Practices Pursuing the Sustainability of A Healthcare Organization: A Systematic Review
Abstract
1. Introduction
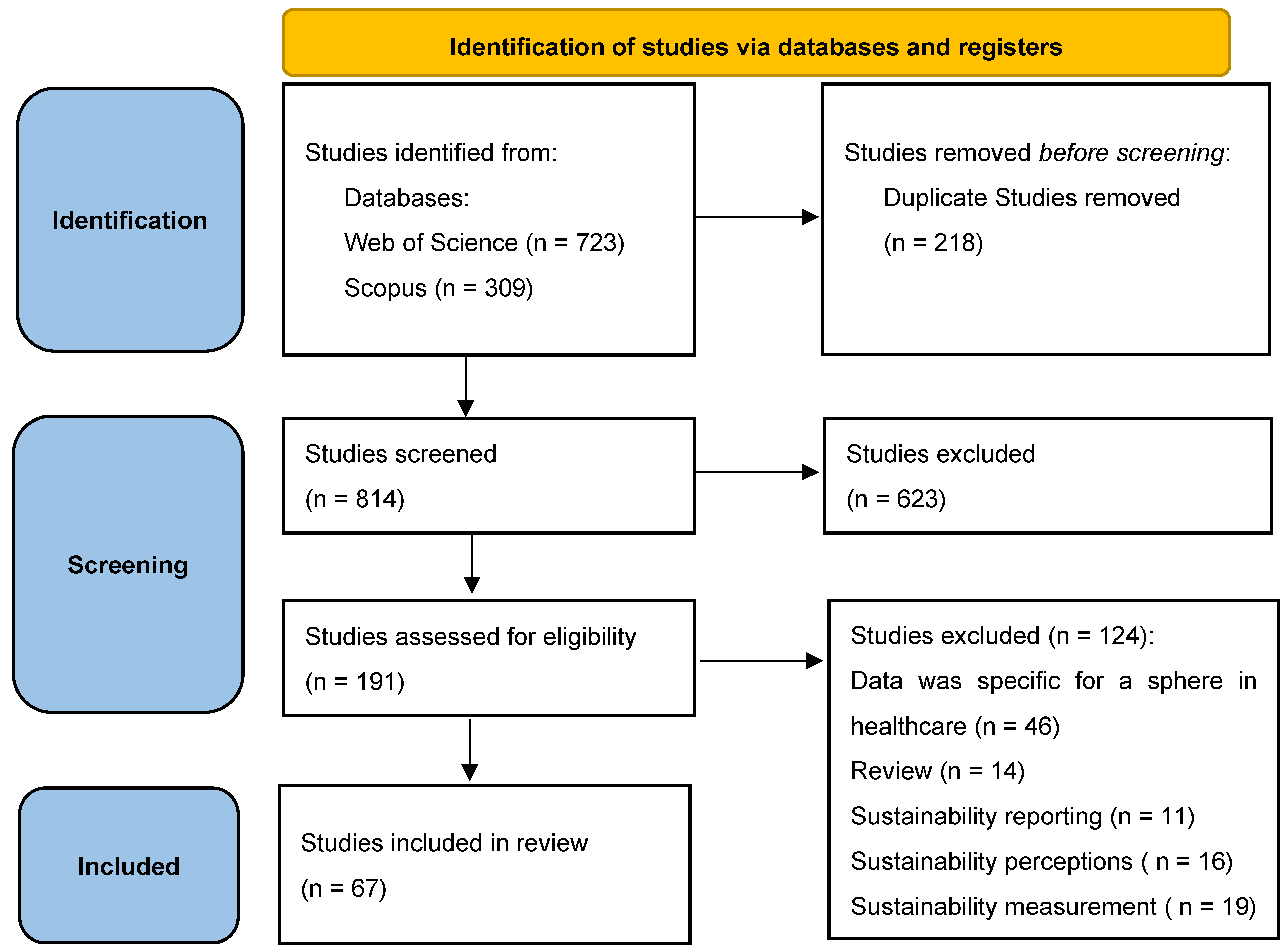
2. Materials and Methods
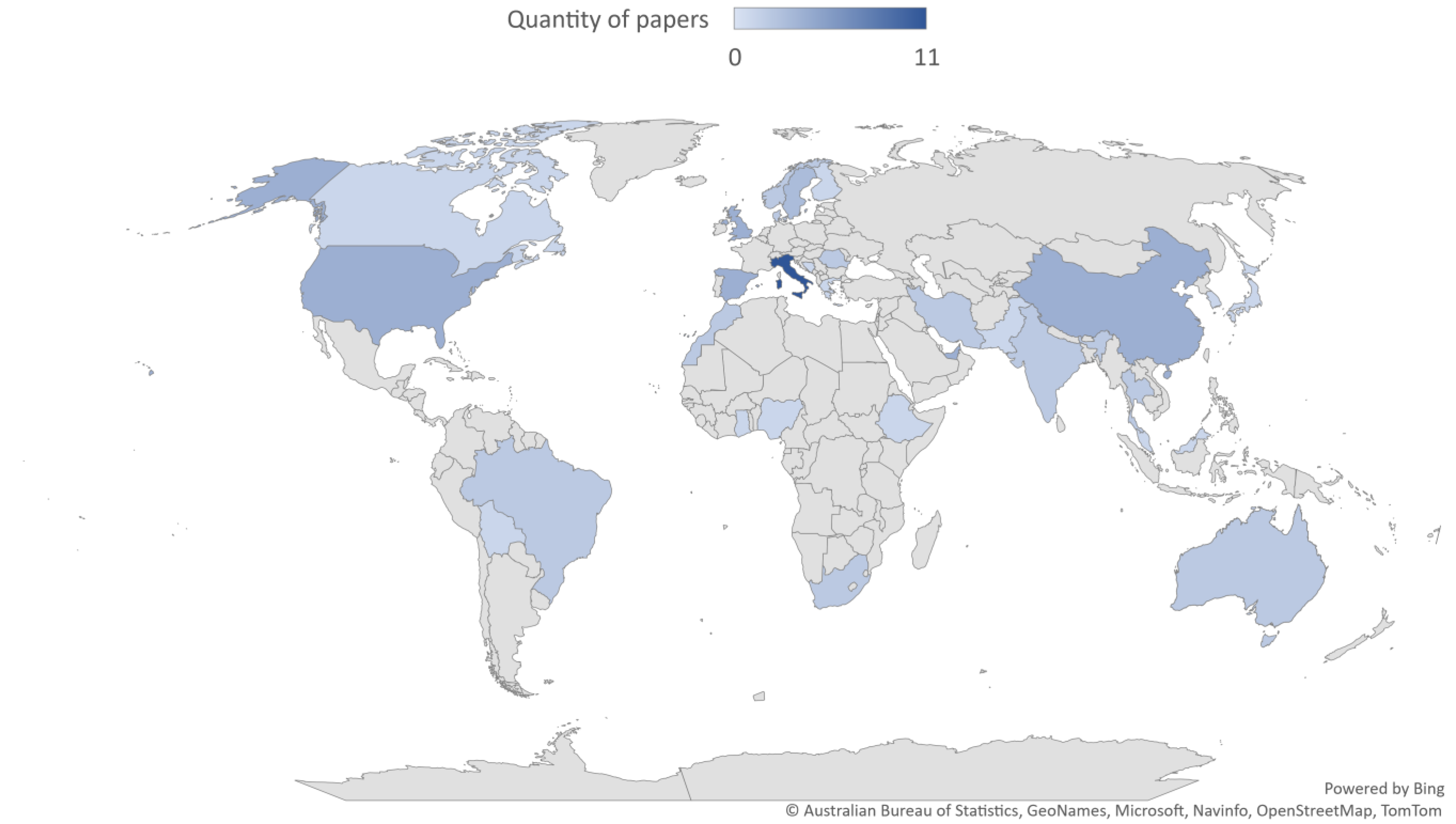
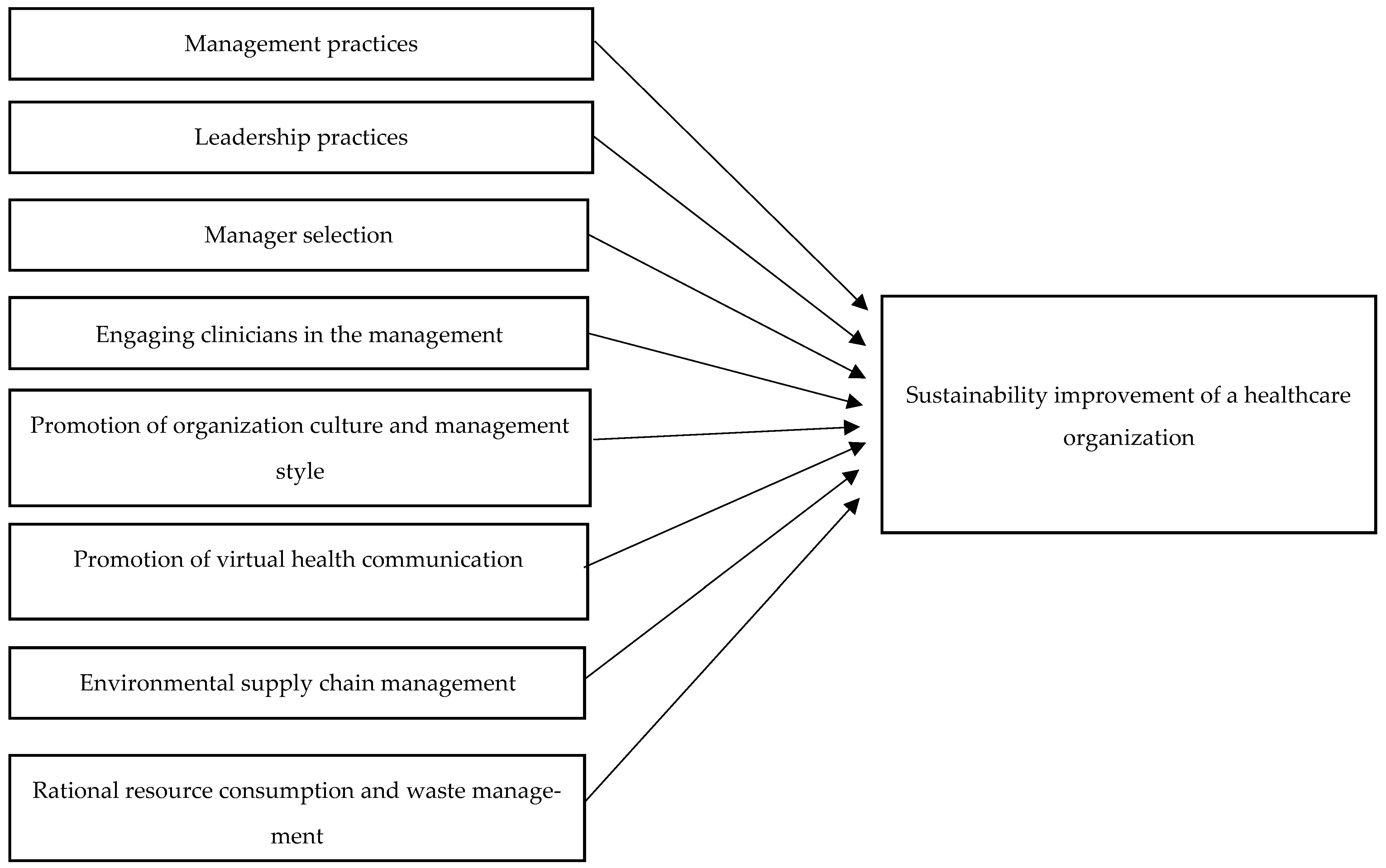
3. Results and Discussion
3.1. Sustainability
3.2. Improvements in Management Practices
3.3. Leadership Practices
3.4. Manager Selection
3.5. Engaging Clinicians in the Management
3.6. Promotion of Organization Culture and Management Style
3.7. Promotion of Virtual Health Communication
3.8. Environmental Supply Chain Management
3.9. Rational Resource Consumption and Waste Management
4. Conclusions
5. Recommendations and Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Author (Year) | Title | Journal | Keywords | ||
|---|---|---|---|---|---|
| 1. | [123] | Beaulieu, M., & Bentahar, O. (2021) | Digitalization of the healthcare supply chain: A roadmap to generate benefits and effectively support healthcare delivery | Technological Forecasting and Social Change | Supply chain; digital supply chain; logistics, healthcare delivery; benefits; technology |
| 2. | [80] | Cafagna, G., Seghieri, C., Vainieri, M., & Nuti, S. (2018) | A turnaround strategy: Improving equity in order to achieve quality of care and financial sustainability in Italy | International Journal for Equity in Health | Health equity; socioeconomic status; education, financial sustainability; quality of care; heart failure; Italy; performance management; clinical pathway |
| 3. | [8] | Cavicchi, C., Oppi, C., & Vagnoni, E. (2022) | Back and Forth on Sustainable Development: A Focus on Healthcare Organisations | Sustainability | Sustainable development; healthcare; intellectual capital; survey; Italy |
| 4. | [48] | Chandra, Y., Shang, L., & Roy, M. J. (2022) | Understanding Healthcare Social Enterprises: A New Public Governance Perspective | Journal of Social Policy | Social enterprise; healthcare; health; intervention; New Public Governance |
| 5. | [158] | Chauhan, A. (2020) | Framework for Sustainable Healthcare Waste Management in India | Transforming Organizations Through Flexible Systems Management | Healthcare waste disposal firms; healthcare waste management framework; multi-criteria decision-making methods; optimization and statistical modeling; sustainability |
| 6. | [107] | Chellaiyan, V. (2020) | Telemedicine: A Paradigm Shift in Healthcare in the wake of COVID-19 in India | Journal of Clinical and Diagnostic Research | Accessibility; health service; sustainability; teleconsultation |
| 7. | [71] | Chi, Y., Yu, C., Qi, X., & Xu, H. (2018) | Knowledge Management in Healthcare Sustainability: A Smart Healthy Diet Assistant in Traditional Chinese Medicine Culture | Sustainability | Healthcare sustainability; healthcare education; healthy diet; knowledge graph; traditional Chinese medicine |
| 8. | [96] | Conte, F., Vitale, P., Vollero, A., & Siano, A. (2018) | Designing a Data Visualization Dashboard for Managing the Sustainability Communication of Healthcare Organizations on Facebook | Sustainability | Sustainability communication management; data visualization dashboard; healthcare organizations; social media; user engagement; managerial dashboard |
| 9. | [127] | Damoah, I. S., Ayakwah, A., & Tingbani, I. (2021) | Artificial intelligence (AI)-enhanced medical drones in the healthcare supply chain (HSC) for sustainability development: A case study | Journal of Cleaner Production | Sustainability; sustainable development; medical drone; AI technology; public healthcare delivery; supply chain management; developing countries |
| 10. | [106] | Dunne, H., Rizan, C., Jones, A., Bhutta, M. F., Taylor, T., Barna, S., Taylor, C. J., & Okorie, M. (2022) | Effectiveness of an online module: Climate-change and sustainability in clinical practice | BMC Medical Education | Sustainability; climate-change; online; multimedia |
| 11. | [114] | Emilsson, M., Ernstson, U., Gustavsson, L., & Svensson, A. (2020) | Sustainable Innovations in Small Enterprises for the Transformation of the Primary Healthcare Sector | Sustainability | Healthcare; digital innovation; sustainability; small enterprises; incremental development; collaborative learning; knowledge integration |
| 12. | [108] | Faezipour, M., & Faezipour, M. (2020) | Sustainable Smartphone-Based Healthcare Systems: A Systems Engineering Approach to Assess the Efficacy of Respiratory Monitoring Apps | Sustainability | System dynamics; modeling; systems engineering; sustainability; respiration |
| 13. | [143] | Faezipour, M., & Ferreira, S. (2018) | A System Dynamics Approach for Sustainable Water Management in Hospitals | IEEE Systems Journal | Healthcare; hospitals; simulation; sustainability; system dynamics; systems thinking; water sustainability |
| 14. | [91] | Faggini, M., Cosimato, S., Nota, F. D., & Nota, G. (2019) | Pursuing Sustainability for Healthcare through Digital Platforms | Sustainability | Sustainability; healthcare; patient-centeredness; digital platforms; interaction type |
| 15. | [88] | Fally, M., Møller, M. E. E., Anhøj, J., Tarp, B., Benfield, T., & Ravn, P. (2022) | Sustainability of healthcare improvements for patients admitted with community-acquired pneumonia: Follow-up data from a quality improvement project | BMJ Open Quality | Sustainability; healthcare; community-acquired pneumonia |
| 16. | [159] | Ferronato, N., Ragazzi, M., Torrez Elias, M. S., Gorritty Portillo, M. A., Guisbert Lizarazu, E. G., & Torretta, V. (2020) | Application of healthcare waste indicators for assessing infectious waste management in Bolivia | Waste Management & Research | Developing countries; circular economy; sustainable development; waste management indicators; management tools |
| 17. | [144] | Gómez-Chaparro, M., García Sanz-Calcedo, J., & Armenta-Márquez, L. (2018) | Study on the use and consumption of water in Spanish private hospitals as related to healthcare activity | Urban Water Journal | Water consumption; healthcare engineering; hospital environmental quality; sustainable water management |
| 18. | [35] | Haddiya, I., Janfi, T., & Guedira, M. (2020) | Application of the Concepts of Social Responsibility, Sustainability, and Ethics to Healthcare Organizations | Risk Management and Healthcare Policy | CSR; sustainability; ethics; healthcare |
| 19. | [128] | Hussain, M., Ajmal, M. M., Gunasekaran, A., & Khan, M. (2018) | Exploration of social sustainability in healthcare supply chain | Journal of Cleaner Production | Social sustainability; healthcare supply chain; stakeholder theory |
| 20. | [129] | Hussain, M., Khan, M., & Ajmal, M. (2019) | Exploration and assessment of the motivators of social sustainability in healthcare supply chains: Multistake holder’s perspective | Sustainable Development | AHP; healthcare supply chain; motivators; social sustainability; stakeholder theory |
| 21. | [115] | Ianculescu, M., & Alexandru, A. (2020) | Microservices—A Catalyzer for Better Managing Healthcare Data Empowerment | Studies in Informatics and Control | Microservices; remote healthcare monitoring system; data empowerment; scalability |
| 22. | [60] | Iandolo, F., Vito, P., Fulco, I., & Loia, F. (2018) | From Health Technology Assessment to Health Technology Sustainability | Sustainability | Health technology assessment; evaluation methods; viable systems approach; healthcare; sustainability |
| 23. | [72] | Karamat, J., Shurong, T., Ahmad, N., Afridi, S., Khan, S., & Mahmood, K. (2019) | Promoting Healthcare Sustainability in Developing Countries: Analysis of Knowledge Management Drivers in Public and Private Hospitals of Pakistan | International Journal of Environmental Research and Public Health | Healthcare sustainability; drivers; knowledge management; interpretive structural modeling; developing countries; Pakistan |
| 24. | [9] | Katz, C. (2022) | The Ethical Duty to Reduce the Ecological Footprint of Industrialized Healthcare Services and Facilities | Journal of Medicine and Philosophy | Andrew Jameton; beneficence; distributive justice; Jessica Pierce; rationing; sustainability |
| 25. | [69] | Ketprapakorn, N., & Kantabutra, S. (2019) | Sustainable Social Enterprise Model: Relationships and Consequences | Sustainability | Sustainable enterprise; corporate sustainability; social enterprise; social healthcare enterprise; sufficiency economy; brand management; socioeconomic |
| 26. | [130] | Khan, M., Hussain, M., Gunasekaran, A., Ajmal, M. M., & Helo, P. T. (2018) | Motivators of social sustainability in healthcare supply chains in the UAE-Stakeholder perspective | Sustainable Production and Consumption | Healthcare supply chains; social sustainability; motivators; UAE |
| 27. | [131] | Khosravi, F., & Izbirak, G. (2019) | A stakeholder perspective of social sustainability measurement in healthcare supply chain management | Sustainable Cities and Society | Social sustainability; sustainability fluctuation; performance measurement; exponentially distributed indicators; stakeholder theory |
| 28. | [10] | Lee, S. M., & Lee, D. (2022) | Developing Green Healthcare Activities in the Total Quality Management Framework | International Journal of Environmental Research and Public Health | Green healthcare; continuous improvement activities; total quality management framework; healthcare industry |
| 29. | [50] | Leite, H., Bateman, N., & Radnor, Z. (2020) | Beyond the ostensible: An exploration of barriers to lean implementation and sustainability in healthcare | Production Planning & Control | Lean production; leanhealthcare; leanimplementation; barriers;public healthcare |
| 30. | [151] | Li, H., Dietl, H., & Li, J. (2021) | Identifying key factors influencing sustainable element in healthcare waste management using the interval-valued fuzzy DEMATEL method | Journal of Material Cycles and Waste Management | Key factor identification; sustainable element; healthcare waste management; interval-valued fuzzy DEMATEL method |
| 31. | [150] | Li, H., Li, J., Zhang, Z., Cao, X., Zhu, J., & Chen, W. (2020) | Establishing an interval-valued fuzzy decision-making method for sustainable selection of healthcare waste treatment technologies in the emerging economies | Journal of Material Cycles and Waste Management | Healthcare waste treatment technology; multi-criteria decision making; interval-valued fuzzy DEMATEL; interval-valued fuzzy TOPSIS; sustainability |
| 32. | [86] | Lister, H. E., Mostert, K., Botha, T., van der Linde, S., van Wyk, E., Rocher, S.-A., Laing, R., Wu, L., Müller, S., des Tombe, A., Kganyago, T., Zwane, N., Mphogo, B., & Maric, F. (2022) | South African Healthcare Professionals’ Knowledge, Attitudes, and Practices Regarding Environmental Sustainability in Healthcare: A Mixed-Methods Study | International Journal of Environmental Research and Public Health | Environmental sustainability; sustainable healthcare; occupational therapy; physiotherapy; planetary health; climate change; healthcare professions |
| 33. | [46] | Liu, X.-L., Wang, T., Tan, J.-Y., Stewart, S., Chan, R. J., Eliseeva, S., Polotan, M. J., & Zhao, I. (2022) | Sustainability of healthcare professionals’ adherence to clinical practice guidelines in primary care | BMC Primary Care | Sustainability; healthcare professionals; adherence; clinical practice guidelines; primary care |
| 34. | [109] | Lo Presti, L., Testa, M., Marino, V., & Singer, P. (2019) | Engagement in Healthcare Systems: Adopting Digital Tools for a Sustainable Approach | Sustainability | Engagement platform; digital health; social sustainability |
| 35. | [152] | Makan, A., & Fadili, A. (2021) | Sustainability assessment of healthcare waste treatment systems using surrogate weights and PROMETHEE method | Waste Management & Research | Sustainability assessment; healthcare waste; treatment systems; surrogate weights; Preference Ranking Organization Method for Enrichment Evaluations |
| 36. | [153] | Maniero Moreira, A. M., & Risso Guenther, W. M. (2019) | Healthcare Waste Management in a Brazilian Higher Education and Health Research Institution | Sustainability on University Campuses: Learning, Skills Building and Best Practices | Sustainability; university; waste management; healthcare waste; hazardous waste |
| 37. | [147] | Meleko, A., Tesfaye, T., & Henok, A. (2018) | Assessment of Healthcare Waste Generation Rate and Its Management System in Health Centers of Bench Maji Zone | Ethiopian Journal of Health Sciences | Healthcare waste; health center; healthcare waste Generation rate; hazardous waste; general waste |
| 38. | [62] | Moldovan, F., Blaga, P., Moldovan, L., & Bataga, T. (2022) | An Innovative Framework for Sustainable Development in Healthcare: The Human Rights Assessment | International Journal of Environmental Research and Public Health | Healthcare; sustainable development; human rights; assessment; reference framework; facility |
| 39. | [36] | Munthe, C., Fumagalli, D., & Malmqvist, E. (2021) | Sustainability principle for the ethics of healthcare resource allocation | Journal of Medical Ethics | Sustainability; ethics; healthcare resource allocation |
| 40. | [111] | Newbould, L., Ariss, S., Mountain, G., & Hawley, M. S. (2021) | Exploring factors that affect the uptake and sustainability of videoconferencing for healthcare provision for older adults in care homes: A realist evaluation | Bmc Medical Informatics and Decision Making | Videoconferencing; care homes; older adults; admissions; implementation; sustainability; uptake, remote consultation |
| 41. | [133] | Nsikan, J., Affiah, E. A., Briggs, I., & Koko, N. (2022) | Sustainable supplier selection factors and supply chain performance in the Nigerian healthcare industry | Journal of Transport and Supply Chain Management | Sustainability; supplier selection; procurement; triple bottom line; sustainable supply chain management |
| 42. | [37] | Nyholm, L., Salmela, S., Nystrom, L., & Koskinen, C. (2018) | Sustainability in care through an ethical practice model | Nursing Ethics | Care; ethics; hermeneutic application research; model; sustainability |
| 43. | [119] | Poba-Nzaou, P., Kume, N., & Kobayashi, S. (2020) | Developing and Sustaining an Open Source Electronic Health Record: Evidence from a Field Study in Japan | Journal of Medical Systems | Electronic health records; open source; sustainability; governance; Japan |
| 44. | [38] | Previtali, P., & Cerchiello, P. (2018) | The Prevention of Corruption as an Unavoidable Way to Ensure Healthcare System Sustainability | Sustainability | Healthcare sustainability; anti-corruption; healthcare organizations; corruption prevention plan; healthcare management; compliance |
| 45. | [154] | Puska, A., Stevic, Z., & Pamucar, D. (2022) | Evaluation and selection of healthcare waste incinerators using extended sustainability criteria and multi-criteria analysis methods | Environment Development and Sustainability | Medical waste; compromise ranking of alternatives from distance to ideal solution (CRADIS); incinerators; full consistency method (FUCOM); Bosnia and Herzegovina |
| 46. | [155] | Ranjbari, M., Esfandabadi, Z. S., Shevchenko, T., Chassagnon-Haned, N., Peng, W., Tabatabaei, M., & Aghbashlo, M. (2022) | Mapping healthcare waste management research: Past evolution, current challenges, and future perspectives towards a circular economy transition | Journal of Hazardous Materials | Waste management; healthcare waste; circular economy; environmental sustainability; hazardous waste; medical waste |
| 47. | [52] | Rattan, T. K., Joshi, M., Vesty, G., & Sharma, S. (2022) | Sustainability indicators in public healthcare: A factor analysis approach | Journal of Cleaner Production | Sustainability; sustainable development goals (SDGs); Ayurveda; healthcare delivery; confirmatory factor analysis; exploratory factor analysis |
| 48. | [112] | Remondino, M. (2018) | Information Technology in Healthcare: HHC-MOTES, a Novel Set of Metrics to Analyse IT Sustainability in Different Areas | Sustainability | Information technology; healthcare; measurement; efficiency; performance; managerial perspective; key performance indicators; decision support; HHC-MOTES framework |
| 49. | [87] | Rodriguez, R., Svensson, G., & Eriksson, D. (2018) | Organizational positioning and planning of sustainability initiatives: Logic and differentiators | International Journal of Public Sector Management | Hospitals; planning; triple bottom line; corporate social responsibility; sustainability; positioning |
| 50. | [135] | Rodriguez, R., Svensson, G., & Eriksson, D. (2021) | Priorities Determining Future Directions of Sustainable Development in Business Models of the Healthcare Industry-Findings and Framework | Sustainability | Sustainable development; sustainability; business model; supply chain; healthcare; Spain |
| 51. | [134] | Rodriguez, R., Svensson, G., & Otero-Neira, C. (2019) | Future direction of sustainable development in private hospitals: General similarities and specific differences | Journal of Business & Industrial Marketing | Healthcare; Spain; sustainable development; sustainability management; private hospital |
| 52. | [53] | Rodriguez, R., Svensson, G., & Wood, G. (2020) | Sustainability trends in public hospitals: Efforts and priorities | Evaluation and Program Planning | Sustainable development; healthcare; trends |
| 53. | [54] | Rodriguez, R., Svensson, G., & Wood, G. (2020) | Assessing corporate planning of future sustainability initiatives in private healthcare organizations | Evaluation and Program Planning | Healthcare; hospital; private; sustainability; corporate; planning |
| 54. | [94] | Russo, G., Tartaglione, A. M., & Cavacece, Y. (2019) | Empowering Patients to Co-Create a Sustainable Healthcare Value | Sustainability | Healthcare sustainability; patient empowerment; value co-creation; structural equation modeling |
| 55. | [44] | Saviano, M., Bassano, C., Piciocchi, P., Di Nauta, P., & Lettieri, M. (2018) | Monitoring Viability and Sustainability in Healthcare Organizations | Sustainability | Healthcare organizations; control; viability; sustainability; systems monitoring |
| 56. | [136] | Scavarda, A., Dau, G. L., Scavarda, L. F., & Korzenowski, A. L. (2019) | A proposed healthcare supply chain management framework in the emerging economies with the sustainable lenses: The theory, the practice, and the policy | Resources Conservation and Recycling | Supply chain; sustainability; healthcare; emerging economy; corporate social responsibility; education |
| 57. | [124] | Schutte, C., Niemann, W., & Kotz, é T. (2022) | Exploring Relationship Power in Supply Chain Sustainability Practices: a Case Study of a South African Hospital Group | South African Journal of Industrial Engineering | Supply chain; sustainability; South African Hospital Group |
| 58. | [156] | Sepetis, A., Zaza, P. N., Rizos, F., & Bagos, P. G. (2022) | Identifying and Predicting Healthcare Waste Management Costs for an Optimal Sustainable Management System: Evidence from the Greek Public Sector | International Journal of Environmental Research and Public Health | Climate change; public health; waste management; healthcare waste; medical waste; sustainability in healthcare; Greece |
| 59. | [141] | Singh, P. (2019) | Lean in healthcare organization: An opportunity for environmental sustainability | Benchmarking-an International Journal | Lean; environmental sustainability; ecology; lean in healthcare organization |
| 60. | [70] | Suriyankietkaew, S., & Kungwanpongpun, P. (2021) | Strategic leadership and management factors driving sustainability in health-care organizations in Thailand | Journal of Health Organization and Management | Leadership; sustainable leadership; sustainable healthcare; pharmaceutical companies; sustainability; performance; factor analysis; SDG; Thailand |
| 61. | [63] | Tooranloo, H. S., Karimi, S., & Vaziri, K. (2018) | Analysis of the Factors Affecting Sustainable Electronic Supply Chains in Healthcare Centers: An Interpretive-Structural Modeling Approach | Information Resources Management Journal | Electronic supply chain; Healthcare centers; interpretive–structural modeling approach; sustainable supply chain |
| 62. | [157] | Torkayesh, A. E., Vandchali, H. R., & Tirkolaee, E. B. (2021) | Multi-Objective Optimization for Healthcare Waste Management Network Design with Sustainability Perspective | Sustainability | Healthcare waste management; sustainability; waste network design; multi-objective optimization; multi-choice goal programming |
| 63. | [113] | Visconti, R. M., Martiniello, L., Morea, D., & Gebennini, E. (2019) | Can Public-Private Partnerships Foster Investment Sustainability in Smart Hospitals? | Sustainability | Project financing; infrastructures; social impact investments; results-based financing (RBF); value co-creation; supply chain; patient-centered care; value-based healthcare; availability payment; bankability |
| 64. | [105] | Wadmann, S., & Hoeyer, K. (2018) | Dangers of the digital fit: Rethinking seamlessness and social sustainability in data-intensive healthcare | Big Data & Society | Denmark; digital fit; electronic medical record; infrastructure; seamlessness; sustainability |
| 65. | [11] | Wagrell, S., Havenvid, M. I., Linné, Å., & Sundquist, V. (2022) | Building sustainable hospitals: A resource interaction perspective | Industrial Marketing Management | Social and economic sustainability; healthcare; hospitals; resource interaction |
| 66. | [12] | Weimann, L., & Weimann, E. (2022) | On the Road to Net Zero Health Care Systems: Governance for Sustainable Health Care in the United Kingdom and Germany | International Journal of Environmental Research and Public Health | Governance; healthcare; systems-thinking; net zero; sustainable development; public health; NHS UK; German healthcare; healthcare law; planetary health |
| 67. | [138] | Zhu, Q., Johnson, S., & Sarkis, J. (2018) | Lean six sigma and environmental sustainability: A hospital perspective | Supply Chain Forum: An International Journal | Healthcare; hospitals; supply chain; environmental sustainability; lean and Six Sigma; green |
References
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development | Department of Economic and Social Affairs. Available online: https://sdgs.un.org/2030agenda (accessed on 22 December 2022).
- UNDP. Socio-Economic Impact of COVID-19 | United Nations Development Programme. Available online: https://www.undp.org/coronavirus/socio-economic-impact-covid-19 (accessed on 1 December 2022).
- United Nations. Everyone Included: Social Impact of COVID-19 | DISD. Available online: https://www.un.org/development/desa/dspd/everyone-included-covid-19.html (accessed on 1 December 2022).
- World Health Organization. Impact of COVID-19 on People’s Livelihoods, Their Health and Our Food Systems. Available online: https://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people’s-livelihoods-their-health-and-our-food-systems (accessed on 1 December 2022).
- Grazhevska, N.; Mostepaniuk, A. The Development of Corporate Social Responsibility in the Context of Overcoming a Welfare State Crisis: A Theoretical and Empirical Analysis. Comp. Econ. Res. Cent. East. Eur. 2021, 24, 123–140. [Google Scholar] [CrossRef]
- Purvis, B.; Mao, Y.; Robinson, D. Three Pillars of Sustainability: In Search of Conceptual Origins. Sustain. Sci. 2019, 14, 681–695. [Google Scholar] [CrossRef]
- Danese, P.; Manfè, V.; Romano, P. A Systematic Literature Review on Recent Lean Research: State-of-the-Art and Future Directions. Int. J. Manag. Rev. 2018, 20, 579–605. [Google Scholar] [CrossRef]
- Cavicchi, C.; Oppi, C.; Vagnoni, E. Back and Forth on Sustainable Development: A Focus on Healthcare Organisations. Sustainability 2022, 14, 4958. [Google Scholar] [CrossRef]
- Katz, C. The Ethical Duty to Reduce the Ecological Footprint of Industrialized Healthcare Services and Facilities. J. Med. Philos. 2022, 47, 32–53. [Google Scholar] [CrossRef]
- Lee, S.M.; Lee, D. Developing Green Healthcare Activities in the Total Quality Management Framework. Int. J. Environ. Res. Public Health 2022, 19, 6504. [Google Scholar] [CrossRef] [PubMed]
- Wagrell, S.; Havenvid, M.I.; Linné, Å.; Sundquist, V. Building Sustainable Hospitals: A Resource Interaction Perspective. Ind. Mark. Manag. 2022, 106, 420–431. [Google Scholar] [CrossRef]
- Weimann, L.; Weimann, E. On the Road to Net Zero Health Care Systems: Governance for Sustainable Health Care in the United Kingdom and Germany. Int. J. Environ. Res. Public Health 2022, 19, 12167. [Google Scholar] [CrossRef]
- Fisch, C.; Block, J. Six Tips for Your (Systematic) Literature Review in Business and Management Research. Manag. Rev. Q. 2018, 68, 103–106. [Google Scholar] [CrossRef]
- PRISMA. Available online: https://prisma-statement.org/Protocols/ProtocolGuidance (accessed on 23 November 2022).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Brundtland, G.H. Our Common Future—Call for Action. Environ. Conserv. 1987, 14, 291–294. [Google Scholar] [CrossRef]
- Du Plessis, C. Towards a Regenerative Paradigm for the Built Environment. Build. Res. Inf. 2012, 40, 7–22. [Google Scholar] [CrossRef]
- Ives, C.D.; Freeth, R.; Fischer, J. Inside-out Sustainability: The Neglect of Inner Worlds. Ambio 2020, 49, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Lenton, T.M.; Rockström, J.; Gaffney, O.; Rahmstorf, S.; Richardson, K.; Steffen, W.; Schellnhuber, H.J. Climate Tipping Points—Too Risky to Bet Against. Nature 2019, 575, 592–595. [Google Scholar] [CrossRef]
- Living Planet Report 2016. Available online: https://www.worldwildlife.org/pages/living-planet-report-2016 (accessed on 23 November 2022).
- Bastianoni, S.; Coscieme, L.; Caro, D.; Marchettini, N.; Pulselli, F.M. The Needs of Sustainability: The Overarching Contribution of Systems Approach. Ecol. Indic. 2019, 100, 69–73. [Google Scholar] [CrossRef]
- Miller, T.R.; Wiek, A.; Sarewitz, D.; Robinson, J.; Olsson, L.; Kriebel, D.; Loorbach, D. The Future of Sustainability Science: A Solutions-Oriented Research Agenda. Sustain. Sci. 2014, 9, 239–246. [Google Scholar] [CrossRef]
- Mostepaniuk, A.; Nasr, E.; Awwad, R.I.; Hamdan, S.; Aljuhmani, H.Y. Managing a Relationship between Corporate Social Responsibility and Sustainability: A Systematic Review. Sustainability 2022, 14, 11203. [Google Scholar] [CrossRef]
- Wiek, A.; Ness, B.; Schweizer-Ries, P.; Brand, F.S.; Farioli, F. From Complex Systems Analysis to Transformational Change: A Comparative Appraisal of Sustainability Science Projects. Sustain. Sci. 2012, 7, 5–24. [Google Scholar] [CrossRef]
- National Research Council. Our Common Journey: A Transition Toward Sustainability; National Academies Press: Washington, DC, USA, 1999; ISBN 978-0-309-08638-7. [Google Scholar]
- Fang, X.; Zhou, B.; Tu, X.; Ma, Q.; Wu, J. “What Kind of a Science Is Sustainability Science?” An Evidence-Based Reexamination. Sustainability 2018, 10, 1478. [Google Scholar] [CrossRef]
- Miller, T.R. Constructing Sustainability Science: Emerging Perspectives and Research Trajectories. Sustain. Sci. 2013, 8, 279–293. [Google Scholar] [CrossRef]
- Wiek, A. Solving Sustainability Problems Tools for a New Generation of Professionals. Available online: https://www.coursehero.com/file/44150058/Solving-Sustainability-Problems-Bookpdf/ (accessed on 23 November 2022).
- Polimeni, J.M.; Polimeni, R.I. Jevons’ Paradox and the Myth of Technological Liberation. Ecol. Complex. 2006, 3, 344–353. [Google Scholar] [CrossRef]
- Sterman, J.D. Sustaining Sustainability: Creating a Systems Science in a Fragmented Academy and Polarized World. In Sustainability Science: The Emerging Paradigm and the Urban Environment; Weinstein, M.P., Turner, R.E., Eds.; Springer: New York, NY, USA, 2012; pp. 21–58. ISBN 978-1-4614-3188-6. [Google Scholar]
- Du Plessis, C.; Brandon, P. An Ecological Worldview as Basis for a Regenerative Sustainability Paradigm for the Built Environment. J. Clean. Prod. 2015, 109, 53–61. [Google Scholar] [CrossRef]
- González-Márquez, I.; Toledo, V.M. Sustainability Science: A Paradigm in Crisis? Sustainability 2020, 12, 2802. [Google Scholar] [CrossRef]
- Abson, D.J.; Fischer, J.; Leventon, J.; Newig, J.; Schomerus, T.; Vilsmaier, U.; von Wehrden, H.; Abernethy, P.; Ives, C.D.; Jager, N.W.; et al. Leverage Points for Sustainability Transformation. Ambio 2017, 46, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Gibbons, L.V. Moving Beyond Sustainability: A Regenerative Community Development Framework for Co-Creating Thriving Living Systems and Its Application. J. Sustain. Dev. 2020, 13, 20. [Google Scholar] [CrossRef]
- Haddiya, I.; Janfi, T.; Guedira, M. Application of the Concepts of Social Responsibility, Sustainability, and Ethics to Healthcare Organizations. Risk Manag. Healthc. Policy 2020, 13, 1029–1033. [Google Scholar] [CrossRef] [PubMed]
- Munthe, C.; Fumagalli, D.; Malmqvist, E. Sustainability Principle for the Ethics of Healthcare Resource Allocation. J. Med. Ethics 2021, 47, 90–97. [Google Scholar] [CrossRef]
- Nyholm, L.; Salmela, S.; Nystrom, L.; Koskinen, C. Sustainability in Care through an Ethical Practice Model. Nurs. Ethics 2018, 25, 264–272. [Google Scholar] [CrossRef]
- Previtali, P.; Cerchiello, P. The Prevention of Corruption as an Unavoidable Way to Ensure Healthcare System Sustainability. Sustainability 2018, 10, 3071. [Google Scholar] [CrossRef]
- Grazhevska, N.; Mostepaniuk, A. Ecological Components of Corporate Social Responsibility: Theoretical Background and Practical Implementation. J. Environ. Manag. Tour. 2020, 11, 1060–1066. [Google Scholar] [CrossRef]
- Kroll, C.; Warchold, A.; Pradhan, P. Sustainable Development Goals (SDGs): Are We Successful in Turning Trade-Offs into Synergies? Palgrave Commun. 2019, 5, 140. [Google Scholar] [CrossRef]
- Mang, P.; Reed, B. Designing from Place: A Regenerative Framework and Methodology. Build. Res. Inf. 2012, 40, 23–38. [Google Scholar] [CrossRef]
- Gibbons, L.V.; Pearthree, G.; Cloutier, S.A.; Ehlenz, M.M. The Development, Application, and Refinement of a Regenerative Development Evaluation Tool and Indicators. Ecol. Indic. 2020, 108, 105698. [Google Scholar] [CrossRef]
- Hes, D.; Stephan, A.; Moosavi, S. Evaluating the Practice and Outcomes of Applying Regenerative Development to a Large-Scale Project in Victoria, Australia. Sustainability 2018, 10, 460. [Google Scholar] [CrossRef]
- Saviano, M.; Bassano, C.; Piciocchi, P.; Di Nauta, P.; Lettieri, M. Monitoring Viability and Sustainability in Healthcare Organizations. Sustainability 2018, 10, 3548. [Google Scholar] [CrossRef]
- Dickinson, H.; Ham, C. Engaging Doctors in Leadership: What Can We Learn from International Experience and Research Evidence; University of Birmingham, Health Services Management Centre: Birmingham, UK, 2008. [Google Scholar]
- Liu, X.-L.; Wang, T.; Tan, J.-Y.; Stewart, S.; Chan, R.J.; Eliseeva, S.; Polotan, M.J.; Zhao, I. Sustainability of Healthcare Professionals’ Adherence to Clinical Practice Guidelines in Primary Care. BMC Prim. Care 2022, 23, 36. [Google Scholar] [CrossRef]
- Street, A.; Carr-Hill, R.; Posnett, J. Is Hospital Performance Related to Expenditure on Management? J. Health Serv. Res. Policy 1999, 4, 16–23. [Google Scholar] [CrossRef]
- Chandra, Y.; Shang, L.; Roy, M.J. Understanding Healthcare Social Enterprises: A New Public Governance Perspective. J. Soc. Policy 2022, 51, 834–855. [Google Scholar] [CrossRef]
- Kumar, K.S.; Babu, R.V.; Paranitharan, K.P. Application of Integrated Lean Six Sigma Quality Healthcare System Practice in Indian Healthcare. Int. J. Value Chain Manag. 2022, 13, 112–139. [Google Scholar] [CrossRef]
- Leite, H.; Bateman, N.; Radnor, Z. Beyond the Ostensible: An Exploration of Barriers to Lean Implementation and Sustainability in Healthcare. Prod. Plan. Control 2020, 31, 1–18. [Google Scholar] [CrossRef]
- Mazzocato, P.; Savage, C.; Brommels, M.; Aronsson, H.; Thor, J. Lean Thinking in Healthcare: A Realist Review of the Literature. BMJ Qual. Saf. 2010, 19, 376–382. [Google Scholar] [CrossRef]
- Rattan, T.K.; Joshi, M.; Vesty, G.; Sharma, S. Sustainability Indicators in Public Healthcare: A Factor Analysis Approach. J. Clean. Prod. 2022, 370, 133253. [Google Scholar] [CrossRef]
- Rodriguez, R.; Svensson, G.; Wood, G. Sustainability Trends in Public Hospitals: Efforts and Priorities. Eval. Program Plann. 2020, 78, 101742. [Google Scholar] [CrossRef]
- Rodriguez, R.; Svensson, G.; Wood, G. Assessing Corporate Planning of Future Sustainability Initiatives in Private Healthcare Organizations. Eval. Program Plann. 2020, 83, 101869. [Google Scholar] [CrossRef]
- Alimo-Metcalfe, B.; Alban-Metcalfe, J.; Bradley, M.; Mariathasan, J.; Samele, C. The Impact of Engaging Leadership on Performance, Attitudes to Work and Wellbeing at Work: A Longitudinal Study. J. Health Organ. Manag. 2008, 22, 586–598. [Google Scholar] [CrossRef]
- Landry, S.; Beaulieu, M.; Roy, J. Strategy Deployment in Healthcare Services: A Case Study Approach. Technol. Forecast. Soc. Change 2016, 113, 429–437. [Google Scholar] [CrossRef]
- Layton, D.; Bloom, N.; Homkes, R.; Sadun, R. Management in Healthcare: Why Good Practice Really Matters; Stephen Dorgan McKinsey & Company: London, UK, 2010; 28p. [Google Scholar]
- McKone-Sweet, K.E.; Hamilton, P.; Willis, S.B. The Ailing Healthcare Supply Chain: A Prescription for Change. J. Supply Chain Manag. 2005, 41, 4–17. [Google Scholar] [CrossRef]
- Budgett, A.; Gopalakrishnan, M.; Schneller, E. Procurement in Public & Private Hospitals in Australia and Costa Rica—A Comparative Case Study. Health Syst. 2017, 6, 56–67. [Google Scholar] [CrossRef]
- Iandolo, F.; Vito, P.; Fulco, I.; Loia, F. From Health Technology Assessment to Health Technology Sustainability. Sustainability 2018, 10, 4748. [Google Scholar] [CrossRef]
- Karliner, J.; Guenther, R. The Global Green and Healthy Hospitals Agenda. Available online: https://noharm-global.org/issues/global/global-green-and-healthy-hospitals-agenda (accessed on 23 November 2022).
- Moldovan, F.; Blaga, P.; Moldovan, L.; Bataga, T. An Innovative Framework for Sustainable Development in Healthcare: The Human Rights Assessment. Int. J. Environ. Res. Public Health 2022, 19, 2222. [Google Scholar] [CrossRef]
- Tooranloo, H.S.; Karimi, S.; Vaziri, K. Analysis of the Factors Affecting Sustainable Electronic Supply Chains in Healthcare Centers: An Interpretive-Structural Modeling Approach. Inf. Resour. Manag. J. 2018, 31, 23–43. [Google Scholar] [CrossRef]
- World Health Organization. Healthy Hospitals, Healthy Planet, Healthy People. Available online: https://www.who.int/publications/m/item/healthy-hospitals-healthy-planet-healthy-people (accessed on 23 November 2022).
- Kotter, J.P. Leading Change; Harvard Business Press: Harvard, MA, USA, 2012; ISBN 978-1-4221-8643-5. [Google Scholar]
- Gilmartin, M.J.; D’Aunno, T.A. 8 Leadership Research in Healthcare. Acad. Manag. Ann. 2007, 1, 387–438. [Google Scholar] [CrossRef]
- Hackman, J.R.; Hackman, R.J. Leading Teams: Setting the Stage for Great Performances; Harvard Business Press: Harvard, MA, USA, 2002; ISBN 978-1-57851-333-8. [Google Scholar]
- Kelle, P.; Woosley, J.; Schneider, H. Pharmaceutical Supply Chain Specifics and Inventory Solutions for a Hospital Case. Oper. Res. Health Care 2012, 1, 54–63. [Google Scholar] [CrossRef]
- Ketprapakorn, N.; Kantabutra, S. Sustainable Social Enterprise Model: Relationships and Consequences. Sustainability 2019, 11, 3772. [Google Scholar] [CrossRef]
- Suriyankietkaew, S.; Kungwanpongpun, P. Strategic Leadership and Management Factors Driving Sustainability in Health-Care Organizations in Thailand. J. Health Organ. Manag. 2021, 36, 448–468. [Google Scholar] [CrossRef]
- Chi, Y.; Yu, C.; Qi, X.; Xu, H. Knowledge Management in Healthcare Sustainability: A Smart Healthy Diet Assistant in Traditional Chinese Medicine Culture. Sustainability 2018, 10, 4197. [Google Scholar] [CrossRef]
- Karamat, J.; Shurong, T.; Ahmad, N.; Afridi, S.; Khan, S.; Mahmood, K. Promoting Healthcare Sustainability in Developing Countries: Analysis of Knowledge Management Drivers in Public and Private Hospitals of Pakistan. Int. J. Environ. Res. Public Health 2019, 16, 508. [Google Scholar] [CrossRef]
- Bloom, N.; Propper, C.; Seiler, S.; Van Reenen, J. The Impact of Competition on Management Quality: Evidence from Public Hospitals. Rev. Econ. Stud. 2015, 82, 457–489. [Google Scholar] [CrossRef]
- Goodall, A.H. Physician-Leaders and Hospital Performance: Is There an Association? Soc. Sci. Med. 2011, 73, 535–539. [Google Scholar] [CrossRef]
- Mascia, D.; Piconi, I. Career Histories and Managerial Performance of Health Care Chief Executive Officers: An Empirical Study in the Italian National Health Service. Health Care Manag. Rev. 2013, 38, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Witman, Y.; Smid, G.A.C.; Meurs, P.L.; Willems, D.L. Doctor in the Lead: Balancing between Two Worlds. Available online: https://journals.sagepub.com/doi/abs/10.1177/1350508410380762 (accessed on 23 November 2022).
- Keroack, M.A.; Youngberg, B.J.; Cerese, J.L.; Krsek, C.; Prellwitz, L.W.; Trevelyan, E.W. Organizational Factors Associated with High Performance in Quality and Safety in Academic Medical Centers. Acad. Med. 2007, 82, 1178–1186. [Google Scholar] [CrossRef]
- Reinertsen, J.L.; Gosfield, A.; Rupp, W. Engaging Physicians in Ashared Quality Agenda. IHI Innov. Ser. White Pap. 2007, 65, 1–48. [Google Scholar]
- Spurgeon, P.; Mazelan, P.M.; Barwell, F. Medical Engagement: A Crucial Underpinning to Organizational Performance. Health Serv. Manag. Res. 2011, 24, 114–120. [Google Scholar] [CrossRef]
- Cafagna, G.; Seghieri, C.; Vainieri, M.; Nuti, S. A Turnaround Strategy: Improving Equity in Order to Achieve Quality of Care and Financial Sustainability in Italy. Int. J. Equity Health 2018, 17, 169. [Google Scholar] [CrossRef]
- Mannion, R.; Davies, H.T.O.; Marshall, M.N. Cultural Characteristics of “High” and “Low” Performing Hospitals. J. Health Organ. Manag. 2005, 19, 431–439. [Google Scholar] [CrossRef]
- Atun, R.A. Doctors and Managers Need to Speak a Common Language. BMJ 2003, 326, 655. [Google Scholar] [CrossRef]
- Curry, L.A.; Spatz, E.; Cherlin, E.; Thompson, J.W.; Berg, D.; Ting, H.H.; Decker, C.; Krumholz, H.M.; Bradley, E.H. What Distinguishes Top-Performing Hospitals in Acute Myocardial Infarction Mortality Rates? Ann. Intern. Med. 2011, 154, 384–390. [Google Scholar] [CrossRef]
- Detmer, D. Clinician-Managers: The ‘Boundary Spanners’ of Health Services. J. Health Serv. Res. Policy 2000, 5, 197–198. [Google Scholar] [CrossRef]
- Harrison, R.; Miller, S. The Contribution of Clinical Directors to the Strategic Capability of the Organization. Br. J. Manag. 1999, 10, 23–39. [Google Scholar] [CrossRef]
- Lister, H.E.; Mostert, K.; Botha, T.; van der Linde, S.; van Wyk, E.; Rocher, S.-A.; Laing, R.; Wu, L.; Müller, S.; des Tombe, A.; et al. South African Healthcare Professionals’ Knowledge, Attitudes, and Practices Regarding Environmental Sustainability in Healthcare: A Mixed-Methods Study. Int. J. Environ. Res. Public Health 2022, 19, 10121. [Google Scholar] [CrossRef]
- Rodriguez, R.; Svensson, G.; Eriksson, D. Organizational Positioning and Planning of Sustainability Initiatives: Logic and Differentiators. Int. J. Public Sect. Manag. 2018, 31, 755–774. [Google Scholar] [CrossRef]
- Fally, M.; Møller, M.E.E.; Anhøj, J.; Tarp, B.; Benfield, T.; Ravn, P. Sustainability of Healthcare Improvements for Patients Admitted with Community-Acquired Pneumonia: Follow-up Data from a Quality Improvement Project. BMJ Open Qual. 2022, 11, e001737. [Google Scholar] [CrossRef] [PubMed]
- Kukreja, P.; Sheehan, A.H.; Riggins, J. Use of Social Media by Pharmacy Preceptors. Am. J. Pharm. Educ. 2011, 75, 176. [Google Scholar] [CrossRef]
- Adams, S.A. Blog-Based Applications and Health Information: Two Case Studies That Illustrate Important Questions for Consumer Health Informatics (CHI) Research. Int. J. Med. Inf. 2010, 79, e89–e96. [Google Scholar] [CrossRef]
- Faggini, M.; Cosimato, S.; Nota, F.D.; Nota, G. Pursuing Sustainability for Healthcare through Digital Platforms. Sustainability 2019, 11, 165. [Google Scholar] [CrossRef]
- Hwang, K.O.; Ottenbacher, A.J.; Green, A.P.; Cannon-Diehl, M.R.; Richardson, O.; Bernstam, E.V.; Thomas, E.J. Social Support in an Internet Weight Loss Community. Int. J. Med. Inf. 2010, 79, 5–13. [Google Scholar] [CrossRef]
- Kim, K.; Kwon, N. Profile of E-Patients: Analysis of Their Cancer Information-Seeking From a National Survey. J. Health Commun. 2010, 15, 712–733. [Google Scholar] [CrossRef]
- Russo, G.; Tartaglione, A.M.; Cavacece, Y. Empowering Patients to Co-Create a Sustainable Healthcare Value. Sustainability 2019, 11, 1315. [Google Scholar] [CrossRef]
- Chou, W.-Y.S.; Hunt, Y.M.; Beckjord, E.B.; Moser, R.P.; Hesse, B.W. Social Media Use in the United States: Implications for Health Communication. J. Med. Internet Res. 2009, 11, e1249. [Google Scholar] [CrossRef]
- Conte, F.; Vitale, P.; Vollero, A.; Siano, A. Designing a Data Visualization Dashboard for Managing the Sustainability Communication of Healthcare Organizations on Facebook. Sustainability 2018, 10, 4447. [Google Scholar] [CrossRef]
- Kontos, E.Z.; Emmons, K.M.; Puleo, E.; Viswanath, K. Communication Inequalities and Public Health Implications of Adult Social Networking Site Use in the United States. J. Health Commun. 2010, 15, 216–235. [Google Scholar] [CrossRef] [PubMed]
- Scanfeld, D.; Scanfeld, V.; Larson, E.L. Dissemination of Health Information through Social Networks: Twitter and Antibiotics. Am. J. Infect. Control 2010, 38, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Correa, T.; Hinsley, A.W.; de Zúñiga, H.G. Who Interacts on the Web?: The Intersection of Users’ Personality and Social Media Use. Comput. Hum. Behav. 2010, 26, 247–253. [Google Scholar] [CrossRef]
- Sanford, A.A. “I Can Air My Feelings Instead of Eating Them”: Blogging as Social Support for the Morbidly Obese. Commun. Stud. 2010, 61, 567–584. [Google Scholar] [CrossRef]
- Takahashi, Y.; Uchida, C.; Miyaki, K.; Sakai, M.; Shimbo, T.; Nakayama, T. Potential Benefits and Harms of a Peer Support Social Network Service on the Internet for People With Depressive Tendencies: Qualitative Content Analysis and Social Network Analysis. J. Med. Internet Res. 2009, 11, e1142. [Google Scholar] [CrossRef] [PubMed]
- Friedman, D.B.; Koskan, A.; Rose, I.D. Prostate Cancer Guidelines on Web 2.0-Based Sites: The Screening Dilemma Continues Online. J. Cancer Educ. 2011, 26, 188–193. [Google Scholar] [CrossRef]
- Orizio, G.; Schulz, P.; Gasparotti, C.; Caimi, L.; Gelatti, U. The World of E-Patients: A Content Analysis of Online Social Networks Focusing on Diseases. Telemed. e-Health 2010, 16, 1060–1066. [Google Scholar] [CrossRef]
- Tian, Y. Organ Donation on Web 2.0: Content and Audience Analysis of Organ Donation Videos on YouTube. Health Commun. 2010, 25, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Wadmann, S.; Hoeyer, K. Dangers of the Digital Fit: Rethinking Seamlessness and Social Sustainability in Data-Intensive Healthcare. Big Data Soc. 2018, 5, 2053951717752964. [Google Scholar] [CrossRef]
- Dunne, H.; Rizan, C.; Jones, A.; Bhutta, M.F.; Taylor, T.; Barna, S.; Taylor, C.J.; Okorie, M. Effectiveness of an Online Module: Climate-Change and Sustainability in Clinical Practice. BMC Med. Educ. 2022, 22, 682. [Google Scholar] [CrossRef]
- Chellaiyan, V. Telemedicine: A Paradigm Shift in Healthcare in the Wake of COVID-19 in India. J. Clin. Diagn. Res. 2020, 14, LA01–LA03. [Google Scholar] [CrossRef]
- Faezipour, M.; Faezipour, M. Sustainable Smartphone-Based Healthcare Systems: A Systems Engineering Approach to Assess the Efficacy of Respiratory Monitoring Apps. Sustainability 2020, 12, 5061. [Google Scholar] [CrossRef]
- Lo Presti, L.; Testa, M.; Marino, V.; Singer, P. Engagement in Healthcare Systems: Adopting Digital Tools for a Sustainable Approach. Sustainability 2019, 11, 220. [Google Scholar] [CrossRef]
- McGain, F.; Naylor, C. Environmental Sustainability in Hospitals—A Systematic Review and Research Agenda. J. Health Serv. Res. Policy 2014, 19, 245–252. [Google Scholar] [CrossRef]
- Newbould, L.; Ariss, S.; Mountain, G.; Hawley, M.S. Exploring Factors That Affect the Uptake and Sustainability of Videoconferencing for Healthcare Provision for Older Adults in Care Homes: A Realist Evaluation. BMC Med. Inform. Decis. Mak. 2021, 21, 13. [Google Scholar] [CrossRef] [PubMed]
- Remondino, M. Information Technology in Healthcare: HHC-MOTES, a Novel Set of Metrics to Analyse IT Sustainability in Different Areas. Sustainability 2018, 10, 2721. [Google Scholar] [CrossRef]
- Visconti, R.M.; Martiniello, L.; Morea, D.; Gebennini, E. Can Public-Private Partnerships Foster Investment Sustainability in Smart Hospitals? Sustainability 2019, 11, 1704. [Google Scholar] [CrossRef]
- Emilsson, M.; Ernstson, U.; Gustavsson, L.; Svensson, A. Sustainable Innovations in Small Enterprises for the Transformation of the Primary Healthcare Sector. Sustainability 2020, 12, 6391. [Google Scholar] [CrossRef]
- Ianculescu, M.; Alexandru, A. Microservices—A Catalyzer for Better Managing Healthcare Data Empowerment. Stud. Inform. Control 2020, 29, 231–242. [Google Scholar] [CrossRef]
- Landry, S.; Philippe, R. How Logistics Can Service Healthcare. Supply Chain Forum Int. J. 2004, 5, 24–30. [Google Scholar] [CrossRef]
- Nabelsi, V.; Gagnon, S. Information Technology Strategy for a Patient-Oriented, Lean, and Agile Integration of Hospital Pharmacy and Medical Equipment Supply Chains. Int. J. Prod. Res. 2017, 55, 3929–3945. [Google Scholar] [CrossRef]
- Pan, Z.X.; Pokharel, S. Logistics in Hospitals: A Case Study of Some Singapore Hospitals. Leadersh. Health Serv. 2007, 20, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Poba-Nzaou, P.; Kume, N.; Kobayashi, S. Developing and Sustaining an Open Source Electronic Health Record: Evidence from a Field Study in Japan. J. Med. Syst. 2020, 44, 159. [Google Scholar] [CrossRef] [PubMed]
- Rakovska, M.A.; Stratieva, S.V. A Taxonomy of Healthcare Supply Chain Management Practices. Supply Chain Forum Int. J. 2018, 19, 4–24. [Google Scholar] [CrossRef]
- Romero, A.; Lefebvre, E. Combining Barcodes and RFID in a Hybrid Solution to Improve Hospital Pharmacy Logistics Processes. Int. J. Inf. Technol. Manag. 2015, 14, 97–123. [Google Scholar] [CrossRef]
- Beaulieu, M.; Roy, J.; Landry, S. L’impartition Des Activités Logistiques Dans Le Secteur de La Santé: Les Leçons d’une Expérience Canadienne. Can. J. Adm. Sci./Rev. Can. Sci. L’adm. 2018, 35, O68–O82. [Google Scholar] [CrossRef]
- Beaulieu, M.; Bentahar, O. Digitalization of the Healthcare Supply Chain: A Roadmap to Generate Benefits and Effectively Support Healthcare Delivery. Technol. Forecast. Soc. Change 2021, 167, 120717. [Google Scholar] [CrossRef]
- Schutte, C.; Niemann, W.; Kotzé, T. Exploring Relationship Power in Supply Chain Sustainability Practices: A Case Study of A South African Hospital Group. S. Afr. J. Ind. Eng. 2022, 33, 154–176. [Google Scholar] [CrossRef]
- Velasco, N.; Moreno, J.-P.; Rebolledo, C. Logistics Practices in Healthcare Organizations in Bogota. Acad. Rev. Latinoam. Adm. 2018, 31, 519–533. [Google Scholar] [CrossRef]
- Adebanjo, D.; Laosirihongthong, T.; Samaranayake, P. Prioritizing Lean Supply Chain Management Initiatives in Healthcare Service Operations: A Fuzzy AHP Approach. Prod. Plan. Control 2016, 27, 953–966. [Google Scholar] [CrossRef]
- Damoah, I.S.; Ayakwah, A.; Tingbani, I. Artificial Intelligence (AI)-Enhanced Medical Drones in the Healthcare Supply Chain (HSC) for Sustainability Development: A Case Study. J. Clean. Prod. 2021, 328, 129598. [Google Scholar] [CrossRef]
- Hussain, M.; Ajmal, M.M.; Gunasekaran, A.; Khan, M. Exploration of Social Sustainability in Healthcare Supply Chain. J. Clean. Prod. 2018, 203, 977–989. [Google Scholar] [CrossRef]
- Hussain, M.; Khan, M.; Ajmal, M. Exploration and Assessment of the Motivators of Social Sustainability in Healthcare Supply Chains: Multistake Holder’s Perspective. Sustain. Dev. 2019, 27, 573–586. [Google Scholar] [CrossRef]
- Khan, M.; Hussain, M.; Gunasekaran, A.; Ajmal, M.M.; Helo, P.T. Motivators of Social Sustainability in Healthcare Supply Chains in the UAE-Stakeholder Perspective. Sustain. Prod. Consum. 2018, 14, 95–104. [Google Scholar] [CrossRef]
- Khosravi, F.; Izbirak, G. A Stakeholder Perspective of Social Sustainability Measurement in Healthcare Supply Chain Management. Sustain. Cities Soc. 2019, 50, 101681. [Google Scholar] [CrossRef]
- Kritchanchai, D.; Hoeur, S.; Engelseth, P. Develop a Strategy for Improving Healthcare Logistics Performance. Supply Chain Forum Int. J. 2018, 19, 55–69. [Google Scholar] [CrossRef]
- Nsikan, J.; Affiah, E.A.; Briggs, I.; Koko, N. Sustainable Supplier Selection Factors and Supply Chain Performance in the Nigerian Healthcare Industry. J. Transp. Supply Chain Manag. 2022, 16, 8. [Google Scholar] [CrossRef]
- Rodriguez, R.; Svensson, G.; Otero-Neira, C. Future Direction of Sustainable Development in Private Hospitals: General Similarities and Specific Differences. J. Bus. Ind. Mark. 2019, 35, 537–550. [Google Scholar] [CrossRef]
- Rodriguez, R.; Svensson, G.; Eriksson, D. Priorities Determining Future Directions of Sustainable Development in Business Models of the Healthcare Industry-Findings and Framework. Sustainability 2021, 13, 6507. [Google Scholar] [CrossRef]
- Scavarda, A.; Dau, G.L.; Scavarda, L.F.; Korzenowski, A.L. A Proposed Healthcare Supply Chain Management Framework in the Emerging Economies with the Sustainable Lenses: The Theory, the Practice, and the Policy. Resour. Conserv. Recycl. 2019, 141, 418–430. [Google Scholar] [CrossRef]
- González González, A.; García-Sanz-Calcedo, J.; Salgado, D.R. A Quantitative Analysis of Final Energy Consumption in Hospitals in Spain. Sustain. Cities Soc. 2018, 36, 169–175. [Google Scholar] [CrossRef]
- Zhu, Q.; Johnson, S.; Sarkis, J. Lean Six Sigma and Environmental Sustainability: A Hospital Perspective. Supply Chain Forum Int. J. 2018, 19, 25–41. [Google Scholar] [CrossRef]
- Laureani, A.; Antony, J. Standards for Lean Six Sigma Certification. Int. J. Product. Perform. Manag. 2012, 61, 110–120. [Google Scholar] [CrossRef]
- Morgan, J.; Brenig-Jones, M. Lean Six Sigma For Dummies; John Wiley & Sons: Hoboken, NJ, USA, 2015; ISBN 978-1-119-06735-1. [Google Scholar]
- Singh, P. Lean in Healthcare Organization: An Opportunity for Environmental Sustainability. Benchmark.—Int. J. 2019, 26, 205–220. [Google Scholar] [CrossRef]
- Wheat, B.; Mills, C.; Carnell, M. Leaning Into Six Sigma: A Parable of the Journey to Six Sigma and a Lean Enterprise, 1st ed.; McGraw Hill: New York, NY, USA, 2003; ISBN 978-0-07-141432-6. [Google Scholar]
- Faezipour, M.; Ferreira, S. A System Dynamics Approach for Sustainable Water Management in Hospitals. IEEE Syst. J. 2018, 12, 1278–1285. [Google Scholar] [CrossRef]
- Gómez-Chaparro, M.; García Sanz-Calcedo, J.; Armenta-Márquez, L. Study on the Use and Consumption of Water in Spanish Private Hospitals as Related to Healthcare Activity. Urban Water J. 2018, 15, 601–608. [Google Scholar] [CrossRef]
- Victorian Government Department of Health. Guidelines for Water Reuse and Recycling in Victorian Health Care Facilities; Victorian Government Department of Health: Melbourne, VIC, Australia, 2009; 58p. [Google Scholar]
- McGain, F. Sustainable Hospitals? An Australian Perspective. Perspect. Public Health 2010, 130, 19–20. [Google Scholar] [CrossRef]
- Meleko, A.; Tesfaye, T.; Henok, A. Assessment of Healthcare Waste Generation Rate and Its Management System in Health Centers of Bench Maji Zone. Ethiop. J. Health Sci. 2018, 28, 125–134. [Google Scholar] [CrossRef]
- Ashourian, K.T.; Young, S.T. Greening Healthcare: The Current State of Sustainability in Manhattan’s Hospitals. Sustainability—J. Rec. 2016, 9, 73–79. [Google Scholar] [CrossRef]
- Doiphode, S.M.; Hinduja, I.N.; Ahuja, H.S. Developing a Novel, Sustainable and Beneficial System for the Systematic Management of Hospital Wastes. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5071971/ (accessed on 23 November 2022).
- Li, H.; Li, J.; Zhang, Z.; Cao, X.; Zhu, J.; Chen, W. Establishing an Interval-Valued Fuzzy Decision-Making Method for Sustainable Selection of Healthcare Waste Treatment Technologies in the Emerging Economies. J. Mater. Cycles Waste Manag. 2020, 22, 501–514. [Google Scholar] [CrossRef]
- Li, H.; Dietl, H.; Li, J. Identifying Key Factors Influencing Sustainable Element in Healthcare Waste Management Using the Interval-Valued Fuzzy DEMATEL Method. J. Mater. Cycles Waste Manag. 2021, 23, 1777–1790. [Google Scholar] [CrossRef]
- Makan, A.; Fadili, A. Sustainability Assessment of Healthcare Waste Treatment Systems Using Surrogate Weights and PROMETHEE Method. Waste Manag. Res. 2021, 39, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Maniero Moreira, A.M.; Risso Guenther, W.M. Healthcare Waste Management in a Brazilian Higher Education and Health Research Institution. In Sustainability on University Campuses: Learning, Skills Building and Best Practices; Filho, W.L., Bardi, U., Eds.; Springer International Publishing Ag: Cham, Switzerland, 2019; pp. 321–338. ISBN 978-3-030-15864-4. [Google Scholar]
- Puska, A.; Stevic, Z.; Pamucar, D. Evaluation and Selection of Healthcare Waste Incinerators Using Extended Sustainability Criteria and Multi-Criteria Analysis Methods. Environ. Dev. Sustain. 2022, 24, 11195–11225. [Google Scholar] [CrossRef]
- Ranjbari, M.; Esfandabadi, Z.S.; Shevchenko, T.; Chassagnon-Haned, N.; Peng, W.; Tabatabaei, M.; Aghbashlo, M. Mapping Healthcare Waste Management Research: Past Evolution, Current Challenges, and Future Perspectives towards a Circular Economy Transition. J. Hazard. Mater. 2022, 422, 126724. [Google Scholar] [CrossRef] [PubMed]
- Sepetis, A.; Zaza, P.N.; Rizos, F.; Bagos, P.G. Identifying and Predicting Healthcare Waste Management Costs for an Optimal Sustainable Management System: Evidence from the Greek Public Sector. Int. J. Environ. Res. Public Health 2022, 19, 9821. [Google Scholar] [CrossRef]
- Torkayesh, A.E.; Vandchali, H.R.; Tirkolaee, E.B. Multi-Objective Optimization for Healthcare Waste Management Network Design with Sustainability Perspective. Sustainability 2021, 13, 8279. [Google Scholar] [CrossRef]
- Chauhan, A. Framework for Sustainable Healthcare Waste Management in India. In Transforming Organizations through Flexible Systems Management; Suri, P.K., Yadav, R., Eds.; Flexible Systems Management; Springer: Singapore, 2020; pp. 189–204. ISBN 9789811396403. [Google Scholar]
- Ferronato, N.; Ragazzi, M.; Torrez Elias, M.S.; Gorritty Portillo, M.A.; Guisbert Lizarazu, E.G.; Torretta, V. Application of Healthcare Waste Indicators for Assessing Infectious Waste Management in Bolivia. Waste Manag. Res. 2020, 38, 4–18. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mostepaniuk, A.; Akalin, T.; Parish, M.R. Practices Pursuing the Sustainability of A Healthcare Organization: A Systematic Review. Sustainability 2023, 15, 2353. https://doi.org/10.3390/su15032353
Mostepaniuk A, Akalin T, Parish MR. Practices Pursuing the Sustainability of A Healthcare Organization: A Systematic Review. Sustainability. 2023; 15(3):2353. https://doi.org/10.3390/su15032353
Chicago/Turabian StyleMostepaniuk, Alla, Turgay Akalin, and Mohammad Reza Parish. 2023. "Practices Pursuing the Sustainability of A Healthcare Organization: A Systematic Review" Sustainability 15, no. 3: 2353. https://doi.org/10.3390/su15032353
APA StyleMostepaniuk, A., Akalin, T., & Parish, M. R. (2023). Practices Pursuing the Sustainability of A Healthcare Organization: A Systematic Review. Sustainability, 15(3), 2353. https://doi.org/10.3390/su15032353






