Decarbonizing the Healthcare Estate: Lessons Learned from NHS Trust Green Plans in England
Abstract
1. Introduction
2. Existing Strategies to Decarbonize Healthcare Estate
2.1. Reaching Net Zero Through Built Asset Management in Healthcare Estate
2.2. Implementing Heat Decarbonisation in Healthcare Estate
2.3. Switching to Renewable and Low-Carbon Sources of Energy in Healthcare Estate
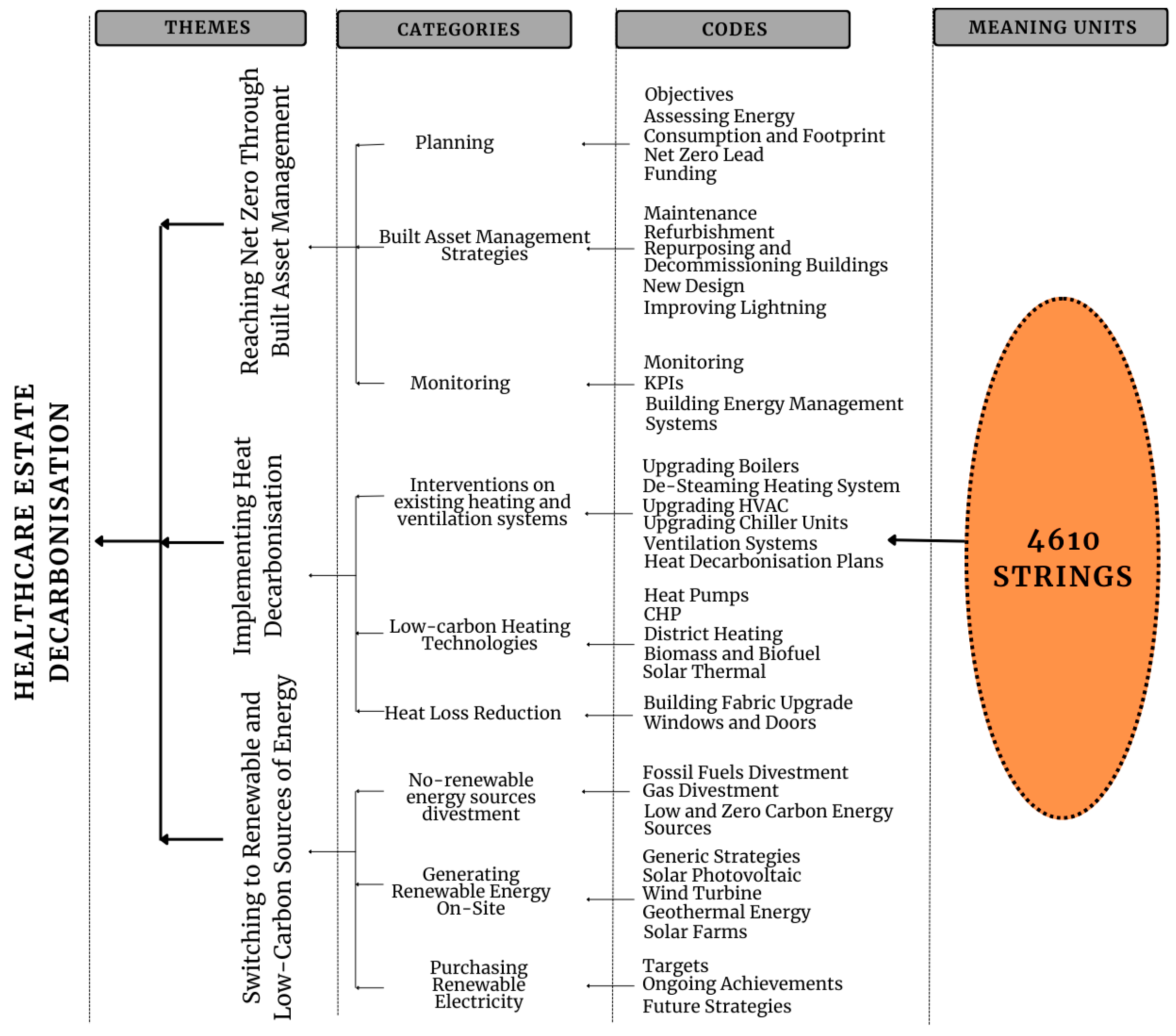
3. Materials and Methods
4. Results
4.1. Reaching Net Zero Through Built Asset Management in the Green Plans
4.1.1. Planning
4.1.2. Built Asset Management Strategies
4.1.3. Monitoring
4.2. Implementing Heat Decarbonisation in the Green Plans
4.2.1. Interventions on Existing Heating and Ventilation Systems
4.2.2. Low-Carbon Heating Technologies
4.2.3. Heat Loss Reduction
4.3. Switching to Renewable and Low-Carbon Sources of Energy in the Green Plans
4.3.1. No-Renewable Energy Sources Divestment
4.3.2. Generating Renewable Energy On-Site
4.3.3. Purchasing Renewable Electricity
5. Discussion
5.1. Reaching Net Zero Through Built Asset Management
5.2. Implementing Heat Decarbonisation
5.3. Switching to Renewable and Low-Carbon Sources of Energy
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
Abbreviations
| BEMSs | Building Energy Management Systems |
| HDP | Heat Decarbonization Plan |
| HVAC | Heating, Ventilation, and Air Conditioning |
| ICBs | Integrated Care Boards |
| KPI | Key Performance Indicators |
| PPAs | Power Purchasing Agreements |
| REGO | Renewable Energy Guarantees of Origin |
| SMART | Specific, Measurable, Achievable, Realistic, Time-bound |
References
- Mosadeghrad, A.M.; Isfahani, P.; Eslambolchi, L.; Zahmatkesh, M.; Afshari, M. Strategies to Strengthen a Climate-Resilient Health System: A Scoping Review. Glob. Health 2023, 19, 62. [Google Scholar] [CrossRef]
- Braithwaite, J.; Smith, C.L.; Leask, E.; Wijekulasuriya, S.; Brooke-Cowden, K.; Fisher, G.; Patel, R.; Pagano, L.; Rahimi-Ardabili, H.; Spanos, S.; et al. Strategies and tactics to reduce the impact of healthcare on climate change: Systematic review. BMJ 2024, 387, e081284. [Google Scholar] [CrossRef]
- Salas, R.N.; Solomon, C.G. The Climate Crisis—Health and Care Delivery. N. Engl. J. Med. 2019, 381, e13. [Google Scholar] [CrossRef]
- Karliner, J.; Slotterback, S.; Boyd, R.; Ashby, B.; Steele, K.; Wang, J. Health Care’s Climate Footprint: The Health Sector Contribution and Opportunities for Action. Eur. J. Public Health 2020, 30. [Google Scholar] [CrossRef]
- Pichler, P.-P.; Jaccard, I.S.; Weisz, U.; Weisz, H. International Comparison of Health Care Carbon Footprints. Environ. Res. Lett. 2019, 14, 064004. [Google Scholar] [CrossRef]
- United Nations Framework Convention on Climate Change. Adoption of the Paris Agreement, Decision 1/CP.21; UNFCCC: Paris, France, 2015; Available online: https://unfccc.int/resource/docs/2015/cop21/eng/10a01.pdf (accessed on 30 April 2025).
- World Health Organization. WHO Guidance for Climate-Resilient and Environmentally Sustainable Health Care Facilities; WHO: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications/i/item/9789240012226 (accessed on 30 April 2025).
- World Health Organization. Alliance for Transformative Action on Climate and Health (ATACH); WHO: Geneva, Switzerland, 2025; Available online: https://www.who.int/initiatives/alliance-for-transformative-action-on-climate-and-health (accessed on 30 April 2025).
- Wise, J. COP26: Fifty Countries Commit to Climate Resilient and Low Carbon Health Systems. BMJ 2021, 375, n2734. [Google Scholar] [CrossRef]
- Health Care Without Harm. Seven European Countries Commit to Developing Climate Resilient, Sustainable Low-Carbon Health Systems. 2022. Available online: https://europe.noharm.org/news/seven-european-countries-commit-developing-climate-resilient-sustainable-low-carbon-health (accessed on 30 April 2025).
- Mirow, J.; Venne, J.; Brand, A. Green Health: How to Decarbonise Global Healthcare Systems. Sustain. Earth Rev. 2024, 7, 28. [Google Scholar] [CrossRef]
- Department of Health and Social Care. Health and Care Act 2022; GOV.UK. 2022. Available online: https://www.gov.uk/government/collections/health-and-care-act-2022 (accessed on 30 April 2025).
- NHS England. Green Plan Guidance; NHS England: London, UK, 2025; Available online: https://www.england.nhs.uk/publication/green-plan-guidance (accessed on 30 April 2025).
- NHS England. Delivering a ‘Net Zero’ National Health Service; NHS England: London, UK, 2020; Available online: https://www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2020/10/delivering-a-net-zero-national-health-service.pdf (accessed on 30 April 2025).
- NHS England. NHS Net Zero Building Standard; NHS England: London, UK, 2023; Available online: https://www.england.nhs.uk/publication/nhs-net-zero-building-standard/ (accessed on 30 April 2025).
- Amamou, A.; Blenkinsop, D.S.; Winter, D.C.; Heidrich, P.O. Net Zero in Healthcare Buildings: Lessons from Assessing the Strategies of 214 NHS Trusts in England. Build. Environ. 2025, 278, 112966. [Google Scholar] [CrossRef]
- NHS England. The NHS Premises Assurance Model (NHS PAM), Version 1.2; NHS England: London, UK, 2023; Available online: https://www.england.nhs.uk/wp-content/uploads/2023/05/Premises-Assurance-Model-NHS-PAM-2023.pdf (accessed on 30 April 2025).
- Department of Health and Social Care. NHS Property and Estates: Why the Estate Matters for Patients; HMSO: London, UK, 2017. Available online: https://www.gov.uk/government/publications/nhs-property-and-estates-naylor-review (accessed on 30 April 2025).
- NHS England. Estates Returns Information Collection (ERIC) 2021/22: Official Statistics; NHS England: London, UK, 2022; Last Updated 31 December 2024; Available online: https://digital.nhs.uk/data-and-information/publications/statistical/estates-returns-information-collection (accessed on 30 April 2025).
- Tomanek, M. Energy Efficiency in Hospitals—Towards Sustainable Healthcare. Builder 2024, 320, 38–41. [Google Scholar] [CrossRef]
- Silva, B.V.F.; Holm-Nielsen, J.B.; Sadrizadeh, S.; Teles, M.P.R.; Kiani-Moghaddam, M.; Arabkoohsar, A. Sustainable, Green, or Smart? Pathways for Energy-Efficient Healthcare Buildings. Sustain. Cities Soc. 2024, 100, 105013. [Google Scholar] [CrossRef]
- Teke, A.; Timur, O. Assessing the Energy Efficiency Improvement Potentials of HVAC Systems Considering Economic and Environmental Aspects at the Hospitals. Renew. Sustain. Energy Rev. 2014, 33, 224–235. [Google Scholar] [CrossRef]
- Atienza-Márquez, A.; Muñoz, F.D.; Hernández, F.F.; López, J.M.C. Domestic hot water production system in a hospital: Energy audit and evaluation of measuresto boost the solar contribution. Energy 2022, 261, 125275. [Google Scholar] [CrossRef]
- Prada, M.; Prada, I.F.; Cristea, M.; Popescu, D.E.; Bungău, C.; Aleya, L.; Bungău, C.C. New Solutions to Reduce Greenhouse Gas Emissions through Energy Efficiency of Buildings of Special Importance—Hospitals. Sci. Total. Environ. 2020, 718, 137446. [Google Scholar] [CrossRef] [PubMed]
- Silvestro, F.; Bagnasco, A.; Lanza, I.; Massucco, S.; Vinci, A. Energy Efficient Policy and Real Time Energy Monitoring in a Large Hospital Facility: A Case Study. Int. J. Heat Technol. 2017, 35, S221–S227. [Google Scholar] [CrossRef]
- Ascione, F.; Bianco, N.; De Masi, R.F.; Vanoli, G.P. Rehabilitation of the Building Envelope of Hospitals: Achievable Energy Savings and Microclimatic Control on Varying the HVAC Systems in Mediterranean Climates. Energy Build. 2013, 60, 125–138. [Google Scholar] [CrossRef]
- Tabakov, P.; Bhutta, M. Policy Brief: A Critical Evaluation of Green Plans to Support Decarbonisation of NHS Trusts in England. 2025. Available online: https://www.bsms.ac.uk/_pdf/about/nhs-decarbonisation-of-trusts-final.pdf (accessed on 1 September 2025).
- Pantzartzis, E.; Price, A.; Edum Fotwe, F. Roadmap Layers and Processes: Resilient and Sustainable Care Facilities. Eng. Constr. Arch. Manag. 2019, 26, 1986–2007. [Google Scholar] [CrossRef]
- Bevere, D.; Faccilongo, N. Shaping the Future of Healthcare: Integrating Ecology and Digital Innovation. Sustainability 2024, 16, 3835. [Google Scholar] [CrossRef]
- Pascale, F.; Jones, K. Existing Hospitals’ Journey into a Sustainable and Climate-Resilient Future: Barriers and Opportunities for Estates and Facilities Management. Facilities 2025. [Google Scholar] [CrossRef]
- Butler, K. How energy benchmarking in healthcare facilities supports greenhouse gas emission reduction. Healthc. Manag. Forum 2023, 36, 199–206. [Google Scholar] [CrossRef]
- García-Sanz-Calcedo, J.; Gómez-Chaparro, M.; Sanchez-Barroso, G. Electrical and Thermal Energy in Private Hospitals: Consumption Indicators Focused on Healthcare Activity. Sustain. Cities Soc. 2019, 47, 101482. [Google Scholar] [CrossRef]
- Wang, T.; Li, X.; Liao, P.-C.; Fang, D. Building Energy Efficiency for Public Hospitals and Healthcare Facilities in China: Barriers and Drivers. Energy 2016, 103, 588–597. [Google Scholar] [CrossRef]
- Yousefli, Z.; Nasiri, F.; Moselhi, O. Healthcare Facilities Maintenance Management: A Literature Review. J. Facil. Manag. 2017, 15, 352–375. [Google Scholar] [CrossRef]
- Pedersen, J.M.; Jebaei, F.; Jradi, M. Assessment of Building Automation and Control Systems in Danish Healthcare Facilities in the COVID-19 Era. Appl. Sci. 2022, 12, 427. [Google Scholar] [CrossRef]
- Peng, Y.; Zhang, M.; Yu, F.; Xu, J.; Gao, S. Digital Twin Hospital Buildings: An Exemplary Case Study through Continuous Lifecycle Integration. Adv. Civ. Eng. 2020, 2020, 8846667. [Google Scholar] [CrossRef]
- Alhurayess, S.; Darwish, M.K. Analysis of Energy Management in Hospitals. In Proceedings of the 2012 47th International Universities Power Engineering Conference (UPEC), Uxbridge, UK, 4–7 September 2012; pp. 1–4. [Google Scholar] [CrossRef]
- Dion, H.; Evans, M. Strategic Frameworks for Sustainability and Corporate Governance in Healthcare Facilities; Approaches to Energy-Efficient Hospital Management. Benchmarking Int. J. 2023, 31, 353–390. [Google Scholar] [CrossRef]
- Marino, A.; Pariso, P. Digital Innovation Government: Organizational and Energy Analysis in Italian Hospitals. Entrep. Sustain. Issues 2023, 10, 214–230. [Google Scholar] [CrossRef]
- Jain, N.; Burman, E.; Stamp, S.; Shrubsole, C.; Bunn, R.; Oberman, T.; Barrett, E.; Aletta, F.; Kang, J.; Raynham, P.; et al. Building Performance Evaluation of a New Hospital Building in the UK: Balancing Indoor Environmental Quality and Energy Performance. Atmosphere 2021, 12, 115. [Google Scholar] [CrossRef]
- Alotaiby, R.; Krenyácz, E. Energy Efficiency in Healthcare Institutions. Soc. Econ. 2023, 45, 494–511. [Google Scholar] [CrossRef]
- Gaspari, J.; Fabbri, K.; Gabrielli, L. Retrofitting Hospitals: A Parametric Design Approach to Optimize Energy Efficiency. IOP Conf. Ser. Earth Environ. Sci. 2019, 290, 012130. [Google Scholar] [CrossRef]
- World Health Organization; Pan American Health Organization. Smart Hospitals Toolkit: Technical Guidance; WHO/PAHO: Geneva, Switzerland, 2017; ISBN 978-92-75-11939-6. [Google Scholar]
- Čongradac, V.; Prebiračević, B.; Jorgovanović, N.; Stanišić, D. Assessing the Energy Consumption for Heating and Cooling in Hospitals. Energy Build. 2012, 48, 146–154. [Google Scholar] [CrossRef]
- Gordo, E.; Campos, A.; Coelho, D. Energy efficiency in a hospital building case study: Hospitais da Universidade de Coimbra. In Proceedings of the 2011 3rd International Youth Conference on Energetics (IYCE), Leiria, Portugal, 7–9 July 2011; pp. 1–6. [Google Scholar]
- Zaza, P.N.; Sepetis, A.; Bagos, P.G. Prediction and Optimization of the Cost of Energy Resources in Greek Public Hospitals. Energies 2022, 15, 381. [Google Scholar] [CrossRef]
- Abd Rahman, N.M.; Lim, C.H.; Fazlizan, A. Optimizing the Energy Saving Potential of Public Hospital through a Systematic Approach for Green Building Certification in Malaysia. J. Build. Eng. 2021, 43, 103088. [Google Scholar] [CrossRef]
- Pina, E.A.; Lozano, M.A.; Serra, L.M. Opportunities for the Integration of Solar Thermal Heat, Photovoltaics and Biomass in a Brazilian Hospital. In Proceedings of the EuroSun 2018—12th International Conference on Solar Energy for Buildings and Industry, Rapperswil, Switzerland, 10–13 September 2018. [Google Scholar] [CrossRef]
- European Bank, Supporting Guide. Energy and Resource Efficiency in Hospitals and Health Care Facilities. 2021. Available online: https://e5p.eu/public/upload/media/Healthcare.pdf (accessed on 30 April 2025).
- Daramola, O.O. A Review of Combined Heat and Power Systems for Hospitals Applications. Int. J. Sci. Eng. Res. 2020, 11, 312–319. [Google Scholar]
- Kalina, J.; Pohl, W. Integration of Hospital’s Thermal Loads with Municipal District Heating System. 2023. Available online: https://ssrn.com/abstract=4561774 (accessed on 30 April 2025).
- Burch, H.; Anstey, M.H.; McGain, F. Renewable Energy Use in Australian Public Hospitals. Med. J. Aust. 2021, 215, 160. [Google Scholar] [CrossRef]
- Duraivelu, R.; Elumalai, N. Performance evaluation of a decentralized rooftop solar photovoltaic system with a heat recovery cooling unit. Environ. Sci. Pollut. Res. 2021, 28, 19351–19366. [Google Scholar] [CrossRef] [PubMed]
- Filho, W.L.; Luetz, J.M.; Thanekar, U.D.; Alzira, M.; Forrester, M. Climate-Friendly Healthcare: Reducing the Impacts of the Healthcare Sector on the World’s Climate. Sustain. Sci. 2024, 19, 1103–1109. [Google Scholar] [CrossRef]
- Kassem, Y.; Gökçekuş, H.; Güvensoy, A. Techno-Economic Feasibility of Grid-Connected Solar PV System at near East University Hospital, Northern Cyprus. Energies 2021, 14, 7627. [Google Scholar] [CrossRef]
- Lemence, A.L.G.; Tamayao, M.M. Energy consumption profile estimation and benefits of hybrid solar energy system adoption for rural health units in the Philippines. Renew. Energy 2021, 178, 651–668. [Google Scholar] [CrossRef]
- Beitelmal, W.H.; Okonkwo, P.C.; Al Housni, F.; Grami, S.; Emori, W.; Uzoma, P.C.; Das, B.K. Renewable energy as a source of electricity for Murzuq health clinic during COVID-19. MRS Energy Sustain. 2022, 9, 79–93. [Google Scholar] [CrossRef]
- Kuckartz, U. Qualitative Text Analysis: A Systematic Approach. In Compendium for Early Career Researchers in Mathematics Education. ICME-13 Monographs; Kaiser, G., Presmeg, N., Eds.; Springer: Berlin/Heidelberg, Germany, 2019; pp. 181–197. [Google Scholar] [CrossRef]
- NHS England and NHS Improvement. How to Produce a Green Plan: A Three-Year Strategy for Carbon Reduction for Your NHS Organisation or System; NHS England: London, UK, 2021; Available online: https://www.england.nhs.uk/greenernhs (accessed on 30 April 2025).
- Erlingsson, C.; Brysiewicz, P. A Hands-on Guide to Doing Content Analysis. Afr. J. Emerg. Med. 2017, 7, 93–99. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pascale, F.; Tabakov, P.; Bhutta, M.F. Decarbonizing the Healthcare Estate: Lessons Learned from NHS Trust Green Plans in England. Sustainability 2025, 17, 8375. https://doi.org/10.3390/su17188375
Pascale F, Tabakov P, Bhutta MF. Decarbonizing the Healthcare Estate: Lessons Learned from NHS Trust Green Plans in England. Sustainability. 2025; 17(18):8375. https://doi.org/10.3390/su17188375
Chicago/Turabian StylePascale, Federica, Petar Tabakov, and Mahmood F. Bhutta. 2025. "Decarbonizing the Healthcare Estate: Lessons Learned from NHS Trust Green Plans in England" Sustainability 17, no. 18: 8375. https://doi.org/10.3390/su17188375
APA StylePascale, F., Tabakov, P., & Bhutta, M. F. (2025). Decarbonizing the Healthcare Estate: Lessons Learned from NHS Trust Green Plans in England. Sustainability, 17(18), 8375. https://doi.org/10.3390/su17188375






