Can AI and Urban Design Optimization Mitigate Cardiovascular Risks Amid Rapid Urbanization? Unveiling the Impact of Environmental Stressors on Health Resilience
Abstract
1. Introduction
| Literature | Year | Key Thematic Interconnections | Focus Area | Core Insights and Study Contributions | Gaps/Opportunities |
|---|---|---|---|---|---|
| [30] [31] [32] [33] [34] [35] [36] [37] [38] [39] [40] | 2024 2024 2024 2024 2024 2024 2023 2023 2021 2024 2020 | Urbanization ↔ Health | The interplay between urban growth and public health challenges. | Identifies the multifaceted impacts of urbanization on physical and mental health, particularly chronic diseases like hypertension. | Limited exploration of holistic frameworks to mitigate urban stressors at a population scale. |
| [41] [42] [43] [44] [45] [46] [47] [48] [49] | 2024 2024 2024 2024 2024 2023 2021 2021 2020 | Traffic ↔ Pollution | The health impacts of air pollution, traffic emissions, and exposure to pollutants. | Establishes a strong link between traffic-related pollution and respiratory/cardiovascular diseases. | Synergistic effects with other stressors like noise and heat remain underexplored. |
| [50] [10] [51] [52] [53] [54] [55] [56] [57] | 2024 2024 2024 2024 2023 2022 2021 2021 2020 | Environmental ↔ Stressors | Synergistic impacts of noise, air pollution, and urban heat islands (UHIs) on chronic health conditions. | Highlights cumulative stressor impacts on cardiovascular health, emphasizing environmental determinants of hypertension. | Lack of integrated studies combining multiple environmental stressors and their systemic effects. |
| [44] [18] [12] [58] [59] [60] | 2024 2024 2023 2023 2021 2021 | Stressors ↔ Hypertension | The mechanistic links between chronic stressors and hypertension-related health risks. | Highlights pathways such as oxidative stress and inflammation linking environmental factors to hypertension. | Few interdisciplinary studies bridging environmental, biological, and societal perspectives. |
| [61] [62] [63] [64] [65] [66] | 2024 2024 2024 2024 2024 2024 | Traffic ↔ Noise ↔ Stress | Psychological impacts of noise pollution and traffic-related stress on mental health. | Explores the rise in mental health disorders (e.g., anxiety, depression) caused by urban noise exposure. | Sparse data on population-level interventions to address traffic noise and associated stressors. |
| [20] [21] [22] [23] [24] [25] [28] [29] | 2024 2024 2024 2024 2024 2024 2024 2021 | Green Spaces ↔ Health | The role of green infrastructure (parks, roofs, walls) in mitigating urban stressors and promoting well-being. | Quantifies health benefits such as reduced urban heat, improved air quality, and enhanced physical and mental health. | Limited adoption of AI-driven models to optimize green space placement for maximum impact. |
| [67] [68] [69] [70] [71] [72] [73] | 2024 2024 2024 2024 2024 2024 2024 | Optimization ↔ Algorithmic Approaches | Use of AI, machine learning, and predictive modeling to design healthier urban environments. | Pioneers data-driven approaches to optimize urban layout, infrastructure placement, and green spaces to reduce health risks. | Underdeveloped integration of AI with traditional urban planning methodologies. |
| [74] [75] [76] [77] [78] [79] [79] | 2024 2024 2024 2024 2023 2022 2021 | Architectural (Arc) ↔ Intelligence (AI) | ArcAI plays an important role in improving the efficiency of and efficacy of urban design processes. | AI-based solutions optimize urban design to address chronic health risks through improved environmental planning. | Few real-world applications of ArcAI for urban health risks; further research is needed on long-term impacts. |
| [15] [80] [81] [82] [83] [84] [85] | 2024 2024 2023 2023 2022 2021 2021 | Environmental Performance ↔ Design | The integration of environmental performance metrics into urban and architectural design strategies. | Provides a bridge between health-conscious urban design and measurable sustainability outcomes. | Insufficient frameworks linking environmental performance with public health outcomes in urban contexts. |
2. Methodology
2.1. Design and Framework
2.2. Research Questions
- What are the primary environmental stressors linked to urbanization, and how do they fuel chronic illnesses, health disorders, and cardiovascular diseases?Despite widespread acknowledgment in the literature of urbanization’s health impacts, systematic analyses remain scarce on how specific stressors—such as air pollution, noise, and extreme temperatures—translate into public health burdens.
- How do urban stressors such as air pollution, noise, and climate-induced heat extremes drive hypertension and cardiovascular incidents?A critical gap remains in understanding the mechanisms by which urban stressors contribute to pathogenesis and disease evolution, particularly through their interaction in complex urban environments.
- To what extent can AI-driven design, optimization algorithms, and performance-based planning mitigate cardiovascular risks from urban environmental stressors?Despite growing interest, the real-world efficacy and applicability of these advanced technologies in reducing urban health risks remain underexplored and poorly evidenced in the literature.
- How do interdisciplinary approaches in urban design and public health converge to mitigate the adverse health effects of environmental stressors, and what scalability do these strategies possess in rapidly urbanizing regions?A critical gap in the literature exists on the scalability and interdisciplinary integration of urban design, planning, and public health interventions. While studies have explored individual interventions, synergies, particularly in rapid urbanization, remain underexplored.
2.3. Search Strategy
2.4. Inclusion and Exclusion Criteria
- Inclusion Criteria:
- -
- Peer-reviewed English publications (1942–2025).
- -
- Studies on environmental stressors (e.g., air pollution, noise, and climate change) and their impact on cardiovascular health, focusing on hypertension and stroke.
- -
- Research integrating AI-driven design, sustainable urban planning, and public health strategies to mitigate health risks.
- -
- Interdisciplinary studies bridging urban health, environmental science, and architectural design, emphasizing the health implications of urbanization.
- Exclusion Criteria:
- -
- Non-urban studies or those lacking clear links between environmental stressors and health outcomes.
- -
- Publications without empirical data or failed causal/correlational evidence between stressors and cardiovascular health.
2.5. Data Extraction and Synthesis
2.6. Visualizing Network and Bibliometric Trends with VOSviewer and VS Code
2.7. Rigorous Overview of the Two-Phase Methodology
2.7.1. Phase 1: Mixed Methods Systematic Review (MMSR)
- Urbanization ↔ Health: Uncovering how urbanization alters environmental conditions and impacts public health, particularly cardiovascular health risks (↔ denotes an interconnected relationship).
- Traffic ↔ Pollution: Investigating the role of traffic-related pollutants (e.g., particulate matter, nitrogen oxides, carbon monoxide, and noise) in increasing long-term cardiovascular health risks.
- Environmental Stressors ↔ Hypertension: Analyzing the contribution of environmental stressors (air pollution, noise, and urban heat islands) to the onset and progression of hypertension.
- Traffic Noise ↔ Chronic Stress ↔ Cardiovascular Disease: Exploring the pathways through which traffic noise leads to chronic stress, which in turn contributes to cardiovascular diseases.
- Green Spaces ↔ Health: Assessing the potential of green spaces (e.g., parks, urban forests) in mitigating the adverse health effects of environmental stressors.
- Optimization ↔ Algorithmic Approaches: Reviewing AI-driven approaches that optimize urban design for health, with a focus on improving air quality, noise reduction, and the availability of green spaces.
- Architectural Intelligence ↔ Public Health: Exploring how AI-augmented architectural intelligence can integrate into urban planning to reduce environmental stressors and enhance public health.
- Environmental Performance ↔ Sustainable Design: Exploring the role of sustainable building techniques, smart city technologies, and resilient design principles in mitigating cardiovascular health risks.
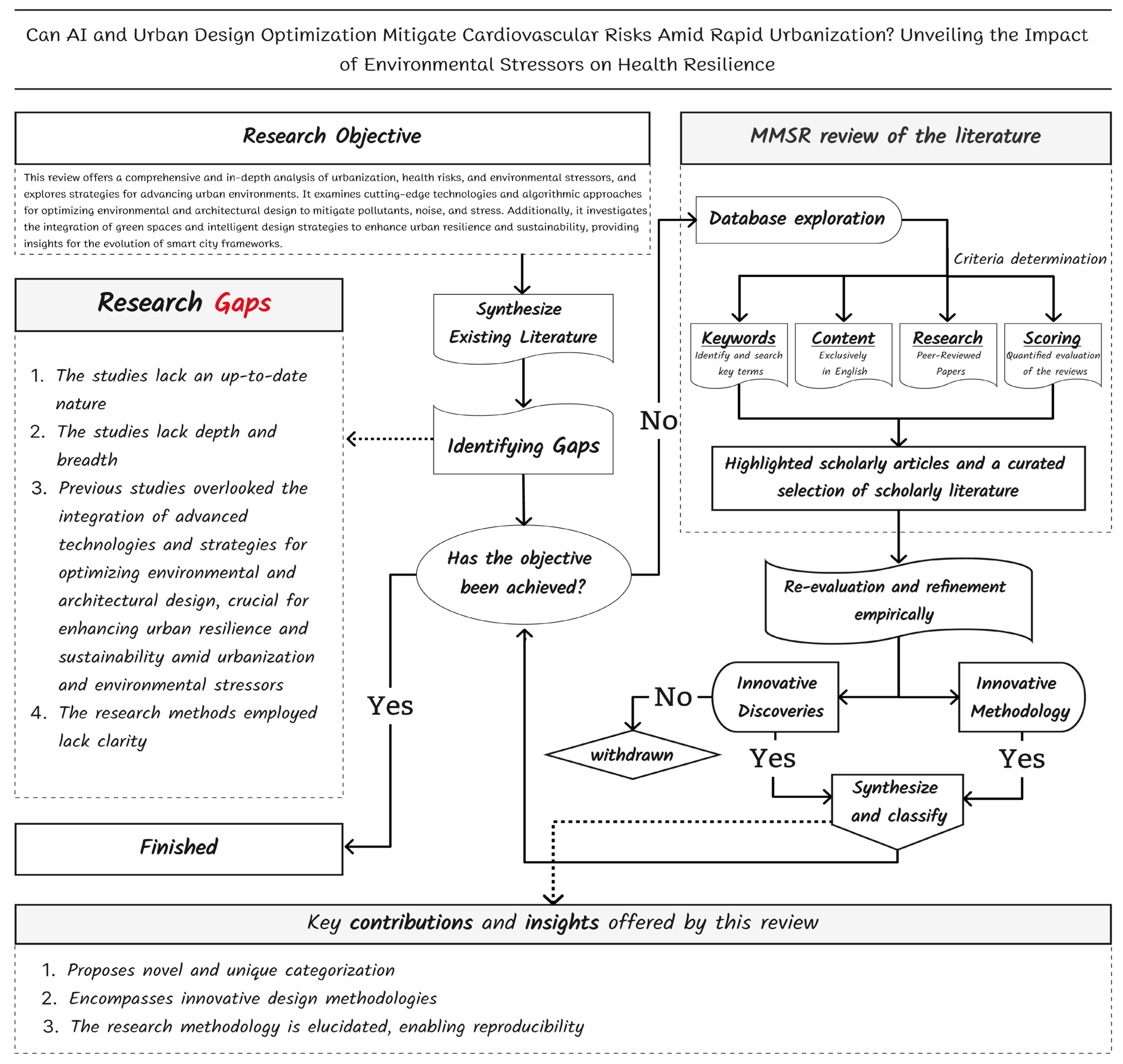
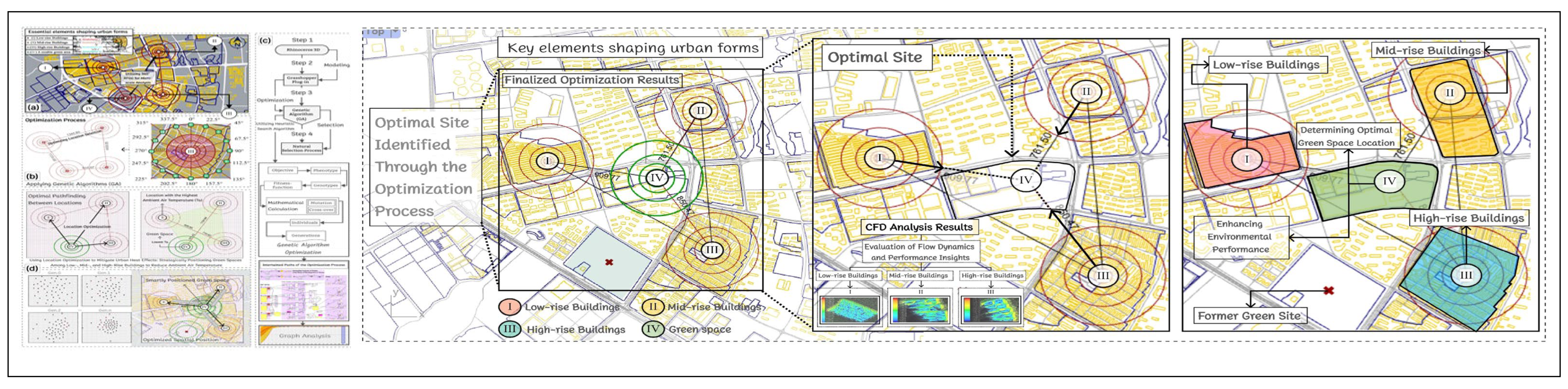
2.7.2. Phase 2: Empirical Data Collection and Analysis (EDCA)
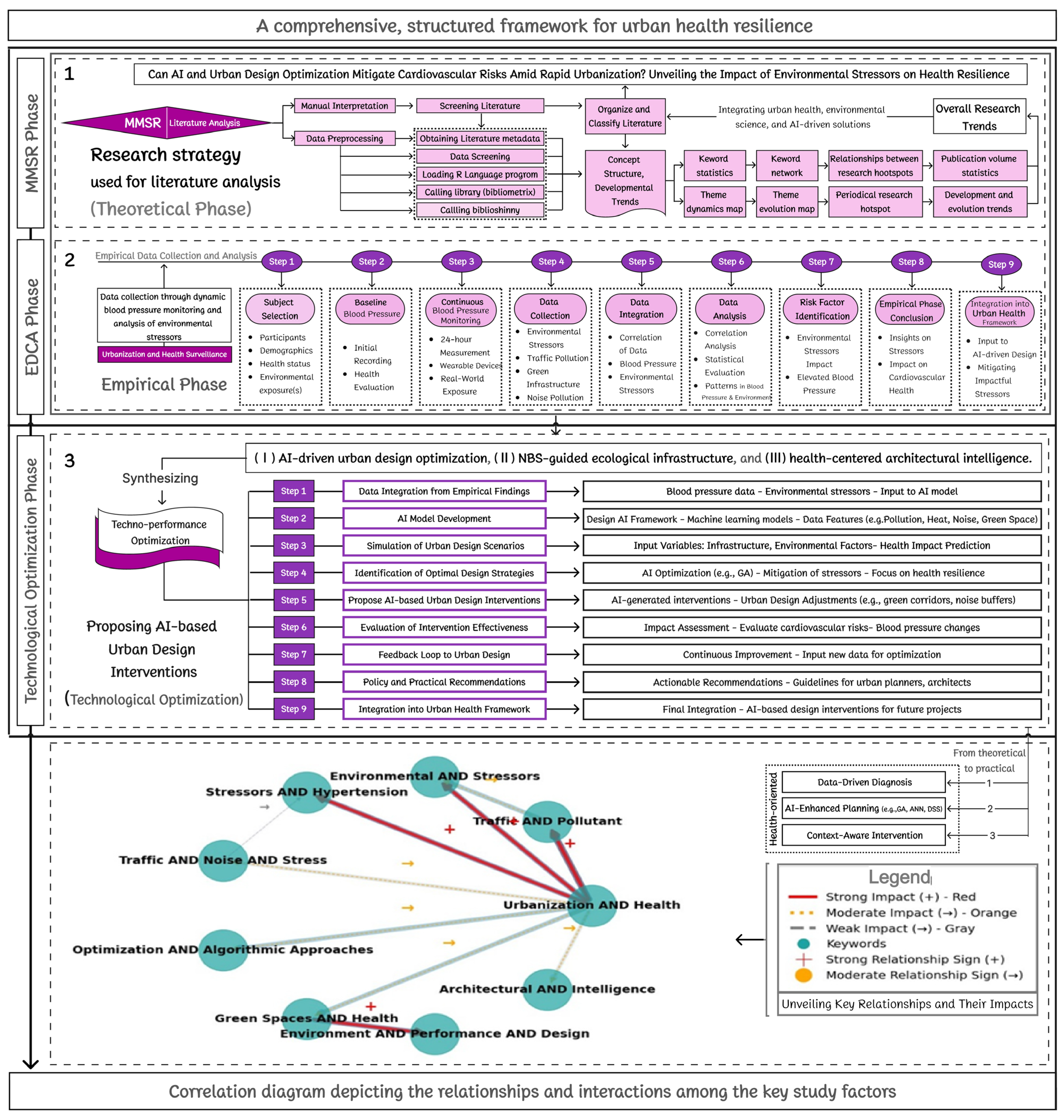
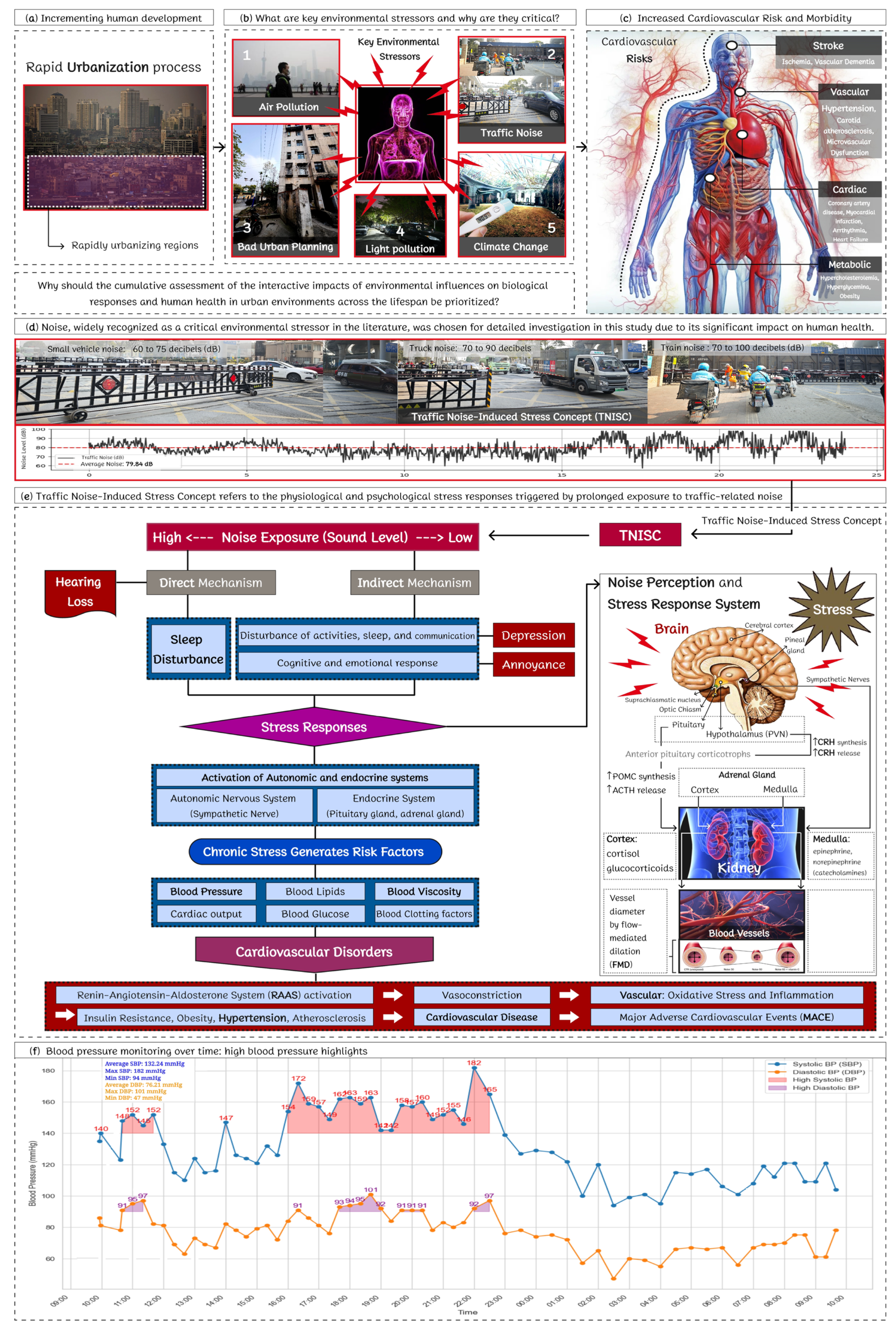
- (1)
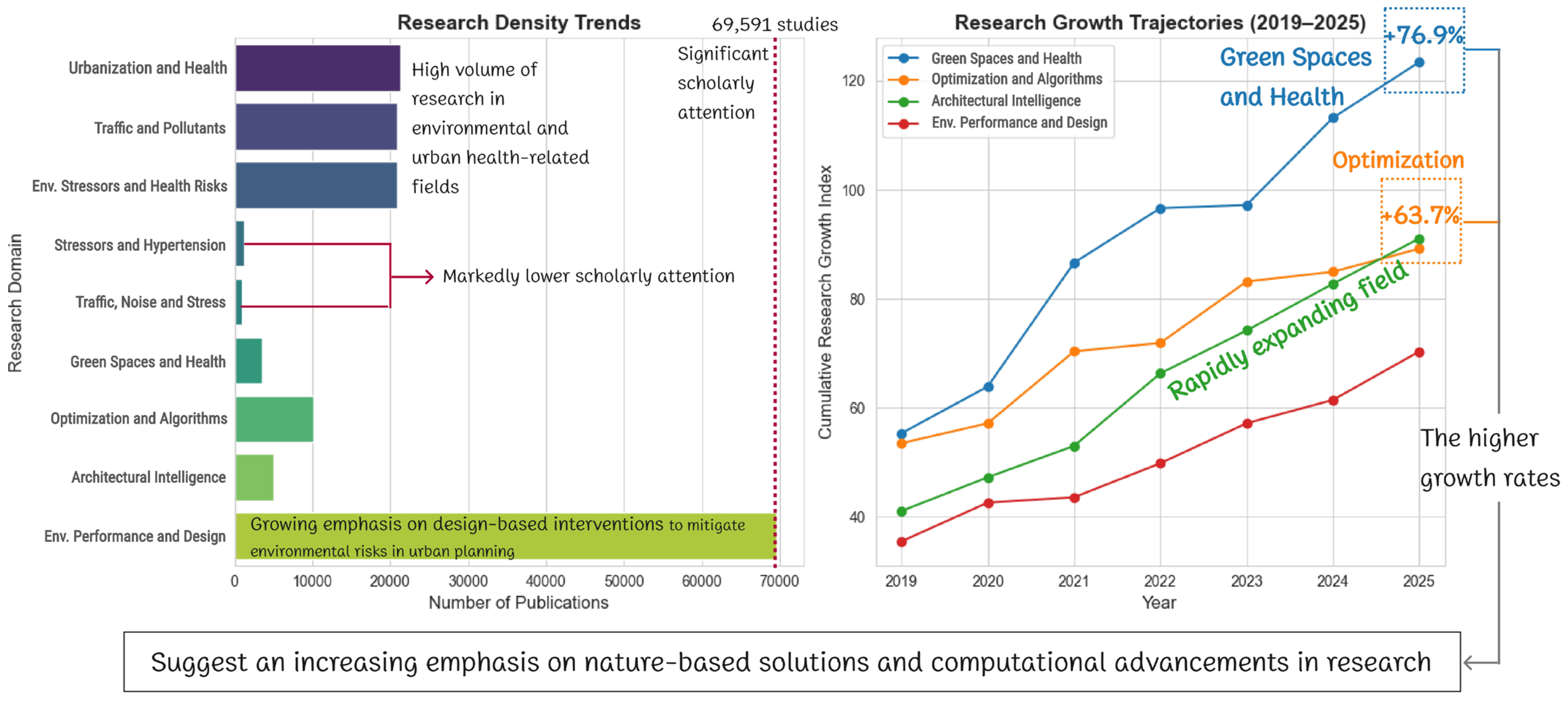
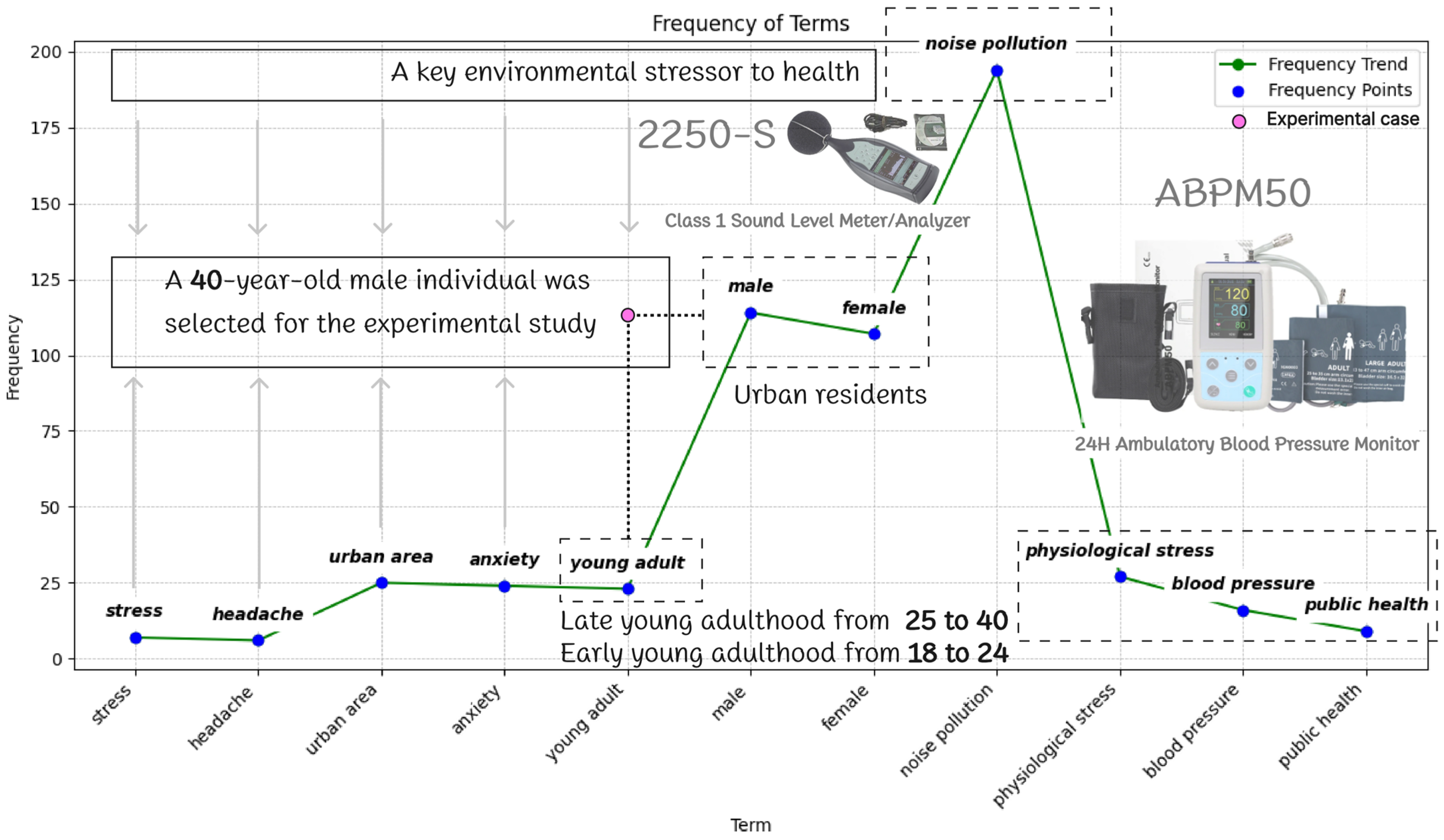
- Data Collection Tools: A 24 h Ambulatory BP Monitoring (ABPM) study was conducted over a 3–9-month period (December 2023–August 2024) using an IEEE/ESH-validated ABPM50 device (Contec Medical Systems Co., Ltd., Qinhuangdao, China) [86], which recorded systolic (SBP) and diastolic (DBP) pressures at 30 min intervals. The study also included additional cardiovascular metrics—including pulse rate (PR), pulse pressure difference (PPD), mean arterial pressure (MAP), and double product (DP)—to support a more comprehensive cardiovascular assessment (see Figure 5). Simultaneously, the research team placed a Type 2250-S (Brüel & Kjær Sound & Vibration Measurement A/S, Copenhagen, Denmark) Class 1 Sound Analyzer (illustrated in Figure 2) at both the subject’s residential and occupational sites (Figure 6b) to collect environmental data. This setup allowed precise temporal alignment between physiological responses and environmental noise exposure—specifically hypertensive episodes (defined as SBP > 140 mmHg) and noise spikes (>85 dB [87]). BP variability was analyzed using linear mixed-effects models [88], adjusted for confounding variables such as circadian rhythms and physical activity levels. The standard deviation across 48 daily readings was used to measure pressure instability (Figure 5). This integrated dataset yielded robust mechanistic evidence of noise-induced vascular dysfunction (Figure 6c), reinforcing the prioritization of chronic noise exposure as a key urban health stressor, as originally identified in the MMSR (Phase 1). It also highlighted the relevance of AI-driven urban optimization strategies—emphasized in Phase 1—as promising tools for mitigating such stressors. By grounding conceptual hypotheses in high-resolution biometric and environmental data, Phase 2 established a methodological bridge between theoretical synthesis and physiological assessment. The analysis further examined the temporal concurrence of hypertensive episodes with high-intensity construction events, underscoring the rationale for implementing real-time adaptive interventions such as sound barriers and vegetative buffers.
- (2)
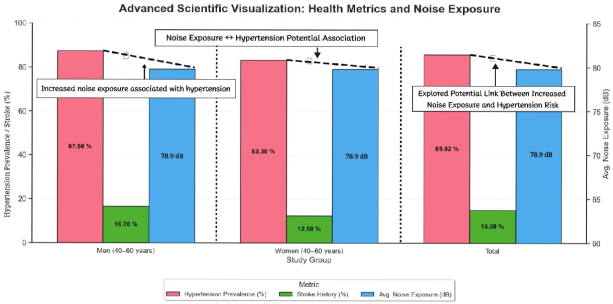
- Participant Selection: The study subject—a 40-year-old male (height: 1.75 m; weight: 85 kg; BMI: 27.8; see Appendix A) without prior hypertension or stroke history—was selected due to prolonged exposure (3 ≤ t ≤ 9 months), investigating correlations with environmental stressors, to one of Shanghai’s known high-risk zones: Yangpu District. As depicted in Figure 6b, this area, where the participant resided and worked for over a year, is subject to chronic noise exposure, a well-documented environmental pollutant [61,62,63,64,65,66]. Located near key transportation corridors and railways (shown in Figure 6b and Figure 7d), noise levels in the area typically range from 60 to 90 dB. However, active road construction and heavy truck traffic frequently push these levels above 100 dB (range: 60–105 dB, from moderate to extreme noise), creating an environment with intense exposure to both vehicular and railway noise. This chronic noise exposure, compounded by additional pollutant levels, significantly exacerbates health risks, contributing to the broader environmental burden faced by residents of the area. To contextualize this selection, Phase 1’s MMSR established the synergistic impacts of multiple urban stressors—particularly air pollution and urban heat—on cardiovascular health. Phase 2, however, strategically narrows its empirical scope to isolate the mechanistic role of chronic noise exposure—a decision not only shaped by methodological and logistical constraints, but also driven by the need for a deeper, high-resolution understanding of its specific cardiovascular impacts. The MMSR thus provides a robust conceptual foundation for future investigations that aim to integrate multiple co-occurring stressors. While this cohort does not constitute a formal control group, it serves as a reference population that underscores the representativeness and ecological relevance of the selected case. The selection reflects a broader local burden, with approximately 85% of long-term residents (N = 20) presenting with hypertension and 15% with stroke history (Appendix B); comparative data from this cohort further support the ecological validity of the single-case design (Appendix C).

3. Classification, Analysis, and Outcomes
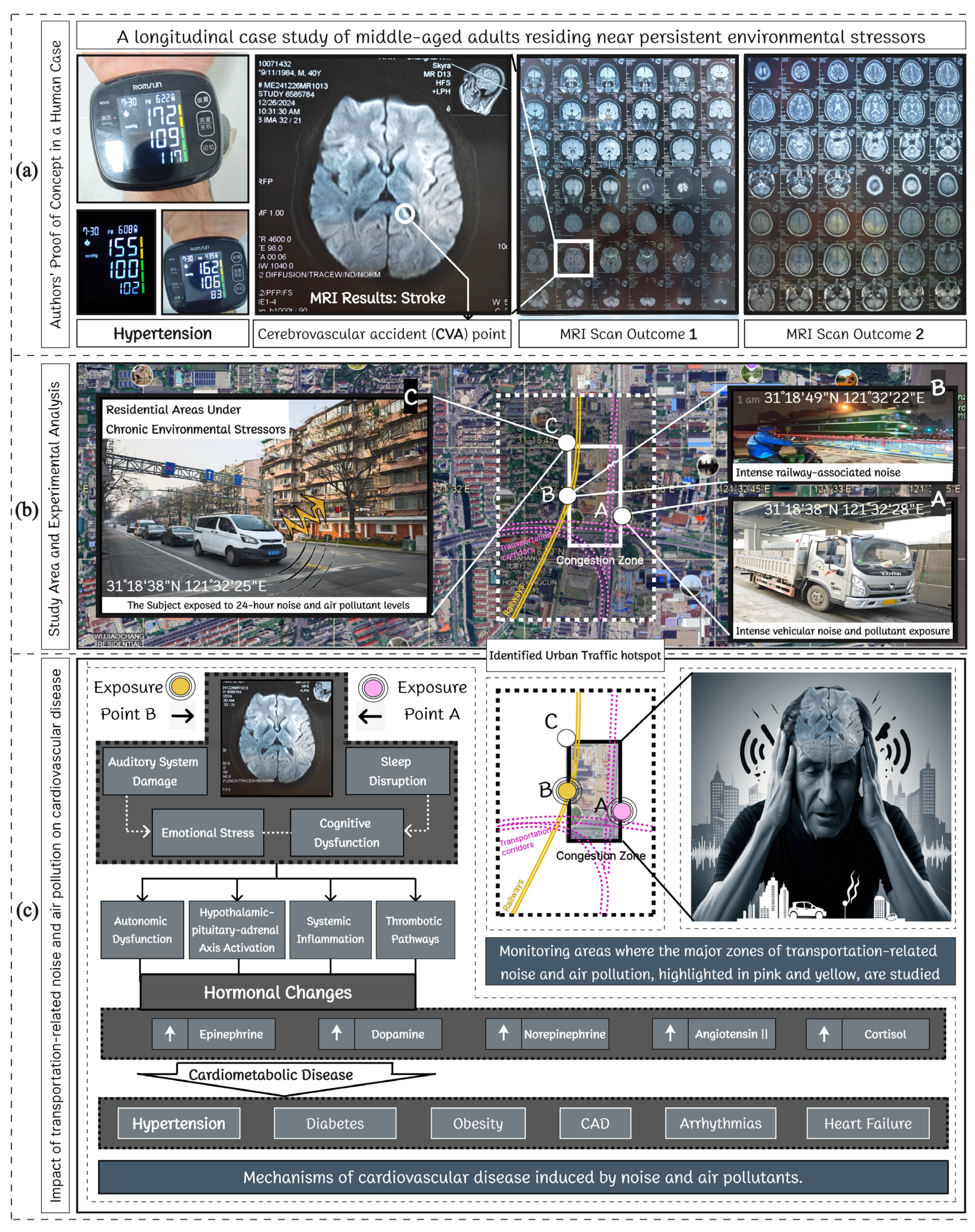
3.1. Systematic Analysis of Urbanization and Health Interactions: A Data-Driven Perspective
3.1.1. Thematic Convergence and Research Density Trends
- Urbanization and Health: A foundational category, comprising 21,266 publications, exhibiting strong associations with environmental and physiological risk factors.
- Traffic and Pollutants: With 20,907 studies, this category signifies an intensifying focus on air quality deterioration, respiratory complications, and cardiovascular diseases.
- Environmental Stressors and Health Risks: The 20,895 documented studies highlight the compounding effects of multiple urban stressors—pollution, heat islands, and socio-environmental disparities—on mental and physical health.
- Stressors and Hypertension: A specific pathway connecting environmental determinants to cardiovascular outcomes, evidenced by 1321 studies, reveals the physiological toll of chronic urban stressor exposure.
- Traffic, Noise, and Stress: A highly interconnected domain (997 studies) identifies the psychological strain associated with urban noise pollution, a rising concern in densely populated regions.
- Green Spaces and Health: Represented by 3578 studies, confirming the restorative potential of green spaces in mitigating urban stressors and enhancing well-being. Table 4 underscores the importance of optimizing urban green spaces (UGSs) to improve public health, environmental quality, and urban resilience, as strongly supported by Athokpam et al.’s study [23].
- Optimization and Algorithmic Approaches: With 10,124 studies, this category explores computational techniques to enhance urban resilience via predictive modeling and decision support systems.
- Architectural Intelligence: Housing 5105 studies, this domain investigates how intelligent design and urban morphology influence environmental sustainability and occupant health.
- Environmental Performance and Design: The most extensive research theme (69,591 studies) reflects the growing emphasis on design-based interventions to mitigate environmental risks in urban planning.
3.1.2. Research Growth Trajectories and Emerging Convergences
- Green spaces and health research exhibited the highest growth rate (+76.9%, 2019–2025), signaling rising recognition of nature-based solutions (NBS) in urban resilience and public health.
- Optimization and algorithmic approaches showed a +63.7% increase, indicating an increasing reliance on computational intelligence for urban and environmental management strategies.
- Architectural intelligence and environmental performance and design both demonstrated sustained growth (+53.6% and +53.4%, respectively), highlighting the integration of AI-driven and sustainable architectural strategies in urban health research.
3.1.3. Multivariate Linkages and Network Dependencies
- Pollution–Stress–Health Nexus: The interdependencies between traffic, pollutants, and stressors formed a distinct cluster, reinforcing the established link between urban environmental degradation and the prevalence of chronic health conditions, such as hypertension and respiratory diseases.
- Green Space as a Mitigating Variable: A notably strong positive correlation was observed between urban green spaces (UGSs) and the reduction in stress-related health conditions, further validating the role of green spaces as key urban interventions for mitigating environmental stressors.
- AI and Design-Driven Urban Health Solutions: The rapid convergence of optimization algorithms, architectural intelligence, and environmental performance metrics highlighted a paradigm shift toward AI-assisted health-centric urban design strategies, signaling an emerging model for future urban health interventions.
3.1.4. Hierarchical Interactions of Environmental Stressors
3.2. From Comprehensive MMSR to Empirical Evidence: Establishing Noise as a Critical Environmental Stressor
The Cardiovascular Toll of Chronic Noise: Mechanisms and Urban Solutions
3.3. Optimizing Urban Green Spaces for Health and Sustainability: The Role of AI and Nature-Based Solutions (NBS) in Mitigating Environmental Stress
3.4. Proposed Framework for Mitigating Urban Health Risks and Enhancing Resilience
4. Conclusions
Limitations and Future Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MMSR | Mixed methods systematic review. |
| EDCA | Empirical data collection and analysis. |
| NBSs | Nature-based solutions. |
| BMI | Body mass index. |
| TNISC | Traffic noise-induced stress concept. |
| UGSs | Urban green spaces. |
| BP | Blood pressure. |
| AI | Artificial intelligence. |
| EA | Evolutionary algorithms. |
| ML | Machine learning |
| PM | Predictive modeling |
| UHIs | Urban heat islands |
| CVD | Cardiovascular disease |
| DBP | Diastolic blood pressure |
| MAP | Mean arterial pressure |
| DP | Double product |
| PR | Pulse rate |
| PPD | Pulse pressure difference |
| CAD | Coronary artery disease |
| SBP | Systolic blood pressure |
| GA | Genetic algorithm |
| PSO | Particle swarm optimization |
| HA | Heuristic algorithm |
| OAs | Optimization algorithms |
| RF | Random forest |
| PM | Particulate matter |
| PM2.5 | Fine particulate matter, <2.5 µm |
| OS | Oxidative stress |
| CO2 | Carbon dioxide |
| USR | Urban soundscape recorder |
| ABPM | Ambulatory blood pressure monitoring |
| dB | Decibels |
| MDS | Multidimensional scaling |
| HPA | Hypothalamic-pituitary-adrenal |
| AIS | Artificial immune systems |
| AAs | Annealing algorithms |
| NDS | Non-dominated sorting |
| PLM | Piecewise linear model |
| ANN | Artificial neural network |
| LR | Linear regression |
| SVM | Support vector machine |
Appendix A
Standard Body Mass Index (BMI) Classification
| BMI Range | Category | BMI: 27.8 |
|---|---|---|
| <18.5 | Underweight | - |
| 18.5–24.9 | Normal weight | - |
| 25.0–29.9 | Overweight | ✓ |
| ≥30.0 | Obese | - |
Appendix B
Community Health Data from the Study Area
| Study Group | Sample Size | Hypertension Prevalence (%) | Stroke History (%) | Avg. Noise Exposure (dB) | Data Source |
|---|---|---|---|---|---|
| Men (40–60 years) | 12 | 87.5 | 16.7 | ± 79.8 | Local clinic medical records |
| Women (40–60 years) | 8 | 83.3 | 12.5 | Local clinic medical records | |
| Total | 20 | ≈85 | 15.0 | ± 79.8 | |
 | |||||
Note:
| |||||
| Metric | Study Community/ N = 20 | National Avg. | Absolute Difference | Relative Difference | Interpretation |
| Hypertension (40–60 years) | ≈85% (17/20) | 32% | +53.8% | +168.1% | Substantially Higher |
| Stroke Incidence | 15% (2/13) | 5.2% | +9.8% | +188.4% | Higher |
Appendix C
Comparative Health and Exposure Metrics: Case Subject vs. Long-Term Urban Residents
| Parameter | Case Subject (During Study) | Long-Term Residents (N = 20) | |
|---|---|---|---|
| Before Exposure | After Exposure | ||
| Age (years) | 40 | 40 | 40–60 |
| Hypertension (%) | 0 (no prior history) | 100 (diagnosed) | ≈85 |
| Stroke History (%) | 0 (no prior history) | 100 (diagnosed) | 15 |
| Noise Exposure (dB) | 60–105 (mean: 79.84) | 60–105 (mean: 79.84) | Similar |
References
- Münzel, T.; Steven, S.; Frenis, K.; Lelieveld, J.; Hahad, O.; Daiber, A. Environmental Factors Such as Noise and Air Pollution and Vascular Disease. Antioxid. Redox Signal. 2020, 33, 581–601. [Google Scholar] [CrossRef] [PubMed]
- Henning, R.J. Particulate Matter Air Pollution is a Significant Risk Factor for Cardiovascular Disease. Curr. Probl. Cardiol. 2023, 49, 102094. [Google Scholar] [CrossRef] [PubMed]
- Russo, A.; Cirella, G.T. Modern Compact Cities: How Much Greenery Do We Need? Int. J. Environ. Res. Public Health 2018, 15, 2180. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Varma, B. Mushrooming traffic congestion and its psychological implications among drivers. Int. J. Creat. Res. Thoughts 2020, 8, 295–301. [Google Scholar]
- Roche, I.V.; Ubalde-López, M.; Daher, C.; Nieuwenhuijsen, M.; Gascón, M. The Health-Related and Learning Performance Effects of Air Pollution and Other Urban-Related Environmental Factors on School-Age Children and Adolescents—A Scoping Review of Systematic Reviews. Curr. Environ. Health Rep. 2024, 11, 300–316. [Google Scholar] [CrossRef]
- Makvandi, M.; Yuan, P.F.; Ji, Q.; Li, C.; Elsadek, M.; Li, W.; Hassan, A.; Li, Y. Resilience to Climate Change by Improving Air Circulation Efficiency and Pollutant Dispersion in Cities: A 3D-UFO Approach to Urban Block Design. Heliyon 2024, 10, e36904. [Google Scholar] [CrossRef]
- Makvandi, M.; Li, W.; Li, Y.; Wu, H.; Khodabakhshi, Z.; Xu, X.; Yuan, P.F. Advancing Urban Resilience Amid Rapid Urbanization: An Integrated Interdisciplinary Approach for Tomorrow’s Climate-Adaptive Smart Cities—A Case Study of Wuhan, China. Smart Cities 2024, 7, 2110–2130. [Google Scholar] [CrossRef]
- Makvandi, M.; Li, W.; Ou, X.; Chai, H.; Khodabakhshi, Z.; Fu, J.; Yuan, P.F.; Horimbere, E.D. Urban Heat Mitigation towards Climate Change Adaptation: An Eco-Sustainable Design Strategy to Improve Environmental Performance under Rapid Urbanization. Atmosphere 2023, 14, 638. [Google Scholar] [CrossRef]
- Hahad, O.; Rajagopalan, S.; Lelieveld, J.; Sørensen, M.; Kuntić, M.; Daiber, A.; Basner, M.; Nieuwenhuijsen, M.; Brook, R.D.; Münzel, T. Noise and Air Pollution as Risk Factors for Hypertension: Part II-Pathophysiologic Insight. Hypertension 2023, 80, 1384–1392. [Google Scholar] [CrossRef]
- Blaustein, J.R.; Quisel, M.J.; Hamburg, N.M.; Wittkopp, S. Environmental Impacts on Cardiovascular Health and Biology: An Overview. Circ. Res. 2024, 134, 1048–1060. [Google Scholar] [CrossRef]
- Cuijpers, P.; Miguel, C.; Ciharova, M.; Kumar, M.; Brander, L.; Kumar, P.; Karyotaki, E. Impact of climate events, pollution, and green spaces on mental health: An umbrella review of meta-analyses. Psychol. Med. 2023, 53, 638–653. [Google Scholar] [CrossRef] [PubMed]
- Hahad, O.; Rajagopalan, S.; Lelieveld, J.; Sørensen, M.; Frenis, K.; Daiber, A.; Basner, M.; Nieuwenhuijsen, M.; Brook, R.D.; Münzel, T. Noise and Air Pollution as Risk Factors for Hypertension: Part I-Epidemiology. Hypertension 2023, 80, 1375–1383. [Google Scholar] [CrossRef] [PubMed]
- Badaloni, C.; De Sario, M.; Caranci, N.; de’ Donato, F.K.; Bolignano, A.; Davoli, M.; Leccese, L.; Michelozzi, P.; Leone, M. A spatial indicator of environmental and climatic vulnerability in Rome. Environ. Int. 2023, 176, 107970. [Google Scholar] [CrossRef] [PubMed]
- Saraswati, C.M.; Judge, M.A.; Weeda, L.J.Z.; Bassat, Q.; Prata, N.; Le Souëf, P.N.; Bradshaw, C.J.A. Net benefit of smaller human populations to environmental integrity and individual health and wellbeing. Front. Public Health 2024, 12, 1339933. [Google Scholar] [CrossRef]
- Rajagopalan, S.; Vergara-Martel, A.; Zhong, J.; Khraishah, H.; Kosiborod, M.N.; Neeland, I.J.; Dazard, J.-E.J.; Chen, Z.; Munzel, T.; Brook, R.D.; et al. The Urban Environment and Cardiometabolic Health. Circulation 2024, 149, 1298–1314. [Google Scholar] [CrossRef]
- Zhang, K.; Brook, R.D.; Li, Y.; Rajagopalan, S.; Kim, J.B. Air Pollution, Built Environment, and Early Cardiovascular Disease. Circ. Res. 2023, 132, 1707–1724. [Google Scholar] [CrossRef]
- Kaczyńska, M. Urban Green Spaces’ Influence on Civilization Diseases—Meta-Analysis and Critical Review. Sustainability 2024, 16, 3925. [Google Scholar] [CrossRef]
- Kuntić, M.; Hahad, O.; Al-Kindi, S.; Oelze, M.; Lelieveld, J.; Daiber, A.; Münzel, T. Pathomechanistic synergy between particulate matter and traffic noise induced cardiovascular damage and the classical risk factor hypertension. Antioxid. Redox Signal. 2024, 42, 827–847. [Google Scholar] [CrossRef]
- Li, W.; Hong, W.; Xu, X.; Makvandi, M.; Zhang, B.; Chen, Q.; Yuan, P.F. A radical shift to probabilistic thinking: Integrating energy analysis in performance-driven building morphology generation. Build. Environ. 2025, 269, 112443. [Google Scholar] [CrossRef]
- Zheng, Y.; Cheng, B.; Dong, L.; Zheng, T.; Wu, R. The Moderating Effect of Social Participation on the Relationship between Urban Green Space and the Mental Health of Older Adults: A Case Study in China. Land 2024, 13, 317. [Google Scholar] [CrossRef]
- Fu, J.; Fu, H.; Zhu, C.; Sun, Y.; Cao, H. Assessing the health risk impacts of urban green spaces on air pollution—Evidence from 31 China’s provinces. Ecol. Indic. 2024, 159, 111725. [Google Scholar] [CrossRef]
- Zhang, F.; Qian, H. A comprehensive review of the environmental benefits of urban green spaces. Environ. Res. 2024, 252, 118837. [Google Scholar] [CrossRef] [PubMed]
- Athokpam, V.; Chamroy, T.; Ngairangbam, H. The Role of Urban Green Spaces in Mitigating Climate Change: An Integrative Review of Ecological, Social, and Health Benefits. Environ. Rep. 2024, 6, 10–14. [Google Scholar] [CrossRef]
- Tate, C.; Wang, R.; Akaraci, S.; Burns, C.; Garcia, L.; Clarke, M.; Hunter, R. The contribution of urban green and blue spaces to the United Nation’s Sustainable Development Goals: An evidence gap map. Cities 2024, 145, 104706. [Google Scholar] [CrossRef]
- Nieuwenhuijsen, M.; de Nazelle, A.; Pradas, M.C.; Daher, C.; Dzhambov, A.M.; Echave, C.; Gössling, S.; Iungman, T.; Khreis, H.; Kirby, N.; et al. The superblock model: A review of an innovative URBAN model for sustainability, liveability, health and well-being. Environ. Res. 2024, 251, 118550. [Google Scholar] [CrossRef]
- Peng, Z.-r.; Lu, K.-F.; Liu, Y.; Zhai, W. The Pathway of Urban Planning AI: From Planning Support to Plan-Making. J. Plan. Educ. Res. 2023, 44. [Google Scholar] [CrossRef]
- Mashhood, M.; Salman, H.; Amjad, R.; Nisar, H. The Advantages of Using Artificial Intelligence in Urban Planning—A Review of Literature. Stat. Comput. Interdiscip. Res. 2023, 5, 1–12. [Google Scholar] [CrossRef]
- Egerer, M.; Annighöfer, P.; Arzberger, S.; Burger, S.; Hecher, Y.; Knill, V.; Probst, B.M.; Suda, M. Urban oases: The social-ecological importance of small urban green spaces. Ecosyst. People 2024, 20, 2315991. [Google Scholar] [CrossRef]
- Rahimi-Ardabili, H.; Astell--Burt, T.; Nguyen, P.Y.; Zhang, J.; Jiang, Y.; Dong, G.-h.; Feng, X. Green Space and Health in Mainland China: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 9937. [Google Scholar] [CrossRef]
- Hepat, A.; Khode, D.; Chakole, S.V. A Narrative Review of Urbanization and Mental Health: An Indian Perspective. Cureus 2024, 16, e55381. [Google Scholar] [CrossRef]
- Kunno, J.; Luangwilai, T.; Manomaipiboon, B.; Onklin, I.; Ong-artborirak, P.; Krainara, P.; Chaichana, T.; Gregory Robson, M. The Urban Health Themes and Urban Factors Associated with Health: A Brief Review. Vajira Med. J. 2024, 68, e269743. [Google Scholar] [CrossRef]
- Lin, K.; Ramos, S.; Sun, J. Urbanization, self-harm, and suicidal ideation in left-behind children and adolescents in China: A systematic review and meta-analysis. Curr. Opin. Psychiatry 2024, 37, 225–236. [Google Scholar] [CrossRef]
- Mugisha, E.K. Hypertension and Its Correlation with Socioeconomic Status in East African Urban and Rural Populations: A Scientific Review. Newport Int. J. Public Health Pharm. 2024, 5, 62–66. [Google Scholar]
- Ikiriko, T.D.; Johnbull, S.W.; Brown, I. Understanding the Nexus Between Urban Planning and Public Health Challenges in Selected Informal Settlements in Port Harcourt Municipal. Glob. Res. Environ. Sustain. 2024, 2, 9–28. [Google Scholar] [CrossRef]
- Gu, K.; Jing, Y.; Tang, J.; Jia, X.; Zhang, X.; Wang, B. Hypertension risk pathways in urban built environment: The case of Yuhui District, Bengbu City, China. Front. Public Health 2024, 12, 1443416. [Google Scholar] [CrossRef] [PubMed]
- Mendoza-Quispe, D.; Chambergo-Michilot, D.; Moscoso-Porras, M.G.; Bernabé-Ortiz, A. Hypertension prevalence by degrees of urbanization and altitude in Peru: Pooled analysis of 186 906 participants. J. Hypertens. 2023, 41, 1142–1151. [Google Scholar] [CrossRef] [PubMed]
- Tyagi, S.K.; Kumar, P.V.; Kumar, K.; Kumar, D. Environmental health quality and the consequences of urbanization: A review. Int. J. Adv. Agric. Sci. Technol. 2023, 10, 13–23. [Google Scholar] [CrossRef]
- Corburn, J. Urbanization and health. In Oxford Textbook of Global Public Health; Detels, R., Karim, Q.A., Baum, F., Li, L., Leyland, A.H., Eds.; Oxford University Press: Mumbai, India, 2021. [Google Scholar]
- Elsadek, M.; Li, Y.; Makvandi, M.; Zhang, D. Seasonal Influence of Sakura Trees on Human Health: Evidence From Physiological and Psycho-logical Responses. Environ. Behav. 2024, 56, 614–648. [Google Scholar] [CrossRef]
- Sampson, L.A.; Ettman, C.K.; Galea, S. Urbanization, urbanicity, and depression: A review of the recent g lobal literature. Curr. Opin. Psychiatry 2020, 33, 233–244. [Google Scholar] [CrossRef]
- Akomolafe, O.O.; Olorunsogo, T.; Anyanwu, E.C.; Osasona, F.; Ogugua, J.O.; Daraojimba, O.H. Air Quality and Public Health: A Review of Urban Pollution Sources and Mitigation Measures. Eng. Sci. Technol. J. 2024, 5, 259–271. [Google Scholar] [CrossRef]
- Debelu, D.; Mengistu, D.A.; Aschalew, A.; Mengistie, B.; Deriba, W. Global Public Health Implications of Traffic Related Air Pollution: Systematic Review. Environ. Health Insights 2024, 18, 11786302241272403. [Google Scholar] [CrossRef]
- Sagheer, U.; Al-Kindi, S.G.; Abohashem, S.; Phillips, C.T.; Rana, J.S.; Bhatnagar, A.; Gulati, M.; Rajagopalan, S.; Kalra, D.K. Environmental Pollution and Cardiovascular Disease. JACC 2024, 3, 100805. [Google Scholar]
- Münzel, T.; Molitor, M.; Kuntić, M.; Hahad, O.; Röösli, M.; Engelmann, N.; Basner, M.; Daiber, A.; Sørensen, M. Transportation Noise Pollution and Cardiovascular Health. Circ. Res. 2024, 134, 1113–1135. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Qian, Z.M.; Chen, L.; Zhao, X.; Cai, M.; Wang, C.; Zou, H.; Wu, Y.; Zhang, Z.; Li, H.; et al. Exposure to Air Pollution during Pre-Hypertension and Subsequent Hypertension, Cardiovascular Disease, and Death: A Trajectory Analysis of the UK Biobank Cohort. Environ. Health Perspect. 2023, 131, 17008. [Google Scholar] [CrossRef] [PubMed]
- Shetty, S.S.; Deepthi, D.; Harshitha, S.; Sonkusare, S.; Naik, P.B.; Kumari, N.S.; Madhyastha, H. Environmental pollutants and their effects on human health. Heliyon 2023, 9, e19496. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.; Well, K. A Review of Traffic-related Air Pollution. Int. J. Eng. Work. 2021, 8, 175–179. [Google Scholar] [CrossRef]
- Saremi, P. A Review of Role of Traffic Culture in Air Pollution Reduction in Metropolis of Developing Countries. J. Adv. Res. Altern. Energy Environ. Ecol. 2020, 7, 19–27. [Google Scholar] [CrossRef]
- Sarla, G.S. Air pollution: Health effects Contaminación del aire. Ef. Sobre La Salud 2020, 37, 33–38. [Google Scholar]
- Heidari, H.; Lawrence, D.A. An integrative exploration of environmental stressors on the microbiome-gut-brain axis and immune mechanisms promoting neurological disorders. J. Toxicol. Environ. Health Part B Crit. Rev. 2024, 27, 233–263. [Google Scholar] [CrossRef]
- Sliwa, K.; Viljoen, C.A.; Stewart, S.; Miller, M.R.; Prabhakaran, D.; Kumar, K.; Thienemann, F.; Piniero, D.; Prabhakaran, P.; Narula, J.; et al. Cardiovascular Disease in Low-and Middle-Income Countries Associated with Environmental Factors. Eur. J. Prev. Cardiol. 2024, 31, 688–697. [Google Scholar] [CrossRef]
- Wicki, B.; Vienneau, D.; Schwendinger, F.; Schmidt-Trucksäss, A.; Wunderli, J.-M.; Schalcher, S.; Röösli, M. Associations of exposure to transportation noise with sleep and cardiometabolic health: Exploration of pathways. Environ. Res. 2025, 279, 121805. [Google Scholar] [CrossRef]
- Heidari, H.; Lawrence, D.A. Climate Stressors and Physiological Dysregulations: Mechanistic Connections to Pathologies. Int. J. Environ. Res. Public Health 2023, 21, 28. [Google Scholar] [CrossRef]
- Awada, M.; Becerik-Gerber, B.; Liu, R.; Seyedrezaei, M.; Lu, Z.; Xenakis, M.; Lucas, G.M.; Roll, S.C.; Narayanan, S.S. Ten questions concerning the impact of environmental stress on office workers. Build. Environ. 2022, 229, 109964. [Google Scholar] [CrossRef]
- Münzel, T.; Hahad, O.; Sørensen, M.; Lelieveld, J.; Duerr, G.D.; Nieuwenhuijsen, M.; Daiber, A. Environmental risk factors and cardiovascular diseases: A comprehensive expert review. Cardiovasc. Res. 2021, 118, 2880–2902. [Google Scholar] [CrossRef] [PubMed]
- Sineva, I.M.; Khafizova, A.A.; Permyakov, I.A. Environmental Determinants of Urban Mental Health: A Literature Review. Public Health Life Environ. 2021, 29, 67–75. [Google Scholar] [CrossRef]
- Ulpiani, G. On the linkage between urban heat island and urban pollution island: Three-decade literature review towards a conceptual framework. Sci. Total Environ. 2020, 751, 141727. [Google Scholar] [CrossRef]
- Fontes, M.A.P.; Marins, F.R.; Patel, D.T.A.; de Paula, C.A.; Dos Santos Machado, L.R.; de Sousa Lima, É.B.; Ventris-Godoy, A.C.; Viana, A.C.R.; Linhares, I.C.S.; Xavier, C.H.; et al. Neurogenic Background for Emotional Stress-Associated Hypertension. Curr. Hypertens. Rep. 2023, 25, 107–116. [Google Scholar] [CrossRef]
- Elsaid, N.; Saied, A.; Kandil, H.; Soliman, A.; Taher, F.; Hadi, M.; Giridharan, G.A.; Jennings, R.; Casanova, M.; Keynton, R.S.; et al. Impact of stress and hypertension on the cerebrovasculature. Front. Biosci. 2021, 26, 1643–1652. [Google Scholar] [CrossRef]
- Cicalese, S.; da Silva, J.F.; Priviero, F.B.M.; Webb, R.C.; Eguchi, S.; Tostes, R.d.C. Vascular Stress Signaling in Hypertension. Circ. Res. 2021, 128, 969–992. [Google Scholar] [CrossRef]
- Arregi, A.; Vegas, O.; Lertxundi, A.; Silva, A.; Ferreira, I.; Bereziartua, A.; Cruz, M.T.; Lertxundi, N. Road traffic noise exposure and its impact on health: Evidence from animal and human studies—Chronic stress, inflammation, and oxidative stress as key components of the complex downstream pathway underlying noise-induced non-auditory health effects. Environ. Sci. Pollut. Res. Int. 2024, 31, 46820–46839. [Google Scholar] [CrossRef]
- Hahad, O.; Kuntić, M.; Al-Kindi, S.; Kuntić, I.; Gilan, D.; Petrowski, K.; Daiber, A.; Münzel, T. Noise and mental health: Evidence, mechanisms, and consequences. J. Expo. Sci. Environ. Epidemiol. 2025, 35, 16–23. [Google Scholar] [CrossRef]
- Hassan, N.E. Noise Pollution and Its Effects on Human Health: A Review. EPRA Int. J. Multidiscip. Res. (IJMR) 2024, 10, 24–37. [Google Scholar] [CrossRef]
- Mehrotra, A.; Shukla, S.P.; Shukla, A.K.; Manar, M.; Singh, S.K.; Mehrotra, M. A Comprehensive Review of Auditory and Non-Auditory Effects of Noise on Human Health. Noise Health 2024, 26, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Karki, T.B.; Manandhar, R.B.; Neupane, D.; Mahat, D.; Ban, P. Critical Analysis of Noise Pollution and Its Effect on Human Health. Int. J. Educ. Life Sci. 2024, 2, 161–176. [Google Scholar] [CrossRef]
- Kuntić, M.; Hahad, O.; Münzel, T.; Daiber, A. Crosstalk between Oxidative Stress and Inflammation Caused by Noise and Air Pollution—Implications for Neurodegenerative Diseases. Antioxidants 2024, 13, 266. [Google Scholar] [CrossRef]
- He, W.; Chen, M. Advancing Urban Life: A Systematic Review of Emerging Technologies and Artificial Intelligence in Urban Design and Planning. Buildings 2024, 14, 835. [Google Scholar] [CrossRef]
- Xu, H.; Omitaomu, F.; Sabri, S.; Zlatanova, S.; Li, X.; Song, Y. Leveraging generative AI for urban digital twins: A scoping review on the autonomous generation of urban data, scenarios, designs, and 3D city models for smart city advancement. Urban Inform. 2024, 3, 29. [Google Scholar] [CrossRef]
- Bolón-Canedo, V.; Morán-Fernández, L.; Cancela, B.; Alonso-Betanzos, A. A review of green artificial intelligence: Towards a more sustainable future. Neurocomputing 2024, 599, 128096. [Google Scholar] [CrossRef]
- Zhang, X.; Wang, X.; Du, S.; Tian, S.; Jia, A.; Ye, Y.; Gao, N.; Kuang, X.; Shi, X. A systematic review of urban form generation and optimization for performance-driven urban design. Build. Environ. 2024, 253, 111269. [Google Scholar] [CrossRef]
- Tay, J.Z.; Ortner, F.P.; Wortmann, T.; Aydin, E.E. Computational Optimisation of Urban Design Models: A Systematic Literature Review. Urban Sci. 2024, 8, 93. [Google Scholar] [CrossRef]
- Xiong, Y.; Liu, T.; Qin, Y.; Chen, H. A Scientometric Examination on Performance-Driven Optimization in Urban Block Design Research: State of the Art and Future Perspectives. Buildings 2024, 14, 403. [Google Scholar] [CrossRef]
- Kidari, R.; Tilioua, A. Improving Health Through Indoor Environmental Quality Monitoring: A Review of Data-Driven Models and Smart Sensor Innovations. ITM Web Conf. 2024, 69, 02007. [Google Scholar] [CrossRef]
- Bittencourt, J.C.N.; Costa, D.G.; Portugal, P.; Vasques, F. A Survey on Adaptive Smart Urban Systems. IEEE Access 2024, 12, 102826–102850. [Google Scholar] [CrossRef]
- Aziz, S.; Sharun, S.M.; Wagiman, K.R.; Moorapun, C. Architectural Intelligence (ArcAI) Evolution and Progress on Sustainable Smartscapes Planning for the Cities of Tomorrow. Environ.-Behav. Proc. J. 2024, 9, 107–114. [Google Scholar] [CrossRef]
- Kommineni, M.; Baseer, K.K. An Architecture and Review of Intelligence Based Traffic Control System for Smart Cities. EAI Endorsed Trans. Energy Web 2024, 11. [Google Scholar] [CrossRef]
- Caetano, I.; Leitão, A. Connecting design and fabrication through algorithms: Current and future prospects for AEC. Autom. Constr. 2024, 164, 105445. [Google Scholar] [CrossRef]
- Živković, M.; Žujović, M.; Milošević, J. Architectural 3D-Printed Structures Created Using Artificial Intelligence: A Review of Techniques and Applications. Appl. Sci. 2023, 13, 10671. [Google Scholar] [CrossRef]
- Snooks, R. Behavioral tectonics: AgentBody prototypes and the compression of tectonics. Archit. Intell. 2022, 1, 9. [Google Scholar] [CrossRef]
- Thijssens, T. The Relation Between Environmental Performance and Environmental Disclosure: A Critical Review of the Performance Measures Used. SSRN Electron. J. 2024, 24, 1140–1157. [Google Scholar] [CrossRef]
- Zhou, Y.; Ma, M.; Tam, V.W.Y.; Le, K.N. Design variables affecting the environmental impacts of buildings: A critical review. J. Clean. Prod. 2023, 387, 135921. [Google Scholar] [CrossRef]
- Attaianese, E.; Barilà, M. Inclusive mental well-being through environmental design. E3S Web Conf. 2023, 436, 06005. [Google Scholar] [CrossRef]
- Faedda, S.; Plaisant, A.; Talu, V.; Tola, G. The Role of Urban Environment Design on Health During the COVID-19 Pandemic: A Scoping Review. Front. Public Health 2022, 10, 791656. [Google Scholar] [CrossRef] [PubMed]
- Mansour Salamé, J.; Leroy, Y.; Saidani, M.; Nicolai, I. Understanding and Monitoring Environmental Performance of Infrastructure Design Projects. Proc. Des. Soc. 2021, 1, 3269–3278. [Google Scholar] [CrossRef]
- Jassem, S.; Zakaria, Z.A.; Azmi, A.A.C. Sustainability balanced scorecard architecture and environmental performance outcomes: A systematic review. Int. J. Product. Perform. Manag. 2021, 71, 1728–1760. [Google Scholar] [CrossRef]
- Hermányi, Z.; Pokoly, B.; Visolyi, G.Á.; Barna, I. Evaluation of Meditech ABPM-06 ambulatory blood pressure measuring device, according to the European Society of Hypertension, the British Hypertension Society and the International Organization for Standardization Protocol. Blood Press. Monit. 2019, 24, 208–211. [Google Scholar] [CrossRef]
- Vienneau, D.; Saucy, A.; Schäffer, B.; Flückiger, B.; Tangermann, L.; Stafoggia, M.; Wunderli, J.M.; Röösli, M. Transportation noise exposure and cardiovascular mortality: 15-years of follow-up in a nationwide prospective cohort in Switzerland. Environ. Int. 2021, 158, 106974. [Google Scholar] [CrossRef]
- Hernandez, M.F.; Chang, T.I. The Need to Reduce Variability in the Study of Blood Pressure Variability. Am. J. Kidney Dis. 2023, 81, 379–381. [Google Scholar] [CrossRef]
- Teixeira, L.R.; Pega, F.; de Abreu, W.; de Almeida, M.S.; de Andrade, C.A.F.; Azevedo, T.M.; Dzhambov, A.M.; Hu, W.; Macedo, M.R.V.; Martinez-Silveira, M.S.; et al. The prevalence of occupational exposure to noise: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2021, 154, 106380. [Google Scholar] [CrossRef]
- Chen, J.; Hart, J.E.; Fisher, N.D.L.; Yanosky, J.D.; Roscoe, C.; James, P.; Laden, F. Multiple Environmental Exposures and the Development of Hypertension in a Prospective US-Based Cohort of Female Nurses: A Mixture Analysis. Environ. Sci. Technol. 2024, 58, 14146–14157. [Google Scholar] [CrossRef]
- Wickramathilaka, N.; Ujang, U.; Azri, S.; Choon, T.L. Influence of Urban Green Spaces on Road Traffic Noise Levels:-A Review. Int. Arch. Photogramm. Remote Sens. Spatial Inf. Sci. 2022, XLVIII-4/W3-2022, 195–201. [Google Scholar] [CrossRef]
- Makvandi, M.; Li, B.; Elsadek, M.; Khodabakhshi, Z.; Ahmadi, M. The Interactive Impact of Building Diversity on the Thermal Balance and Micro-Climate Change under the Influence of Rapid Urbanization. Sustainability 2019, 11, 1662. [Google Scholar] [CrossRef]
- Chen, J.; Hoek, G. Long-term exposure to PM and all-cause and cause-specific mortality: A systematic review and meta-analysis. Environ. Int. 2020, 143, 105974. [Google Scholar] [CrossRef]
- Tota, M.; Karska, J.; Kowalski, S.; Piątek, N.; Pszczołowska, M.; Mazur, K.; Piotrowski, P. Environmental pollution and extreme weather conditions: Insights into the effect on mental health. Front. Psychiatry 2024, 15, 1389051. [Google Scholar] [CrossRef]
- Sunena; Mishra, D.N. Stress Etiology of Type 2 Diabetes. Curr. Diabetes Rev. 2022, 18, e240222201413. [Google Scholar] [CrossRef]
- Cozma, D.; Siatra, P.; Bornstein, S.R.; Steenblock, C. Sensitivity of the Neuroendocrine Stress Axis in Metabolic Diseases. Horm. Metab. Res. 2023, 56, 65–77. [Google Scholar] [CrossRef]
- Stojanovski, T.; Zhang, H.; Frid, E.; Chhatre, K.; Peters, C.; Samuels, I.; Sanders, P.; Partanen, J.; Lefosse, D. Rethinking Computer-Aided Architectural Design (CAAD)—From Generative Algorithms and Architectural Intelligence to Environmental Design and Ambient Intelligence. In Proceedings of the Computer-Aided Architectural Design Futures, Los Angeles, CA, USA, 16–18 July 2021. [Google Scholar]
- Newton, D.W. Fostering Augmented Intelligence in Architectural Education to Address Complexity. In Proceedings of the 2021 AIA/ACSA Intersections Research Conference: Communities, Washington, DC, USA, 29 September–1 October 2021. [Google Scholar] [CrossRef]
- Li, J. Transforming architecture: The synergy of digital fabrication and parametric design. Appl. Comput. Eng. 2024, 66, 243–248. [Google Scholar] [CrossRef]
- Yu, H.; Wen, B.; Zahidi, I.; Fai, C.M.; Madsen, D.Ø. Constructing the future: Policy-driven digital fabrication in China’s urban development. Results Eng. 2024, 22, 102096. [Google Scholar] [CrossRef]
| No. | Search Query | Total Documents Found | Documents Found Between 2019 and 2025 | Study Growth Pattern: Increment in Research Activity Over the Last 5 Years | Identified Article Documents (n=) | Language Filter: English Only? |
|---|---|---|---|---|---|---|
| 1 | Urbanization and Health | 21,266 (1956–2025) | 10,843 |  Research growth: 50.9%  | 7486 | Yes |
| 2 | Traffic and Pollutant | 20,907 (1962–2025) | 8375 | 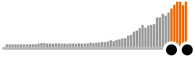 Research growth: 40.0%  | 7118 | Yes |
| 3 | Environmental and Stressors | 20,895 (1961–2025) | 10,011 |  Research growth: 47.9%  | 4172 | Yes |
| 4 | Stressors and Hypertension | 1321 (1951–2025) | 431 |  Research growth: 32.6%  | 318 | Yes |
| 5 | Traffic, Noise, and Stress | 997 (1969–2025) | 392 | 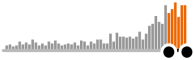 Research growth: 39.3%  | 236 | Yes |
| 6 | Green Spaces and Health | 3578 (1975–2025) | 2754 |  Research growth: 76.9%  | 982 | Yes |
| 7 | Optimization and Algorithmic Approaches | 10,124 (1970–2025) | 6449 | 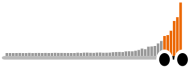 Research growth: 63.7%  | 4272 | Yes |
| 8 | Architectural and Intelligence | 5105 (1942–2025) | 738 |  Research growth: 53.6%  | 1090 | Yes |
| 9 | Environmental Performance and Design | 69,591 (1942–2025) | 37,211 | 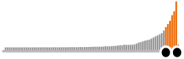 Research growth: 53.4%  | 4335 | Yes |
| Total | 153,784 | 78,194 | 50.8 %  | 30,009 | ||
| No. | ‘Urbanization’ and ‘Health’ occurrence analysis | Examination of Significant Interactions between Urbanization and Health Risk factors |
| 1 | 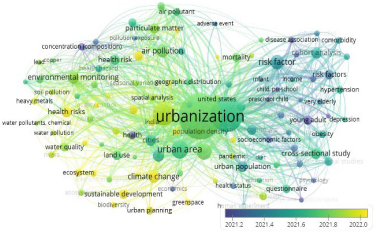 | 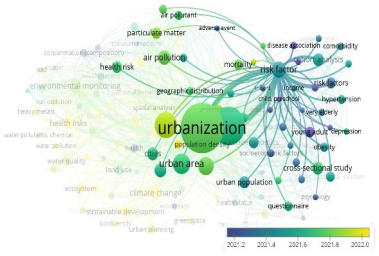 |
| No. | ‘Traffic’ and ‘Pollutant’ occurrence analysis | Examination of Significant Interactions between Traffic and Pollutant |
| 2 |  | 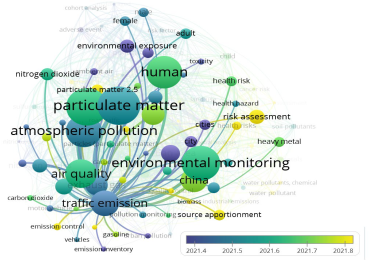 |
| No. | ‘Environmental’ and ‘Stressors’ occurrence analysis | Examination of Significant Interactions between Environmental and Stressors Risks |
| 3 | 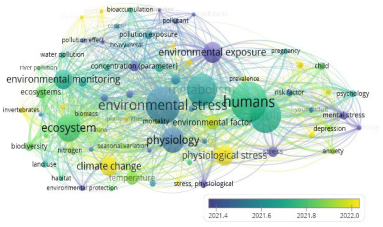 |  |
| No. | ‘Stressors’ and ‘Hypertension’ occurrence analysis | Examination of Significant Interactions between Stressors and Hypertension |
| 4 | 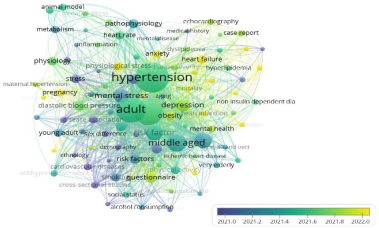 |  |
| No. | ‘Traffic’ and ‘Noise’ and ‘Stress’ occurrence analysis | Examination of Significant Interactions between Traffic, Noise, and Stress |
| 5 |  |  |
| No. | ‘Green Spaces’ and ‘Health’ occurrence analysis | Examination of Significant Interactions between Green Spaces and Public Health |
| 6 |  |  |
| No. | ‘Optimization’ and ‘Algorithmic Approaches’ occurrence analysis | Examination of Significant Interactions between Optimization and Algorithmic Approaches |
| 7 | 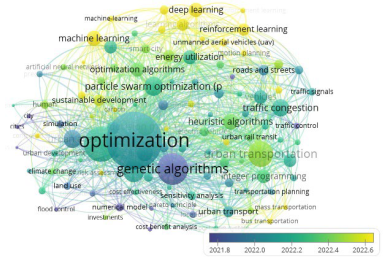 | 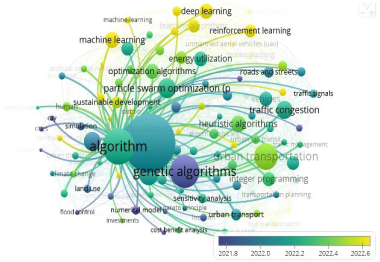 |
| No. | ‘Architectural’ and ‘Intelligence’ occurrence analysis | Examination of Significant Interactions between Architectural and Intelligence |
| 8 |  | 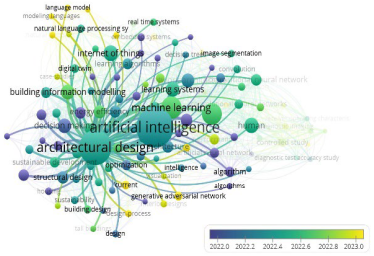 |
| No. | ‘Environmental Performance’ and ‘Design’ occurrence analysis | Examination of Significant Interactions between Environment Performance and Design |
| 9 | 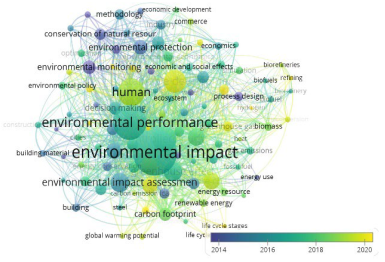 | 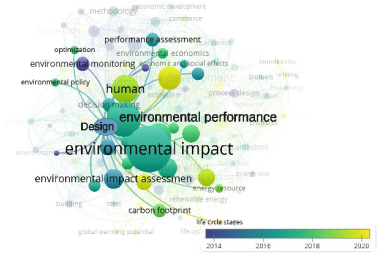 |
| No. | Benefit Classification | Identifiable Impacts and Tangible Advantages | Specifics |
|---|---|---|---|
| 1 | Ecological benefits | Carbon sequestration | UGSs function as carbon sinks, sequestering atmospheric CO2, thereby contributing to the mitigation of climate change. |
| Biodiversity support | UGSs serve as habitats for diverse species, fostering biodiversity and bolstering ecosystem resilience. | ||
| UHIs mitigation | Vegetation mitigates the UHIs effect by providing shade and facilitating evapotranspiration, thereby reducing ambient temperatures and lowering energy consumption for cooling. | ||
| 2 | Social benefits | Community integration and solidarity | UGSs serve as gathering spots for social interactions, fostering community ties and reducing isolation. |
| Economic rejuvenation | Proximity to UGSs has been shown to enhance property values, attract business investment and tourism, thereby contributing to local economic growth. | ||
| Recreation and leisure opportunities | Parks and UGSs facilitate recreational activities, thereby improving residents’ overall quality of life. | ||
| 3 | Health benefits | Physical health improvement | Access to UGSs promotes physical activity, thereby reducing the incidence of chronic conditions such as obesity, diabetes, and cardiovascular diseases. |
| Mental health improvement | Exposure to natural environments and UGSs effectively reduces stress, anxiety, and depression, fostering psychological resilience and enhancing residents’ mental health. | ||
| Air quality improvement | UGSs, through vegetation, filter pollutants, improving air quality and mitigating respiratory illnesses. |
| Stress Class | Subtype | Sources | Health Impact | Thresholds | Interactions |
|---|---|---|---|---|---|
| Physical | Noise Pollution | Traffic, construction | HPA axis activation; elevated cortisol; hypertension | >65 dB (daytime) [1] | Amplifies air pollution effects |
| Urban Heat Islands | Heat emissions | Stress, CVD mortality, heat stroke | ΔT ≥2 °C [92] (urban vs. rural) | Increases PM2.5 toxicity | |
| Chemical | PM2.5, NO2 | Vehicular emissions | Atherosclerosis, lung disease, systemic inflammation | WHO: PM2.5 < 10 μg/m3 [93] | Synergistic with noise |
| Biological | Green Space Loss | Urban densification | Higher cortisol levels (stress hormone), anxiety | <9 m2/capita (WHO) [3] | Increases heat, pollution, and noise |
| Urban Health Under Siege: The Role of Key Environmental Stressors | |||
|---|---|---|---|
| Ref. | Year | The noise/stress concept and the associated adverse mental health consequences | The effects of noise on different organ systems and on mental health |
| [62] | 2024 |  |  |
| Molecular pathways of traffic noise-induced stress and inflammation | Environmental pollution in the pathogenesis of mental disorders | ||
| [94] | 2024 | 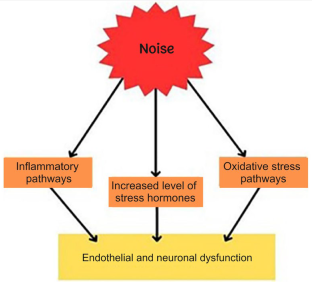 |  ICAM-1, intercellular cell adhesion molecule-1; VCAM-1, vascular cell adhesion molecule-1; DCF, density compensation function; CBF, cerebrospinal fluid; ROS, reactive oxygen species. |
| Major environmental exposures and cardiovascular health | The exposome concept of Noise-stress | ||
| [10] [55] | 2024 2024 | 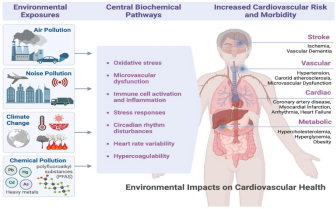 | 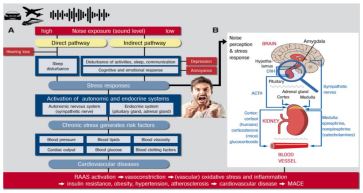 |
| Interplay between neuroinflammation and oxidative stress in neurodegeneration | Mechanisms of air pollution-induced neuroinflammation and oxidative stress | ||
| [66] | 2024 |  | 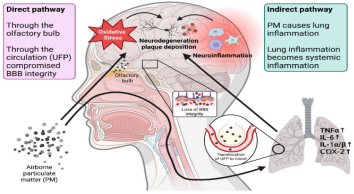 |
| Models | Objectives | Infrastructure Type | Scale | |
|---|---|---|---|---|
| Evolutionary Algorithms (EA) | Genetic algorithm (GA) | Urban health and design: optimizing urban green spaces (UGSs), enhance biodiversity and ecological balance, reduce UHI effects, ensure equitable green space access, minimize noise, improve air quality, and promote public health and well-being. | Urban green spaces (UGSs) | Urban spatial structure |
| Artificial Immune Systems (AIS) | Public health: optimize UGSs, reducing environmental impact, enhancing accessibility, and preserving biodiversity within constraints. AIS effectively handles complex, multi-dimensional UGSs optimization, particularly in large, dynamic search spaces. | Urban green spaces (UGSs) | Urban spatial structure | |
| Annealing algorithms (AAs) | Urban health and design: AAs, especially simulated annealing (SA), optimize urban green spaces by improving layout, accessibility, and connectivity, enhancing air quality and biodiversity. | Urban green spaces (UGSs) | Urban spatial structure | |
| Non- Dominated Sorting (NDS) | Public health and design: given conflicting objectives like green space coverage, environmental impact reduction (e.g., noise, pollution), accessibility, biodiversity preservation, and space utilization, NDS efficiently addresses multi-objective optimization. It identifies Pareto optimal solutions, balancing these factors for effective UGSs design. | Urban green spaces (UGSs) | Urban spatial structure | |
| Particle Swarm-based Optimization (PSO) Algorithm | Urban health and design: a solution for urban green space placement that maximizes noise attenuation in high-traffic zones, optimizes land use within zoning constraints, enhances biodiversity, ecosystem services (e.g., air purification, carbon sequestration, water management), improves energy efficiency, and mitigates urban heat islands (UHIs). | Urban green spaces (UGSs) | Urban spatial structure | |
| Heuristic algorithm (HA) | HA | Urban health: enhancing biodiversity, ecosystem security, and access to green spaces to improve mental and physical health. Strategically placing green spaces near high-risk areas (e.g., pollution, noise) to buffer noise, improve air quality, regulate temperature (urban heat island effect), and promote sustainability. Ensuring aesthetic quality, livability, and social equity by providing green spaces to underserved communities. | Urban green spaces (UGSs) | Urban spatial structure |
| Machine learning (ML) | Artificial Neural Network (ANN) | Urban health: optimizing urban green spaces (UGS) to mitigate environmental stressors like noise, air pollution, and heat. ANNs can model complex, non-linear relationships between urban factors (e.g., noise levels, population density) and desired outcomes (e.g., health improvements, pollution reduction). | Urban green spaces (UGSs) | Urban spatial structure |
| Linear Regression (LR) | Urban and public health: improving urban health by addressing environmental stressors such as noise, air pollution, and heat. | Urban green spaces (UGSs) | Urban spatial structure | |
| Random Forest (RF) | Urban design and health: optimizing urban green spaces (UGS) by analyzing factors like green space size, vegetation, noise, and air pollution. | Urban green spaces (UGSs) | Urban spatial structure | |
| Support Vector Machine (SVM) | Urban health: SVM optimizes urban green spaces by classifying regions based on health outcomes and environmental stressors. It handles complex, non-linear relationships but faces challenges in scalability and interpretability. With proper tuning, it is a valuable tool for urban health optimization. | Urban green spaces (UGSs) | Urban spatial structure | |
| Optimization Algorithms (OAs) | OAs | Urban health and design: OAs help urban planners design green space layouts, considering factors like size, distribution, accessibility, environmental stressors (e.g., noise, pollution), and their impact on urban health, energy efficiency, heat islands, air quality, biodiversity, and urban cooling. | Urban green spaces (UGSs) | Urban spatial structure |
| Other optimization methods | Piecewise Linear Model (PLM) | PLM optimizes UGSs by capturing non-linear relationships between green space size and urban health factors. Its segmented approach enhances decision-making, allowing planners to design effective, context-specific green spaces that adapt to varying urban conditions and stages of development. | Urban green spaces (UGSs) | Urban spatial structure |
| Taguchi Method | The Taguchi Method optimizes UGSs by identifying optimal design parameters (e.g., size, plant species, accessibility) to enhance health outcomes, reduce environmental stressors (e.g., noise, pollution), and improve energy efficiency and heat island mitigation. It defines an objective function to balance these factors, ensuring effective, long-term UGSs design. | Urban green spaces (UGSs) | Urban spatial structure | |
| 3D Spatial Optimization Model 3D-SOM | 3D-SOM optimizes UGSs by considering spatial arrangements, accessibility, and environmental impacts like noise, air pollution, and heat islands. It enables multi-objective optimization, balancing noise reduction, air quality, health benefits, and heat mitigation. The model adapts to urban constraints and scales for dynamic, sustainable green space design, despite challenges in computational complexity and data requirements. | Urban green spaces (UGSs) | Urban spatial structure |
| Ref. | Year | Exploration | Summary | Visual Synopsis | Can It Influence Environmental Performance? | Can It Impact Health Outcomes? | Can It Reduce Environmental Stressors? |
|---|---|---|---|---|---|---|---|
| [97] | 2021 | Rethinking Computer-Aided Architectural Design (CAAD)—From Generative Algorithms and Architectural Intelligence to Environmental Design and Ambient Intelligence | Architectural intelligence augmented by AI can refine urban design strategies to enhance environmental performance and foster healthier urban environments. | 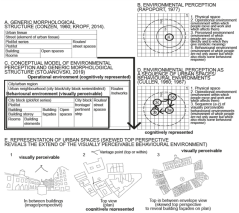 | YES. AI-driven design leads to more efficient and sustainable urban spaces, improving air quality, biodiversity, and energy use. | YES. Enhances mental and physical health through better-designed spaces that reduce stressors. | YES. Reduces urban heat islands, pollution, and noise. |
| [75] | 2024 | Architectural Intelligence (ArcAI) Evolution and Progress on Sustainable Smartscapes Planning for the Cities of Tomorrow | Architectural intelligence and AI can integrate eco-friendly practices and smart technologies to create sustainable smart urban environments. |  | YES. Promotes eco-friendly practices, energy efficiency, and reduced carbon footprints. | YES. Improved health outcomes through smarter urban planning and better access to green spaces. | YES. Addresses air pollution, reduces heat effects, and promotes efficient use of space. |
| [98] | 2021 | Fostering Augmented Intelligence in Architectural Education to Address Complexity | Augmented intelligence combining human and AI can help architectural education address complex design problems for sustainable urban environments. |  | YES. Improves sustainable building designs, optimizing material usage and energy consumption. | YES. Supports mental health by creating environments that address the psychological impact of urban living. | YES. Reduces resource waste and environmental degradation. |
| [99] | 2024 | Transforming architecture: The synergy of digital fabrication and parametric design | The integration of digital fabrication and parametric design enables more sustainable, efficient, and innovative architectural solutions. | 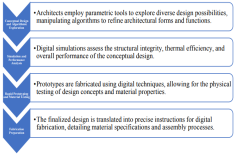 | YES. Enhances energy efficiency, reduces waste, and supports sustainability in urban environments. | YES. Contributes to healthier urban areas by creating environments that support social well-being. | YES. Reduces construction waste, pollution, and resource consumption. |
| [100] | 2024 | Constructing the future: Policy-driven digital fabrication in urban development | Digital fabrication technologies (e.g., 3D printing and CNC machining) are revolutionizing architectural design, improving construction efficiency, enabling smart city innovations, and promoting sustainability. |  | YES. Improves the sustainability of urban infrastructure, reducing carbon emissions and material waste. | YES. Provides access to health-optimizing green spaces and reduces urban heat islands. | YES. Helps reduce environmental stressors such as noise, pollution, and energy consumption. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Makvandi, M.; Khodabakhshi, Z.; Liu, Y.; Li, W.; Yuan, P.F. Can AI and Urban Design Optimization Mitigate Cardiovascular Risks Amid Rapid Urbanization? Unveiling the Impact of Environmental Stressors on Health Resilience. Sustainability 2025, 17, 6973. https://doi.org/10.3390/su17156973
Makvandi M, Khodabakhshi Z, Liu Y, Li W, Yuan PF. Can AI and Urban Design Optimization Mitigate Cardiovascular Risks Amid Rapid Urbanization? Unveiling the Impact of Environmental Stressors on Health Resilience. Sustainability. 2025; 17(15):6973. https://doi.org/10.3390/su17156973
Chicago/Turabian StyleMakvandi, Mehdi, Zeinab Khodabakhshi, Yige Liu, Wenjing Li, and Philip F. Yuan. 2025. "Can AI and Urban Design Optimization Mitigate Cardiovascular Risks Amid Rapid Urbanization? Unveiling the Impact of Environmental Stressors on Health Resilience" Sustainability 17, no. 15: 6973. https://doi.org/10.3390/su17156973
APA StyleMakvandi, M., Khodabakhshi, Z., Liu, Y., Li, W., & Yuan, P. F. (2025). Can AI and Urban Design Optimization Mitigate Cardiovascular Risks Amid Rapid Urbanization? Unveiling the Impact of Environmental Stressors on Health Resilience. Sustainability, 17(15), 6973. https://doi.org/10.3390/su17156973







