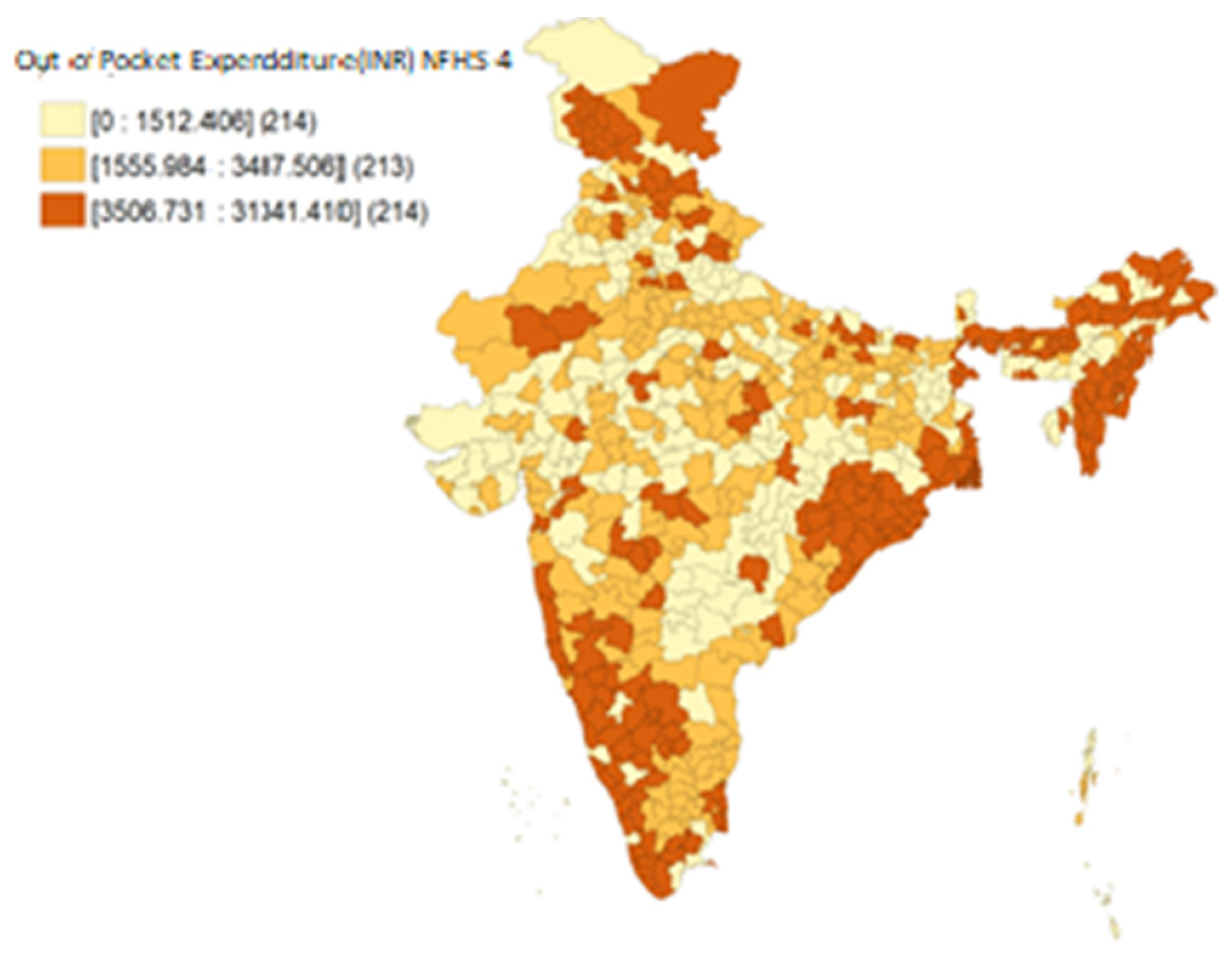
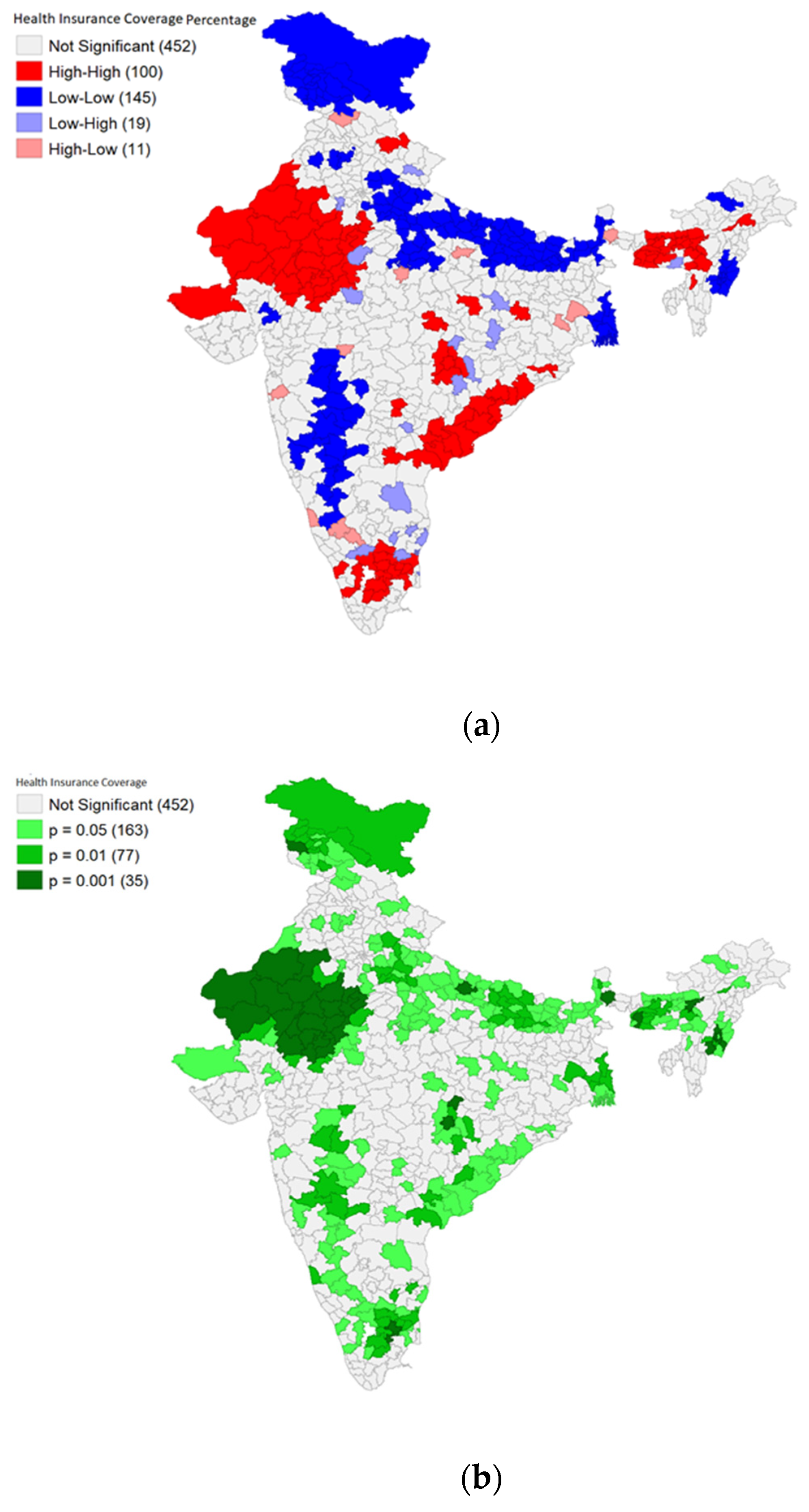
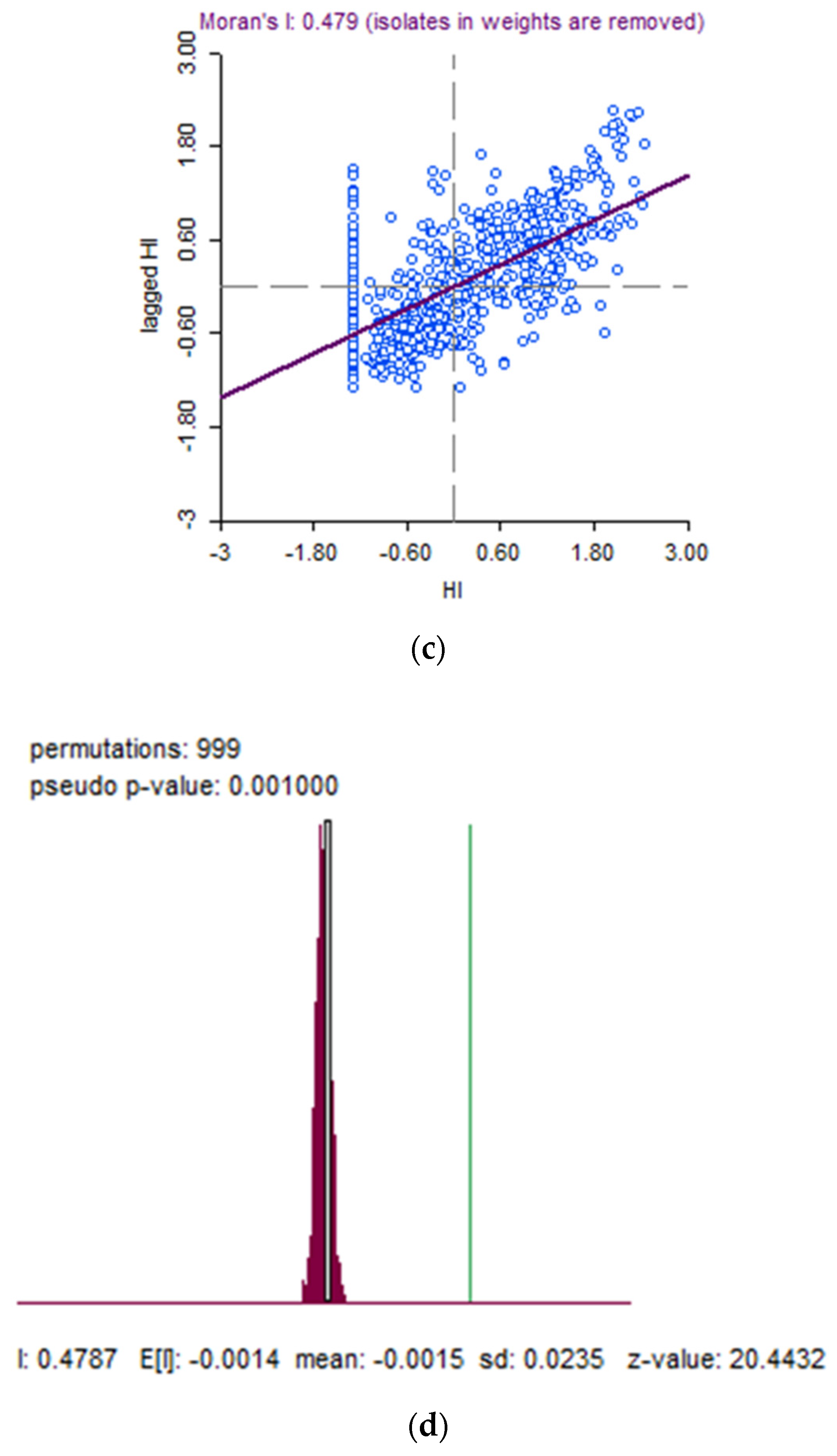
District-Level Patterns of Health Insurance Coverage and Out-of-Pocket Expenditure on Caesarean Section Deliveries in Public Health Facilities in India
Abstract
1. Introduction
2. Methodology
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Azam, M. Does social health insurance reduce financial burden? Panel data evidence from India. World Dev. 2018, 102, 1–17. [Google Scholar] [CrossRef]
- Dasgupta, R.; Nandi, S.; Kanungo, K.; Nundy, M.; Murugan, G.; Neog, R. What the good doctor said: A critical examination of design issues of the RSBY through provider perspectives in Chhattisgarh, India. Soc. Chang. 2013, 43, 227–243. [Google Scholar] [CrossRef]
- Furtado, K.M.; Raza, A.; Mathur, D.; Vaz, N.; Agrawal, R.; Shroff, Z.C. The trust and insurance models of healthcare purchasing in the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana in India: Early findings from case studies of two states. BMC Health Serv. Res. 2022, 22, 1056. [Google Scholar] [CrossRef] [PubMed]
- Hooda, S. Decoding Ayushman Bharat. Econ. Political Wkly. 2020, 55, 107–115. [Google Scholar]
- Karan, A.; Yip, W.; Mahal, A. Extending health insurance to the poor in India: An impact evaluation of Rashtriya Swasthya Bima Yojana on out of pocket spending for healthcare. Soc. Sci. Med. 2017, 181, 83–92. [Google Scholar] [CrossRef]
- Sen, A. Check Hospital Pulse Regularly to Detect Bogus Claims: Insurers Told. The Economic Times, 25 October 2010. [Google Scholar]
- TNN. Duplicate Cards, Fraudulent Users Pose Challenge to Rashtriya Swasthya Bima Yojana: Lucknow News-Times of India. The Times of India, 13 April 2013. [Google Scholar]
- Keralakaumudi Daily. Massive Fraud Under Ayushman Bharat Health Insurance Scheme; Doctor Couple Behind Racket Embezzling Money from Govt Using Fake Patients. Keralakaumudi Daily, 29 August 2022. [Google Scholar]
- Saraswathy, M. Nearly 3000 fraud cases detected under Ayushman Bharat Health Insurance Scheme. Moneycontrol, 12 November 2019. [Google Scholar]
- Bureau, M.D. 23000 fraud transactions done by hospitals under Ayushman Bharat: Health Ministry Data. Medical Dialogues, 7 August 2022. [Google Scholar]
- Ghosh, A. 18,606 Fraudulent Hospital Transactions Found in Ayushman Bharat Insurance Scheme, Govt Tells rs. ThePrint, 5 April 2022. [Google Scholar]
- Has Ayushman Bharat delivered on its promises? IDR. India Development Review, 4 July 2022.
- Dash, A.; Mohanty, S.K. Do poor people in the poorer states pay more for healthcare in India? BMC Public Health 2019, 19, 1020. [Google Scholar] [CrossRef]
- Pandey, A.; Kumar, G.A.; Dandona, R.; Dandona, L. Variations in catastrophic health expenditure across the states of India: 2004 to 2014. PLoS ONE 2018, 13, e0205510. [Google Scholar] [CrossRef]
- Shahrawat, R.; Rao, K.D. Insured yet vulnerable: Out-of-pocket payments and India’s poor. Health Policy Plan. 2012, 27, 213–221. [Google Scholar] [CrossRef]
- Dwivedi, R.; Pradhan, J. Does affordability matter? Examining the trends and patterns in health care expenditure in India. Health Serv. Manag. Res. 2020, 33, 207–218. [Google Scholar] [CrossRef]
- Das, S.K.; Ladusingh, L. Why is the inpatient cost of dying increasing in India? PLoS ONE 2018, 13, e0203454. [Google Scholar] [CrossRef]
- Mohanty, S.K.; Dwivedi, L.K. Addressing data and methodological limitations in estimating catastrophic health spending and impoverishment in India, 2004–2018. Int. J. Equity Health 2021, 20, 85. [Google Scholar] [CrossRef] [PubMed]
- Selvaraj, S.; Farooqui, H.H.; Karan, A. Quantifying the financial burden of households’ out-of-pocket payments on medicines in India: A repeated cross-sectional analysis of National Sample Survey data, 1994–2014. BMJ Open 2018, 8, e018020. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Gupta, N.D. Targeting and effects of Rashtriya Swasthya Bima Yojana on access to care and financial protection. Econ. Political Wkly. 2017, 52, 61–70. [Google Scholar]
- A crisis of plenty: The poor in india have access to surgeries but not basic healthcare. Econ. Political Wkly. 2016, 51, 8. Available online: www.scopus.com (accessed on 19 October 2022).
- Peters, D.H.; Muraleedharan, V.R. Regulating India’s health services: To what end? What future? Soc. Sci. Med. 2008, 66, 2133–2144. [Google Scholar] [CrossRef]
- Betrán, A.P.; Ye, J.; Moller, A.B.; Zhang, J.; Gülmezoglu, A.M.; Torloni, M.R. The increasing trend in caesarean section rates: Global, regional and national estimates: 1990–2014. PLoS ONE 2016, 11, e0148343. [Google Scholar] [CrossRef]
- Dieleman, J.L.; Squires, E.; Bui, A.L.; Campbell, M.; Chapin, A.; Hamavid, H.; Horst, C.; Li, Z.; Matyasz, T.; Reynolds, A.; et al. Factors associated with increases in US health care spending, 1996–2013. JAMA 2017, 318, 1668–1678. [Google Scholar] [CrossRef] [PubMed]
- Niino, Y. The increasing cesarean rate globally and what we can do about it. Biosci. Trends 2011, 5, 139–150. [Google Scholar] [CrossRef]
- Bonu, S.; Bhushan, I.; Rani, M.; Anderson, I. Incidence and correlates of ‘catastrophic’maternal health care expenditure in India. Health Policy Plan. 2009, 24, 445–456. [Google Scholar] [CrossRef]
- Mohanty, S.K.; Kastor, A. Out-of-pocket expenditure and catastrophic health spending on maternal care in public and private health centres in India: A comparative study of pre and post national health mission period. Health Econ. Rev. 2017, 7, 31. [Google Scholar] [CrossRef] [PubMed]
- Storeng, K.T.; Baggaley, R.F.; Ganaba, R.; Ouattara, F.; Akoum, M.S.; Filippi, V. Paying the price: The cost and consequences of emergency obstetric care in Burkina Faso. Soc. Sci. Med. 2008, 66, 545–557. [Google Scholar] [CrossRef]
- He, Z.; Cheng, Z.; Wu, T.; Zhou, Y.; Chen, J.; Fu, Q.; Feng, Z. The costs and their determinant of cesarean section and vaginal delivery: An exploratory study in Chongqing Municipality, China. BioMed Res. Int. 2016, 2016, 5685261. [Google Scholar] [CrossRef]
- Hsia, R.Y.; Antwi, Y.A.; Weber, E. Analysis of variation in charges and prices paid for vaginal and caesarean section births: A cross-sectional study. BMJ Open 2014, 4, e004017. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Zaman, S. Costs of vaginal delivery and Caesarean section at a tertiary level public hospital in Islamabad, Pakistan. BMC Pregnancy Childbirth 2010, 10, 2. [Google Scholar] [CrossRef] [PubMed]
- Althabe, F.; Sosa, C.; Belizán, J.M.; Gibbons, L.; Jacquerioz, F.; Bergel, E. Cesarean section rates and maternal and neonatal mortality in low-, medium-, and high-income countries: An ecological study. Birth 2006, 33, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Betrán, A.P.; Merialdi, M.; Lauer, J.A.; Bing-Shun, W.; Thomas, J.; Van Look, P.; Wagner, M. Rates of caesarean section: Analysis of global, regional and national estimates. Paediatr. Perinat. Epidemiol. 2007, 21, 98–113. [Google Scholar] [CrossRef]
- Molina, G.; Weiser, T.G.; Lipsitz, S.R.; Esquivel, M.M.; Uribe-Leitz, T.; Azad, T.; Shah, N.; Semrau, K.; Berry, W.R.; Gawande, A.A.; et al. Relationship between cesarean delivery rate and maternal and neonatal mortality. JAMA 2015, 314, 2263–2270. [Google Scholar] [CrossRef]
- Ronsmans, C.; Holtz, S.; Stanton, C. Socioeconomic differentials in caesarean rates in developing countries: A retrospective analysis. Lancet 2006, 368, 1516–1523. [Google Scholar] [CrossRef]
- World Health Organization. WHO Statement on Caesarean Section Rates; (No. WHO/RHR/15.02); World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Roberts, C.L.; Nippita, T.A. International caesarean section rates: The rising tide. Lancet Glob. Health 2015, 3, e241–e242. [Google Scholar] [CrossRef]
- Boatin, A.A.; Schlotheuber, A.; Betran, A.P.; Moller, A.B.; Barros, A.J.; Boerma, T.; Torloni, M.R.; Victora, C.G.; Hosseinpoor, A.R. Within country inequalities in caesarean section rates: Observational study of 72 low and middle income countries. BMJ 2018, 360, k55. [Google Scholar] [CrossRef]
- Kyu, H.H.; Shannon, H.S.; Georgiades, K.; Boyle, M.H. Caesarean delivery and neonatal mortality rates in 46 low-and middle-income countries: A propensity-score matching and meta-analysis of Demographic and Health Survey data. Int. J. Epidemiol. 2013, 42, 781–791. [Google Scholar] [CrossRef] [PubMed]
- Volpe, F.M. Correlation of Cesarean rates to maternal and infant mortality rates: An ecologic study of official international data. Rev. Panam. Salud Pública 2011, 29, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Lei, J.; Tan, H.; Walker, M.; Zhou, J.; Wen, S.W. Cesarean delivery for first pregnancy and neonatal morbidity and mortality in second pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011, 158, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Marshall, N.E.; Fu, R.; Guise, J.M. Impact of multiple cesarean deliveries on maternal morbidity: A systematic review. Am. J. Obstet. Gynecol. 2011, 205, 262.e1–262.e8. [Google Scholar] [CrossRef] [PubMed]
- Mi, J.; Liu, F. Rate of caesarean section is alarming in China. Lancet 2014, 383, 1463–1464. [Google Scholar] [CrossRef]
- Timor-Tritsch, I.E.; Monteagudo, A. Unforeseen consequences of the increasing rate of cesarean deliveries: Early placenta accreta and cesarean scar pregnancy. A review. Am. J. Obstet. Gynecol. 2012, 207, 14–29. [Google Scholar] [CrossRef]
- Mascarello, K.C.; Horta, B.L.; Silveira, M.F. Maternal complications and cesarean section without indication: Systematic review and meta-analysis. Revista Saude Publica 2017, 51, 105. [Google Scholar] [CrossRef]
- Souza, J.P.; Gülmezoglu, A.M.; Lumbiganon, P.; Laopaiboon, M.; Carroli, G.; Fawole, B.; Ruyan, P. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: The 2004–2008 WHO Global Survey on Maternal and Perinatal Health. BMC Med. 2010, 8, 71. [Google Scholar] [CrossRef]
- Vogel, J.P.; Betrán, A.P.; Vindevoghel, N.; Souza, J.P.; Torloni, M.R.; Zhang, J.; Tunçalp, Ö.; Mori, R.; Morisaki, N.; Ortiz-Panozo, E.; et al. Use of the Robson classification to assess caesarean section trends in 21 countries: A secondary analysis of two WHO multicountry surveys. Lancet Glob. Health 2015, 3, e260–e270. [Google Scholar] [CrossRef]
- Bangal, V.B.; Thorat, P.S.; Patel, N.H.; Borawake, S.K. Caesarean sections-are we doing right. IJBR 2012, 3, 281–284. [Google Scholar] [CrossRef]
- Feng, X.L.; Xu, L.; Guo, Y.; Ronsmans, C. Factors influencing rising caesarean section rates in China between 1988 and 2008. Bull. World Health Organ. 2012, 90, 30–39A. [Google Scholar] [CrossRef]
- Gould, J.B.; Davey, B.; Stafford, R.S. Socioeconomic differences in rates of cesarean section. N. Engl. J. Med. 1989, 321, 233–239. [Google Scholar] [CrossRef]
- Lin, H.C.; Xirasagar, S. Institutional factors in cesarean delivery rates: Policy and research implications. Obstet. Gynecol. 2004, 103, 128–136. [Google Scholar] [CrossRef]
- Leone, T.; Padmadas, S.S.; Matthews, Z. Community factors affecting rising caesarean section rates in developing countries: An analysis of six countries. Soc. Sci. Med. 2008, 67, 1236–1246. [Google Scholar] [CrossRef] [PubMed]
- Mazzoni, A.; Althabe, F.; Liu, N.H.; Bonotti, A.M.; Gibbons, L.; Sánchez, A.J.; Belizán, J.M. Women’s preference for caesarean section: A systematic review and meta-analysis of observational studies. BJOG Int. J. Obstet. Gynaecol. 2011, 118, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Pang, S.M.; Leung, D.T.; Leung, T.Y.; Lai, C.Y.; Lau, T.K.; Chung, T.K. Determinants of preference for elective caesarean section in Hong Kong Chinese pregnant women. Hong Kong Med. J. 2007, 13, 100. [Google Scholar] [PubMed]
- Sufang, G.; Padmadas, S.S.; Fengmin, Z.; Brown, J.J.; Stones, R.W. Delivery settings and caesarean section rates in China. Bull. World Health Organ. 2007, 85, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Zwecker, P.; Azoulay, L.; Abenhaim, H.A. Effect of fear of litigation on obstetric care: A nationwide analysis on obstetric practice. Am. J. Perinatol. 2011, 28, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Cavallaro, F.L.; Cresswell, J.A.; França, G.V.; Victora, C.G.; Barros, A.J.; Ronsmans, C. Trends in caesarean delivery by country and wealth quintile: Cross-sectional surveys in southern Asia and sub-Saharan Africa. Bull. World Health Organ. 2013, 91, 914–922D. [Google Scholar] [CrossRef] [PubMed]
- Neuman, M.; Alcock, G.; Azad, K.; Kuddus, A.; Osrin, D.; More, N.S.; Nair, N.; Tripathy, P.; Sikorski, C.; Saville, N.; et al. Prevalence and determinants of caesarean section in private and public health facilities in underserved South Asian communities: Cross-sectional analysis of data from Bangladesh, India and Nepal. BMJ Open 2014, 4, e005982. [Google Scholar] [CrossRef] [PubMed]
- Sreevidya, S.; Sathiyasekaran, B.W.C. High caesarean rates in Madras (India): A population-based cross sectional study. BJOG Int. J. Obstet. Gynaecol. 2003, 110, 106–111. [Google Scholar] [CrossRef]
- Khunpradit, S.; Tavender, E.; Lumbiganon, P.; Laopaiboon, M.; Wasiak, J.; Gruen, R.L. Non-clinical interventions for reducing unnecessary caesarean section. Cochrane Database Syst. Rev. 2011. [Google Scholar] [CrossRef] [PubMed]
- Althabe, F.; Belizán, J.M.; Villar, J.; Alexander, S.; Bergel, E.; Ramos, S.; Romero, M.; Donner, A.; Lindmark, G.; Langer, A.; et al. Mandatory second opinion to reduce rates of unnecessary caesarean sections in Latin America: A cluster randomised controlled trial. Lancet 2004, 363, 1934–1940. [Google Scholar] [CrossRef] [PubMed]
- Joe, W.; Perkins, J.M.; Kumar, S.; Rajpal, S.; Subramanian, S.V. Institutional delivery in India, 2004–2014: Unravelling the equity-enhancing contributions of the public sector. Health Policy Plan. 2018, 33, 645–653. [Google Scholar] [CrossRef]
- Singh, P.; Hashmi, G.; Swain, P.K. High prevalence of cesarean section births in private sector health facilities-analysis of district level household survey-4 (DLHS-4) of India. BMC Public Health 2018, 18, 613. [Google Scholar] [CrossRef]
- Vellakkal, S.; Reddy, H.; Gupta, A.; Chandran, A.; Fledderjohann, J.; Stuckler, D. A qualitative study of factors impacting accessing of institutional delivery care in the context of India’s cash incentive program. Soc. Sci. Med. 2017, 178, 55–65. [Google Scholar] [CrossRef]
- International Institute for Population Sciences. India National Family Health Survey NFHS-4 2015-16; Mumbai IIPS ICF; International Institute for Population Sciences: Deonar, Mumbai, 2017; pp. 1255–1259. [Google Scholar]
- Ghosh, S.; James, K.S. Levels and trends in caesarean births: Cause for concern? Econ. Political Wkly. 2010, 45, 19–22. [Google Scholar]
- Mishra, U.S.; Ramanathan, M. Delivery-related complications and determinants of caesarean section rates in India. Health Policy Plan. 2002, 17, 90–98. [Google Scholar] [CrossRef]
- Mohanty, S.K.; Panda, B.K.; Khan, P.K.; Behera, P. Out-of-pocket expenditure and correlates of caesarean births in public and private health centres in India. Soc. Sci. Med. 2019, 224, 45–57. [Google Scholar] [CrossRef]
- Trivedi, M.; Saxena, D.B. Third angle of RSBY: Service providers’ perspective to RSBY-operational issues in Gujarat. J. Fam. Med. Prim. Care 2013, 2, 169. [Google Scholar]
- Chowdhury, S.; Ramandeep, A.R.; Indrani, G. Ayushman Bharat Costs and Finances of the Prime Minister’s Jan Arogya Yojana. Project Report; Institute of Economic Growth: Delhi, India, 2019; Available online: https://fincomindia.nic.in/writereaddata/html_en_files/fincom15/StudyReports/Ayushman%20Bharat%20Costs%20and%20Finances.pdf (accessed on 23 October 2022).
- Tripathi, N.; Saini, S.K.; Prinja, S. Impact of Janani Shishu Suraksha Karyakaram on out-of-pocket expenditure among urban slum dwellers in northern India. India Pediatr. 2014, 51, 475–477. [Google Scholar] [CrossRef] [PubMed]
- Leone, T.; James, K.S.; Padmadas, S.S. The burden of maternal health care expenditure in India: Multilevel analysis of national data. Matern Child Health J. 2013, 17, 1622–1630. [Google Scholar] [CrossRef] [PubMed]
- Garg, C.C.; Pratheeba, J.; Negi, J. Utilisation of health facilities for childbirth and out-of-pocket expenditure impact of government policies. Econ. Political Wkly. 2018, 53, 53–61. [Google Scholar]
- Goli, S.; Rammohan, A. Out-of-pocket expenditure on maternity care for hospital births in Uttar Pradesh, India. Health Econ. Rev. 2018, 8, 5. [Google Scholar] [CrossRef]
- Issac, A.; Chatterjee, S.; Srivastava, A.; Bhattacharyya, S. Out of pocket expenditure to deliver at public health facilities in India: A cross sectional analysis. Reprod. Health 2016, 13, 99. [Google Scholar] [CrossRef] [PubMed]
- Horton, R.; Das, P. Indian health: The path from crisis to progress. Lancet 2011, 377, 181–183. [Google Scholar] [CrossRef]
- Goli, S.; Moradhvaj Rammohan, A.; Shruti Pradhan, J. High spending on maternity care in India: What are the factors explaining it? PLoS ONE 2016, 11, e0156437. [Google Scholar] [CrossRef]











Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamath, R.; Brand, H.; Nayak, N.; Lakshmi, V.; Verma, R.; Salins, P. District-Level Patterns of Health Insurance Coverage and Out-of-Pocket Expenditure on Caesarean Section Deliveries in Public Health Facilities in India. Sustainability 2023, 15, 4608. https://doi.org/10.3390/su15054608
Kamath R, Brand H, Nayak N, Lakshmi V, Verma R, Salins P. District-Level Patterns of Health Insurance Coverage and Out-of-Pocket Expenditure on Caesarean Section Deliveries in Public Health Facilities in India. Sustainability. 2023; 15(5):4608. https://doi.org/10.3390/su15054608
Chicago/Turabian StyleKamath, Rajesh, Helmut Brand, Nisha Nayak, Vani Lakshmi, Reena Verma, and Prajwal Salins. 2023. "District-Level Patterns of Health Insurance Coverage and Out-of-Pocket Expenditure on Caesarean Section Deliveries in Public Health Facilities in India" Sustainability 15, no. 5: 4608. https://doi.org/10.3390/su15054608
APA StyleKamath, R., Brand, H., Nayak, N., Lakshmi, V., Verma, R., & Salins, P. (2023). District-Level Patterns of Health Insurance Coverage and Out-of-Pocket Expenditure on Caesarean Section Deliveries in Public Health Facilities in India. Sustainability, 15(5), 4608. https://doi.org/10.3390/su15054608





