Retrofitting for Improving Indoor Air Quality and Energy Efficiency in the Hospital Building
Abstract
1. Introduction
- What retrofitting strategies are promising in improving indoor air quality in hospital buildings?
- What retrofitting strategies are promising in improving energy efficiency in hospital buildings?
- What challenges are experienced in facility attempts to embrace retrofitting?
- What measures are required to address existing challenges and enhance indoor quality and energy efficiency in hospitals in the future?
2. Energy Flows in Hospital Buildings
2.1. Energy-Saving Measures in Hospitals
- Hospital buildings can be refurbished by adopting the most efficient and advanced technical solutions (such as efficient energy components, building services, and new materials).
- Users of various facilities in the hospital, such as nurses, medical staff, patients, and administrators, could be made aware of inefficient practices. Thus, these shareholders need to be trained more on the efficient use of energy resources within their clinical or workplace settings.
2.2. Retrofitting Strategies in Hospitals
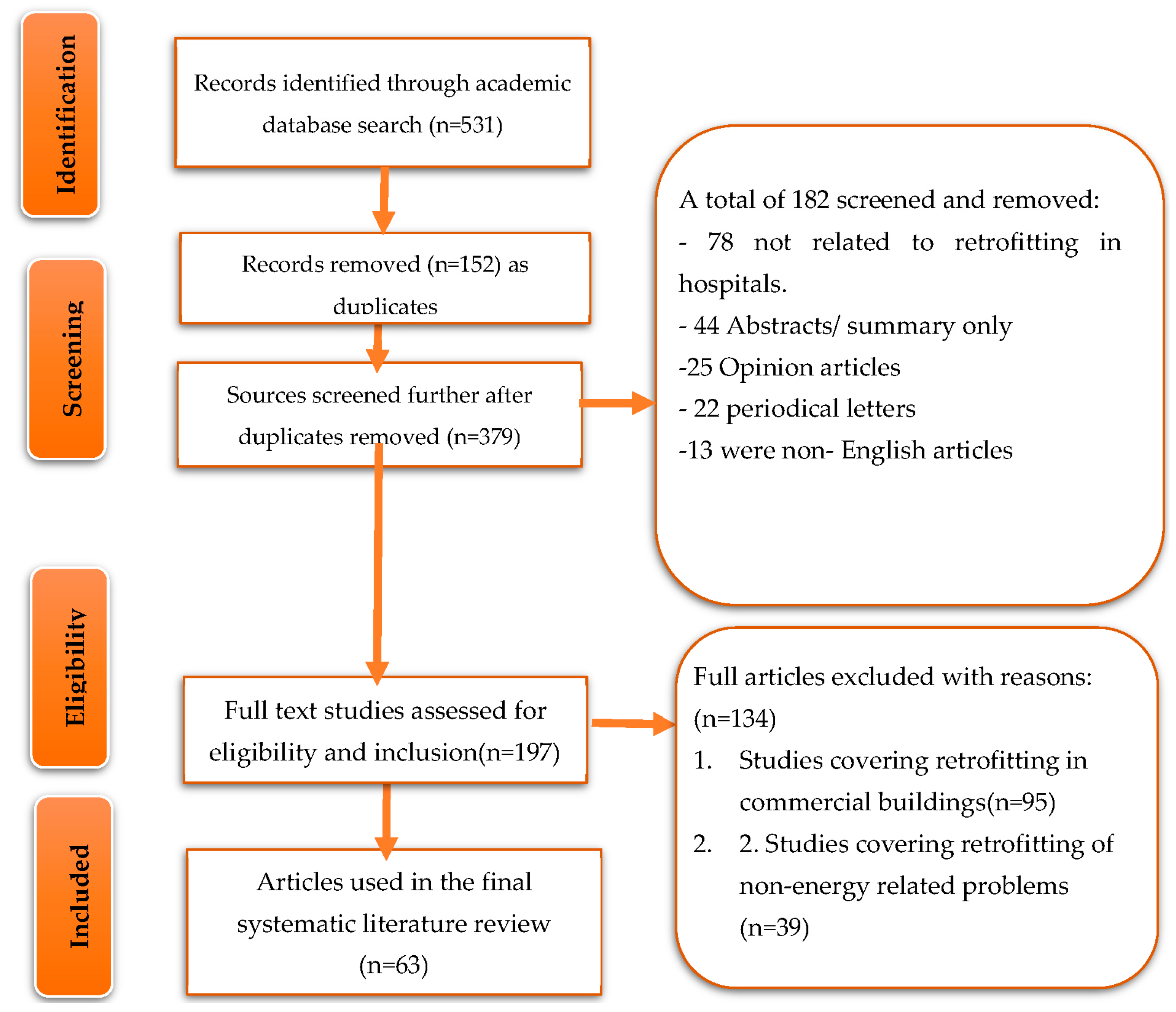
3. Materials and Methods
3.1. Search Criteria
3.2. Inclusion and Exclusion Criteria
3.3. Data Coding and Analysis
4. Data Findings
4.1. Retrofit Methods to Improve Indoor Air Quality
4.2. Energy Efficiency
- Natural ventilation: Utilizing natural ventilation strategies such as operable windows, skylights, and other openings to allow air to flow through the building can reduce energy costs associated with heating and cooling.
- Passive Solar Design: Incorporating passive solar design strategies such as orienting the building to maximize solar gain, using light-colored materials on the roof and walls, and incorporating shading devices can reduce energy costs associated with heating and cooling.
- Insulation: Installing insulation in walls, ceilings, floors, and other building areas can reduce energy costs associated with heating and cooling by reducing air leakage.
- Air Sealing: Sealing air leaks around windows, doors, ducts, pipes, and other building areas can reduce energy costs associated with heating and cooling by reducing air leakage.
- High-Efficiency HVAC Systems: Installing high-efficiency HVAC systems such as heat pumps or geothermal systems can reduce energy costs associated with heating and cooling by using less energy to achieve desired temperatures.
- Heat Recovery Ventilation Systems: Heat recovery ventilation systems (HRVs) can reduce energy costs associated with heating and cooling by recovering heat from exhaust air before it is vented outside the building.
4.3. Barriers to Uptake of Building Energy Retrofitting
4.4. Energy Conservation Techniques for Hospital Buildings
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- García-Sanz-Calcedo, J. Study of CO2 emissions from energy consumption in Spanish hospitals. Vibroeng. Procedia 2019, 26, 46–51. [Google Scholar] [CrossRef]
- González González, A.; García-Sanz-Calcedo, J.; Rodríguez Salgado, D. Evaluation of energy consumption in German hospitals: Benchmarking in the public sector. Energies 2018, 11, 2279. [Google Scholar] [CrossRef]
- Ji, R.; Qu, S. Investigation and evaluation of energy consumption performance for hospital buildings in China. Sustainability 2019, 11, 1724. [Google Scholar] [CrossRef]
- González, A.G.; García-Sanz-Calcedo, J.; Salgado, D.R. A quantitative analysis of final energy consumption in hospitals in Spain. Sustain. Cities Soc. 2018, 36, 169–175. [Google Scholar] [CrossRef]
- García-Sanz-Calcedo, J.; Gómez-Chaparro, M.; Sanchez-Barroso, G. Electrical and thermal energy in private hospitals: Consumption indicators focused on healthcare activity. Sustain. Cities Soc. 2019, 47, 101482. [Google Scholar] [CrossRef]
- Bawaneh, K.; Ghazi Nezami, F.; Rasheduzzaman, M.; Deken, B. Energy consumption analysis and characterization of healthcare facilities in the United States. Energies 2019, 12, 3775. [Google Scholar] [CrossRef]
- Prada, M.; Prada, I.F.; Cristea, M.; Popescu, D.E.; Bungău, C.; Aleya, L.; Bungău, C.C. New solutions to reduce greenhouse gas emissions through energy efficiency of buildings of special importance—Hospitals. Sci. Total Environ. 2020, 718, 137446. [Google Scholar] [CrossRef] [PubMed]
- Vaziri, S.M.; Rezaee, B.; Monirian, M.A. Utilizing renewable energy sources efficiently in hospitals using demand dispatch. Renew. Energy 2020, 151, 551–562. [Google Scholar] [CrossRef]
- Nematchoua, M.K.; Yvon, A.; Kalameu, O.; Asadi, S.; Choudhary, R.; Reiter, S. Impact of climate change on demands for heating and cooling energy in hospitals: An in-depth case study of six islands located in the Indian Ocean region. Sustain. Cities Soc. 2019, 44, 629–645. [Google Scholar] [CrossRef]
- Eckelman, M.J.; Sherman, J.D.; MacNeill, A.J. Life cycle environmental emissions and health damages from the Canadian healthcare system: An economic-environmental-epidemiological analysis. PLoS Med. 2018, 15, e1002623. [Google Scholar] [CrossRef]
- Sherman, J.; MacNeill, A.; Thiel, C. Reducing pollution from the health care industry. JAMA 2019, 322, 1043–1044. [Google Scholar] [CrossRef] [PubMed]
- Alazazmeh, A.; Asif, M. Commercial building retrofitting: Assessment of improvements in energy performance and indoor air quality. Case Stud. Therm. Eng. 2021, 26, 100946. [Google Scholar] [CrossRef]
- Anand, P.; Sekhar, C.; Cheong, D.; Santamouris, M.; Kondepudi, S. Occupancy-based zone-level VAV system control implications on thermal comfort, ventilation, indoor air quality and building energy efficiency. Energy Build. 2019, 204, 109473. [Google Scholar] [CrossRef]
- Zhao, Y.; Yu, B.; Yu, G.; Li, W. Study on the water-heat coupled phenomena in thawing frozen soil around a buried oil pipeline. Appl. Therm. Eng. 2014, 73, 1477–1488. [Google Scholar] [CrossRef]
- El-Darwish, I.; Gomaa, M. Retrofitting strategy for building envelopes to achieve energy efficiency. Alex. Eng. J. 2017, 56, 579–589. [Google Scholar] [CrossRef]
- Ergin, A.; Tekce, I. Enhancing sustainability benefits through green retrofitting of healthcare buildings. IOP Conf. Series Mater. Sci. Eng. 2020, 960, 032066. [Google Scholar] [CrossRef]
- Kahwash, F.; Barakat, B.; Taha, A.; Abbasi, Q.H.; Imran, M.A. Optimising Electrical Power Supply Sustainability Using a Grid-Connected Hybrid Renewable Energy System—An NHS Hospital Case Study. Energies 2021, 14, 7084. [Google Scholar] [CrossRef]
- Rizan, C.; Steinbach, I.; Nicholson, R.; Lillywhite, R.; Reed, M.; Bhutta, M.F. The carbon footprint of surgical operations: A systematic review. Ann. Surg. 2020, 272, 986–995. [Google Scholar] [CrossRef]
- Dursun, S.; Aykut, E.; Dursun, B. Assessment of optimum renewable energy system for the Somalia–Turkish training and research hospital in Mogadishu. J. Renew. Energy Environ. 2021, 8, 54–67. [Google Scholar]
- Alotaibi, D.M.; Akrami, M.; Dibaj, M.; Javadi, A.A. Smart energy solution for an optimised sustainable hospital in the green city of NEOM. Sustain. Energy Technol. Assess. 2019, 35, 32–40. [Google Scholar] [CrossRef]
- Meitei, I.C.; Irungbam, A.K.; Shimray, B.A. Performance evaluation of hybrid renewable energy system for supplying electricity to an institution and a hospital using HOMER. In Proceedings of the International Conference on Intelligent Computing and Smart Communication 2019: Proceedings of ICSC 2019, Thdc Ihet, Tehri, 20–21 April 2019; pp. 1317–1326. [Google Scholar]
- Chobanov, V. Renewable energy sources: Beneficial for the climate, risky for the hospital energy supply in case of pandemic. In Proceedings of the 2020 International Conference on Smart Grids and Energy Systems (SGES), Perth, Australia, 26 November 2020; pp. 870–875. [Google Scholar]
- Geissler, S.; Charalambides, A.G.; Hanratty, M. Public access to building related energy data for better decision making in implementing energy efficiency strategies: Legal barriers and technical challenges. Energies 2019, 12, 2029. [Google Scholar] [CrossRef]
- Rosenberg, D.I.; Moss, M.M.; Care, S.O.C.; Care, C.O.H. Guidelines and levels of care for pediatric intensive care units. Pediatrics 2004, 114, 1114–1125. [Google Scholar] [CrossRef]
- De Vecchi, F.; DeSantis, P. Design and Qualification of Controlled Environments. In Handbook of Validation in Pharmaceutical Processes; CRC Press: Boca Raton, FL, USA, 2021; pp. 67–88. [Google Scholar]
- Hick, J.L.; Christian, M.D.; Sprung, C.L. Chapter 2. Surge capacity and infrastructure considerations for mass critical care. Intensive Care Med. 2010, 36, 11–20. [Google Scholar] [CrossRef]
- Calcaterra, L.; Cesari, M.; Lim, W.S. Long-term care facilities (LTCFs) during the COVID-19 pandemic—Lessons from the Asian approach: A narrative review. J. Am. Med. Dir. Assoc. 2022, 23, 399–404. [Google Scholar] [CrossRef]
- Kastner, W.; Neugschwandtner, G.; Soucek, S.; Newman, H.M. Communication systems for building automation and control. Proc. IEEE 2005, 93, 1178–1203. [Google Scholar] [CrossRef]
- Peiponen, N. Preliminary Feasibility Study of a Forest Biomass Fueled Small-Scale District Heating Network in the Town of Marathon, Canada. 2015. Available online: https://www.theseus.fi/handle/10024/93188 (accessed on 29 April 2015).
- Kim, B.; Anderson, J.; Mueller, S.; Gaines, W.; Kendall, A. Literature review—Efficacy of various disinfectants against Legionella in water systems. Water Res. 2002, 36, 4433–4444. [Google Scholar] [CrossRef]
- Suen, C.Y.; Lai, Y.T.; Lui, K.H.; Li, Y.; Kwok, H.H.L.; Chang, Q.; Lee, J.H.; Han, W.; Yang, X.; Yang, Z. Virucidal, bactericidal, and sporicidal multilevel antimicrobial HEPA-ClO2 filter for air disinfection in a palliative care facility. Chem. Eng. J. 2022, 433, 134115. [Google Scholar] [CrossRef]
- Lipfert, F.W. Air Pollution and Community Health: A Critical Review and Data Sourcebook; Wiley: Hoboken, NJ, USA, 1994. [Google Scholar]
- Zhou, H.; Liang, B.; Jiang, H.; Deng, Z.; Yu, K. Magnesium-based biomaterials as emerging agents for bone repair and regeneration: From mechanism to application. J. Magnes. Alloy. 2021, 9, 779–804. [Google Scholar] [CrossRef]
- He, Q.; Zhao, H.; Shen, L.; Dong, L.; Cheng, Y.; Xu, K. Factors influencing residents’ intention toward green retrofitting of existing residential buildings. Sustainability 2019, 11, 4246. [Google Scholar] [CrossRef]
- Lomas, K.J.; Giridharan, R. Thermal comfort standards, measured internal temperatures and thermal resilience to climate change of free-running buildings: A case-study of hospital wards. Build. Environ. 2012, 55, 57–72. [Google Scholar] [CrossRef]
- Schicker, P.C.; Spayde, D.; Cho, H. Design and Feasibility Study of Biomass-Driven Combined Heat and Power Systems for Rural Communities. J. Energy Resour. Technol. 2022, 144, 070909. [Google Scholar] [CrossRef]
- Schüppler, S.; Fleuchaus, P.; Blum, P. Techno-economic and environmental analysis of an Aquifer Thermal Energy Storage (ATES) in Germany. Geotherm. Energy 2019, 7, 1–24. [Google Scholar] [CrossRef]
- Iqbal, S.J.; Mohammad, S.S. Power management, control and optimization of photovoltaic/battery/fuel cell/stored hydrogen-based microgrid for critical hospital loads. Distrib. Gener. Altern. Energy J. 2022, 37, 1027–1054. [Google Scholar] [CrossRef]
- Li, S. Low-frequency oscillations of wind power systems caused by doubly-fed induction generators. Renew. Energy 2017, 104, 129–138. [Google Scholar] [CrossRef]
- Bulté, M.; Duren, T.; Bouhon, O.; Petitclerc, E.; Agniel, M.; Dassargues, A. Numerical Modeling of the Interference of Thermally Unbalanced Aquifer Thermal Energy Storage Systems in Brussels (Belgium). Energies 2021, 14, 6241. [Google Scholar] [CrossRef]
- Arabkoohsar, A.; Sadi, M. A solar PTC powered absorption chiller design for Co-supply of district heating and cooling systems in Denmark. Energy 2020, 193, 116789. [Google Scholar] [CrossRef]
- Rahman, N.M.A.; Haw, L.C.; Fazlizan, A. A literature review of naturally ventilated public hospital wards in tropical climate countries for thermal comfort and energy saving improvements. Energies 2021, 14, 435. [Google Scholar] [CrossRef]
- Bhagat, R.K.; Linden, P. Displacement ventilation: A viable ventilation strategy for makeshift hospitals and public buildings to contain COVID-19 and other airborne diseases. R. Soc. Open Sci. 2020, 7, 200680. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, L.; Kemp, S.; James, P.; Harper, M. Noisy and restless: 24 h in an NHS community hospital ward, a qualitative and quantitative analysis of the patient environment. Build. Environ. 2020, 175, 106795. [Google Scholar] [CrossRef]
- Patel, B.V.; Haar, S.; Handslip, R.; Auepanwiriyakul, C.; Lee, T.M.-L.; Patel, S.; Harston, J.A.; Hosking-Jervis, F.; Kelly, D.; Sanderson, B. Natural history, trajectory, and management of mechanically ventilated COVID-19 patients in the United Kingdom. Intensive Care Med. 2021, 47, 549–565. [Google Scholar] [CrossRef]
- Arabkoohsar, A.; Andresen, G.B. Design and optimization of a novel system for trigeneration. Energy 2019, 168, 247–260. [Google Scholar] [CrossRef]
- Pop, O.G.; Abrudan, A.C.; Adace, D.S.; Pocola, A.G.; Balan, M.C. Potential of HVAC and solar technologies for hospital retrofit to reduce heating energy consumption. Adv. Heat Transf. Built Environ. 2018, 32, 01016. [Google Scholar] [CrossRef]
- Steffen, B.; Matsuo, T.; Steinemann, D.; Schmidt, T.S. Opening new markets for clean energy: The role of project developers in the global diffusion of renewable energy technologies. Bus. Politics 2018, 20, 553–587. [Google Scholar] [CrossRef]
- Fifield, L.-J.; Lomas, K.; Giridharan, R.; Allinson, D. Hospital wards and modular construction: Summertime overheating and energy efficiency. Build. Environ. 2018, 141, 28–44. [Google Scholar] [CrossRef]
- Zhang, Y.; Huang, J.; Fang, X.; Ling, Z.; Zhang, Z. Optimal roof structure with multilayer cooling function materials for building energy saving. Int. J. Energy Res. 2020, 44, 1594–1606. [Google Scholar] [CrossRef]
- Kishore, R.A.; Bianchi, M.V.; Booten, C.; Vidal, J.; Jackson, R. Parametric and sensitivity analysis of a PCM-integrated wall for optimal thermal load modulation in lightweight buildings. Appl. Therm. Eng. 2021, 187, 116568. [Google Scholar] [CrossRef]
- Hwang, R.-L.; Chen, B.-L.; Chen, W.-A. Analysis of Incorporating a Phase Change Material in a Roof for the Thermal Management of School Buildings in Hot-Humid Climates. Buildings 2021, 11, 248. [Google Scholar] [CrossRef]
- Heye, T.; Knoerl, R.; Wehrle, T.; Mangold, D.; Cerminara, A.; Loser, M.; Plumeyer, M.; Degen, M.; Lüthy, R.; Brodbeck, D. The energy consumption of radiology: Energy-and cost-saving opportunities for CT and MRI operation. Radiology 2020, 295, 593–605. [Google Scholar] [CrossRef]
- Guzović, Z.; Duic, N.; Piacentino, A.; Markovska, N.; Mathiesen, B.V.; Lund, H. Recent advances in methods, policies and technologies at sustainable energy systems development. Energy 2022, 245, 123276. [Google Scholar] [CrossRef]
- Tam, S.Y.; Tam, V.C.; Ramkumar, S.; Khaw, M.L.; Law, H.K.; Lee, S.W. Review on the cellular mechanisms of low-level laser therapy use in oncology. Front. Oncol. 2020, 10, 1255. [Google Scholar] [CrossRef]
- Renedo, C.; Ortiz, A.; Manana, M.; Silio, D.; Perez, S. Study of different cogeneration alternatives for a Spanish hospital center. Energy Build. 2006, 38, 484–490. [Google Scholar] [CrossRef]
- Vanhoudt, D.; Desmedt, J.; Van Bael, J.; Robeyn, N.; Hoes, H. An aquifer thermal storage system in a Belgian hospital: Long-term experimental evaluation of energy and cost savings. Energy Build. 2011, 43, 3657–3665. [Google Scholar] [CrossRef]
- Ortega, F.; Edwards, R.; Hsin, A. The economic effects of providing legal status to DREAMers. IZA J. Labor Policy 2018, 9, 1–39. [Google Scholar] [CrossRef]
- Verde, S.C.; Almeida, S.M.; Matos, J.; Guerreiro, D.; Meneses, M.; Faria, T.; Botelho, D.; Santos, M.; Viegas, C. Microbiological assessment of indoor air quality at different hospital sites. Res. Microbiol. 2015, 166, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Memarzadeh, F.; Xu, W. Role of air changes per hour (ACH) in possible transmission of airborne infections. Build. Simul. 2012, 5, 15–28. [Google Scholar] [CrossRef]
- Chen, J.-S. Enhancing air quality for embedded hospital germicidal lamps. Sustainability 2021, 13, 2389. [Google Scholar] [CrossRef]
- Shah, S.H. Spectroscopic analysis of ultraviolet lamps for disinfection of air in hospitals. Water Air Soil Pollut. Focus 2009, 9, 529–537. [Google Scholar] [CrossRef]
- Helmis, C.; Tzoutzas, J.; Flocas, H.; Halios, C.; Stathopoulou, O.; Assimakopoulos, V.; Panis, V.; Apostolatou, M.; Sgouros, G.; Adam, E. Indoor air quality in a dentistry clinic. Sci. Total Environ. 2007, 377, 349–365. [Google Scholar] [CrossRef] [PubMed]
- Forner, A.; Vilana, R.; Bianchi, L.; Rodríguez-Lope, C.; Reig, M.; García-Criado, M.Á.; Rimola, J.; Solé, M.; Ayuso, C.; Bru, C. Lack of arterial hypervascularity at contrast-enhanced ultrasound should not define the priority for diagnostic work-up of nodules < 2 cm. J. Hepatol. 2015, 62, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Dascalaki, E.G.; Lagoudi, A.; Balaras, C.A.; Gaglia, A.G. Air quality in hospital operating rooms. Build. Environ. Sci. Pollut. Res. 2008, 43, 1945–1952. [Google Scholar] [CrossRef]
- Araujo, R.; Cabral, J.P.; Rodrigues, A.G. Air filtration systems and restrictive access conditions improve indoor air quality in clinical units: Penicillium as a general indicator of hospital indoor fungal levels. Am. J. Infect. Control. 2008, 36, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Emuren, K.; Ordinioha, B. Microbiological assessment of indoor air quality at different sites of a tertiary hospital in South-South Nigeria. Port Harcourt Med. J. 2016, 10, 79. [Google Scholar] [CrossRef]
- Sudharsanam, S.; Srikanth, P.; Sheela, M.; Steinberg, R. Study of the indoor air quality in hospitals in South Chennai, India—Microbial profile. Indoor Built Environ. 2008, 17, 435–441. [Google Scholar] [CrossRef]
- Hellgren, U.-M.; Hyvärinen, M.; Holopainen, R.; Reijula, K. Perceived indoor air quality, air-related symptoms and ventilation in Finnish hospitals. Int. J. Occup. Med. Environ. Health 2011, 24, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.D.; Yao, X.; Zhou, S.J. Seismic fragility analysis for typical multi-span simply supported railway box girder bridges. Appl. Mech. Mater. 2016, 858, 137–144. [Google Scholar] [CrossRef]
- Soliman, A.; O’Connell, J.F.; Tamaddoni-Nezhad, A. A data-driven approach for characterising revenues of South-Asian long-haul low-cost carriers per equivalent flight capacity per block hour. J. Air Transp. Manag. 2022, 103, 102242. [Google Scholar] [CrossRef]
- Sá, A.V.; Azenha, M.; De Sousa, H.; Samagaio, A. Thermal enhancement of plastering mortars with Phase Change Materials: Experimental and numerical approach. Energy Build. 2012, 49, 16–27. [Google Scholar] [CrossRef]
- Melikov, A.K. Advanced air distribution: Improving health and comfort while reducing energy use. Indoor Air 2016, 26, 112–124. [Google Scholar] [CrossRef] [PubMed]
- Miller, S.L.; Linnes, J.; Luongo, J. Ultraviolet germicidal irradiation: Future directions for air disinfection and building applications. Photochem. Photobiol. 2013, 89, 777–781. [Google Scholar] [CrossRef] [PubMed]
- Memarzadeh, F.; Olmsted, R.N.; Bartley, J.M. Applications of ultraviolet germicidal irradiation disinfection in health care facilities: Effective adjunct, but not stand-alone technology. Am. J. Infect. Control. 2010, 38, S13–S24. [Google Scholar] [CrossRef] [PubMed]
- Mphaphlele, M.; Dharmadhikari, A.S.; Jensen, P.A.; Rudnick, S.N.; Van Reenen, T.H.; Pagano, M.A.; Leuschner, W.; Sears, T.A.; Milonova, S.P.; van der Walt, M. Institutional tuberculosis transmission. Controlled trial of upper room ultraviolet air disinfection: A basis for new dosing guidelines. Am. J. Respir. Crit. Care Med. 2015, 192, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Luksamijarulkul, P.; Aiempradit, N.; Vatanasomboon, P. Microbial contamination on used surgical masks among hospital personnel and microbial air quality in their working wards: A hospital in Bangkok. Oman Med. J. 2014, 29, 346. [Google Scholar] [CrossRef] [PubMed]
- Onmek, N.; Kongcharoen, J.; Singtong, A.; Penjumrus, A.; Junnoo, S. Environmental factors and ventilation affect concentrations of microorganisms in hospital wards of Southern Thailand. J. Environ. Public Health 2020, 2020, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Jung, C.-C.; Wu, P.-C.; Tseng, C.-H.; Su, H.-J. Indoor air quality varies with ventilation types and working areas in hospitals. Build. Environ. 2015, 85, 190–195. [Google Scholar] [CrossRef]
- Śmiełowska, M.; Marć, M.; Zabiegała, B. Indoor air quality in public utility environments—A review. Environ. Sci. Pollut. Res. 2017, 24, 11166–11176. [Google Scholar] [CrossRef] [PubMed]
- Meek, A.; Jayasuriya, N.; Horan, E.; Adams, R. Environmental benefits of retrofitting green roofs to a city block. J. Hydrol. Eng. 2015, 20, 05014020. [Google Scholar] [CrossRef]
- Radwan, A.F.; Hanafy, A.A.; Elhelw, M.; El-Sayed, A.E.-H.A. Retrofitting of existing buildings to achieve better energy-efficiency in commercial building case study: Hospital in Egypt. Alex. Eng. J. 2016, 55, 3061–3071. [Google Scholar] [CrossRef]
- Sala, M.; Alcamo, G.; Nelli, L.C. Energy-saving solutions for five hospitals in Europe. In Proceedings of the Mediterranean Green Buildings & Renewable Energy: Selected Papers from the World Renewable Energy Network’s Med Green Forum; Springer: Berlin/Heidelberg, Germany, 2016; pp. 1–17. [Google Scholar]
- Šujanová, P.; Rychtáriková, M.; Sotto Mayor, T.; Hyder, A. A healthy, energy-efficient and comfortable indoor environment, a review. Energies 2019, 12, 1414. [Google Scholar] [CrossRef]
- Wang, B.; Xia, X. Optimal maintenance planning for building energy efficiency retrofitting from optimization and control system perspectives. Energy Build. 2015, 96, 299–308. [Google Scholar] [CrossRef]
- Wang, T.; Li, X.; Liao, P.-C.; Fang, D. Building energy efficiency for public hospitals and healthcare facilities in China: Barriers and drivers. Energy 2016, 103, 588–597. [Google Scholar] [CrossRef]
- William, M.A.; Elharidi, A.M.; Hanafy, A.A.; Attia, A.; Elhelw, M. Energy-efficient retrofitting strategies for healthcare facilities in hot-humid climate: Parametric and economical analysis. Alex. Eng. J. 2020, 59, 4549–4562. [Google Scholar] [CrossRef]
- Castleton, H.F.; Stovin, V.; Beck, S.B.; Davison, J.B. Green roofs; building energy savings and the potential for retrofit. Energy Build. 2010, 42, 1582–1591. [Google Scholar] [CrossRef]
- Gaspari, J.; Fabbri, K.; Gabrielli, L. Retrofitting Hospitals: A parametric design approach to optimize energy efficiency. Proc. IOP Conf. Ser. Earth Environ. Sci. 2019, 290, 012130. [Google Scholar] [CrossRef]
- Chiang, C.-Y.; Yang, R.; Yang, K.-H.; Lee, S.-K. Performance analysis of an integrated heat pump with air-conditioning system for the existing hospital building application. Sustainability 2017, 9, 530. [Google Scholar] [CrossRef]
- Taseli, B.K.; Kilkis, B. Ecological sanitation, organic animal farm, and cogeneration: Closing the loop in achieving sustainable development—A concept study with on-site biogas fueled trigeneration retrofit in a 900-bed university hospital. Energy Build. 2016, 129, 102–119. [Google Scholar] [CrossRef]
- Asim, N.; Badiei, M.; Mohammad, M.; Razali, H.; Rajabi, A.; Chin Haw, L.; Jameelah Ghazali, M. Sustainability of heating, ventilation and air-conditioning (HVAC) systems in buildings—An overview. Int. J. Environ. Res. Public Health 2022, 19, 1016. [Google Scholar] [CrossRef] [PubMed]
- Cesari, S.; Valdiserri, P.; Coccagna, M.; Mazzacane, S. The energy saving potential of wide windows in hospital patient rooms, optimizing the type of glazing and lighting control strategy under different climatic conditions. Energies 2020, 13, 2116. [Google Scholar] [CrossRef]
- Chirarattananon, S.; Taweekun, J. A technical review of energy conservation programs for commercial and government buildings in Thailand. Energy Convers. Manag. 2003, 44, 743–762. [Google Scholar] [CrossRef]
- Gomes, M.G.; Rodrigues, A.M.; Natividade, F. Thermal and energy performance of medical offices of a heritage hospital building. J. Build. Eng. 2021, 40, 102349. [Google Scholar] [CrossRef]
- Khahro, S.H.; Kumar, D.; Siddiqui, F.H.; Ali, T.H.; Raza, M.S.; Khoso, A.R. Optimizing energy use, cost and carbon emission through building information modelling and a sustainability approach: A case-study of a hospital building. Sustainability 2021, 13, 3675. [Google Scholar] [CrossRef]
- Sadek, A.H.; Mahrous, R. Adaptive glazing technologies: Balancing the benefits of outdoor views in healthcare environments. Sol. Energy 2018, 174, 719–727. [Google Scholar] [CrossRef]
- Short, C.A.; Lomas, K.J.; Giridharan, R.; Fair, A.J. Building resilience to overheating into 1960’s UK hospital buildings within the constraint of the national carbon reduction target: Adaptive strategies. Build. Environ. 2012, 55, 73–95. [Google Scholar] [CrossRef]
- Taleb, H.M. Enhancing the skin performance of hospital buildings in the UAE. J. Build. Eng. 2016, 7, 300–311. [Google Scholar] [CrossRef]
- Odhong’, C.; Wilkes, A.; van Dijk, S.; Vorlaufer, M.; Ndonga, S.; Sing’ora, B.; Kenyanito, L. Financing large-scale mitigation by smallholder farmers: What roles for public climate finance? Front. Sustain. Food Syst. 2019, 3, 3. [Google Scholar] [CrossRef]
- Luthfiyyah, D.N.; Widjajanti, R. Green Roof to Overcome Urban Heat Island Effects in the Center of Semarang. E3S Web Conf. 2019, 125, 07018. [Google Scholar] [CrossRef]
- Alabdullatief, A.; Omer, S.; Elabdein, R.Z.; Alfraidi, S. Green Roof and Louvers Shading for Sustainable Mosque Buildings in Riyadh, Saudi Arabia. 2016. Available online: https://nottingham-repository.worktribe.com/output/836216/green-roof-and-louvers-shading-for-sustainable-mosque-buildings-in-riyadh-saudi-arabia (accessed on 7 December 2016).
- Reeve, A.; Nieberler-Walker, K.; Desha, C. Healing gardens in children’s hospitals: Reflections on benefits, preferences and design from visitors’ books. Urban For. Urban Green. 2017, 26, 48–56. [Google Scholar] [CrossRef]
- Kolokotsa, D.; Tsoutsos, T.; Papantoniou, S. Energy conservation techniques for hospital buildings. Adv. Build. Energy Res. 2012, 6, 159–172. [Google Scholar] [CrossRef]
- Vickers, N.J. Animal communication: When I’m calling you, will you answer too? Curr. Biol. 2017, 27, R713–R715. [Google Scholar] [CrossRef]
- Nourdine, B.; Saad, A. About energy efficiency in Moroccan health care buildings. Mater. Today Proc. 2021, 39, 1141–1147. [Google Scholar] [CrossRef]
- Montiel-Santiago, F.J.; Hermoso-Orzáez, M.J.; Terrados-Cepeda, J. Sustainability and energy efficiency: BIM 6D. Study of the BIM methodology applied to hospital buildings. Value of interior lighting and daylight in energy simulation. Sustainability 2020, 12, 5731. [Google Scholar] [CrossRef]
- Lavy, S.; Shohet, I.M. Integrated maintenance management of hospital buildings: A case study. Constr. Manag. Econ. 2004, 22, 25–34. [Google Scholar] [CrossRef]
- Shi, Y.; Yan, Z.; Li, C.; Li, C. Energy consumption and building layouts of public hospital buildings: A survey of 30 buildings in the cold region of China. Sustain. Cities Soc. 2021, 74, 103247. [Google Scholar] [CrossRef]
- Ahuja, A.S.; Ramteke, D.S.; Parey, A. Vibration-based fault diagnosis of a bevel and spur gearbox using continuous wavelet transform and adaptive neuro-fuzzy inference system. In Soft Computing in Condition Monitoring and Diagnostics of Electrical and Mechanical Systems: Novel Methods for Condition Monitoring Diagnostics; Springer: Berlin/Heidelberg, Germany, 2020. [Google Scholar] [CrossRef]
- Shohet, I.M. Building evaluation methodology for setting maintenance priorities in hospital buildings. Constr. Manag. Econ. 2003, 21, 681–692. [Google Scholar] [CrossRef]
- Arif, S.; Taweekun, J.; Ali, H.M.; Theppaya, T. Techno economic evaluation and feasibility analysis of a hybrid net zero energy building in Pakistan: A case study of hospital. Front. Energy Res. 2021, 9, 668908. [Google Scholar] [CrossRef]
- GhaffarianHoseini, A.; Zhang, T.; Nwadigo, O.; GhaffarianHoseini, A.; Naismith, N.; Tookey, J.; Raahemifar, K. Application of nD BIM Integrated Knowledge-based Building Management System (BIM-IKBMS) for inspecting post-construction energy efficiency. Renew. Sustain. Energy Rev. 2017, 72, 935–949. [Google Scholar] [CrossRef]
- Walker, A. Natural Ventilation. Whole Building Design Guide: A Program of the National Institute of Building Sciences. J. Build. Constr. Plan. Res. 2010, 9. Available online: https://www.wbdg.org/resources/natural-ventilation (accessed on 8 February 2016).
- Ascione, F.; Bianco, N.; De Stasio, C.; Mauro, G.M.; Vanoli, G.P. Multi-stage and multi-objective optimization for energy retrofitting a developed hospital reference building: A new approach to assess cost-optimality. Appl. Energy 2016, 174, 37–68. [Google Scholar] [CrossRef]
- D’agostino, D.; Zangheri, P.; Castellazzi, L. Towards nearly zero energy buildings in Europe: A focus on retrofit in non-residential buildings. Energies 2017, 10, 117. [Google Scholar] [CrossRef]
- Bertone, E.; Stewart, R.A.; Sahin, O.; Alam, M.; Zou, P.X.; Buntine, C.; Marshall, C. Guidelines, barriers and strategies for energy and water retrofits of public buildings. J. Clean. Prod. 2018, 174, 1064–1078. [Google Scholar] [CrossRef]
- Hou, J.; Liu, Y.; Wu, Y.; Zhou, N.; Feng, W. Comparative study of commercial building energy-efficiency retrofit policies in four pilot cities in China. Energy Policy 2016, 88, 204–215. [Google Scholar] [CrossRef]
- Chapman, R.; Howden-Chapman, P.; Viggers, H.; O’dea, D.; Kennedy, M. Retrofitting houses with insulation: A cost–benefit analysis of a randomised community trial. J. Epidemiol. Community Health 2009, 63, 271–277. [Google Scholar] [CrossRef]
- Nuti, C.; Vanzi, I. To retrofit or not to retrofit? Eng. Struct. 2003, 25, 701–711. [Google Scholar] [CrossRef]
- Gaspari, J.; Fabbri, K.; Gabrielli, L. A study on parametric design application to hospital retrofitting for improving energy savings and comfort conditions. Buildings 2019, 9, 220. [Google Scholar] [CrossRef]
- Bizzarri, G.; Morini, G.L. New technologies for an effective energy retrofit of hospitals. Appl. Therm. Eng. 2006, 26, 161–169. [Google Scholar] [CrossRef]
- Besen, P.; Boarin, P.; Haarhoff, E. Energy and Seismic Retrofit of Historic Buildings in New Zealand: Reflections on Current Policies and Practice. Hist. Environ. Policy Pract. 2020, 11, 91–117. [Google Scholar] [CrossRef]
| No. | Setting | Usage |
|---|---|---|
| 1 | Indoor air quality |
|
| 2 | High safety of energy supply |
|
| 3 | Domestic hot water |
|
| 4 | High-efficiency particulate air (HEPA) |
|
| 5 | Laundry facilities |
|
| 6 | Climate control |
|
| No. | Researcher(s) | Research Focus | Findings |
|---|---|---|---|
| 1 | Schicker, Spayde, and Cho [36] | Building combined heat and power (BCHP) technology and the energy efficiency of health facilities in rural settings. | Hospitals are the most promising structures for BCHP owing to the consistent thermal load demands that they have and the favourable heat-to-power ratio that they have. |
| 2 | Schüppler et al. [37] | An aquifer thermal energy storage (ATES) system was combined with a heat pump and installed in a Belgian hospital. | The primary energy consumption of the heat pump system is 71% less than that of a reference installation based on common gas-fired boilers and water-cooling machines. |
| 3 | Iqbal and Mohammad [38] | The contribution that fuel cells (FCs), photovoltaic (PV) systems, and solar thermal systems can make to hospitals, as well as the environmental benefits of installing such systems using a hybrid concept. |
|
| 4 | Li [39] | Solar-powered cooling systems for hospitals. | It is friendly to the environment and helps bring about a sizeable reduction in carbon dioxide emissions produced. |
| 5 | Bulté et al. [40] | Solar-powered cooling systems for hospitals. | Using solar-powered cooling ensures the total thermal and cooling load that originates from solar energy cuts costs, thereby ensuring collector performance. |
| 6 | Arabkoohsar and Sadi [41] | Solar-powered cooling systems for hospitals. |
|
| 7 | Rahman and colleagues [42] | Natural ventilation. |
|
| 8 | Bhagat and Linden [43] | Promotion of natural ventilation. | Along with significant initial expenses and managerial resistance, the healthcare facility’s location and immediate surroundings are also an underestimated barrier. |
| 9 | Sawyer et al. [44] | High indoor environmental quality impacts in hospitals. | The staff members complained of health problems that they believed were caused by the poor comfort conditions and air quality inside. |
| 10 | Patel et al. [45] | Environmental design to achieve energy efficiency. | Hypothesized that up to 70% of the net floor area of small to medium-sized health facilities could be naturally ventilated and that both staff and patients could benefit from more naturally sustained environments. |
| 11 | Arabkoohsar and Andresen [46] | Hospital energy demands and operational profiles using linear programming optimization methods. |
|
| No. | Researcher(s) | Research Focus | Findings |
|---|---|---|---|
| 1 | Heye, Knoerl, Wehrle, Mangold, Cerminara, Loser, Plumeyer, Degen, Lüthy, and Brodbeck [53] | Energy consumption in CT and MRI operational rooms in Switzerland. |
|
| 2 | Guzović et al. [54] | Implementing a pinch technology. |
|
| 3 | Miecznik and Skrzypczak (2019) | Investigated two healthcare facilities in Poland with 470 beds regarding the seasonal shifts in the heat required to generate hot water for household use. |
|
| 4 | Tam et al. [55] | Investigating the flux of usable energy and the coefficient of energy conservation of an incinerator used for the combustion process of medical waste in an Oncological Hospital in Hong Kong. |
|
| 5 | Renedo et al. [56] | Various possibilities for domestic hot water use, cooling, and heating in local hospitals in Santander, Basque Country, Spain. |
|
| 6 | Vanhoudt et al. [57] | An aquifer thermal storage system in a Belgian hospital: Long-term experimental evaluation of energy and cost savings. |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hama Radha, C. Retrofitting for Improving Indoor Air Quality and Energy Efficiency in the Hospital Building. Sustainability 2023, 15, 3464. https://doi.org/10.3390/su15043464
Hama Radha C. Retrofitting for Improving Indoor Air Quality and Energy Efficiency in the Hospital Building. Sustainability. 2023; 15(4):3464. https://doi.org/10.3390/su15043464
Chicago/Turabian StyleHama Radha, Chro. 2023. "Retrofitting for Improving Indoor Air Quality and Energy Efficiency in the Hospital Building" Sustainability 15, no. 4: 3464. https://doi.org/10.3390/su15043464
APA StyleHama Radha, C. (2023). Retrofitting for Improving Indoor Air Quality and Energy Efficiency in the Hospital Building. Sustainability, 15(4), 3464. https://doi.org/10.3390/su15043464






