Assessing the Big Data Adoption Readiness Role in Healthcare between Technology Impact Factors and Intention to Adopt Big Data
Abstract
1. Introduction
2. Related Work
2.1. Healthcare in Developing Countries
2.2. Challenges in Healthcare Implementation in Developing Countries
2.3. Theoretical framework and Development Hypothesis
2.3.1. Technology–Organization–Environment (TOE)
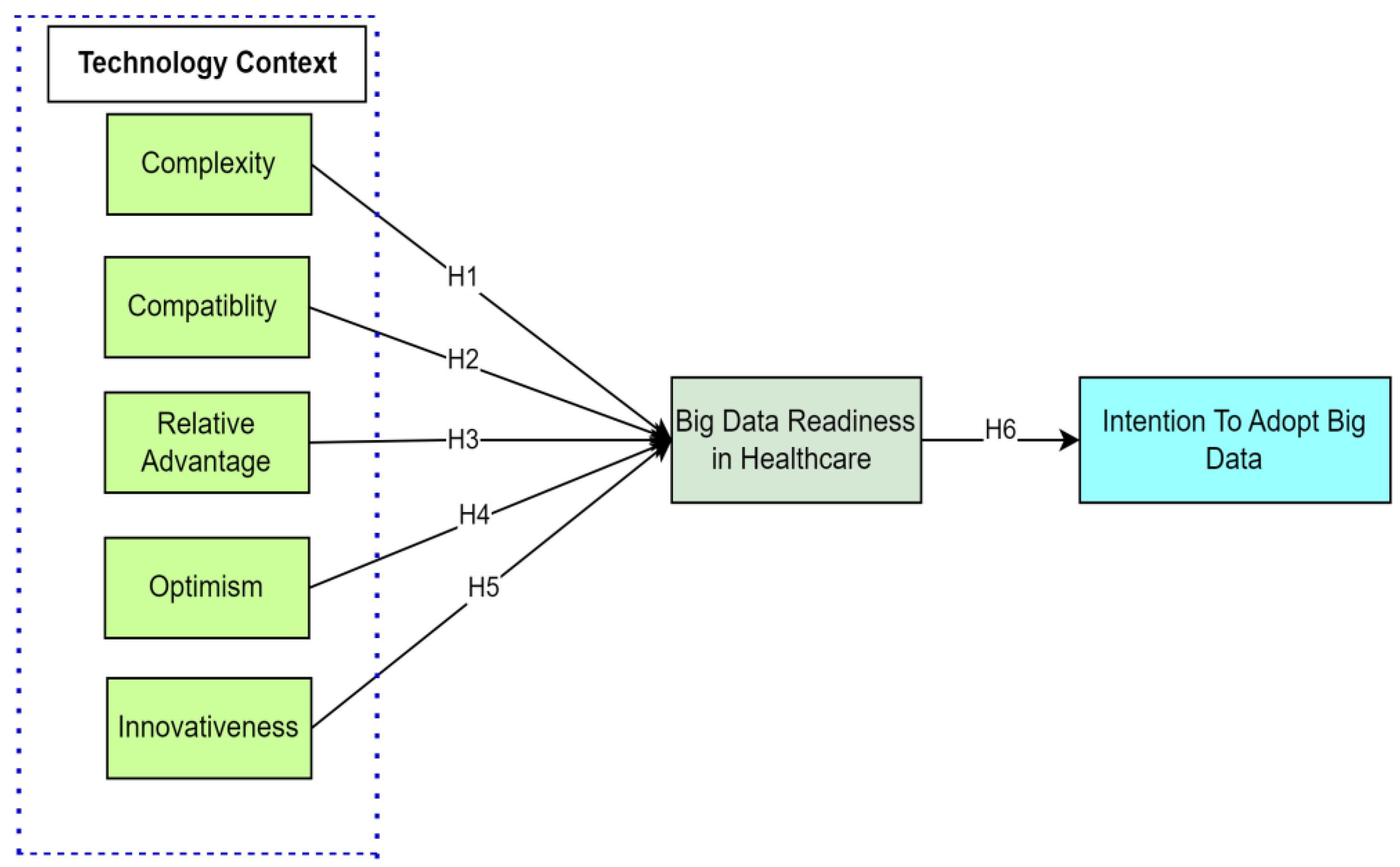
2.3.2. Technology Context
2.3.3. The Readiness of Healthcare Sectors for Big Data
3. Research Methodology
3.1. Pilot Test
- o Health professionals are required to attend;
- o A regular user of technology is required for participation;
- o Participants must be somewhat familiar with cutting-edge medical technology.
3.2. Measurement Items
4. Data Analysis and Results
4.1. Instrument Design
4.1.1. Demographic Data
4.1.2. The Results of Personal Information Collected from Participants
4.2. Common Method Bias
4.3. Measurement Framework
Convergent Validity
4.4. Structural Model Assessment
5. Discussion
6. Conclusions
6.1. Theoretical Contribution and Implications
6.2. Practical Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Constructs | Items | References |
|---|---|---|
| Complexity (CX) | ||
| BD allows me to manage business operations in an efficient way. | CX1 | [119,120,121,122,123,124] |
| The use of BD is frustrating. | CX2 | |
| The skills needed to improve and use the new technologies are easy for me. | CX3 | |
| The use of BD requires a lot of mental effort. | CX4 | |
| Compatibility (CT) | ||
| The use of BD is compatible with my healthcare corporate culture and value system. | (CT1) | [119,120,122,123,124,125,126] |
| The use of BD will be compatible with existing hardware and software. | (CT2) | |
| BD is easy to use and manage. | (CT3) | |
| BD is compatible with existing emerging technologies. | (CT4) | |
| Relative Advantage (RA) | ||
| Cloud-based ERP will enhance the efficiency of our company. | (RA1) | [127,128,129] |
| Cloud-based ERP will improve the performance of our company. | (RA2) | |
| Cloud-based ERP will provide timely information for decision making. | (RA3) | |
| With cloud-based ERP adoption, we expect to see cost savings effect. | (RA4) | |
| With cloud-based ERP adoption, we will be able to respond quickly and flexibly to our business expansion and pay only for what we use. | (RA5) | |
| Optimism (OP) | ||
| New technologies contribute to a better quality of life. | (OP1) | [130,131,132,133,134] |
| Technology gives me more freedom of mobility. | (OP2) | |
| Technology gives people more control over their daily lives. | (OP3) | |
| Technology makes me more productive in my personal life. | (OP4) | |
| Technology makes me more efficient in my occupation. | (OP5) | |
| Innovativeness | ||
| Innovativeness its big data Opinion leader | [126,135] | |
| Innovativeness tries to use new technology | ||
| Our organization top management actively pursues Innovativeness ideas. | ||
| Our organization gives us a penalty if the proposed idea does not work. | ||
| Our organization accepts Innovativeness well. | ||
| BD Readiness (BDR) in Healthcare Sector | ||
| The healthcare management understands how they can be used in the healthcare sector. | (BDR1) | [120,126,136,137,138,139] |
| The healthcare IT infrastructure is good (internet service/devices) and can be used for big data. | (BDR2) | |
| The healthcare management already promoted the usage of the BD to the staff very well. | (BDR3) | |
| The healthcare staff have the right skills to work with big data. | (BDR4) | |
| The healthcare IT department and the healthcare management have the right skills to lead the healthcare transformation, and they give very good support to help the staff. | (BDR5) | |
| Intention to adoption BD (ITABD) | ||
| BD adoption is effective to enhance the behavioral intentions to use the BD analytics system in healthcare. | (ITABD1) | [126,136,137,140] |
| BD technology adoption will increase the performance and effectiveness of healthcare. | (ITABD2) | |
| I would use BD technology adoption to gather health data. | (ITABD3) | |
| I would use the services provided by use BD technology adoption. | (ITABD4) | |
| I would not hesitate to provide information for use BD technology adoption | (ITABD5) |
References
- Ghaleb, E.A.; Dominic, P.; Fati, S.M.; Muneer, A.; Ali, R.F. The assessment of big data adoption readiness with a technology–organization–environment framework: A perspective towards healthcare employees. Sustainability 2021, 13, 8379. [Google Scholar] [CrossRef]
- Bhavnani, S.P.; Parakh, K.; Atreja, A.; Druz, R.; Graham, G.N.; Hayek, S.S.; Krumholz, H.M.; Maddox, T.M.; Majmudar, M.D.; Rumsfeld, J.S.; et al. 2017 Roadmap for Innovation—ACC Health Policy Statement on Healthcare Transformation in the Era of Digital Health, Big Data, and Precision Health: A Report of the American College of Cardiology Task Force on Health Policy Statements and Systems of Care. J. Am. Coll. Cardiol. 2017, 70, 2696–2718. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, A.; Najafabadi, M.K.; Wah, Y.B.; Zaman, E.A.K.; Maskat, R. The state of the art and taxonomy of big data analytics: View from new big data framework. Artif. Intell. Rev. 2020, 53, 989–1037. [Google Scholar] [CrossRef]
- Sun, T.Q.; Medaglia, R. Mapping the challenges of Artificial Intelligence in the public sector: Evidence from public healthcare. Gov. Inf. Q. 2019, 36, 368–383. [Google Scholar] [CrossRef]
- Vukmirović, A.; Rajnai, Z.; Radojičić, M.; Vukmirović, J.; Milenković, M.J. Infrastructural model for the healthcare system based on emerging technologies. Acta Polytech. Hung. 2018, 15, 33–48. [Google Scholar]
- Wang, Y.; Kung, L.; Byrd, T.A. Big data analytics: Understanding its capabilities and potential benefits for healthcare organizations. Technol. Forecast. Soc. Chang. 2018, 126, 3–13. [Google Scholar] [CrossRef]
- Petersen, A.; Tanner, C.; Munsie, M. Citizens’ use of digital media to connect with health care: Socio-ethical and regulatory implications. Health 2019, 23, 367–384. [Google Scholar] [CrossRef]
- Merendino, A.; Dibb, S.; Meadows, M.; Quinn, L.; Wilson, D.; Simkin, L.; Canhoto, A. Big data, big decisions: The impact of big data on board level decision-making. J. Bus. Res. 2018, 93, 67–78. [Google Scholar] [CrossRef]
- Quinn, L.; Dibb, S.; Simkin, L.; Canhoto, A.; Analogbei, M. Troubled waters: The transformation of marketing in a digital world. Eur. J. Mark. 2016, 50, 2103–2133. [Google Scholar] [CrossRef]
- Olivo, J.F.L.; Guzmán, J.G.; Colomo-Palacios, R.; Stantchev, V. IT innovation strategy: Managing the implementation communication and its generated knowledge through the use of an ICT tool. J. Knowl. Manag. 2016, 20, 512–533. [Google Scholar] [CrossRef]
- Gantz, J.; Reinsel, D. The digital universe in 2020: Big data, bigger digital shadows, and biggest growth in the far east. IDC Iview IDC Anal. Future 2012, 2007, 1–16. [Google Scholar]
- Chen, M.; Mao, S.; Liu, Y. Big data: A survey. Mob. Netw. Appl. 2014, 19, 171–209. [Google Scholar] [CrossRef]
- Jaseena, K.; David, J.M. Issues, challenges, and solutions: Big data mining. CS IT-CSCP 2014, 4, 131–140. [Google Scholar]
- Gopal, G.; Suter-Crazzolara, C.; Toldo, L.; Eberhardt, W.J.C.C.; Medicine, L. Digital transformation in healthcare–architectures of present and future information technologies. Clin. Chem. Lab. Med. 2019, 57, 328–335. [Google Scholar] [CrossRef]
- Gao, J.; Koronios, A.; Selle, S. Towards a process view on critical success factors in big data analytics projects. In Proceedings of the Twenty-First Americas Conference on Information Systems, Fajardo, Puerto Rico, 13–15 August 2015. [Google Scholar]
- Al-Sai, Z.A.; Abdullah, R. Big data impacts and challenges: A review. In Proceedings of the 2019 IEEE Jordan International Joint Conference on Electrical Engineering and Information Technology (JEEIT), Amman, Jordan, 9–11 April 2019; IEEE: New York, NY, USA, 2019; pp. 150–155. [Google Scholar]
- Alexandru, A.G.; Radu, I.M.; Bizon, M.-L. Big Data in Healthcare-Opportunities and Challenges. Inform. Econ. 2018, 22, 43–54. [Google Scholar] [CrossRef]
- LaValle, S.; Lesser, E.; Shockley, R.; Hopkins, M.S.; Kruschwitz, N. Big data, analytics and the path from insights to value. MIT Sloan Manag. Rev. 2011, 52, 21–32. [Google Scholar]
- Hardin, T.; Kotz, D. Amanuensis: Information provenance for health-data systems. Inf. Process. Manag. 2021, 58, 102460. [Google Scholar] [CrossRef]
- Yang, H.; Guo, X.; Peng, Z.; Lai, K.-H. The antecedents of effective use of hospital information systems in the chinese context: A mixed-method approach. Inf. Process. Manag. 2021, 58, 102461. [Google Scholar] [CrossRef]
- Saleem, M.S.; Isha, A.S.N.; Mohd Yusop, Y.; Awan, M.I.; Naji, G.M.A. Agility and safety performance among nurses: The mediating role of mindful organizing. Nurs. Rep. 2021, 11, 666–679. [Google Scholar] [CrossRef]
- Bai, J. Humanistic Spirit Training of Medical Students Based on Multisource Medical Data Fusion. Comput. Math. Methods Med. 2022, 2022, 7896367. [Google Scholar] [CrossRef]
- Neunaber, T.; Meister, S. Digital Maturity and Its Measurement of General Practitioners: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 4377. [Google Scholar] [CrossRef] [PubMed]
- Amin, I.M.; Hussein, S.S.; Isa, W. Assessing user satisfaction of using hospital information system (HIS) in Malaysia. People 2011, 12, 13. [Google Scholar]
- Salleh, M.I.M.; Abdullah, R.; Zakaria, N. Evaluating the effects of electronic health records system adoption on the performance of Malaysian health care providers. BMC Med. Inform. Decis. Mak. 2021, 21, 75. [Google Scholar] [CrossRef] [PubMed]
- Sarlan, A.; Ahmad, R.; Ahmad, W.F.W.; Dominic, P. Private Healthcare in Malaysia: Investigation on Technology Profiles and Technology Acceptance Factors. ISICO 2013, 2013, 2013. [Google Scholar]
- Zakaria, N.; Yusof, S.A.M. Understanding technology and people issues in hospital information system (HIS) adoption: Case study of a tertiary hospital in Malaysia. J. Infect. Public Health 2016, 9, 774–780. [Google Scholar] [CrossRef] [PubMed]
- Samah, B.A.; Shaffril, H.M.; Hassan, M.A.; D’Silva, J.L. Can technology acceptance model be applied on the rural setting: The case of village development and security committee in Malaysia. J. Soc. Sci. 2011, 7, 113–119. [Google Scholar] [CrossRef]
- Ngai, E.W.; Poon JK, L.; Suk FF, C.; Ng, C.C. Design of an RFID-based healthcare management system using an information system design theory. Inf. Syst. Front. 2009, 11, 405–417. [Google Scholar] [CrossRef]
- Baharuddin, H.E.A.; Othman, A.F.; Adnan, H.; Ismail, N.A.A. Evaluating the Influence of Training on Attitudes to Building Information Modelling (BIM) Adoption in Malaysian Construction Industry by Using Extended Technology Acceptance Model (TAM). In Collaboration and Integration in Construction, Engineering, Management and Technology; Springer: Berlin/Heidelberg, Germany, 2021; pp. 577–582. [Google Scholar]
- Bakar, N.A.A.; ChePa, N.; Jasin, N.M. Challenges in the implementation of hospital information systems in Malaysian public hospitals. In Proceedings of the 6th International Conference on Computing & Informatics, Akamatsu, Japan, 2–4 August 2017; pp. 636–642. [Google Scholar]
- Song, S.; Imai, K.S. Does the hunger safety net programme reduce multidimensional poverty? Evidence from Kenya. Dev. Stud. Res. 2019, 6, 47–61. [Google Scholar] [CrossRef]
- Ho, B.S.; Chui, K.H.; Fong, B.Y.F. Monitoring Elderly Healthcare and Social Services. In Ageing with Dignity in Hong Kong and Asia: Holistic and Humanistic Care; Springer Nature: Singapore, 2022; pp. 159–175. [Google Scholar]
- Stenberg, K.; Hanssen, O.; Bertram, M.; Brindley, C.; Meshreky, A.; Barkley, S.; Edejer, T.T.-T. Guide posts for investment in primary health care and projected resource needs in 67 low-income and middle-income countries: A modelling study. Lancet Glob. Health 2019, 7, e1500–e1510. [Google Scholar] [CrossRef]
- Cerchione, R.; Centobelli, P.; Riccio, E.; Abbate, S.; Oropallo, E. Blockchain’s coming to hospital to digitalize healthcare services: Designing a distributed electronic health record ecosystem. Technovation 2023, 120, 102480. [Google Scholar] [CrossRef]
- Büyüközkan, G.; Göçer, F. Digital supply chain: Literature review and a proposed framework for future research. Comput. Ind. 2018, 97, 157–177. [Google Scholar] [CrossRef]
- Patel, A.B.; Birla, M.; Nair, U. Addressing big data problem using Hadoop and Map Reduce. In Proceedings of the 2012 Nirma University International Conference on Engineering (NUiCONE), Ahmedabad, India, 6–8 December 2012; IEEE: New York, NY, USA, 2012; pp. 1–5. [Google Scholar]
- Hilbert, M.; López, P. The world’s technological capacity to store, communicate, and compute information. Science 2011, 332, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Rajagopal, S. Data Science: Recent Developments and Future Insights. In Deep Learning Innovations and Their Convergence with Big Data; IGI Global: Hershey, PA, USA, 2018; pp. 141–151. [Google Scholar]
- Yang, Z.; Sun, J.; Zhang, Y.; Wang, Y. Understanding SaaS adoption from the perspective of organizational users: A tripod readiness model. Comput. Hum. Behav. 2015, 45, 254–264. [Google Scholar] [CrossRef]
- Bag, S.; Wood, L.C.; Xu, L.; Dhamija, P.; Kayikci, Y. Big data analytics as an operational excellence approach to enhance sustainable supply chain performance. Resour. Conserv. Recycl. 2020, 153, 104559. [Google Scholar] [CrossRef]
- Raguseo, E. Big data technologies: An empirical investigation on their adoption, benefits and risks for companies. Int. J. Inf. Manag. 2018, 38, 187–195. [Google Scholar] [CrossRef]
- Troshani, I.; Rampersad, G.; Plewa, C. Adopting innovation management software in university innovation commercialization. J. Comput. Inf. Syst. 2011, 52, 83–92. [Google Scholar]
- Amini, A. A state-of-the-art analysis of innovation models and innovation software tools. In Proceedings of the Conference: 10th European Conference on Innovation and Entrepreneurship, ECIE, Genova, Italy, 17–18 September 2015; pp. 1–9. [Google Scholar]
- Saghafian, M.; Laumann, K.; Skogstad, M.R. Stagewise Overview of Issues Influencing Organizational Technology Adoption and Use. Front. Psychol. 2021, 12, 654. [Google Scholar] [CrossRef] [PubMed]
- Luo, X.; Zhang, W.; Li, H.; Bose, R.; Chung, Q.B. Cloud computing capability: Its technological root and business impact. J. Organ. Comput. Electron. Commer. 2018, 28, 193–213. [Google Scholar] [CrossRef]
- Rather, M.-K.; Rather, S.-A. Impact of smartphones on young generation. Libr. Philos. Pract. 2019, 2384, 1–9. [Google Scholar]
- Giotopoulos, I.; Kontolaimou, A.; Korra, E.; Tsakanikas, A. What drives ICT adoption by SMEs? Evidence from a large-scale survey in Greece. J. Bus. Res. 2017, 81, 60–69. [Google Scholar] [CrossRef]
- Subramani Parasuraman, A.T.S.; Yee, S.W.K.; Chuon, B.L.C.; Ren, L.Y. Smartphone usage and increased risk of mobile phone addiction: A concurrent study. Int. J. Pharm. Investig. 2017, 7, 125. [Google Scholar] [CrossRef]
- Baig, M.I.; Shuib, L.; Yadegaridehkordi, E. Big data in education: A state of the art, limitations, and future research directions. Int. J. Educ. Technol. High. Educ. 2020, 17, 44. [Google Scholar] [CrossRef]
- Silow-Carroll, S.; Edwards, J.N.; Rodin, D. Using electronic health records to improve quality and efficiency: The experiences of leading hospitals. Issue Brief Commonw Fund 2012, 17, 40. [Google Scholar]
- Pan, Y.; Froese, F.; Liu, N.; Hu, Y.; Ye, M. The adoption of artificial intelligence in employee recruitment: The influence of contextual factors. Int. J. Hum. Resour. Manag. 2022, 33, 1125–1147. [Google Scholar] [CrossRef]
- Wisdom, J.P.; Chor, K.H.B.; Hoagwood, K.E.; Horwitz, S.M. Innovation adoption: A review of theories and constructs. Adm. Policy Ment. Health Ment. Health Serv. Res. 2014, 41, 480–502. [Google Scholar] [CrossRef]
- Tornatzky, L.G.; Fleischer, M.; Chakrabarti, A.K. Processes of Technological Innovation; Lexington Books: Lexington, KY, USA, 1990. [Google Scholar]
- Naji, G.M.A.; Isha, A.S.N.; Alazzani, A.; Brough, P.; Saleem, M.S.; Mohyaldinn, M.E.; Alzoraiki, M. Do leadership, organizational communication, and work environment impact employees’ psychosocial hazards in the oil and gas industry? Int. J. Environ. Res. Public Health 2022, 19, 4432. [Google Scholar] [CrossRef]
- Isha, A.S.N.; Naji, G.M.A.; Saleem, M.S.; Brough, P.; Alazzani, A.; Ghaleb, E.A.; Muneer, A.; Alzoraiki, M. Validation of “Depression, Anxiety, and Stress Scales” and “Changes in Psychological Distress during COVID-19” among University Students in Malaysia. Sustainability 2023, 15, 4492. [Google Scholar] [CrossRef]
- Alzoraiki, M.; Ahmad, A.R.; Ateeq, A.A.; Naji, G.M.A.; Almaamari, Q.; Beshr, B.A.H. Impact of Teachers’ Commitment to the Relationship between Transformational Leadership and Sustainable Teaching Performance. Sustainability 2023, 15, 4620. [Google Scholar] [CrossRef]
- Aboelmaged, M.G. Predicting e-readiness at firm-level: An analysis of technological, organizational and environmental (TOE) effects on e-maintenance readiness in manufacturing firms. Int. J. Inf. Manag. 2014, 34, 639–651. [Google Scholar] [CrossRef]
- Kapoor, K.K.; Dwivedi, Y.K.; Williams, M.D. Empirical examination of the role of three sets of innovation attributes for determining adoption of IRCTC mobile ticketing service. Inf. Syst. Manag. 2015, 32, 153–173. [Google Scholar] [CrossRef][Green Version]
- Baker, J. The technology–organization–environment framework. Inf. Syst. Theory 2012, 1, 231–245. [Google Scholar]
- Gu, V.C.; Cao, Q.; Duan, W. Unified Modeling Language (UML) IT adoption—A holistic model of organizational capabilities perspective. Decis. Support Syst. 2012, 54, 257–269. [Google Scholar] [CrossRef]
- McNaughton, B.L.; O’Keefe, J.; Barnes, C.A. The stereotrode: A new technique for simultaneous isolation of several single units in the central nervous system from multiple unit records. J. Neurosci. Methods 1983, 8, 391–397. [Google Scholar] [CrossRef]
- Bolonne, H.; Wijewardene, P. Critical factors affecting the intention to adopt big data analytics in apparel sector, Sri Lanka. Int. J. Adv. Comput. Sci. Appl. 2020, 11, 149–162. [Google Scholar] [CrossRef]
- Sharma, M.; Gupta, R.; Acharya, P. Analysing the adoption of cloud computing service: A systematic literature review. Glob. Knowl. Mem. Commun. 2020, 70, 114–153. [Google Scholar] [CrossRef]
- Ijab, M.T.; Wahab, S.M.A.; Salleh, M.A.M.; Bakar, A.A. Investigating Big Data Analytics Readiness in Higher Education Using the Technology-Organisation-Environment (TOE) Framework. In Proceedings of the 2019 6th International Conference on Research and Innovation in Information Systems (ICRIIS), Johor Bahru, Malaysia, 2–3 December 2019; IEEE: New York, NY, USA, 2019; pp. 1–7. [Google Scholar]
- Harindranath, G.; Dyerson, R.; Barnes, D. ICT in small firms: Factors affecting the adoption and use of ICT in Southeast England SMEs. In Proceedings of the 2008 European Conference on Information Systems, Galway, Ireland, 9–11 June 2008. [Google Scholar]
- Kandil, A.M.N.A.; Ragheb, M.A.; Ragab, A.A.; Farouk, M. Examining the effect of TOE model on cloud computing adoption in Egypt. Bus. Manag. Rev. 2018, 9, 113–123. [Google Scholar]
- Asiaei, A.; Rahim, N.Z.A. A multifaceted framework for adoption of cloud computing in Malaysian SMEs. J. Sci. Technol. Policy Manag. 2019, 10, 708–750. [Google Scholar] [CrossRef]
- Alshamaila, Y.; Papagiannidis, S.; Li, F. Cloud computing adoption by SMEs in the north east of England. J. Enterp. Inf. Manag. 2013, 26, 250–275. [Google Scholar] [CrossRef]
- Rowe, F.; Truex, D.; Huynh, M.Q. An empirical study of determinants of e-commerce adoption in SMEs in Vietnam: An economy in transition. J. Glob. Inf. Manag. JGIM 2012, 20, 23–54. [Google Scholar]
- Gangwar, H. Understanding the determinants of Big data adoption in India: An analysis of the manufacturing and services sectors. Inf. Resour. Manag. J. IRMJ 2018, 31, 1–22. [Google Scholar] [CrossRef]
- Lai, Y.; Sun, H.; Ren, J. Understanding the determinants of big data analytics (BDA) adoption in logistics and supply chain management. Int. J. Logist. Manag. 2018, 29, 676–703. [Google Scholar] [CrossRef]
- Awa, H.O.; Ukoha, O.; Igwe, S.R. Revisiting technology-organization-environment (TOE) theory for enriched applicability. Bottom Line 2017, 30, 2–22. [Google Scholar] [CrossRef]
- Azeem, M.; Ahmed, M.; Haider, S.; Sajjad, M. Expanding competitive advantage through organizational culture, knowledge sharing and organizational innovation. Technol. Soc. 2021, 66, 101635. [Google Scholar] [CrossRef]
- Ren, J.-f.; Fosso Wamba, S.; Akter, S.; Dubey, R.; Childe, S.J. Modelling quality dynamics on business value and firm performance in big data analytics environment. Int. J. Prod. Res. 2017, 55, 5011–5026. [Google Scholar]
- Gangwar, H.; Date, H.; Ramaswamy, R. Understanding determinants of cloud computing adoption using an integrated TAM-TOE model. J. Enterp. Inf. Manag. 2015, 28, 107–130. [Google Scholar] [CrossRef]
- Al-Sharafi, M.A.; Arshah, R.A.; Abu-Shanab, E.A. Factors influencing the continuous use of cloud computing services in organization level. In Proceedings of the International Conference on Advances in Image Processing, Bangkok, Thailand, 25–27 August 2017; pp. 189–194. [Google Scholar]
- Saleem, M.S.; Isha, A.S.N.; Awan, M.I.; Yusop, Y.B.; Naji, G.M.A. Fostering academic engagement in post-graduate students: Assessing the role of positive emotions, positive psychology, and stress. Front. Psychol. 2022, 13, 920395. [Google Scholar] [CrossRef]
- Ghaleb, E.A.; Dominic, P.D.; Alzoraiki, M.; Mohamed, I.; Naji, G.M.A.; Ammar, A.A. The role of transformational leadership style and intellectual capital in improving the service quality of the public healthcare sector in developing countries–conceptual study. Int. J. Intellect. Hum. Resour. Manag. (IJIHRM) 2022, 3, 1–7. [Google Scholar] [CrossRef]
- Sam, K.M.; Chatwin, C.R. Understanding adoption of Big data analytics in China: From organizational users perspective. In Proceedings of the 2018 IEEE International Conference on Industrial Engineering and Engineering Management (IEEM), Bangkok, Thailand, 16–19 December 2018; IEEE: New York, NY, USA, 2018; pp. 507–510. [Google Scholar]
- Yoon, J.; Li, S.; Hao, Y. Design-mediated positive emotion regulation: The development of an interactive device that supports daily practice of positive mental time traveling. Int. J. Hum.–Comput. Interact. 2022, 38, 432–446. [Google Scholar] [CrossRef]
- Naji, G.M.A.; Isha, A.S.N.; Alazzani, A.; Saleem, M.S.; Alzoraiki, M. Assessing the mediating role of safety communication between safety culture and employees safety performance. Front. Public Health 2022, 10, 840281. [Google Scholar] [CrossRef] [PubMed]
- Etim, E.; Daramola, O. Investigating the E-Readiness of Informal Sector Operators to Utilize Web Technology Portal. Sustainability 2023, 15, 3449. [Google Scholar] [CrossRef]
- Goutam, D.; Ganguli, S.; Gopalakrishna, B. Technology readiness and e-service quality–impact on purchase intention and loyalty. Mark. Intell. Plan. 2022, 40, 242–255. [Google Scholar] [CrossRef]
- Chen, S.-C.; Li, S.-H.; Liu, S.-C.; Yen, D.C.; Ruangkanjanases, A. Assessing Determinants of Continuance Intention towards Personal Cloud Services: Extending UTAUT2 with Technology Readiness. Symmetry 2021, 13, 467. [Google Scholar] [CrossRef]
- Shim, H.-S.; Han, S.-L.; Ha, J. The Effects of Consumer Readiness on the Adoption of Self-Service Technology: Moderating Effects of Consumer Traits and Situational Factors. Sustainability 2021, 13, 95. [Google Scholar] [CrossRef]
- Adiyarta, K.; Napitupulu, D.; Nurdianto, H.; Rahim, R.; Ahmar, A. User acceptance of E-Government Services Based on TRAM model. In IOP Conference Series: Materials Science and Engineering, Proceedings of the 7th AIC-ICMR on Sciences and Engineering 2017, Banda Aceh, Indonesia, 18–20 October 2017; IOP Publishing: Bristol, UK, 2017; p. 012057. [Google Scholar]
- Haddad, A.; Ameen, A.; Isaac, O.; Alrajawy, I.; Al-Shbami, A.; Midhun Chakkaravarthy, D. The impact of technology readiness on the big data adoption among UAE organisations. In Proceedings of the Data Management, Analytics and Innovation: Proceedings of ICDMAI 2019, Kuala Lumpur, Malaysia, 18–20 January 2019; Springer: Berlin/Heidelberg, Germany, 2019; Volume 2, pp. 249–264. [Google Scholar]
- Ramírez-Correa, P.; Grandón, E.E.; Rondán-Cataluña, F.J. Users segmentation based on the Technological Readiness Adoption Index in emerging countries: The case of Chile. Technol. Forecast. Soc. Chang. 2020, 155, 120035. [Google Scholar] [CrossRef]
- Chong, A.Y.-L.; Chan, F.T. Structural equation modeling for multi-stage analysis on Radio Frequency Identification (RFID) diffusion in the health care industry. Expert Syst. Appl. 2012, 39, 8645–8654. [Google Scholar] [CrossRef]
- Chen, D.Q.; Preston, D.S.; Swink, M. How the use of big data analytics affects value creation in supply chain management. J. Manag. Inf. Syst. 2015, 32, 4–39. [Google Scholar] [CrossRef]
- Marr, B. How big data is changing healthcare. Forbes, 21 April 2015. [Google Scholar]
- Chong, A.Y.-L.; Liu, M.J.; Luo, J.; Keng-Boon, O. Predicting RFID adoption in healthcare supply chain from the perspectives of users. Int. J. Prod. Econ. 2015, 159, 66–75. [Google Scholar] [CrossRef]
- Gefen, D.; Rigdon, E.E.; Straub, D. Editor’s comments: An update and extension to SEM guidelines for administrative and social science research. Mis Q. 2011, 35, 3–14. [Google Scholar] [CrossRef]
- Hair, J.F., Jr.; Hult, G.T.M.; Ringle, C.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM), 2nd ed.; Sage Publications: Thousand Oaks, CA, USA, 2017; Volume 2. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modeling; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Dong, K.; Ali, R.F.; Dominic, P.; Ali, S.E.A. The Effect of Organizational Information Security Climate on Information Security Policy Compliance: The Mediating Effect of Social Bonding towards Healthcare Nurses. Sustainability 2021, 13, 2800. [Google Scholar] [CrossRef]
- Premkumar, G.; Ramamurthy, K. The role of interorganizational and organizational factors on the decision mode for adoption of interorganizational systems. Decis. Sci. 1995, 26, 303–336. [Google Scholar] [CrossRef]
- Cabrera-Sánchez, J.-P.; Villarejo-Ramos, A.F. Factors affecting the adoption of big data analytics in companies. Rev. Adm. Empresas 2020, 59, 415–429. [Google Scholar] [CrossRef]
- Gupta, A.C.; Srivastava, A.; Wiita, P.J. Periodic oscillations in the intra-day optical light curves of the blazar S5 0716+ 714. Astrophys. J. 2008, 690, 216. [Google Scholar] [CrossRef]
- Abu-Rub, H.; Holtz, J.; Rodriguez, J.; Baoming, G. Medium-voltage multilevel converters—State of the art, challenges, and requirements in industrial applications. IEEE Trans. Ind. Electron. 2010, 57, 2581–2596. [Google Scholar] [CrossRef]
- Naji, G.M.A.; Isha, A.S.N.; Mohyaldinn, M.E.; Leka, S.; Saleem, M.S.; Rahman, S.M.N.B.S.A.; Alzoraiki, M. Impact of safety culture on safety performance; mediating role of psychosocial hazard: An integrated modelling approach. Int. J. Environ. Res. Public Health 2021, 18, 8568. [Google Scholar] [CrossRef]
- Lin, C.H.; Shih, H.Y.; Sher, P.J. Integrating technology readiness into technology acceptance: The TRAM model. Psychol. Mark. 2007, 24, 641–657. [Google Scholar] [CrossRef]
- Ifinedo, P. An empirical analysis of factors influencing Internet/e-business technologies adoption by SMEs in Canada. Int. J. Inf. Technol. Decis. Mak. 2011, 10, 731–766. [Google Scholar] [CrossRef]
- Hair, J.F.; Sarstedt, M.; Ringle, C.M. Rethinking some of the rethinking of partial least squares. Eur. J. Mark. 2019, 53, 566–583. [Google Scholar] [CrossRef]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Mark. Sci. 2015, 43, 115–135. [Google Scholar] [CrossRef]
- Ramayah, T.; Cheah, J.; Chuah, F.; Ting, H.; Memon, M. Partial least squares structural equation modeling (PLS-SEM) using smartPLS 3.0. In An Updated Guide and Practical Guide to Statistical Analysis; Pearson: London, UK, 2018. [Google Scholar]
- Sarstedt, M.; Ringle, C.M.; Hair, J.F. Partial least squares structural equation modeling. Handb. Mark. Res. 2017, 26, 1–40. [Google Scholar]
- Hair, J.F., Jr.; Sarstedt, M.; Hopkins, L.; Kuppelwieser, V.G. Partial least squares structural equation modeling (PLS-SEM). Eur. Bus. Rev. 2014, 26, 106–121. [Google Scholar] [CrossRef]
- Kothari, C.R. Research Methodology: Methods and Techniques; New Age International Limited: New York, NY, USA, 2004; p. 401. ISBN 8122415229, 9788122415223. [Google Scholar]
- Wahyuni, D. The research design maze: Understanding paradigms, cases, methods and methodologies. J. Appl. Manag. Account. Res. 2012, 10, 69–80. [Google Scholar]
- Hassan, S.T.; Batool, B.; Zhu, B.; Khan, I. Environmental complexity of globalization, education, and income inequalities: New insights of energy poverty. J. Clean. Prod. 2022, 340, 130735. [Google Scholar] [CrossRef]
- Chong, K.W.; Kim, Y.S.; Choi, J. A Study of Factors Affecting Intention to Adopt a Cloud-Based Digital Signature Service. Information 2021, 12, 60. [Google Scholar] [CrossRef]
- Tornatzky, L.G.; Klein, K.J. Innovation characteristics and innovation adoption-implementation: A meta-analysis of findings. IEEE Trans. Eng. Manag. 1982, EM-29, 28–45. [Google Scholar] [CrossRef]
- Mndzebele, N. The effects of relative advantage, compatibility and complexity in the adoption of EC in the hotel industry. Int. J. Comput. Commun. Eng. 2013, 2, 473. [Google Scholar] [CrossRef]
- Mairura, K.O. Relative advantage as a determinant of technology adoption among automobile mechanics in micro and small enterprises in Kenya. Int. J. Acad. Res. Bus. Soc. Sci. 2016, 21, 86–92. [Google Scholar]
- Kock, N. WarpPLS User Manual: Version 7.0. 141; ScriptWarp Systems: Laredo, TX, USA, 2020. [Google Scholar]
- Kessler, S.R.; Pindek, S.; Kleinman, G.; Andel, S.A.; Spector, P.E. Information security climate and the assessment of information security risk among healthcare employees. Health Inform. J. 2020, 26, 461–473. [Google Scholar] [CrossRef]
- Gutierrez, A.; Boukrami, E.; Lumsden, R. Technological, organisational and environmental factors influencing man-agers’ decision to adopt cloud computing in the UK. J. Enterp. Inf. Manag. 2015, 28, 788–807. [Google Scholar] [CrossRef]
- Oliveira, T.; Thomas, M.; Espadanal, M. Assessing the determinants of cloud computing adoption: An analysis of the manufacturing and services sectors. Inf. Manag. 2014, 51, 497–510. [Google Scholar] [CrossRef]
- Grönlund, Å.; Islam, Y.M. A mobile e-learning environment for developing countries: The Bangladesh virtual interactive classroom. Inf. Technol. Dev. 2010, 16, 244–259. [Google Scholar] [CrossRef]
- Mansour, R.F.; Escorcia-Gutierrez, J.; Gamarra, M.; Díaz, V.G.; Gupta, D.; Kumar, S. Artificial intelligence with big data analytics-based brain intracranial hemorrhage e-diagnosis using CT images. Neural Comput. Appl. 2021, 1–13. [Google Scholar] [CrossRef]
- Maroufkhani, P.; Ismail, W.K.W.; Ghobakhloo, M. Big data analytics adoption model for small and medium enterprises. J. Sci. Technol. Policy Manag. 2020. [Google Scholar] [CrossRef]
- Agrawal, K. Investigating the determinants of Big Data Analytics (BDA) adoption in Asian emerging economies. Acad. Manag. Annu. Meet. Proc. 2015, 2015, 11290. [Google Scholar]
- Zhu, K.; Dong, S.; Xu, S.X.; Kraemer, K.L. Innovation diffusion in global contexts: Determinants of post-adoption digital transformation of European companies. Eur. J. Inf. Syst. 2006, 15, 601–616. [Google Scholar] [CrossRef]
- Ho, J.C.; Wu, C.G.; Lee, C.S.; Pham, T.T.T. Factors affecting the behavioral intention to adopt mobile banking: An international comparison. Technol. Soc. 2020, 63, 101360. [Google Scholar] [CrossRef]
- Ashraf, M.; Hoque, R. An illustration of information communication technology (ICT)-mediated innovation–adoption–implementation in rural Bangladesh. Tékhne 2016, 14, 45–51. [Google Scholar] [CrossRef]
- Rogers, E.M. Chapter 1-Elements of diffusion. In Diffusion of Innovations; The Free Press: New York, NY, USA, 2003; pp. 1–22. [Google Scholar]
- Premkumar, G.; Roberts, M. Adoption of new information technologies in rural small businesses. Omega 1999, 27, 467–484. [Google Scholar] [CrossRef]
- Kim, T.; Chiu, W.; Chow, M.K.F. Sport technology consumers: Segmenting users of sports wearable devices based on technology readiness. Sport Bus. Manag. Int. J. 2019. [Google Scholar] [CrossRef]
- Chiu, W.; Cho, H. The role of technology readiness in individuals’ intention to use health and fitness applications: A comparison between users and non-users. Asia Pac. J. Mark. Logist. 2020. [Google Scholar] [CrossRef]
- Liljander, V.; Gillberg, F.; Gummerus, J.; Van Riel, A. Technology readiness and the evaluation and adoption of self-service technologies. J. Retail. Consum. Serv. 2006, 13, 177–191. [Google Scholar] [CrossRef]
- Parasuraman, A.; Colby, C.L. An updated and streamlined technology readiness index: TRI 2.0. J. Serv. Res. 2015, 18, 59–74. [Google Scholar] [CrossRef]
- Nugroho, M.A.; Fajar, M.A. Effects of Technology Readiness Towards Acceptance of Mandatory Web-Based Attendance System. Procedia Comput. Sci. 2017, 124, 319–328. [Google Scholar] [CrossRef]
- Culliford, A.; Bradbury, J. A cross-sectional survey of the readiness of consumers to adopt an environmentally sustainable diet. Nutr. J. 2020, 19, 138. [Google Scholar] [CrossRef]
- Banerjee, A.; Chakraborty, C.; Kumar, A.; Biswas, D. Emerging trends in IoT and big data analytics for biomedical and health care technologies. In Handbook of Data Science Approaches for Biomedical Engineering; Elsevier: Amsterdam, The Netherlands, 2020; pp. 121–152. [Google Scholar]
- Caesarius, L.M.; Hohenthal, J. Searching for big data: How incumbents explore a possible adoption of big data technologies. Scand. J. Manag. 2018, 34, 129–140. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming (Multivariate Applications Series); Taylor & Francis Group: New York, NY, USA, 2010; Volume 396, p. 7384. [Google Scholar]
- Nugroho, M.A. Impact of Government Support and Competitor Pressure on the Readiness of SMEs in Indonesia in Adopting the Information Technology. Procedia Comput. Sci. 2015, 72, 102–111. [Google Scholar] [CrossRef]
- Mukred, M.; Yusof, Z.M.; Alotaibi, F.M.; Asma’Mokhtar, U.; Fauzi, F. The key factors in adopting an electronic records management system (ERMS) in the educational sector: A UTAUT-based framework. IEEE Access 2019, 7, 35963–35980. [Google Scholar] [CrossRef]


| Constructs | Mean | Standard Deviation | T-Statistics |
|---|---|---|---|
| Complexity (CX) | 4.350 | 0.035 | 1.254 |
| Compatibility (CT) | 4.371 | 0.029 | 4.566 |
| Relative Advantage (RA) | 3.783 | 0.050 | 2.628 |
| Optimism (OP) | 3.663 | 0.032 | 2.678 |
| Innovativeness (IV) | 3.768 | 0.052 | 4.566 |
| Demographic Variable | Categories | Frequency (n = 328) | Percentage (%) |
|---|---|---|---|
| Gender | Male | 208 | 63.41 |
| Female | 120 | 36.58 |
| Demographic Variable | Categories | Frequency (n = 328) | Percentage (%) |
|---|---|---|---|
| Age | 21–32 | 109 | 33.2 |
| 33–42 | 75 | 22.9 | |
| 43–52 | 81 | 24.7 | |
| 53–64 | 59 | 18.0 | |
| 64 or above | 4 | 1.2 |
| Demographic Variable | Categories | Frequency (n = 328) | Percentage (%) |
|---|---|---|---|
| Education | Diploma | 38 | 11.6 |
| Bachelor | 73 | 22.3 | |
| Master | 131 | 39.9 | |
| Doctorate | 86 | 26.2 |
| Demographic Variable | Categories | Frequency (n = 328) | Percentage (%) |
|---|---|---|---|
| Position | Doctor | 65 | 19.8 |
| Nurse | 118 | 36.0 | |
| Technician | 74 | 22.6 | |
| IT staff | 71 | 21.6 |
| Demographic Variable | Categories | Frequency (n = 328) | Percentage (%) |
|---|---|---|---|
| Your experience in the current job | 1–6 years | 117 | 35.7 |
| 6–16 years | 87 | 26.5 | |
| 16–26 years | 82 | 25.0 | |
| 26–36 years | 42 | 12.8 |
| Demographic Variable | Categories | Frequency (n = 328) | Percentage (%) |
|---|---|---|---|
| Information technology competence | Low | 87 | 26.5 |
| High | 241 | 73.5 |
| Demographic Variable | Categories | Frequency (n = 328) | Percentage (%) |
|---|---|---|---|
| Daily usage of computers (hours) | 4–7 h | 146 | 44.5 |
| 8–11 h | 123 | 37.5 | |
| More than 11 h | 59 | 18.0 |
| CX | CT | IN | OP | RA | BDR |
|---|---|---|---|---|---|
| 1.041 | 1.030 | 1.763 | 1.028 | 1.720 | 1.000 |
| Constructs | Reliability | |||
|---|---|---|---|---|
| Cronbach’s Alpha | rho_A | CR | AVE | |
| Complexity (CX) | 0.805 | 0.816 | 0.862 | 0.614 |
| Compatibility (CT) | 0.848 | 0.981 | 0.892 | 0.673 |
| Relative Advantage | 0.747 | 0.748 | 0.818 | 0.575 |
| Optimism (OP) | 0.796 | 0.870 | 0.852 | 0.539 |
| Innovativeness (IV) | 0.834 | 0.838 | 0.889 | 0.668 |
| BD Readiness (BDR) In Healthcare Sector | 0.864 | 0.869 | 0.902 | 0.649 |
| Intention To Adopt BD (ITABD) | 0.817 | 0.860 | 0.877 | 0.599 |
| Construct | (1) | (2) | (3) | (4) | (5) | (6) | (7) |
|---|---|---|---|---|---|---|---|
| Big Data Readiness In Healthcare | 0.806 | ||||||
| Compatibility | 0.195 | 0.821 | |||||
| Complexity | 0.141 | 0.119 | 0.784 | ||||
| Innovativeness | 0.434 | 0.026 | 0.153 | 0.817 | |||
| Intention To Adopt Big Data | 0.765 | 0.111 | 0.139 | 0.35 | 0.774 | ||
| Optimism | 0.174 | 0.124 | 0.043 | 0.109 | 0.177 | 0.734 | |
| Relative Advantage | 0.367 | −0.018 | 0.057 | 0.645 | 0.364 | 0.074 | 0.689 |
| Hypothesis | Path | Beta-Value (N = 254) | t-Value Deviation | p-Value | f2 | Result |
|---|---|---|---|---|---|---|
| H1 | CX -> BDR | 0.061 | 1.332 | 0.000 | 0.005 | Not Supported |
| H2 | CT -> BDR | 0.169 | 4.456 | 0.184 | 0.037 | Supported |
| H3 | RA -> BDR | 0.162 | 2.557 | 0.011 | 0.020 | Supported |
| H4 | OP -> BDR | 0.105 | 2.505 | 0.013 | 0.014 | Supported |
| H5 | IN -> BDR | 0.304 | 4.395 | 0.000 | 0.070 | Supported |
| H6 | BDR -> ITABD | 0.765 | 26.716 | 0.000 | 1.408 | Supported |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghaleb, E.A.A.; Dominic, P.D.D.; Singh, N.S.S.; Naji, G.M.A. Assessing the Big Data Adoption Readiness Role in Healthcare between Technology Impact Factors and Intention to Adopt Big Data. Sustainability 2023, 15, 11521. https://doi.org/10.3390/su151511521
Ghaleb EAA, Dominic PDD, Singh NSS, Naji GMA. Assessing the Big Data Adoption Readiness Role in Healthcare between Technology Impact Factors and Intention to Adopt Big Data. Sustainability. 2023; 15(15):11521. https://doi.org/10.3390/su151511521
Chicago/Turabian StyleGhaleb, Ebrahim A. A., P. D. D. Dominic, Narinderjit Singh Sawaran Singh, and Gehad Mohammed Ahmed Naji. 2023. "Assessing the Big Data Adoption Readiness Role in Healthcare between Technology Impact Factors and Intention to Adopt Big Data" Sustainability 15, no. 15: 11521. https://doi.org/10.3390/su151511521
APA StyleGhaleb, E. A. A., Dominic, P. D. D., Singh, N. S. S., & Naji, G. M. A. (2023). Assessing the Big Data Adoption Readiness Role in Healthcare between Technology Impact Factors and Intention to Adopt Big Data. Sustainability, 15(15), 11521. https://doi.org/10.3390/su151511521








