Perceived Health Impacts, Sources of Information and Individual Actions to Address Air Quality in Two Cities in Nigeria
Abstract
1. Introduction
2. Literature Review
2.1. Health Impacts of Poor Air Quality
2.2. Sources of Information on Air Quality
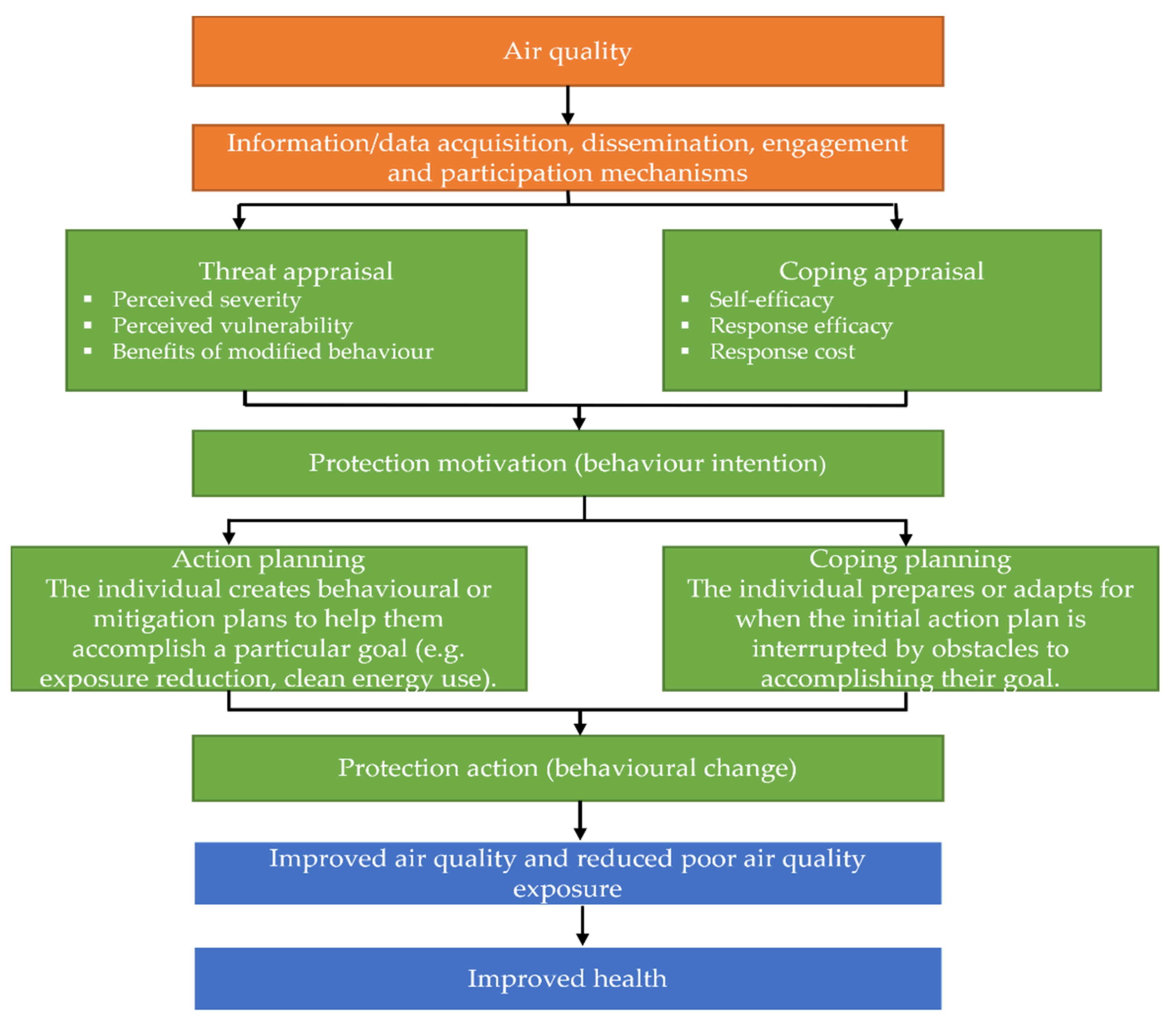
2.3. Individual Actions in Response to Poor Air Quality
3. Materials and Methods
3.1. Research Locations
3.2. Sample Participants and Demographics
3.3. Data Collection and Analysis
4. Results
4.1. Health Impacts of Poor Air Quality
“I want to believe that in this case, it is education. Most of these things are taught in schools. Education plays a major role here. The younger ones are more educated than the older ones in Enugu.”—Eof1.
“The understanding of the meaning of air quality. The awareness of the air quality of the cities. The more educated and higher income earners are more aware or exposed to what air quality implies and can know why air quality is poor more than the less educated and lower income earners.”—Aom7.
4.2. Age Groups Perceived to Be most Affected by Poor Air Quality
“The higher income earners and higher educated people are more aware of poor air quality due to their education and where they live.”—Aof9.
4.3. Gender Perceived to Be most Affected by Poor Air Quality
4.4. Interaction between Poor Air Quality and COVID-19
4.5. Perceived Health Effects of Poor Air Quality on Individuals in the Past Year
“Those with higher income and higher education are more aware of what contributes to poor air quality than the less educated and lower income earners who do not know much about air quality.”—Ayf8
“Many older people in Enugu who have had the experience of how the city environment used to be or has changed with many activities can say the air quality is poorer than before while the younger who do not have much of experience would say the environment or air quality is better.”—Aom4.
“The older people are more affected or vulnerable and they may rate air quality poorer in the Enugu city, and the younger ones may not be as concerned about their air quality like the older people.”—Ayf5.
“The older people must have lived in the area when there were less population and activities that contribute to poor air quality. That is to say that the older ones are more experienced with the locations and that is why they rated the areas poorer than the younger ones.”—Eof6.
4.6. Sources of Information on Air Quality
“At the moment, the younger ones are having more access to information on air quality due to the new technology coming up than the older ones. They have more access to the internet and are more aware of the control measures than the older ones.”—Eym12.
“Miseducation has made the older generation 35+ and above not decode the need for clean air and the ills from air pollution. Younger people even without witnessing clean air or a good ecosystem have seen it on the internet which they access more than the older generation and are more educated to understand that it could have been better than what it is in the present”—Eym3.
“I believe that there is no difference in Abuja because Abuja is a developed city. Everybody tends to believe in the same thing as most of the activities by old and young are almost the same way. There are not many ghettos in Abuja but there are in Enugu.”—Ayf3.
4.7. Individual Actions for Clean Air
“It is the government that should be in the prime position to control poor air quality.”—Eyf4.
“It is the primary responsibility of government to implement air pollution control, but it is a collective responsibility of both citizens and government to control poor air quality with organized public knowledge, sensitization & orientation”.—Eym3
“In this case, I think the government should take the primary responsibility. The government should set rules for managing poor air quality and should be held responsible”.—Eof5.
5. Discussion
6. Conclusions
- The beliefs of residents on the health impacts of PAQ are similar in two different developing-world cities (Abuja and Enugu) in Nigeria.
- The perceptions of people in the study areas are mainly because of awareness and knowledge of AQ.
- The majority of the residents believe that they are affected by PAQ and were affected in the year prior to the research (74% in Abuja and 75% in Enugu).
- Older people are identified to be the group of people most vulnerable to the deleterious effects of PAQ (mean scores: 1.91 in Abuja and 1.58 in Enugu).
- PAQ was perceived to make COVID-19 worse and to increase the chances of COVID-19 infection and aggravate the effects of the pandemic.
- The Internet is the major source of information about AQ in Abuja and Enugu (mean scores: 2.04 in Abuja and 2.06 in Enugu).
- Action on proper waste disposal was identified by residents as the most highly ranked option to reduce PAQ (mean scores: 1.54 in Abuja and 1.52 in Enugu).
- Residents considered PAQ an issue for the government but were unwilling to pay the government to manage PAQ.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Ambient (Outdoor) Air Pollution. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 19 October 2022).
- European Environment Agency. Europe’s Air Quality Status. 2022. Available online: https://www.eea.europa.eu//publications/status-of-air-quality-in-Europe-2022 (accessed on 19 October 2022).
- Word Health Organization. Air Pollution: Impacts. 2022. Available online: https://www.who.int/health-topics/air-pollution#tab=tab_2 (accessed on 28 October 2022).
- Chukwu, T.M.; Morse, S.; Murphy, R. Poor Air Quality in Urban Settings: A Comparison of Perceptual Indicators, Causes and Management in Two Cities. Sustainability 2022, 14, 1438. [Google Scholar] [CrossRef]
- Chukwu, T.M.; Morse, S.; Murphy, R.J. Spatial Analysis of Air Quality Assessment in Two Cities in Nigeria: A Comparison of Perceptions with Instrument-Based Methods. Sustainability 2022, 14, 5403. [Google Scholar] [CrossRef]
- Ramírez, A.S.; Ramondt, S.; van Bogart, K.; Perez-Zuniga, R. Public Awareness of Air Pollution and Health Threats: Challenges and Opportunities for Communication Strategies to Improve Environmental Health Literacy. J. Health Commun. 2019, 24, 75–83. [Google Scholar] [CrossRef]
- Benney, T.M.; Cantwell, D.; Singer, P.; Derhak, L.; Bey, S.; Saifee, Z. Understanding perceptions of health risk and behavioral responses to air pollution in the state of utah (USA). Atmosphere 2021, 12, 1373. [Google Scholar] [CrossRef]
- Noël, C.; Vanroelen, C.; Gadeyne, S. Qualitative research about public health risk perceptions on ambient air pollution. A review study. In SSM—Population Health; Elsevier Ltd.: Amsterdam, The Netherlands, 2021; Volume 15. [Google Scholar] [CrossRef]
- Ammons, S.; Aja, H.; Ghazarian, A.A.; Lai, G.Y.; Ellison, G.L. Perception of worry of harm from air pollution: Results from the Health Information National Trends Survey (HINTS). BMC Public Health 2022, 22, 1254. [Google Scholar] [CrossRef]
- McCarron, A.; Semple, S.; Braban, C.F.; Swanson, V.; Gillespie, C.; Price, H.D. Public engagement with air quality data: Using health behaviour change theory to support exposure-minimising behaviours. J. Expo. Sci. Environ. Epidemiol. 2022, 1–11. [Google Scholar] [CrossRef]
- Huang, W.; Hu, M. Estimation of the Impact of Traveler Information Apps on Urban Air Quality Improvement. Engineering 2018, 4, 224–229. [Google Scholar] [CrossRef]
- Abubakar, I.; Dalglish, S.L.; Angell, B.; Sanuade, O.; Abimbola, S.; Adamu, A.L.; Adetifa, I.M.; Colbourn, T.; Ogunlesi, A.O.; Onwujekwe, O.; et al. The Lancet Nigeria Commission: Investing in health and the future of the nation. Lancet 2022, 399, 1155–1200. [Google Scholar] [CrossRef]
- Abah, V.O. Poor Health Care Access in Nigeria: A Function of Fundamental Misconceptions and Misconstruction of the Health System. Healthc. Access 2022, 1–8. [Google Scholar] [CrossRef]
- Tijani, B.; Jaiyeola, T.; Oladejo, B.; Kassam, Z. Improving Data Integrity in Public Health: A Case Study of an Outbreak Management System in Nigeria. Glob. Health Sci. Pract. 2021, 9, S226–S233. [Google Scholar] [CrossRef]
- Fuller, R.; Landrigan, P.J.; Balakrishnan, K.; Bathan, G.; Bose-O’Reilly, S.; Brauer, M.; Caravanos, J.; Chiles, T.; Cohen, A.; Corra, L.; et al. Pollution and health: A progress update. Lancet Planet. Health 2022, 6, e535–e547. [Google Scholar] [CrossRef]
- Bourdrel, T.; Bind, M.A.; Béjot, Y.; Morel, O.; Argacha, J.F. Cardiovascular effects of air pollution. Arch. Cardiovasc. Dis. 2017, 110, 634–642. [Google Scholar] [CrossRef]
- Lee, K.K.; Miller, M.R.; Shah, A.S.V. Air Pollution and Stroke. J. Stroke 2018, 20, 2. [Google Scholar] [CrossRef]
- Lemprière, S. Air pollution linked to multiple sclerosis and stroke. Nat. Rev. Neurol. 2020, 16, 127. [Google Scholar] [CrossRef]
- Manisalidis, I.; Stavropoulou, E.; Stavropoulos, A.; Bezirtzoglou, E. Environmental and Health Impacts of Air Pollution: A Review. Front. Public Health 2020, 8, 14. [Google Scholar] [CrossRef]
- Roberts, W. Air pollution and skin disorders. Int. J. Women’s Dermatol. 2021, 7, 91–97. [Google Scholar] [CrossRef]
- Lin, C.C.; Chiu, C.C.; Lee, P.Y.; Chen, K.J.; He, C.X.; Hsu, S.K.; Cheng, K.C. The Adverse Effects of Air Pollution on the Eye: A Review. Int. J. Environ. Res. Public Health 2022, 19, 1186. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Yang, B.; Liu, P.; Zhang, J.; Liu, Y.; Yao, Y.; Lu, Y. The longitudinal relationship between exposure to air pollution and depression in older adults. Int. J. Geriatr. Psychiatry 2020, 35, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Environment Protection Agency. Research on Health Effects from Air Pollution. 2022. Available online: https://www.epa.gov/air-research/research-health-effects-air-pollution (accessed on 27 October 2022).
- Badeenezhad, A.; Baghapour, M.A.; Azhdarpoor, A.; Keshavarz, M.; Amrane, A.; Goudarzi, G.; Hoseini, M. The effects of short-term exposure to selected heavy metals carried by airborne fine particles on neural biomarkers during dust storms. Hum. Ecol. Risk Assess. Int. J. 2020, 27, 1309–1323. [Google Scholar] [CrossRef]
- United Nations Environment Programme. How is Air Quality Measured? 2022. Available online: https://www.unep.org/news-and-stories/story/how-air-quality-measured (accessed on 19 October 2022).
- Ngo, N.; Kokoyo, S.; Klopp, J. Why participation matters for air quality studies: Risk perceptions, understandings of air pollution and mobilization in a poor neighborhood in Nairobi, Kenya. Public Health 2017, 142, 177–185. [Google Scholar] [CrossRef]
- Wu, X.; Nethery, R.; Sabath, B.; Braun, D.; Dominici, F. Exposure to air pollution and COVID-19 mortality in the United States. ISEE Conf. Abstr. 2020, 1, 2–5. [Google Scholar] [CrossRef]
- Petroni, M.; Hill, D.; Younes, L.; Barkman, L.; Howard, S.; Howell, I.B.; Mirowsky, J.; Collins, M.B. Hazardous air pollutant exposure as a contributing factor to COVID-19 mortality in the United States. Environ. Res. Lett. 2020, 15, 0940a9. [Google Scholar] [CrossRef]
- Xu, J.; Chi, C.S.F.; Zhu, K. Concern or apathy: The attitude of the public toward urban air pollution. J. Risk Res. 2017, 20, 482–498. [Google Scholar] [CrossRef]
- Reames, T.G.; Bravo, M.A. People, place and pollution: Investigating relationships between air quality perceptions, health concerns, exposure, and individual- and area-level characteristics. Environ. Int. 2019, 122, 244–255. [Google Scholar] [CrossRef] [PubMed]
- Jurek, M. Communicating Air Quality to the Public as a Tool to Raise Awareness of Air Pollution Issues. Geographica 2006, 39, 31. Available online: https://geography.upol.cz/soubory/vyzkum/aupo/Acta-39/Acta-39-03.pdf. (accessed on 25 October 2022).
- Qian, X.; Xu, G.; Li, L.; Shen, Y.; He, T.; Liang, Y.; Yang, Z.; Zhou, W.W.; Xu, J. Knowledge and perceptions of air pollution in Ningbo, China. BMC Public Health 2016, 16, 1–7. [Google Scholar] [CrossRef]
- Al-Shidi, H.K.; Ambusaidi, A.K.; Sulaiman, H. Public awareness, perceptions and attitudes on air pollution and its health effects in Muscat, Oman. J. Air Waste Manag. Assoc. 2021, 71, 1159–1174. [Google Scholar] [CrossRef]
- Saptutyningsih, E.; Paripurna Kamiel, B. Public Awareness of Air Pollution and Mitigation of Its Risk. J. War. LPM 2022, 25, 55–63. Available online: http://journals.ums.ac.id/index.php/warta (accessed on 10 December 2022).
- Environment Protection Agency. Actions You Can Take to Reduce Air Pollution. 2022. Available online: https://www3.epa.gov/region1/airquality/reducepollution.html (accessed on 27 October 2022).
- Minnesota Pollution Control Agency. What Can You Do about Air Pollution. 2022. Available online: https://www.pca.state.mn.us/news-and-stories/what-you-can-do-about-air-pollution (accessed on 11 November 2022).
- Muindi, K.; Egondi, T.; Kimani-Murage, E.; Rocklov, J.; Ng, N. “We are used to this”: A qualitative assessment of the perceptions of and attitudes towards air pollution amongst slum residents in Nairobi. BMC Public Health 2014, 14, 1–9. [Google Scholar] [CrossRef] [PubMed]
- United Nations Population Fund. World Population Dashboard Nigeria. 2022. Available online: https://www.unfpa.org/data/world-population/NG (accessed on 26 October 2022).
- World Bank Urban Development. 2020. Available online: https://www.worldbank.org/en/topic/urbandevelopment/overview#1 (accessed on 26 October 2022).
- Macrotrends. Abuja, Nigeria Metro Area Population 1950–2022. 2022. Available online: https://www.macrotrends.net/cities/21976/abuja/population#:~:text=The%20current%20metro%20area%20population,a%205.91%25%20increase%20from%202019 (accessed on 26 October 2022).
- Population Stat. Abuja, Nigeria Population. 2022. Available online: https://populationstat.com/nigeria/abuja (accessed on 26 October 2022).
- Ayegba, A.; Yusuf, Y.; Simeon, A.U.; Justin, I.O.; Augustine, O.E.; Suleiman, A.O.; Joshua, A.; Chioma, O.R. A Study of the Daily Weather Variation of Abuja, North Central, Nigeria. 2019. Available online: https://www.ijeas.org/download_data/IJEAS0608032.pdf (accessed on 26 October 2022).
- Macrotrends. Enugu, Nigeria Metro Area Population 1950–2022. 2022. Available online: https://www.macrotrends.net/cities/21986/enugu/population (accessed on 26 October 2022).
- Okwu-Delunzu, V.U.; Oweifighe, W.J.; Ugochukwu, U.C. Assessment of air quality levels in heavy traffic areas in Enugu urban, Nigeria. In Monograph of Atmospheric Research; Centre for Atmospheric Research: Boulder, CO, USA, 2018; Available online: https://carnasrda.com/wp-content/uploads/2019/06/Okwu-et-al.pdf (accessed on 3 November 2022).
- Agu, A.; Tukur, K.; Omede, H. An Assessment of Heatwave Impact in Enugu Metropolis of Enugu State. 2020. Available online: https://www.researchgate.net/publication/346665778_An_Assessment_of_Heatwave_Impact_in_Enugu_Metropolis_of_Enugu_State (accessed on 27 December 2022).
- Federal Ministry of Youths and Sports. National Youth Policy. Enhancing Youth Development and Participation in the Context of Sustainable Development. 2019. Available online: https://www.prb.org/wp-content/uploads/2020/06/Nigeria-National-Youth-Policy-2019-2023.pdf (accessed on 26 October 2022).
- Evans, G.W.; Jacobs, S.V.; Frager, N.B. Adaptation to air pollution. J. Environ. Psychol. 1982, 2, 99–108. [Google Scholar] [CrossRef]
- Wiedmaier, B. Post Hoc Tests. In The SAGE Encyclopedia of Communication Research Methods; SAGE: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Xia, Y. Correlation, and association analyses in microbiome study integrating multiomics in health and disease. Prog. Mol. Biol.Transl. Sci. 2020, 171, 309–491. [Google Scholar] [PubMed]
- Okobia, E.L. Carbon Monoxide: Its impacts on human health in Abuja, Nigeria. 2015. Available online: https://www.researchgate.net/publication/276278580_Carbon_Monoxide_Its_impacts_on_human_health_in_Abuja_Nigeria (accessed on 20 October 2022).
- Emodi, E.E. Environmental quality of Enugu, Nigeria as impacted by the primary air pollutants in the area. Int. J. Environ. Pollut. Res. 2020, 8, 1–20. [Google Scholar]
- Andersen, Z.J.; Hvidberg, M.; Jensen, S.S.; Ketzel, M.; Loft, S.; Sørensen, M.; Tjønneland, A.; Overvad, K.; Raaschou-Nielsen, O. Chronic obstructive pulmonary disease and long-term exposure to traffic-related air pollution: A cohort study. Am. J. Respir. Crit. Care Med. 2011, 183, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Ujunwa, F.; Ezeonu, C. Risk factors for acute respiratory tract infections in under-five children in Enugu Southeast Nigeria. Ann. Med. Health Sci. Res. 2014, 4, 95. [Google Scholar] [CrossRef]
- Chukwu, M.N.; Ubosi, N.I. Impact of cement dust pollution on respiratory systems of Lafarge cement workers, Ewekoro, Ogun State, Nigeria. Glob. J. Pure Appl. Sci. 2016, 22, 1. [Google Scholar] [CrossRef]
- Mannucci, P.M.; Franchini, M. Health effects of ambient air pollution in developing countries. Int. J. Environ. Res. Public Health 2017, 14, 1048. [Google Scholar] [CrossRef] [PubMed]
- Aliyu, Y.A.; Botai, J.O. An exposure appraisal of outdoor air pollution on the respiratory well-being of a developing city population. J. Epidemiol. Glob. Health 2018, 8, 91–100. [Google Scholar] [CrossRef]
- Patella, V.; Florio, G.; Magliacane, D.; Giuliano, A.; Crivellaro, M.A.; Bartolomeo, D.; Genovese, A.; Palmieri, M.; Postiglione, A.; Ridolo, E.; et al. Urban air pollution and climate change: “The Decalogue: Allergy Safe Tree” for allergic and respiratory diseases care. Clin. Mol. Allergy 2018, 16, 1. [Google Scholar] [CrossRef]
- Sweileh, W.M.; Al-Jabi, S.W.; Zyoud, S.H.; Sawalha, A.F. Outdoor air pollution and respiratory health: A bibliometric analysis of publications in peer-reviewed journals (1900–2017). Multidiscip. Respir. Med. 2018, 13, 15. [Google Scholar] [CrossRef]
- Zakaria, M.F.; Ezani, E.; Hassan, N.; Ramli, N.A.; Wahab, M.I.A. Traffic-related Air Pollution (TRAP), Air Quality Perception and Respiratory Health Symptoms of Active Commuters in a University Outdoor Environment. IOP Conf. Ser. Earth Environ. Sci. 2019, 228, 012017. [Google Scholar] [CrossRef]
- De Marco, A.; Proietti, C.; Anav, A.; Ciancarella, L.; D’Elia, I.; Fares, S.; Fornasier, M.F.; Fusaro, L.; Gualtieri, M.; Manes, F.; et al. Impacts of air pollution on human and ecosystem health, and implications for the National Emission Ceilings Directive: Insights from Italy-NC-ND. Environ. Int. 2019, 125, 320–333. [Google Scholar] [CrossRef]
- Khaniabadi, Y.O.; Sicard, P.; Takdastan, A.; Hopke, P.K.; Taiwo, A.M.; Khaniabadi, F.O.; de Marco, A.; Daryanoosh, M. Mortality and morbidity due to ambient air pollution in Iran. Clin. Epidemiol. Glob. Health 2019, 7, 222–227. [Google Scholar] [CrossRef]
- Finkelman, R.B.; Wolfe, A.; Hendryx, M.S. The future environmental and health impacts of coal. Energy Geosci. 2021, 2, 99–112. [Google Scholar] [CrossRef]
- Ventriglio, A.; Bellomo, A.; di Gioia, I.; di Sabatino, D.; Favale, D.; de Berardis, D.; Cianconi, P. Environmental pollution and mental health: A narrative review of literature. CNS Spectr. 2021, 26, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Niu, Z.; Liu, F.; Yu, H.; Wu, S.; Xiang, H. Association between exposure to ambient air pollution and hospital admission, incidence, and mortality of stroke: An updated systematic review and meta-analysis of more than 23 million participants. Environ. Health Prev. Med. 2021, 26, 15. [Google Scholar] [CrossRef] [PubMed]
- Adams, D.R.; Ajmani, G.S.; Pun, V.C.; Wroblewski, K.E.; Kern, D.W.; Schumm, L.P.; McClintock, M.K.; Suh, H.H.; Pinto, J.M. Nitrogen dioxide pollution exposure is associated with olfactory dysfunction in older US adults. Int. Forum Allergy Rhinol. 2016, 6, 1245. [Google Scholar] [CrossRef]
- Ma, T.; Yazdi, M.D.; Schwartz, J.; Réquia, W.J.; Di, Q.; Wei, Y.; Chang, H.H.; Vaccarino, V.; Liu, P.; Shi, L. Long-term air pollution exposure and incident stroke in American older adults: A national cohort study. Glob. Epidemiol. 2022, 4, 100073. [Google Scholar] [CrossRef]
- Miller, K.A.; Siscovick, D.S.; Sheppard, L.; Shepherd, K.; Sullivan, J.H.; Anderson, G.L.; Kaufman, J.D. Long-Term Exposure to Air Pollution and Incidence of Cardiovascular Events in Women. N. Engl. J. Med. 2007, 356, 447–458. [Google Scholar] [CrossRef]
- Brunekreef, B.; Downwar, G.; Forastiere, F.; Gehring, U.; Heederik, D.J.; Hoek, G.; Koopmans, M.P.; Smit, L.A.; Vermeulen, R.C. Air pollution and COVID-19. 2021. Available online: http://www.europarl.europa.eu/supporting-analyses (accessed on 26 October 2021).
- Bourdrel, T.; Annesi-Maesano, I.; Alahmad, B.; Maesano, C.N.; Bind, M.A. The impact of outdoor air pollution on COVID-19: A review of evidence from in vitro, animal, and human studies. Eur. Respir. Rev. 2021, 30, 200242. [Google Scholar] [CrossRef]
- Ali, N.; Fariha, K.A.; Islam, F.; Mishu, M.A.; Mohanto, N.C.; Hosen, M.J.; Hossain, K. Exposure to air pollution and COVID-19 severity: A review of current insights, management, and challenges. Integr. Environ. Assess. Manag. 2021, 17, 1114–1122. [Google Scholar] [CrossRef]
- Ogunjo, S.; Olaniyan, O.; Olusegun, C.F.; Kayode, F.; Okoh, D.; Jenkins, G. The Role of Meteorological Variables and Aerosols in the Transmission of COVID-19 during Harmattan Season. GeoHealth 2022, 6, e2021GH000521. [Google Scholar] [CrossRef] [PubMed]
- Pereira, A.; Patrício, B.; Fonte, F.; Marques, S.; Reis, C.I.; Maximiano, M. Collecting information about air quality using smartphones. Procedia Comput. Sci. 2018, 138, 33–40. [Google Scholar] [CrossRef]
- Abulude, F.O. Right and Cheap Information on Air Quality: The Cases of Real-time Air Quality Index Monitors (Satellite and Phone apps). Acad. Lett. 2021, 2, 3401. [Google Scholar] [CrossRef]
- Wang, S.; Paul, M.J.; Dredze, M. Social media as a sensor of air quality and public response in China. J. Med. Internet Res. 2015, 17, e22. [Google Scholar] [CrossRef]
- Charitidis, P.; Papadopoulos, S.; Apostolidis, L. Social media monitoring tools for air quality accounts. In Proceedings of the IEEE/WIC/ACM International Conference on Web Intelligence-Companion Volume, Thessaloniki, Greece, 17 October 2019. [Google Scholar] [CrossRef]
- Wang, J.; Jia, Y. Social media’s influence on air quality improvement: Evidence from China. J. Clean. Prod. 2021, 298, 126769. [Google Scholar] [CrossRef]
- Chang, F.J.; Ashfold, M.J. Public perceptions of air pollution and its health impacts in Greater Kuala Lumpur. IOP Conf. Ser. Earth Environ. Sci. 2020, 489, 012027. [Google Scholar] [CrossRef]
- Verma, R.; Vinoda, K.S.; Papireddy, M.; Gowda, A.N.S. Toxic Pollutants from Plastic Waste- A Review. Procedia Environ. Sci. 2016, 35, 701–708. [Google Scholar] [CrossRef]
- Sonibare, O.O.; Adeniran, J.A.; Bello, I.S. Landfill air and odour emissions from an integrated waste management facility. J. Environ. Health Sci. Eng. 2019, 17, 13. [Google Scholar] [CrossRef]
- Okedere, O.B.; Olalekan, A.P.; Fakinle, B.S.; Elehinafe, F.B.; Odunlami, O.A.; Sonibare, J.A. Urban air pollution from the open burning of municipal solid waste. Environ. Qual. Manag. 2019, 28, 67–74. [Google Scholar] [CrossRef]
- World Health Organization. Solid Waste Management, Air Pollution and Health. 2021. Available online: https://www.who.int/publications/i/item/WHO-HEP-ECH-AQH-2021.8 (accessed on 27 October 2022).
- Pratap, C.M.; Garg, V. Causes, Consequences and Control of Air Pollution. 2013. Available online: https://www.researchgate.net/publication/279202084 (accessed on 7 November 2022).
- International Energy Agency. Energy and Air Pollution—World Energy Outlook 2016 Special Report. 2016. Available online: www.iea.org/t&c/ (accessed on 7 November 2022).
- European Environment Agency. How Can I Reduce Air Pollution? 2017. Available online: https://www.eea.europa.eu/themes/air/air-quality/more-about-air-pollutants/ozone-1/whatcanIdo/avoid-ozone-pollution (accessed on 7 November 2022).
- Department for Environment Food and Rural Affairs. Clean air strategy 2019. 2019. Available online: https://www.gov.uk/government/publications/clean-air-strategy-2019 (accessed on 7 November 2022).









| Characteristic | Abuja (N = 137) | Enugu (N = 125) |
|---|---|---|
| Gender | ||
| Male | 76 (55%) | 63 (50%) |
| Female | 61 (45%) | 62 (50%) |
| Age (cohort) | ||
| 18–34 years | 61 (45%) | 60 (45%) |
| ≥35 years | 76 (55%) | 65 (55%) |
Average monthly income ( ) ) | ||
| 0–50,000 | 57 (42%) | 68 (54%) |
| 51,000–100,000 | 24 (18%) | 39 (31%) |
| ≥101,000 | 56 (40%) | 18 (15%) |
| Highest education qualification | ||
| ≥Secondary/equivalent | 28 (21%) | 25 (20%) |
| Bachelor/diploma or equivalent | 59 (43%) | 78 (62%) |
| PhD/master’s or equivalent | 50 (36%) | 22 (18%) |
| Main occupation | ||
| Unemployed | 27 (19%) | 21 (17%) |
| Employed (wage) | 93 (69%) | 79 (63%) |
| Self-employed | 17 (12%) | 25 (20%) |
| The main modes of transportation used | ||
| Walking/cycling | 18 (13%) | 5 (4%) |
| Taxi | 55 (40%) | 46 (37%) |
| Public mass transit | 8 (6%) | 52 (41%) |
| Personal car | 56 (41%) | 22 (18%) |
| Likert Scale Scores | |||||
|---|---|---|---|---|---|
| Questions | 1 | 2 | 3 | 4 | 5 |
| Health impacts of PAQ | Strongly agree | Agree | Do not know | Disagree | Strongly disagree |
| Age group most vulnerable impacts of PAQ | Badly impacted | Well impacted | Slightly impacted | No impact | Do not know |
| Gender most vulnerable impacts of PAQ | Male | Female | Do not know | ||
| Does PAQ worsen COVID-19 | Yes | No | Do not know | ||
| Does PAQ increase the chance of COVID-19 infection | Yes | No | Do not know | ||
| Health impact of PAQ in the past year | Very affected | Moderately affected | Slightly affected | Not affected | Do not know |
| Sources of information on AQ | Extremely important | Very important | Moderately important | Slightly important | Not at all important |
| Individual actions for clean air | Strongly agree | Agree | Neutral | Disagree | Strongly disagree |
| Health Impacts of PAQ | Cities | Gender | Age | Income | Education | Occupation | Transportation |
|---|---|---|---|---|---|---|---|
| Respiratory diseases | Abuja | 2.728 | 6.524 | 4.265 | 3.858 | 4.205 | 12.568 ** |
| Enugu | 5.456 | 8.251 | 1.528 | 11.159 * | 10.676 * | 2.553 | |
| Eye/skin problem | Abuja | 2.053 | 3.660 | 2.092 | 4.088 | 1.360 | 3.463 |
| Enugu | 4.435 | 9.414 * | 2.637 | 5.985 | 2.335 | 2.854 | |
| Heart diseases | Abuja | 2.551 | 7.748 | 11.406 * | 7.198 | 5.012 | 6.822 |
| Enugu | 1.643 | 4.754 | 2.675 | 11.362 * | 3.599 | 1.345 | |
| Low immune system | Abuja | 11.659 * | 3.505 | 9.720 * | 7.478 | 1.294 | 6.510 |
| Enugu | 1.822 | 3.095 | 1.058 | 7.452 | 2.072 | 2.773 | |
| Cancer | Abuja | 2.299 | 2.679 | 3.167 | 0.841 | 0.744 | 0.548 |
| Enugu | 4.502 | 6.772 | 4.288 | 9.798 * | 1.850 | 2.236 | |
| Depression | Abuja | 1.878 | 2.333 | 3.442 | 2.044 | 2.987 | 2.698 |
| Enugu | 7.806 | 3.999 | 2.175 | 4.920 | 5.781 | 3.030 |
| Age Group Most Affected by PAQ | Cities | Gender | Age | Income | Education | Occupation | Transportation |
|---|---|---|---|---|---|---|---|
| Less than 18 years | Abuja | 1.418 | 2.364 | 5.809 | 2.921 | 3.996 | 7.540 |
| Enugu | 2.153 | 7.362 | 2.828 | 8.676 | 8.917 | 4.913 | |
| 18–24 | Abuja | 0.871 | 3.537 | 12.083 * | 9.264 | 0.861 | 5.234 |
| Enugu | 2.997 | 5.787 | 3.537 | 1.670 | 5.933 | 3.371 | |
| 25–34 | Abuja | 0.703 | 3.061 | 6.403 | 9.087 | 1.379 | 9.140 |
| Enugu | 0.516 | 9.120 | 3.222 | 5.028 | 3.546 | 2.806 | |
| 35–44 | Abuja | 1.771 | 6.026 | 9.401 | 5.627 | 4.030 | 5.337 |
| Enugu | 2.813 | 12.397 * | 2.793 | 4.981 | 2.576 | 2.766 | |
| 45–54 | Abuja | 3.167 | 6.052 | 11.413 * | 2.884 | 1.437 | 3.978 |
| Enugu | 2.276 | 3.741 | 1.371 | 4.582 | 4.522 | 9.145 | |
| 55–64 | Abuja | 1.928 | 10.528 * | 12.546 ** | 5.217 | 1.235 | 2.574 |
| Enugu | 2.480 | 2.382 | 2.060 | 4.051 | 2.458 | 4.736 | |
| 65–74 | Abuja | 6.593 | 7.012 | 8.087 | 2.556 | 10.855 * | 12.172 * |
| Enugu | 1.694 | 3.863 | 2.170 | 5.122 | 5.825 | 5.061 | |
| 75 years and above | Abuja | 1.961 | 8.049 | 3.336 | 11.820 * | 2.972 | 6.049 |
| Enugu | 3.452 | 0.856 | 2.129 | 2.127 | 2.811 | 1.733 |
| Cities | Gender | Age | Income | Education | Occupation | Transportation |
|---|---|---|---|---|---|---|
| Abuja | 2.818 | 1.382 | 4.405 | 1.153 | 0.359 | 2.336 |
| Enugu | 8.840 ** | 1.572 | 0.297 | 0.331 | 1.653 | 1.359 |
| Cities | Gender | Age | Income | Education | Occupation | Transportation |
|---|---|---|---|---|---|---|
| Abuja | 0.835 | 5.057 | 3.423 | 5.216 | 6.017 | 6.591 |
| Enugu | 17.296 ** | 12.077 * | 2.637 | 9.198 * | 1.293 | 5.527 |
| Source of Information | Cities | Gender | Age | Income | Education | Occupation | Transportation |
|---|---|---|---|---|---|---|---|
| Internet | Abuja | 3.632 | 2.623 | 4.823 | 0.527 | 2.568 | 3.251 |
| Enugu | 3.527 | 12.022 * | 3.276 | 6.258 | 5.036 | 2.649 | |
| Television | Abuja | 5.539 | 6.706 | 6.019 | 7.860 | 0.257 | 4.265 |
| Enugu | 3.296 | 5.632 | 0.496 | 9.278* | 8.598 | 10.550 * | |
| Social media | Abuja | 11.122 * | 8.738 | 3.368 | 2.022 | 2.683 | 7.484 |
| Enugu | 2.753 | 18.540 ** | 4.123 | 5.762 | 12.053 ** | 6.745 | |
| Radio | Abuja | 1.245 | 10.736 * | 2.288 | 0.994 | 1.748 | 1.153 |
| Enugu | 2.076 | 1.912 | 4.820 | 10.640 * | 8.633 | 4.027 | |
| Friends | Abuja | 5.670 | 9.319 * | 7.111 | 6.136 | 5.705 | 8.400 |
| Enugu | 4.974 | 13.406 ** | 0.853 | 2.985 | 4.919 | 4.758 | |
| Newspapers | Abuja | 0.578 | 3.248 | 5.371 | 2.574 | 3.925 | 8.907 |
| Enugu | 2.617 | 4.874 | 3.245 | 1.847 | 6.326 | 5.421 | |
| Posters | Abuja | 11.695 * | 1.839 | 7.199 | 2.099 | 4.873 | 5.668 |
| Enugu | 5.067 | 10.389 * | 4.172 | 2.143 | 6.355 | 3.053 | |
| Leaflets | Abuja | 3.282 | 3.790 | 3.852 | 2.764 | 5.218 | 4.057 |
| Enugu | 1.796 | 5.337 | 1.875 | 2.967 | 5.204 | 1.002 | |
| Magazines | Abuja | 1.029 | 1.582 | 10.811 * | 6.174 | 3.307 | 5.629 |
| Enugu | 1.795 | 3.004 | 1.712 | 4.633 | 5.819 | 5.261 |
| Abuja | Enugu | ||||||
|---|---|---|---|---|---|---|---|
| Source of Information | Age Groups | Mean | SD | KW | Mean | SD | KW |
| Internet | 18–34 | 1.92 | 0.988 | 2.623 ns | 1.79 | 1.051 | 12.022 * |
| 35 and over | 2.13 | 1.215 | 2.31 | 1.139 | |||
| Television | 18–34 | 2.03 | 0.912 | 6.706 ns | 2.30 | 1.243 | 5.632 ns |
| 35 and over | 2.07 | 1.124 | 2.55 | 1.284 | |||
| Social media | 18–34 | 1.97 | 1.032 | 8.738 ns | 1.89 | 0.968 | 18.540 ** |
| 35 and over | 2.24 | 1.165 | 2.58 | 1.066 | |||
| Radio | 18–34 | 2.28 | 0.878 | 10.736 * | 2.51 | 1.260 | 1.912 ns |
| 35 and over | 2.22 | 1.207 | 2.50 | 1.182 | |||
| Friends | 18–34 | 2.49 | 1.043 | 9.319* | 2.44 | 1.162 | 13.406 ** |
| 35 and over | 2.47 | 1.270 | 3.03 | 1.098 | |||
| Newspapers | 18–34 | 2.75 | 1.150 | 3.248 ns | 2.75 | 1.299 | 4.874 ns |
| 35 and over | 2.71 | 1.335 | 3.22 | 1.240 | |||
| Posters | 18–34 | 3.00 | 1.270 | 1.839 ns | 3.02 | 1.335 | 10.389 * |
| 35 and over | 2.96 | 0.988 | 3.22 | 1.133 | |||
| Leaflets | 18–34 | 3.15 | 1.152 | 3.790 ns | 3.07 | 1.263 | 5.337 ns |
| 35 and over | 2.99 | 1.160 | 3.25 | 1.069 | |||
| Magazines | 18–34 | 3.15 | 1.263 | 1.582 ns | 3.25 | 1.274 | 3.004 ns |
| 35 and over | 3.04 | 1.270 | 3.53 | 1.221 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chukwu, T.M.; Morse, S.; Murphy, R.J. Perceived Health Impacts, Sources of Information and Individual Actions to Address Air Quality in Two Cities in Nigeria. Sustainability 2023, 15, 6124. https://doi.org/10.3390/su15076124
Chukwu TM, Morse S, Murphy RJ. Perceived Health Impacts, Sources of Information and Individual Actions to Address Air Quality in Two Cities in Nigeria. Sustainability. 2023; 15(7):6124. https://doi.org/10.3390/su15076124
Chicago/Turabian StyleChukwu, Timothy M., Stephen Morse, and Richard J. Murphy. 2023. "Perceived Health Impacts, Sources of Information and Individual Actions to Address Air Quality in Two Cities in Nigeria" Sustainability 15, no. 7: 6124. https://doi.org/10.3390/su15076124
APA StyleChukwu, T. M., Morse, S., & Murphy, R. J. (2023). Perceived Health Impacts, Sources of Information and Individual Actions to Address Air Quality in Two Cities in Nigeria. Sustainability, 15(7), 6124. https://doi.org/10.3390/su15076124








