Impact of Airflow Rate and Supply-Exhaust Configuration on Displacement Ventilation in Airborne Pathogen Removal
Abstract
1. Introduction
2. Methodology
2.1. Governing Equations
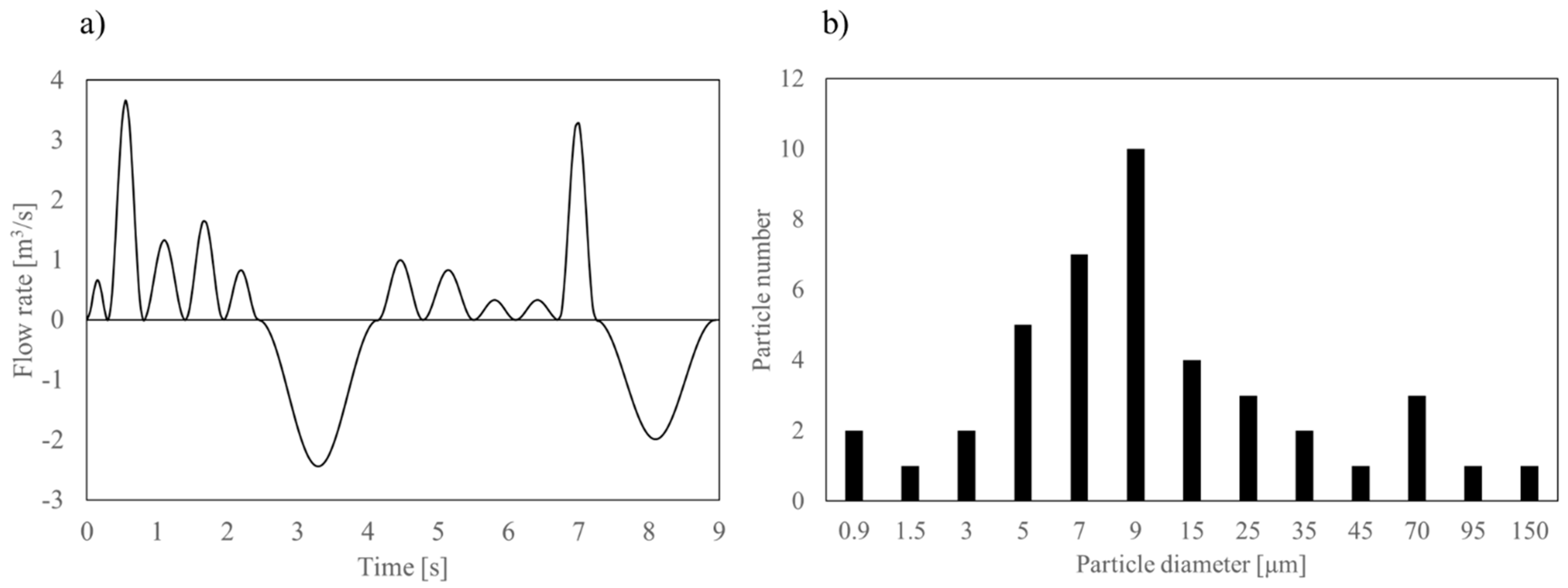
2.2. Droplet Model
2.3. Speaking Model and Exhaled Contaminants
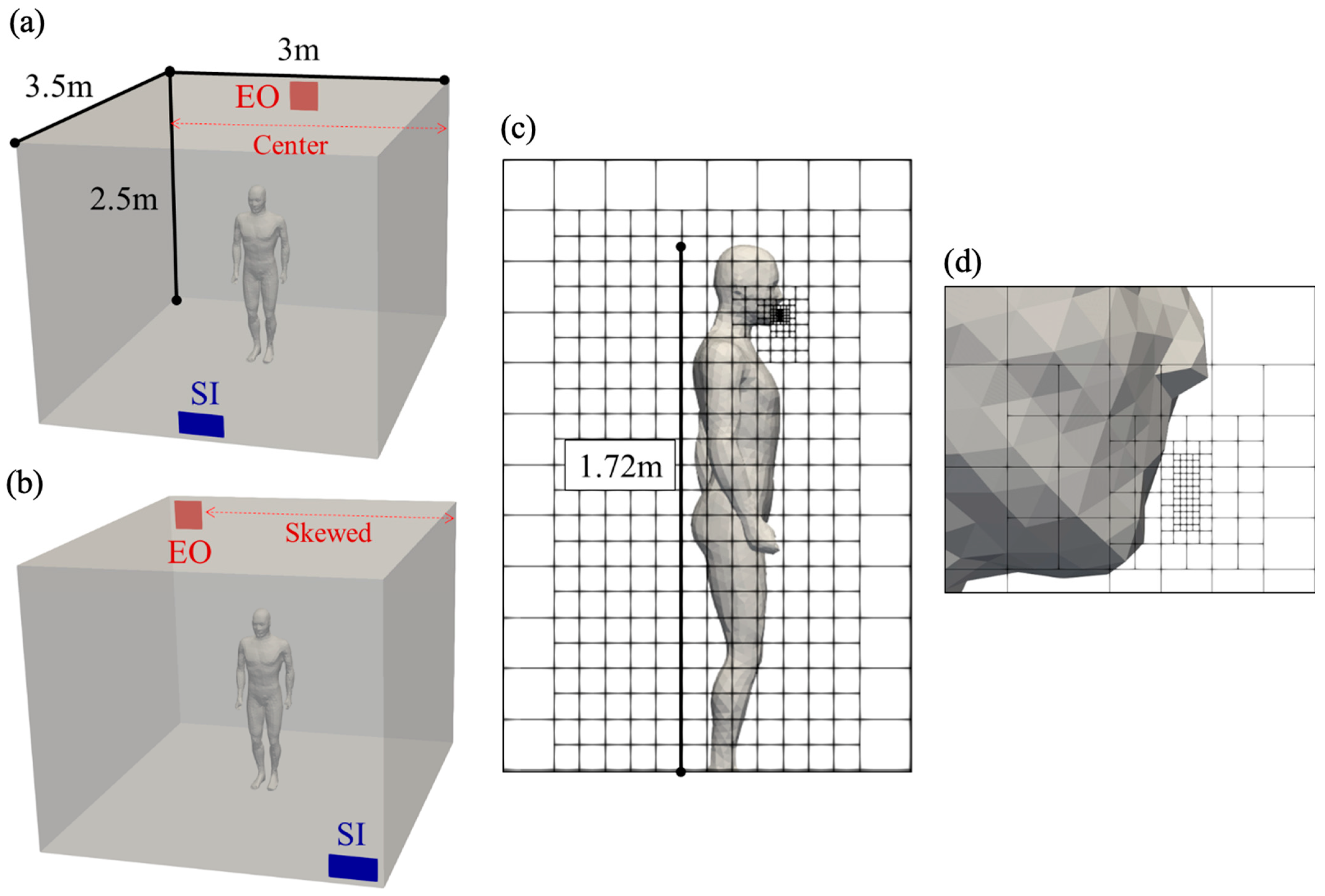
2.4. Case Set-Up
2.5. Mesh Design and Boundary Conditions
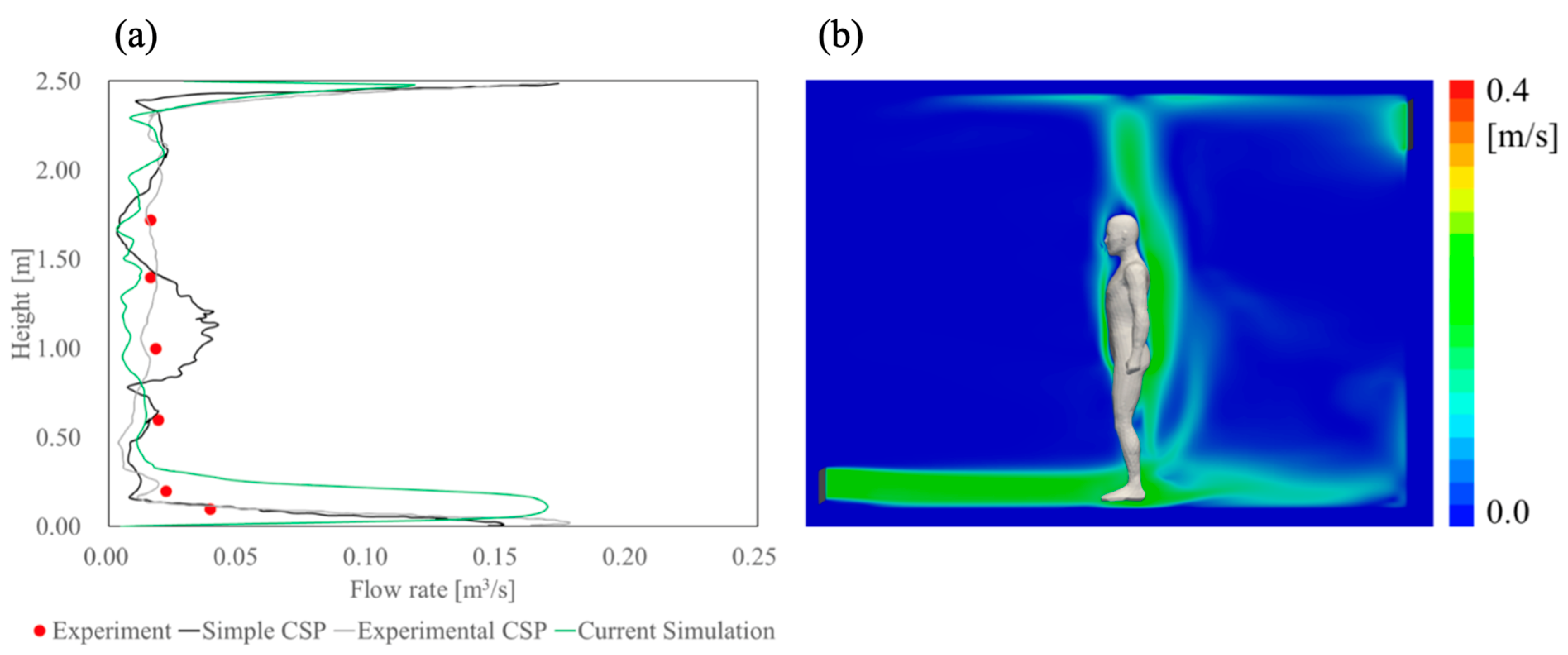
2.6. Validation
3. Results
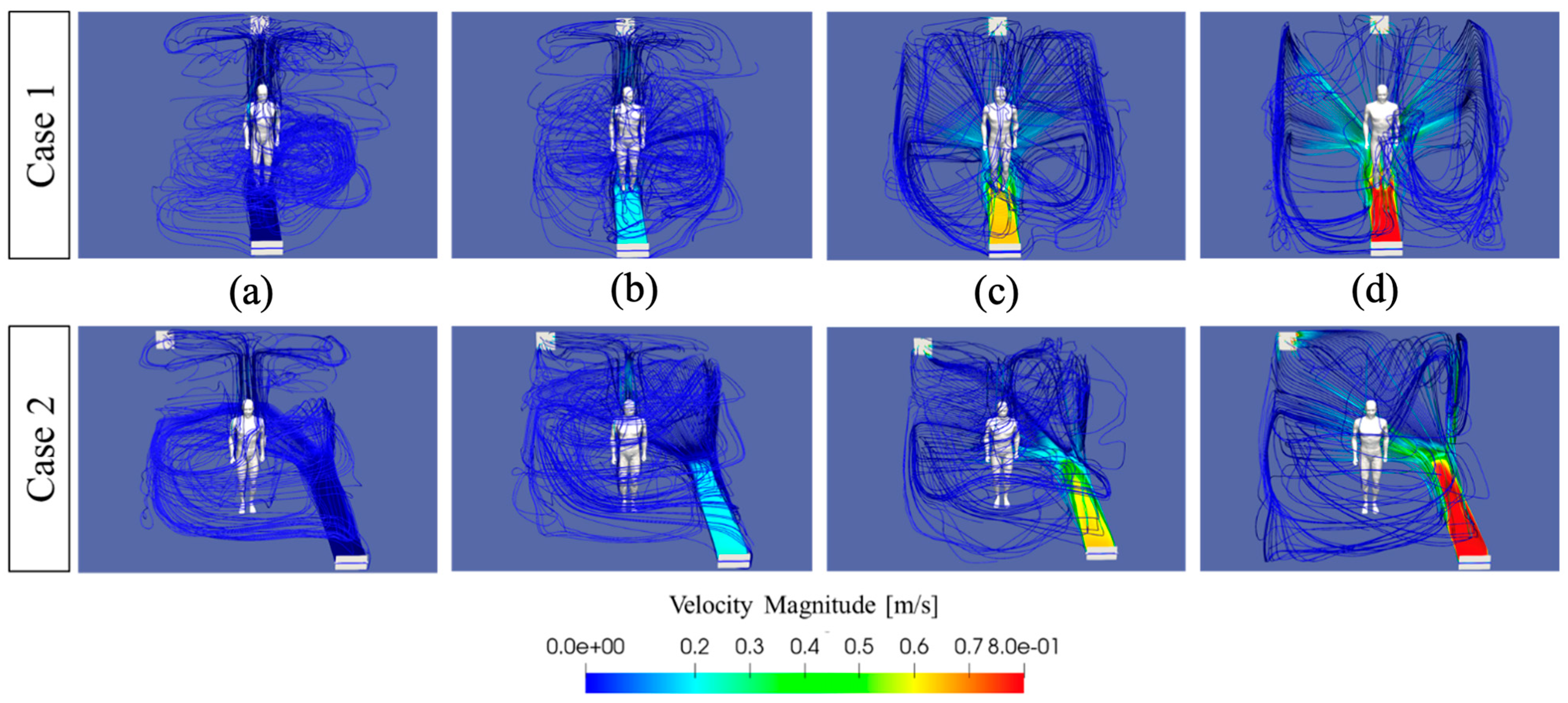
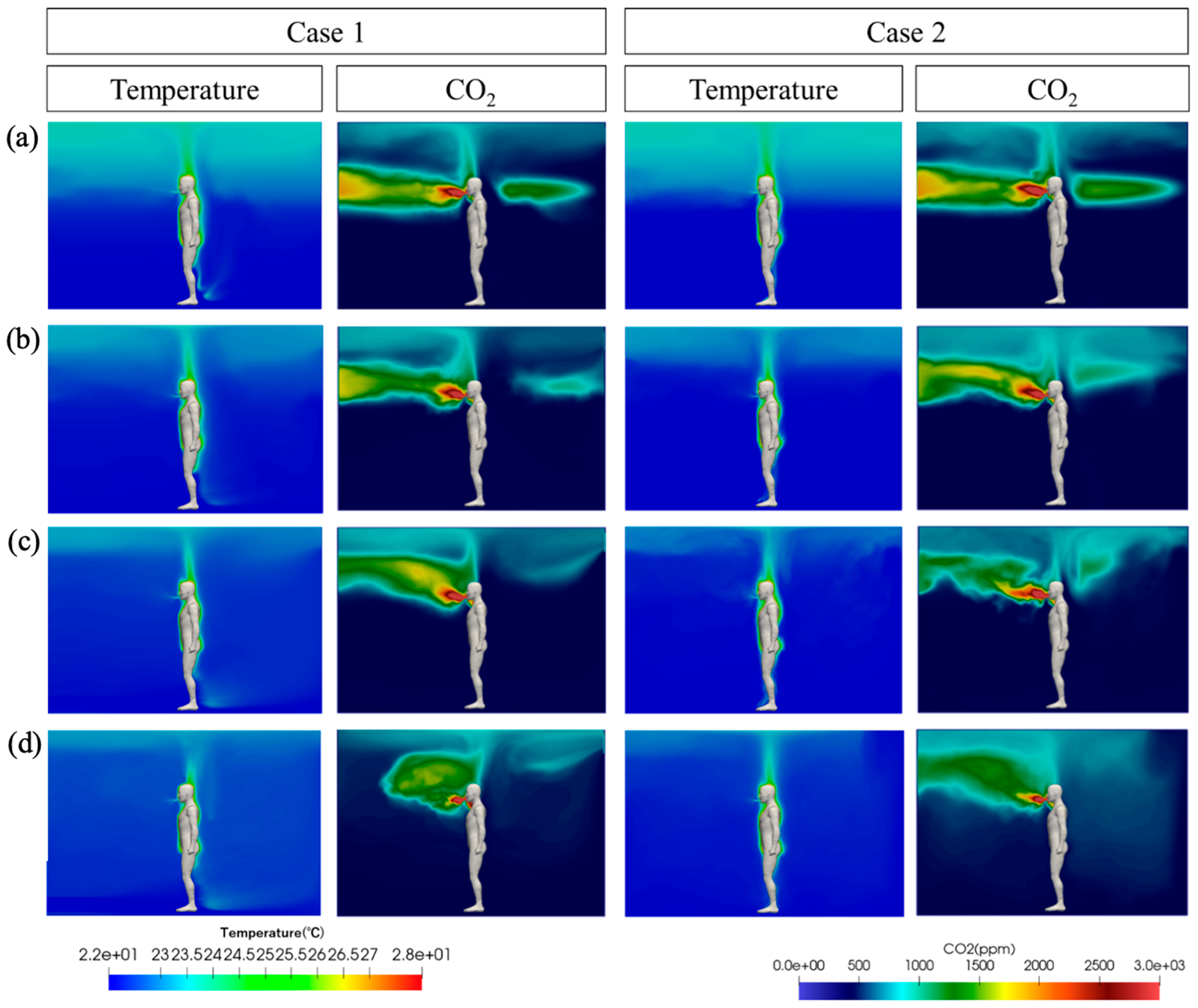
3.1. Indoor Flow, Temperature, and CO2 Fields
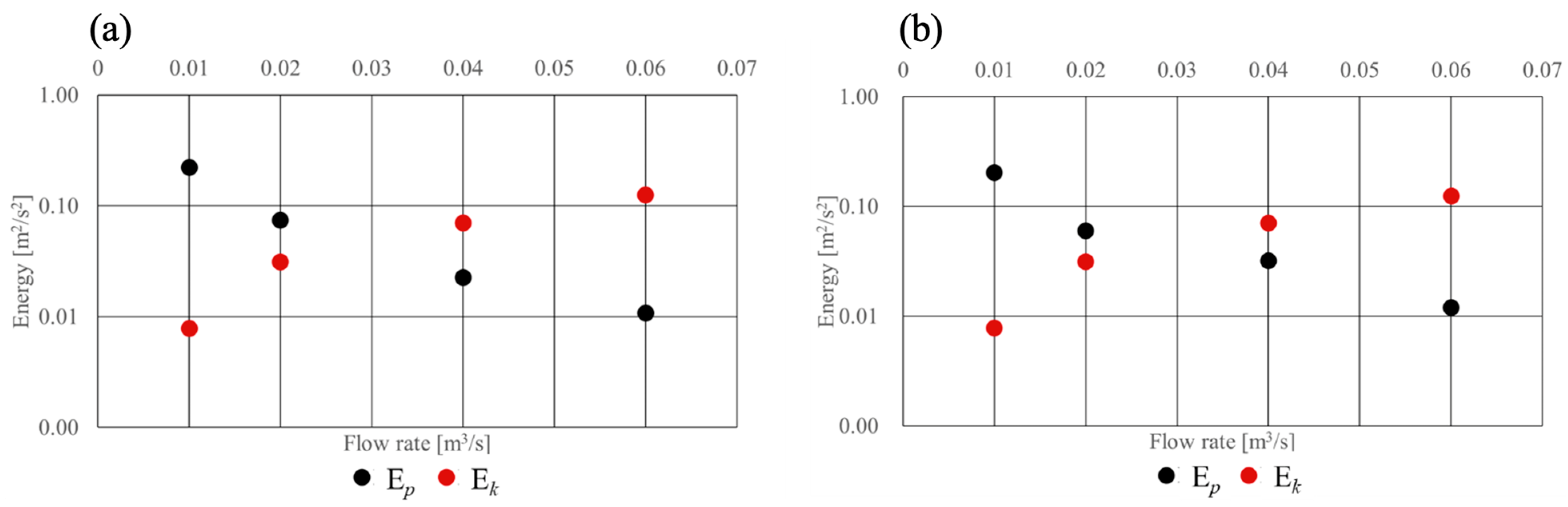
3.2. Transition from Displacement to Mixing Ventilation
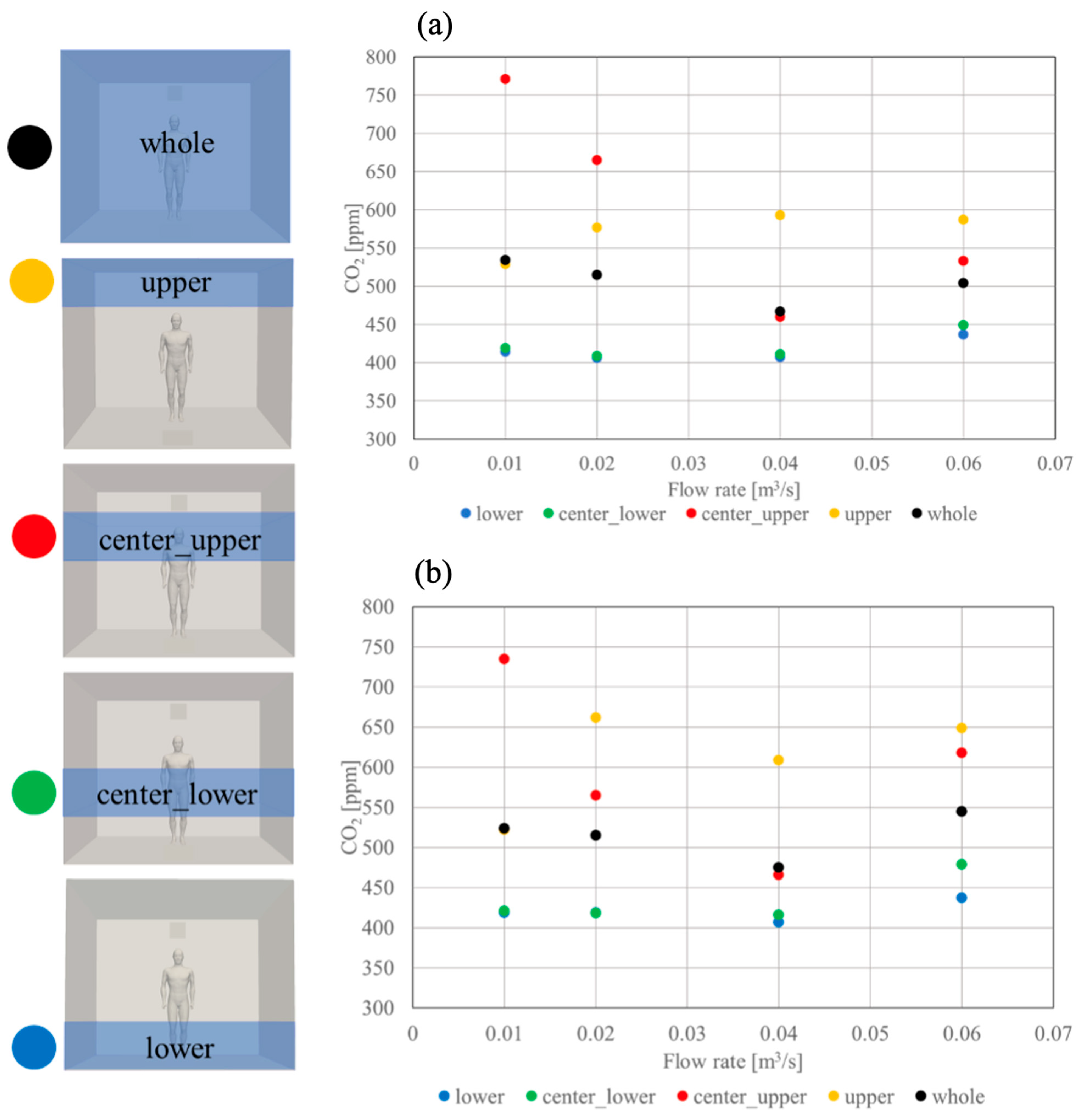
3.3. Impact of Increased Airflow Rate on Volume-Averaged CO2
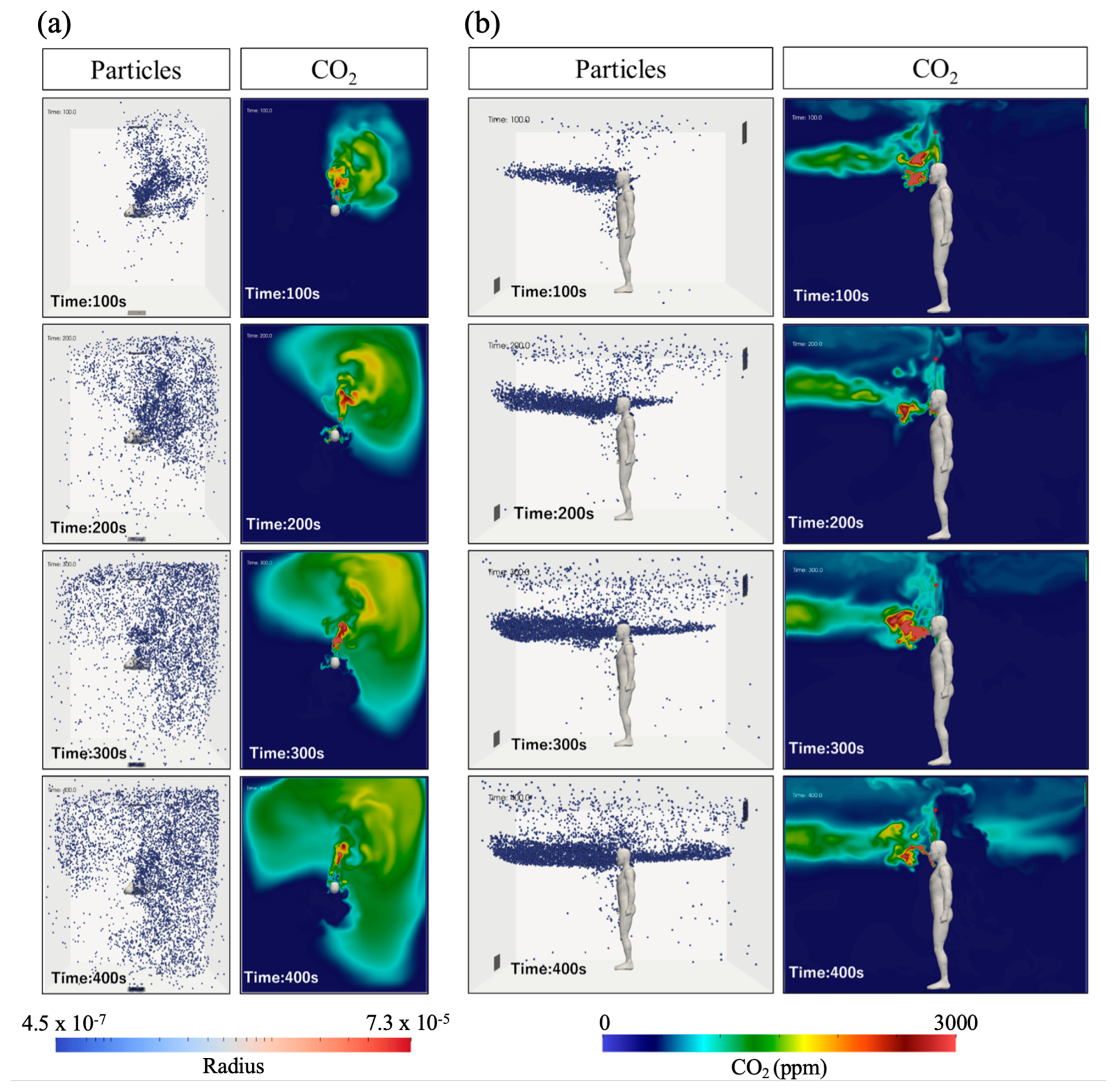
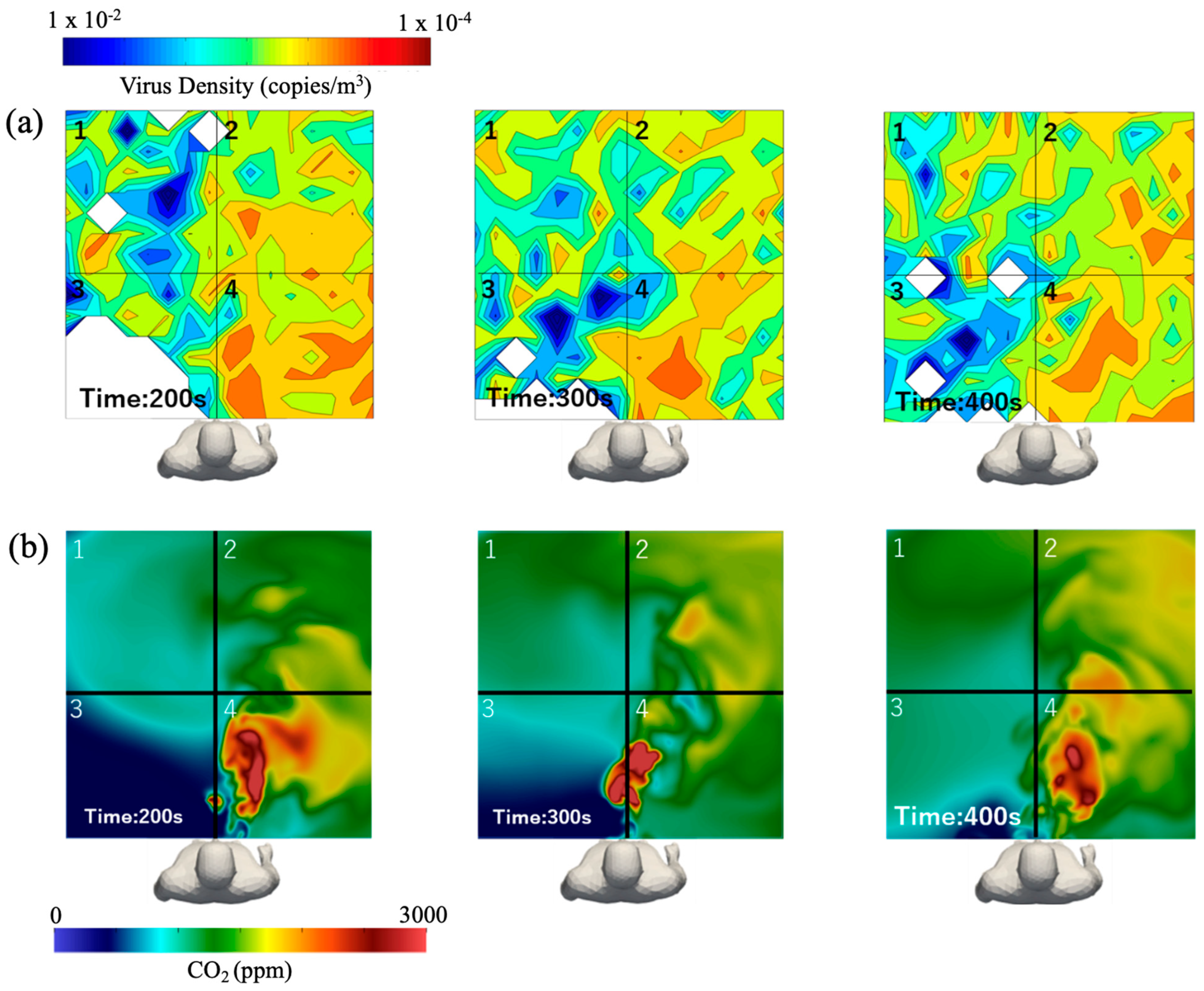
3.4. Respiratory CO2 Distribution Correlated to Respiratory Airborne Particles
3.5. Respiratory CO2 Distribution Correlated to Airborne Viral Density
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sze To, G.N.; Chao, C.Y.H. Review and comparison between the Wells–Riley and dose-response approaches to risk assessment of infectious respiratory diseases. Indoor Air 2010, 20, 2–16. [Google Scholar] [CrossRef]
- Domingo, J.L.; Marquès, M.; Rovira, J. Influence of airborne transmission of SARS-CoV-2 on COVID-19 pandemic. A review. Environ. Res. 2020, 188, 109861. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Zhang, N.; Wei, J.; Yen, H.L.; Li, Y. Short-range airborne route dominates exposure of respiratory infection during close contact. Build. Environ. 2020, 176, 106859. [Google Scholar] [CrossRef]
- Al-Rikabi, I.J.; Karam, J.; Alsaad, H.; Ghali, K.; Ghaddar, N.; Voelker, C. The impact of mechanical and natural ventilation modes on the spread of indoor airborne contaminants: A review. J. Build. Eng. 2024, 85, 108715. [Google Scholar] [CrossRef]
- Cao, G.; Awbi, H.; Yao, R.; Fan, Y.; Sirén, K.; Kosonen, R.; Zhang, J.J. A review of the performance of different ventilation and airflow distribution systems in buildings. Build. Environ. 2014, 73, 171–186. [Google Scholar] [CrossRef]
- Yang, B.; Melikov, A.K.; Kabanshi, A.; Zhang, C.; Bauman, F.S.; Cao, G.; Awbi, H.; Wigö, H.; Niu, J.; Cheong, K.W.D.; et al. A review of advanced air distribution methods—Theory, practice, limitations and solutions. Energy Build. 2019, 202, 109359. [Google Scholar] [CrossRef]
- Cheong, K.W.D.; Yu, W.J.; Tham, K.W.; Sekhar, S.C.; Kosonen, R. A study of perceived air quality and sick building syndrome in a field environment chamber served by displacement ventilation system in the tropics. Build. Environ. 2006, 41, 1530–1539. [Google Scholar] [CrossRef]
- Tomasi, R.; Krajčík, M.; Simone, A.; Olesen, B.W. Experimental evaluation of air distribution in mechanically ventilated residential rooms: Thermal comfort and ventilation effectiveness. Energy Build. 2013, 60, 28–37. [Google Scholar] [CrossRef]
- Nielsen, P.V. Velocity distribution in a room ventilated by displacement ventilation and wall-mounted air terminal devices. Energy Build. 2000, 31, 179–187. [Google Scholar] [CrossRef]
- Zhang, Y.; Shankar, S.N.; Vass, W.B.; Lednicky, J.A.; Fan, Z.H.; Agdas, D.; Makuch, R.; Wu, C.-Y. Air Change Rate and SARS-CoV-2 Exposure in Hospitals and Residences: A Meta-Analysis. Aerosol. Sci. Technol. 2024, 58, 217–243. [Google Scholar] [CrossRef]
- Ding, J.; Yu, C.W.; Cao, S.-J. HVAC systems for environmental control to minimize the COVID-19 infection. Indoor Built Environ. 2020, 29, 1195–1201. [Google Scholar] [CrossRef]
- Li, Y.; Leung, G.M.; Tang, J.W.; Yang, X.; Chao, C.Y.H.; Lin, J.Z.; Lu, J.W.; Nielsen, P.V.; Niu, J.; Qian, H.; et al. Role of ventilation in airborne transmission of infectious agents in the built environment—A multidisciplinary systematic review. Indoor Air 2007, 17, 2–18. [Google Scholar] [CrossRef]
- Morawska, L.; Afshari, A.; Bae, G.N.; Buonanno, G.; Chao, C.Y.H.; Hänninen, O.; Hofmann, W.; Isaxon, C.; Jayaratne, E.R.; Pasanen, P.; et al. Indoor aerosols: From personal exposure to risk assessment. Indoor Air 2013, 23, 462–487. [Google Scholar] [CrossRef] [PubMed]
- Tellier, R. Review of aerosol transmission of influenza A virus. Emerg. Infect. Dis. 2006, 12, 1657–1662. [Google Scholar] [CrossRef]
- Nicas, M.; Nazaroff, W.W.; Hubbard, A. Toward understanding the risk of secondary airborne infection: Emission of respirable pathogens. J. Occup. Environ. Hyg. 2005, 2, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Buonanno, G.; Stabile, L.; Morawska, L. Estimation of airborne viral emission: Quanta emission rate of SARS-CoV-2 for infection risk assessment. Environ. Int. 2020, 141, 105794. [Google Scholar] [CrossRef]
- Dietz, L.; Horve, P.F.; Coil, D.A.; Fretz, M.; Eisen, J.A.; Van Den Wymelenberg, K. 2019 Novel Coronavirus (COVID-19) Pandemic: Built Environment Considerations to Reduce Transmission. mSystems 2020, 5, e00245-20. [Google Scholar] [CrossRef]
- Park, S.; Song, D. CO2 concentration as an indicator of indoor ventilation performance to control airborne transmission of SARS-CoV-2. J. Infect. Public Health 2023, 16, 1037–1044. [Google Scholar] [CrossRef]
- Di Gilio, A.; Palmisani, J.; Pulimeno, M.; Cerino, F.; Cacace, M.; Miani, A.; de Gennaro, G. CO2 concentration monitoring inside educational buildings as a strategic tool to reduce the risk of Sars-CoV-2 airborne transmission. Environ. Res. 2021, 202, 111560. [Google Scholar] [CrossRef]
- Rudnick, S.N.; Milton, D.K. Risk of indoor airborne infection transmission estimated from carbon dioxide concentration. Indoor Air 2003, 13, 237–245. [Google Scholar] [CrossRef] [PubMed]
- van Hooff, T.; Blocken, B.; Tominaga, Y. On the accuracy of CFD simulations of cross-ventilation flows for a generic isolated building: Comparison of RANS, LES and experiments. Build. Environ. 2017, 114, 148–165. [Google Scholar] [CrossRef]
- Bale, R.; Li, C.; Fukudome, H.; Yumino, S.; Iida, A.; Tsubokura, M. Characterizing infection risk in a restaurant environment due to airborne diseases using discrete droplet dispersion simulations. Heliyon 2023, 9, e20540. [Google Scholar] [CrossRef]
- Jansson, N.; Bale, R.; Onishi, K.; Tsubokura, M. CUBE: A scalable framework for large-scale industrial simulations. Int. J. High Perform. Comput. Appl. 2019, 33, 678–698. [Google Scholar] [CrossRef]
- Bale, R.; Wang, W.H.; Li, C.-G.; Onishi, K.; Uchida, K.; Fujimoto, H.; Kurose, R.; Tsubokura, M. A Scalable Framework for Numerical Simulation of Combustion in Internal Combustion Engines. In Proceedings of the Platform for Advanced Scientific Computing Conference, in PASC 20, New York, NY, USA, 5–8 July 2021; Association for Computing Machinery: New York, NY, USA, 2020. [Google Scholar] [CrossRef]
- Grinstein, F.F.; Margolin, L.G.; Rider, W.J. Implicit Large Eddy Simulation—Computing Turbulent Fluid Dynamics, 1st ed.; Cambridge University Press: Cambridge, UK, 2007. [Google Scholar]
- Roe, P.L. Approximate Riemann solvers, parameter vectors, and difference schemes. J. Comput. Phys. 1981, 43, 357–372. [Google Scholar] [CrossRef]
- Mofakham, A.A.; Ahmadi, G. On random walk models for simulation of particle-laden turbulent flows. Int. J. Multiph. Flow 2020, 122, 103157. [Google Scholar] [CrossRef]
- Ranz, W.E. Evaporation from drops: Part I. Chem. Eng. Prog. 1952, 48, 141–146. [Google Scholar]
- Ranz, W.E. Evaporation from drops: Part II. Chem. Eng. Prog. 1952, 48, 173–180. [Google Scholar]
- Nakamura, M.; Nishioka, D.; Hayashi, J.; Akamatsu, F. Soot formation, spray characteristics, and structure of jet spray flames under high pressure. Combust. Flame 2011, 158, 1615–1623. [Google Scholar] [CrossRef]
- Miller, R.S.; Harstad, K.; Bellan, J. Evaluation of equilibrium and non-equilibrium evaporation models for many-droplet gas-liquid flow simulations. Int. J. Multiph. Flow 1998, 24, 1025–1055. [Google Scholar] [CrossRef]
- Bale, R.; Li, C.-G.; Yamakawa, M.; Iida, A.; Kurose, R.; Tsubokura, M. Simulation of Droplet Dispersion in COVID-19 Type Pandemics on Fugaku. In Proceedings of the Platform for Advanced Scientific Computing Conference, in PASC 21, New York, NY, USA, 5–9 July 2021; Association for Computing Machinery: New York, NY, USA, 2021. [Google Scholar] [CrossRef]
- Bale, R.; Iida, A.; Yamakawa, M.; Li, C.-G.; Tsubokura, M. Quantifying the COVID19 infection risk due to droplet/aerosol inhalation. Sci. Rep. 2022, 12, 11186. [Google Scholar] [CrossRef]
- Gupta, J.K.; Lin, C.-H.; Chen, Q. Characterizing exhaled airflow from breathing and talking. Indoor Air 2010, 20, 31–39. [Google Scholar] [CrossRef]
- Nielsen, P.V. Displacement Ventilation. In Rehva Guidebook; no. 23; Federation of European Heating and Air-Conditioning Associations: Brussels, Belgium, 2017. [Google Scholar]
- Bale, R.; Patankar, N.A.; Jansson, N.; Onishi, K.; Tsubokura, M. Stencil Penalty approach based constraint immersed boundary method. Comput. Fluids 2020, 200, 104457. [Google Scholar] [CrossRef]
- Mittal, R.; Iaccarino, G. Immersed Boundary Methods. Annu. Rev. Fluid Mech. 2005, 37, 239–261. [Google Scholar] [CrossRef]
- Li, C.-G.; Tsubokura, M.; Bale, R. Framework for simulation of natural convection in practical applications. Int. Commun. Heat Mass Transf. 2016, 75, 52–58. [Google Scholar] [CrossRef]
- Nakahashi, K.; Kim, L. Building-Cube Method for Large-Scale, High Resolution Flow Computations. In Proceedings of the 42nd AIAA Aerospace Sciences Meeting and Exhibit, Reno, NV, USA, 5–8 January 2004; American Institute of Aeronautics and Astronautics: Reston, VA, USA, 2004. [Google Scholar] [CrossRef]
- ANSI/ASHRAE Standard 62.I-2022; Ventilation and Acceptable Indoor Air Quality. ASHRAE: Atlanta, GA, USA, 2022. Available online: https://www.ashrae.org/technical-resources/bookstore/standards-62-1-62-2 (accessed on 7 September 2025).
- Deevy, M. CFD Modelling of the Benchmark Displacement Ventilation Test Case; Health and Safety Laboratory: Derbyshire, UK, 2006. [Google Scholar]
- Yoo, S.-J.; Ito, K. Validation, verification, and quality control of computational fluid dynamics analysis for indoor environments using a computer-simulated person with respiratory tract. Jpn. Archit. Rev. 2022, 5, 714–727. [Google Scholar] [CrossRef]
- Nielsen, P.V.; Murakami, S.; Kato, S.; Topp, C.N.; Yang, J.H. Benchmark Test for a Computer Simulated Person; Aalborg University: Aalborg, Denmark, 2003. [Google Scholar]
- Yuan, X.; Chen, Q.; Glicksman, L.; Hu, Y.; Yang, X. Measurements and computations of room airflow with displacement ventilation. ASHRAE Trans. 1999, 105, 340–352. [Google Scholar]
- Li, Y.; Nielsen, P.V.; Sandberg, M. Displacement ventilation in hospital environments. ASHRAE J. 2011, 53, 86–88. [Google Scholar]
- Yang, R.; Ng, C.S.; Chong, K.L.; Verzicco, R.; Lohse, D. Do increased flow rates in displacement ventilation always lead to better results? J. Fluid Mech. 2022, 932, A3. [Google Scholar] [CrossRef]
- Yang, J.; Sekhar, C.; Cheong, D.K.W.; Raphael, B. A time-based analysis of the personalized exhaust system for airborne infection control in healthcare settings. Sci. Technol. Built Environ. 2015, 21, 172–178. [Google Scholar] [CrossRef]
- Villafruela, J.M.; Olmedo, I.; San José, J.F. Influence of human breathing modes on airborne cross infection risk. Build. Environ. 2016, 106, 340–351. [Google Scholar] [CrossRef]
- Ai, Z.; Hashimoto, K.; Melikov, A.K. Influence of pulmonary ventilation rate and breathing cycle period on the risk of cross-infection. Indoor Air 2019, 29, 993–1004. [Google Scholar] [CrossRef] [PubMed]
- Kappelt, N.; Russell, H.S.; Kwiatkowski, S.; Afshari, A.; Johnson, M.S. Correlation of Respiratory Aerosols and Metabolic Carbon Dioxide. Sustainability 2021, 13, 12203. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bale, R.; Murga, A.; Yamamoto, H.; Tsubokura, M. Impact of Airflow Rate and Supply-Exhaust Configuration on Displacement Ventilation in Airborne Pathogen Removal. Sustainability 2025, 17, 8193. https://doi.org/10.3390/su17188193
Bale R, Murga A, Yamamoto H, Tsubokura M. Impact of Airflow Rate and Supply-Exhaust Configuration on Displacement Ventilation in Airborne Pathogen Removal. Sustainability. 2025; 17(18):8193. https://doi.org/10.3390/su17188193
Chicago/Turabian StyleBale, Rahul, Alicia Murga, Haruhiro Yamamoto, and Makoto Tsubokura. 2025. "Impact of Airflow Rate and Supply-Exhaust Configuration on Displacement Ventilation in Airborne Pathogen Removal" Sustainability 17, no. 18: 8193. https://doi.org/10.3390/su17188193
APA StyleBale, R., Murga, A., Yamamoto, H., & Tsubokura, M. (2025). Impact of Airflow Rate and Supply-Exhaust Configuration on Displacement Ventilation in Airborne Pathogen Removal. Sustainability, 17(18), 8193. https://doi.org/10.3390/su17188193





