Under Fire: A Brazilian Perspective on Climate Change and Child Health
Abstract
1. Introduction
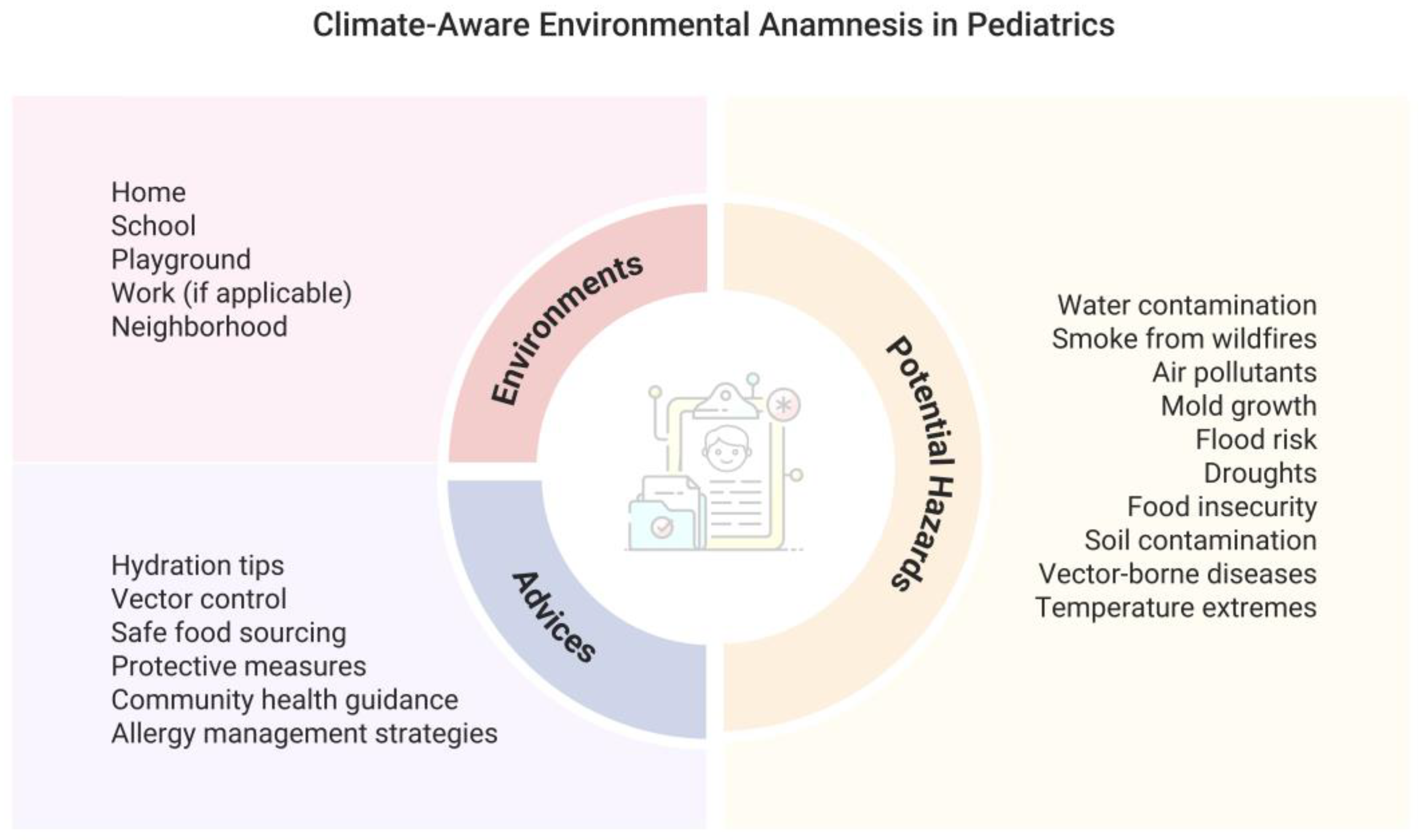
2. Environmental History in Pediatric Care
3. The Impact of Pollution and Climate Extremes on the Pediatric Population
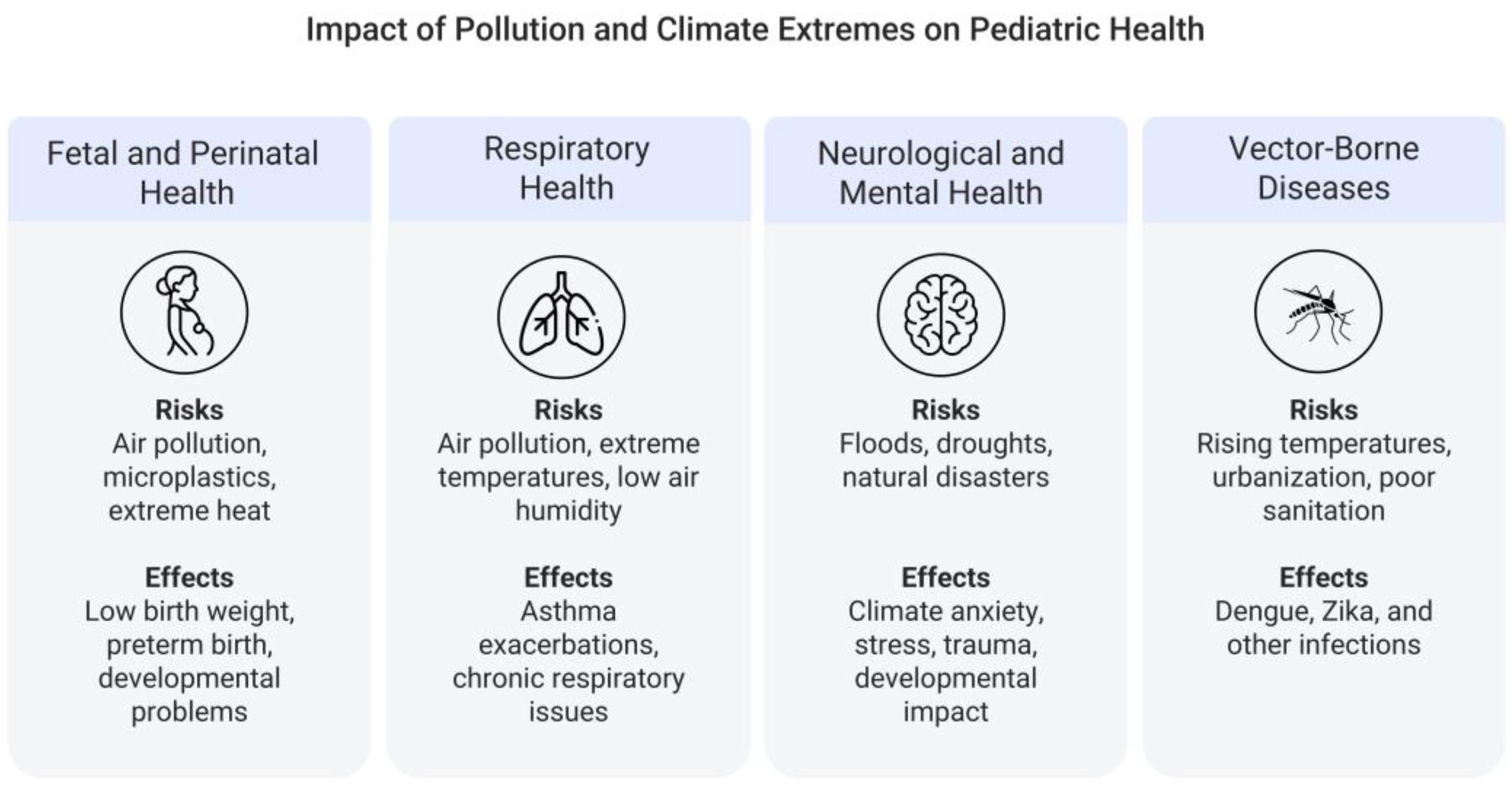
3.1. Fetal and Perinatal Health
3.2. Respiratory Health
3.3. Neurological Development and Mental Health
3.4. Increase in Vector-Borne Diseases
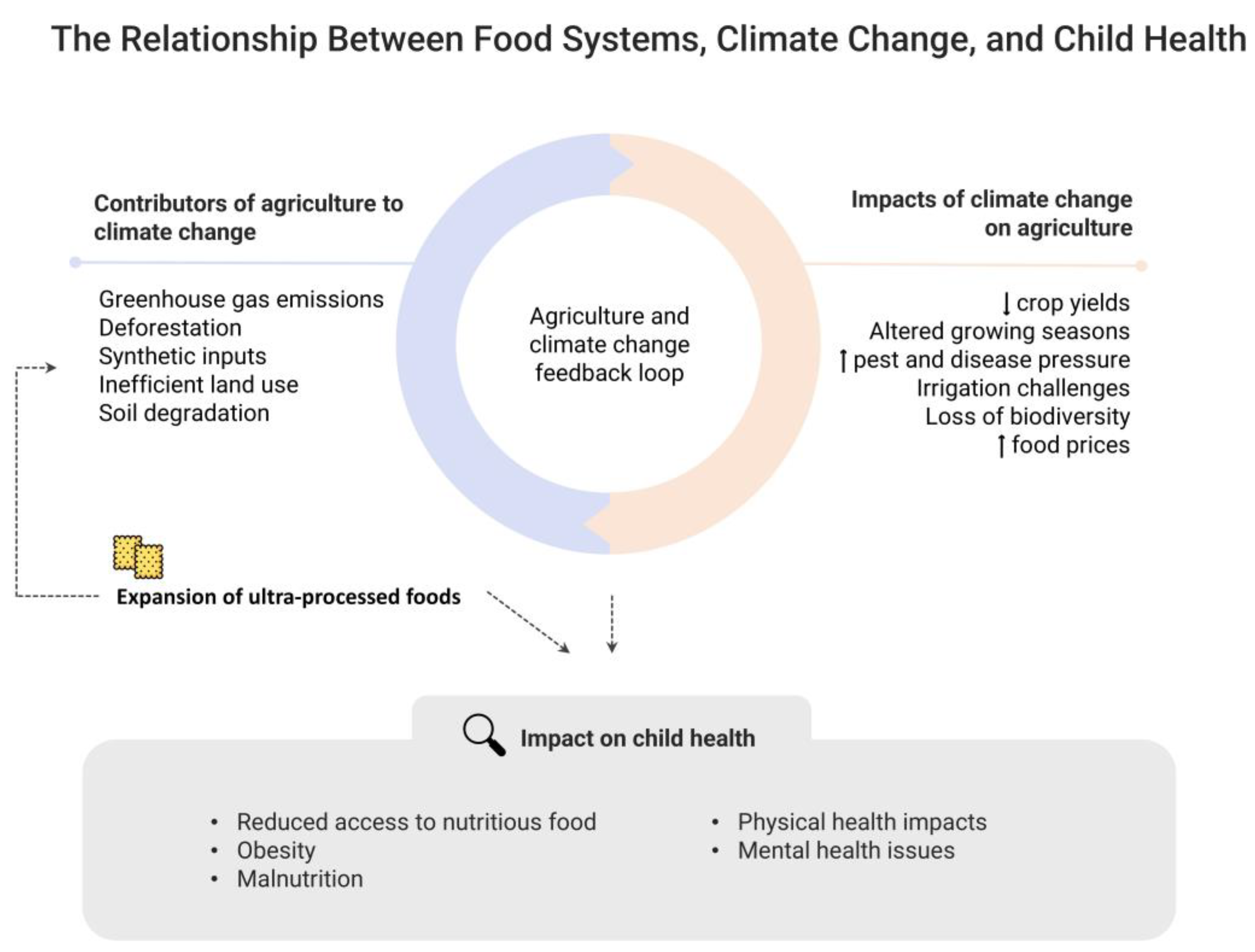
4. Food Systems, Climate Change, Food Security and Child Nutrition
5. Solutions and Intervention Models
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sheffield, P.E.; Landrigan, P.J. Global Climate Change and Children’s Health: Threats and Strategies for Prevention. Environ. Health Perspect. 2010, 119, 291. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.J.; American Academy of Pediatrics Committee on Environmental Health. Ambient Air Pollution: Health Hazards to Children. Pediatrics 2004, 114, 1699–1707. [Google Scholar] [CrossRef] [PubMed]
- Tang, B.; Liu, X.; Liu, Y.; Xue, C.; Zhang, L. A Meta-Analysis of Risk Factors for Depression in Adults and Children after Natural Disasters. BMC Public Health 2014, 14, 623. [Google Scholar] [CrossRef]
- Rubens, S.L.; Felix, E.D.; Hambrick, E.P. A Meta-Analysis of the Impact of Natural Disasters on Internalizing and Externalizing Problems in Youth. J. Trauma. Stress 2018, 31, 332–341. [Google Scholar] [CrossRef]
- McClafferty, H. Environmental Health: Children׳s Health, a Clinician׳s Dilemma. Curr. Probl. Pediatr. Adolesc. Health Care 2016, 46, 184–189. [Google Scholar] [CrossRef]
- Mello da Silva, C.A.; Fruchtengarten, L.V.; Dall’Agnese, R.M. Anamnese Ambiental Em Pediatria; Departamento Científico de Toxicologia e Saúde Ambiental, Sociedade Brasileira de Pediatria: São Paulo, Brazil, 2019; Volume 2, pp. 1–15. [Google Scholar]
- Behinaein, P.; Hutchings, H.; Knapp, T.; Okereke, I.C. The Growing Impact of Air Quality on Lung-Related Illness: A Narrative Review. J. Thorac. Dis. 2023, 15, 5055. [Google Scholar] [CrossRef]
- Zhang, Y.; Steiner, A.L. Projected Climate-Driven Changes in Pollen Emission Season Length and Magnitude over the Continental United States. Nat. Commun. 2022, 13, 1234. [Google Scholar] [CrossRef]
- American Academy of Pediatrics Taking an Environmental History. Available online: https://www.aap.org/en/patient-care/environmental-health/promoting-healthy-environments-for-children/taking-an-environmental-history/?srsltid=AfmBOornwwHeqiDPXduDyJjWNE-86YWWsdeob4ym2zf8B5HlFb_kLTXI (accessed on 28 October 2024).
- Buka, I.; Brennan, L.; Tarrabain, J.; Aghazadeh, S.; Drisse, M.N.B. Need for Global Core Competencies in Child Health and the Environment: A Canadian Perspective. J. Epidemiol. Community Health 2020, 74, 1056–1059. [Google Scholar] [CrossRef]
- World Health Organization Children’s Environmental Health: The Paediatric Environmental History. Available online: https://www.who.int/news-room/questions-and-answers/item/q-a-the-paediatric-environmental-history (accessed on 28 October 2024).
- Kim, E.; Park, H.; Park, E.A.; Hong, Y.-C.; Ha, M.; Kim, H.-C.; Ha, E.-H. Particulate Matter and Early Childhood Body Weight. Environ. Int. 2016, 94, 591–599. [Google Scholar] [CrossRef]
- van den Hooven, E.H.; Pierik, F.H.; de Kluizenaar, Y.; Willemsen, S.P.; Hofman, A.; van Ratingen, S.W.; Zandveld, P.Y.J.; Mackenbach, J.P.; Steegers, E.A.P.; Miedema, H.M.E.; et al. Air Pollution Exposure during Pregnancy, Ultrasound Measures of Fetal Growth, and Adverse Birth Outcomes: A Prospective Cohort Study. Environ. Health Perspect. 2012, 120, 150–156. [Google Scholar] [CrossRef]
- Lee, A.C.; Katz, J.; Blencowe, H.; Cousens, S.; Kozuki, N.; Vogel, J.P.; Adair, L.; Baqui, A.H.; Bhutta, Z.A.; Caulfield, L.E.; et al. National and Regional Estimates of Term and Preterm Babies Born Small for Gestational Age in 138 Low-Income and Middle-Income Countries in 2010. Lancet Glob. Health 2013, 1, e26. [Google Scholar] [CrossRef] [PubMed]
- Lawn, J.E.; Wilczynska-Ketende, K.; Cousens, S.N. Estimating the Causes of 4 Million Neonatal Deaths in the Year 2000. Int. J. Epidemiol. 2006, 35, 706–718. [Google Scholar] [CrossRef] [PubMed]
- Fu, J.; Lin, Q.; Ai, B.; Li, M.; Luo, W.; Huang, S.; Yu, H.; Yang, Y.; Lin, H.; Wei, J.; et al. Associations between Maternal Exposure to Air Pollution during Pregnancy and Trajectories of Infant Growth: A Birth Cohort Study. Ecotoxicol. Environ. Saf. 2024, 269, 115792. [Google Scholar] [CrossRef] [PubMed]
- Veras, M.; Waked, D.; Saldiva, P. Safe in the Womb? Effects of Air Pollution to the Unborn Child and Neonates. J. Pediatr. 2022, 98, 27–31. [Google Scholar] [CrossRef]
- Akdogan, Z.; Guven, B. Microplastics in the Environment: A Critical Review of Current Understanding and Identification of Future Research Needs. Environ. Pollut. Barking Essex 1987 2019, 254, 113011. [Google Scholar] [CrossRef]
- Ragusa, A.; Svelato, A.; Santacroce, C.; Catalano, P.; Notarstefano, V.; Carnevali, O.; Papa, F.; Rongioletti, M.C.A.; Baiocco, F.; Draghi, S.; et al. Plasticenta: First Evidence of Microplastics in Human Placenta. Environ. Int. 2021, 146, 106274. [Google Scholar] [CrossRef]
- Braun, T.; Ehrlich, L.; Henrich, W.; Koeppel, S.; Lomako, I.; Schwabl, P.; Liebmann, B. Detection of Microplastic in Human Placenta and Meconium in a Clinical Setting. Pharmaceutics 2021, 13, 921. [Google Scholar] [CrossRef]
- Hunt, K.; Davies, A.; Fraser, A.; Burden, C.; Howell, A.; Buckley, K.; Harding, S.; Bakhbakhi, D. Exposure to Microplastics and Human Reproductive Outcomes: A Systematic Review. BJOG Int. J. Obstet. Gynaecol. 2024, 131, 675–683. [Google Scholar] [CrossRef]
- Jeong, B.; Baek, J.Y.; Koo, J.; Park, S.; Ryu, Y.-K.; Kim, K.-S.; Zhang, S.; Chung, C.; Dogan, R.; Choi, H.-S.; et al. Maternal Exposure to Polystyrene Nanoplastics Causes Brain Abnormalities in Progeny. J. Hazard. Mater. 2022, 426, 127815. [Google Scholar] [CrossRef]
- Marcelino, R.C.; Cardoso, R.M.; Domingues, E.L.B.C.; Gonçalves, R.V.; Lima, G.D.A.; Novaes, R.D. The Emerging Risk of Microplastics and Nanoplastics on the Microstructure and Function of Reproductive Organs in Mammals: A Systematic Review of Preclinical Evidence. Life Sci. 2022, 295, 120404. [Google Scholar] [CrossRef]
- Wager, J.L.; Thompson, J.A. Development and Child Health in a World of Synthetic Chemicals. Pediatr. Res. 2024. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Samuels, L.; Nakstad, B.; Roos, N.; Bonell, A.; Chersich, M.; Havenith, G.; Luchters, S.; Day, L.-T.; Hirst, J.E.; Singh, T.; et al. Physiological Mechanisms of the Impact of Heat during Pregnancy and the Clinical Implications: Review of the Evidence from an Expert Group Meeting. Int. J. Biometeorol. 2022, 66, 1505. [Google Scholar] [CrossRef] [PubMed]
- Maccari, S.; Darnaudery, M.; Morley-Fletcher, S.; Zuena, A.R.; Cinque, C.; Van Reeth, O. Prenatal Stress and Long-Term Consequences: Implications of Glucocorticoid Hormones. Neurosci. Biobehav. Rev. 2003, 27, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Wadhwa, P.D.; Sandman, C.A.; Garite, T.J. The Neurobiology of Stress in Human Pregnancy: Implications for Prematurity and Development of the Fetal Central Nervous System. Prog. Brain Res. 2001, 133, 131–142. [Google Scholar] [CrossRef]
- Weinstock, M. Alterations Induced by Gestational Stress in Brain Morphology and Behaviour of the Offspring. Prog. Neurobiol. 2001, 65, 427–451. [Google Scholar] [CrossRef]
- Rubin, L.P. Maternal and Pediatric Health and Disease: Integrating Biopsychosocial Models and Epigenetics. Pediatr. Res. 2016, 79, 127–135. [Google Scholar] [CrossRef]
- Wadhwa, P.D.; Buss, C.; Entringer, S.; Swanson, J.M. Developmental Origins of Health and Disease: Brief History of the Approach and Current Focus on Epigenetic Mechanisms. Semin. Reprod. Med. 2009, 27, 358–368. [Google Scholar] [CrossRef]
- Indrio, F.; Pietrobelli, A.; Dargenio, V.N.; Marchese, F.; Grillo, A.; Vural, M.; Giardino, I.; Pettoello-Mantovani, M. The Key 1000 Life-Changing Days. Glob. Pediatr. 2023, 4, 100049. [Google Scholar] [CrossRef]
- Instituto Nacional de Pesquisas Espaciais, Ministério de Ciência, Tecnologia e Inovações Situação Atual—Programa Queimadas—INPE. Available online: https://terrabrasilis.dpi.inpe.br/queimadas/situacao-atual/situacao_atual/ (accessed on 29 October 2024).
- Bignier, C.; Havet, L.; Brisoux, M.; Omeiche, C.; Misra, S.; Gonsard, A.; Drummond, D. Climate Change and Children’s Respiratory Health. Paediatr. Respir. Rev. 2024, 53, 64–73. [Google Scholar] [CrossRef]
- Melén, E.; Faner, R.; Allinson, J.P.; Bui, D.; Bush, A.; Custovic, A.; Garcia-Aymerich, J.; Guerra, S.; Breyer-Kohansal, R.; Hallberg, J.; et al. Lung-Function Trajectories: Relevance and Implementation in Clinical Practice. Lancet 2024, 403, 1494–1503. [Google Scholar] [CrossRef]
- Silverman, R.A.; Ito, K. Age-Related Association of Fine Particles and Ozone with Severe Acute Asthma in New York City. J. Allergy Clin. Immunol. 2010, 125, 367–373.e5. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Ding, H.; Jiang, L.; Chen, S.; Zheng, J.; Qiu, M.; Zhou, Y.; Chen, Q.; Guan, W. Association between Air Pollutants and Asthma Emergency Room Visits and Hospital Admissions in Time Series Studies: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0138146. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Li, S.; Fan, C.; Bai, Z.; Yang, K. The Impact of PM2.5 on Asthma Emergency Department Visits: A Systematic Review and Meta-Analysis. Environ. Sci. Pollut. Res. Int. 2016, 23, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Mirabelli, M.C.; Vaidyanathan, A.; Flanders, W.D.; Qin, X.; Garbe, P. Outdoor PM2.5, Ambient Air Temperature, and Asthma Symptoms in the Past 14 Days among Adults with Active Asthma. Environ. Health Perspect. 2016, 124, 1882–1890. [Google Scholar] [CrossRef] [PubMed]
- Han, A.; Deng, S.; Yu, J.; Zhang, Y.; Jalaludin, B.; Huang, C. Asthma Triggered by Extreme Temperatures: From Epidemiological Evidence to Biological Plausibility. Environ. Res. 2023, 216, 114489. [Google Scholar] [CrossRef]
- Deng, S.; Han, A.; Jin, S.; Wang, S.; Zheng, J.; Jalaludin, B.B.; Hajat, S.; Liang, W.; Huang, C. Effect of Extreme Temperatures on Asthma Hospital Visits: Modification by Event Characteristics and Healthy Behaviors. Environ. Res. 2023, 226, 115679. [Google Scholar] [CrossRef]
- Xu, Z.; Huang, C.; Hu, W.; Turner, L.R.; Su, H.; Tong, S. Extreme Temperatures and Emergency Department Admissions for Childhood Asthma in Brisbane, Australia. Occup. Environ. Med. 2013, 70, 730–735. [Google Scholar] [CrossRef]
- Guilbert, A.; Hough, I.; Seyve, E.; Rolland, M.; Quentin, J.; Slama, R.; Lyon-Caen, S.; Kloog, I.; Bayat, S.; Siroux, V.; et al. Association of Prenatal and Postnatal Exposures to Warm or Cold Air Temperatures with Lung Function in Young Infants. JAMA Netw. Open 2023, 6, e233376. [Google Scholar] [CrossRef]
- World Health Organization Global Health Estimates. Available online: https://www.who.int/data/global-health-estimates (accessed on 30 October 2024).
- Institute for Health Metrics and Evaluation GBD Results. Available online: https://vizhub.healthdata.org/gbd-results (accessed on 30 October 2024).
- Hickman, C.; Marks, E.; Pihkala, P.; Clayton, S.; Lewandowski, R.E.; Mayall, E.E.; Wray, B.; Mellor, C.; Susteren, L. van Climate Anxiety in Children and Young People and Their Beliefs about Government Responses to Climate Change: A Global Survey. Lancet Planet. Health 2021, 5, e863–e873. [Google Scholar] [CrossRef]
- Stanley, S.K.; Hogg, T.L.; Leviston, Z.; Walker, I. From Anger to Action: Differential Impacts of Eco-Anxiety, Eco-Depression, and Eco-Anger on Climate Action and Wellbeing. J. Clim. Change Health 2021, 1, 100003. [Google Scholar] [CrossRef]
- Kirkbride, J.B.; Anglin, D.M.; Colman, I.; Dykxhoorn, J.; Jones, P.B.; Patalay, P.; Pitman, A.; Soneson, E.; Steare, T.; Wright, T.; et al. The Social Determinants of Mental Health and Disorder: Evidence, Prevention and Recommendations. World Psychiatry 2024, 23, 58. [Google Scholar] [CrossRef] [PubMed]
- Oliveros, B.; Agulló-Tomás, E.; Márquez-Álvarez, L.-J. Risk and Protective Factors of Mental Health Conditions: Impact of Employment, Deprivation and Social Relationships. Int. J. Environ. Res. Public. Health 2022, 19, 6781. [Google Scholar] [CrossRef] [PubMed]
- Carnie, T.-L.; Berry, H.L.; Blinkhorn, S.A.; Hart, C.R. In Their Own Words: Young People’s Mental Health in Drought-Affected Rural and Remote NSW. Aust. J. Rural Health 2011, 19, 244–248. [Google Scholar] [CrossRef] [PubMed]
- Neas, S.; Ward, A.; Bowman, B. Young People’s Climate Activism: A Review of the Literature. Front. Polit. Sci. 2022, 4, 940876. [Google Scholar] [CrossRef]
- Li, C.F.; Lim, T.W.; Han, L.L.; Fang, R. Rainfall, Abundance of Aedes Aegypti and Dengue Infection in Selangor, Malaysia. Southeast Asian J. Trop. Med. Public Health 1985, 16, 560–568. [Google Scholar]
- Johansson, M.A.; Cummings, D.A.T.; Glass, G.E. Multiyear Climate Variability and Dengue—El Niño Southern Oscillation, Weather, and Dengue Incidence in Puerto Rico, Mexico, and Thailand: A Longitudinal Data Analysis. PLoS Med. 2009, 6, e1000168. [Google Scholar] [CrossRef]
- Ferreira, H.d.S.; Nóbrega, R.S.; Brito, P.V.d.S.; Farias, J.P.; Amorim, J.H.; Moreira, E.B.M.; Mendez, É.C.; Luiz, W.B. Impacts of El Niño Southern Oscillation on the Dengue Transmission Dynamics in the Metropolitan Region of Recife, Brazil. Rev. Soc. Bras. Med. Trop. 2022, 55, e0671. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control Dengue Worldwide Overview. Available online: https://www.ecdc.europa.eu/en/dengue-monthly (accessed on 30 October 2024).
- Pereira, E.D.A.; Carmo, C.N.d.; Araujo, W.R.M.; Branco, M.D.R.F.C. Spatial Distribution of Arboviruses and Its Association with a Social Development Index and the Waste Disposal in São Luís, State of Maranhão, Brazil, 2015 to 2019. Rev. Bras. Epidemiol. Braz. J. Epidemiol. 2024, 27, e240017. [Google Scholar] [CrossRef]
- Martins, M.M.; Prata-Barbosa, A.; Cunha, A.J.L.A. da Arboviral Diseases in Pediatrics. J. Pediatr. 2020, 96, 2–11. [Google Scholar] [CrossRef]
- Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento de Vigilância das Doenças Transmissíveis Dengue. Diagnóstico e Manejo Clínico: Adulto e Criança, 6th ed.; Ministério Da Saúde: Brasília, Brazil, 2024. Available online: https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/svsa/dengue/dengue-diagnostico-e-manejo-clinico-adulto-e-crianca/view (accessed on 31 October 2024).
- Adachi, K.; Nielsen-Saines, K. Zika Clinical Updates: Implications for Pediatrics. Curr. Opin. Pediatr. 2018, 30, 105. [Google Scholar] [CrossRef]
- Economopoulou, A.; Dominguez, M.; Helynck, B.; Sissoko, D.; Wichmann, O.; Quenel, P.; Germonneau, P.; Quatresous, I. Atypical Chikungunya Virus Infections: Clinical Manifestations, Mortality and Risk Factors for Severe Disease during the 2005–2006 Outbreak on Réunion. Epidemiol. Infect. 2009, 137, 534–541. [Google Scholar] [CrossRef]
- Burt, F.J.; Rolph, M.S.; Rulli, N.E.; Mahalingam, S.; Heise, M.T. Chikungunya: A Re-Emerging Virus. Lancet 2012, 379, 662–671. [Google Scholar] [CrossRef] [PubMed]
- Cambaúva, D. Entenda Como Funciona a Vacina Contra Dengue Ofertada Pelo SUS. Available online: https://agenciagov.ebc.com.br/noticias/202401/entenda-como-funciona-a-vacina-contra-dengue-ofertada-pelo-sus (accessed on 31 October 2024).
- Chen, Y.; Xu, Y.; Wang, L.; Liang, Y.; Li, N.; Lourenço, J.; Yang, Y.; Lin, Q.; Wang, L.; Zhao, H.; et al. Indian Ocean Temperature Anomalies Predict Long-Term Global Dengue Trends. Science 2024, 384, 639–646. [Google Scholar] [CrossRef] [PubMed]
- Pingault, N. (Ed.) C.P. Nutrition and Food Systems. A Report by the High Level Panel of Experts on Food Security and Nutrition of the Committee on World Food Security. Available online: https://publications.cirad.fr/une_notice.php?dk=604475 (accessed on 10 December 2024).
- Lei No 11.346. Available online: https://www.planalto.gov.br/ccivil_03/_ato2004-2006/2006/lei/l11346.htm (accessed on 10 December 2024).
- BRASIL. Mudança do Clima no Brasil: Síntese Atualizada e Perspectivas Para Decisões Estratégicas; Ministério da Ciência, Tecnologia e Inovação: Brasília, Brazil, 2024. Available online: https://www.gov.br/mcti/pt-br/acompanhe-o-mcti/cgcl/paginas/mudanca-do-clima-no-brasil-sintese-atualizada-e-perspectivas-para-decisoes-estrategicas (accessed on 10 December 2024).
- IPCC. Climate Change 2023: Synthesis Report; Contribution of Working Groups I, II and III to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change; Core Writing Team, Lee, H., Romero, J., Eds.; IPCC: Geneva, Switzerland, 2023; 184p. [Google Scholar]
- Oliveira, W.; Silva, J.L.S.; Porto, R.G.; Cruz-Neto, O.; Tabarelli, M.; Viana, B.F.; Peres, C.A.; Lopes, A.V. 62 signatories Plant and Pollination Blindness: Risky Business for Human Food Security. BioScience 2020, 70, 109–110. [Google Scholar] [CrossRef]
- Oliveira, W.; Cruz-Neto, O.; Tabarelli, M.; Galetto, L.; Peres, C.A.; Lopes, A.V. Markedly Declining Reproductive Functional Diversity of Food Plants in the World’s Largest Tropical Country despite Rapid Cropland Expansion. Agric. Ecosyst. Environ. 2023, 357, 108673. [Google Scholar] [CrossRef]
- Mirzabaev, A.; Bezner Kerr, R.; Hasegawa, T.; Pradhan, P.; Wreford, A.; Cristina Tirado von der Pahlen, M.; Gurney-Smith, H. Severe Climate Change Risks to Food Security and Nutrition. Clim. Risk Manag. 2023, 39, 100473. [Google Scholar] [CrossRef]
- Castellanos, E.; Lemos, M.F.; Astigarraga, L.; Chacón, N.; Cuvi, N.; Huggel, C.; Miranda, L.; Moncassim Vale, M.; Ometto, J.P.; Peri, P.L.; et al. Central and South America. In Climate Change 2022: Impacts, Adaptation and Vulnerability; Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change; Pörtner, H.-O., Roberts, D.C., Tignor, M., Poloczanska, E.S., Mintenbeck, K., Alegría, A., Craig, M., Langsdorf, S., Löschke, S., Möller, V., et al., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2022; pp. 1689–1816. [Google Scholar] [CrossRef]
- Birkmann, J.; Liwenga, E.; Pandey, R.; Boyd, E.; Djalante, R.; Gemenne, F.; Leal Filho, W.; Pinho, P.F.; Stringer, L.; Wrathall, D. Poverty, Livelihoods and Sustainable Development. In Climate Change 2022: Impacts, Adaptation and Vulnerability; Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change; Pörtner, H.-O., Roberts, D.C., Tignor, M., Poloczanska, E.S., Mintenbeck, K., Alegría, A., Craig, M., Langsdorf, S., Löschke, S., Möller, V., et al., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2022; pp. 1171–1274. [Google Scholar] [CrossRef]
- Kotz, M.; Kuik, F.; Lis, E.; Nickel, C. Global Warming and Heat Extremes to Enhance Inflationary Pressures. Commun. Earth Environ. 2024, 5, 116. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Moubarac, J.-C.; Cannon, G.; Ng, S.W.; Popkin, B. Ultra-Processed Products Are Becoming Dominant in the Global Food System. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2013, 14 (Suppl. S2), 21–28. [Google Scholar] [CrossRef]
- Passos, C.M.D.; Maia, E.G.; Levy, R.B.; Martins, A.P.B.; Claro, R.M. Association between the Price of Ultra-Processed Foods and Obesity in Brazil. Nutr. Metab. Cardiovasc. Dis. NMCD 2020, 30, 589–598. [Google Scholar] [CrossRef]
- Costa, C.D.S.; Buffarini, R.; Flores, T.R.; Neri, D.; Freitas Silveira, M.; Monteiro, C.A. Consumption of Ultra-Processed Foods and Growth Outcomes in Early Childhood: 2015 Pelotas Birth Cohort. Br. J. Nutr. 2023, 129, 2153–2160. [Google Scholar] [CrossRef]
- Leite, F.H.M.; Khandpur, N.; Andrade, G.C.; Anastasiou, K.; Baker, P.; Lawrence, M.; Monteiro, C.A. Ultra-Processed Foods Should Be Central to Global Food Systems Dialogue and Action on Biodiversity. BMJ Glob. Health 2022, 7, e008269. [Google Scholar] [CrossRef] [PubMed]
- Seferidi, P.; Scrinis, G.; Huybrechts, I.; Woods, J.; Vineis, P.; Millett, C. The Neglected Environmental Impacts of Ultra-Processed Foods. Lancet Planet. Health 2020, 4, e437–e438. [Google Scholar] [CrossRef] [PubMed]
- Rede PENSSAN. II Inquérito Nacional Sobre Insegurança Alimentar No Contexto Da Pandemia Da COVID-19 No Brasil; Fundação Friedrich Ebert: São Paulo, SP, Brazil, 2022; ISBN 978-65-87504-50-6. [Google Scholar]
- Whitaker, R.C.; Phillips, S.M.; Orzol, S.M. Food Insecurity and the Risks of Depression and Anxiety in Mothers and Behavior Problems in Their Preschool-Aged Children. Pediatrics 2006, 118, e859–e868. [Google Scholar] [CrossRef] [PubMed]
- Slopen, N.; Fitzmaurice, G.; Williams, D.R.; Gilman, S.E. Poverty, Food Insecurity, and the Behavior for Childhood Internalizing and Externalizing Disorders. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 444–452. [Google Scholar] [CrossRef]
- Melchior, M.; Chastang, J.-F.; Falissard, B.; Galéra, C.; Tremblay, R.E.; Côté, S.M.; Boivin, M. Food Insecurity and Children’s Mental Health: A Prospective Birth Cohort Study. PLoS ONE 2012, 7, e52615. [Google Scholar] [CrossRef]
- Weinreb, L.; Wehler, C.; Perloff, J.; Scott, R.; Hosmer, D.; Sagor, L.; Gundersen, C. Hunger: Its Impact on Children’s Health and Mental Health. Pediatrics 2002, 110, e41. [Google Scholar] [CrossRef]
- Murphy, J.M.; Wehler, C.A.; Pagano, M.E.; Little, M.; Kleinman, R.E.; Jellinek, M.S. Relationship between Hunger and Psychosocial Functioning in Low-Income American Children. J. Am. Acad. Child Adolesc. Psychiatry 1998, 37, 163–170. [Google Scholar] [CrossRef]
- Rose-Jacobs, R.; Black, M.M.; Casey, P.H.; Cook, J.T.; Cutts, D.B.; Chilton, M.; Heeren, T.; Levenson, S.M.; Meyers, A.F.; Frank, D.A. Household Food Insecurity: Associations with at-Risk Infant and Toddler Development. Pediatrics 2008, 121, 65–72. [Google Scholar] [CrossRef]
- McIntyre, L.; Williams, J.V.A.; Lavorato, D.H.; Patten, S. Depression and Suicide Ideation in Late Adolescence and Early Adulthood Are an Outcome of Child Hunger. J. Affect. Disord. 2013, 150, 123–129. [Google Scholar] [CrossRef]
- Alaimo, K.; Olson, C.M.; Frongillo, E.A. Family Food Insufficiency, but Not Low Family Income, Is Positively Associated with Dysthymia and Suicide Symptoms in Adolescents. J. Nutr. 2002, 132, 719–725. [Google Scholar] [CrossRef]
- Leung, C.W.; Stewart, A.L.; Portela-Parra, E.T.; Adler, N.E.; Laraia, B.A.; Epel, E.S. Understanding the Psychological Distress of Food Insecurity: A Qualitative Study of Children’s Experiences and Related Coping Strategies. J. Acad. Nutr. Diet. 2020, 120, 395. [Google Scholar] [CrossRef] [PubMed]
- BRASIL. Guia Alimentar Para Crianças Brasileiras Menores de 2 Anos—Versão Resumida/Ministério Da Saúde, Secretaria de Atenção Primária à Saúde; Ministério Da Saúde: Brasília, Brazil, 2019.
- Summary for Policymakers. In Climate Change 2021—The Physical Science Basis: Working Group I Contribution to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change; Intergovernmental Panel on Climate Change (IPCC), Ed.; Cambridge University Press: Cambridge, UK, 2023; pp. 1–2. ISBN 978-1-00-915788-9. [Google Scholar]
- Dutra, D.J.; Silveira, M.V.F.; Mataveli, G.; Ferro, P.D.; Magalhães, D.d.S.; de Medeiros, T.P.; Anderson, L.O.; de Aragão, L.E.O.e.C. Challenges for Reducing Carbon Emissions from Land-Use and Land Cover Change in Brazil. Perspect. Ecol. Conserv. 2024, 22, 213–218. [Google Scholar] [CrossRef]
- Soterroni, A.C.; Império, M.; Scarabello, M.C.; Seddon, N.; Obersteiner, M.; Rochedo, P.R.R.; Schaeffer, R.; Andrade, P.R.; Ramos, F.M.; Azevedo, T.R.; et al. Nature-Based Solutions Are Critical for Putting Brazil on Track towards Net-Zero Emissions by 2050. Glob. Change Biol. 2023, 29, 7085–7101. [Google Scholar] [CrossRef] [PubMed]
- Ferrante, L.; Fearnside, P.M. Brazil’s New President and ‘Ruralists’ Threaten Amazonia’s Environment, Traditional Peoples and the Global Climate. Environ. Conserv. 2019, 46, 261–263. [Google Scholar] [CrossRef]
- Ruiz-Mallén, I.; Satorras, M.; March, H.; Baró, F. Community Climate Resilience and Environmental Education: Opportunities and Challenges for Transformative Learning. Environ. Educ. Res. 2022, 28, 1088–1107. [Google Scholar] [CrossRef]
- Thiel, C.L.; Mehta, N.; Sejo, C.S.; Qureshi, L.; Moyer, M.; Valentino, V.; Saleh, J. Telemedicine and the Environment: Life Cycle Environmental Emissions from in-Person and Virtual Clinic Visits. NPJ Digit. Med. 2023, 6, 87. [Google Scholar] [CrossRef]
- Feliciano, D. Factors Influencing the Adoption of Sustainable Agricultural Practices: The Case of Seven Horticultural Farms in the United Kingdom. Scott. Geogr. J. 2022, 138, 291–320. [Google Scholar] [CrossRef]
- Azeem, M.I.; Alotaibi, B.A. Farmers’ Beliefs and Concerns about Climate Change, and Their Adaptation Behavior to Combat Climate Change in Saudi Arabia. PLoS ONE 2023, 18, e0280838. [Google Scholar] [CrossRef]
- Silva, J.M.C.; Araujo, L.S.; Torres, R.R.; Barbosa, L.C.F. The Sustainability of Development Pathways and Climate Change Vulnerability in the Americas. Ecol. Econ. 2024, 220, 108164. [Google Scholar] [CrossRef]
- Food and Agriculture Organization of the United Nations The State of Food and Agriculture. 2013. Available online: https://www.fao.org/4/i3300e/i3300e00.htm (accessed on 17 April 2025).
- Okunogbe, A.; Nugent, R.; Spencer, G.; Powis, J.; Ralston, J.; Wilding, J. Economic Impacts of Overweight and Obesity: Current and Future Estimates for 161 Countries. BMJ Glob. Health 2022, 7, e009773. [Google Scholar] [CrossRef]
- Arpin, E.; de Oliveira, C.; Siddiqi, A.; Laporte, A. The “Long-Arm” of Chronic Conditions in Childhood: Evidence from Canada Using Linked Survey-Administrative Data. Econ. Hum. Biol. 2023, 50, 101257. [Google Scholar] [CrossRef]
- United Nations Children’s Fund. The Climate Crisis Is a Child Rights Crisis. Available online: https://www.unicef.org/reports/climate-crisis-child-rights-crisis (accessed on 30 October 2024).
| Actor | Proposed Action | Pathways to Improve Child Health | Priority |
|---|---|---|---|
| Government | Enforce deforestation control and promote large-scale native vegetation restoration. | Reduce emissions; protect ecosystems essential for nutrition and air quality. | ★★★ |
| Government | Redirect policies and subsidies away from extractive economic models toward sustainable, equity-based development. | Address structural drivers of the climate crisis; promote equitable health and development. | ★★★ |
| Government | Tax ultra-processed foods and subsidize healthy, minimally processed options. | Improve nutrition and reduce the risk of diet-related diseases. | ★★★ |
| Government/Education system/Health professionals | Provide climate adaptation education. | Increase knowledge; support adaptive behaviors to reduce climate-related health risks. | ★★ |
| Government/Health sector | Expand access to climate-sensitive prenatal and pediatric care. | Address early vulnerabilities and reduce inequalities. | ★★ |
| Government | Strengthen community-based mental health support networks and emergency preparedness programs for children. | Reduce trauma-related effects from climate disasters; support emotional resilience. | ★★ |
| Public health authorities | Implement integrated strategies to prevent arboviral diseases, including community education, vector control initiatives, increased access to dengue vaccination, and the use of climate-based forecasting tools to guide interventions. | Reduces incidence and severity of dengue and other mosquito-borne diseases | ★★★ |
| Health sector | Train pediatricians to recognize and respond to climate-related health symptoms. | Ensure earlier detection and preventive care. | ★★★ |
| Family/caregiver | Promote dietary shifts toward fresh/minimally processed foods and reduce ultra-processed intake. | Support healthy growth and prevent malnutrition. | ★★ |
| Family/caregiver | Implement protective behaviors: hydration, reduced smoke exposure, indoor cooling. | Reduce the risk of heat illness and air pollution-related symptoms. | ★★ |
| Academia | Advance research on how climate policies influence child health outcomes and identify child-specific vulnerabilities | Inform more effective, evidence-based climate policies. | ★★ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cabral-Miranda, W.; Solé, D.; Wandalsen, G.F.; Urrutia-Pereira, M.; Corrêa, M.d.P.; Silveira, C.M.; Constantino, C.F.; de Albuquerque, M.P.; Waksman, R.D.; de Araujo, E.d.M.P.A.; et al. Under Fire: A Brazilian Perspective on Climate Change and Child Health. Sustainability 2025, 17, 4482. https://doi.org/10.3390/su17104482
Cabral-Miranda W, Solé D, Wandalsen GF, Urrutia-Pereira M, Corrêa MdP, Silveira CM, Constantino CF, de Albuquerque MP, Waksman RD, de Araujo EdMPA, et al. Under Fire: A Brazilian Perspective on Climate Change and Child Health. Sustainability. 2025; 17(10):4482. https://doi.org/10.3390/su17104482
Chicago/Turabian StyleCabral-Miranda, William, Dirceu Solé, Gustavo Falbo Wandalsen, Marilyn Urrutia-Pereira, Marcelo de Paula Corrêa, Camila Magalhães Silveira, Clovis Francisco Constantino, Maria Paula de Albuquerque, Renata Dejtiar Waksman, Evangelina da Motta Pacheco Alves de Araujo, and et al. 2025. "Under Fire: A Brazilian Perspective on Climate Change and Child Health" Sustainability 17, no. 10: 4482. https://doi.org/10.3390/su17104482
APA StyleCabral-Miranda, W., Solé, D., Wandalsen, G. F., Urrutia-Pereira, M., Corrêa, M. d. P., Silveira, C. M., Constantino, C. F., de Albuquerque, M. P., Waksman, R. D., de Araujo, E. d. M. P. A., Parschalk, G., Filho, L. V. R. F. d. S., Lapchik, M., Mallet, A., Sato, H. K., Fernandes, F. R., Setúbal, J. L. E., & Nobre, C. A. (2025). Under Fire: A Brazilian Perspective on Climate Change and Child Health. Sustainability, 17(10), 4482. https://doi.org/10.3390/su17104482






