The Relationship between the Parameters That Characterize a Built Living Space and the Health Status of Its Inhabitants
Abstract
1. Introduction
- Provide a comprehensive overview of the connection between the living environment and health conditions, with a particular emphasis on housing factors, interior air quality, green building practices, and the implications of technology transfer for health issues according to building construction approaches;
- Update the current state of knowledge by targeting this relationship, which can generate major health risks, especially as many studies have investigated the effect of environmental factors on health outcomes but very few have examined the relationship between housing and health;
- Contribute to the scientific field by providing novel insights into the most significant stakeholders with implications for the interaction of housing factors with health and the environment in order to reduce the risks of housing-related diseases, increase IAQ, and increase awareness of sustainable building approaches.
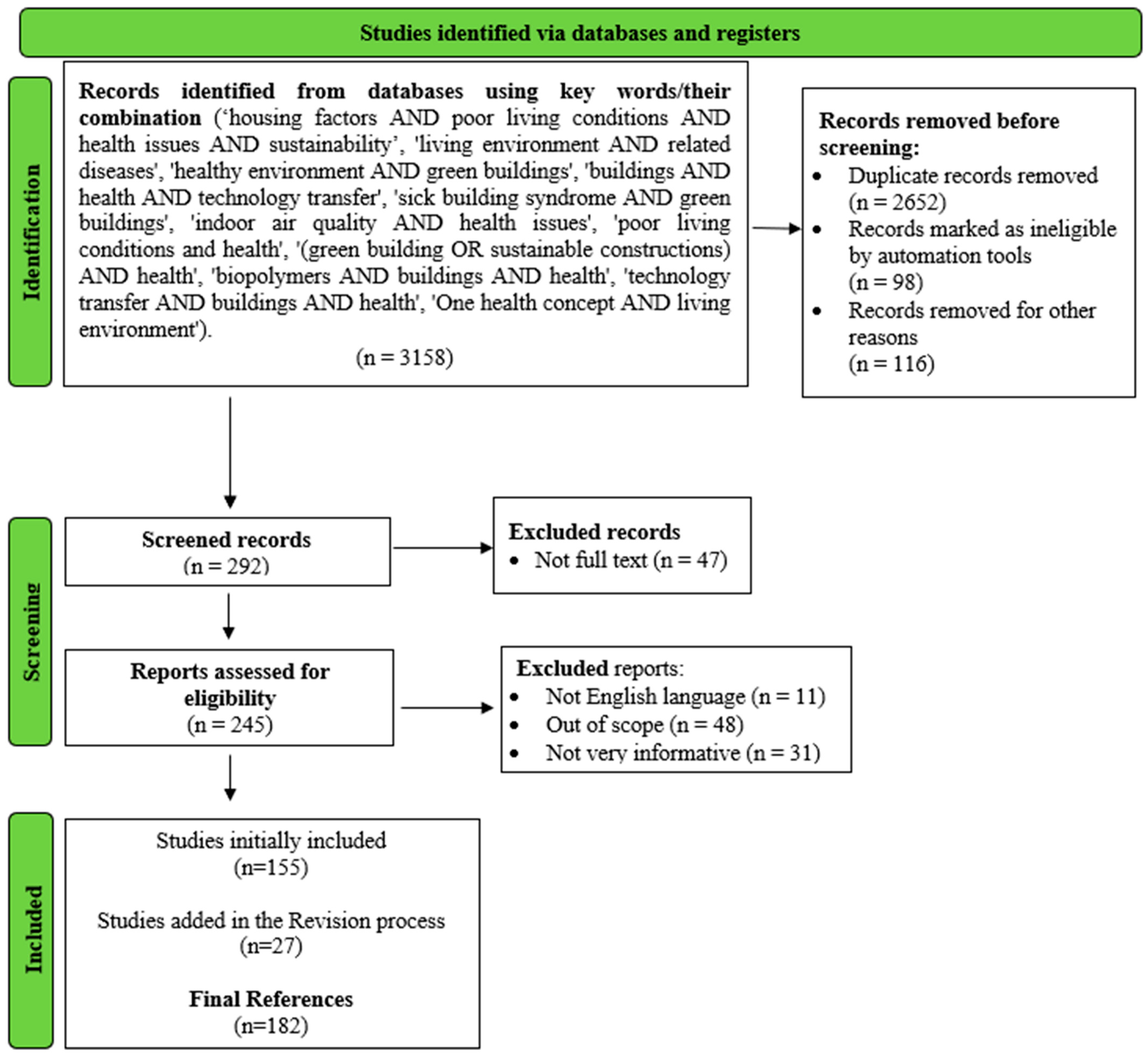
2. Methodology of Research
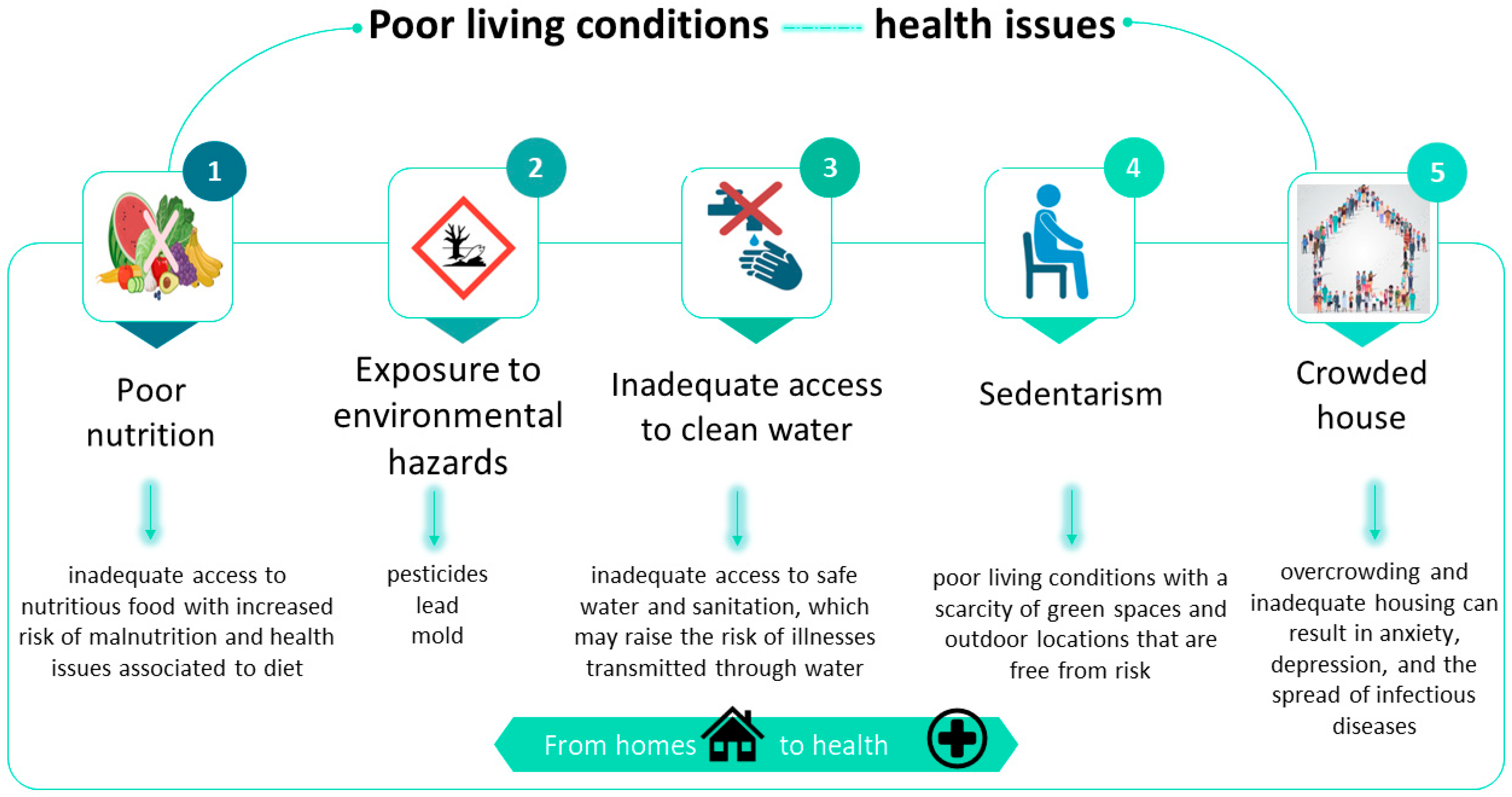
3. Diseases Resulting from Living Conditions
3.1. Respiratory Diseases
3.1.1. Asthma
3.1.2. Lung Cancer
- →
- Housing conditions are believed to influence cancer care and its results through various mechanisms, with substandard housing potentially elevating the likelihood of lung cancer [30]. Among the factors that affect IAQ and are implicated in the development of lung cancer are volatile organic compounds (VOCs), passive smoking, and solid fuel emissions [31].
- →
- Presently, exposure to radon in residential settings is acknowledged as the primary cause of lung cancer among non-smokers and the second leading cause among smokers, second only to tobacco [32]. When uranium and radium decompose in the soil, radon is produced as a radioactive natural gas [33]. A 2019 research work conducted in Spain found that non-smoker lung cancer sufferers had radon exposure levels in their homes that were higher than 200 Bq/m3 [32]. Additionally, between 2.2% and 12.4% of lung cancer fatalities in France in 1999 were linked to radon presence in their homes.
3.1.3. Chronic Bronchitis
3.1.4. Respiratory Infections
3.2. Cardiovascular Diseases
3.3. Dermatological Diseases
3.4. Rheumatism
3.5. COVID-19
3.6. Sick Building Syndrome
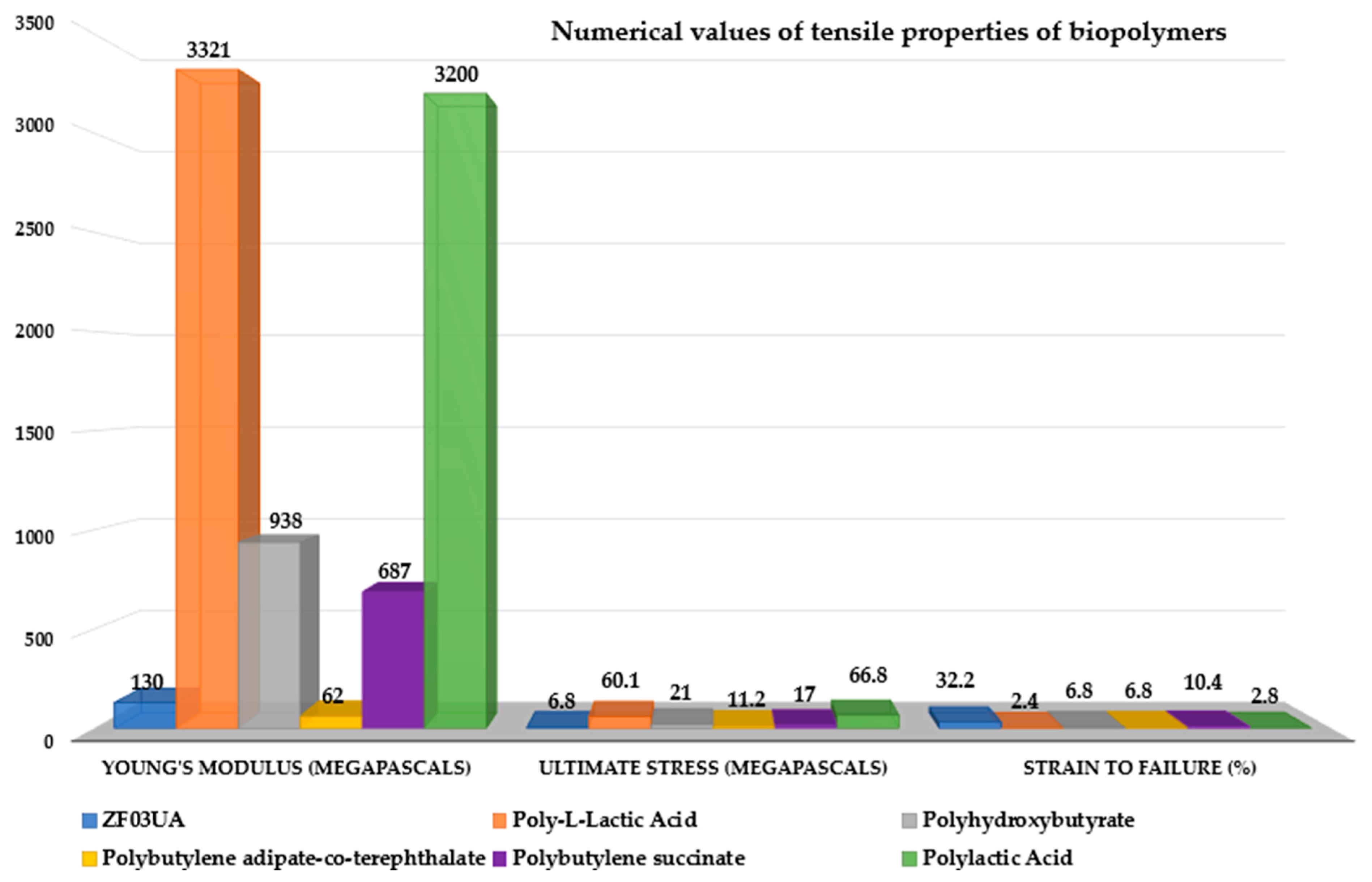
4. Sustainable Construction: Standards, Materials, and Biocomposites
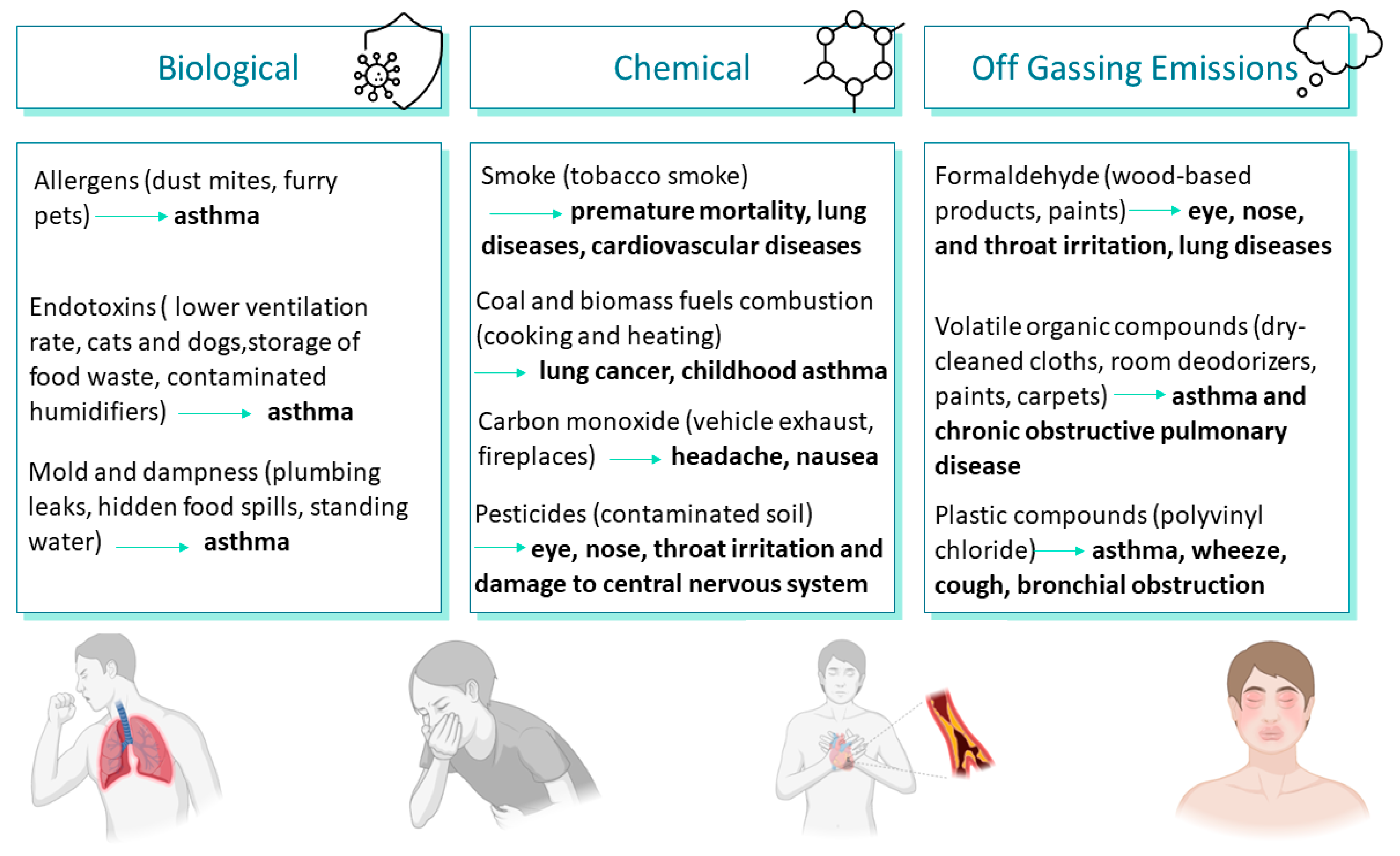
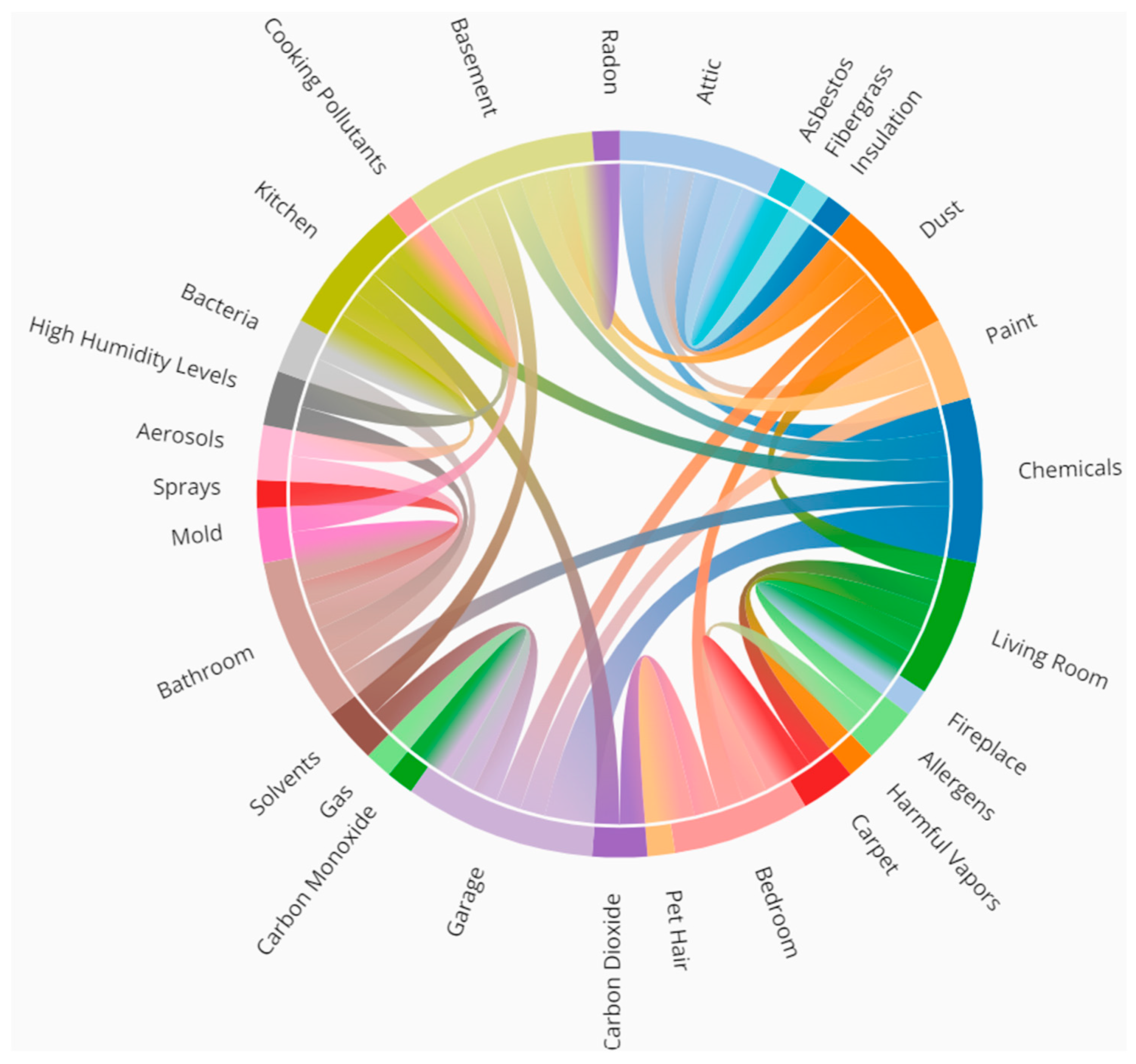
5. Indoor Air Quality Impacting Health Status
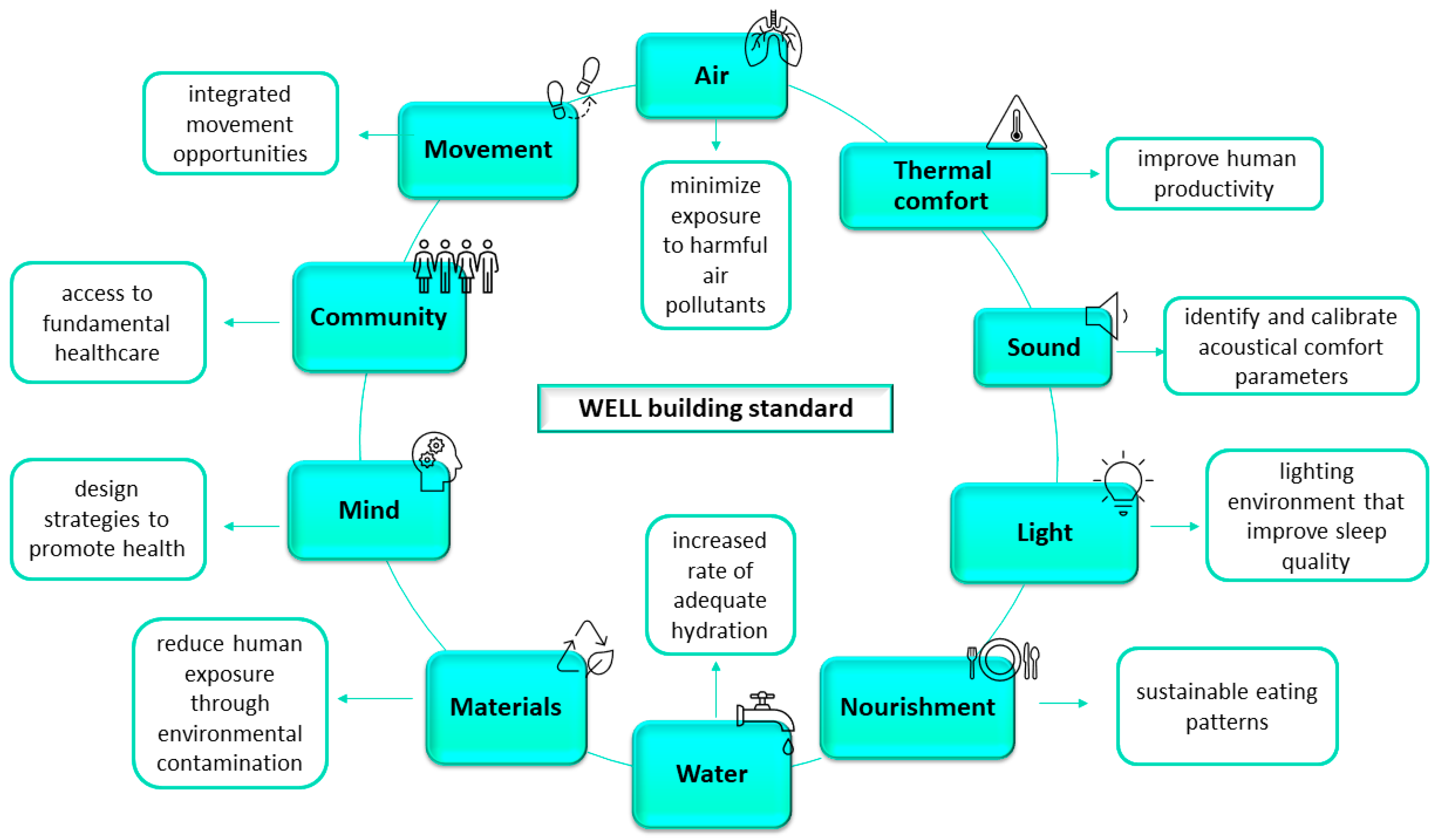
6. Green Buildings’ Importance in Health
7. Technology Transfer in Building Construction and Health
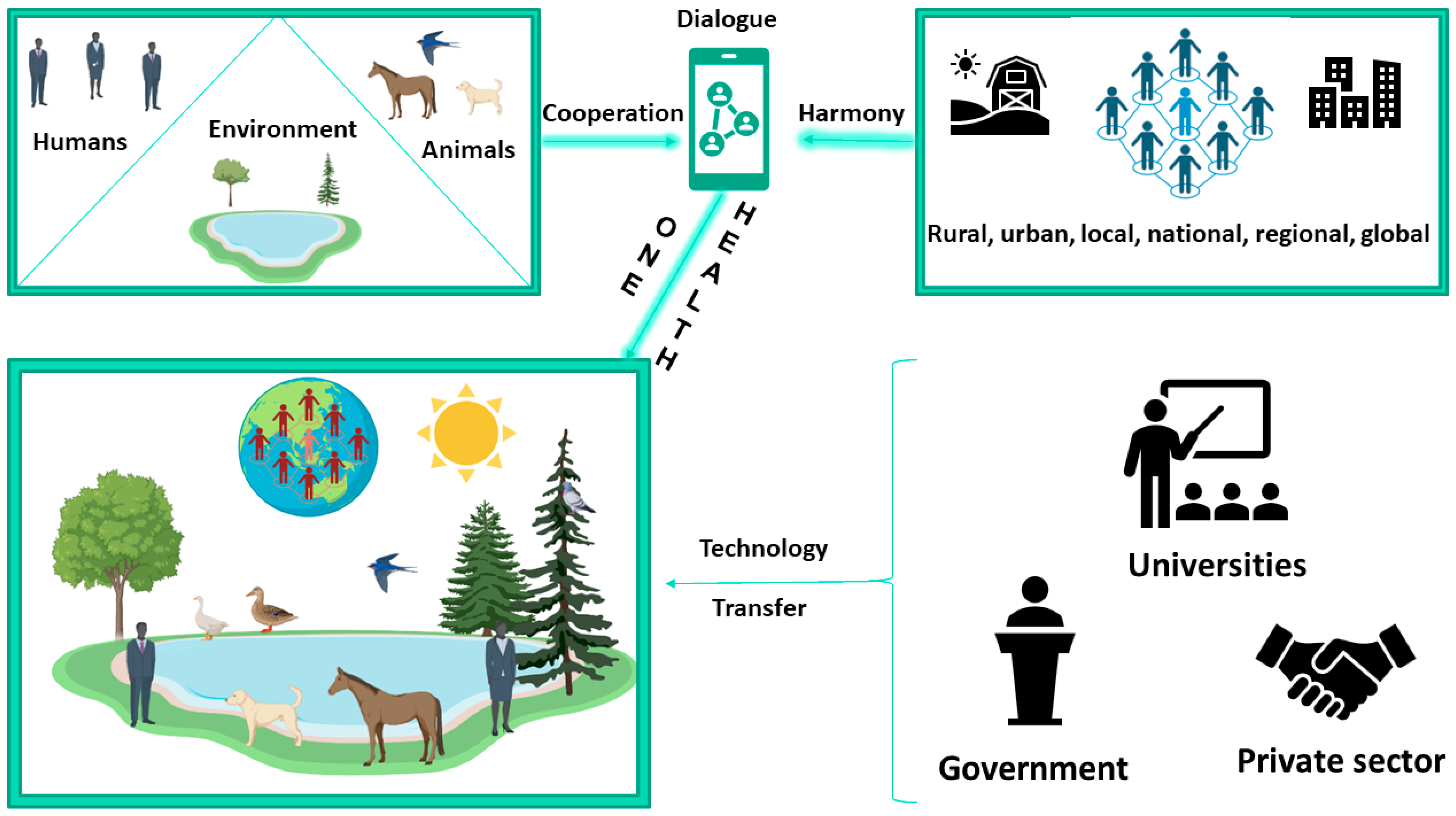
8. The One Health Concept Integrating Green Building into a Larger Context
9. Discussions and Future Perspectives
10. Conclusions
- The link between living conditions and health status implies health risks for residents, especially when building quality standards are not met;
- Poor living conditions are mainly associated with respiratory, cardiovascular, and dermatological diseases;
- Inadequate ventilation, mold, and exposure to contaminants are among the most common items that increase health risks;
- Volatile organic compounds and particulate matter are blamed for altering health status by degrading the indoor air quality;
- Given the novelty of green building concepts and technology transfer implementations in promoting indoor health, additional research is essential to comprehensively grasp the long-term health implications of such practices;
- The imperative for more evidence-based strategies to address housing-related health risks becomes apparent.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shaw, M. Housing and Public Health. Annu. Rev. Public Health 2004, 25, 397–418. [Google Scholar] [CrossRef] [PubMed]
- Krieger, J.; Higgins, D.L. Housing and Health: Time Again for Public Health Action. Am. J. Public Health 2002, 92, 758–768. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, D.E.; Kelly, T.; Sobolewski, J. Linking Public Health, Housing, and Indoor Environmental Policy: Successes and Challenges at Local and Federal Agencies in the United States. Environ. Health Perspect. 2007, 115, 976–982. [Google Scholar] [CrossRef] [PubMed]
- Mannan, M.; Al-Ghamdi, S.G. Indoor Air Quality in Buildings: A Comprehensive Review on the Factors Influencing Air Pollution in Residential and Commercial Structure. Int. J. Environ. Res. Public Health 2021, 18, 3276. [Google Scholar] [CrossRef]
- United States Environmental Protection Agency. What Are the Trends in Indoor Air Quality and Their Effects on Human Health? Available online: https://www.epa.gov/report-environment/indoor-air-quality (accessed on 2 February 2024).
- Van Tran, V.; Park, D.; Lee, Y.C. Indoor Air Pollution, Related Human Diseases, and Recent Trends in the Control and Improvement of Indoor Air Quality. Int. J. Environ. Res. Public Health 2020, 17, 2927. [Google Scholar] [CrossRef] [PubMed]
- Perdue, W.C.; Stone, L.A.; Gostin, L.O. The Built Environment and Its Relationship to the Public’s Health: The Legal Framework. Am. J. Public Health 2003, 93, 1390–1394. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services. The Surgeon General’s Call to Action to Promote Healthy Homes; U.S. Department of Health and Human Services: Washington, DC, USA, 2009.
- Wei, W.; Ramalho, O.; Mandin, C. Indoor Air Quality Requirements in Green Building Certifications. Build. Environ. 2015, 92, 10–19. [Google Scholar] [CrossRef]
- Popescu, D.E.; Prada, M.F.; Dodescu, A.; Hemanth, D.J.; Bungau, C. A Secure Confident Cloud Computing Architecture Solution for a Smart Campus. In Proceedings of the 7th International Conference on Computers Communications and Control, ICCCC, Oradea, Romania, 19 June 2018; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2018; pp. 240–245. [Google Scholar]
- Popescu, D.E.; Bungau, C.; Prada, M.; Domuta, C.; Bungau, S.; Tit, D.M. Waste Management Strategy at a Public University in Smart City Context. J. Environ. Prot. Ecol. 2016, 17, 1011–1020. [Google Scholar]
- Zimmer, A.T.; Ha, H.S. People, Planet and Profit: Unintended Consequences of Legacy Building Materials. J. Environ. Manag. 2017, 204, 472–485. [Google Scholar] [CrossRef]
- Laden, F.; Schwartz, J.; Speizer, F.E.; Dockery, D.W. Reduction in Fine Particulate Air Pollution and Mortality: Extended Follow-up of the Harvard Six Cities Study. Am. J. Respir. Crit. Care Med. 2006, 173, 667–672. [Google Scholar] [CrossRef]
- Allen, J.G.; MacNaughton, P.; Laurent, J.G.C.; Flanigan, S.S.; Eitland, E.S.; Spengler, J.D. Green Buildings and Health. Curr. Environ. Health Rep. 2015, 2, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, 105906. [Google Scholar]
- Bryant-Stephens, T.C.; Strane, D.; Robinson, E.K.; Bhambhani, S.; Kenyon, C.C. Housing and Asthma Disparities. J. Allergy Clin. Immunol. 2021, 148, 1121–1129. [Google Scholar] [CrossRef] [PubMed]
- Jayawardene, W.P.; YoussefAgha, A.H.; Lohrmann, D.K.; El Afandi, G.S. Prediction of Asthma Exacerbations among Children through Integrating Air Pollution, Upper Atmosphere, and School Health Surveillances. Allergy Asthma Proc. 2013, 34, e1–e8. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.M.; Chiang, K.H.; Hung, J.Y.; Chang, W.A.; Lin, H.P.; Shieh, J.M.; Chong, I.W.; Hsu, Y.L. Der F1 Induces Pyroptosis in Human Bronchial Epithelia via the NLRP3 Inflammasome. Int. J. Mol. Med. 2018, 41, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Calderón, M.A.; Linneberg, A.; Kleine-Tebbe, J.; De Blay, F.; Hernandez Fernandez De Rojas, D.; Virchow, J.C.; Demoly, P. Respiratory Allergy Caused by House Dust Mites: What Do We Really Know? J. Allergy Clin. Immunol. 2015, 136, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.Y. The Innate Immune Response in House Dust Mite-Induced Allergic Inflammation. Allergy Asthma Immunol. Res. 2013, 5, 68–74. [Google Scholar] [CrossRef]
- Portnoy, J.; Miller, J.D.; Williams, P.B.; Chew, G.L.; Miller, J.D.; Zaitoun, F.; Phipatanakul, W.; Kennedy, K.; Barnes, C.; Grimes, C.; et al. Environmental Assessment and Exposure Control of Dust Mites: A Practice Parameter. Ann. Allergy Asthma Immunol. 2013, 111, 465–507. [Google Scholar] [CrossRef]
- Weitzman, M.; Baten, A.; Rosenthal, D.G.; Hoshino, R.; Tohn, E.; Jacobs, D.E. Housing and Child Health. Curr. Probl. Pediatr. Adolesc. Health Care 2013, 43, 187–224. [Google Scholar] [CrossRef]
- Wilson, J.; Dixon, S.L.; Breysse, P.; Jacobs, D.; Adamkiewicz, G.; Chew, G.L.; Dearborn, D.; Krieger, J.; Sandel, M.; Spanier, A. Housing and Allergens: A Pooled Analysis of Nine US Studies. Environ. Res. 2010, 110, 189–198. [Google Scholar] [CrossRef]
- Adamkiewicz, G.; Zota, A.R.; Patricia Fabian, M.; Chahine, T.; Julien, R.; Spengler, J.D.; Levy, J.I. Moving Environmental Justice Indoors: Understanding Structural Influences on Residential Exposure Patterns in Low-Income Communities. Am. J. Public Health 2011, 101, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Salo, P.M.; Arbes, S.J.; Crockett, P.W.; Thorne, P.S.; Cohn, R.D.; Zeldin, D.C. Exposure to Multiple Indoor Allergens in US Homes and Its Relationship to Asthma. J. Allergy Clin. Immunol. 2008, 121, 678–684.e2. [Google Scholar] [CrossRef] [PubMed]
- Gaffin, J.M.; Phipatanakul, W. The Role of Indoor Allergens in the Development of Asthma. Curr. Opin. Allergy Clin. Immunol. 2009, 9, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Norback, D.; Wieslander, G.; Nordstrom, K.; Walinder, R. Asthma Symptoms in Relation to Measured Building Dampness in Upper Concrete Floor Construction, and 2-Ethyl-1-Hexanol in Indoor Air. Int. J. Tuberc. Lung Dis. 2000, 4, 1016–1025. [Google Scholar] [PubMed]
- Jaakkola, J.J.K.; Ieromnimon, A.; Jaakkola, M.S. Interior Surface Materials and Asthma in Adults: A Population-Based Incident Case-Control Study. Am. J. Epidemiol. 2006, 164, 742–749. [Google Scholar] [CrossRef] [PubMed]
- Barry, A.C.; Mannino, D.M.; Hopenhayn, C.; Bush, H. Exposure to Indoor Biomass Fuel Pollutants and Asthma Prevalence in Southeastern Kentucky: Results from the Burden of Lung Disease (BOLD) Study. J. Asthma 2010, 47, 735–741. [Google Scholar] [CrossRef] [PubMed]
- Fan, Q.; Nogueira, L.; Yabroff, K.R.; Hussaini, S.M.Q.; Pollack, C.E. Housing and Cancer Care and Outcomes: A Systematic Review. J. Natl. Cancer Inst. 2022, 114, 1601–1618. [Google Scholar] [CrossRef]
- Sidhu, M.K.; Ravindra, K.; Mor, S.; John, S. Household Air Pollution from Various Types of Rural Kitchens and Its Exposure Assessment. Sci. Total Environ. 2017, 586, 419–429. [Google Scholar] [CrossRef]
- Lorenzo-González, M.; Ruano-Ravina, A.; Torres-Durán, M.; Kelsey, K.T.; Provencio, M.; Parente-Lamelas, I.; Leiro-Fernández, V.; Vidal-García, I.; Castro-Añón, O.; Martínez, C.; et al. Lung Cancer and Residential Radon in Never-Smokers: A Pooling Study in the Northwest of Spain. Environ. Res. 2019, 172, 713–718. [Google Scholar] [CrossRef]
- Catelinois, O.; Rogel, A.; Laurier, D.; Billon, S.; Hemon, D.; Verger, P.; Tirmarche, M. Lung Cancer Attributable to Indoor Radon Exposure in France: Impact of the Risk Models and Uncertainty Analysis. Environ. Health Perspect. 2006, 114, 1361–1366. [Google Scholar] [CrossRef]
- Ferrante, D.; Mirabelli, D.; Tunesi, S.; Terracini, B.; Magnani, C. Pleural Mesothelioma and Occupational and Non-Occupational Asbestos Exposure: A Case-Control Study with Quantitative Risk Assessment. Occup. Environ. Med. 2016, 73, 147–153. [Google Scholar] [CrossRef]
- Pyana Kitenge, J.; Kapinga Kayembe, D.; Tshibangu Muamba, M.; Kachil Rubing, H.; De Vos, B.; Van Bouwel, J.; Nemery, B. Malignant Mesothelioma in Sub-Saharan Africa: A Case Report from Lubumbashi, DR Congo. Environ. Res. 2019, 176, 108556. [Google Scholar] [CrossRef]
- Järvholm, B.; Åstrom, E. The Risk of Lung Cancer after Cessation of Asbestos Exposure in Construction Workers Using Pleural Malignant Mesothelioma as a Marker of Exposure. J. Occup. Environ. Med. 2014, 56, 1297–1301. [Google Scholar] [CrossRef]
- Kagan, E. Asbestos-Induced Mesothelioma: Is Fiber Biopersistence Really a Critical Factor? Am. J. Pathol. 2013, 183, 1378–1381. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Agents Classified by the IARC Monographs. Available online: https://monographs.iarc.who.int/agents-classified-by-the-iarc/ (accessed on 5 March 2023).
- Sapkota, A.; Gajalakshmi, V.; Jetly, D.H.; Roychowdhury, S.; Dikshit, R.P.; Brennan, P.; Hashibe, M.; Boffetta, P. Indoor Air Pollution from Solid Fuels and Risk of Hypopharyngeal/Laryngeal and Lung Cancers: A Multicentric Case-Control Study from India. Int. J. Epidemiol. 2008, 37, 321–328. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shankar, A.; Dubey, A.; Saini, D.; Singh, M.; Prasad, C.P.; Roy, S.; Bharati, S.J.; Rinki, M.; Singh, N.; Seth, T.; et al. Environmental and Occupational Determinants of Lung Cancer. Transl. Lung Cancer Res. 2019, 8, S31–S49. [Google Scholar] [CrossRef] [PubMed]
- Järvholm, B.; Englund, A. The Impact of Asbestos Exposure in Swedish Construction Workers. Am. J. Ind. Med. 2014, 57, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Van Deurssen, E.; Pronk, A.; Spaan, S.; Goede, H.; Tielemans, E.; Heederik, D.; Meijster, T. Quartz and Respirable Dust in the Dutch Construction Industry: A Baseline Exposure Assessment as Part of a Multidimensional Intervention Approach. Ann. Occup. Hyg. 2014, 58, 724–738. [Google Scholar] [PubMed]
- Monsó, E.; Riu, E.; Radon, K.; Magarolas, R.; Danuser, B.; Iversen, M.; Morera, J.; Nowak, D. Chronic Obstructive Pulmonary Disease in Never-Smoking Animal Farmers Working inside Confinement Buildings. Am. J. Ind. Med. 2004, 46, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Tavakol, E.; Azari, M.; Zendehdel, R.; Salehpour, S.; Khodakrim, S.; Nikoo, S.; Saranjam, B. Risk Evaluation of Construction Workers’ Exposure to Silica Dust and the Possible Lung Function Impairments. Tanaffos 2017, 16, 295–303. [Google Scholar]
- Rinne, S.T.; Rodas, E.J.; Bender, B.S.; Rinne, M.L.; Simpson, J.M.; Galer-Unti, R.; Glickman, L.T. Relationship of Pulmonary Function among Women and Children to Indoor Air Pollution from Biomass Use in Rural Ecuador. Respir. Med. 2006, 100, 1208–1215. [Google Scholar] [CrossRef]
- Sood, A.; Petersen, H.; Blanchette, C.M.; Meek, P.; Picchi, M.A.; Belinsky, S.A.; Tesfaigzi, Y. Wood Smoke Exposure and Gene Promoter Methylation Are Associated with Increased Risk for COPD in Smokers. Am. J. Respir. Crit. Care Med. 2010, 182, 1098–1104. [Google Scholar] [CrossRef] [PubMed]
- Raju, S.; Keet, C.A.; Paulin, L.M.; Matsui, E.C.; Peng, R.D.; Hansel, N.N.; McCormack, M.C. Rural Residence and Poverty Are Independent Risk Factors for Chronic Obstructive Pulmonary Disease in the United States. Am. J. Respir. Crit. Care Med. 2019, 199, 961–969. [Google Scholar] [CrossRef] [PubMed]
- Wimalasena, N.N.; Chang-Richards, A.; Wang, K.I.-K.; Dirks, K.N. Housing Risk Factors Associated with Respiratory Disease: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 2815. [Google Scholar] [CrossRef] [PubMed]
- Cortes-Ramirez, J.; Wilches-Vega, J.D.; Paris-Pineda, O.M.; Rod, J.E.; Ayurzana, L.; Sly, P.D. Environmental Risk Factors Associated with Respiratory Diseases in Children with Socioeconomic Disadvantage. Heliyon 2021, 7, e06820. [Google Scholar] [CrossRef] [PubMed]
- Addisu, A.; Getahun, T.; Deti, M.; Negesse, Y.; Mekonnen, B. Association of Acute Respiratory Infections with Indoor Air Pollution from Biomass Fuel Exposure among Under-Five Children in Jimma Town, Southwestern Ethiopia. J. Environ. Public Health 2021, 2021, 7112548. [Google Scholar] [CrossRef] [PubMed]
- Forouzanfar, M.H.; Alexander, L.; Bachman, V.F.; Biryukov, S.; Brauer, M.; Casey, D.; Coates, M.M.; Delwiche, K.; Estep, K.; Frostad, J.J.; et al. Global, Regional, and National Comparative Risk Assessment of 79 Behavioural, Environmental and Occupational, and Metabolic Risks or Clusters of Risks in 188 Countries, 1990–2013: A Systematic Analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. [Google Scholar] [CrossRef] [PubMed]
- Dherani, M.; Pope, D.; Mascarenhas, M.; Smith, K.R.; Weber, M.; Bruce, N. Indoor Air Pollution from Unprocessed Solid Fuel Use and Pneumonia Risk in Children Aged under Five Years: A Systematic Review and Meta-Analysis. Bull. World Health Organ. 2008, 86, 390–394. [Google Scholar] [PubMed]
- Klepeis, N.E.; Nelson, W.C.; Ott, W.R.; Robinson, J.P.; Tsang, A.M.; Switzer, P.; Behar, J.V.; Hern, S.C.; Engelmann, W.H. The National Human Activity Pattern Survey (NHAPS): A Resource for Assessing Exposure to Environmental Pollutants. J. Expo. Sci. Environ. Epidemiol. 2001, 11, 231–252. [Google Scholar] [CrossRef]
- Turpin, B.J.; Weisel, C.F.; Morandi, M.; Colome, S.; Stock, T.; Eisenreich, S.; Buckley, B. Relationships of Indoor, Outdoor, and Personal Air (RIOPA): Part II. Analyses of Concentrations of Particulate Matter Species. Res. Rep./HEI 2007, 130, 79–92. [Google Scholar]
- Cesaroni, G.; Forastiere, F.; Stafoggia, M.; Andersen, Z.J.; Badaloni, C.; Beelen, R.; Caracciolo, B.; De Faire, U.; Erbel, R.; Eriksen, K.T.; et al. Long Term Exposure to Ambient Air Pollution and Incidence of Acute Coronary Events: Prospective Cohort Study and Meta-Analysis in 11 European Cohorts from the ESCAPE Project. BMJ 2014, 348, f7412. [Google Scholar] [CrossRef]
- Mccracken, J.; Smith, K.R.; Stone, P.; Díaz, A.; Arana, B.; Schwartz, J. Intervention to Lower Household Wood Smoke Exposure in Guatemala Reduces ST-Segment Depression on Electrocardiograms. Environ. Health Perspect. 2011, 119, 1562–1568. [Google Scholar] [CrossRef]
- Painschab, M.S.; Davila-Roman, V.G.; Gilman, R.H.; Vasquez-Villar, A.D.; Pollard, S.L.; Wise, R.A.; Miranda, J.J.; Checkley, W. Chronic Exposure to Biomass Fuel Is Associated with Increased Carotid Artery Intima-Media Thickness and a Higher Prevalence of Atherosclerotic Plaque. Heart 2013, 99, 984–991. [Google Scholar] [CrossRef]
- Fatmi, Z.; Coggon, D. Coronary Heart Disease and Household Air Pollution from Use of Solid Fuel: A Systematic Review. Br. Med. Bull. 2016, 118, 91–109. [Google Scholar] [CrossRef] [PubMed]
- Nunes, K.V.R.; Ignotti, E.; Hacon, S.D.S. Circulatory Disease Mortality Rates in the Elderly and Exposure to PM(2.5) Generated by Biomass Burning in the Brazilian Amazon in 2005. Cad. Saude Publica 2013, 29, 589–598. [Google Scholar] [CrossRef] [PubMed]
- Karri, V.; Schuhmacher, M.; Kumar, V. Heavy Metals (Pb, Cd, As and MeHg) as Risk Factors for Cognitive Dysfunction: A General Review of Metal Mixture Mechanism in Brain. Environ. Toxicol. Pharmacol. 2016, 48, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Tong, S.; von Schirnding, Y.E.; Prapamontol, T. Environmental Lead Exposure: A Public Health Problem of Global Dimensions. Bull. World Health Organ. 2000, 78, 1068–1077. [Google Scholar] [PubMed]
- Navas-Acien, A.; Guallar, E.; Silbergeld, E.K.; Rothenberg, S.J. Lead Exposure and Cardiovascular Disease-a Systematic Review. Environ. Health Perspect. 2007, 115, 472–482. [Google Scholar] [CrossRef] [PubMed]
- Osorio-Yáñez, C.; Ayllon-Vergara, J.C.; Aguilar-Madrid, G.; Arreola-Mendoza, L.; Hernández-Castellanos, E.; Barrera-Hernández, A.; De Vizcaya-Ruiz, A.; Del Razo, L.M. Carotid Intima-Media Thickness and Plasma Asymmetric Dimethylarginine in Mexican Children Exposed to Inorganic Arsenic. Environ. Health Perspect. 2013, 121, 1090–1096. [Google Scholar] [CrossRef] [PubMed]
- Gold, D.R.; Litonjua, A.; Schwartz, J.; Lovett, E.; Larson, A.; Nearing, B.; Allen, G.; Verrier, M.; Cherry, R.; Verrier, R. Ambient Pollution and Heart Rate Variability. Circulation 2000, 101, 1267–1273. [Google Scholar] [CrossRef] [PubMed]
- Brook, R.D. Why Physicians Who Treat Hypertension Should Know More about Air Pollution. J. Clin. Hypertens. 2007, 9, 629–635. [Google Scholar] [CrossRef] [PubMed]
- Mancebo, S.E.; Wang, S.Q. Recognizing the Impact of Ambient Air Pollution on Skin Health. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 2326–2332. [Google Scholar] [CrossRef] [PubMed]
- Vierkötter, A.; Schikowski, T.; Ranft, U.; Sugiri, D.; Matsui, M.; Krämer, U.; Krutmann, J. Airborne Particle Exposure and Extrinsic Skin Aging. J. Investig. Dermatol. 2010, 130, 2719–2726. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Jiang, P.; Chen, J.; Zhu, C.; Mao, Z.; Gao, C. Application of Melatonin-Loaded Poly(N-Isopropylacrylamide) Hydrogel Particles to Reduce the Toxicity of Airborne Pollutes to RAW264.7 Cells. J. Colloid Interface Sci. 2017, 490, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Parrado, C.; Mercado-Saenz, S.; Perez-Davo, A.; Gilaberte, Y.; Gonzalez, S.; Juarranz, A. Environmental Stressors on Skin Aging. Mechanistic Insights. Front. Pharmacol. 2019, 10, 759. [Google Scholar] [CrossRef] [PubMed]
- U.S Department of State. Stockholm Convention on Persistent Organic Pollutants. Available online: https://www.state.gov/key-topics-office-of-environmental-quality-and-transboundary-issues/stockholm-convention-on-persistent-organic-pollutants/ (accessed on 5 March 2023).
- Froehner, S.; Rizzi, J.; Vieira, L.M.; Sanez, J. PAHs in Water, Sediment and Biota in an Area with Port Activities. Arch. Environ. Contam. Toxicol. 2018, 75, 236–246. [Google Scholar] [CrossRef]
- Tsuji, G.; Takahara, M.; Uchi, H.; Takeuchi, S.; Mitoma, C.; Moroi, Y.; Furue, M. An Environmental Contaminant, Benzo(a)Pyrene, Induces Oxidative Stress-Mediated Interleukin-8 Production in Human Keratinocytes via the Aryl Hydrocarbon Receptor Signaling Pathway. J. Dermatol. Sci. 2011, 62, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Turner, S.; Cherry, N. Rheumatoid Arthritis in Workers Exposed to Silica in the Pottery Industry. Occup. Environ. Med. 2000, 57, 443–477. [Google Scholar] [CrossRef] [PubMed]
- Reckner Olsson, Å.; Skogh, T.; Axelson, O.; Wingren, G. Occupations and Exposures in the Work Environment as Determinants for Rheumatoid Arthritis. Occup. Environ. Med. 2004, 61, 233–238. [Google Scholar] [CrossRef]
- Lundberg, I.; Alfredsson, L.; Plato, N.; Sverdrup, B.; Klareskog, L.; Kleinau, S. Occupation, Occupational Exposure to Chemicals and Rheumatological Disease. A Register Based Cohort Study. Scand. J. Rheumatol. 1994, 23, 305–310. [Google Scholar] [CrossRef]
- Koureas, M.; Rachiotis, G.; Tsakalof, A.; Hadjichristodoulou, C. Increased Frequency of Rheumatoid Arthritis and Allergic Rhinitis among Pesticide Sprayers and Associations with Pesticide Use. Int. J. Environ. Res. Public Health 2017, 14, 865. [Google Scholar] [CrossRef]
- Sverdrup, B.; Källberg, H.; Bengtsson, C.; Lundberg, I.; Padyukov, L.; Alfredsson, L.; Klareskog, L. Association between Occupational Exposure to Mineral Oil and Rheumatoid Arthritis: Results from the Swedish EIRA Case-Control Study. Arthritis Res. Ther. 2005, 7, 1296–1303. [Google Scholar] [CrossRef]
- WHO Housing and Health Guidelines. Available online: https://www.who.int/publications/i/item/9789241550376 (accessed on 3 February 2024).
- Lima, V. Pandemic Housing Policies: Mitigation Strategies and Protection of Rights. Hous. Soc. 2024, 51, 34–49. [Google Scholar] [CrossRef]
- Luo, W.; Baldwin, E.; Jiang, A.Y.; Li, S.; Yang, B.; Li, H. Effects of Housing Environments on COVID-19 Transmission and Mental Health Revealed by COVID-19 Participant Experience Data from the All of Us Research Program in the USA: A Case-Control Study. BMJ Open 2022, 12, e063714. [Google Scholar] [CrossRef] [PubMed]
- Keller, A.; Groot, J.; Matta, J.; Bu, F.; El Aarbaoui, T.; Melchior, M.; Fancourt, D.; Zins, M.; Goldberg, M.; Nybo Andersen, A.M.; et al. Housing Environment and Mental Health of Europeans during the COVID-19 Pandemic: A Cross-Country Comparison. Sci. Rep. 2022, 12, 5612. [Google Scholar] [CrossRef] [PubMed]
- Amerio, A.; Brambilla, A.; Morganti, A.; Aguglia, A.; Bianchi, D.; Santi, F.; Costantini, L.; Odone, A.; Costanza, A.; Signorelli, C.; et al. COVID-19 Lockdown: Housing Built Environment’s Effects on Mental Health. Int. J. Environ. Res. Public Health 2020, 17, 5973. [Google Scholar] [CrossRef] [PubMed]
- Dubey, S.; Sahoo, K.C.; Dash, G.C.; Sahay, M.R.; Mahapatra, P.; Bhattacharya, D.; Del Barrio, M.O.; Pati, S. Housing-Related Challenges during COVID-19 Pandemic among Urban Poor in Low- and Middle-Income Countries: A Systematic Review and Gap Analysis. Front. Public Health 2022, 10, 1029394. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, K.; Erqou, S.; Shah, N.; Nazir, U.; Morrison, A.R.; Choudhary, G.; Wu, W.-C. Association of Poor Housing Conditions with COVID-19 Incidence and Mortality across US Counties. PLoS ONE 2020, 15, e0241327. [Google Scholar] [CrossRef] [PubMed]
- United States Environmental Protection Agency. Indoor Air Quality. Sick Building Syndrome Fact Sheet Indoor Air Facts No. 4. Available online: https://www.epa.gov/indoor-air-quality-iaq (accessed on 5 March 2023).
- Kipen, H.M.; Fiedler, N. Environmental Factors in Medically Unexplained Symptoms and Related Syndromes: The Evidence and the Challenge. Environ. Health Perspect. 2002, 110, 597–599. [Google Scholar] [CrossRef] [PubMed]
- Quoc, C.H.; Huong, G.V.; Duc, H.N. Working Conditions and Sick Building Syndrome among Health Care Workers in Vietnam. Int. J. Environ. Res. Public Health 2020, 17, 3635. [Google Scholar] [CrossRef]
- Sayan, H.E.; Dülger, S. Evaluation of the Relationship between Sick Building Syndrome Complaints among Hospital Employees and Indoor Environmental Quality. Med. Lav. 2021, 112, 153–161. [Google Scholar] [PubMed]
- Smajlović, S.K.; Kukec, A.; Dovjak, M. Association between Sick Building Syndrome and Indoor Environmental Quality in Slovenian Hospitals: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 3224. [Google Scholar] [CrossRef] [PubMed]
- Vafaeenasab, M.R.; Morowatisharifabad, M.A.; Taghi Ghaneian, M.; Hajhosseini, M.; Ehrampoush, M.H. Assessment of Sick Building Syndrome and Its Associating Factors among Nurses in the Educational Hospitals of Shahid Sadoughi University of Medical Sciences, Yazd, Iran. Glob. J. Health Sci. 2014, 7, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Salvaraji, L.; Shamsudin, S.B.; Avoi, R.; Saupin, S.; Kim Sai, L.; Asan, S.B.; Toha, H.R.B.; Jeffree, M.S. Ecological Study of Sick Building Syndrome among Healthcare Workers at Johor Primary Care Facilities. Int. J. Environ. Res. Public Health 2022, 19, 17099. [Google Scholar] [CrossRef] [PubMed]
- Naldzhiev, D.; Mumovic, D.; Strlic, M. Polyurethane Insulation and Household Products—A Systematic Review of Their Impact on Indoor Environmental Quality. Build. Environ. 2020, 169, 106559. [Google Scholar] [CrossRef]
- Little, J.C.; Hodgson, A.T.; Gadgil, A.J. Modeling Emissions of Volatile Organic Compounds from New Carpets. Atmos. Environ. 1994, 28, 227–234. [Google Scholar] [CrossRef]
- Woolrich, P.F. Toxicology, Industrial Hygiene and Medical Control of TDI, MDI and PMPPI. Am. Ind. Hyg. Assoc. J. 1982, 43, 89–97. [Google Scholar] [CrossRef]
- Fengamo, D.; Wong, L.N.; Hanley, V.; Gress, J.; Schnell, J. Summary of Technical Information and Scientific Conclusions for Designating Spray Polyurethane Foam Systems with Unreacted Methylene Diphenyl Diisocyanates as a Priority Product. Available online: https://assets.contentstack.io/v3/assets/blt5775cc69c999c255/blt9747bcbe74d82e57/170324-technical-report.pdf (accessed on 10 May 2023).
- Chang, Y.H.; Huang, P.H.; Wu, B.Y.; Chang, S.W. A Study on the Color Change Benefits of Sustainable Green Building Materials. Constr. Build. Mater. 2015, 83, 1–6. [Google Scholar] [CrossRef]
- Khovalyg, D.; Kazanci, O.B.; Halvorsen, H.; Gundlach, I.; Bahnfleth, W.P.; Toftum, J.; Olesen, B.W. Critical Review of Standards for Indoor Thermal Environment and Air Quality. Energy Build. 2020, 213, 109819. [Google Scholar] [CrossRef]
- Loftness, V.; Hakkinen, B.; Adan, O.; Nevalainen, A. Elements That Contribute to Healthy Building Design. Environ. Health Perspect. 2007, 115, 965–970. [Google Scholar] [CrossRef]
- de Dear, R.J.; Brager, G.S. Thermal Comfort in Naturally Ventilated Buildings: Revisions to ASHRAE Standard 55. Energy Build. 2002, 34, 549–561. [Google Scholar] [CrossRef]
- ANSI/ASHRAE Addendum d to ANSI/ASHRAE Standard 55-2017. Thermal Environmental Conditions for Human Occupancy. Available online: https://www.ashrae.org/file library/technical resources/standards and guidelines/standards addenda/55_2017_d_20200731.pdf (accessed on 1 February 2024).
- Joshi, S. The Sick Building Syndrome. Indian J. Occup. Environ. Med. 2008, 12, 61–64. [Google Scholar] [CrossRef]
- Wang, Z.; de Dear, R.; Luo, M.; Lin, B.; He, Y.; Ghahramani, A.; Zhu, Y. Individual Difference in Thermal Comfort: A Literature Review. Build. Environ. 2018, 138, 181–193. [Google Scholar] [CrossRef]
- Kramer, T.; Garcia-Hansen, V.; Omrani, S.; Zhou, J.; Chen, D. Personal Differences in Thermal Comfort Perception: Observations from a Field Study in Brisbane, Australia. Build. Environ. 2023, 245, 110873. [Google Scholar] [CrossRef]
- Huang, L.; Fantke, P.; Ritscher, A.; Jolliet, O. Chemicals of Concern in Building Materials: A High-Throughput Screening. J. Hazard. Mater. 2022, 424, 127574. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.B.; Joseph, R. Eco-Friendly Bio-Composites Using Natural Rubber (NR) Matrices and Natural Fiber Reinforcements. In Chemistry, Manufacture and Applications of Natural Rubber; Woodhead Publishing: Sawston, UK, 2014; pp. 249–283. ISBN 9780857096838. [Google Scholar]
- Ramsay, B.A.; Lomaliza, K.; Chavarie, C.; Dube, B.; Bataille, P.; Ramsay, J.A. Production of Poly-(Beta-Hydroxybutyric-Co-Beta-Hydroxyvaleric) Acids. Appl. Environ. Microbiol. 1990, 56, 2093–2098. [Google Scholar] [CrossRef] [PubMed]
- Hodzic, A. Properties of Poly(3-Hydroxybutyric Acid) Composites with Flax Fibres Modified by Plasticiser Absorption. Macromol. Mater. Eng. 2002, 287, 647–655. [Google Scholar]
- Mohanty, A.K.; Wibowo, A.; Misra, M.; Drzal, L.T. Effect of Process Engineering on the Performance of Natural Fiber Reinforced Cellulose Acetate Biocomposites. Compos. Part A Appl. Sci. Manuf. 2004, 35, 363–370. [Google Scholar] [CrossRef]
- Bodros, E.; Pillin, I.; Montrelay, N.; Baley, C. Could Biopolymers Reinforced by Randomly Scattered Flax Fibre Be Used in Structural Applications? Compos. Sci. Technol. 2007, 67, 462–470. [Google Scholar] [CrossRef]
- Mohanty, A.K.; Khan, M.A.; Hinrichsen, G. Surface Modification of Jute and Its Influence on Performance of Biodegradable Jute-Fabric/Biopol Composites. Compos. Sci. Technol. 2000, 60, 1115–1124. [Google Scholar] [CrossRef]
- Donnet, J.B.; Bahl, O.P.; Bansal, R.C.; Wang, T.K. Carbon Fibers. In Encyclopedia of Physical Science and Technology, 3rd ed.; Meyers, R.A., Ed.; Academic Press: New York, NY, USA, 2003; pp. 431–455. ISBN 978-0-12-227410-7. [Google Scholar]
- Burla, F.; Mulla, Y.; Vos, B.; Aufderhorst-Roberts, A.; Koenderink, G. From Mechanical Resilience to Active Material Properties in Biopolymer Networks. Nat. Rev. Phys. 2019, 1, 249–263. [Google Scholar] [CrossRef]
- Jung, G.; Qin, Z.; Buehler, M.J. Mechanical Properties and Failure of Biopolymers: Atomistic Reactions to Macroscale Response. Top. Curr. Chem. 2015, 369, 317–343. [Google Scholar] [PubMed]
- Roig, I. Biocomposites for Interior Facades and Partitions to Improve Air Quality in New Buildings and Restorations. Reinf. Plast. 2018, 62, 270–274. [Google Scholar] [CrossRef]
- Leech, J.A.; Nelson, W.C.; Burnett, R.T.; Aaron, S.; Raizenne, M.E. It’s about Time: A Comparison of Canadian and American Time-Activity Patterns. J. Expo. Anal. Environ. Epidemiol. 2002, 12, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Cincinelli, A.; Martellini, T. Indoor Air Quality and Health. Int. J. Environ. Res. Public Health 2017, 14, 1286. [Google Scholar] [CrossRef]
- Dales, R.; Liu, L.; Wheeler, A.J.; Gilbert, N.L. Quality of Indoor Residential Air and Health. CMAJ 2008, 179, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Spiegelman, D.L.; Burge, H.A.; Gold, D.R.; Chew, G.L.; Milton, D.K. Longitudinal Study of Dust and Airborne Endotoxin in the Home. Environ. Health Perspect. 2000, 108, 1023–1028. [Google Scholar] [CrossRef]
- Fisk, W.J.; Lei-Gomez, Q.; Mendell, M.J. Meta-Analyses of the Associations of Respiratory Health Effects with Dampness and Mold in Homes. Indoor Air 2007, 17, 284–296. [Google Scholar] [CrossRef]
- Zhang, J.J.; Smith, K.R. Household Air Pollution from Coal and Biomass Fuels in China: Measurements, Health Impacts, and Interventions. Environ. Health Perspect. 2007, 115, 848–855. [Google Scholar] [CrossRef]
- Liu, K.S.; Paz, M.K.; Flessel, P.; Waldman, J.; Girman, J. Unintentional Carbon Monoxide Deaths in California from Residential and Other Nonvehicular Sources. Arch. Environ. Health 2000, 55, 375–381. [Google Scholar] [CrossRef]
- Jaakkola, J.J.; Verkasalo, P.K.; Jaakkola, N. Plastic Wall Materials in the Home and Respiratory Health in Young Children. Am. J. Public Health 2000, 90, 797–799. [Google Scholar] [PubMed]
- Ryan, P.H.; Brokamp, C.; Fan, Z.H.; Rao, M.B. Analysis of Personal and Home Characteristics Associated with the Elemental Composition of PM2.5 in Indoor, Outdoor, and Personal Air in the RIOPA Study. Res. Rep. 2015, 185, 3–40. [Google Scholar]
- Macneill, M.; Kearney, J.; Wallace, L.; Gibson, M.; Héroux, M.E.; Kuchta, J.; Guernsey, J.R.; Wheeler, A.J. Quantifying the Contribution of Ambient and Indoor-Generated Fine Particles to Indoor Air in Residential Environments. Indoor Air 2014, 24, 362–375. [Google Scholar] [CrossRef] [PubMed]
- Weichenthal, S.; Dufresne, A.; Infante-Rivard, C.; Joseph, L. Indoor Ultrafine Particle Exposures and Home Heating Systems: A Cross-Sectional Survey of Canadian Homes during the Winter Months. J. Expo. Sci. Environ. Epidemiol. 2007, 17, 288–297. [Google Scholar] [CrossRef] [PubMed]
- McCormack, M.C.; Breysse, P.N.; Matsui, E.C.; Hansel, N.N.; Peng, R.D.; Curtin-Brosnan, J.; Williams, D.L.; Wills-Karp, M.; Diette, G.B. Indoor Particulate Matter Increases Asthma Morbidity in Children with Non-Atopic and Atopic Asthma. Ann. Allergy Asthma Immunol. 2011, 106, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Saborit, J.M.; Aquilina, N.J.; Meddings, C.; Baker, S.; Harrison, R.M. Relationship of Personal Exposure to Volatile Organic Compounds to Home, Work and Fixed Site Outdoor Concentrations. Sci. Total Environ. 2011, 409, 478–488. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Lee, H.S.; Park, M.R.; Lee, S.W.; Kim, E.H.; Cho, J.B.; Kim, J.; Han, Y.; Jung, K.; Cheong, H.K.; et al. Relationship between Indoor Air Pollutant Levels and Residential Environment in Children with Atopic Dermatitis. Allergy Asthma Immunol. Res. 2014, 6, 517–524. [Google Scholar] [CrossRef]
- Saini, J.; Dutta, M.; Marques, G. Indoor Air Pollution: A Comprehensive Review of Public Health Challenges and Prevention Policies. In Intelligent Data-Centric Systems; Marques, G., Ighalo, J.O., Eds.; Academic Press: Cambridge, MA, USA, 2022; pp. 105–126. ISBN 978-0-323-85597-6. [Google Scholar]
- Rumchev, K.; Spickett, J.; Bulsara, M.; Phillips, M.; Stick, S. Association of Domestic Exposure to Volatile Organic Compounds with Asthma in Young Children. Thorax 2004, 59, 746–751. [Google Scholar] [CrossRef]
- Polyzois, D.; Polyzoi, E.; Wells, J.A.; Koulis, T. Poor Indoor Air Quality, Mold Exposure, and Upper Respiratory Tract Infections-Are We Placing Our Children at Risk? J. Environ. Health 2016, 78, 20–27. [Google Scholar]
- Weinmayr, G.; Gehring, U.; Genuneit, J.; Büchele, G.; Kleiner, A.; Siebers, R.; Wickens, K.; Crane, J.; Brunekreef, B.; Strachan, D.P. Dampness and Moulds in Relation to Respiratory and Allergic Symptoms in Children: Results from Phase Two of the International Study of Asthma and Allergies in Childhood (ISAAC Phase Two). Clin. Exp. Allergy 2013, 43, 762–774. [Google Scholar] [CrossRef]
- Yu, B.F.; Hu, Z.B.; Liu, M.; Yang, H.L.; Kong, Q.X.; Liu, Y.H. Review of Research on Air-Conditioning Systems and Indoor Air Quality Control for Human Health. Int. J. Refrig. 2009, 32, 3–20. [Google Scholar] [CrossRef]
- Seppänen, O.A.; Fisk, W.J. Summary of Human Responses to Ventilation. Indoor Air 2004, 14 (Suppl. S7), 102–118. [Google Scholar] [CrossRef]
- Bungau, C.C.; Bungau, T.; Prada, I.F.; Prada, M.F. Green Buildings as a Necessity for Sustainable Environment Development: Dilemmas and Challenges. Sustainability 2022, 14, 13121. [Google Scholar] [CrossRef]
- Dovjak, D.M.; Kukec, A.P.A. Health Outcomes Related to Built Environments. In Creating Healthy and Sustainable Buildings; Springer: Berlin/Heidelberg, Germany, 2019; pp. 43–74. [Google Scholar]
- Wagner, A.; O’Brien, W.; Dong, B. Exploring Occupant Behavior in Buildings: Methods and Challenges; Springer: Berlin/Heidelberg, Germany, 2017. [Google Scholar]
- Prada, M.; Prada, I.F.; Cristea, M.; Popescu, D.E.; Bungău, C.; Aleya, L.; Bungău, C.C. New Solutions to Reduce Greenhouse Gas Emissions through Energy Efficiency of Buildings of Special Importance—Hospitals. Sci. Total Environ. 2020, 718, 137446. [Google Scholar] [CrossRef]
- Bungau, C.C.; Bungau, C.; Toadere, M.T.; Prada-Hanga, I.F.; Bungau, T.; Popescu, D.E.; Prada, M.F. Solutions for an Ecological and Healthy Retrofitting of Buildings on the Campus of the University of Oradea, Romania, Built Starting from 1911 to 1913. Sustainability 2023, 15, 6541. [Google Scholar] [CrossRef]
- Popescu, D.E.; Prada, M. Some Aspects about Smart Building Management Systems—Solutions for Green, Secure and Smart Buildings. In Proceedings of the Recent Advances in Environmental Science, Lemesos, Cyprus, 21–23 March 2013; pp. 126–132. [Google Scholar]
- Terzopoulou, Z.N.; Papageorgiou, G.Z.; Papadopoulou, E.; Athanassiadou, E.; Alexopoulou, E.; Bikiaris, D.N. Green Composites Prepared from Aliphatic Polyesters and Bast Fibers. Ind. Crops Prod. 2015, 68, 60–79. [Google Scholar] [CrossRef]
- Saba, N.; Jawaid, M.; Sultan, M.T.H.; Alothman, O.Y. Green Biocomposites for Structural Applications. In Green Biocomposites Design and Applications; Springer: Berlin/Heidelberg, Germany, 2017; pp. 1–27. [Google Scholar]
- Fowler, P.A.; Hughes, J.M.; Elias, R.M. Biocomposites: Technology, Environmental Credentials and Market Forces. J. Sci. Food Agric. 2006, 86, 1781–1789. [Google Scholar] [CrossRef]
- Khoshnava, S.M.; Rostami, R.; Zin, R.M.; Štreimikienė, D.; Mardani, A.; Ismail, M. The Role of Green Building Materials in Reducing Environmental and Human Health Impacts. Int. J. Environ. Res. Public Health 2020, 17, 2589. [Google Scholar] [CrossRef] [PubMed]
- Green Building Performance: A Post Occupancy Evaluation of 22 GSA Buildings. Available online: https://searchworks.stanford.edu/view/13580863 (accessed on 6 March 2023).
- LEED 2009 for New Construction and Major Renovations. Available online: https://energy.nv.gov/uploadedFiles/energynvgov/content/2009_NewConstruction.pdf (accessed on 6 March 2023).
- McArthur, J.J.; Powell, C. Health and Wellness in Commercial Buildings: Systematic Review of Sustainable Building Rating Systems and Alignment with Contemporary Research. Build. Environ. 2020, 171, 106635. [Google Scholar] [CrossRef]
- WELL Building Standard® V1. Available online: https://www.wellcertified.com/certification/v1/standard/ (accessed on 24 April 2023).
- WELL v2 Overview. Available online: https://v2.wellcertified.com/en/wellv2/overview (accessed on 24 April 2023).
- Marberry, S.O.; Guenther, R.; Berry, L.L. Advancing Human Health, Safety, and Well-Being with Healthy Buildings. J. Hosp. Manag. Health Policy 2021, 6, 18. [Google Scholar] [CrossRef]
- U.S. Environmental Protection Agency. Green Building: Components of Green Building. Available online: https://archive.epa.gov/greenbuilding/web/html/components.html (accessed on 6 March 2023).
- Malenbaum, S.; Keefe, F.J.; Williams, A.C.D.C.; Ulrich, R.; Somers, T.J. Pain in Its Environmental Context: Implications for Designing Environments to Enhance Pain Control. Pain 2008, 134, 241–244. [Google Scholar] [CrossRef]
- BaHammam, A. Sleep in Acute Care Units. Sleep Breath. 2006, 10, 6–15. [Google Scholar] [CrossRef]
- National Institute for Health Research. Getting Hospital Patients Up and Moving Shortens Stay and Improves Fitness. Available online: https://evidence.nihr.ac.uk/alert/getting-hospital-patients-up-and-moving-shortens-stay-and-improves-fitness/ (accessed on 6 March 2023).
- Ulrich, R.S.; Zimring, C.; Zhu, X.; DuBose, J.; Seo, H.B.; Choi, Y.S.; Quan, X.; Joseph, A. A Review of the Research Literature on Evidence-Based Healthcare Design. HERD 2008, 1, 61–125. [Google Scholar] [CrossRef] [PubMed]
- The Center for Health Design. Achieving EBD Goals through Flooring Selection & Design. Available online: https://www.healthdesign.org/chd/research/achieving-ebd-goals-through-flooring-selection-design (accessed on 6 March 2023).
- Case Study: Lucile Packard Children’s Hospital Stanford A Sustainable, Technologically Innovative, and Family-Focused Children’s Healthcare Center. Available online: https://www.usgbc.org/resources/case-study-lucile-packard-childrens-hospital-stanford (accessed on 7 March 2023).
- Growing Green Rating Systems in Healthcare Design. Available online: https://healthcaredesignmagazine.com/trends/growing-green/ (accessed on 7 March 2023).
- MacNaughton, P.; Satish, U.; Laurent, J.G.C.; Flanigan, S.; Vallarino, J.; Coull, B.; Spengler, J.D.; Allen, J.G. The Impact of Working in a Green Certified Building on Cognitive Function and Health. Build. Environ. 2017, 114, 178–186. [Google Scholar] [CrossRef]
- Arens, E.; Humphreys, M.A.; de Dear, R.; Zhang, H. Are ‘Class A’ Temperature Requirements Realistic or Desirable? Build. Environ. 2010, 45, 4–10. [Google Scholar] [CrossRef]
- Craiut, L.; Bungau, C.; Negru, P.A.; Bungau, T.; Radu, A.-F. Technology Transfer in the Context of Sustainable Development-A Bibliometric Analysis of Publications in the Field. Sustainability 2022, 14, 11973. [Google Scholar] [CrossRef]
- Craiut, L.; Bungau, C.; Bungau, T.; Grava, C.; Otrisal, P.; Radu, A.F. Technology Transfer, Sustainability, and Development, Worldwide and in Romania. Sustainability 2022, 14, 15728. [Google Scholar] [CrossRef]
- Technology Transfer and Innovation for Low-Carbon Development. Available online: https://www.worldbank.org/en/topic/macroeconomics/publication/technology-transfer-and-innovation-for-low-carbon-development (accessed on 7 March 2023).
- Gallini, N.T.; Wright, B.D. Technology Transfer under Asymmetric Information. RAND J. Econ. 1990, 21, 147–160. [Google Scholar] [CrossRef]
- Ockwell, D.G.; Mallett, A. Introduction: Low-Carbon Technology Transfer—From Rhetoric to Reality. In Low-Carbon Technology Transfer: From Rhetoric to Reality; Routledge: London, UK, 2012; pp. 1–20. ISBN 978-1-84971-269-9. [Google Scholar]
- Shang, Y.; Lyu, G.; Mi, Z. Green Technology Transfer, Environmental Regulation, and Regional Green Development Chasm: Based on the Empirical Evidence from Yangtze River Delta. Int. J. Environ. Res. Public Health 2022, 19, 13925. [Google Scholar] [CrossRef]
- Jolliet, O.; Ernstoff, A.S.; Csiszar, S.A.; Fantke, P. Defining Product Intake Fraction to Quantify and Compare Exposure to Consumer Products. Environ. Sci. Technol. 2015, 49, 8924–8931. [Google Scholar] [CrossRef]
- MacDonald, S.; Connors, B.F.; Myatt, T.; Allen, J.G. Beyond Traditional Biosafety. Appl. Biosaf. 2013, 18, 138–141. [Google Scholar] [CrossRef]
- Schroeder, H. Demolition, Recycling, and Disposal of Earth Building Materials. In Sustainable Building with Earth; Springer: Cham, Switzerland, 2016; pp. 505–526. [Google Scholar]
- Deng, B.; Tang, S.; Kim, J.T.; Kim, C.N. Numerical Modeling of Volatile Organic Compound Emissions from Multi-Layer Dry Building Materials. Korean J. Chem. Eng. 2010, 27, 1049–1055. [Google Scholar] [CrossRef]
- Yuan, H.; Little, J.C.; Marand, E.; Liu, Z. Using Fugacity to Predict Volatile Emissions from Layered Materials with a Clay/Polymer Diffusion Barrier. Atmos. Environ. 2007, 41, 9300–9308. [Google Scholar] [CrossRef]
- Mielke, H.W.; Gonzales, C. Mercury (Hg) and Lead (Pb) in Interior and Exterior New Orleans House Paint Films. Chemosphere 2008, 72, 882–885. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.J.B.D.; Gebreyes, W.A. One Health: Connecting Environmental, Social and Corporate Governance (ESG) Practices for a Better World. One Health 2022, 15, 100435. [Google Scholar] [CrossRef] [PubMed]
- The Impact of Healthy Buildings. Available online: https://www.hsph.harvard.edu/healthybuildings/overview/ (accessed on 7 March 2023).
- Designing for Human Health Is the Next Frontier in Sustainable Building. Available online: https://www.usgbc.org/articles/designing-human-health-next-frontier-sustainable-building (accessed on 6 March 2023).
- LEED Rating System. Available online: https://www.usgbc.org/leed (accessed on 8 March 2023).
- Green Buildings and Human Health. Available online: https://blogs.cdc.gov/niosh-science-blog/2013/06/10/green-buildings/ (accessed on 8 March 2023).
- Healthy Buildings, Healthier People. Available online: https://www.env-health.org/wp-content/uploads/2018/05/Healthy-Buildings-Briefing.pdf (accessed on 8 March 2023).
- Adisasmito, W.B.; Almuhairi, S.; Behravesh, C.B.; Bilivogui, P.; Bukachi, S.A.; Casas, N.; Becerra, N.C.; Charron, D.F.; Chaudhary, A.; Ciacci Zanella, J.R.; et al. One Health: A New Definition for a Sustainable and Healthy Future. PLoS Pathog. 2022, 18, e1010537. [Google Scholar]
- Zhang, R. Warming Boosts Air Pollution. Nat. Clim. Chang. 2017, 7, 238–239. [Google Scholar] [CrossRef]
- Zhang, R.; Tang, X.; Liu, J.; Visbeck, M.; Guo, H.; Murray, V.; Mcgillycuddy, C.; Ke, B.; Kalonji, G.; Zhai, P.; et al. From Concept to Action: A United, Holistic and One Health Approach to Respond to the Climate Change Crisis. Infect. Dis. Poverty 2022, 11, 17. [Google Scholar] [CrossRef]
- The Surgeon General’s Call to Action to Promote Healthy Homes. The Connection between Health and Homes. Available online: https://www.ncbi.nlm.nih.gov/books/NBK44199/ (accessed on 1 February 2024).

| Building Items | Construction Materials—Substances | Adverse Health Effects |
|---|---|---|
| Adhesives | Silicone, epoxy resins, polyurethane, acrylic latex—isocyanates, lead, formaldehyde | Skin irritation and sensitization, respiratory conditions, cancer, neurological and endocrine effects |
| Ceilings | Gypsum, fiberglass)—asbestos, formaldehyde | Pulmonary disease, eye and skin irritation, cancer, |
| Composite wood | Particleboard, plywood—isocyanates, formaldehyde | Skin and eye irritation, pulmonary effects, cancer |
| Flooring | Tile, wood, polyvinyl chloride—phthalates, formaldehyde, plasticizers | Eye and skin irritation, lung cancer, endocrine effects |
| Thermal insulation | Rigid foam, spray foam, fibre—asbestos, formaldehyde, polybrominated diphenyl ethers | Reproductive effects, lung disease, endocrine effects |
| Carpets | Nylon, wool—styrene, xylenes, formaldehyde, ethylbenzene | Respiratory effects, eye and skin irritation, cancer |
| Electrical equipment | Switches, thermostats—mercury, polychlorinated biphenyls | Endocrine and lung effects, lung cancer, neurological effects |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bungau, C.C.; Bendea, C.; Bungau, T.; Radu, A.-F.; Prada, M.F.; Hanga-Farcas, I.F.; Vesa, C.M. The Relationship between the Parameters That Characterize a Built Living Space and the Health Status of Its Inhabitants. Sustainability 2024, 16, 1771. https://doi.org/10.3390/su16051771
Bungau CC, Bendea C, Bungau T, Radu A-F, Prada MF, Hanga-Farcas IF, Vesa CM. The Relationship between the Parameters That Characterize a Built Living Space and the Health Status of Its Inhabitants. Sustainability. 2024; 16(5):1771. https://doi.org/10.3390/su16051771
Chicago/Turabian StyleBungau, Constantin C., Codruta Bendea, Tudor Bungau, Andrei-Flavius Radu, Marcela Florina Prada, Ioana Francesca Hanga-Farcas, and Cosmin Mihai Vesa. 2024. "The Relationship between the Parameters That Characterize a Built Living Space and the Health Status of Its Inhabitants" Sustainability 16, no. 5: 1771. https://doi.org/10.3390/su16051771
APA StyleBungau, C. C., Bendea, C., Bungau, T., Radu, A.-F., Prada, M. F., Hanga-Farcas, I. F., & Vesa, C. M. (2024). The Relationship between the Parameters That Characterize a Built Living Space and the Health Status of Its Inhabitants. Sustainability, 16(5), 1771. https://doi.org/10.3390/su16051771







