiezell, J. The Role of Nursing Leadership in Successful Technology Implementation. JONA J. Nurs. Adm. 2009, 39, 313–314. [Google Scholar] [CrossRef]
- Mekonnen, M.; Bayissa, Z. The Effect of Transformational and Transactional Leadership Styles on Organizational Readiness for Change Among Health Professionals. SAGE Open Nurs. 2023, 9, 23779608231185923. [Google Scholar] [CrossRef]
- Rider, E.A.; Keefer, C.H. Communication Skills Competencies: Definitions and a Teaching Toolbox. Med. Educ. 2006, 40, 624–629. [Google Scholar] [CrossRef] [PubMed]
- Wittenberg-Lyles, E.; Goldsmith, J.; Ferrell, B. Oncology Nurse Communication Barriers to Patient-Centered Care. Clin. J. Oncol. Nurs. 2013, 17, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Lorber, M.; Treven, S.; Mumel, D. The Examination of Factors Relating to the Leadership Style of Nursing Leaders in Hospitals. Nase Gospod. Our Econ. 2016, 62, 27–36. [Google Scholar] [CrossRef]
- Flaig, J.; Alam, A.; Huynh, J.; Reid-Hector, J.; Heuer, A. Examining How Formal Leadership Development Programs Positively Influence Hospital Leaders’ Individual Competencies and Organizational Outcomes—An Evidence-Based Literature Review. J. Healthc. Leadersh. 2020, 12, 69–83. [Google Scholar] [CrossRef]
- Jahromi, V.K.; Tabatabaee, S.S.; Abdar, Z.E.; Rajabi, M. Active Listening: The Key of Successful Communication in Hospital Managers. Electron. Physician 2016, 8, 2123–2128. [Google Scholar] [CrossRef]
- Bregenzer, A.; Milfelner, B.; Šarotar Žižek, S.; Jiménez, P. Health-Promoting Leadership and Leaders’ Listening Skills Have an Impact on the Employees’ Job Satisfaction and Turnover Intention. Int. J. Bus. Commun. 2023, 60, 239–255. [Google Scholar] [CrossRef]
- Cutting, L.E.; Scarborough, H.S. Prediction of Reading Comprehension: Relative Contributions of Word Recognition, Language Proficiency, and Other Cognitive Skills Can Depend on How Comprehension Is Measured. Sci. Stud. Read. 2006, 10, 277–299. [Google Scholar] [CrossRef]
- Wolf, M.S.; Wilson, E.A.; Rapp, D.N.; Waite, K.R.; Bocchini, M.V.; Davis, T.C.; Rudd, R.E. Literacy and Learning in Health Care. Pediatrics 2009, 124 (Suppl. S3), S275–S281. [Google Scholar] [CrossRef]
- Provvidenza, C.; Townley, A.; Wincentak, J.; Peacocke, S.; Kingsnorth, S. Building Knowledge Translation Competency in a Community-Based Hospital: A Practice-Informed Curriculum for Healthcare Providers, Researchers, and Leadership. Implement. Sci. 2020, 15, 22. [Google Scholar] [CrossRef]
- Shepard, D.S.; Hodgkin, D.; Anthony, Y.E. Analysis of Hospital Costs: A Manual for Managers; World Health Organization: Geneva, Switzerland, 2000; Available online: https://iris.who.int/handle/10665/42197 (accessed on 30 June 2023).
- Heng, H.; McGeorge, W.; Loosemore, M. Beyond Strategy: Exploring the Brokerage Role of Facilities Manager in Hospitals. J. Health Organ. Manag. 2005, 19, 16–31. [Google Scholar] [CrossRef]
- McLarty, J.; McCartney, D. The Nurse Manager, the Neglected Middle: Hospitals Can Improve Operational and Financial Effectiveness by Providing Nurse Managers with Data-Driven, Evidence-Based Management Tools and Training. Healthc. Financ. Manag. 2009, 63, 74–80. [Google Scholar]
- Bennett, A.C. Focus on Management Methods: Role of Personnel Administration in Employee Development. Hosp. Top. 1969, 47, 57–62. [Google Scholar] [CrossRef]
- Warshawsky, N.E.; Havens, D.S.; Knafl, G. The Influence of Interpersonal Relationships on Nurse Managers’ Work Engagement and Proactive Work Behavior. J. Nurs. Adm. 2012, 42, 418–425. [Google Scholar] [CrossRef]
- Ojo, T.O.; Akinwumi, A.F. Doctors as Managers of Healthcare Resources in Nigeria: Evolving Roles and Current Challenges. Niger. Med. J. 2015, 56, 375–380. [Google Scholar] [CrossRef]
- Gapenski, L.C.; Pink, G.H. Understanding Healthcare Financial Management, 7th ed.; Health Administration Press: Chicago, IL, USA, 2015. [Google Scholar]
- Paarima, Y.; Kwashie, A.A.; Ofei, A.M.A. Financial Management Skills of Nurse Managers in the Eastern Region of Ghana. Int. J. Afr. Nurs. Sci. 2021, 14, 100269. [Google Scholar] [CrossRef]
- Srinivasan, A.V. Managing a Modern Hospital; SAGE Publications India: New Delhi, India, 2008. [Google Scholar]
- Garcia, S.D.; Gil, R.B.; Haddad, M.d.C.L.; Vannuchi, M.T.O.; da Costa, D.B. The Role of a Nurse in the Management of Medical-Hospital Material: An Integrative Review. Online Braz. J. Nurs. 2013, 12, 411–4260. [Google Scholar] [CrossRef]
- Kidholm, K.; Ølholm, A.M.; Birk-Olsen, M.; Cicchetti, A.; Fure, B.; Halmesmäki, E.; Wild, C. Hospital Managers’ Need for Information in Decision-Making–An Interview Study in Nine European Countries. Health Policy 2015, 119, 1424–1432. [Google Scholar] [CrossRef] [PubMed]
- Janati, A.; Hasanpoor, E.; Hajebrahimi, S.; Sadeghi-Bazargani, H. Health Care Managers’ Perspectives on the Sources of Evidence in Evidence-Based Hospital Management: A Qualitative Study in Iran. Ethiop. J. Health Sci. 2017, 27, 659–668. [Google Scholar] [CrossRef]
- Dehcheshmeh, N.; Dashti, R.; Moradi-Joo, E.; Faraji Khiavi, F. Association between Social Capital and Quality of Health Services from the Perspective of Hospital Managers. Health Manag. Inform. Sci. 2020, 7, 14–19. [Google Scholar] [CrossRef]
- Covaleski, M.A.; Dirsmith, M.W. Building tents for nursing services through budgeting negotiation skills. Nurs. Adm. Q. 1984, 8, 1–11. Available online: https://journals.lww.com/naqjournal/Fulltext/1984/00820/Building_tents_for_nursing_services_through.3.aspx (accessed on 30 June 2023). [CrossRef] [PubMed]
- Dubnicki, C.; Sloan, S. Excellence in Nursing Management: Competency-Based Selection and Development. JONA J. Nurs. Adm. 1991, 21, 40–45. Available online: https://journals.lww.com/jonajournal/Fulltext/1991/06000/Excellence_in_Nursing_Management__Competency_Based.8.aspx (accessed on 30 June 2023). [CrossRef]
- Stevenson, J. Persuasion as a strategy for managing up. Am. J. Health-Syst. Pharm. 2001, 58 (Suppl. S1), S4–S6. [Google Scholar] [CrossRef] [PubMed]
- Vesterinen, S.; Suhonen, M.; Isola, A.; Paasivaara, L.; Laukkala, H. Nurse Managers’ Perceptions Related to Their Leadership Styles, Knowledge, and Skills in These Areas—A Viewpoint: Case of Health Centre Wards in Finland. Int. Sch. Res. Not. 2013, 2013, 951456. [Google Scholar] [CrossRef] [PubMed]
- Nurmeksela, A.; Zedreck Gonzalez, J.F.; Kinnunen, J.; Kvist, T. Components of the Magnet(R) model provide structure for the future vision of nurse managers’ work: A qualitative perspective of nurse managers. J. Nurse Manag. 2021, 29, 2028–2036. [Google Scholar] [CrossRef]
- Pillay, R. Managerial Competencies of Hospital Managers in South Africa: A Survey of Managers in the Public and Private Sectors. Hum. Resour. Health 2008, 6, 4. [Google Scholar] [CrossRef]
- Barati, O.; Sadeghi, A.; Khammarnia, M.; Siavashi, E.; Oskrochi, G. A Qualitative Study to Identify Skills and Competency Required for Hospital Managers. Electron. Physician 2016, 8, 2458–2465. [Google Scholar] [CrossRef][Green Version]
- Moradi, F.; Toghroli, R.; Abbas, J.; Ziapour, A.; Lebni, J.Y.; Aghili, A.; Soroush, A. Hospital Managers’ Skills Required and Onward Challenges: A Qualitative Study. J. Educ. Health Promot. 2020, 9, 228. [Google Scholar] [CrossRef]
- Shieh, J.-I.; Wu, H.-H.; Huang, K.-K. A DEMATEL Method in Identifying Key Success Factors of Hospital Service Quality. Knowl.-Based Syst. 2010, 23, 277–282. [Google Scholar] [CrossRef]
- Toygar, S.A.; Akbulut, Y. Managerial Skills of Hospital Administrators: Case Study of Turkey. J. Health Manag. 2013, 15, 579–594. [Google Scholar] [CrossRef]
- Shafii, M.; Hosseini, S.M.; Arab, M.; Asgharizadeh, E.; Farzianpour, F. Performance Analysis of Hospital Managers Using Fuzzy AHP and Fuzzy TOPSIS: Iranian Experience. Glob. J. Health Sci. 2016, 8, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Hua, D.; Petrina, N.; Young, N.; Cho, J.G.; Poon, S.K. Understanding the factors influencing acceptability of AI in medical imaging domains among healthcare professionals: A scoping review. Artif. Intell. Med. 2024, 147, 102698. [Google Scholar] [CrossRef] [PubMed]
- Lamprinos, I.; Demski, H.; Mantwill, S.; Kabak, Y.; Hildebrand, C.; Ploessnig, M. Modular ICT-based patient empowerment framework for self-management of diabetes: Design perspectives and validation results. Int. J. Med. Inf. 2016, 91, 31–43. [Google Scholar] [CrossRef] [PubMed]
- Stoumpos, A.I.; Kitsios, F.; Talias, M.A. Digital Transformation in Healthcare: Technology Acceptance and Its Applications. Int. J. Environ. Res. Public Health 2023, 20, 3407. [Google Scholar] [CrossRef]
- Safi, S.; Thiessen, T.; Schmailzl, K.J.G. Acceptance and Resistance of New Digital Technologies in Medicine: Qualitative Study. JMIR Res. Protoc. 2018, 7, e11072. [Google Scholar] [CrossRef]
- Pinto, A.M.; Carvalho, F.S.; dos Santos, B.C. Digital transformation for sustainability: Barriers and enablers. Sustainability 2021, 13, 9176. [Google Scholar] [CrossRef]
- Lederer, A.L.; Maupin, D.J.; Sena, M.P.; Zhuang, Y. The Technology Acceptance Model and the World Wide Web. Decis. Support Syst. 2000, 29, 269–282. [Google Scholar] [CrossRef]
- Legris, P.; Ingham, J.; Collerette, P. Why Do People Use Information Technology? A Critical Review of the Technology Acceptance Model. Inf. Manag. 2003, 40, 191–204. [Google Scholar] [CrossRef]
- Holden, R.J.; Karsh, B.-T. The Technology Acceptance Model: Its Past and Its Future in Health Care. J. Biomed. Inform. 2010, 43, 159–172. [Google Scholar] [CrossRef]
- Zuiderwijk, A.; Janssen, M.; Dwivedi, Y.K. Acceptance and Use Predictors of Open Data Technologies: Drawing upon the Unified Theory of Acceptance and Use of Technology. Gov. Inf. Q. 2015, 32, 429–440. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef] [PubMed]
- Pai, F.-Y.; Huang, K.-I. Applying the technology acceptance model to the introduction of healthcare information systems. Technol. Forecast. Soc. Change 2011, 78, 650–660. [Google Scholar] [CrossRef]
- Strudwick, G. Predicting Nurses’ Use of Healthcare Technology Using the Technology Acceptance Model: An Integrative Review. Comput. Inform. Nurs. 2015, 33, 189–198. [Google Scholar] [CrossRef]
- Aggelidis, V.P.; Chatzoglou, P.D. Using a Modified Technology Acceptance Model in Hospitals. Int. J. Med. Inform. 2009, 78, 115–126. [Google Scholar] [CrossRef]
- Dünnebeil, S.; Sunyaev, A.; Blohm, I.; Leimeister, J.M.; Krcmar, H. Determinants of Physicians’ Technology Acceptance for E-Health in Ambulatory Care. Int. J. Med. Inform. 2012, 81, 746–760. [Google Scholar] [CrossRef]
- Esmaeilzadeh, P.; Sambasivan, M.; Kumar, N.; Nezakati, H. The Effect of Knowledge Sharing on Technology Acceptance among Physicians. Glob. Adv. Res. J. Eng. Technol. Innov. 2013, 2, 48–57. [Google Scholar]
- AlQudah, A.A.; Salloum, S.A.; Shaalan, K. The Role of Technology Acceptance in Healthcare to Mitigate COVID-19 Outbreak. In Emerging Technologies During the Era of COVID-19 Pandemic; Hassanien, A.E., Slowik, A., Snášel, V., Eds.; Studies in Systems, Decision and Control; Springer: Cham, Switzerland, 2021; Volume 308, pp. 223–244. [Google Scholar] [CrossRef]
- Prasanna, R.; Huggins, T.J. Factors Affecting the Acceptance of Information Systems Supporting Emergency Operations Centres. Comput. Hum. Behav. 2016, 57, 168–181. [Google Scholar] [CrossRef]
- Setiawati, E.; Trisnawati, R.; Diana, U. The Analysis of Acceptance of Hospital Information Management System (HIMS) Using Technology Acceptance Model Method. Ris. Akunt. Dan Keuang. Indones. 2019, 4, 186–195. [Google Scholar] [CrossRef]
- Chau, P.Y. Influence of Computer Attitude and Self-Efficacy on IT Usage Behavior. J. Organ. End User Comput. 2001, 13, 26–33. [Google Scholar] [CrossRef]
- Taherdoost, H. A Review of Technology Acceptance and Adoption Models and Theories. Procedia Manuf. 2018, 22, 960–967. [Google Scholar] [CrossRef]
- Rahimi, B.; Nadri, H.; Afshar, H.L.; Timpka, T. A Systematic Review of the Technology Acceptance Model in Health Informatics. Appl. Clin. Inform. 2018, 9, 604–634. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Manea, L.; Sandu, D.; Oprea, D. Digital knowledge management in hospitals: A driver for sustainability. Sustainability 2023, 15, 4192. [Google Scholar] [CrossRef]
- Nguyen, T.H.; Ngo, L.V.; Ruël, H. Knowledge sharing in healthcare institutions: Impact on sustainability outcomes. Sustainability 2021, 13, 5002. [Google Scholar] [CrossRef]
- Batbaatar, E.; Dorjdagva, J.; Luvsannyam, A. The role of digital repositories in achieving sustainable health care outcomes. Sustainability 2021, 13, 6018. [Google Scholar] [CrossRef]
- Tajudeen, F.P.; Jaafar, N.I.; Ainin, S. Social media and sustainability in public hospitals: Knowledge sharing perspective. Sustainability 2022, 14, 445. [Google Scholar] [CrossRef]
- Brommeyer, M.; Liang, Z.; Whittaker, M.; Mackay, M. Developing Health Management Competency for Digital Health Transformation: Protocol for a Qualitative Study. JMIR Res. Protoc. 2023, 12, e51884. [Google Scholar] [CrossRef]
- Kocot, M.; Kwasek, A.; Maciaszczyk, M.; Golińska-Pieszyńska, M.; Protasowicki, I.; Kandefer, K.; Soboń, J. The Role of Employee Competencies in the Sustainable Development and Energy Efficiency of Agile Organizations. Sustainability 2024, 16, 9755. [Google Scholar] [CrossRef]
- Gracia, A.; Rojas, J. Policy implications of sustainability in healthcare innovation. Sustainability 2021, 13, 7321. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).