Does Digitization Lead to Sustainable Economic Behavior? Investigating the Roles of Employee Well-Being and Learning Orientation
Abstract
1. Introduction
- In what ways does digitalization influence both employee well-being and sustainable economic behavior?
- Does employee well-being mediate the relationship between digitalization and sustainable economic behavior?
- To what extent does learning orientation moderate the effects of digitalization on employee well-being and sustainable economic behavior?
- Does learning orientation enhance the mediating influence of employee well-being in the relationship between digitalization and sustainable economic behavior?
2. Theoretical Framework and Hypotheses Development
2.1. JD–R Model
2.2. Digitalization
2.3. Sustainable Economic Behavior
2.4. Digitalization and Sustainable Economic Behavior
2.5. Digitalization and Employee Mental Health
2.6. Employee Mental Health and Sustainable Economic Behavior
2.7. The Mediating Role of Employee Mental Health
2.8. The Moderating Role of Learning Orientation
3. Methodology
3.1. Sample and Data Collection
3.2. Measures
3.3. Analytical Methods
3.4. Common Method Bias
4. Analysis and Results
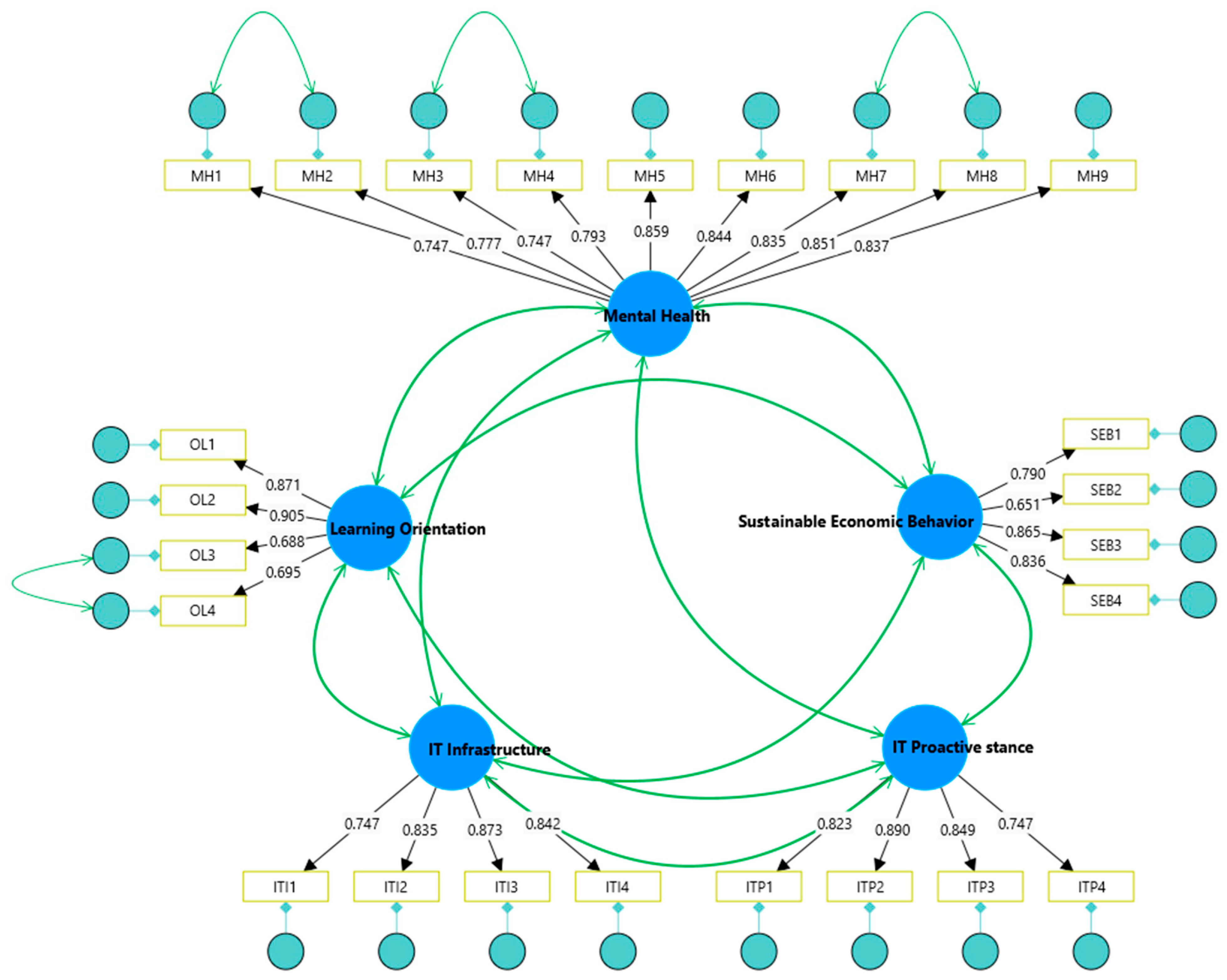
4.1. Construct Reliability and Validity
4.2. Hypotheses Testing
4.2.1. Direct Effect
4.2.2. Indirect Effect
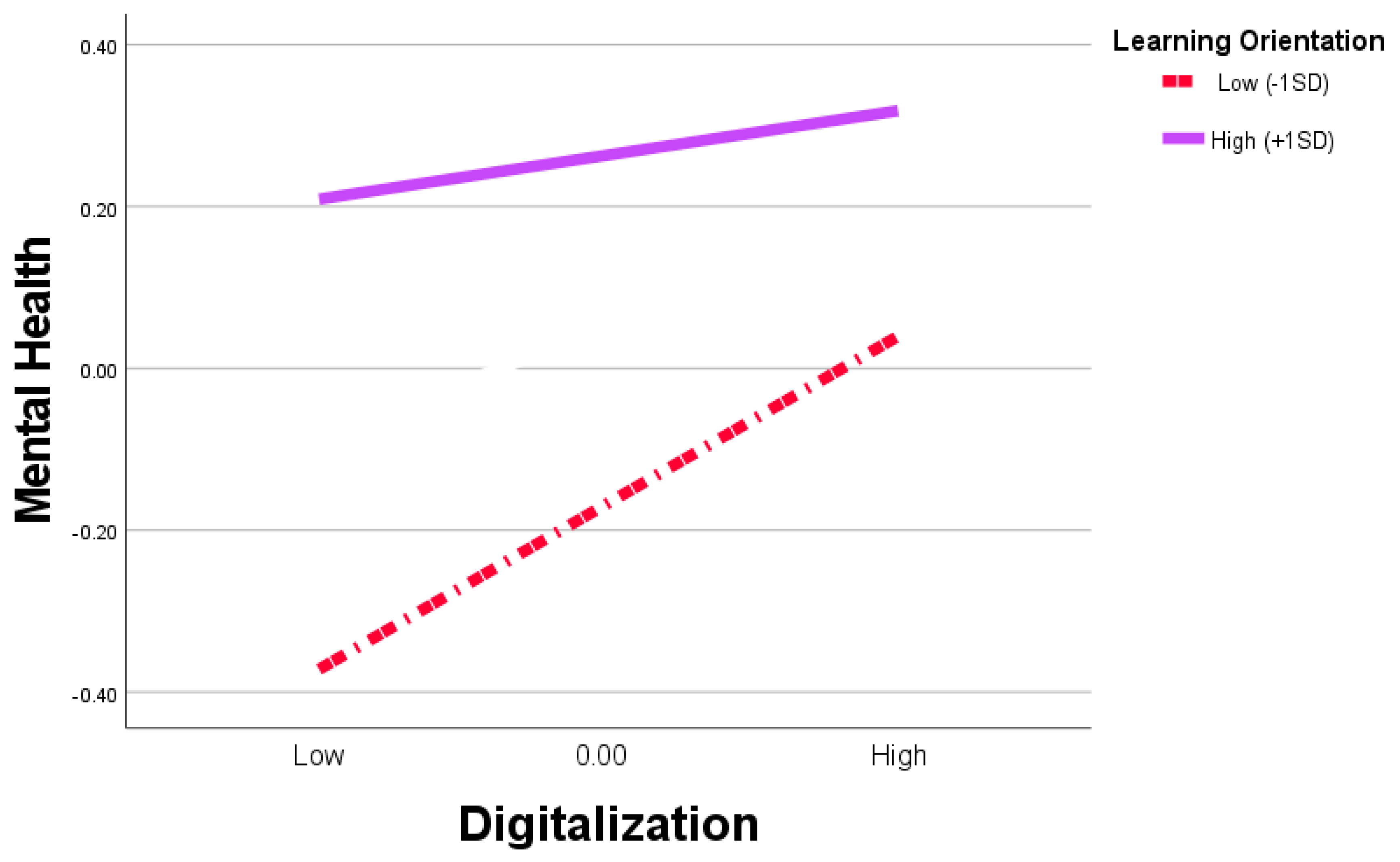
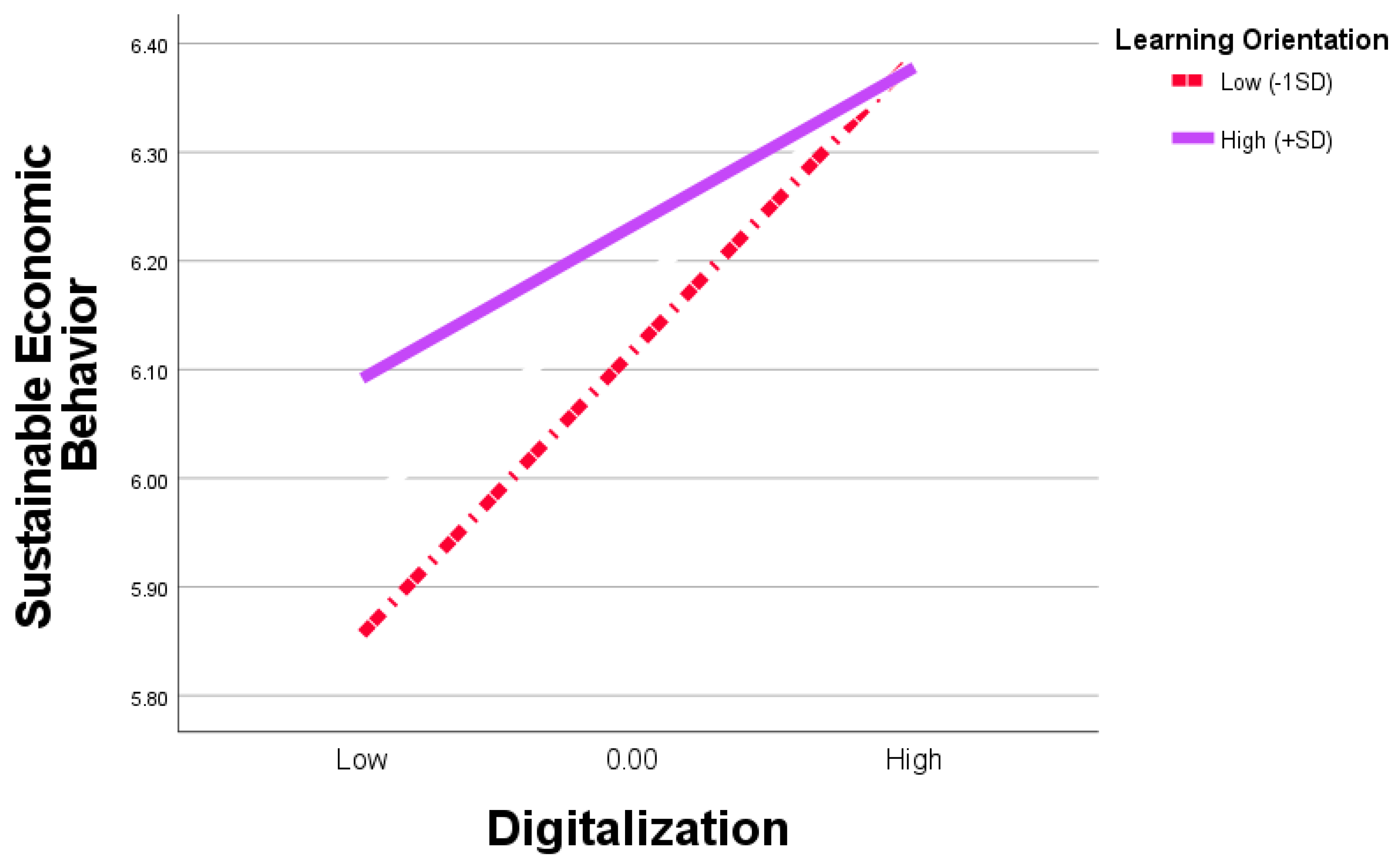
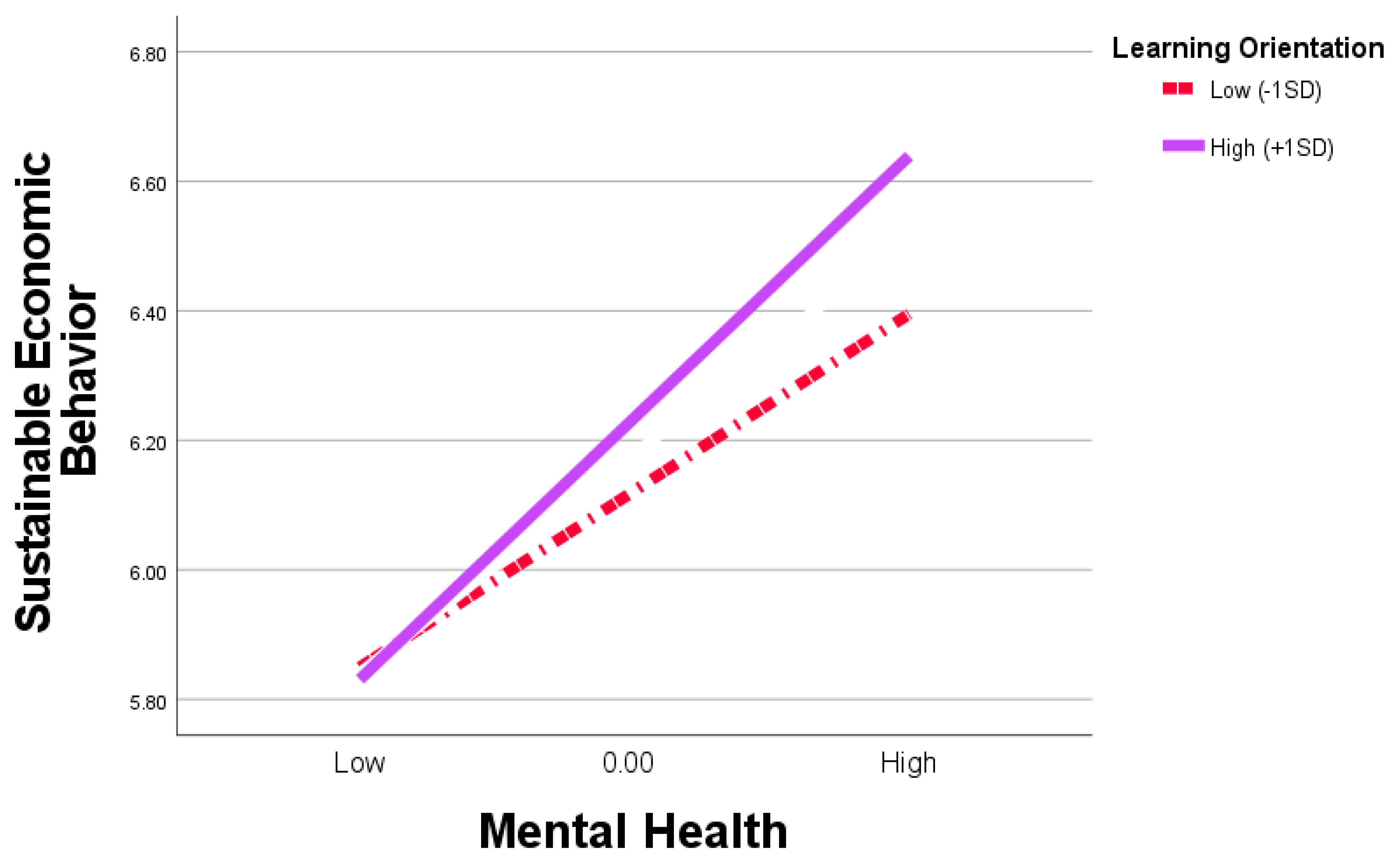
4.2.3. Moderation and Moderated Mediation Analyses
5. Discussion
6. Conclusions
6.1. Theoretical Contribution
6.2. Practical and Managerial Implications
6.3. Limitations and Future Studies
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kraus, S.; Schiavone, F.; Pluzhnikova, A.; Invernizzi, A.C. Digital Transformation in Healthcare: Analyzing the Current State-of-Research. J. Bus. Res. 2021, 123, 557–567. [Google Scholar] [CrossRef]
- Massaro, M. Digital Transformation in the Healthcare Sector through Blockchain Technology. Insights from Academic Research and Business Developments. Technovation 2023, 120, 102386. [Google Scholar] [CrossRef]
- Marques, I.C.P.; Ferreira, J.J.M. Digital Transformation in the Area of Health: Systematic Review of 45 Years of Evolution. Health Technol. 2020, 10, 575–586. [Google Scholar] [CrossRef]
- Mauro, M.; Noto, G.; Prenestini, A.; Sarto, F. Digital Transformation in Healthcare: Assessing the Role of Digital Technologies for Managerial Support Processes. Technol. Forecast. Soc. Change 2024, 209, 123781. [Google Scholar] [CrossRef]
- Henke, R.M. Knowing Well, Being Well: Well-Being Born of Understanding: Supporting Workforce Mental Health During the Pandemic. Am. J. Health Promot. 2022, 36, 1213–1244. [Google Scholar] [CrossRef]
- Karamat, J.; Shurong, T.; Ahmad, N.; Afridi, S.; Khan, S.; Mahmood, K. Promoting Healthcare Sustainability in Developing Countries: Analysis of Knowledge Management Drivers in Public and Private Hospitals of Pakistan. Int. J. Environ. Res. Public Health 2019, 16, 508. [Google Scholar] [CrossRef]
- Kong, L.; Sial, M.S.; Ahmad, N.; Sehleanu, M.; Li, Z.; Zia-Ud-Din, M.; Badulescu, D. CSR as a Potential Motivator to Shape Employees’ View towards Nature for a Sustainable Workplace Environment. Sustainability 2021, 13, 1499. [Google Scholar] [CrossRef]
- Alkadash, T.M.; Nagi, M.; Ateeq, A.A.; Alzoraiki, M.; Alkadash, R.M.; Nadam, C.; Allaymoun, M.; Dawwas, M. The Effects of Leadership Style on Employee Sustainable Behaviour: A Theoretical Perspective. In Artificial Intelligence and Transforming Digital Marketing; Hamdan, A., Aldhaen, E.S., Eds.; Springer Nature: Cham, Switzerland, 2024; pp. 205–213. ISBN 978-3-031-35828-9. [Google Scholar]
- Qiu, Y.; Zhang, Y.; Liu, M. Dual Process Model of Farmers’ Mindfulness and Sustainable Economic Behavior: Mediating Role of Mental Health and Emotional Labor. Front. Psychiatry 2022, 13, 79. [Google Scholar] [CrossRef] [PubMed]
- Sepetis, A.; Parlavatzas, I.; Zaza, P.N.; Platis, C.; Fotios, R.; Nikolaou, I.E. The Role of Organizational Behavior to Sustainable Health Care: The Case of Greece. Environ. Health Insights 2024, 18, 11786302241298788. [Google Scholar] [CrossRef]
- Faulks, B.; Song, Y.; Waiganjo, M.; Obrenovic, B.; Godinic, D. Impact of Empowering Leadership, Innovative Work, and Organizational Learning Readiness on Sustainable Economic Performance: An Empirical Study of Companies in Russia during the COVID-19 Pandemic. Sustainability 2021, 13, 12465. [Google Scholar] [CrossRef]
- Al’Ararah, K.; Çağlar, D.; Aljuhmani, H.Y. Mitigating Job Burnout in Jordanian Public Healthcare: The Interplay between Ethical Leadership, Organizational Climate, and Role Overload. Behav. Sci. 2024, 14, 490. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Promoting Mental Health: Concepts, Emerging Evidence, Practice: Summary Report; Herrman, H., Saxena, S., Moodie, R., Eds.; WHO: Geneva, Switzerland, 2005; ISBN 978-92-4-156294-2. [Google Scholar]
- Stuber, F.; Seifried-Dübon, T.; Rieger, M.A.; Gündel, H.; Ruhle, S.; Zipfel, S.; Junne, F. The Effectiveness of Health-Oriented Leadership Interventions for the Improvement of Mental Health of Employees in the Health Care Sector: A Systematic Review. Int. Arch. Occup. Environ. Health 2021, 94, 203–220. [Google Scholar] [CrossRef] [PubMed]
- Wampold, B.E.; Flückiger, C. The Alliance in Mental Health Care: Conceptualization, Evidence and Clinical Applications. World Psychiatry 2023, 22, 25–41. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Seah, R.Y.T.; Yuen, K.F. Mental Wellbeing in Digital Workplaces: The Role of Digital Resources, Technostress, and Burnout. Technol. Soc. 2025, 81, 102844. [Google Scholar] [CrossRef]
- Ross, S.; Pirraglia, C.; Aquilina Alexandra, M.; Zulla, R. Effective Competency-Based Medical Education Requires Learning Environments That Promote a Mastery Goal Orientation: A Narrative Review. Med. Teach. 2022, 44, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Arboh, F.; Zhu, X.; Atingabili, S.; Yeboah, E.; Drokow, E.K. From Fear to Empowerment: The Impact of Employees AI Awareness on Workplace Well-Being—A New Insight from the JD–R Model. J. Health Organ. Manag. 2025. [Google Scholar] [CrossRef] [PubMed]
- Joo, B.; Ready, K.J. Career Satisfaction: The Influences of Proactive Personality, Performance Goal Orientation, Organizational Learning Culture, and Leader-member Exchange Quality. Career Dev. Int. 2012, 17, 276–295. [Google Scholar] [CrossRef]
- Moe-Byrne, T.; Shepherd, J.; Merecz-Kot, D.; Sinokki, M.; Naumanen, P.; Roijen, L.H.; Feltz-Cornelis, C.V.D. Effectiveness of Tailored Digital Health Interventions for Mental Health at the Workplace: A Systematic Review of Randomised Controlled Trials. PLoS Digit. Health 2022, 1, e0000123. [Google Scholar] [CrossRef]
- Demerouti, E.; Bakker, A.B.; Nachreiner, F.; Schaufeli, W.B. The Job Demands-Resources Model of Burnout. J. Appl. Psychol. 2001, 86, 499–512. [Google Scholar] [CrossRef] [PubMed]
- Scholze, A.; Hecker, A. The Job Demands-Resources Model as a Theoretical Lens for the Bright and Dark Side of Digitization. Comput. Hum. Behav. 2024, 155, 108177. [Google Scholar] [CrossRef]
- Wang, H.; Ding, H.; Kong, X. Understanding Technostress and Employee Well-Being in Digital Work: The Roles of Work Exhaustion and Workplace Knowledge Diversity. Int. J. Manpow. 2022, 44, 334–353. [Google Scholar] [CrossRef]
- Awwad, R.I.; Aljuhmani, H.Y.; Hamdan, S. Examining the Relationships Between Frontline Bank Employees’ Job Demands and Job Satisfaction: A Mediated Moderation Model. Sage Open 2022, 12, 21582440221079880. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. The Job Demands-Resources Model: State of the Art. J. Manag. Psychol. 2007, 22, 309–328. [Google Scholar] [CrossRef]
- Bakker, A.B.; Hakanen, J.J.; Demerouti, E.; Xanthopoulou, D. Job Resources Boost Work Engagement, Particularly When Job Demands Are High. J. Educ. Psychol. 2007, 99, 274–284. [Google Scholar] [CrossRef]
- Kaiser, S.; Patras, J.; Adolfsen, F.; Richardsen, A.M.; Martinussen, M. Using the Job Demands–Resources Model to Evaluate Work-Related Outcomes Among Norwegian Health Care Workers. SAGE Open 2020, 10, 2158244020947436. [Google Scholar] [CrossRef]
- Abdou, A.H.; El-Amin, M.A.-M.M.; Mohammed, E.F.A.; Alboray, H.M.M.; Refai, A.M.S.; Almakhayitah, M.Y.; Albohnayh, A.S.M.; Alismail, A.M.; Almulla, M.O.; Alsaqer, J.S.; et al. Work Stress, Work-Family Conflict, and Psychological Distress among Resort Employees: A JD-R Model and Spillover Theory Perspectives. Front. Psychol. 2024, 15, 181. [Google Scholar] [CrossRef] [PubMed]
- Bakker, A.B.; Xanthopoulou, D.; Demerouti, E. How Does Chronic Burnout Affect Dealing with Weekly Job Demands? A Test of Central Propositions in JD-R and COR-theories. Appl. Psychol. 2023, 72, 389–410. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. Job Demands–Resources Theory. In Wellbeing; Cooper, C.L., Ed.; Wiley: Hoboken, NJ, USA, 2014; pp. 1–28. ISBN 978-1-118-53882-1. [Google Scholar]
- Bakker, A.B.; Demerouti, E. Job Demands–Resources Theory: Taking Stock and Looking Forward. J. Occup. Health Psychol. 2017, 22, 273–285. [Google Scholar] [CrossRef]
- Schaufeli, W.B. Applying the Job Demands-Resources Model: A ‘How to’ Guide to Measuring and Tackling Work Engagement and Burnout. Organ. Dyn. 2017, 46, 120–132. [Google Scholar] [CrossRef]
- Nahrgang, J.D.; Morgeson, F.P.; Hofmann, D.A. Safety at Work: A Meta-Analytic Investigation of the Link between Job Demands, Job Resources, Burnout, Engagement, and Safety Outcomes. J. Appl. Psychol. 2011, 96, 71–94. [Google Scholar] [CrossRef]
- Simbula, S.; Guglielmi, D.; Schaufeli, W.B. A Three-Wave Study of Job Resources, Self-Efficacy, and Work Engagement among Italian Schoolteachers. Eur. J. Work Organ. Psychol. 2011, 20, 285–304. [Google Scholar] [CrossRef]
- Scholze, A.; Hecker, A. Digital Job Demands and Resources: Digitization in the Context of the Job Demands-Resources Model. Int. J. Environ. Res. Public Health 2023, 20, 6581. [Google Scholar] [CrossRef]
- Bakker, A.; Demerouti, E.; Schaufeli, W. Dual Processes at Work in a Call Centre: An Application of the Job Demands—Resources Model. Eur. J. Work Organ. Psychol. 2003, 12, 393–417. [Google Scholar] [CrossRef]
- Day, A.; Scott, N.; Kelloway, E.K. Information and Communication Technology: Implications for Job Stress and Employee Well-Being. In New Developments in Theoretical and Conceptual Approaches to Job Stress; Emerald Group Publishing Limited: Leeds, UK, 2010; Volume 8, pp. 317–350. ISBN 978-1-84950-712-7. [Google Scholar]
- Carlson, J.R.; Carlson, D.S.; Zivnuska, S.; Harris, R.B.; Harris, K.J. Applying the Job Demands Resources Model to Understand Technology as a Predictor of Turnover Intentions. Comput. Hum. Behav. 2017, 77, 317–325. [Google Scholar] [CrossRef]
- Sun, J.; Shen, H.; Ibn-ul-Hassan, S.; Riaz, A.; Domil, A.E. The Association between Digitalization and Mental Health: The Mediating Role of Wellbeing at Work. Front. Psychiatry 2022, 13, 57. [Google Scholar] [CrossRef]
- Nwankpa, J.; Roumani, Y. IT Capability and Digital Transformation: A Firm Performance Perspective. In Proceedings of the International Conference on Information Systems, Dublin, Ireland, 11–14 December 2016. [Google Scholar]
- Lim, T.K.; Rajabifard, A.; Khoo, V.; Sabri, S.; Chen, Y. Chapter 3—The Smart City in Singapore: How Environmental and Geospatial Innovation Lead to Urban Livability and Environmental Sustainability. In Smart Cities for Technological and Social Innovation; Kim, H.M., Sabri, S., Kent, A., Eds.; Academic Press: Warsaw, Poland, 2021; pp. 29–49. ISBN 978-0-12-818886-6. [Google Scholar]
- Favoretto, C.; de Mendes, G.H.S.; Filho, M.G.; de Oliveira, M.G.; Ganga, G.M.D. Digital Transformation of Business Model in Manufacturing Companies: Challenges and Research Agenda. J. Bus. Amp Ind. Mark. 2021, 37, 748–767. [Google Scholar] [CrossRef]
- Byrd, T.A.; Turner, D.E. An Exploratory Examination of the Relationship between Flexible IT Infrastructure and Competitive Advantage. Inf. Manag. 2001, 39, 41–52. [Google Scholar] [CrossRef]
- Lu, Y.; Ramamurthy, K. Understanding the Link Between Information Technology Capability and Organizational Agility: An Empirical Examination. MIS Q. 2011, 35, 931–954. [Google Scholar] [CrossRef]
- Ayoub, H.S.; Aljuhmani, H.Y. Artificial Intelligence Capabilities as a Catalyst for Enhanced Organizational Performance: The Importance of Cultivating a Data-Driven Culture. In Achieving Sustainable Business Through AI, Technology Education and Computer Science: Volume 2: Teaching Technology and Business Sustainability; Hamdan, A., Ed.; Springer: Cham, Switzerlnd, 2024; pp. 345–356. ISBN 978-3-031-71213-5. [Google Scholar]
- Swanson, E.B.; Ramiller, N.C. Innovating Mindfully with Information Technology. MIS Q. 2004, 28, 553–583. [Google Scholar] [CrossRef]
- Wu, T.-J.; Li, J.-M.; Wu, Y.J. Employees’ Job Insecurity Perception and Unsafe Behaviours in Human–Machine Collaboration. Manag. Decis. 2022, 60, 2409–2432. [Google Scholar] [CrossRef]
- Schueller, S.M.; Torous, J. Scaling Evidence-Based Treatments through Digital Mental Health. Am. Psychol. 2020, 75, 1093–1104. [Google Scholar] [CrossRef] [PubMed]
- Anastasiadou, O.; Mpogiatzidis, P.; Angelidis, P. Ethical Issues Regarding the Digitalization and Interoperability of Health Services. J. Biotechnol. Bioinform. Res. 2024, 6, 2–7. [Google Scholar]
- Saukkonen, P.; Elovainio, M.; Virtanen, L.; Kaihlanen, A.-M.; Nadav, J.; Lääveri, T.; Vänskä, J.; Viitanen, J.; Reponen, J.; Heponiemi, T. The Interplay of Work, Digital Health Usage, and the Perceived Effects of Digitalization on Physicians’ Work: Network Analysis Approach. J. Med. Internet Res. 2022, 24, e38714. [Google Scholar] [CrossRef] [PubMed]
- Rudd, B.N.; Beidas, R.S. Digital Mental Health: The Answer to the Global Mental Health Crisis? JMIR Ment. Health 2020, 7, e18472. [Google Scholar] [CrossRef]
- Khawaja, K.F.; Sarfraz, M.; Rashid, M.; Rashid, M. How Is COVID-19 Pandemic Causing Employee Withdrawal Behavior in the Hospitality Industry? An Empirical Investigation. J. Hosp. Tour. Insights 2021, 5, 687–706. [Google Scholar] [CrossRef]
- Iyamu, I.; Xu, A.X.T.; Gómez-Ramírez, O.; Ablona, A.; Chang, H.-J.; Mckee, G.; Gilbert, M. Defining Digital Public Health and the Role of Digitization, Digitalization, and Digital Transformation: Scoping Review. JMIR Public Health Surveill. 2021, 7, e30399. [Google Scholar] [CrossRef]
- Aljuhmani, H.Y.; Awwad, R.I.; Albuhisi, B.; Hamdan, S. The Impact of Digital Transformation Leadership Competencies on Firm Performance Through the Lens of Organizational Creativity and Digital Strategy. In Innovative and Intelligent Digital Technologies; Towards an Increased Efficiency; Al Mubarak, M., Hamdan, A., Eds.; Springer: Cham, Switzerland, 2024; Volume 1, pp. 283–293. ISBN 978-3-031-70399-7. [Google Scholar]
- Kilbourne, A.M.; Beck, K.; Spaeth-Rublee, B.; Ramanuj, P.; O’Brien, R.W.; Tomoyasu, N.; Pincus, H.A. Measuring and Improving the Quality of Mental Health Care: A Global Perspective. World Psychiatry 2018, 17, 30–38. [Google Scholar] [CrossRef]
- Diebig, M.; Müller, A.; Angerer, P. Impact of the Digitization in the Industry Sector on Work, Employment, and Health. In Handbook of Socioeconomic Determinants of Occupational Health: From Macro-Level to Micro-Level Evidence; Theorell, T., Ed.; Springer International Publishing: Cham, Switzerland, 2020; pp. 1–15. ISBN 978-3-030-05031-3. [Google Scholar]
- Hariram, N.P.; Mekha, K.B.; Suganthan, V.; Sudhakar, K. Sustainalism: An Integrated Socio-Economic-Environmental Model to Address Sustainable Development and Sustainability. Sustainability 2023, 15, 10682. [Google Scholar] [CrossRef]
- Mostepaniuk, A.; Nasr, E.; Awwad, R.I.; Hamdan, S.; Aljuhmani, H.Y. Managing a Relationship between Corporate Social Responsibility and Sustainability: A Systematic Review. Sustainability 2022, 14, 11203. [Google Scholar] [CrossRef]
- Hussain, A.; Umair, M.; Khan, S.; Alonazi, W.B.; Almutairi, S.S.; Malik, A. Exploring Sustainable Healthcare: Innovations in Health Economics, Social Policy, and Management. Heliyon 2024, 10, e33186. [Google Scholar] [CrossRef] [PubMed]
- Tommasetti, A.; Singer, P.; Troisi, O.; Maione, G. Extended Theory of Planned Behavior (ETPB): Investigating Customers’ Perception of Restaurants’ Sustainability by Testing a Structural Equation Model. Sustainability 2018, 10, 2580. [Google Scholar] [CrossRef]
- Syed, S.; Acquaye, A.; Khalfan, M.M.; Obuobisa-Darko, T.; Yamoah, F.A. Decoding Sustainable Consumption Behavior: A Systematic Review of Theories and Models and Provision of a Guidance Framework. Resour. Conserv. Recycl. Adv. 2024, 23, 200232. [Google Scholar] [CrossRef]
- Sandra Marcelline, T.R.; Ye, C.; Ralison Ny Avotra, A.A.; Hussain, Z.; Zonia, J.E.; Nawaz, A. Impact of Green Construction Procurement on Achieving Sustainable Economic Growth Influencing Green Logistic Services Management and Innovation Practices. Front. Environ. Sci. 2022, 9, 815928. [Google Scholar] [CrossRef]
- Enbaia, E.; Alzubi, A.; Iyiola, K.; Aljuhmani, H.Y. The Interplay Between Environmental Ethics and Sustainable Performance: Does Organizational Green Culture and Green Innovation Really Matter? Sustainability 2024, 16, 10230. [Google Scholar] [CrossRef]
- Moro Visconti, R.; Morea, D. Healthcare Digitalization and Pay-For-Performance Incentives in Smart Hospital Project Financing. Int. J. Environ. Res. Public Health 2020, 17, 2318. [Google Scholar] [CrossRef]
- Mousa, S.K.; Othman, M. The Impact of Green Human Resource Management Practices on Sustainable Performance in Healthcare Organisations: A Conceptual Framework. J. Clean. Prod. 2020, 243, 118595. [Google Scholar] [CrossRef]
- Serbanati, L.D. Health Digital State and Smart EHR Systems. Inform. Med. Unlocked 2020, 21, 100494. [Google Scholar] [CrossRef]
- Bevere, D.; Faccilongo, N. Shaping the Future of Healthcare: Integrating Ecology and Digital Innovation. Sustainability 2024, 16, 3835. [Google Scholar] [CrossRef]
- Jones, C.H.; Madhavan, S.; Natarajan, K.; Corbo, M.; True, J.M.; Dolsten, M. Rewriting the Textbook for Pharma: How to Adapt and Thrive in a Digital, Personalized and Collaborative World. Drug Discov. Today 2024, 29, 104112. [Google Scholar] [CrossRef] [PubMed]
- Stoumpos, A.I.; Kitsios, F.; Talias, M.A. Digital Transformation in Healthcare: Technology Acceptance and Its Applications. Int. J. Environ. Res. Public Health 2023, 20, 3407. [Google Scholar] [CrossRef] [PubMed]
- Liang, R.; Huang, C.; Zhang, C.; Li, B.; Saydam, S.; Canbulat, I. Exploring the Fusion Potentials of Data Visualization and Data Analytics in the Process of Mining Digitalization. IEEE Access 2023, 11, 40608–40628. [Google Scholar] [CrossRef]
- Aljuhmani, H.Y.; Neiroukh, S. From AI Capability to Enhanced Organizational Performance: The Path Through Organizational Creativity. In Achieving Sustainable Business Through AI, Technology Education and Computer Science: Volume 2: Teaching Technology and Business Sustainability; Hamdan, A., Ed.; Springer: Cham, Switzerland, 2024; pp. 667–676. ISBN 978-3-031-71213-5. [Google Scholar]
- Costin, A.; Roman, A.F.; Balica, R.-S. Remote Work Burnout, Professional Job Stress, and Employee Emotional Exhaustion during the COVID-19 Pandemic. Front. Psychol. 2023, 14, 1193854. [Google Scholar] [CrossRef] [PubMed]
- Kane, H.; Baumgart, J.G.; El-Hage, W.; Deloyer, J.; Maes, C.; Lebas, M.-C.; Marazziti, D.; Thome, J.; Fond-Harmant, L.; Denis, F. Opportunities and Challenges for Professionals in Psychiatry and Mental Health Care Using Digital Technologies During the COVID-19 Pandemic: Systematic Review. JMIR Hum. Factors 2022, 9, e30359. [Google Scholar] [CrossRef] [PubMed]
- Bail, C.; Harth, V.; Mache, S. Digitalization in Urology—A Multimethod Study of the Relationships between Physicians’ Technostress, Burnout, Work Engagement and Job Satisfaction. Healthcare 2023, 11, 2255. [Google Scholar] [CrossRef]
- Jain, A.; Hassard, J.; Leka, S.; Di Tecco, C.; Iavicoli, S. The Role of Occupational Health Services in Psychosocial Risk Management and the Promotion of Mental Health and Well-Being at Work. Int. J. Environ. Res. Public Health 2021, 18, 3632. [Google Scholar] [CrossRef]
- Hn, A.; Khan, N.; Hasmi, S.; Chitra, S.A.; Doshi, S.S.; Mahesh, R.; Shetti, A.N. Rescuing the Rescuers: Combating Burnout in the Emergency Medicine Department. Mathews J. Emerg. Med. 2023, 8, 59. [Google Scholar] [CrossRef]
- Dion, H.; Evans, M.; Farrell, P. Hospitals Management Transformative Initiatives; towards Energy Efficiency and Environmental Sustainability in Healthcare Facilities. J. Eng. Des. Technol. 2022, 21, 552–584. [Google Scholar] [CrossRef]
- Søvold, L.E.; Naslund, J.A.; Kousoulis, A.A.; Saxena, S.; Qoronfleh, M.W.; Grobler, C.; Münter, L. Prioritizing the Mental Health and Well-Being of Healthcare Workers: An Urgent Global Public Health Priority. Front. Public Health 2021, 9, 679397. [Google Scholar] [CrossRef]
- Caruso, R.; Toffanin, T.; Folesani, F.; Biancosino, B.; Romagnolo, F.; Riba, M.B.; McFarland, D.; Palagini, L.; Belvederi Murri, M.; Zerbinati, L.; et al. Violence Against Physicians in the Workplace: Trends, Causes, Consequences, and Strategies for Intervention. Curr. Psychiatry Rep. 2022, 24, 911–924. [Google Scholar] [CrossRef]
- Zhang, Z.; Li, Y.; Wang, S.; Wang, J.; Huang, Y.; Wang, X.; Guo, H.; Zhou, J. Exploring the Impact of Workplace Violence on the Mental Health of Chinese Correctional Officers: A JD-R Model Approach. Psychol. Res. Behav. Manag. 2024, 17, 2865–2874. [Google Scholar] [CrossRef] [PubMed]
- Brouwers, E.P.M. Social Stigma Is an Underestimated Contributing Factor to Unemployment in People with Mental Illness or Mental Health Issues: Position Paper and Future Directions. BMC Psychol. 2020, 8, 36. [Google Scholar] [CrossRef]
- Kruize, H.; van der Vliet, N.; Staatsen, B.; Bell, R.; Chiabai, A.; Muiños, G.; Higgins, S.; Quiroga, S.; Martinez-Juarez, P.; Aberg Yngwe, M.; et al. Urban Green Space: Creating a Triple Win for Environmental Sustainability, Health, and Health Equity through Behavior Change. Int. J. Environ. Res. Public Health 2019, 16, 4403. [Google Scholar] [CrossRef] [PubMed]
- Hanna, P.; Wijesinghe, S.; Paliatsos, I.; Walker, C.; Adams, M.; Kimbu, A. Active Engagement with Nature: Outdoor Adventure Tourism, Sustainability and Wellbeing. J. Sustain. Tour. 2019, 27, 1355–1373. [Google Scholar] [CrossRef]
- Folker, A.P.; Mathiasen, K.; Lauridsen, S.M.; Stenderup, E.; Dozeman, E.; Folker, M.P. Implementing Internet-Delivered Cognitive Behavior Therapy for Common Mental Health Disorders: A Comparative Case Study of Implementation Challenges Perceived by Therapists and Managers in Five European Internet Services. Internet Interv. 2018, 11, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of Depression, Anxiety, and Insomnia among Healthcare Workers during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Sarfraz, M.; Ivascu, L.; Iqbal, K.; Mansoor, A. How Did Work-Related Depression, Anxiety, and Stress Hamper Healthcare Employee Performance during COVID-19? The Mediating Role of Job Burnout and Mental Health. Int. J. Environ. Res. Public Health 2022, 19, 10359. [Google Scholar] [CrossRef]
- Haddon, J. The Impact of Employees’ Well-Being on Performance in the Workplace. Strateg. HR Rev. 2018, 17, 72–75. [Google Scholar] [CrossRef]
- Seaton, C.L.; Bottorff, J.L.; Oliffe, J.L.; Medhurst, K.; DeLeenheer, D. Mental Health Promotion in Male-Dominated Workplaces: Perspectives of Male Employees and Workplace Representatives. Psychol. Men Masculinities 2019, 20, 541–552. [Google Scholar] [CrossRef]
- Howarth, A.; Quesada, J.; Silva, J.; Judycki, S.; Mills, P.R. The Impact of Digital Health Interventions on Health-Related Outcomes in the Workplace: A Systematic Review. Digit. Health 2018, 4, 2055207618770861. [Google Scholar] [CrossRef]
- Saleem, F.; Malik, M.I.; Qureshi, S.S. Work Stress Hampering Employee Performance During COVID-19: Is Safety Culture Needed? Front. Psychol. 2021, 12, 655839. [Google Scholar] [CrossRef]
- Lei, L.; Huang, X.; Zhang, S.; Yang, J.; Yang, L.; Xu, M. Comparison of Prevalence and Associated Factors of Anxiety and Depression Among People Affected by versus People Unaffected by Quarantine During the COVID-19 Epidemic in Southwestern China. Med. Sci. Monit. 2020, 26, e924609. [Google Scholar] [CrossRef] [PubMed]
- Adamopoulos, I.P.; Syrou, N.F. Associations and Correlations of Job Stress, Job Satisfaction and Burn out in Public Health Sector. Eur. J. Environ. Public Health 2022, 6, em0113. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.-W.; Gao, G.; Agarwal, R. Reciprocity or Self-Interest? Leveraging Digital Social Connections for Healthy Behavior. MIS Q. 2022, 46, 261–298. [Google Scholar] [CrossRef]
- Chuang, L.-M.; Huang, S.-H. AI-Supported Healthcare Technology Resistance and Behavioral Intention: A Serial Mediation Empirical Study on the JD-R Model and Employee Engagement. Systems 2025, 13, 268. [Google Scholar] [CrossRef]
- Chen, S.; Ebrahimi, O.V.; Cheng, C. New Perspective on Digital Well-Being by Distinguishing Digital Competency from Dependency: Network Approach. J. Med. Internet Res. 2025, 27, e70483. [Google Scholar] [CrossRef]
- Kumi, E.; Amoako, G.K.; Appiah, T.; Dartey-Baah, K. The Impact of Digital Transformation on Organisational Dynamics, HR Practices, and Wellbeing in Ghana’s Healthcare Sector: A Social Exchange Perspective. Futur. Bus. J. 2025, 11, 64. [Google Scholar] [CrossRef]
- Ahsan, M.J. Cultivating a Culture of Learning: The Role of Leadership in Fostering Lifelong Development. Learn. Organ. 2024, 32, 282–306. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Pratap Singh, R.; Suman, R. Medical 4.0 Technologies for Healthcare: Features, Capabilities, and Applications. Internet Things Cyber-Phys. Syst. 2022, 2, 12–30. [Google Scholar] [CrossRef]
- Satar, M.S.; Alharthi, S.; Omeish, F.; Alshibani, S.M.; Saqib, N. Digital Learning Orientation and Entrepreneurial Competencies in Graduates: Is Blended Learning Sustainable? Sustainability 2024, 16, 7794. [Google Scholar] [CrossRef]
- Xanthopoulou, D.; Bakker, A.B.; Demerouti, E.; Schaufeli, W.B. The Role of Personal Resources in the Job Demands-Resources Model. Int. J. Stress Manag. 2007, 14, 121–141. [Google Scholar] [CrossRef]
- Gong, Y.; Huang, J.-C.; Farh, J.-L. Employee Learning Orientation, Transformational Leadership, and Employee Creativity: The Mediating Role of Employee Creative Self-Efficacy. Acad. Manag. J. 2009, 52, 765–778. [Google Scholar] [CrossRef]
- Liang, X.; Guo, G.; Shu, L.; Gong, Q.; Luo, P. Investigating the Double-Edged Sword Effect of AI Awareness on Employee’s Service Innovative Behavior. Tour. Manag. 2022, 92, 104564. [Google Scholar] [CrossRef]
- Maurer, T.J. Employee Learning and Development Orientation: Toward an Integrative Model of Involvement in Continuous Learning. Hum. Resour. Dev. Rev. 2002, 1, 9–44. [Google Scholar] [CrossRef]
- Zahoor, N.; Donbesuur, F.; Christofi, M.; Miri, D. Technological Innovation and Employee Psychological Well-Being: The Moderating Role of Employee Learning Orientation and Perceived Organizational Support. Technol. Forecast. Soc. Change 2022, 179, 121610. [Google Scholar] [CrossRef]
- Sajwani, R.A. Sustainability in Healthcare Practice. In Proceedings of the BUiD Doctoral Research Conference 2023, Dubai, United Arab Emirates, 8 July 2023; Al Marri, K., Mir, F.A., David, S.A., Al-Emran, M., Eds.; Springer Nature Switzerland: Cham, Switzerland, 2024; pp. 255–263. [Google Scholar]
- Tucmeanu, E.R.; Tucmeanu, A.I.; Iliescu, M.G.; Żywiołek, J.; Yousaf, Z. Successful Management of IT Projects in Healthcare Institutions after COVID-19: Role of Digital Orientation and Innovation Adaption. Healthcare 2022, 10, 2005. [Google Scholar] [CrossRef] [PubMed]
- Nasr, E.; Emeagwali, O.L.; Aljuhmani, H.Y.; Al-Geitany, S. Destination Social Responsibility and Residents’ Environmentally Responsible Behavior: Assessing the Mediating Role of Community Attachment and Involvement. Sustainability 2022, 14, 14153. [Google Scholar] [CrossRef]
- Aljuhmani, H.Y.; Emeagwali, O.L.; Ababneh, B. The Relationships between CEOs’ Psychological Attributes, Top Management Team Behavioral Integration and Firm Performance. Int. J. Organ. Theory Behav. 2021, 24, 126–145. [Google Scholar] [CrossRef]
- Podsakoff, P.M.; MacKenzie, S.B.; Lee, J.-Y.; Podsakoff, N.P. Common Method Biases in Behavioral Research: A Critical Review of the Literature and Recommended Remedies. J. Appl. Psychol. 2003, 88, 879–903. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Luo, C.; Pan, L. Do Digitalization and Intellectual Capital Drive Sustainable Open Innovation of Natural Resources Sector? Evidence from China. Resour. Policy 2024, 88, 104345. [Google Scholar] [CrossRef]
- Demo, G.; Paschoal, T. Well-Being at Work Scale: Exploratory and Confirmatory Validation in the USA. Paidéia 2016, 26, 35–43. [Google Scholar] [CrossRef]
- Vandewalle, D. Development and Validation of a Work Domain Goal Orientation Instrument. Educ. Psychol. Meas. 1997, 57, 995–1015. [Google Scholar] [CrossRef]
- Aljuhmani, H.Y.; Emeagwali, O.L.; Ababneh, B. Revisiting the Miles and Snow Typology of Organizational Strategy: Uncovering Interrelationships between Strategic Decision-Making and Public Organizational Performance. Int. Rev. Public Adm. 2021, 26, 209–229. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson: Upper Saddle River, NJ, USA, 2009; ISBN 978-0-13-813263-7. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 3rd ed.; Methodology in the Social Sciences; The Guilford Press: New York, NY, USA; London, UK, 2022; ISBN 978-1-4625-4903-0. [Google Scholar]
- Ayouz, H.; Alzubi, A.; Iyiola, K. Using Benevolent Leadership to Improve Safety Behaviour in the Construction Industry: A Moderated Mediation Model of Safety Knowledge and Safety Training and Education. Int. J. Occup. Saf. Ergon. 2024, 31, 167–180. [Google Scholar] [CrossRef] [PubMed]
- Iyiola, K.; Alzubi, A.; Dappa, K. The Influence of Learning Orientation on Entrepreneurial Performance: The Role of Business Model Innovation and Risk-Taking Propensity. J. Open Innov. Technol. Mark. Complex. 2023, 9, 100133. [Google Scholar] [CrossRef]
- Aiken, L.S.; West, S.G. Multiple Regression: Testing and Interpreting Interactions; SAGE Publications, Inc: Newbury Park, CA, USA, 1991; ISBN 978-0-7619-0712-1. [Google Scholar]
- Abuzawida, S.S.; Alzubi, A.B.; Iyiola, K. Sustainable Supply Chain Practices: An Empirical Investigation from the Manufacturing Industry. Sustainability 2023, 15, 14395. [Google Scholar] [CrossRef]
- Alsafadi, Y.; Aljuhmani, H.Y. The Influence of Entrepreneurial Innovations in Building Competitive Advantage: The Mediating Role of Entrepreneurial Thinking. Kybernetes 2023, 53, 4051–4073. [Google Scholar] [CrossRef]
- Lindell, M.K.; Whitney, D.J. Accounting for Common Method Variance in Cross-Sectional Research Designs. J. Appl. Psychol. 2001, 86, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, J.S.; Overton, T.S. Estimating Nonresponse Bias in Mail Surveys. J. Mark. Res. 1977, 14, 396–402. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming, 3rd ed.; Routledge: Vienna, Austria, 2016. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Aljuhmani, H.Y.; Ababneh, B.; Emeagwali, L.; Elrehail, H. Strategic Stances and Organizational Performance: Are Strategic Performance Measurement Systems the Missing Link? Asia-Pac. J. Bus. Adm. 2022, 16, 282–306. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria versus New Alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Iyiola, K.; Rjoub, H. Using Conflict Management in Improving Owners and Contractors Relationship Quality in the Construction Industry: The Mediation Role of Trust. Sage Open 2020, 10, 2158244019898834. [Google Scholar] [CrossRef]
- Ramadhan, A.; Iyiola, K.; Alzubi, A.B. Linking Absorptive Capacity to Project Success via Mediating Role of Customer Knowledge Management Capability: The Role of Environmental Complexity. Bus. Process Manag. J. 2024, 30, 939–962. [Google Scholar] [CrossRef]
- Neiroukh, S.; Emeagwali, O.L.; Aljuhmani, H.Y. Artificial Intelligence Capability and Organizational Performance: Unraveling the Mediating Mechanisms of Decision-Making Processes. Manag. Decis. 2024. [Google Scholar] [CrossRef]
- Preacher, K.J.; Rucker Derek, D.; Hayes, A.F. Addressing Moderated Mediation Hypotheses: Theory, Methods, and Prescriptions. Multivar. Behav. Res. 2007, 42, 185–227. [Google Scholar] [CrossRef]
- Bachmann, N.; Tripathi, S.; Brunner, M.; Jodlbauer, H. The Contribution of Data-Driven Technologies in Achieving the Sustainable Development Goals. Sustainability 2022, 14, 2497. [Google Scholar] [CrossRef]
- Sony, M.; Antony, J.; Tortorella, G.L. Critical Success Factors for Successful Implementation of Healthcare 4.0: A Literature Review and Future Research Agenda. Int. J. Environ. Res. Public Health 2023, 20, 4669. [Google Scholar] [CrossRef] [PubMed]
- Beaulieu, M.; Bentahar, O. Digitalization of the Healthcare Supply Chain: A Roadmap to Generate Benefits and Effectively Support Healthcare Delivery. Technol. Forecast. Soc. Change 2021, 167, 120717. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Bakker, A.B.; Van Rhenen, W. How Changes in Job Demands and Resources Predict Burnout, Work Engagement, and Sickness Absenteeism. J. Organ. Behav. 2009, 30, 893–917. [Google Scholar] [CrossRef]
- Skogstad, L.F. Institutional Work Aimed at Increasing Employment Orientation in Mental Health Services. J. Health Organ. Manag. 2024, 39, 130–146. [Google Scholar] [CrossRef] [PubMed]
- Xu, G.; Xue, M.; Zhao, J. The Relationship of Artificial Intelligence Opportunity Perception and Employee Workplace Well-Being: A Moderated Mediation Model. Int. J. Environ. Res. Public Health 2023, 20, 1974. [Google Scholar] [CrossRef]
- Gagliardi, A.R.; Tomaselli, G. Aligning Corporate Social Responsibility with Artificial Intelligence in Healthcare in the Context of the Post-COVID-19 Recovery: A Viewpoint. J. Health Organ. Manag. 2025. [Google Scholar] [CrossRef] [PubMed]
- Tarafdar, M.; Cooper, C.L.; Stich, J. The Technostress Trifecta-Techno Eustress, Techno Distress and Design: Theoretical Directions and an Agenda for Research. Inf. Syst. J. 2019, 29, 6–42. [Google Scholar] [CrossRef]
- Bernburg, M.; Gebhardt, J.S.; Groneberg, D.A.; Mache, S. Impact of Digitalization in Dentistry on Technostress, Mental Health, and Job Satisfaction: A Quantitative Study. Healthcare 2025, 13, 72. [Google Scholar] [CrossRef] [PubMed]
- Pansini, M.; Buonomo, I.; De Vincenzi, C.; Ferrara, B.; Benevene, P. Positioning Technostress in the JD-R Model Perspective: A Systematic Literature Review. Healthcare 2023, 11, 446. [Google Scholar] [CrossRef] [PubMed]
- Wahab, M.A.; Tatoglu, E. Chasing Productivity Demands, Worker Well-Being, and Firm Performance: The Moderating Effects of HR Support and Flexible Work Arrangements. Pers. Rev. 2020, 49, 1823–1843. [Google Scholar] [CrossRef]
- Singelis, T.M.; Triandis, H.C.; Bhawuk, D.P.S.; Gelfand, M.J. Horizontal and Vertical Dimensions of Individualism and Collectivism: A Theoretical and Measurement Refinement. Cross-Cult. Res. 1995, 29, 240–275. [Google Scholar] [CrossRef]

| Information (n = 503) | Category | Number | (%) Proportion |
|---|---|---|---|
| Gender | |||
| Male | 306 | 60.83 | |
| Female | 197 | 39.17 | |
| Education | |||
| Below graduate degree | 9 | 1.79 | |
| Graduate degree | 382 | 75.94 | |
| Postgraduate and above | 112 | 22.27 | |
| Marital status | |||
| Single | 207 | 41.15 | |
| Married | 266 | 52.88 | |
| Prefer not to say | 30 | 5.97 |
| Constructs | Items | α | λ | CR | AVE |
|---|---|---|---|---|---|
| Digitalization | |||||
| IT Infrastructure | ITI1 | 0.894 | 0.747 | 0.895 | 0.681 |
| ITI2 | 0.835 | ||||
| ITI3 | 0.873 | ||||
| ITI4 | 0.842 | ||||
| IT Proactive Stance | ITP1 | 0.895 | 0.823 | 0.897 | 0.687 |
| ITP2 | 0.890 | ||||
| ITP3 | 0.849 | ||||
| ITP4 | 0.747 | ||||
| Mental Health | MH1 | 0.948 | 0.747 | 0.945 | 0.658 |
| MH2 | 0.777 | ||||
| MH3 | 0.747 | ||||
| MH4 | 0.793 | ||||
| MH5 | 0.859 | ||||
| MH6 | 0.844 | ||||
| MH7 | 0.835 | ||||
| MH8 | 0.851 | ||||
| MH9 | 0.837 | ||||
| Learning Orientation | LO1 | 0.879 | 0.871 | 0.872 | 0.633 |
| LO2 | 0.905 | ||||
| LO3 | 0.688 | ||||
| LO4 | 0.695 | ||||
| Sustainable Economic Behavior | SEB1 | 0.869 | 0.790 | 0.868 | 0.624 |
| SEB2 | 0.651 | ||||
| SEB3 | 0.865 | ||||
| SEB4 | 0.836 |
| Variables | Mean | STD | ITI | ITP | MH | LO | SEB | Gen | Edu |
|---|---|---|---|---|---|---|---|---|---|
| ITI | 6.153 | 0.742 | (0.825) | ||||||
| ITP | 6.130 | 0.732 | 0.719 ** | (0.829) | |||||
| MH | 6.120 | 0.692 | 0.697 ** | 0.730 ** | (0.811) | ||||
| LO | 6.149 | 0.709 | 0.602 ** | 0.652 ** | 0.713 ** | (0.796) | |||
| SEB | 6.343 | 0.623 | 0.656 ** | 0.662 ** | 0.698 ** | 0.682 ** | (0.790) | ||
| Gen | - | - | 0.023 | 0.033 | 0.032 | 0.054 | 0.001 | - | |
| Edu | - | - | 0.015 | 0.018 | 0.024 | 0.010 | 0.023 | 0.011 | - |
| Model | χ2/df | CFI | TLI | IFI | NFI | RMSEA |
|---|---|---|---|---|---|---|
| Criterion | <3 | >0.9 | >0.9 | >0.9 | >0.9 | <0.08 |
| One-factor model | 11.876 | 0.412 | 0.399 | 0.409 | 0.378 | 0.254 |
| Four-factor model (research model) | 2.700 | 0.940 | 0.931 | 0.940 | 0.908 | 0.070 |
| Five-factor model | 3.964 | 0.701 | 0.690 | 0.700 | 0.657 | 0.183 |
| Response Variable | Independent Variable | β | S.E | T-Values | p-Values | 95% CI |
|---|---|---|---|---|---|---|
| Model I: EMH | Constant | 3.429 | 0.304 | 11.278 | 0.001 | [2.831, 4.028] |
| H1 | Digitalization | 0.450 | 0.049 | 9.151 | 0.001 | [0.353, 0.547] |
| R2 = 0.195 | ||||||
| Model II: SEB | Constant | 0.969 | 0.308 | 3.154 | 0.002 | [0.365, 1.574] |
| H2 | Digitalization | 0.342 | 0.047 | 7.223 | 0.001 | [0.249, 0.436] |
| H3 | EMH | 0.500 | 0.046 | 10.747 | 0.001 | [0.409, 0.591] |
| R2 = 0.460 | ||||||
| The indirect effect of digitalization on SEB through EMH | ||||||
| Direct effect of X on Y | 0.342 | 0.047 | 7.223 | 0.001 | [0.249, 0.436] | |
| Total effect of X on Y | 0.568 | 0.049 | 11.565 | 0.001 | [0.471, 0.664] | |
| H4: Bootstrap indirect effects | Bootse | BootLLCI | BootULCI | |||
| Digitalization → EMH → SEB | 0.226 | 0.049 | - | 0.135 | 0.330 | |
| Relationship | β | S.E | T-Values | p-Values | 95% CI |
|---|---|---|---|---|---|
| Model I: Mediator construct model for predicting EMH | |||||
| Constant | 0.049 | 0.037 | 1.326 | 0.186 | [−0.023, 0.121] |
| Gender | 0.025 | 0.071 | 0.608 | 0.729 | [−0.202, 0.049] |
| Education | 0.023 | 0.070 | 0.602 | 0.704 | [−0.198, 0.038] |
| Digitalization | 0.186 | 0.064 | 2.912 | 0.004 | [0.061, 0.313] |
| LO | 0.299 | 0.060 | 4.967 | 0.001 | [0.181, 0.417] |
| H5: Digitalization × LO | 0.151 | 0.052 | 2.881 | 0.004 | [0.048, 0.253] |
| R2 = 0.273 | |||||
| The conditional direct effect of digitalization on EMH at different levels of LO | |||||
| LO (−1SD) | 0.078 | 0.083 | 0.946 | 0.345 | [−0.085, 0.241] |
| LO (+1SD) | 0.295 | 0.065 | 4.558 | 0.000 | [0.168, 0.422] |
| Model II: Dependent variable model for predicting SEB | |||||
| Intercept | 5.245 | 0.033 | 185.358 | 0.001 | [6.113, 6.244] |
| Gender | 0.044 | 0.048 | 1.227 | 0.202 | [−0.019, 0.053] |
| Education | 0.040 | 0.053 | 1.199 | 0.218 | [−0.20, 0.055] |
| Digitalization | 0.293 | 0.058 | 5.009 | 0.001 | [0.177, 0.407] |
| EMH | 0.476 | 0.049 | 9.798 | 0.001 | [0.380, 0.571] |
| LO | 0.078 | 0.058 | 1.356 | 0.175 | [−0.035, 0.192] |
| H6: Digitalization × LO | 0.122 | 0.054 | 2.262 | 0.024 | [0.016, 0.228] |
| Interaction: EMH × LO | 0.128 | 0.047 | 2.713 | 0.007 | [0.035, 0.221] |
| R2 = 0.730 | |||||
| The conditional direct effect of digitalization on SEB at different levels of LO | |||||
| LO (−1SD) | 0.205 | 0.078 | 2.640 | 0.009 | [0.052, 0.357] |
| LO (+1SD) | 0.380 | 0.062 | 6.164 | 0.001 | [0.259, 0.501] |
| H7: The conditional indirect effect of digitalization on SEB via EMH at different levels of LO | |||||
| LO (−1SD) | 0.046 | 0.057 | - | - | [−0.069, 0.164] |
| LO (+1SD) | 0.113 | 0.055 | - | - | [0.036, 0.248] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alkish, I.; Iyiola, K.; Alzubi, A.B.; Aljuhmani, H.Y. Does Digitization Lead to Sustainable Economic Behavior? Investigating the Roles of Employee Well-Being and Learning Orientation. Sustainability 2025, 17, 4365. https://doi.org/10.3390/su17104365
Alkish I, Iyiola K, Alzubi AB, Aljuhmani HY. Does Digitization Lead to Sustainable Economic Behavior? Investigating the Roles of Employee Well-Being and Learning Orientation. Sustainability. 2025; 17(10):4365. https://doi.org/10.3390/su17104365
Chicago/Turabian StyleAlkish, Ibrahim, Kolawole Iyiola, Ahmad Bassam Alzubi, and Hasan Yousef Aljuhmani. 2025. "Does Digitization Lead to Sustainable Economic Behavior? Investigating the Roles of Employee Well-Being and Learning Orientation" Sustainability 17, no. 10: 4365. https://doi.org/10.3390/su17104365
APA StyleAlkish, I., Iyiola, K., Alzubi, A. B., & Aljuhmani, H. Y. (2025). Does Digitization Lead to Sustainable Economic Behavior? Investigating the Roles of Employee Well-Being and Learning Orientation. Sustainability, 17(10), 4365. https://doi.org/10.3390/su17104365







