Integrated Quality and Environmental Management in Healthcare: Impacts, Implementation, and Future Directions Toward Sustainability
Abstract
1. Introduction
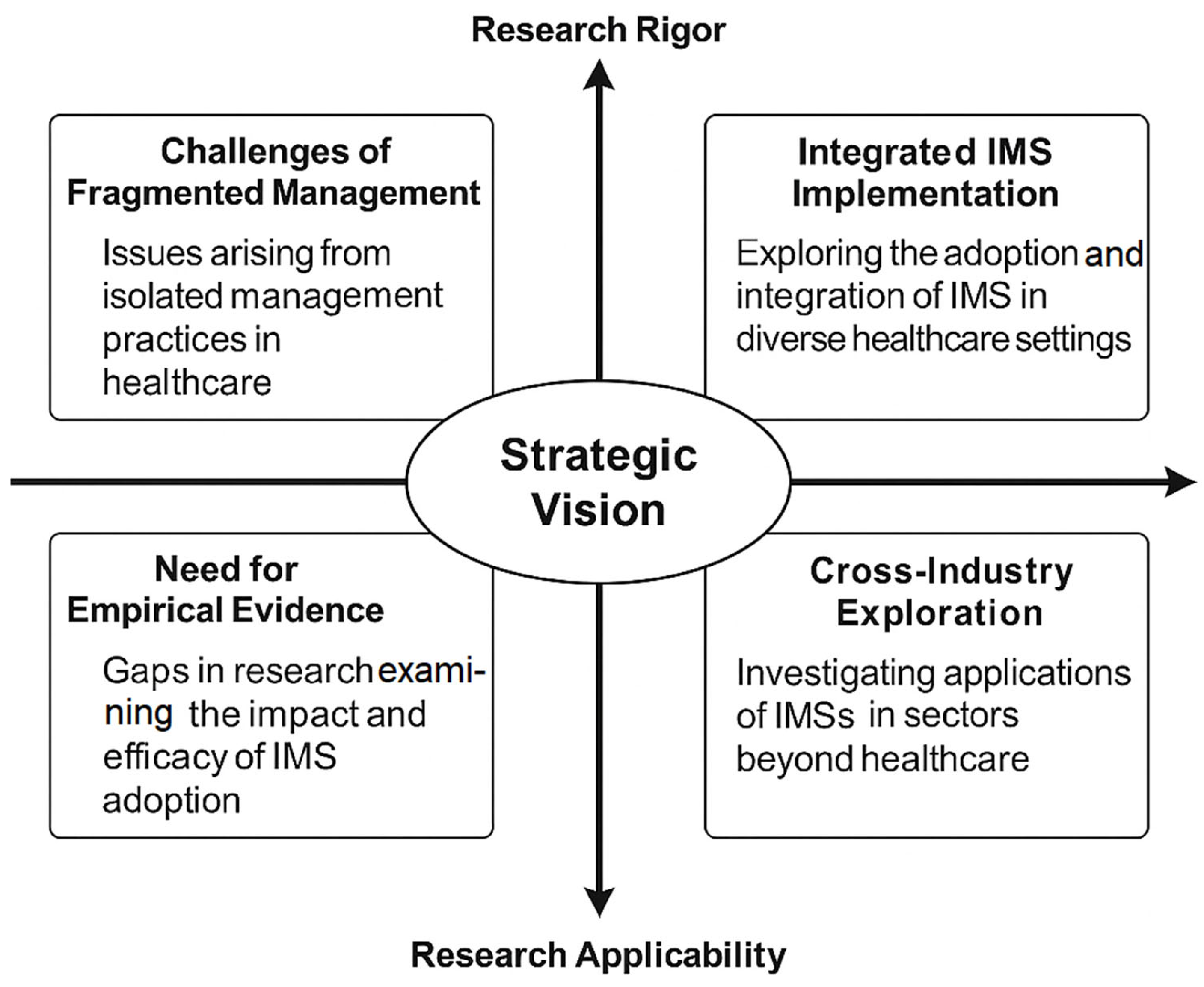
2. Integrated Quality and Environmental Management in Healthcare: Current Research and Knowledge Gaps
3. Framework and Standards
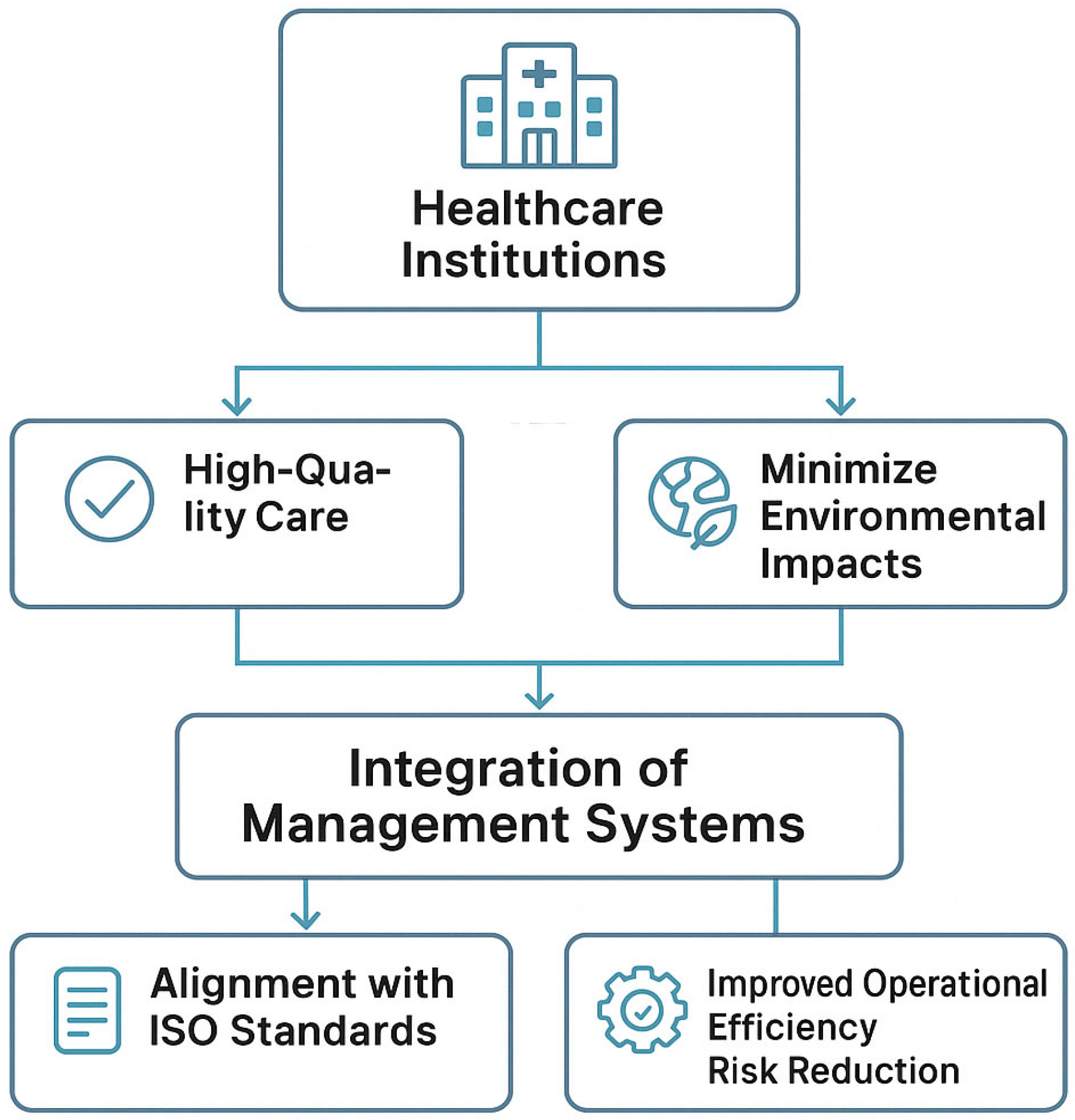
3.1. Theoretical Foundations of IMSs in Healthcare Institutions
3.2. Standards-Based Framework for IMS Implementation in Healthcare
3.3. Barriers and Challenges in IMS Implementation
3.4. Operationalizing Integrated Quality and Environmental Management
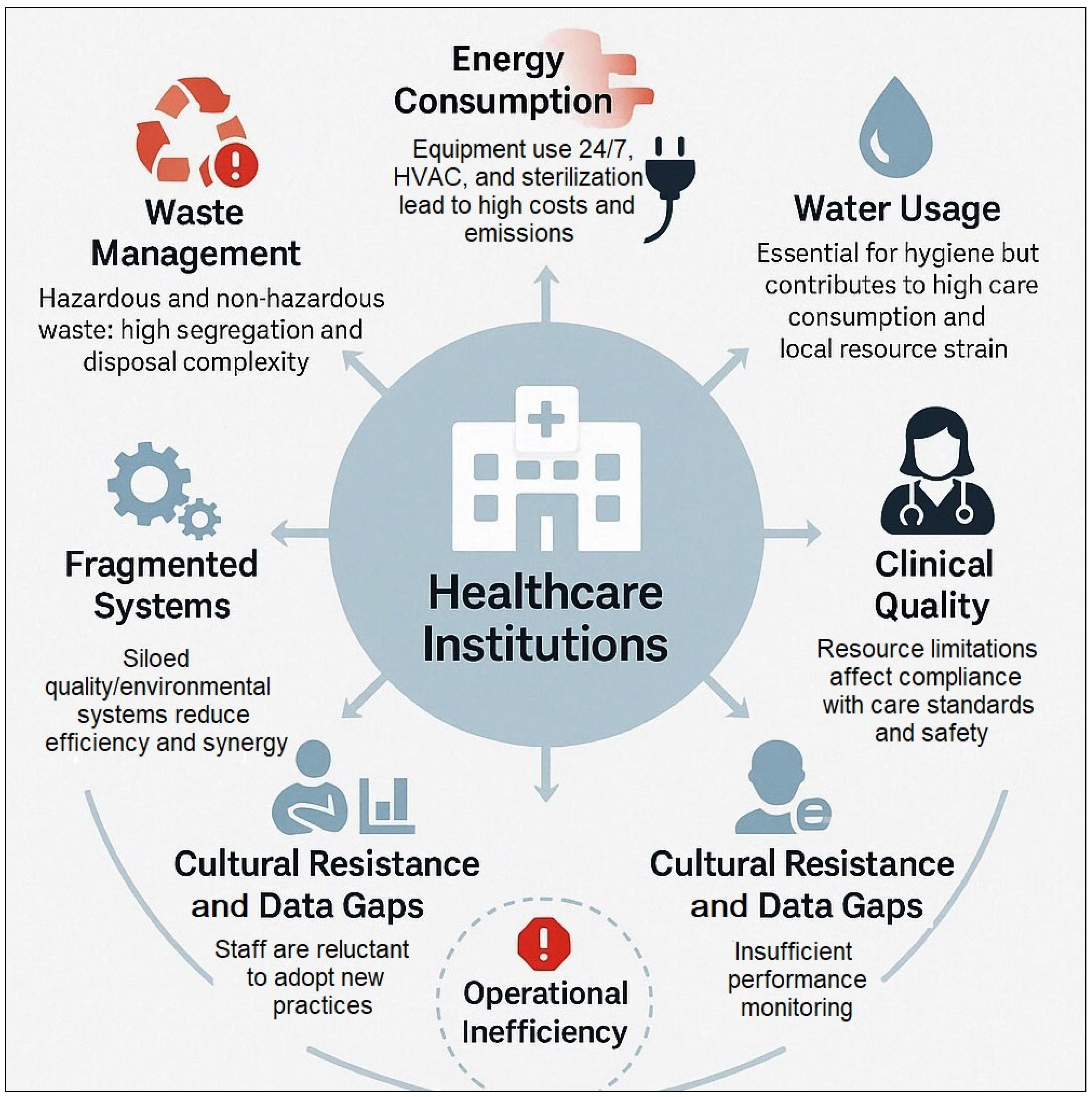
4. Environmental and Quality Challenges in Healthcare
4.1. Energy Management and Efficiency in Healthcare Facilities
4.2. Managing Water Use in Healthcare: Patterns, Challenges, and Infection Control Considerations
4.3. Systemic Challenges to Quality and Sustainability in Healthcare
4.4. Operational Challenges at the Intersection of Quality and Environmental Sustainability
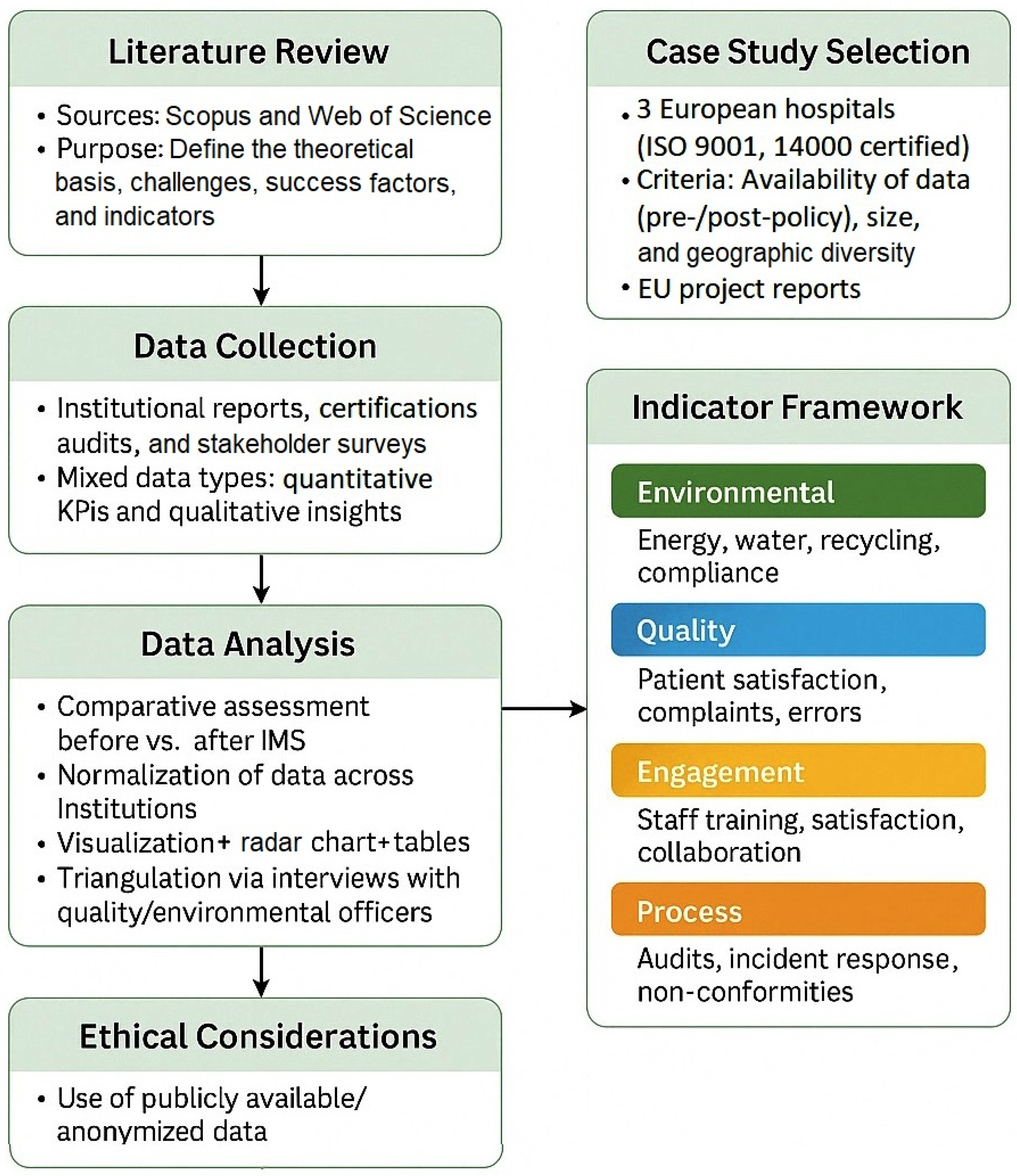
5. Methodology
5.1. Methodological Framework for Comparative Evaluation of IMS in Healthcare
5.2. Literature-Informed Framework and Review Strategy
5.3. Case Study Selection
5.4. Indicator Selection and Comparative Framework
- Environmental indicators—energy consumption per patient (kWh), water usage per patient (liters), percentage of medical waste recycled, and number of environmental non-compliance incidents;
- Quality indicators—patient satisfaction scores, average number of patient complaints, clinical error rate, and staff turnover;
- Engagement indicators—percentage of staff participating in training, employee satisfaction with workplace conditions, and cross-departmental collaboration scores;
- Process indicators—frequency of internal audits, incident response time, and procedural non-conformity rates.
5.5. Data Analysis
5.6. Ethical Considerations
6. Case Studies
6.1. Case Study 1: Regional Hospital in Southern Germany (a Pediatric Clinic)
6.2. Case Study 2: University Hospital in Northern Italy (a Pediatric Clinic)
6.3. Case Study 3: Public Hospital in Eastern Europe (Northwestern Romania)
6.4. Comparative Insights
- A strong leadership commitment and visible management support;
- Cross-functional teams and training programs;
- Clear alignment of IMS objectives with institutional goals;
- Continuous monitoring and reporting of key performance metrics.
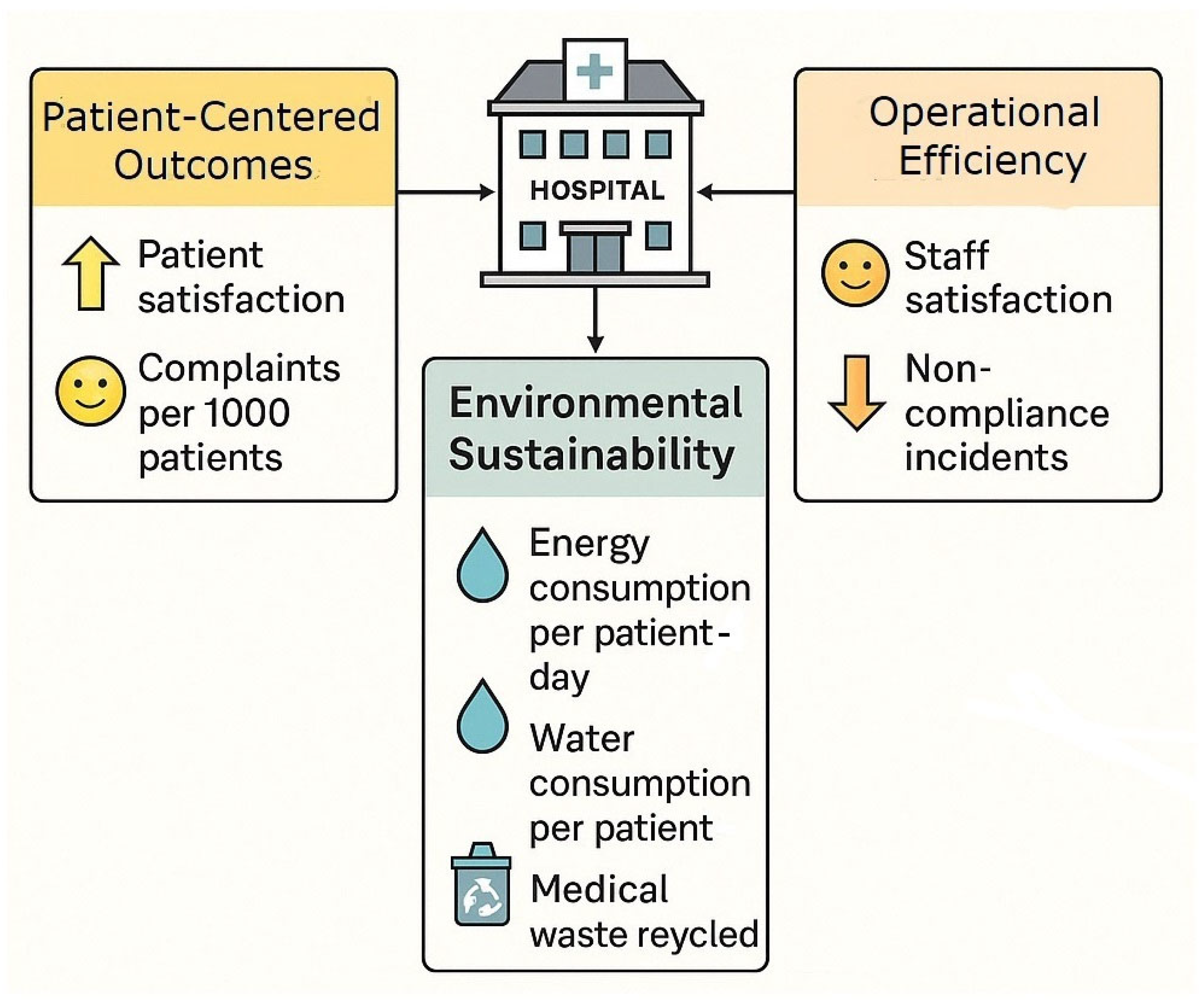
7. Results and Analysis
7.1. Quantitative Results
- Patient satisfaction
- Staff satisfaction
- Energy efficiency
- Water efficiency
- Recycling rate
- Complaint reduction
- Compliance improvement
7.2. Qualitative Insights
7.3. Organizational Culture and Employee Engagement in IMS Implementation
7.4. Long-Term Implications and Benefits of an IMS in Healthcare
7.5. From Implementation to Institutionalization: Sustaining IMSs over Time
8. Discussion
8.1. Integrating Quality and Environmental Management for Strategic Transformation in Healthcare
8.2. Alignment of IMS Outcomes with the United Nations Sustainable Development Goals (SDGs)
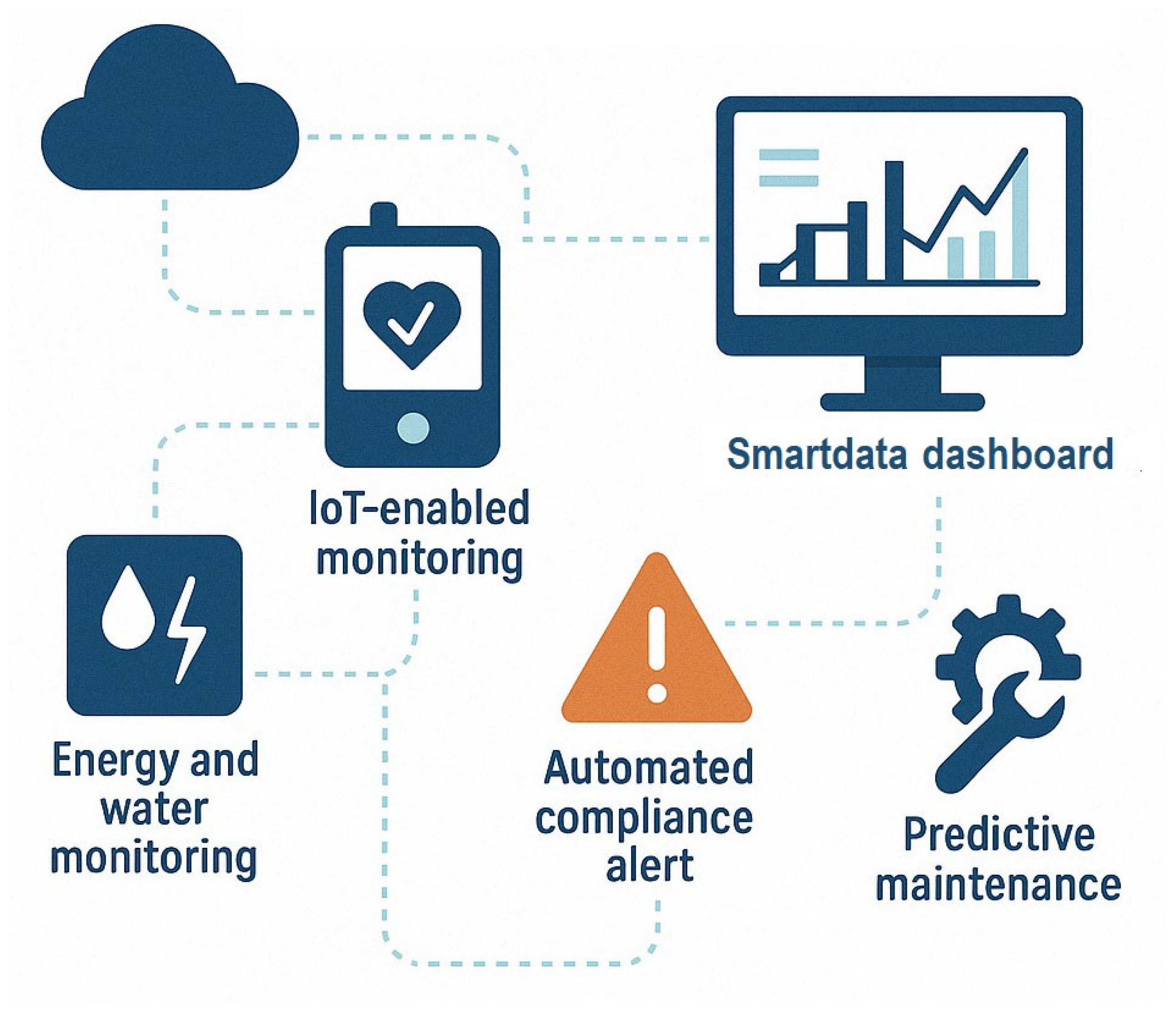
8.3. Digitalization and Smart Healthcare as Enablers of IMS Effectiveness
8.4. Strategic Value and Future Perspectives
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Health Care Without Harm. Health Care’s Climate Footprint. How the Health Sector Contributes to the Global Climate Crisis and Opportunities for Action; Climate-Smart Health Care Series: Green Paper Number One, in Collaboration with Arup. September 2019. Available online: https://global.noharm.org/sites/default/files/documents-files/5961/HealthCaresClimateFootprint_092319.pdf (accessed on 15 April 2025).
- Cristiano, W.; De Marchi, C.; di Domenico, K.; Punzo, O.; Mancini, A.; Mancini, L. The Elephant in the Room in Greenhouse Gases Emissions: Rethinking Healthcare Systems to Face Climate Change. A Rapid Scoping Review. Environ. Sci. Eur. 2024, 36, 24. [Google Scholar] [CrossRef]
- Aljerf, L. Development of a Method for Classification of Hospitals Based on Results of the Diagnosis-Related Groups and the Principle of Case-Mix Index. East. Mediterr. Health J. 2016, 22, 327–334. [Google Scholar] [CrossRef]
- Karliner, J.; Slotterback, S.; Boyd, R.; Ashby, B.; Steele, K.; Wang, J. Health care’s climate footprint: The health sector contribution and opportunities for action. Eur. J. Public Health 2020, 30, ckaa165.843. [Google Scholar] [CrossRef]
- Dutchen, S. Confronting Health Care’s Carbon Footprint. HMS Mag. 2023. Available online: https://magazine.hms.harvard.edu/articles/confronting-health-cares-carbon-footprint (accessed on 19 May 2025).
- Tarí, J.J.; Molina-Azorín, J.F.; Heras, I. Benefits of the ISO 9001 and ISO 14001 Standards: A Literature Review. J. Ind. Eng. Manag. 2012, 5, 297–322. [Google Scholar] [CrossRef]
- Talib, F.; Josaiman, S.K.; Faisal, M.N. An Integrated AHP and ISO14000, ISO26000 Based Approach for Improving Sustainability in Supply Chains. Int. J. Qual. Reliab. Manag. 2021, 38, 1301–1327. [Google Scholar] [CrossRef]
- Shams, K.H.; Talapatra, S.; Islam, F.; Abedin, A. Identification of Benefits from Integrated Management Systems (IMS) to Achieve Sustainability: A Systematic Literature Review. J. Adv. Res. Rev. 2023, 20, 514–529. [Google Scholar] [CrossRef]
- de Souza Barbosa, A.; da Silva, L.B.; Morioka, S.N.; Norte da Silva, J.M. Integrated Management Systems and Organizational Performance: A Multidimensional Perspective. Total Qual. Manag. Bus. Excell. 2023, 34, 1469–1507. [Google Scholar] [CrossRef]
- Sroufe, R.P. Integrated Management Resources Guide. In Integrated Management, 1st ed.; Emerald Publishing Limited: Leeds, UK, 2018; pp. 335–366. [Google Scholar] [CrossRef]
- Ferreira Rebelo, M.; Santos, G.; Silva, R. Integrated Management Systems: Critical Success Factors. J. Glob. Econ. Manag. Bus. Res. 2016, 5, 109–124. [Google Scholar]
- Shahbaz, M.; Gao, C.; Zhai, L.; Shahzad, F.; Khan, I. Environmental air Pollution Management System: Predicting user Adoption Behavior of Big Data Analytics. Technol. Soc. J. 2021, 64, 101473. [Google Scholar] [CrossRef]
- Mezinska, I.; Lapina, I.; Mazais, J. Integrated Management Systems towards Sustainable and Socially Responsible Organization. Total Qual. Manag. Bus. Excell. 2015, 26, 469–481. [Google Scholar] [CrossRef]
- Ramos, D.; Afonso, P.; Rodrigues, M.A. Integrated Management Systems as a Key Facilitator of Occupational Health and Safety Risk Management: A Case Study in a Medium Sized Waste Management Firm. J. Clean. Prod. 2024, 262, 121346. [Google Scholar] [CrossRef]
- Hung, S.-Y.; Chen, C.; Wang, K.-H. Critical Success Factors for the Implementation of Integrated Healthcare Information Systems Projects: An Organizational Fit Perspective. Commun. Assoc. Inf. Syst. 2014, 34, 39. [Google Scholar] [CrossRef]
- Abdulmalek, S.; Nasir, A.; Jabbar, W.A.; Almuhaya, M.A.; Bairagi, A.K.; Khan, M.A.M.; Kee, S.H. IoT-Based Healthcare-Monitoring System towards Improving Quality of Life: A Review. Healthcare 2022, 10, 1993. [Google Scholar] [CrossRef] [PubMed]
- Santamato, V.; Tricase, C.; Faccilongo, N.; Iacoviello, M.; Marengo, A. Exploring the Impact of Artificial Intelligence on Healthcare Management: A Combined Systematic Review and Machine-Learning Approach. Appl. Sci. 2024, 14, 10144. [Google Scholar] [CrossRef]
- Wang, J.; Liu, F. Examining the Link Between Integrated Management Systems and Firm Performance: Do the Integration Strategies Matter? Int. J. Oper. Prod. Manag. 2023, 43, 332–372. [Google Scholar] [CrossRef]
- Wilkinson, G.; Dale, B.G. Integrated Management Systems: A Model Based on a Total Quality Approach. Manag. Serv. Qual. 2001, 11, 318–330. [Google Scholar] [CrossRef]
- Antony, J.; Kaul, A.; Sony, M.; Singh, N.; Vij, P.; Bhat, S.; Yamini, S.; Laureani, A. A study into the themes of quality management: Early findings from a global research project and agenda for future research. TQM J. 2024. ahead-of-print. [Google Scholar] [CrossRef]
- Franchina, V.; Stabile, S.; Cenna, R.; Mannozzi, F.; Federici, I.; Testoni, S.; Sinno, V.; Cagnazzo, C. ISO 9001:2015 Standard Implementation in Clinical Trial Centers: An Exploratory Analysis of Benefits and Barriers in Italy. Contemp. Clin. Trials Commun. 2023, 33, 101104. [Google Scholar] [CrossRef]
- Kyriakeli, G.; Georgiadou, A.; Lithoxopoulou, M.; Tsimtsiou, Z.; Kotsis, V. The Impact of ISO Certification Procedures on Patient Safety Culture in Public Hospital Departments. Healthcare 2025, 13, 661. [Google Scholar] [CrossRef]
- Pohle, A.; Blind, K.; Neustroev, D. The Impact of International Management Standards on Academic Research. Sustainability 2018, 10, 4656. [Google Scholar] [CrossRef]
- Natarajan, D. ISO 9001 Quality Management Systems, 1st ed.; Springer International Publishing: Cham, Switzerland, 2017; pp. 1–250. [Google Scholar] [CrossRef]
- Astrini, N. ISO 9001 and Performance: A Method Review. Total Qual. Manag. Bus. Excell. 2021, 32, 5–32. [Google Scholar] [CrossRef]
- Voorhees, J.; Woellner, R.A. International Environmental Risk Management. ISO 14000 and the Systems Approach, 1st ed.; CRC Press: Boca Raton, FL, USA, 2018; pp. 1–300. [Google Scholar] [CrossRef]
- Welch, T.E. Moving Beyond Environmental Compliance. A Handbook for Integrating Pollution Prevention with ISO 14000, 1st ed.; CRC Press: Boca Raton, FL, USA, 2018; pp. 1–250. [Google Scholar] [CrossRef]
- McGain, F.; Moore, G.; Black, J. Hospital steam sterilizer usage: Could we switch off to save electricity and water? J. Health Serv. Res. Policy 2016, 21, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, N.H.; Khan, S.; Jagtap, S. Waste 4.0: Transforming medical waste management through digitalization and automated segregation. Discov. Sustain. 2024, 5, 353. [Google Scholar] [CrossRef]
- Tian, S.; Yang, W.; Le Grange, J.M.; Wang, P.; Huang, W.; Ye, Z. Smart Healthcare: Making Medical Care More Intelligent. Glob. Health J. 2019, 3, 62–65. [Google Scholar] [CrossRef]
- Resnik, D.B. Standards of Evidence for Institutional Review Board Decision-Making. Account. Res. 2021, 28, 428–455. [Google Scholar] [CrossRef]
- Scott, G.; Hogden, A.; Taylor, R.; Mauldon, E. Exploring the impact of employee engagement and patient safety. Int. J. Qual. Health Care 2022, 34, mzac059. [Google Scholar] [CrossRef]
- Mbunge, E.; Muchemwa, B.; Jiyane, S.; Batani, J. Sensors and Healthcare 5.0: Transformative Shift in Virtual Care through Emerging Digital Health Technologies. Glob. Health J. 2021, 5, 169–177. [Google Scholar] [CrossRef]
- Petkovic, J.; Riddle, A.; Akl, E.A.; Khabsa, J.; Lytvyn, L.; Atwere, P.; Campbell, P.; Chalkidou, K.; Chang, S.M.; Crowe, S.; et al. Protocol for the development of guidance for stakeholder engagement in health and healthcare guideline development and implementation. Syst. Rev. 2020, 9, 21. [Google Scholar] [CrossRef]
- Fraczkiewicz-Wronka, A.; Ingram, T.; Szymaniec-Mlicka, K.; Tworek, P. Risk Management and Financial Stability in the Polish Public Hospitals: The Moderating Effect of the Stakeholders’ Engagement in the Decision-Making. Risks 2021, 9, 87. [Google Scholar] [CrossRef]
- Awewomom, J.; Dzeble, F.; Takyi, Y.D.; Ashie, W.B.; Ettey, E.N.Y.O.; Afua, P.E.; Sackey, L.N.A.; Opoku, F.; Akoto, O. Addressing global environmental pollution using environmental control techniques: A focus on environmental policy and preventive environmental management. Discov. Environ. 2024, 2, 8. [Google Scholar] [CrossRef]
- Eckelman, M.J.; Sherman, J.D.; MacNeill, A.J. Life Cycle Environmental Emissions and Health Damages from the Canadian Healthcare System: An Economic-Environmental-Epidemiological Analysis. PLoS Med. 2018, 15, e1002623. [Google Scholar] [CrossRef] [PubMed]
- Windfeld, E.S.; Su-Ling Brooks, M. Medical Waste Management—A Review. J. Environ. Manag. 2015, 163, 98–108. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Ogunseitan, O.A.; Tang, Y. Medical Waste: Current Challenges and Future Opportunities for Sustainable Management. Crit. Rev. Environ. Sci. Technol. 2022, 52, 2000–2022. [Google Scholar] [CrossRef]
- Kumar, S.; Tarei, P.K.; Swarnakar, V. Analyzing Barriers to Sustainable Healthcare Waste Disposal: A Hybrid Decision-Making Framework. Benchmark. Int. J. 2024. ahead-of-print. [Google Scholar] [CrossRef]
- WHO. Health-Care Waste. World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/health-care-waste (accessed on 22 May 2025).
- Senge, P.M. The Fifth Discipline: The Art and Practice of the Learning Organization; Doubleday: New York, NY, USA, 1990. [Google Scholar]
- Pfeffer, J.; Sutton, R.I. Hard Facts, Dangerous Half-Truths, and Total Nonsense: Profiting from Evidence-Based Management; Harvard Business Press: Boston, MA, USA, 2006. [Google Scholar]
- Franco, A.; Shaker, M.; Kalubi, D.; Hostettler, S. A Review of Sustainable Energy Access and Technologies for Healthcare Facilities in the Global South. Sustain. Energy Technol. Assess. 2017, 22, 92–105. [Google Scholar] [CrossRef]
- Saleem, H.; Khan, M.B.; Shabbir, M.S. Nexus between Non-Renewable Energy Production, CO2 Emissions, and Healthcare Spending in OECD Economies. Environ. Sci. Pollut. Res. 2022, 29, 47286–47297. [Google Scholar] [CrossRef]
- Ghaffarianhoseini, A.; Berardi, U.; AlWaer, H.; Chang, S.; Halawa, E.; Ghaffarianhoseini, A.; Clements-Croome, D. What is an Intelligent Building? Analysis of Recent Interpretations from an International Perspective. Archit. Sci. Rev. 2018, 61, 298–307. [Google Scholar] [CrossRef]
- Borges de Oliveira, K.; Ferro dos Santos, E.; Faria Neto, A.; de Mello Santos, V.H.; de Oliveira, O.J. Guidelines for Efficient and Sustainable Energy Management in Hospital Buildings. J. Clean. Prod. 2021, 321, 129644. [Google Scholar] [CrossRef]
- Psillaki, M.; Apostolopoulos, N.; Makris, I.; Liargovas, P.; Apostolopoulos, S.; Dimitrakopoulos, P.; Sklias, G. Hospitals’ Energy Efficiency in the Perspective of Saving Resources and Providing Quality Services through Technological Options: A Systematic Literature Review. Energies 2023, 16, 755. [Google Scholar] [CrossRef]
- Lenzen, M.; Malik, A.; Li, M. The Environmental Footprint of Health Care: A Global Assessment. Lancet Planet. Health 2020, 4, e271–e279. [Google Scholar] [CrossRef]
- Lee, S.M.; Lee, D. Developing Green Healthcare Activities in the Total Quality Management Framework. Int. J. Environ. Res. Public Health 2022, 19, 6504. [Google Scholar] [CrossRef] [PubMed]
- Krause, S.; Joel, E.; Schaum, C.; Bäumer, J.; Rücker, N.; Wienand, I.; Sturm, C.; Jahn-Mühl, B.; Geiger, M.; Fekete, A.; et al. Water Safety Planning for Healthcare Facilities for Extreme Events. J. Water Health 2024, 22, 77–96. [Google Scholar] [CrossRef] [PubMed]
- Inkster, T.; Walker, J.; Weinbren, M. Water-Free Patient Care: A Narrative Review of the Literature and Discussion of the Pressing Need for a Way Forward. J. Hosp. Infect. 2024, 152, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Verlicchi, P. (Ed.) Hospital Wastewaters: Characteristics, Management, Treatment and Environmental Risks; Springer: Cham, Switzerland, 2018. [Google Scholar]
- Dancer, S.J. Controlling Hospital-Acquired Infection: Focus on the Role of the Environment and New Technologies for Decontamination. Clin. Microbiol. Rev. 2014, 27, 665–690. [Google Scholar] [CrossRef]
- Naranjo-Gil, D. Accomplishing Water Strategy Policies in Hospitals: The Role of Management Information Systems and Managerial Styles. Water 2017, 9, 107. [Google Scholar] [CrossRef]
- Miron Batista, K.J.; da Silva, S.R.; Rahnemay Kohlman Rabbani, E.; Zlatar, T. Systematic review of indicators for the assessment of water consumption rates at hospitals. Water Supply 2020, 20, 373–382. [Google Scholar] [CrossRef]
- Kruk, M.E.; Gage, A.D.; Arsenault, C. High-Quality Health Systems in the Sustainable Development Goals Era: Time for a Revolution. Lancet Glob. Health 2018, 6, e1196–e1252. [Google Scholar] [CrossRef]
- Kokangul, A. A Combination of Deterministic and Stochastic Approaches to Optimize Bed Capacity in a Hospital Unit. Comput. Methods Programs Biomed. 2008, 90, 56–65. [Google Scholar] [CrossRef]
- WHO. Prevention of Hospital-Acquired Infections: A Practical Guide, 2nd ed.; Ducel, G., Fabry, J., Nicolle, L., Eds.; World Health Organization: Geneva, Switzerland, 2002; Available online: https://iris.who.int/handle/10665/67350 (accessed on 22 May 2025).
- Sun, B.C.; Hsia, R.Y.; Weiss, R.E.; Zingmond, D.; Liang, L.J.; Han, W.; McCreath, H.; Asch, S.M. Effect of Emergency Department Crowding on Outcomes of Admitted Patients. Ann. Emerg. Med. 2013, 61, 605–611. [Google Scholar] [CrossRef]
- Kripalani, S.; Jackson, A.T.; Schnipper, J.L.; Coleman, E.A. Promoting Effective Transitions of Care at Hospital Discharge: A Review of Key Issues for Hospitalists. J. Hosp. Med. 2007, 2, 314–323. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Boone, S.; Tan, L.; Dyrbye, L.N.; Sotile, W.; Satele, D.; Sloan, J.; Oreskovich, M.R. Burnout and Satisfaction with Work-Life Balance Among US Physicians Relative to the General US Population. Arch. Intern. Med. 2015, 172, 1377–1385. [Google Scholar] [CrossRef] [PubMed]
- Aiken, L.H.; Clarke, S.P.; Sloane, D.M.; Sochalski, J.; Silber, J.H. Hospital Nurse Staffing and Patient Mortality, Nurse Burnout, and Job Dissatisfaction. JAMA 2002, 288, 1987–1993. [Google Scholar] [CrossRef] [PubMed]
- Lawton, R.; McEachan, R.R.C.; Giles, S.J.; Sirriyeh, R.; Watt, I.S.; Wright, J. Development of an evidence-based framework of factors contributing to patient safety incidents in hospital settings: A systematic review. BMJ Qual. Saf. 2012, 21, 369–380. [Google Scholar] [CrossRef] [PubMed]
- Kerrissey, M.; Satterstrom, P.; Leydon, N. Integrating a Managerial Practice That Enables Implementation in Fragmented Health Care Environments. Health Care Manag. Rev. 2017, 42, 213–225. [Google Scholar] [CrossRef]
- Shahbaz, M.; Gao, C.; Zhai, L. Investigating the Adoption of Big Data Analytics in Healthcare: The Moderating Role of Resistance to Change. J. Big Data 2019, 6, 6. [Google Scholar] [CrossRef]
- de Wit, K.; Curran, J.; Thoma, B. Review of Implementation Strategies to Change Healthcare Provider Behaviour in the Emergency Department. Can. J. Emerg. Med. 2018, 20, 453–460. [Google Scholar] [CrossRef]
- Byhoff, E.; LeClair, A.M.; Smith, C.N. Designing an Implementation Strategy to Increase Health-Related Social Needs Screening: Applying the PRISM Framework in a Resource-Limited Clinical Setting. Transl. Behav. Med. 2024, 14, 197–205. [Google Scholar] [CrossRef]
- Auschra, C. Barriers to the Integration of Care in Inter-Organizational Settings: A Literature Review. Int. J. Integr. Care 2018, 18, 5. [Google Scholar] [CrossRef]
- Gonzalez-Pizarro, P.; Brazzi, L.; Koch, S. European Society of Anaesthesiology and Intensive Care Consensus Document on Sustainability: 4 Scopes to Achieve a More Sustainable Practice. Eur. J. Anaesthesiol. 2021, 41, 260–277. [Google Scholar] [CrossRef]
- Provost, L.P.; Murray, S.K. The Health Care Data Guide: Learning from Data for Improvement, 2nd ed.; John Wiley & Sons: New York, NY, USA, 2022; pp. 1–432. [Google Scholar]
- Enticott, J.; Johnson, A.; Teede, H. Learning Health Systems Using Data to Drive Healthcare Improvement and Impact: A Systematic Review. BMC Health Serv. Res. 2021, 21, 200. [Google Scholar] [CrossRef]
- Cascini, F.; Santaroni, F.; Lanzetti, R.; Failla, G.; Gentili, A.; Ricciardi, W. Developing a Data-Driven Approach in Order to Improve the Safety and Quality of Patient Care. Front. Public Health 2021, 9, 667819. [Google Scholar] [CrossRef] [PubMed]
- Willmington, C.; Belardi, P.; Murante, A.M.; Vainieri, M. The Contribution of Benchmarking to Quality Improvement in Healthcare. A Systematic Literature Review. BMC Health Serv. Res. 2022, 22, 139. [Google Scholar] [CrossRef] [PubMed]
- Williamson, S.M.; Prybutok, V. Balancing Privacy and Progress: A Review of Privacy Challenges, Systemic Oversight, and Patient Perceptions in AI-Driven Healthcare. Appl. Sci. 2024, 14, 675. [Google Scholar] [CrossRef]
- Gerek, Y.; Aydin, M.N. Management Frameworks and Management System Standards in the Context of Integration and Unification: A Review and Classification of Core Building Blocks for Consilience. Systems 2025, 13, 234. [Google Scholar] [CrossRef]
- Yin, R.K. Case Study Research: Design and Methods, 3rd ed.; Sage Publications: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Eisenhardt, K.M.; Graebner, M.E. Theory Building from Cases: Opportunities and Challenges. Acad. Manag. J. 2007, 50, 25–32. [Google Scholar] [CrossRef]
- de Nadae, J.; Carvalho, M.M.; Vieira, D.R. Integrated Management Systems as a Driver of Sustainability Performance: Exploring Evidence From Multiple-Case Studies. Int. J. Qual. Reliab. Manag. 2021, 38, 800–821. [Google Scholar] [CrossRef]
- Vieira Nunhes, T.; Espuny, M.; Lauá Reis Campos, T.; Santos, G.; Bernardo, M.; Oliveira, O.J. Guidelines to Build the Bridge Between Sustainability and Integrated Management Systems: A Way to Increase Stakeholder Engagement Toward Sustainable Development. Corp. Soc. Responsib. Environ. Manag. 2022, 29, 1617–1635. [Google Scholar] [CrossRef]
- Hadian, S.A.; Rezayatmand, R.; Shaarbafchizadeh, N. Hospital Performance Evaluation Indicators: A Scoping Review. BMC Health Serv. Res. 2024, 24, 561. [Google Scholar] [CrossRef]
- da Silva Fernandes, R.; Rodrigues da Rocha, T.; Mendes Coelho, J.; de Andrade, D.F. Development of a Measurement Instrument to Evaluate Integrated Management Systems and Differences in Perception: An Approach to Item Response Theory and the Quality Management Process. Production 2023, 33, e20220069. [Google Scholar] [CrossRef]
- Sippy, R.; Efstathopoulou, L.; Simes, E.; Davis, M.; Howell, S.; Morris, B.; Owrid, O.; Stoll, N.; Fonagy, P.; Moore, A. Effect of a Needs-Based Model of Care on the Characteristics of Healthcare Services in England: The i-THRIVE National Implementation Programme. Epidemiol. Psychiatr. Sci. 2023, 34, e21. [Google Scholar] [CrossRef]
- Salgado, H.O.; Andreucci, C.B.; Gomes, A.C.R. The Perinatal Bereavement Project: Development and Evaluation of Supportive Guidelines for Families Experiencing Stillbirth and Neonatal Death in Southeast Brazil—A Quasi-Experimental Before-and-After Study. Reprod. Health 2021, 18, 5. [Google Scholar] [CrossRef] [PubMed]
- Darzi, M.A. Overcoming Barriers to Integrated Management Systems via Developing Guiding Principles Using G-AHP and F-TOPSIS. Expert Syst. Appl. 2024, 239, 122305. [Google Scholar] [CrossRef]
- Domingues, P.; Sampaio, P.; Arezes, P.M. Integrated Management Systems Assessment: A Maturity Model Proposal. J. Clean. Prod. 2016, 124, 164–174. [Google Scholar] [CrossRef]
- Reynolds, K.A.; Harikumar, V.B.; Poon, E. While Ethical Considerations Predominate, Scientific Merit Can Impact Institutional Review Board (IRB) Determinations: A Cross-Sectional Study. J. Clin. Epidemiol. 2022, 150, 12–17. [Google Scholar] [CrossRef]
- González, A.G.; García-Sanz-Calcedo, J.; Salgado, D.R. Evaluation of Energy Consumption in German Hospitals: Benchmarking in the Public Sector. Energies 2018, 11, 2279. [Google Scholar] [CrossRef]
- Attrah, M.; Elmanadely, A.; Akter, D.; Rene, E.R. A Review on Medical Waste Management: Treatment, Recycling, and Disposal Options. Environments 2022, 9, 146. [Google Scholar] [CrossRef]
- Steeb, T.; Wessely, A.; Merkl, H.; Kirchberger, M.C.; Voskens, C.; Erdmann, M.; Heinzerling, L.; Berking, C.; Heppt, M.V. I Feel I’m in Best Hands with You!: A Survey of Patient Satisfaction in a German University Skin Cancer Centre. Acta Derm. Venereol. 2021, 101, 655. [Google Scholar] [CrossRef]
- Marino, A.; Pariso, P.; Picariello, M. Organizational and Energy Efficiency Analysis of Italian Hospitals and Identification of Improving AI Solutions. Int. J. Energy Econ. Policy 2024, 14, 628–640. [Google Scholar] [CrossRef]
- Ruggieri, T.G.; Berta, P.; Murante, A.M.; Nuti, S. Patient Satisfaction, Patients Leaving Hospital Against Medical Advice and Mortality in Italian University Hospitals: A Cross-Sectional Analysis. BMC Health Serv. Res. 2018, 18, 51. [Google Scholar] [CrossRef]
- Madar, A.; Neacșu, N.A. The Importance of Implementing the Quality Management System and Using Quality Strategies to Improve the Quality of Medical Services and Increase Customer Satisfaction. Sciendo 2021, 15, 1150–1161. [Google Scholar] [CrossRef]
- Szabó, S.; Feier, B.; Capatina, D.; Tertis, M.; Cristea, C.; Popa, A. An Overview of Healthcare-Associated Infections and Their Detection Methods Caused by Pathogen Bacteria in Romania and Europe. J. Clin. Med. 2022, 11, 3204. [Google Scholar] [CrossRef]
- Trinca, V.-T. Romanian Municipalities and the Smart City Framework. Rev. Int. Comp. Manag. 2023, 24, 637–649. [Google Scholar] [CrossRef]
- Blobel, B.; Ruotsalainen, P.; Oemig, F.; Giacomini, M.; Sottile, P.A.; Endsleff, F. Principles and Standards for Designing and Managing Integrable and Interoperable Transformed Health Ecosystems. J. Pers. Med. 2023, 13, 1579. [Google Scholar] [CrossRef] [PubMed]
- Vieira Nunhes, T.; Bernardo, M.; Oliveira, O.J. Guiding Principles of Integrated Management Systems: Towards Unifying a Starting Point for Researchers and Practitioners. J. Clean. Prod. 2019, 210, 977–993. [Google Scholar] [CrossRef]
- Silva, C.; Magano, J.; Moskalenko, A.; Nogueira, T.; Dinis, M.A.P.; Pedrosa e Sousa, H.F. Sustainable Management Systems Standards (SMSS): Structures, Roles, and Practices in Corporate Sustainability. Sustainability 2020, 12, 5892. [Google Scholar] [CrossRef]
- Hariyani, D.; Hariyani, P.; Mishra, S.; Sharma, M.K. A Review of the Structured Framework for Sustainability Audits in Manufacturing Organizations. GRETS 2025, 3, 100170. [Google Scholar] [CrossRef]
- Hut-Mossel, L.; Ahaus, K.; Welker, G.; Gans, R. Understanding How and Why Audits Work in Improving the Quality of Hospital Care: A systematic Realist Review. PLoS ONE 2021, 16, e0248677. [Google Scholar] [CrossRef]
- Melo e Castro, J.; Monteiro, M.H. Unlocking Healthcare 4.0: Navigating Critical Success Factors for Effective Integration in Health Systems. Adv. Med. Sci. Int. J. 2024, 11, 1–14. [Google Scholar] [CrossRef]
- Dion, H.; Evans, M. Strategic Frameworks for Sustainability and Corporate Governance in Healthcare Facilities; Approaches to Energy-Efficient Hospital Management. Benchmark. Int. J. 2024, 31, 353–390. [Google Scholar] [CrossRef]
- Masud, F.N.; Sasangohar, F.; Ratnani, I.; Fatima, S.; Hernandez, M.A.; Riley, T.; Fischer, J.; Dhala, A.; Gooch, M.E.; Keeling-Johnson, K. Past, Present, and Future of Sustainable Intensive Care: Narrative Review and a Large Hospital System Experience. Crit. Care 2024, 28, 154. [Google Scholar] [CrossRef]
- Myin-Germeys, I.; Schick, A.; Ganslandt, T. The Experience Sampling Methodology as a Digital Clinical Tool for More Person-Centered Mental Health Care: An Implementation Research Agenda. Psychol. Med. 2024, 54, 2785–2793. [Google Scholar] [CrossRef] [PubMed]
- Khodabakhshian, N.; Gaeul Lee, K.; Marawi, T. Virtual Reality for Developing Patient-Facing Communication Skills in Medical and Graduate Education: Protocol for a Scoping Review. JMIR Res. Protoc. 2024, 13, e53901. [Google Scholar] [CrossRef] [PubMed]
- Fausett, C.M.; Korentsides, J.M.; Miller, Z.N.; Keebler, J.R. Adaptive Leadership in Health Care Organizations: Five Insights to Promote Effective Teamwork. Psychol. Lead. Lead. 2024, 27, 6–26. [Google Scholar] [CrossRef]
- Ennis-O’Connor, M.; O’Connor, W.T. Charting the Future of Patient Care: A Strategic Leadership Guide to Harnessing the Potential of Artificial Intelligence. Healthc. Manag. Forum 2024, 37, 290–295. [Google Scholar] [CrossRef]
- WHO. State of the World’s Nursing 2020: Investing in Education, Jobs and Leadership; World Health Organisation: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications/i/item/9789240003279 (accessed on 23 May 2025).
- Löfqvist, N. Enhancing Capability for Continuous Organisational Improvement and Learning in Healthcare Organisations: A Systematic Review of the Literature 2013–2022. BMJ Open Qual. 2024, 13, e002566. [Google Scholar] [CrossRef]
- Reeves, S.; Pelone, F.; Harrison, R.; Goldman, J.; Zwarenstein, M. Interprofessional Collaboration to Improve Professional Practiceand Healthcare Outcomes (Review). Cochrane Database Syst. Rev. 2017, 6, CD000072. [Google Scholar] [CrossRef]
- Krczal, E.; Behrens, D.A. Trust-Building in Temporary Public Health Partnerships: A Qualitative Study of the Partnership Formation Process of a Covid-19 Test, Trace and Protect Service. BMC Health Serv. Res. 2024, 24, 467. [Google Scholar] [CrossRef]
- Karikumpu, V.; Häggman-Laitila, A.; Romppanen, J. Trust in the Leader and Trust in the Organization in Healthcare: A Concept Analysis Based on a Systematic Review. J. Nurs. Manag. 2024, 2024, 8776286. [Google Scholar] [CrossRef]
- Culot, G.; Nassimbeni, G.; Podrecca, M.; Sartor, M. The ISO/IEC 27001 Information Security Management Standard: Literature Review and Theory-Based Research Agenda. TQM J. 2021, 33, 76–105. [Google Scholar] [CrossRef]
- Simon, A. Organizational Citizenship Behavior for Integrated Management Systems Performance. Environ. Eng. Manag. J. 2023, 22, 2117–2126. [Google Scholar] [CrossRef]
- Jeyar, M.; El Moudden, A.; Taouab, O. Healthcare Service Quality Management: Evidence from Morocco. Int. J. Appl. Econ. Finance Account. 2024, 19, 196–2015. [Google Scholar] [CrossRef]
- Deepa, N.R.; Naikodi, T.A.; Bhagyashree, L.C.R.P.; Baby, D.; Neeraj, S.C.; Umar, M. The Impact of Sustainable Development Goals on Healthcare and Nursing Care Delivery: A Comprehensive Review Article. Int. J. Nurs. Health Sci. 2025, 7, 11–17. [Google Scholar] [CrossRef]
- Aftab, W.; Siddiqui, F.J.; Tasic, H.; Perveen, S.; Siddiqi, S.; Bhutta, Z.A. Implementation of Health and Health-Related Sustainable Development Goals: Progress, Challenges and Opportunities—A Systematic Literature Review. BMJ Glob. Health 2020, 5, e002273. [Google Scholar] [CrossRef] [PubMed]
- Griffith, A.; Bhutto, K. Better Environmental Performance: A Framework for Integrated Management Systems (IMS). Manag. Environ. Qual. 2009, 20, 566–580. [Google Scholar] [CrossRef]
- Aggarwal, R.; Visram, S.; Martin, G.; Sounderajah, V.; Gautama, S.; Jarrold, K.; Klaber, R.; Maxwell, S.; Neal, J.; Pegg, J.; et al. Defining the Enablers and Barriers to the Implementation of Large-scale, Health Care–Related Mobile Technology: Qualitative Case Study in a Tertiary Hospital Setting. JMIR Mhealth Uhealth 2022, 10, e31497. [Google Scholar] [CrossRef]
- Stefan, A.-M.; Rusu, N.-R.; Ovreiu, E.; Ciuc, M. Empowering Healthcare: A Comprehensive Guide to Implementing a Robust Medical Information System—Components, Benefits, Objectives, Evaluation Criteria, and Seamless Deployment Strategies. Appl. Syst. Innov. 2024, 7, 51. [Google Scholar] [CrossRef]
- Bevere, D.; Faccilongo, N. Shaping the Future of Healthcare: Integrating Ecology and Digital Innovation. Sustainability 2024, 16, 3835. [Google Scholar] [CrossRef]
- Mannion, R.; Davies, H. Understanding Organizational Culture for Healthcare Quality Improvement. BMJ 2018, 363, k4907. [Google Scholar] [CrossRef]
- King, W.R. Knowledge Management and Organizational Learning. Springer: Berlin/Heidelberg, Germany. [CrossRef]
- Santos Geraidine, R.; Ferreira da Silva, L. Healthcare Ecosystem Integrated Project Management Oriented to the Patient Journey: A Systematic Literature Review. Int. J. Manag. Proj. Bus. 2025, 18, 353–387. [Google Scholar] [CrossRef]
- Ikram, M.; Sroufe, R.; Zhang, Q. Prioritizing and Overcoming Barriers to Integrated Management System (IMS) Implementation using AHP and G-TOPSIS. J. Clean. Prod. 2020, 254, 120121. [Google Scholar] [CrossRef]
- Leal Filho, W.; Sigahi, T.F.A.C.; Anholon, R.; Gasparetto Rebelatto, B.; Schmidt-Ross, I.; Hensel-Börner, S.; Franco, D.; Treacy, T.; Londero Brandli, L. Promoting Sustainable Development Via Stakeholder Engagement in Higher Education. Environ. Sci. Eur. 2025, 37, 64. [Google Scholar] [CrossRef]
- van Schie, V. Governance Related Factors Influencing the Implementation of Sustainability in Hospitals: A Systematic Literature Review. Health Policy 2024, 146, 105115. [Google Scholar] [CrossRef] [PubMed]
- Jayashree, P.; El Barachi, M.; Hamza, F. Practice of Sustainability Leadership: A Multi-Stakeholder Inclusive Framework. Sustainability 2022, 14, 6346. [Google Scholar] [CrossRef]
- Lepore, D.; Dolui, K.; Tomashchuk, O.; Shim, H.; Puri, C.; Li, Y.; Chen, N.; Spigarelli, F. Interdisciplinary Research Unlocking Innovative Solutions in Healthcare. Technovation 2023, 120, 102511. [Google Scholar] [CrossRef]
- Jeffries, P.R.; Bushardt, R.L.; DuBose-Morris, R.; Hood, C.; Kardong-Edgren, S.; Pintz, C.; Posey, L.; Sikka, N. The Role of Technology in Health Professions Education during the COVID-19 Pandemic. Acad. Med. 2022, 97, S104–S109. [Google Scholar] [CrossRef]
- Realyvásquez-Vargas, A.; Arredondo-Soto, K.C.; Carrillo-Gutiérrez, T.; Ravelo, G. Applying the Plan-Do-Check-Act (PDCA) Cycle to Reduce the Defects in the Manufacturing Industry. A Case Study. Appl. Sci. 2018, 8, 2181. [Google Scholar] [CrossRef]
- Muzaimi, H.; Chew, B.C.; Hamid, S.R. Integrated management system: The integration of ISO 9001, ISO 14001, OHSAS 18001 and ISO 31000. AIP Conf. Proc. 2017, 1818, 020034. [Google Scholar] [CrossRef]
- Baker, J. The Technology–Organization–Environment Framework. In Information Systems Theory. Integrated Series in Information Systems; Dwivedi, Y., Wade, M., Schneberger, S., Eds.; Springer: New York, NY, USA, 2012; Volume 28. [Google Scholar] [CrossRef]


| Aspect | ISO 9001 (Quality Management) | ISO 14001 (Environmental Management) | Integration in an IMS |
|---|---|---|---|
| Purpose | Ensures consistent quality and continuous improvement in healthcare | Controls environmental impacts and improves sustainability | Aligns quality and environmental objectives for holistic performance |
| Core principles | Customer focus, leadership, process approach, improvement | Compliance, pollution prevention, resource optimization | Shared commitment to continuous improvement and stakeholder satisfaction |
| Main activities | Clinical process control, audits, corrective actions, risk management | Identification of environmental aspects, monitoring, legal compliance | Unified auditing, documentation, and corrective actions |
| Key outcomes | Improved patient safety and satisfaction | Reduced waste, emissions, and resource use | Enhanced efficiency, accountability, and stakeholder trust |
| Structural framework | High-level structure (Annex SL) | High-level structure (Annex SL) | Facilitates harmonization through common clauses and terminology |
| Application in healthcare | Clinical governance, infection control, and service quality | Waste management, energy and water efficiency, and environmental hygiene | Encourages cross-departmental collaboration and strategic alignment |
| Hospital ID | Country | Type | Size (Approx. Beds) | Core Services |
|---|---|---|---|---|
| A | Germany | Regional pediatric hospital | 350 | General pediatric care, support departments |
| B | Italy | University teaching hospital | 900 | Tertiary care, emergency, outpatient services |
| C | Romania | Public hospital | 250 | General services, regulatory compliance focus |
| Indicator | Before IMS | After IMS | % Change | Industry Benchmark (Range) | Reference Source |
|---|---|---|---|---|---|
| Patient satisfaction score (0–10) | 6.9 | 8.3 | +20.3 | 7.0–8.5 | WHO, national health agencies |
| Staff satisfaction index (%) | 62 | 75 | +21.0 | 65–80 | EU-funded workforce surveys |
| Energy use per patient-day (kWh) | 2.4 | 1.8 | −25.0 | 1.8–2.6 | [88] |
| Water use per patient-day (liters) | 165 | 125 | −24.2 | 120–170 | [46] |
| Medical waste recycled (%) | 24 | 47 | +95.8 | 30–50 | [1,89] |
| Patient complaints per 1000 patients | 15 | 9 | −40.0 | 10–20 | Hospital quality audits |
| Non-compliance incidents per year | 11 | 4 | −63.6 | <10 | Institutional benchmarks |
| KPI Category | Hospital A | Hospital B | Hospital C |
|---|---|---|---|
| Energy consumption | ↓ 28% total energy | ↓ 25% per patient-day | ↓ ~17% total consumption |
| Medical waste recycling | ↑ 31% | ↑ 25% | ↑ 42% |
| Compliance incidents | ↓ 22% | ↓ 18% | ↓ 35% |
| Internal audit completion | ↑ from 70% to 100% | ↑ from 60% to 90% | ↑ from 50% to 95% |
| Patient satisfaction (score) | ↑ 12% (post-implementation) | ↑ 15% | ↑ 10% |
| Performance Domain | Before IMS | After IMS | % Change |
|---|---|---|---|
| Quality (e.g., satisfaction, complaints) | 64 | 82 | +28.1 |
| Environmental (e.g., energy, water, waste) | 55 | 78 | +41.8 |
| Engagement (e.g., staff satisfaction) | 62 | 75 | +21.0 |
| Process (e.g., compliance, audit readiness) | 58 | 83 | +43.1 |
| IMS Outcome/Impact | Relevant SDG(s) | Contribution Description |
|---|---|---|
| Increased patient satisfaction and improved care quality | SDG 3—Good health and well-being | Enhances patient-centered service delivery, safety, and experience |
| Higher staff satisfaction and cross-departmental collaboration | SDG 8—Decent work and economic growth | Fosters improved working conditions, employee engagement, and institutional resilience |
| Reduced energy consumption per patient-day | SDG 12—Responsible consumption and production SDG 13—Climate action | Promotes energy efficiency and supports climate mitigation efforts |
| Lower water consumption per patient-day | SDG 6—Clean water and sanitation | Encourages responsible water use without compromising hygiene and infection control |
| Increase in medical waste recycling rates | SDG 12—Responsible consumption and production SDG 3—Good health and well-being | Reduces the environmental impact of healthcare waste and improves sanitation and public health outcomes |
| Fewer compliance incidents and improved documentation practices | SDG 16—Peace, justice, and strong institutions | Strengthens institutional transparency, accountability, and regulatory alignment |
| Adoption of integrated, cross-functional management practices | SDG 17—Partnerships for the goals | Encourages interdisciplinary collaboration and systems thinking in support of the Sustainable Development Goals |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simion Ludușanu, D.-G.; Fertu, D.-I.; Tinică, G.; Gavrilescu, M. Integrated Quality and Environmental Management in Healthcare: Impacts, Implementation, and Future Directions Toward Sustainability. Sustainability 2025, 17, 5156. https://doi.org/10.3390/su17115156
Simion Ludușanu D-G, Fertu D-I, Tinică G, Gavrilescu M. Integrated Quality and Environmental Management in Healthcare: Impacts, Implementation, and Future Directions Toward Sustainability. Sustainability. 2025; 17(11):5156. https://doi.org/10.3390/su17115156
Chicago/Turabian StyleSimion Ludușanu, Dana-Gabriela, Daniela-Ionela Fertu, Grigore Tinică, and Maria Gavrilescu. 2025. "Integrated Quality and Environmental Management in Healthcare: Impacts, Implementation, and Future Directions Toward Sustainability" Sustainability 17, no. 11: 5156. https://doi.org/10.3390/su17115156
APA StyleSimion Ludușanu, D.-G., Fertu, D.-I., Tinică, G., & Gavrilescu, M. (2025). Integrated Quality and Environmental Management in Healthcare: Impacts, Implementation, and Future Directions Toward Sustainability. Sustainability, 17(11), 5156. https://doi.org/10.3390/su17115156







