Sleep Deficit as a Risk Factor for Hypertension in Korean Adults
Abstract
1. Introduction
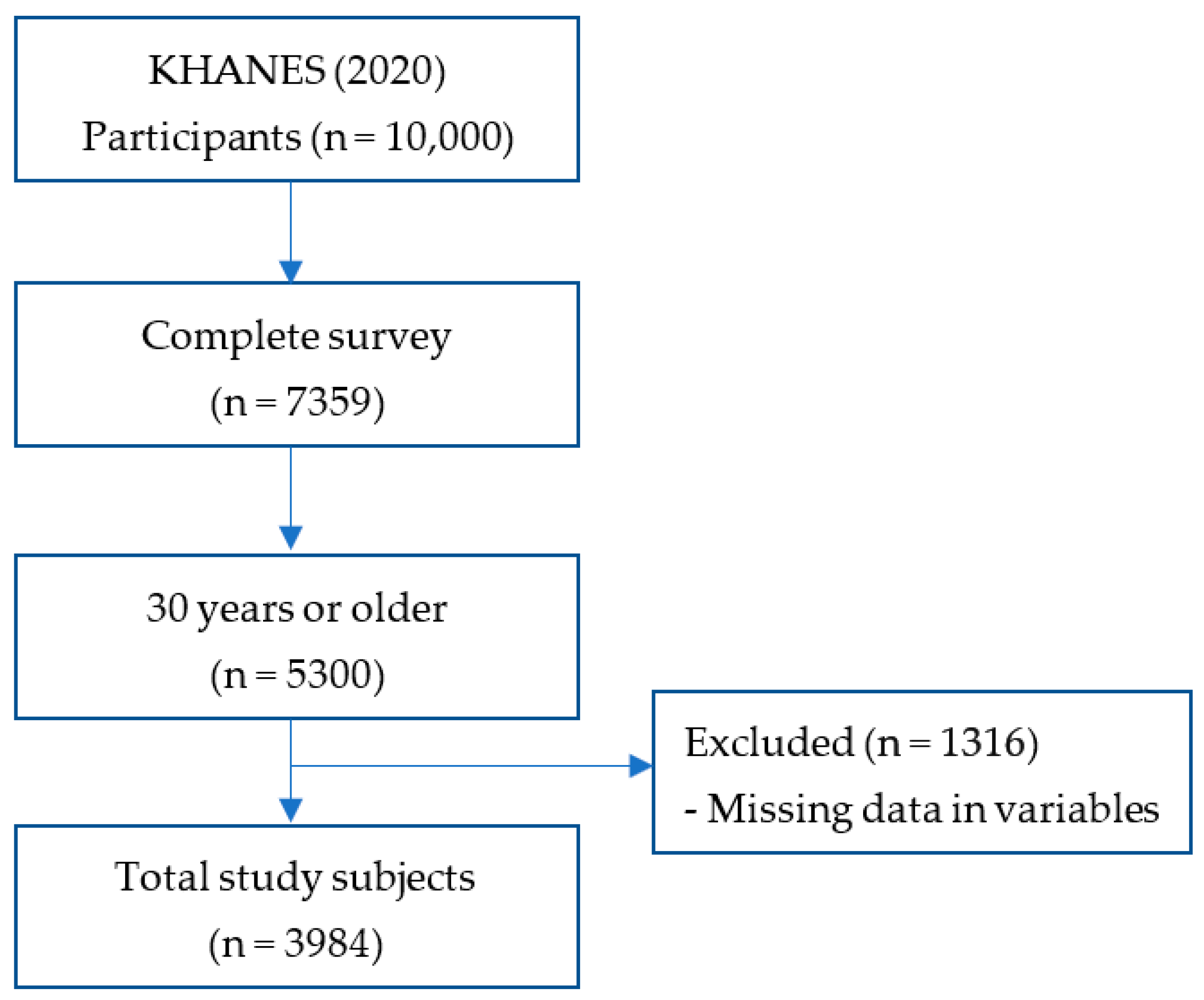
2. Materials and Methods
2.1. Data
2.2. Outcome Measure
2.3. Sociodemographic Characteristics
2.4. Health-Related Characteristic
2.5. Statistical Analysis
3. Results
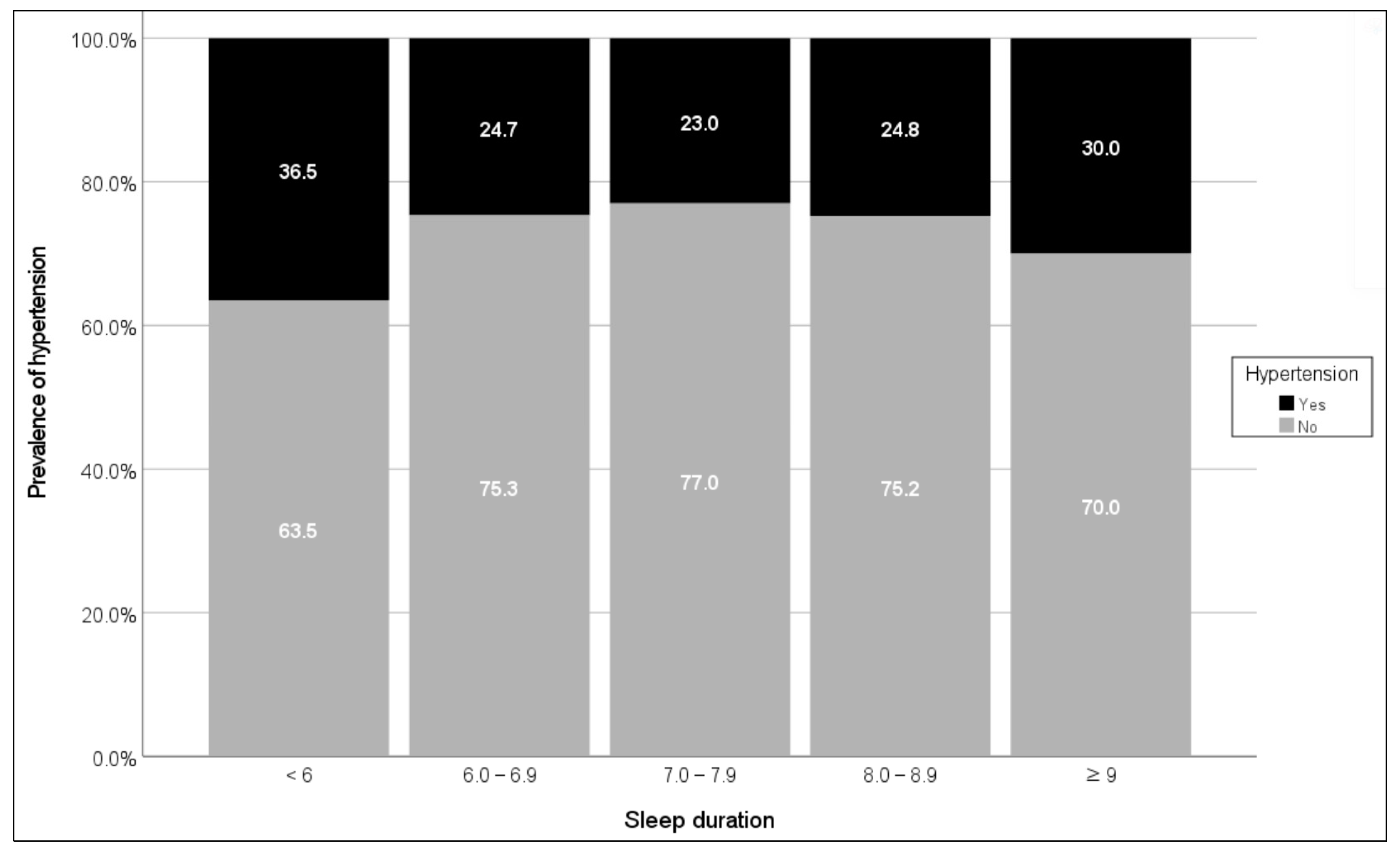
3.1. Prevalence of Hypertension by Sociodemographic and Health-Related Charactersitics
3.2. Comparison of Sleep Duration According to Sociodemographic Characteristics
3.3. Comparison of Sleep Duration According to Health-Related Characteristics
3.4. Odds Ratio in Logistic Regression Analysis for Hypertension According to Sleep Duration
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, H.C.; Lee, H.; Lee, H.H.; Seo, E.; Kim, E.; Han, J.; Kwon, J.Y.; Korean Society of Hypertension (KSH)–Hypertension Epidemiology Research Working Group. Korea hypertension fact sheet 2021: Analysis of nationwide population-based data with special focus on hypertension in women. Clin. Hypertens. 2022, 28, 1. [Google Scholar] [CrossRef] [PubMed]
- Seo, S.Y.; Kim, H.J.; Oh, H.K.; Lee, S.K. Propulsion status of a community-based hypertension and diabetes control program. Public Health Wkly. Rep. 2021, 14, 1414–1421. Available online: https://kdca.go.kr/filepath/boardSyview.es?bid=0024&list_no=713376&seq=1 (accessed on 21 April 2022).
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L., Jr.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T., Jr.; et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003, 42, 1206–1252. [Google Scholar] [CrossRef] [PubMed]
- Kanjilal, S.; Gregg, E.W.; Cheng, Y.J.; Zhang, P.; Nelson, D.E.; Mensah, G.; Beckles, G.L. Socioeconomic status and trends in disparities in 4 major risk factors for cardio-vascular disease among US adults, 1971–2002. Arch. Intern. Med. 2006, 166, 2348–2355. [Google Scholar] [CrossRef]
- Wang, W.; Lee, E.T.; Fabsitz, R.R.; Devereux, R.; Best, L.; Welty, T.K.; Howard, B.V. A longitudinal study of hypertension risk factors and their relation to cardiovascular disease: The Strong Heart Study. Hypertension 2006, 47, 403–409. [Google Scholar] [CrossRef]
- World Health Organization. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis: World Health Day 2013. 2013. Available online: https://www.who.int/publications-detail-redirect/a-global-brief-on-hypertension-silent-killer-global-public-health-crisis-world-health-day-2013 (accessed on 14 May 2022).
- Stranges, S.; Dorn, J.M.; Cappuccio, F.P.; Donahue, R.P.; Rafalson, L.B.; Hovey, K.M.; Freudenheim, J.L.; Kandala, N.B.; Miller, M.A.; Trevisan, M. A population-based study of reduced sleep duration and hypertension: The strongest association may be in premenopausal women. J. Hypertens. 2010, 28, 896–902. [Google Scholar] [CrossRef]
- Park, E. Sleep Duration and the Related Factors of Hypertension among Korean Middle-aged Adults. Korean J. Adult Nurs. 2014, 26, 372–381. [Google Scholar] [CrossRef]
- Foreman, M.D.; Wykle, M. Nursing standard-of-practice protocol: Sleep disturbances in elderly patients. The NICHE Fac-ulty. Geriatr. Nurs. 1995, 16, 238–243. [Google Scholar] [CrossRef]
- Kim, J.A.; Lee, S.Y. Health Behaviors and Dietary Habits according to Sleep Duration in Korean Adults Based on the 2013–2015 Korea National Health and Nutrition Examination Survey. Korean J. Health Promot. 2019, 19, 237–247. [Google Scholar] [CrossRef]
- Organization for Economic Co-Operation and Development. Society at a Glance 2014—OECD Social Indicators. 2014. Available online: https://read.oecd-ilibrary.org/social-issues-migration-health/society-at-a-glance-2014_soc_glance-2014-en (accessed on 6 July 2022).
- Kim, H.J.; Oh, S.Y.; Joo, J.H.; Choi, D.W.; Park, E.C. The Relationship between Sleep Duration and Perceived Stress: Findings from the 2017 Community Health Survey in Korea. Int. J. Environ. Res. Public Health 2019, 16, 3208. [Google Scholar] [CrossRef]
- Hwang, H.R.; Lee, J.G.; Lee, S.; Cha, K.S.; Choi, J.H.; Jeong, D.W.; Yi, Y.H.; Cho, Y.H.; Tak, Y.J.; Kim, Y.J. The relationship between hypertension and sleep duration: An analysis of the fifth Korea National Health and Nutrition Examination Survey (KNHANES V-3). Clin. Hypertens. 2015, 21, 8. [Google Scholar] [CrossRef]
- Ko, Y.J.; Park, E. Factors Related to Blood Pressure Control in Hypertensive Patients in Jeju Province. J. Korean Public Health Nurs. 2013, 27, 267–279. [Google Scholar] [CrossRef]
- Ryu, S.Y.; Kim, K.S.; Han, M.A. Factors associated with sleep duration in Korean adults: Results of a 2008 community health survey in Gwangju metropolitan city, Korea. J. Korean Med. Sci. 2011, 26, 1124–1131. [Google Scholar] [CrossRef]
- Eun, K.S.; Cha, S.E. Gender differentials and covariates of sleep time in daily life of Korea. Stat. Res. 2010, 15, 82–103. Available online: https://www.kci.go.kr/kciportal/ci/sereArticleSearch/ciSereArtiView.kci?sereArticleSearchBean.artiId=ART001492850 (accessed on 20 April 2022).
- Kim, J.H.; Jo, I.H. Age-Dependent Association Between Sleep Duration and Hypertension in the Adult Korean Population. Am. J. Hypertens. 2010, 23, 1286–1291. [Google Scholar] [CrossRef]
- Korea Disease Control and Prevention Agency. Guidebook for Using the 8th Korean National Health and Nutrition Exam-ination Survey (KNHANES VIII). 2022. Available online: https://knhanes.kdca.go.kr/knhanes/sub03/sub03_02_05.do (accessed on 5 March 2022).
- Lee, G.B.; Kim, Y.; Park, S.; Kim, H.C.; Oh, K. Obesity, hypertension, diabetes mellitus, and hypercholesterolemia in Korean adults before and during the COVID-19 pandemic: A special report of the 2020 Korea National Health and Nutrition Examination Survey. Epidemiol. Health 2022, 44, e2022041. [Google Scholar] [CrossRef]
- Hanyang University College of Medicine. Report: Quality Control and Assurance of Blood Pressure Measurement: KNHANES 7. Korea Centers for Disease Control and Prevention. 2018, pp. 18–167. (In Korean). Available online: https://library.nih.go.kr/ncmiklib/mlib/mlibViewReport.do?bibctrlno=7863442 (accessed on 23 March 2022).
- Cho, S.M.; Lee, H.; Pyun, W.B.; Kim, H.C. Differential Control Rate of Systolic and Diastolic Blood Pressure among Korean Adults with Hypertension: The Sixth Korean National Health and Nutrition Examination Survey, 2013–2015 (KNHANES VI). Korean Circ. J. 2019, 49, 1035–1048. [Google Scholar] [CrossRef] [PubMed]
- Alkerwi, A.; Pagny, S.; Lair, M.L.; Delagardelle, C.; Beissel, J. Level of unawareness and management of diabetes, hy-pertension, and dyslipidemia among adults in Luxembourg: Findings from ORISCAV-LUX study. PLoS ONE 2013, 8, e57920. [Google Scholar] [CrossRef]
- Korea National Health Insurance Service. National Health Insurance: Population Coverage. 2022. Available online: https://www.nhis.or.kr/english/wbheaa02400m01.do (accessed on 11 April 2022).
- Vioque, J.; Torres, A.; Quiles, J. Time spent watching television, sleep duration and obesity in adults living in Valencia, Spain. Int. J. Obes. 2000, 24, 1683–1688. [Google Scholar] [CrossRef]
- Schoenborn, C.A.; Adams, P.E. Health behaviors of adults: United States, 2005–2007. Vital Health Stat. 2010, 245, 1–132. [Google Scholar]
- Cha, S.E.; Eun, K.S. Gender Difference in Sleep Problems: Focused on Time Use in Daily Life of Korea. JSTOR 2014, 119, 1447–1465. Available online: http://www.jstor.org/stable/24721494 (accessed on 11 May 2022). [CrossRef]
- Seo, M.H.; Lee, W.Y.; Kim, S.S.; Kang, J.-H.; Kim, K.K.; Kim, B.-Y.; Kim, Y.-H.; Kim, W.-J.; Kim, E.M.; Kim, H.S.; et al. Corrigendum: 2018 Korean Society for the Study of Obesity Guideline for the Management of Obesity in Korea. J. Obes. Metab. Syndr. 2019, 28, 143. [Google Scholar] [CrossRef] [PubMed]
- Hosmer, D.; Lemshow, S.; Sturdivant, R. Applied Logistic Regression; John Wiley & Sons: Hoboken, NJ, USA, 2013; Available online: https://onlinelibrary.wiley.com/doi/book/10.1002/9781118548387 (accessed on 10 April 2022).
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Katz, E.S.; Kheirandish-Gozal, L.; et al. National Sleep Foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health 2015, 1, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Altman, N.G.; Izci-Balserak, B.; Schopfer, E.; Jackson, N.; Rattanaumpawan, P.; Gehrman, P.R.; Patel, N.P.; Grandner, M.A. Sleep duration versus sleep insufficiency as predictors of cardiometabolic health outcomes. Sleep Med. 2012, 13, 1261–1270. [Google Scholar] [CrossRef]
- Kim, S.J.; Lee, S.K.; Kim, S.H.; Yun, C.H.; Kim, J.H.; Thomas, R.J.; Shin, C. Genetic association of short sleep duration with hypertension incidence--a 6-year fol-low-up in the Korean genome and epidemiology study. Circ. J. 2012, 76, 907–913. [Google Scholar] [CrossRef]
- Wang, Q.; Xi, B.; Liu, M.; Zhang, Y.; Fu, M. Short sleep duration is associated with hypertension risk among adults: A sys-tematic review and meta-analysis. Hypertens. Res. 2012, 35, 1012–1018. [Google Scholar] [CrossRef]
- Oliveros, E.; Patel, H.; Kyung, S.; Fugar, S.; Goldberg, A.; Madan, N.; Williams, K.A. Hypertension in older adults: Assessment, management, and challenges. Clin. Cardiol. 2020, 43, 99–107. [Google Scholar] [CrossRef]
- Ohayon, M.M.; Vecchierini, M.F. Normative sleep data, cognitive function and daily living activities in older adults in the community. Sleep 2005, 28, 981–989. [Google Scholar]
- Diaz, K.M.; Shimbo, D. Physical activity and the prevention of hypertension. Curr. Hypertens. Rep. 2013, 15, 659–668. [Google Scholar] [CrossRef]
- Chobanian, A.V.; Alderman, M.H.; DeQuattro, V.; Frohlich, E.D.; Gifford, R.W.; Hill, M.N.; Kaplan, N.M.; Langford, H.G.; Langford, M.A.; Weiss, S.M.; et al. The 1988 Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch. Intern. Med. 1988, 148, 1023–1038. [Google Scholar] [CrossRef]
- Flack, D.J.M.; Adekoka, B. Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc. Med. 2020, 30, 160–164. [Google Scholar] [CrossRef]
- Ihm, S.H.; Park, J.H.; Kim, J.Y.; Kim, J.H.; Kim, K.I.; Lee, E.M.; Park, S.; Shin, J.; Kim, C.H. Home blood pressure monitoring: A position statement from the Korean Society of Hypertension Home Blood Pressure Forum. Clin. Hypertens. 2022, 28, 38. [Google Scholar] [CrossRef]
- Levin, K.A. Study design III: Cross-sectional studies. Evid. Based Dent. 2006, 7, 24–25. [Google Scholar] [CrossRef]
- Lauderdale, D.S.; Knutson, K.L.; Yan, L.L.; Liu, K.; Rathouz, P.J. Self-Reported and Measured Sleep Duration: How Similar Are They? Epidemiology 2008, 19, 838–845. [Google Scholar] [CrossRef]
| Variable | Total | Hypertension | t, χ2 | p-Value | |
|---|---|---|---|---|---|
| Yes | No | ||||
| n (%), Mean ± SD | |||||
| Sex | 42.400 *** | <0.001 | |||
| Male | 1927 (48.4) | 605 (31.4) | 1322 (68.6) | ||
| Female | 2057 (51.6) | 458 (22.3) | 1599 (77.7) | ||
| Age 1 | 636.773 *** | <0.001 | |||
| 30–49 | 1567 (39.3) | 115 (7.3) | 1452 (92.7) | ||
| 50–69 | 1794 (45.0) | 590 (32.9) | 1204 (67.1) | ||
| ≥70 | 623 (15.7) | 358 (57.5) | 265 (42.5) | ||
| Marital status | 62.304 *** | <0.001 | |||
| Not married | 387 (9.7) | 38 (9.8) | 349 (90.2) | ||
| Married | 3597 (90.3) | 1025 (28.5) | 2572 (71.5) | ||
| Education level | 394.323 *** | <0.001 | |||
| ≤primary education | 634 (15.9) | 329 (51.9) | 305 (48.1) | ||
| Middle school | 425 (10.7) | 183 (43.1) | 242 (56.9) | ||
| High school | 1304 (32.7) | 319 (24.5) | 985 (75.5) | ||
| ≥College | 1621 (40.7) | 232 (14.3) | 1389 (85.7) | ||
| Income level | 2.322 | 0.508 | |||
| Low | 921 (23.1) | 253 (27.5) | 668 (72.5) | ||
| Low middle | 1011 (25.4) | 272 (26.9) | 739 (73.1) | ||
| Upper middle | 1017 (25.5) | 280 (27.5) | 737 (72.5) | ||
| High | 1035 (26.0) | 258 (24.9) | 777 (75.1) | ||
| Occupation | 73.219 *** | <0.001 | |||
| Unemployed | 1426 (35.8) | 495 (34.7) | 931 (65.3) | ||
| Employed | 2558 (64.2) | 568 (22.2) | 1990 (77.8) | ||
| Health Insurance | 68.370 *** | <0.001 | |||
| Self-employed | 1251 (31.4) | 339 (27.1) | 912 (72.9) | ||
| Employment-based | 2591 (65.0) | 644 (24.9) | 1947 (75.1) | ||
| Medicaid | 142 (3.6) | 62 (43.7) | 80 (56.3) | ||
| Sleep duration 2 | 6.75 ± 1.32 | 6.53 ± 1.47 | 6.83 ± 1.25 | 6.284 *** | <0.001 |
| <6 | 748 (18.8) | 273 (36.5) | 475 (63.5) | 49.856 *** | <0.001 |
| 6.0–6.9 | 1082 (27.1) | 267 (24.7) | 815 (75.3) | ||
| 7.0–7.9 | 1183 (29.7) | 272 (23.0) | 911 (77.0) | ||
| 8.0–8.9 | 771 (19.4) | 191 (24.8) | 580 (75.2) | ||
| ≥9 | 200 (5.0) | 60 (30.0) | 140 (70.0) | ||
| Smoking | 30.475 *** | <0.001 | |||
| Non-smoker | 2185 (54.9) | 522 (23.9) | 1663 (76.1) | ||
| Current-smoker | 714 (17.9) | 184 (25.8) | 530 (74.2) | ||
| Ex-smoker | 1085 (27.2) | 357 (32.9) | 728 (67.1) | ||
| Drinking frequency | 44.056 *** | <0.001 | |||
| Never | 917 (23.0) | 311 (33.9) | 606 (66.1) | ||
| Rarely | 816 (20.5) | 189 (23.2) | 627 (76.8) | ||
| Occasionally | 1294 (32.5) | 289 (22.3) | 1005 (77.7) | ||
| Frequently | 957 (24.0) | 274 (28.6) | 683 (71.4) | ||
| Physical activity 3 | 11.344 ** | 0.010 | |||
| 0 | 757 (19.0) | 224 (29.6) | 533 (70.4) | ||
| 1–3 | 1185 (29.7) | 283 (23.9) | 902 (76.1) | ||
| 4–6 | 956 (24.0) | 243 (25.4) | 713 (74.6) | ||
| 7 | 1086 (27.3) | 313 (28.8) | 773 (71.2) | ||
| BMI 4 | 155.849 *** | <0.001 | |||
| Underweight | 116 (2.9) | 11 (9.5) | 105 (90.5) | ||
| Normal | 2293 (57.6) | 465 (20.3) | 1828 (79.7) | ||
| Overweight | 1575 (39.5) | 587 (37.3) | 988 (62.7) | ||
| Stress | 47.255 *** | <0.001 | |||
| Rarely stressed | 566 (14.2) | 213 (47.6) | 353 (62.4) | ||
| Slightly stressed | 2335 (58.6) | 612 (26.2) | 1723 (73.8) | ||
| Quite stressed | 892 (22.4) | 195 (21.9) | 697 (78.1) | ||
| Very stressed | 191 (4.8) | 43 (22.5) | 148 (77.5) | ||
| Diabetes | 262.232 *** | <0.001 | |||
| No | 3527 (88.5) | 797 (22.6) | 2730 (77.4) | ||
| Yes | 457 (11.5) | 266 (58.2) | 191 (41.8) | ||
| Variable | Sleep Duration 1, n (%) | χ2 | p-Value | ||||
|---|---|---|---|---|---|---|---|
| <6 | 6.0–6.9 | 7.0–7.9 | 8.0–8.9 | ≥9.0 | |||
| Sex | 10.850 * | 0.028 | |||||
| Male | 372 (19.3) | 522 (27.1) | 600 (31.1) | 353 (18.3) | 80 (4.2) | ||
| Female | 376 (18.3) | 560 (27.2) | 583 (28.3) | 418 (20.3) | 120 (5.8) | ||
| Age 2 | |||||||
| 30–49 | 204 (13.0) | 440 (28.1) | 517 (33.0) | 324 (20.7) | 82 (5.2) | 104.838 *** | <0.001 |
| 50–69 | 373 (20.8) | 504 (28.1) | 512 (28.5) | 342 (19.1) | 63 (3.5) | ||
| ≥70 | 171 (27.4) | 138 (22.2) | 154 (24.7) | 105 (16.9) | 55 (8.8) | ||
| Marital status | 8.652 | 0.070 | |||||
| Not married | 53 (13.7) | 103 (26.6) | 126 (32.5) | 85 (22.0) | 20 (5.2) | ||
| Married | 695 (19.3) | 979 (27.2) | 1057 (29.4) | 686 (19.1) | 180 (5.0) | ||
| Education level | 119.251 *** | <0.001 | |||||
| ≤primary education | 189 (29.8) | 153 (24.1) | 140 (22.1) | 105 (16.6) | 47 (7.4) | ||
| Middle school | 106 (24.9) | 109 (25.6) | 100 (23.5) | 87 (20.6) | 23 (5.4) | ||
| High school | 222 (17.0) | 354 (27.2) | 393 (30.1) | 263 (20.2) | 72 (5.5) | ||
| ≥College | 231 (14.3) | 466 (28.7) | 550 (33.9) | 316 (19.5) | 58 (3.6) | ||
| Income level | 24.781 * | 0.016 | |||||
| Low | 201 (21.8) | 255 (27.7) | 238 (25.8) | 173 (18.8) | 54 (5.9) | ||
| Low middle | 186 (18.4) | 243 (24.0) | 320 (31.7) | 209 (20.7) | 53 (5.2) | ||
| Upper middle | 193 (19.0) | 291 (28.6) | 303 (29.8) | 182 (17.9) | 48 (4.7) | ||
| High | 168 (16.2) | 293 (28.3) | 322 (31.1) | 207 (20.0) | 45 (4.4) | ||
| Occupation | 70.790 *** | <0.001 | |||||
| Unemployed | 317 (22.2) | 337 (23.6) | 366 (25.7) | 296 (20.8) | 110 (7.7) | ||
| Employed | 431 (16.8) | 745 (29.1) | 817 (31.9) | 475 (18.6) | 90 (3.6) | ||
| Health Insurance | 31.436 *** | <0.001 | |||||
| Self-employed | 242 (19.3) | 339 (27.1) | 359 (28.7) | 240 (19.2) | 71 (5.7) | ||
| Employment- based | 458 (17.7) | 712 (27.5) | 798 (30.8) | 504 (19.4) | 119 (4.6) | ||
| Medicaid | 48 (33.8) | 31 (21.8) | 26 (18.3) | 27 (19.1) | 10 (7.0) | ||
| Variable | Coefficient | 95% CI | t | p-Value | |
|---|---|---|---|---|---|
| Min | Max | ||||
| Sex | |||||
| Male | Ref | ||||
| Female | 0.049 | −0.036 | 0.135 | 1.129 | 0.259 |
| Age 1 | |||||
| 30–49 | Ref | ||||
| 50–69 | −0.300 | −0.402 | −0.199 | −5.790 *** | <0.001 |
| ≥70 | −0.279 | −0.436 | −0.121 | −3.466 *** | <0.001 |
| Marital status | |||||
| Not married | Ref | ||||
| Married | −0.135 | −0.282 | 0.011 | −1.815 | 0.070 |
| Education level | |||||
| ≤primary education | Ref | ||||
| Middle school | 0.158 | −0.005 | 0.322 | 1.896 | 0.058 |
| High school | 0.308 | 0.167 | 0.449 | 4.296 *** | <0.001 |
| ≥College | 0.266 | 0.118 | 0.414 | 3.522 *** | <0.001 |
| Income level | |||||
| Low | Ref | ||||
| Low middle | 0.148 | 0.029 | 0.266 | 2.447 * | 0.014 |
| Upper middle | 0.071 | −0.050 | 0.191 | 1.149 | 0.251 |
| High | 0.128 | 0.006 | 0.250 | 2.062 * | 0.039 |
| Occupation | |||||
| Unemployed | Ref | ||||
| Employed | −0.049 | −0.142 | 0.044 | −1.037 | 0.300 |
| Health Insurance | |||||
| Self-employed | Ref | ||||
| Employment-based | 0.029 | −0.060 | 0.119 | 0.641 | 0.522 |
| Medicaid | −0.309 | −0.542 | −0.076 | −2.595 ** | 0.009 |
| Variable | Sleep Duration 1, n (%) | χ2 | p-Value | ||||
|---|---|---|---|---|---|---|---|
| <6 | 6.0–6.9 | 7.0–7.9 | 8.0–8.9 | ≥9.0 | |||
| Smoking | 20.322 | 0.061 | |||||
| Non-smoker | 393 (18.3) | 594 (27.2) | 620 (28.4) | 465 (21.3) | 113 (5.2) | ||
| Current-smoker | 152 (21.3) | 194 (27.2) | 229 (32.1) | 104 (14.6) | 35 (4.9) | ||
| Ex-smoker | 203 (18.7) | 294 (27.1) | 334 (30.8) | 202 (18.6) | 52 (4.8) | ||
| Drinking frequency | 17.329 | 0.138 | |||||
| Never | 197 (21.5) | 222 (24.2) | 260 (28.4) | 183 (20.0) | 55 (6.0) | ||
| Rarely | 132 (16.2) | 228 (27.9) | 251 (30.8) | 158 (19.4) | 47 (5.8) | ||
| Occasionally | 227 (17.5) | 379 (29.3) | 383 (29.6) | 252 (19.5) | 53 (4.1) | ||
| Frequently | 192 (20.1) | 253 (26.4) | 289 (30.2) | 178 (18.6) | 45 (4.7) | ||
| Physical activity 2 | 73.958 *** | <0.001 | |||||
| 0 | 159 (21.0) | 189 (25.0) | 218 (28.8) | 146 (19.3) | 45 (5.9) | ||
| 1–3 | 218 (18.4) | 342 (28.9) | 322 (27.2) | 237 (20.0) | 66 (5.6) | ||
| 4–6 | 171 (17.9) | 270 (28.2) | 305 (31.9) | 174 (18.2) | 36 (3.8) | ||
| 7 | 200 (18.4) | 281 (25.9) | 338 (31.1) | 214 (19.7) | 53 (4.9) | ||
| BMI 3 | 19.394 * | 0.013 | |||||
| Underweight | 19 (16.4) | 27 (23.3) | 39 (33.6) | 26 (22.4) | 5 (4.3) | ||
| Normal | 383 (16.7) | 605 (26.4) | 712 (31.1) | 478 (20.8) | 115 (5.0) | ||
| Overweight | 346 (22.0) | 450 (28.6) | 432 (27.4) | 267 (17.0) | 80 (5.1) | ||
| Stress | 29.226 *** | <0.001 | |||||
| Rarely stressed | 88 (15.5) | 133 (23.5) | 168 (29.7) | 137 (24.2) | 40 (7.1) | ||
| Slightly stressed | 388 (16.6) | 652 (27.9) | 737 (31.6) | 447 (19.1) | 111 (4.8) | ||
| Quite stressed | 206 (23.1) | 252 (28.3) | 240 (26.9) | 154 (17.3) | 40 (4.5) | ||
| Very stressed | 66 (34.6) | 45 (23.6) | 38 (19.9) | 33 (17.3) | 9 (4.7) | ||
| Diabetes | 75.546 *** | <0.001 | |||||
| No | 676 (17.9) | 1049 (27.7) | 1146 (30.3) | 735 (19.4) | 175 (4.6) | ||
| Yes | 72 (35.5) | 33 (16.3) | 37 (18.2) | 36 (17.7) | 25 (12.3) | ||
| Variable | Coefficient | 95% CI | t | p-Value | |
|---|---|---|---|---|---|
| Min | Max | ||||
| Smoking | |||||
| Non-smoker | Ref | ||||
| Current-smoker | −0.077 | −0.195 | 0.040 | −1.287 | 0.198 |
| Ex-smoker | −0.028 | −0.127 | 0.072 | −0.542 | 0.588 |
| Drinking frequency | |||||
| Never | Ref | ||||
| Rarely | 0.123 | −0.002 | 0.248 | 1.929 | 0.054 |
| Occasionally | 0.086 | −0.027 | 0.199 | 1.494 | 0.135 |
| Frequently | 0.070 | −0.055 | 0.196 | 1.103 | 0.270 |
| Physical activity 1 | |||||
| 0 | Ref | ||||
| 1–3 | 0.057 | −0.064 | 0.177 | 0.921 | 0.357 |
| 4–6 | −0.005 | −0.131 | 0.121 | −0.074 | 0.941 |
| 7 | 0.019 | −0.104 | 0.142 | 0.304 | 0.761 |
| BMI 2 | |||||
| Underweight | Ref | ||||
| Normal | −0.049 | −0.295 | 0.197 | −0.389 | 0.697 |
| Overweight | −0.215 | −0.464 | 0.035 | −1.688 | 0.092 |
| Stress | |||||
| Rarely stressed | Ref | ||||
| Slightly stressed | −0.130 | −0.251 | −0.009 | −2.100 * | 0.036 |
| Quite stressed | −0.302 | −0.441 | −0.163 | −4.250 *** | 0.000 |
| Very stressed | −0.549 | −0.766 | −0.332 | −4.971 *** | 0.000 |
| Diabetes | |||||
| No | Ref | ||||
| Yes | −0.101 | −0.231 | 0.028 | −1.534 | 0.125 |
| Crude Model 1 | Adjusted Model 1 2 | Adjusted Model 2 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | OR | 95% CI | OR | 95% CI | OR | 95% CI | |||
| Min | Max | Max | Max | Min | Max | ||||
| Sleep duration 4 | |||||||||
| <6 | 1.00 | 1.00 | 1.00 | ||||||
| 6.0–6.9 | 0.57 *** | 0.47 | 0.70 | 0.78 * | 0.63 | 0.98 | 0.82 | 0.65 | 1.04 |
| 7.0–7.9 | 0.52 *** | 0.42 | 0.64 | 0.74 ** | 0.59 | 0.92 | 0.79 | 0.63 | 1.00 |
| 8.0–8.9 | 0.57 *** | 0.46 | 0.71 | 0.76 * | 0.60 | 0.98 | 0.80 | 0.62 | 1.04 |
| ≥9 | 0.75 | 0.53 | 1.04 | 0.81 | 0.55 | 1.19 | 0.77 | 0.51 | 1.14 |
| Sex | |||||||||
| Male | 1.00 | 1.00 | |||||||
| Female | 0.57 *** | 0.48 | 0.67 | 0.63 *** | 0.53 | 0.75 | |||
| Age 5 | |||||||||
| 30–49 | 1.00 | 1.00 | |||||||
| 50–69 | 4.60 *** | 3.66 | 5.77 | 4.56 *** | 3.60 | 5.79 | |||
| ≥70 | 8.55 *** | 6.37 | 11.49 | 9.12 *** | 6.67 | 12.48 | |||
| Education level | |||||||||
| ≤primary education | 1.00 | 1.00 | |||||||
| Middle school | 0.85 | 0.65 | 1.10 | 0.97 | 0.73 | 1.28 | |||
| High school | 0.60 *** | 0.48 | 0.76 | 0.68 ** | 0.53 | 0.88 | |||
| ≥College | 0.41 *** | 0.32 | 0.53 | 0.46 *** | 0.35 | 0.60 | |||
| Income level | |||||||||
| Low | 1.00 | 1.00 | |||||||
| Low middle | 1.08 | 0.86 | 1.36 | 1.05 | 0.83 | 1.33 | |||
| Upper middle | 1.17 | 0.92 | 1.47 | 1.14 | 0.90 | 1.45 | |||
| High | 1.16 | 0.91 | 1.47 | 1.11 | 0.86 | 1.42 | |||
| Occupation | |||||||||
| Unemployed | 1.00 | 1.00 | |||||||
| Employed | 0.85 | 0.71 | 1.01 | 0.84 | 0.70 | 1.01 | |||
| Health Insurance | |||||||||
| Self-employed | 1.00 | 1.00 | |||||||
| Employment-based | 1.08 | 0.91 | 1.29 | 1.06 | 0.89 | 1.27 | |||
| Medicaid | 2.21 *** | 1.48 | 3.31 | 1.95 ** | 1.28 | 2.96 | |||
| Physical activity 6 | |||||||||
| 0 | 1.00 | ||||||||
| 1–3 | 1.00 | 0.79 | 1.28 | ||||||
| 4–6 | 1.03 | 0.80 | 1.32 | ||||||
| 7 | 1.07 | 0.84 | 1.35 | ||||||
| BMI 7 | |||||||||
| Underweight | 1.00 | ||||||||
| Normal | 1.91 | 0.95 | 3.82 | ||||||
| Overweight | 5.10 *** | 2.54 | 10.24 | ||||||
| Stress | |||||||||
| Rarely stressed | 1.00 | ||||||||
| Slightly stressed | 0.88 | 0.71 | 1.10 | ||||||
| Quite stressed | 0.94 | 0.71 | 1.23 | ||||||
| Very stressed | 0.93 | 0.59 | 1.44 | ||||||
| Diabetes | |||||||||
| No | |||||||||
| Yes | 2.53 *** | 2.02 | 3.17 | ||||||
| Cox & Snell R2/ Nagelkerke’s R2 | 0.012/0.017 | 0.181/0.264 | 0.227/0.330 | ||||||
| χ2(df), p-value | 47.811(4), <0.001 | 795.14(16), <0.001 | 1024.227(25), <0.001 | ||||||
| Hosmer–Lemeshow Test χ2(df), p-value | 0.000(3), 1.000 | 14.767(8), 0.064 | 13.138(8), 0.106 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, M.-J.; Seo, B.-J.; Song, I. Sleep Deficit as a Risk Factor for Hypertension in Korean Adults. Sustainability 2023, 15, 2586. https://doi.org/10.3390/su15032586
Lee M-J, Seo B-J, Song I. Sleep Deficit as a Risk Factor for Hypertension in Korean Adults. Sustainability. 2023; 15(3):2586. https://doi.org/10.3390/su15032586
Chicago/Turabian StyleLee, Mi-Joon, Bum-Jeun Seo, and Inmyung Song. 2023. "Sleep Deficit as a Risk Factor for Hypertension in Korean Adults" Sustainability 15, no. 3: 2586. https://doi.org/10.3390/su15032586
APA StyleLee, M.-J., Seo, B.-J., & Song, I. (2023). Sleep Deficit as a Risk Factor for Hypertension in Korean Adults. Sustainability, 15(3), 2586. https://doi.org/10.3390/su15032586







