Abstract
Worldwide, the number of users of medical facilities is increasing due to the pandemic phenomenon and extended life expectancy. In addition, the majority of medical facility occupants are patients, leading to issues of inconvenience in movement and increased vulnerability during evacuations in the event of a fire. Therefore, the availability of nursing personnel, who serve as assistants in tasks such as transporting beds and wheelchairs essential for patient evacuation, is crucial for ensuring evacuation safety. However, a global shortage of nursing personnel has led to ongoing research on optimizing workforce allocation. In this study, the Available Safe Egress Time (ASET) and Required Safe Egress Time (RSET) were quantitatively compared for medical facilities with a combination of intensive care units and general wards, utilizing a Fire Dynamics Simulator (FDS) and Flexsim Healthcare simulations to assess fire risk. The research goal here is to provide sustainable research directions for determining the minimum ratio of nurses to patients required for evacuation in a disaster, ensuring the continuous availability of nursing personnel in medical facilities. To achieve this, the variable was set to five stages based on the total number of patients per nurse. As a result of this study, it was confirmed that when the nurse-to-patient ratio exceeded 1:6, more than 70% of bedridden patients died. Additionally, it was verified that maintaining a patient-to-nurse ratio of less than 1:1 is effective for ensuring evacuation safety.
1. Introduction
The average life expectancy in the Organization for Economic Cooperation and Development (OECD) increased by about 1.3%, from 79.3 years old in 2010 to 80.3 years old in 2022. Consequently, current medical expenses as a percentage of Gross Domestic Products (GDPs) rose by 2.2% annually [1]. This is anticipated to lead to an increase in medical costs and a rise in the number of medical facility users as life expectancy continues to grow. Furthermore, since 2019, coronavirus disease 2019 (COVID-19) has had a global impact, underscoring the significance of medical facilities, including hospital infrastructure, and the need for an increased workforce to cope with the surge in patient numbers [2]. This global pandemic has highlighted the importance of having sufficient intensive care units to accommodate inpatients [3].
Nevertheless, medical facilities face challenges that can intensify fires, stemming from internal hazardous and combustible substances, including alcohol, radiation, and mattresses. Patients hospitalized in intensive care units are particularly vulnerable during emergency evacuations, such as fires [4]. Consequently, doctors and other nursing staff play a crucial role in assisting patients with evacuation in the event of a disaster situation [5].
On 24 April 2021, an oxygen cylinder explosion at a hospital in Baghdad, Iraq, resulted in a fire that claimed the lives of 82 people and injured 110 [6]. Fires in medical facilities pose a higher risk than in ordinary buildings due to the potential for numerous casualties. Recognizing this, the World Health Organization (WHO) presented the need for hospital safety measures, including fire prevention and suppression systems, design structures, exit routes, and disaster management systems, to ensure hospitals can effectively respond to emergencies and disasters [7].
Table 1 shows fires and casualties in medical facilities around the world.

Table 1.
Fire accidents across global medical facilities [8].
In a previous study on the safety of medical facilities, Kim et al. conducted fire simulations for each type of interior building finishing material, emphasizing the significance of flame-retardant building finishing materials and the use of fire risk evaluation methods for each evacuation route [8].
Building on two successful hospital evacuation cases caused by wildfires in Israel, Kreinin A. et al. highlighted the importance of accessible evacuation routes and outlined the necessity and methodology of emergency operation plans [9].
An et al. selected three evacuation routes with equal travel distances and conducted a quantitative comparison between Available Safe Egress Time (ASET) and Required Safe Egress Time (RSET). Their study revealed the necessity of including a ramp in the evacuation route of medical facilities, particularly for patients with mobility challenges [10].
Vinay et al. utilized the Fire Dynamics Simulator (FDS) to compare the impact of changes in oxygen concentration on fires caused by ventilators in hospital intensive care units. They suggested the necessity of a fire safety management system for this scenario, as the Heat Release Rate (HRR) increases with higher oxygen concentrations [11].
Hostikka S. et al. conducted a life safety assessment considering gas temperature, toxic gas concentration, and the fractional effective dose (FED) and fractional irritant concentration (FIC) for assessing the effects of fire prevention sprinklers on patients. In their study, the findings indicate that sprinklers are effective in controlling fires, but there is an emphasis on the importance of accurate fire toxicity assessments due to the potential risks posed by toxic gases [12].
Wood et al. investigated oxygen-related fires at hospitals, revealing an increase in such incidents in facilities treating COVID-19 patients. Additionally, they highlighted the potential dangers of oxygen-related fires in hospitals and provided a checklist [13].
Jahangiri et al. conducted a fire risk assessment on hospitals affiliated with the Shiraz University of Medical Sciences using a checklist based on NFPA101. They emphasized the necessity of implementing measures in exit areas, such as improving access to exits and increasing emergency exits, to mitigate fire risk levels in hospitals [14].
Hospital rooms in medical facilities generally consist of an intensive care unit (ICU) and a general ward. Intensive care units are essential components of the medical system, providing facilities for specialists, doctors, and nurses to effectively treat severely ill patients [15,16]. In particular, as the number of patients per nurse increases, the patient mortality rate and hospital infection rate also increase. Therefore, the appropriate level of nurse placement in the intensive care unit recommends a ratio of nurses to patients at 1:1 or 1:2 [17,18].
Cartaxo et al. investigated general wards of Austrian hospitals, defining the ratio of nursing staff to patients as a patient-to-nurse ratio (PtN) value. Their study revealed that, on average, one nurse was responsible for 18.4 patients, leading to the conclusion that the staffing was deemed inappropriate [19].
Zraychikova et al. surveyed nurses in 116 wards across 13 mental hospitals in Switzerland, revealing that the average number of patients per nurse was 7.5 to 9.4 per week and 16.2 at night [20].
Tenorio et al. randomly selected 400 nurses from King Saud Medical City (KSMC) in Riyadh, Saudi Arabia, and analyzed the nurse-patient ratio (n:p ratio) and “missed nursing care”. Their analysis revealed that as the number of patients assigned to nurses increases, the incidence of “missed nursing care” also rises, negatively impacting nurses [21].
Currently, there is a worldwide shortage of nursing personnel, contributing to the deterioration of the quality of medical care for patients [21]. Additionally, medical facilities require support from medical staff, especially given the vulnerability of occupants during evacuations. The lack of nursing staff can have a detrimental impact on patient evacuation in the event of a fire or other disaster.
Previous studies on the safety of medical facilities have primarily focused on assessing the risks associated with the facilities and materials used within, emphasizing the significance of safety management systems and evacuation routes. Additionally, prior studies on the shortage of healthcare personnel have highlighted the ratio of nurses to patients, surveys on the current state of the nurse–patient ratio, and risks associated with a shortage of nursing staff.
However, there is a lack of research on the impact of the nurse-to-patient ratio during emergencies such as fires. Furthermore, there is a need for sustainable research on securing nursing personnel. This study selected one medical facility as a representative and conducted a risk assessment associated with the nurse-to-patient ratio through fire risk assessment. The research goal is to determine the minimum ratio of nurses to patients required for successful evacuation in the event of a disaster. Additionally, the aim is to suggest sustainable research directions for ensuring the continuous availability of nursing personnel in medical facilities.
2. Fire Risk Assessment
2.1. Fire Scenario
In this study, a fire risk assessment was conducted for medical facilities with an ICU and general wards situated on one floor. The risk assessment was performed by comparing the Available Safe Egress Time (ASET) and Required Safe Egress Time (RSET). Each analysis simulation used the FDS, a fire analysis program of NIST, and Flexsim Healthcare, developed by Flexsim Software Products, Inc. (Orem, UT, USA).
Figure 1 shows the research flow chart.
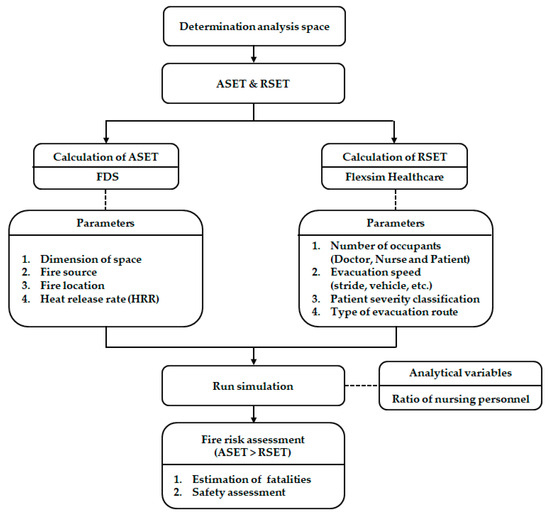
Figure 1.
Flowchart of this study.
The medical facility under consideration for the fire scenario is a general hospital with a floor area of 1153.15 m2 per floor. The fire occurrence layer was chosen as the third floor, where both an ICU and general wards coexist. The hospital rooms on this floor comprise general wards with a total of 34 beds distributed across four single rooms and six 5-bed rooms, as well as an ICU with 15 beds. Additionally, the evacuation facility is equipped with six elevators and three sets of emergency stairs. Figure 2 illustrates the layout of the medical facilities used in this study, and Figure 3 displays the location of the simulation model and the fire source implemented with the FDS.
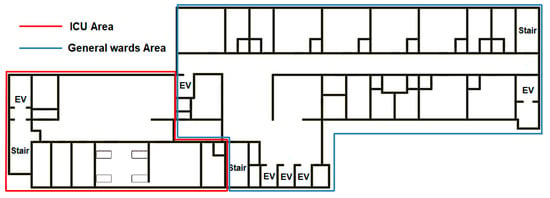
Figure 2.
Plan of the medical facilities’ layout.
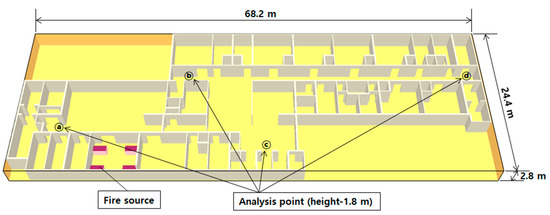
Figure 3.
Simulation modeling conditions.
The fire scenario in this study was configured to simulate a fire breaking out in an intensive care unit bed, with the heat release rate of the bed mattress, set as the ignition source, ranging from 210 to 270 s and reaching a maximum of 1778.95 kW [22]. Table 2 presents the fire boundary conditions used in the FDS.

Table 2.
Boundary conditions for the fire simulation.
The calculation accuracy is strongly dependent on the FDS mesh size. The size of the analysis grid can be determined by the characteristic fire diameter using Equation (1) in the fire plume analysis:
where is the characteristic fire diameter, is the total heat release rate (kW), is the outside air density (kg/m3), is the specific heat (kJ/kg·K), is the outside air temperature (K), is the acceleration of gravity (m/s2), and is the nominal size of a mesh cell.
The parameter is valid only if the value falls between 4 and 16 [23]. The value applied to this analysis is 1.207 m, and has a value of 9.05 in this paper. Therefore, the mesh size used in this study satisfies the convergence condition.
2.2. Evacuation Simulation Conditions
The assessment of the evacuation time for occupants was conducted using Flexsim Healthcare (version 24.0), developed by Flexsim Software Products, Inc. Flexsim Healthcare is a discrete-event simulation (DES) tool used to evaluate and validate scenarios in medical institutions [24,25]. Figure 4 illustrates the simulation model implemented in Flexsim Healthcare.
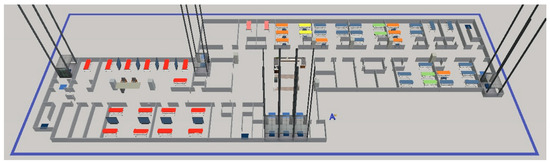
Figure 4.
Evacuation simulation modeling via Flexsim Healthcare.
In this study, the ICU comprised bedridden patients, while the general ward included bedridden patients, wheelchair patients, and self-reliant walking patients, categorized by the severity of the patient. The occupancy density of the fire floor was set based on the actual occupancy ratio of medical facilities using the occupancy load coefficient of the International Building Code of 2003 (IBC 2003) [26].
Table 3 presents the proportions and movement speeds of the different patient categories, and Figure 5 displays patient movement patterns according to evacuation routes.

Table 3.
Patient severity rate and speed of movement [26,27].
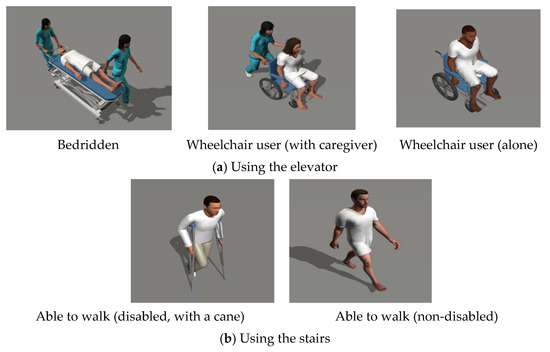
Figure 5.
Patient groups and their evacuation routes.
Patients who have difficulty moving on their own use beds and wheelchairs as auxiliary means of transportation depending on the severity of their injury, and require assistance from nursing personnel. Specifically, the bed, among the patients’ means of transportation, necessitates a series of preparatory steps to release the lock in case of a disaster involving the wheel lock. In this study, two nursing personnel were set to assist in moving bedridden patients, and Table 4 presents the specifications of the beds and wheelchairs, along with the preparation time required for moving them [28,29].

Table 4.
Size and preparation time of the beds and wheelchairs [28,29].
Assuming that there was one visitor for every three general ward patients and one for every ICU patient, totaling 26 people, a movement speed of 1.2 m/s was set. Additionally, visitors were configured to evacuate immediately in the event of a fire.
Currently, there is a worldwide shortage of nurses, and the quality of medical care and emergency responses varies depending on the patient-to-nurse ratio [30]. In this study, the role of assisting in patient evacuation was given to both doctors and nurses. The number of doctors for all cases was set at three, based on a ratio of one doctor per 20 patients [31], while the number of nurses was determined at different proportions to the total number of patients in each case. Consequently, the simulation was conducted by varying the proportion of patients assigned to one nurse. Table 5 displays the ratios and numbers of nurses to patients as set in this study.

Table 5.
Variable setting conditions.
3. Results and Discussions
3.1. Analysis Results
3.1.1. Analysis Results for the ASET
The ASET measurement for medical facilities was established by determining the point at which life safety criteria for each factor were surpassed, with a focus on the evacuation route of the fire floor. The ASET was measured using the fractional effective dose (FED), visibility, temperature, oxygen, carbon monoxide, and carbon dioxide, based on life safety standards set at a height of 1.8 m, which is the respiratory limit [32]. Table 6 outlines the life safety standards, while Figure 6 illustrates the change in life safety standards measured with the FDS.

Table 6.
Performance criteria for life safety [32].
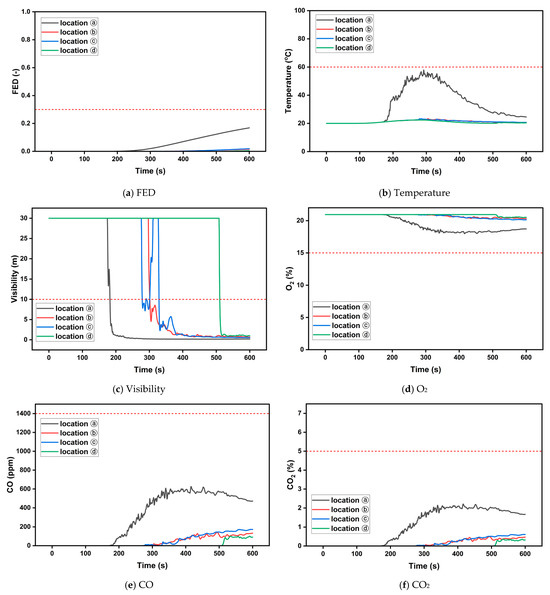
Figure 6.
Variations in life safety standards according to the FDS.
The walls of the fire room were composed of concrete, and the fire in the bed did not spread because there were no other combustible materials nearby. As a result of the FDS simulation, the excess time point was not measured for criteria other than visibility among the life safety standards during operational time. Consequently, the ASET was determined based on the excess time related to visibility. Table 7 displays the ASET for each evacuation route.

Table 7.
ASET for each evacuation route.
3.1.2. Results of RSET Measurements and Estimated Casualties Analysis
The RSET was measured in Flexsim Healthcare as the time when all occupants had left the floor through the evacuation path. The simulation involved randomly placing the nurse’s position while keeping the patient’s position fixed, and it was run 30 times.
Conditions for the safe evacuation of occupants can be defined by Equation (2) [33,34]. Therefore, if the ASET for any evacuation route was exceeded, it was estimated as a casualty.
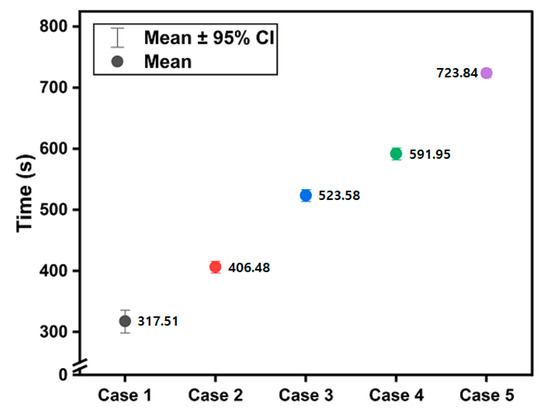
Figure 7.
Average RSET for each case.

Table 8.
Casualties analysis according to the evacuation routes in each case.
The simulation analysis revealed a significant increase in the RSET in Case 3 with a nurse-to-patient ratio of 1:6, as well as in Case 5 with a ratio of 1:10. Conversely, the number of casualties surged in Case 2 and Case 3.
An average of two to four bedridden patients were confirmed to have moved to location ⓐ. However, at location ⓐ, most mobile personnel suffered casualties due to their proximity to the fire source and the lowest ASET.
Typically, occupants choose an evacuation route that avoids the area where the fire originated. Thus, the RSET was compared with and without the use of location ⓐ. Table 9 presents the RSET with and without the use of location ⓐ in Case 1, while Table 10 displays the estimated number of casualties when location ⓐ is not utilized.

Table 9.
RSET in cases with and without the use of location ⓐ.

Table 10.
Casualties analysis for each evacuation route when location ⓐ is not used.
In the simulation results, not using location ⓐ did not significantly impact the RSET, but it led to a decrease of one to two in the number of casualties compared to when location ⓐ was used. This suggests that, in the event of a fire, securing evacuation safety for occupants is effective if evacuation routes near the fire site are not used.
The evacuation time for visitors and ambulatory patients (patients able to walk) was measured within 1 min in both cases based on the condition of utilizing location ⓐ, confirming the feasibility of evacuation within the ASET. However, for bedridden or wheelchair-bound patients, the waiting time for elevator use negatively impacted the RSET. Consequently, location ⓒ, where three elevators operated regardless of the utilization of location ⓐ, showed the highest number of casualties due to its concentration of a large number of patients.
Figure 8 illustrates the trend of increasing casualties for each case, while Table 11 presents the number of casualties and the rate of increase.
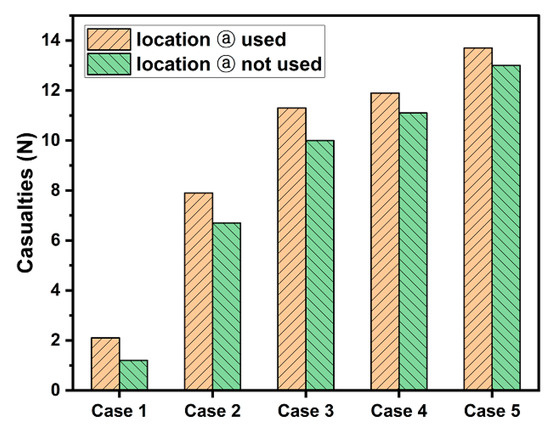
Figure 8.
Distribution of estimated casualties by case.

Table 11.
The number of casualties and the rate of increase in each case.
As the proportion of patients assigned to one nurse increased, the number of casualties tended to rise due to increased waiting times for evacuation. However, the trend showed a rapid increase in Case 2, followed by a gradual decrease as the number of nurses decreased. Nevertheless, in Case 5, the trend of increasing casualties appeared to rise again, indicating that playing an auxiliary role in evacuating patients becomes challenging if the nurse-to-patient ratio exceeds 1:8.
3.2. Discussions
In this study, the assistance of bed movement was initially set to involve two nurses. However, the number of assistants may vary in emergency situations, such as fires. Consequently, the number of nurses assisting with bed movement was adjusted to one, and additional simulations were conducted. Additionally, evacuation routes were simulated both with and without the use of location ⓐ. Figure 9 illustrates the transfer of bedridden patients observed in these simulations, and Table 12 details the transfer conditions based on the number of assistants.
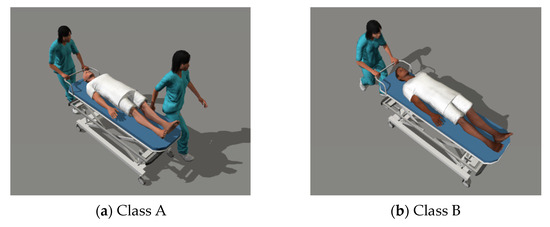
Figure 9.
Conditions of assistance personnel for bedridden patients.

Table 12.
Bed transfer preparation time and transfer speed based on the number of assisting personnel.
Table 13 presents the RSET for Class B. Class B involves a longer travel preparation time and lower travel speed for bedridden patients compared to Class A. However, as observed in the simulation, the RSET showed a decrease ranging from at least 7.01 s to up to 145.01 s when compared to Class A.

Table 13.
RSET for Class B with and without the use of location ⓐ.
In Class B, there was a tendency for the RSET to increase when location ⓐ was not used, as opposed to when location ⓐ was utilized. This increase was attributed to differences in the speed of bedridden patient movement and an extended travel distance resulting from the inability to use nearby evacuation routes.
Figure 10 illustrates the distribution of casualties in Class B, and Table 14 shows the number of casualties by class.
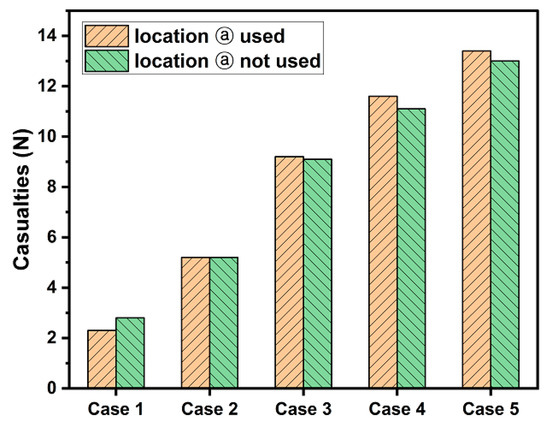
Figure 10.
Distribution of casualties within Class B by case.

Table 14.
Comparison of casualties for Class A and Class B cases.
Following the simulation, Class B confirmed a notable increase in casualties in Case 3 with nine nurses, gradually decreasing afterward. Nevertheless, overall, Class B demonstrated the ability to assist in evacuating bedridden patients with a smaller team, leading to a reduction in the overall casualties. However, in Case 1, it was confirmed that there was no significant difference from Class A since sufficient manpower could be secured regardless of the number of bed assistants.
In addition, the number of casualties in Class B decreased by up to three compared to Class A in Case 2 and Case 3. This confirms that when the ratio of nurses to patients is 1:4 or 1:6, having one nurse assist each bedridden patient is effective in reducing casualties.
However, in Case 4 and Case 5, there was no significant difference in the number of casualties between Class A and Class B due to insufficient auxiliary personnel. These results indicate that additional measures to reduce casualties are meaningless when the nurse-to-patient ratio is greater than or equal to 1:6.
In the event of a fire within a medical facility, the majority of fatalities are among bedridden patients. This is attributed to their increased evacuation time caused by limitations on elevator movements due to the volume of beds used and the need for auxiliary personnel. To further investigate, we simulated the presence of 50% bedridden patients (ICU: 8, general ward: 1) to determine the required number of nurses based on the patient count. However, this simulation was conducted only in cases where location ⓐ, confirmed for reducing the number of casualties, was not utilized.
Figure 11 displays the RSET and distribution of casualties under conditions without location ⓐ when the number of bedridden patients decreases by 50% among all patients.
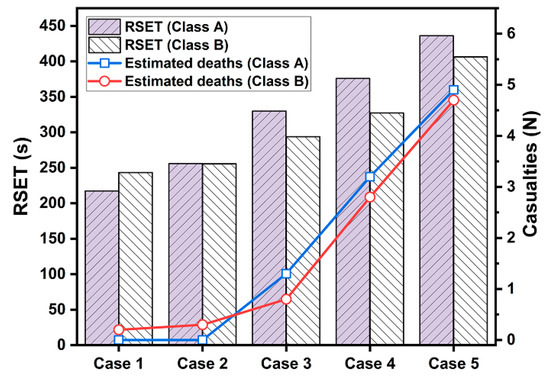
Figure 11.
RSET and distribution of casualties without location ⓐ—50% reduction in bedridden patients.
As a result of the simulation, it was observed that the RSET decreased by at least 99.66 s and up to 295.48 s when the bedridden patients were set at 50%. Furthermore, casualties were reduced by at least 1.2 and up to 8.7 casualties. This underscores the significance of the number of bedridden patients as a crucial factor in assessing the fire risk of medical facilities. Table 15 presents the proportion of bedridden patients assigned to one nurse, while Figure 12 depicts the relationship between the NtoB (nurse-to-bedridden patient ratio) and the number of deceased individuals by class when location ⓐ is not used.

Table 15.
Nurse-to-bedridden patient ratio (NtoB).
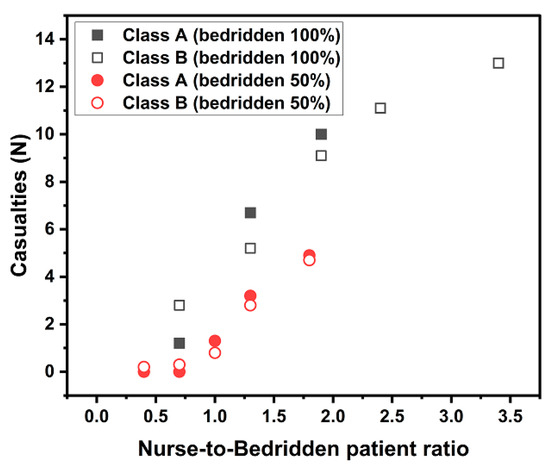
Figure 12.
Distribution of casualties based on the nurse-to-bedridden patient ratio.
Upon analyzing the casualties according to the NtoB, it was confirmed that the number of casualties in both classes increased rapidly when the NtoB exceeded 1.0, with 50% of patients being bedridden. Additionally, in the case of 100% of patients being bedridden, it was also observed that the casualties toll increased rapidly as the NtoB exceeded 1.0. This indicates the effectiveness of evacuation when the ratio of bedridden patients to one nurse does not exceed a maximum of 1:1.
4. Conclusions
In this study, fire risk assessments were conducted using the FDS (version 5.5.3) and Flexsim Healthcare simulations for medical facilities, with variables set as the ratio of nurses to patients. Analysis of the fire risk assessment’s results confirmed the following by comparing the ASET, RSET, and the estimated number of casualties.
Firstly, upon comparing the number of casualties based on the utilization of evacuation routes near the fire source, it was observed that the number of casualties decreased when the evacuation route around the fire source was not used. This confirms that avoiding an evacuation route near the fire source is effective for ensuring the safety of occupants during a fire evacuation.
Secondly, when elevators used as evacuation routes were concentrated in one location, the number of casualties was also concentrated along that route. This suggests that bedridden patients, the most vulnerable during evacuations in medical facilities, face an increased risk in their RSET and encounter challenges in securing evacuation safety due to prolonged elevator waiting times.
Thirdly, in comparing cases where the number of nurses assisting bedridden patients was either two or one, Class B, assisted by one nurse, demonstrated a reduction effect of up to three casualties. These results indicate that Class B effectively ensures an adequate number of nurses for moving bedridden patients compared to Class A. Therefore, it has been established that prioritizing the number of nurses per bed is crucial for the evacuation safety of occupants in medical facilities.
Fourthly, in analyzing the number of casualties based on the ratio of nurses to patients, the number decreased after the casualty toll surged at 1:4 in Class A and 1:6 in Class B. Additionally, if the ratio of nurses to patients exceeds 1:6, more than 70% of bedridden patients are observed to become casualties. This is confirmed to be due to a shortage of nurses available to evacuate bedridden patients. Consequently, it was affirmed that the number of patients assigned to one nurse in a medical facility should not exceed six to help secure evacuation personnel in case of an emergency.
Finally, upon comparing the number of casualties based on the ratio of nurses to bedridden patients, it was confirmed that the number of casualties increased rapidly when the NtoB exceeded 1:1. These results suggest that if the NtoB is less than 1:1, it is effective in ensuring the evacuation safety of patients in case of an emergency. Additionally, the number of bedridden patients indicates that it is an essential consideration in determining the staffing levels of nurses in medical facilities.
Occupants of medical facilities are characterized by their vulnerability during evacuations. Consequently, the number of nurses in medical facilities is a critical factor for ensuring the evacuation safety of occupants. Moreover, the nurse-to-patient ratio is closely tied to the quality of medical care. However, owing to the global shortage of nursing personnel, ongoing research should focus on determining the appropriate staffing levels.
This study selected one typical medical facility and evaluated the risk of the nurse-to-patient ratio through a fire risk assessment. However, research results may differ depending on scenarios such as the structure of the medical facility, its internal arrangement, and the nature of the fire. Therefore, sustained research is needed to refine the minimum ratio of nurses to patients and the required evacuation time for the safe evacuation of patients. It is believed that this study will contribute to sustainable research on the minimum number of nurses required in medical facilities.
Author Contributions
Conceptualization, D.R.; methodology, Y.K., J.K. and M.K.; formal analysis, Y.K.; investigation, Y.K., J.K. and M.K.; resources, Y.K.; writing—original draft preparation, Y.K., J.K. and M.K.; writing—review and editing, D.R.; visualization, Y.K.; supervision, D.R.; funding acquisition, D.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
This work was supported by Incheon National University Research Grant in 2023.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- OECD Homepage. OECD Health Statistics 2023. Available online: https://www.oecd.org/health/health-data.htm (accessed on 16 October 2023).
- Boltürk, E.; Seker, S. Spherical Fuzzy Present Worth Analysis Method for Emergency Hospital Investment Analysis. IEEE Trans. Eng. Manag. 2023, 70, 2891–2902. [Google Scholar] [CrossRef]
- Almuqbil, M.; Almoteer, A.I.; Suwayyid, A.M.; Bakarman, A.H.; Alrashed, R.F.; Alrobish, M.; Alasalb, F.; Alhusaynan, A.A.; Alnefaie, M.H.; Altayar, A.S.; et al. Characteristics of COVID-19 Patients Admitted to Intensive Care Unit in Multispecialty Hospital of Riyadh, Saudi Arabia: A Retrospective Study. Healthcare 2023, 11, 2500. [Google Scholar] [CrossRef] [PubMed]
- Bray, K.; Wren, I.; Baldwin, A.; Ledger, U.S.; Gibson, V.; Goodman, S.; Walsh, D. Standards for nurse staffing in critical care units determined by: The british association of critical care nurses, the critical care networks national nurse leads, royal college of nursing critical care and in-flight forum. Nurs. Crit. Care 2010, 15, 109–111. [Google Scholar] [CrossRef] [PubMed]
- Bongiovanni, I.; Leo, E.; Ritrovato, M.; Santoro, A.; Derrico, P. Implementation of best practices for emergency response and recovery at a large hospital: A fire emergency case study. Saf. Sci. 2017, 96, 121–131. [Google Scholar] [CrossRef]
- WHO. Hospital Safety Index: Guide for Evaluators, 2nd ed.; WHO: Geneva, Switzerland, 2015; ISBN 9789241548984. Available online: https://iris.paho.org/handle/10665.2/51448 (accessed on 16 October 2023).
- Wikipedia, 2021 Baghdad Hospital Fire. Available online: https://en.wikipedia.org/w/index.php?title=2021_Baghdad_hospital_fire&oldid=1190819750 (accessed on 16 October 2023).
- Kim, Y.; Park, D.; Kim, S.; Rie, D. A Study on the Quantitative Fire Performance Evaluation Method of Building Finishing Materials with a Focus on Medical Facilities. Sustainability 2023, 15, 9373. [Google Scholar] [CrossRef]
- Kreinin, A.; Lyansberg, A.; Yusupov, M.; Moran, D.S. Fire Disaster Readiness: Preparation for the Evacuation of Medical Facilities During Fires in Haifa, Israel, 2016. Disaster Med. Public Health Prep. 2019, 13, 375–379. [Google Scholar] [CrossRef]
- Ahn, C.; Kim, H.; Choi, I.; Rie, D. A Study on the Safety Evaluation of Escape Routes for Vulnerable Populations in Residential Facilities. Sustainability 2022, 14, 5998. [Google Scholar] [CrossRef]
- Vinay; Raja, S.; Tauseef, S.M.; Varadharajan, S. Investigating the impact of oxygen concentration on fire dynamics using numerical simulation with FDS. Process Saf. Environ. Prot. 2023, 178, 195–203. [Google Scholar] [CrossRef]
- Hostikka, S.; Veikkanen, E.; Hakkarainen, T.; Kajolinna, T. Experimental investigation of human tenability and sprinkler protection in hospital room fires. Fire Mater. 2021, 45, 823–832. [Google Scholar] [CrossRef]
- Wood, M.H.; Hailwood, M.; Koutelos, K. Reducing the risk of oxygen-related fires and explosions in hospitals treating COVID-19 patients. Process Saf. Environ. Prot. 2021, 153, 278–288. [Google Scholar] [CrossRef]
- Jahangiri, M.; Rajabi, F.; Darooghe, F. Fire risk assessment in selected hospitals of Shiraz University of Medical Sciences in accordance with NFPA101. Iran Occup. Health 2016, 13, 99–106. [Google Scholar]
- Marshall, J.C.; Bosco, L.; Adhikari, N.K.; Connolly, B.; Diaz, J.V.; Dorman, T.; Fowler, R.A.; Meyfroidt, G.; Nakagawa, S.; Pelosi, P.; et al. What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and Critical Care Medicine. J. Crit. Care 2017, 37, 270–276. [Google Scholar] [CrossRef]
- Marzook, M.; Rajapaksha, M.; Chanakya, T.; Dampage, U. A Mobile Application That Employs Artificial Intelligence to Forecast the Required Number of Beds for Intensive Care Units in Sri Lanka. In Proceedings of the 2023 IEEE 17th International Conference on Industrial and Information Systems (ICIIS), Peradeniya, Sri Lanka, 25–26 August 2023; pp. 221–226. [Google Scholar] [CrossRef]
- Park, M.; Yang, E.; Lee, M.; Cho, S.-H.; Shim, M.; Lee, S.H. The Nurse Staffing in Intensive Care Units based on Nursing Care Needs: A Multicenter Study. J. Korean Crit. Care Nurs. 2021, 14, 1–11. [Google Scholar] [CrossRef]
- World Health Organization. State of the World’s Nursing 2020: Investing in Education, Jobs and Leadership; WHO: Geneva, Switzerland, 2020. Available online: https://www.who.int/publications/i/item/9789240003279 (accessed on 16 October 2023).
- Cartaxo, A.; Eberl, I.; Mayer, H. Die MISSCARE-Austria-Studie—Teil II. HeilberufeScience 2022, 13, 43–60. [Google Scholar] [CrossRef]
- Zraychikova, E.; Gehri, B.; Zúñiga, F.; Bachnick, S.; Simon, M. The Interaction Between Leadership, the Patient-to-Nurse Ratio and Nurses’ Work-Life Balance in the Psychiatric Inpatient Setting in Switzerland: A Secondary Data Analysis of Cross-Sectional Data. Adm. Policy Ment. Health Ment. Health Serv. Res. 2023, 50, 317–326. [Google Scholar] [CrossRef]
- Tenorio, M.; Aletreby, W.; Shammari, B.; Almuabbadi, B.; Mwawish, H.; Montegrico, J. The Interrelation between nurse-to-patient ratio, nurse engagement, and missed nursing care in King Saud Medical City: Basis for development of nurse–patient quality of care. Saudi J. Health Sci. 2021, 10, 115. [Google Scholar] [CrossRef]
- Seo, B.Y.; Jang, W.B.; Park, K.W.; Hong, W.H. Experimental Study on the Measurement of Fire Behavior and Heat Release Rate in Building Compartment Space—Focus on Full Scale Fire Test of the Bed Mattress. Fire Sci. Eng. 2018, 32, 28–33. [Google Scholar] [CrossRef]
- Salley, M.H.; Kassawara, R.P. Verification and validation of selected fire models for nuclear power plant applications In Fire Dynamics Simulator (FDS); US Nuclear Regulatory Commission, Office of Nuclear Regulatory Research (RES): Rockville, MD, USA, 2007; Volume 7, ISBN 1800553684.
- Wijgergangs, G. Validation of Flexsim HC Simulation Models Using an Integrated View of Process Mining Results. Master’s Thesis, Eindhoven University of Technology, Eindhoven, The Netherlands, 2014. [Google Scholar]
- Pongjetanapong, K.; O’Sullivan, M.; Walker, C.; Furian, N. Implementing complex task allocation in a cytology lab via HCCM using Flexsim HC. Simul. Model. Pract. Theory 2018, 86, 139–154. [Google Scholar] [CrossRef]
- International Code Council, Inc. International Buildng Code 2003; International Code Council, Inc.: Washington, DC, USA, 2003; ISBN 1-892395-7. [Google Scholar]
- Kim, E.S.; Lee, J.S.; Kim, M.H.; You, H.K.; Song, Y.H.; Min, K.C. A Study on Evacuation of Patients in Hospital: Part I. Fire Sci. Eng. 2005, 19, 20–28. [Google Scholar]
- No. 2017-16; Standard for Mattress. Ministry of Food and Drug Safety: Seoul, Republic of Korea, 2017.
- KS P 6113; Wheelchair Standard. National Standard Certification Integrated Information System: Seoul, Republic of Korea, 2007.
- Shekelle, P.G. Nurse–Patient Ratios as a Patient Safety Strategy. Ann. Intern. Med. 2013, 158, 404–409. [Google Scholar] [CrossRef]
- Medical Service Act: Changes to the Law; Republic of Korea. 2023. Available online: https://www.law.go.kr/LSW/eng/engLsSc.do?menuId=2§ion=lawNm&query=medical&x=21&y=34#liBgcolor32 (accessed on 12 October 2023).
- National Fire Safety Codes 203: Changes to the Law; Republic of Korea. 2021. Available online: https://www.law.go.kr/admRulSc.do?menuId=5&subMenuId=41&tabMenuId=183&query=nfsc203#liBgcolor0 (accessed on 13 August 2023).
- Poon, S.L. A dynamic approach to ASET/RSET assessment in performance based design. Procedia Eng. 2014, 71, 173–181. [Google Scholar] [CrossRef]
- Abir, I.M.; Mohd Ibrahim, A.; Toha, S.F.; Shafie, A.A. A review on the hospital evacuation simulation models. Int. J. Disaster Risk Reduct. 2022, 77, 103083. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).