Abstract
The main objective of this paper is to understand and characterize the healthy work environment of organizations during the COVID-19 pandemic. The study was carried out in 2021 including organizations from different sectors at the national level and involved 460 participants, 50.3% of which were female. The workers’ ages ranged between 18 and 67 years, with a mean of 44 years and a standard deviation of 11.36. The Healthy Workplaces Ecosystems Tool was used. Data was collected online from professionals in the organizations who agreed to participate in the study. Our results show that organizational culture has a strong relationship with the other components of a healthy work environment. Values, policies, and practices related to leadership engagement and professional involvement are related to the psychosocial work environment, the physical work environment, the social responsibility, heath, and stress management resources. The results confirm that an organizational culture that values the well-being and health of the organization’s professionals has a positive relationship with the psychosocial environment, the physical environment, and the relationship with the community and has more resources for professionals’ health. It was also found that an organizational culture mediated by the psychosocial environment is associated with more effective stress management. Management can use this model and this tool for systemic assessment of healthy workplace ecosystems within organizations, thus contributing to continuous monitoring improvements, helping to face the challenges proposed by the Sustainable Development Goals of the United Nations’ 2030 Agenda, namely the SDG3, Good Health and Wellbeing and Decent Work; SDG5, Gender Equality; and SDG 10, Sustainable cities and communities.
1. Introduction
Organizations and labor environments face increasing internal and external, complex, and multidimensional challenges. Organizations are in a paradoxical situation: (a) on the one hand, they are confronted with and sometimes co-create various changes in the social, economic, public health, and health behaviors of professionals and the consequent increase of labor diseases, such as stress and burnout. They also face internal struggles, namely weaknesses in terms of management, relations with leadership, dissatisfaction, burnout, and turnover of professionals [1,2,3]; (b) on the other hand, organizations need to be responsible actors according to the United Nations’ 2030 Agenda for Sustainable Development, in particular where Goal 3, Good Health and Wellbeing, and Goal 5, Gender Equality, are concerned.
The COVID-19 pandemic had an unprecedented impact worldwide regarding the health of populations and organizations, as well as social, economic, educational, and labor impacts. It becomes a necessity, in this context of change, to understand how organizations and professionals adapt and respond to these organizational, social, and political reforms [4,5].
The potential difficulties in studying the dynamics of organizations and external influences lie in their complexity and multidimensional nature, since they involve professional identities and practices, the experience, satisfaction, and rights of professionals, the cultures and structures of organizations, and the value and belief systems of society. Exploring and understanding these aspects requires research methodologies that analyze the process and change and take into consideration diverse and contradictory perspectives. From an ecological perspective, for a better understanding of a complex and multidimensional phenomenon, factors of the organization, factors of the professionals, and factors related to other stakeholders, as well as societal factors, should be included [6,7].
Success in management, concern for the health and well-being of professionals and the organization, and professional satisfaction contribute to the success, adaptation, and sustainability of organizations [8,9,10].
The COVID-19 pandemic led to a global public health crisis and, simultaneously, to an economic and social crisis. Lack of financial liquidity, indebtedness, prolonged growth of unemployment, deteriorating health, and poverty in the long term caused a slow accumulation of social impacts. Research had already demonstrated the devastating consequences the 2008 economic crisis had on certain social groups and for more disadvantaged countries [11,12]. A study by [13] suggests that financial difficulty is the factor that has the most negative impact on health, the quality of life, and the perception of well-being of individuals, rather than the situation of unemployment or low pay per se. The economic and financial crisis affects working conditions in various countries differently. However, there is a common pattern: more unemployment, reduction in total working hours (part-time work), less overtime, growing job insecurity, fewer options for workers, freezing and reducing wages. Quality of life and stress at work are closely linked to the economic crisis and people’s mental health [14,15], thus becoming fundamental variables in the study of and intervention in economic crisis situations [3,15], with special incidence in women and people with social disadvantage [16,17,18,19,20], workers with health conditions [21], and health professionals [22,23].
The Healthy Workplaces Model proposed by the World Health Organization [1] becomes a very useful framework for understanding the systems and dynamics that interact in an organization. The model also includes how each one of systems by itself and the interaction with different systems makes an organization a healthier work environment, promoting the health and well-being of professionals and the organization as a whole. The model integrates dimensions of organizational culture, such as the ethics and values system, leadership engagement, and professionals’ involvement, and includes dimensions related to the psychosocial work environment, physical work environment, social responsibility, and personal health resources.
Deep knowledge of management and organizational culture is closely linked to the ability of organizations to improve excellence, quality of services provided, clients support services, and market positioning. In organization management, one must consider how change strategies are implemented, how leaders promote organizational success, and how the culture affects the performance and satisfaction of professionals and the organization as a whole [24,25].
The success of the organization can be associated with the use of new knowledge to ensure the effective implementation of strategic change initiatives. Often, the evaluation of organizations is carried out considering results that measure only one dimension of success at one level of the system. Organizational assessment would benefit from a multidimensional analysis of different types of outcomes and initiatives in the process of change and improvement [26,27].
The COVID-19 pandemic brought changes at the individual, workplace, and societal levels [28,29]. Organizations and professionals both experienced the direct and devastating impact of COVID-19; it is therefore essential to understand the changes that have taken place. It is also relevant to identify needs and practices that are fundamental to both the recovery of management and quality and health improvements in organizations and work environments. Areas of priority are those related to mental health [19], to some more complex professional contexts such as the health area [28], and to challenges of working at a distance [30].
Several studies have been conducted to understand the impact of COVID-19 on the work environment and on personal and organizational health. We found an increase in psychosocial risks at work, an increase in difficulties in reconciling work and family life, and a greater perception of stress and pressure aggravated by social and gender inequalities [4,20,21].
Organizations and the labor system as a whole deal with a huge challenge, with immediate needs for adjustment, and with consequences for the regular functioning of organizations at diverse levels: at the level of management, professionals, clients, and at the financial economic level [28]. Detailed analysis of the Sustainable Development Goals (SDG) allows for reflecting on how SARS-Cov-2 influenced the goal attainment, making inferences, and finding evidence to support a generalization of quality and universal access to organizations and sustainability. These are fundamental factors in the overall organization and health and well-being of professionals and an indicator of a society’s development [31]. The study of the management and quality of organizations allows the identification of needs at the organizational and health level, at the psychosocial work level, and at the level of equity towards the most disadvantaged and most at-risk groups. In relation to SDG—3, the outcomes of the paper will make it possible to characterize organizations as healthy workplaces and assess the relation between organizational culture, psychosocial work environment, social responsibility, and resources to promote health and well-being for the professional, provided from a systemic perspective. In regard to SDG 5, Gender Equality, the paper has a special focus on the impact of COVID-19. Recent studies show [32,33,34,35] that the negative impact of the pandemic was greater on women, because women had to input greater effort into work/family reconciliation in lockdown situations, were left without jobs, and had greater salary cuts. As well, some professions of greater exposure to COVID-19 are more often held by women (nurses, assistants, cleaning staff, etc.) [32,33,35]. The results obtained in the paper can serve as a basis for adapting the measures necessary to promote equality and empowerment for women. In regard to SDG 10, Sustainable Cities and Communities, the paper will include organizations from different regions of the country, so that it can understand and characterize needs and best practices specific to each region and to areas with different resources and population densities [30,36].
The following hypotheses have been proposed: (1) an organizational culture that values the well-being and health of the organization’s professionals has a positive relationship with the psychosocial environment, the physical environment, and the community and more resources for the professionals’ health, and (2) more positive organizational culture, psychosocial, physical, and community relations, and health resource environments are associated with more effective stress management.
The main objective of this paper is to understand and characterize the healthy work environment of organizations during a COVID-19 pandemic and the relationship between core principles related to content, such as organizational culture (ethics and value system, leadership engagement, and professional involvement), psychosocial work environment (related to work content and relationships with leadership), physical work environment, social responsibility engagement, and resources for occupational health. Stress management is introduced as an adaptive process in the face of challenges caused by the pandemic.
2. Materials and Methods
2.1. Study Design and Participants
A cross-sectional, exploratory study was developed using quantitative methodology. The study involved 460 participants; 231 (50.3%) were female. The workers’ ages ranged between 18 and 67 years, with a mean of 44 years and a standard deviation of 11.36. A convenience sample was included. Professionals who agreed voluntarily to participate in the study were included.
2.2. Instruments
The Healthy Work Environment Ecosystems Tool (EATS) [37] is composed of 62 items organized into 9 dimensions based on the Healthy Workplaces model proposed by the World Health Organization [1]. The dimension Organizational Culture (OC)—Ethics and Values (EV) has 8 items (for example: “The organization values personal and professional development, based on trust, openness and participation”), the dimension Organizational Culture (OC)—Engagement to Leadership (EL) has 6 items (for example: “Leadership values communication and information among workers”), Professionals’ Involvement (PI) has 7 items (for example: “I have a sense of belonging with the company”), Psychosocial work environment related to work content and relationships with leadership (PWECL) has 12 items (for example: “At my place of work, I am informed in advance of important decisions, changes or plans for the future”), Psychosocial of Work Environment related to Well-being and Mental Health (PWEWBMH) has 5 items (for example: “In the past 4 weeks I have felt physically exhausted”), the Physical work environment (PWE) has 5 items (for example: “I am satisfied with the quality of my workspace (organization, comfort, cleanliness, etc.”), teleworking has 3 items (for example: “When I’m teleworking, I have access to the means (technological or otherwise) and to the necessary conditions to support my teleworking activity”), Enterprise Community Involvement (ECI) has 12 items (for example: “Contributes and supports organizations, projects or campaigns that promote community well-being”), and Personal Health Resources (PHR) has 4 items (for example: “The organization provides workers with actions and programs to adopt healthy behaviors (smoking cessation, nutrition, stress management, healthy sleep habits, etc.)”). All questions have a 5-point Likert-type scale where 1 represents strongly disagree and 5 represents strongly agree. A higher score obtained in each domain reveals a more positive perception of a healthy workplace environment, except for the dimension related to Psychosocial of Work Environment related to Well-being and Mental Health, where a higher score reveals a more negative perception regarding the domain. The Cronbach’s alpha levels obtained for each factor show that they have adequate internal consistency (between 0.82 and 0.95).
For the present study, the dimensions that are considered by the authors to be core [1] were computed, and the resulting variable was named Organizational Culture (OC). The dimensions of Psychosocial work environment related to work content and relationships with leadership and Psychosocial of Work Environment related to Well-being and Mental Health were also grouped together, thus constituting for the present study the variable Psychosocial work environment (PsyWe).
The 4-item version of the Stress Perception Scale (EPS) was used to assess the degree to which an individual evaluates their life situations as stressful and their stress management skills [38,39], which, in the present study, revealed adequate internal consistency (α = 0.77). All questions have a 5-point Likert-type scale where 1 represents strongly disagree and 5 represents strongly agree. A higher score obtained in the scale reveals a more positive perception of stress management.
2.3. Procedure
The instrument was submitted and approved by the ethics committee of a national hospital (Prof. Fernando Fonseca Hospital, EPE reference 031/2021). For data collection, organizations from different industries and different regions of the country and of different sizes were contacted. The sample was by convenience. We included large- and medium-sized organizations from various sectors of activity. Public, private, and social organizations were invited to participate.
The organizations that agreed to participate received the instrument through a link and disseminated the link internally among their workers. Data collection was carried out during the pandemic period and respective social and labor restrictions and took place from April to June 2021.
The link gave access to the explanation of the study, contact information of the researchers for clarification of doubts, and information on confidentiality, anonymity, and the voluntary nature of participation. The participant only had access to the beginning of the instrument after signing the informed consent. The questionnaire was conducted via an online platform. On the first page, participants had access to an explanation of the study and objectives and an informed consent statement that they had to validate. Only after validating the informed consent did they access the page where they started filling out the questionnaire.
2.4. Data Analysis
To calculate the final scores of the questionnaires, the results of the items per dimension were summarized and divided by the respective number of items. This procedure was used in order to obtain comparable values since the different dimensions have different numbers of items.
Firstly, the descriptive statistics and analysis Student t-test for all variables was computed according to sex, age, and educational level; it also estimated the effect size of the differences with Cohen’s d. Effect size was interpreted following Cohen [38]: small effect for values around 0.30, moderate effect for values between 0.30 to 0.50, and strong effect for values equal to or higher than 0.50. Secondly, a structural equation model was developed to analyze how the Organizational Culture influences Stress Management through the avenues of influence related to organizational environments.
The statistical software for descriptive statistics and mean comparison was the IBM SPSS Statistics 22 and, for the model of structural equations and invariance analysis, the JASP 0.14.1 program, based on R, was used.
2.5. Model Construction
A structural equation model, with the unweighted least squares method (ULS), was used to analyze how the Organizational Culture influences Stress Management through the avenues of influence related to organizational environments [1]. The fit of the model was evaluated through different adjustment indices: Chi-square (χ2); Comparative Fit Index (CFI), considering appropriate values greater than 0.90; Root Mean Square Error of Approximation (RMSEA); and Standardized Root Mean Squared Residual (SRMR) with values near or below 0.08 and 0.05 considered acceptable.
On the other hand, the intensity of the direct and indirect effects on the model was analyzed through standardized coefficients and their effect size. Eta-square (η2) was considered as Effect size and was calculated following the procedure of Peterson and Brown [40], transforming the standardized β coefficients into r and this indicator into eta-square (η2). The values considered were small effect for values around 0.05, moderate effect for values from 0.06 to 0.11, and a large effect when the values were equal to or greater than 0.14 [38].
Finally, a configurational invariance analysis was realized according to the sex, age, and educational level. The adjustment indices of the models are presented, considering an increase of 0.01 as an indicator of significant change in the models [41].
Incremental fit indices are those indices that evaluate the improvement of the proposed model relative to a base model [42]. Examples are the CFI (Comparative fit index), IFI (Incremental Fit Index), and NNFI (Non-Normed Fit Index), among others. In these indexes, a value of greater than or equal to 0.90 is generally considered adequate, and, if it is greater than or equal to 0.95, it is considered optimal, with the ideal score being 1 [43,44]. Likewise, when the CFI gives a value greater than or equal to 0.95, it is considered that the model fits the sample [45].
3. Results
The great majority of the participants (62.8%) report being married or living with a partner, while 26.7% are single, 9.8% are divorced or separated, and 0.7% are widowed. A majority of 65.9 report having children. As regards education, 30.7% have completed secondary education (mandatory schooling, 12 years), 30.2% have a degree, and 24.8% have a master’s degree.
Participants work in companies from different sectors of activity: 19.3% in the transport and storage sector, 18.7% in the education sector, 13.5% in the health sector, 6.7% in the social sector, 3.9% in the commerce and retail sector, 2.6% in the financial area, and the rest in other areas of activity, such as agriculture, industry, construction, catering, hotels, real estate activities, insurance, etc.
The study was conducted at the national level, in the different regions of Portugal. Of the participants, 59.1% are from the greater Lisbon area, 21.3% from the North and Porto area, 14.3% from the Central area, 2.6% from the Alentejo, and 2.6% from the Algarve.
Regarding the size of the company: 62.1% of the participants belong to large companies (250 employees or more), 20.5% work in medium companies (50 to 249 employees), 9.9% work in small companies (10 to 49 employees), and 8.5% work in micro-enterprise (up to 9 workers).
Table 1 shows the comparison of groups related to gender, age, and educational level obtained in each of the variables. It is observed that the women obtained significantly higher scores in all the variables of the study except Stress Management. The effect size was moderate, except in Personal Health Resources, where it was small. In other words, women reveal a more positive perception of healthy working environments when compared to men. Thus, in relation to each of the dimensions: Organizational Culture (woman—M = 3.57; SD = 0.80; p < 0.001; man—M = 3.17; SD = 0.80; p < 0.001); Psychosocial work environment (woman—M = 3.64; SD = 0.70; p < 0.001; man—M = 3.25; SD = 0.67; p < 0.001); Physical work environment (woman—M = 3.79; SD = 0.82; p < 0.001; man—M = 3.18; SD = 0.96; p < 0.001); Enterprise Community Involvement (woman—M = 3.76; SD = 0.64; p < 0.001; man—M = 3.38; SD = 0.69; p < 0.001); Personal Health Resources (woman—M = 3.04; SD = 0.88; p < 0.001; man—M = 2.84; SD = 0.80; p < 0.001); Stress Management (woman—M = 6.20; SD = 1.30 p < 0.001; man—M = 6.09; SD = 1.30; p = 0.341 (n.s.).

Table 1.
Descriptive Statistics and Comparison analysis according to sex, age, and educational level.
When the sample was divided into age groups, the differences between the scores remained significant in most variables in favor of the younger sample. Participants aged 18 to 40 years were observed to score significantly higher and with small and moderate effect size values in all variables except Stress Management, which was higher in the group of participants over 40 years, with a small effect size. In other words, younger workers reveal a more positive perception of healthy working environments when compared to older workers. Thus, in relation to each of the dimensions: Organizational Culture (young group—18–40 years old—M = 3.60; SD = 0.83; p < 0.001; older group—41–67 years old—M = 3.24; SD = 0.84; p < 0.001); Psychosocial work environment (young group—18–40 years old—M = 3.67; SD = 0.69; p < 0.001; older group—41–67 years old—M = 3.32; SD = 0.69; p < 0.001); Physical work environment (young group—18–40 years old—M = 3.90; SD = 0.85 p < 0.001; older group—41–67 years old—M = 3.26; SD = 0.91; p < 0.001); Enterprise Community Involvement (young group—18–40 years old—M = 3.75; SD = 0.69; p < 0.001; older group—41–67 years old—M = 3.47; SD = 0.68; p < 0.001); Personal Health Resources (young group—18–40 years old—M = 3.12; SD = 0.93; p < 0.001; older group—41–67 years old—M = 2.85; SD = 0.77; p < 0.001); Stress Management (young group—18–40 years old—M = 5.94; SD = 1.31; p = 0.017; older group—41–67 years old—M = 6.25; SD = 1.28; p = 0.017).
According to the educational level, men and women who had a high educational level perceived a better Organizational Culture and scored higher in the rest of the variables under the study than those who had lower levels of education. The effect size took moderate and large values, in most cases, and was small for Stress Management. In other words, workers with a high education level reveal a more positive perception of healthy working environments when compared to workers with compulsory education (12 years of schooling) or less. Thus, in relation to each of the dimensions: Organizational Culture (low education—M = 3.01; SD = 0.81; p < 0.001; high education—M = 3.58; SD = 0.80; p < 0.001); Psychosocial work environment (low education—M = 3.14; SD = 0.63; p < 0.001; high education—M = 3.63; SD = 0.69; p < 0.001); Physical work environment (low education—M = 2.97; SD = 0.83; p < 0.001; high education—M = 3.79; SD = 0.87; p < 0.001); Enterprise Community Involvement (low education—M = 3.26; SD = 0.62; p < 0.001; high education—M = 3.76; SD = 0.67; p < 0.001); Personal Health Resources (low education—M = 2.67; SD = 0.66; p < 0.001; high education—M = 3.10; SD = 0.90; p < 0.001); Stress Management (low education—M = 5.19; SD = 1.32; p < 0.001; high education—M = 6.28; SD = 1.26; p = 0.003).
Summarizing the results, we find that women have more positive perceptions in relation to the different healthy working environments when compared to men. The same is true for younger professionals (aged between 18 years and 40 years). Older professionals (aged between 41 years and 67 years) reveal more stress management skills. With regard to education, professionals with higher education (university education) showed more positive perceptions about the different healthy working environments when compared to professionals with less education (up to 12 years of schooling—compulsory education).
Mediation model of the influence of Organizational Culture on Stress Management through the Core Principles (Burton, 2010) and its invariance across sex, age, and educational level.
Results shows excellent fit indices of the hypothesized mediation model (CFI = 0.976; RMSEA = 0.079; SRMR = 0.075; χ2/df = 3.83), and Figure 1 presents the standardized coefficient of the model estimating.
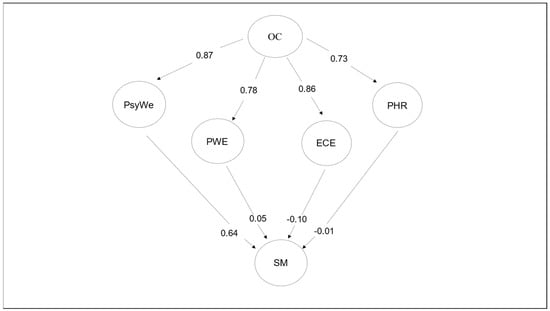
Figure 1.
Representation of the standardized estimations of the path coefficients of the global model. Note: OC, Organizational Culture; PsyWe, Psychosocial Work Environment; PWE, Physical Work Environment; ECE, Enterprise Community Involvement; PHR, Personal Health Resources; SM, Stress Management.
The model explained 75.7% of the variance of Psychosocial work environment (PsyWe), 62.0% of the variance of Physical work environment (PWE), 74.9% of Enterprise Community Involvement (ECI), 53% of Personal Health Resources (PHR), and 23.4% of the variance of Stress Management (SM). The direct paths from Organizational Culture (OC) to SM showed low factor loadings and were not significant. However, the mediation effects assessed suggested that the effect of OC on SM operates mainly through the effects of PsyWe with a strong intensity and a large effect size (β = 0.55; η2 = 0.250). On the other hand, the indirect effect of OC on SM, through of PWE (β = 0.04; η2 = 0.008) and through PHR (β = −0.01; η2 = 0.003), was of low intensity and with a negligible effect in both cases. As for the association between OC and SM through ECE, this was of low intensity with a small effect size PHR (β = −0.09; η2 = 0.020). Regarding the direct effects from the OC on PsyWe, PWE, ECE, and PHR, results showed high factor loadings with a large effect size in all of them.
Finally, configurational invariance analyses were run with samples segmented by sex, age, and educational level. Fit indices for all three variables were excellent and are shown in Table 2. In addition, an increase of 0.01 in CFI is not observed in any of the models, confirming the invariance of the three models.

Table 2.
Goodness of fit for the proposed factorial model and the configurational invariance analysis.
4. Discussion
The main objective of this paper is to understand and characterize the healthy work environment of organizations during the COVID-19 pandemic and the relationship between the core principles related to organizational culture (ethics and value system, leadership engagement, and professional involvement), psychosocial work environment, physical work environment, social responsibility engagement, and resources for occupational health. Stress management was introduced as an adaptive process in the face of the challenges caused in a pandemic context.
The results confirm that an organizational culture that values the well-being and health of the organization’s professionals has a positive relationship with the psychosocial environment, the physical environment, and the relationship with the community and has more resources for the professionals’ health. Was found that an organizational culture mediated by the psychosocial environment is associated with more effective stress management.
Our results show that organizational culture, linked to leadership engagement and professional involvement, has a strong relationship with the other components of a healthy work environment. We emphasize the relationship between stress management skills and the psychosocial work environment, physical work environment, social responsibility and community involvement, and policies and practices for occupational health resources.
The way the organization values and develops strategies to promote the well-being and health of professionals and the type of relationship it establishes with professionals and other stakeholders are aspects of organizational culture that reflect and influence the other systems of the organization. The leadership style, and horizontal and vertical relationships, the type of goals and outcomes, and the way integrity and fairness are valued can be considered other relevant aspects for healthy workplaces [1,2,3,9].
Our results reveal a strong relationship between the psychosocial work environment, related to the relationship with job content, relationship with supervisors and colleagues, perceived autonomy and recognition, and levels of burnout with perceived stress and stress management skills.
The psychosocial work environment is one of the factors most associated with quality of life, well-being, performance, and job satisfaction. The psychosocial work environment integrates aspects related to the type of work that is performed and the relationship with managers, associated with autonomy, recognition, fairness, appreciation, career development expectations, and performance management. The psychosocial work environment also involves aspects related to well-being and mental health, namely levels of stress and burnout, feelings of sadness, and work-life balance [4,14,15,22,46].
Professionals’ involvement—which is reflected in their perceived belonging, motivation, commitment, meaning of work, appreciation, and alignment with goals—can also be more or less valued and mirrored in the organization’s human resource management policies and strategies [4,14].
A healthy workplace can be characterized as having a strong culture that focuses more on professionals’ well-being, a more positive and fair leadership style, and a greater effective involvement of the professional in relation to his/her work, in the definition of objectives and goals, and in a greater connection with the organization as a whole [2,3,25,47].
Results also demonstrate an important relationship between organizational culture and health resources. An organizational culture characterized by well-defined and communicated values, greater leadership commitment, and better staff engagement is associated with better resources and active health promotion practices.
The organization may make more or fewer resources available for the health of professionals, such as encouraging the adoption of a healthy lifestyle, promoting health education actions and programs, and facilitating access to health resources within or outside the organization. An organization that prioritizes the management and mitigation of psychosocial risks at work provides a healthier working environment with fewer unsolved conflicts, fewer incidents/accidents, greater well-being, and better performance [19,48,49].
The results highlight that the organizational culture is associated with the physical environment. A more positive organizational culture is related to a more positive perception of the physical conditions for performing work, such as lighting, noise, space planning, access to technologies, transports accesses, etc.
The physical work environment, associated with physical conditions and satisfaction with the workplace and workspace facilities and/or equipment, particularly in telework situations [50,51,52], are also important factors for job satisfaction, job motivation, quality of life, and well-being [53,54].
The relationship with the community also emerges in our results as strongly related to organizational culture. The relationship with the community is associated with social responsibility, environmental commitment, and the relationship with customers and suppliers. A more positive organizational culture is associated with greater commitment to and involvement in the community.
The organization’s engagement and integration with and connection to the community and the social responsibility towards various stakeholder, such as customers/clients/users [55], as well as suppliers, future generations, minorities, intergenerational and environmental sustainability [56], are associated with healthier workplaces. Additionally, respect for equal opportunities, implementation of actions to promote community’s well-being, and support of professionals and their families in situations of fragility [57,58] are essential for the professionals’ health and well-being [47,59].
The data collection for this study took place in the middle of the COVID-19 pandemic, in periods when measures were very restrictive. Such a life event can be considered stressful, making it all the more relevant to understand the stress management capacity of workers and the key role of organizational culture and psychosocial work environment in mitigating and managing more successfully the impact of the pandemic on personal, work, and even societal levels.
Life events and the work environment can promote high levels of stress when professionals perceive that they cannot control important things, when difficulties or workloads accumulate and they cannot perform with quality, when they consider that they lack the ability to deal with problems and conflicts, and when things do not go their way. In order for professionals to manage their stress situations, they should develop coping and conflict-management strategies, thereby avoiding or reducing serious consequences in terms of their physical, psychological, and social health and job performance [4,53,54].
The COVID-19 pandemic, with all the changes it brought at a personal, social, labor, and societal level, is considered a potentially stressful life event [3] and may even be a traumatic event, in some cases [28,60,61].
Lockdown brought about several changes and consequent work and family challenges that need to be analyzed in depth. People working from home were exposed to specific psychosocial risks, such as isolation, blurred boundaries between work and family, increased risk of domestic violence, and others. Fear of losing their jobs, wage cuts and reductions, redundancies, and reduced benefits caused job insecurity in many workers. I Insecurity, economic loss, and unemployment can have a severe impact on mental health [3,28,60,61,62,63].
Since stress and burnout are major risk factors at work, high levels of stress and its chronicity has a negative impact on the professional’s health, their relationship with the organization in terms of well-being, work relationships, involvement, and performance [19,30,60].
These and other psychosocial risks may arise or increase as a result of COVID-19 and, if not properly assessed and managed, psychosocial risks can increase stress, decrease productivity, and lead to physical and mental health problems [19,30,53,54,64].
In a complementary way, the study allows us to understand the perception of the working environments during the pandemic of some specific groups, and it is possible to identify differences linked to gender, age, and education of the workers. Women, younger professionals, and those with higher education reveal a more positive perception of healthy working environments.
The results in relation to women contradict the results found in the literature, which argue that women were more negatively affected by the pandemic. The pandemic has created greater challenges for women than for men. Women have lost more of their jobs [3,17,20], there are more women than men in essential jobs that expose them to infection and psychological stress, and women have experienced more work problems and overload than men due to increased childcare and other responsibilities. Moreover, teleworking has increased the amount of childcare and domestic care more often provided by women [16]. We can hypothesize that women are less assertive and demanding in relation to their expectations of the responsibility of work organizations to look after their health and promote healthy environments [65].
The results related to age and education are consistent with results found in other studies conducted during the pandemic [4,66,67,68]. Professionals with less education generally have jobs with lower pay, less job stability, and greater risk of losing their jobs.
Regarding age, on the one hand, younger professionals may have jobs associated with greater digital literacy and a greater ability to carry out their work remotely.
The health and well-being of professionals and the organization should be considered as an integrated whole. A healthy workplace and an organization promoting health and well-being at work are increasingly fundamental to the quality and performance of professionals and organizations. The ecological and systemic approach to organizations that we present in this model also integrates the relationship of the organization and professionals with the community and other stakeholders, social and environmental responsibility, and fundamental components for the sustainability of organizations, societies, and our future. The model obtained will allow the diagnosis and monitoring of measures promoting organizational well-being, well-being of professionals, and well-being of other stakeholders belonging to different gender, educational, and age groups. This will allow for the identification and characterization of how organizations can increasingly become healthy workplaces that promote the health of the entire population in an equitable manner. This paper will identify and characterize the factors linked to the organization, professionals, and other stakeholders that most contribute to the economic and financial performance results of professionals. This will allow us to understand and promote the factors associated with better performance and a better quality of life, health, and well-being at work and better health resources.
5. Conclusions
We conclude that an organizational culture that values the well-being and health of the organization’s professionals has a positive relationship with the psychosocial environment, the physical environment, and the relationship with the community, as well as more resources for the professionals’ health. We also found that an organizational culture mediated by the psychosocial environment is associated with more effective stress management.
5.1. Limitations
The main limitations of the study are that the study is cross-sectional and does not allow a rigorous comparison with the pre-COVID period. We have chosen to include professionals at various stages of their working life, from the age of 18 to retirement age. This aspect may be considered a limitation due to the wide age spectrum, but the results are also enriched by having information from every stage of working life. We will continue to increase the sample in order to reduce this limitation and enhance its opportunity.
The results obtained do not incorporate in-depth analysis of the behavior of specific risk groups, such as women, older workers, and workers with a lower level of education. It would be important to increase the sample and study different sectors of activity and different professional groups separately in order to identify and implement specific measures to mitigate this.
5.2. Contributions
One main contribution of the study is that it is the only study that analyses work organizations from a systemic perspective, integrating all the dimensions advocated by the WHO [1] as fundamental for a comprehensive understanding of healthy work environments. Other studies carried out only include some of the dimensions and systems. A second contribution is to the understanding of the role of stress management in its relationship with healthy work environments and how it can be considered a protective factor against the COVID-19 pandemic. The findings suggest that promoting stress management skills among workers will be a priority if they are to cope more effectively with daily challenges, as well as more global challenges, such as other health crises, war, and economic recession.
The main recommendations proposed as a result of the study: (a) To assess and monitor the healthy working environment in a systemic and integrative perspective and on a regular basis; (b) To actively involve all stakeholders in the assessment and monitoring process; (c) Specific and realistic objectives and targets should be set and, consequently, the necessary pre-established changes planned, implemented, and evaluated; evaluated results should be given as feedback and discussed with all stakeholders; (d) To set an appropriate number of objectives to be achieved within a well-timed timeframe using realistic resources; (e) Managers and leaders need to have continuous training in relevant areas for optimizing the performance of their functions; (f) Professionals would benefit from having greater involvement with greater autonomy and accountability; (g) To prioritize the promotion of healthy workplaces through the implementation of policies and activities aimed at improving psychosocial working conditions and promoting the physical, social and mental health of professionals; (h) To promote greater social and environmental responsibility and engagement between the organization and the community and favor green policies and practices.
Author Contributions
Conceptualization, T.G. and M.F.C.; methodology, T.G. and V.S.; software, F.B.G.; validation, T.G. and M.d.C.M.; formal analysis, T.G. and V.S.; investigation, T.G., F.B.G. and M.F.C.; writing—original draft preparation, T.G. and V.S.; writing—review and editing, T.G., F.B.G. and M.F.C.; supervision, M.G.M. and M.d.C.M.; project administration, T.G. All authors have read and agreed to the published version of the manuscript.
Funding
This work was developed in the framework of national funds through FCT—Fundação para a Ciência e a Tecnologia, I.P., under project UIDB/05380/2020.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the ethics committee of a national hospital (Prof. Fernando Fonseca Hospital, EPE reference 031/2021), and approval validated by the Ethics Committee of Lusofona University, CEDIC.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data is unavailable due to privacy or ethical restriction.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Burton, J. WHO Healthy Workplaces Framework and Model: Background and Supporting Literature and Practice; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- BNQ. Psychological Health and Safety in the Workplace: Prevention, Promotion, and Guidance to Staged Implementation; Bureau de normalisation du Québec: Québec, QC, Canada, 2018. [Google Scholar]
- International Labour Organization. ILO Monitor: COVID-19 and the World of Work; International Labour Organization: Geneva, Switzerland, 2020; Available online: https://reliefweb.int/report/world/ilo-monitor-covid-19-and-world-work-eighth-edition-enardeitpttrthvi?gclid=CjwKCAjwtuOlBhBREiwA7agf1oDFEG6SMRbbFH0DmaOWwM8IhvTMIK7uLXm3uRXiidyT5Yzh94X2HRoCovQQAvD_BwE (accessed on 1 May 2023).
- Gaspar, T.; Paiva, T.; Matos, M.G. Impact of COVID-19 in Global Health and Psychosocial Risks at Work. J. Occup. Environ. Med. 2021, 63, 581–587. [Google Scholar] [CrossRef]
- International Labour Organization. Managing Work-Related Psychosocial Risks during the COVID-19 Pandemic; International Labour Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Bronfenbrenner, U. Making Human Beings Human: Bioecological Perspectives on Human Development; Sage Publications: New York, NY, USA, 2005. [Google Scholar]
- Eriksson, M.; Ghazinour, M.; Hammarström, A. Different Uses of Bronfenbrenner’s Ecological Theory in Public Mental Health Research: What Is Their Value for Guiding Public Mental Health Policy and Practice? Soc. Theory Health 2018, 16, 414–433. [Google Scholar] [CrossRef]
- Choudhury, T.; Debski, M.; Wiper, A.; Abdelrahman, A.; Wild, S.; Chalil, S.; More, R.; Goode, G.; Patel, B.; Abdelaziz, H.K. COVID-19 Pandemic: Looking after the Mental Health of Our Healthcare Workers. J. Occup. Environ. Med. 2020, 62, e373–e376. [Google Scholar] [CrossRef] [PubMed]
- European Agency for Safety and Health at Work (EU-OSHA). OSH in Figures: Stress at Work-Facts and Figures; Office for Official Publications of the European Communities, European Agency for Safety and Health at Work: Bilbao, Spain, 2009. [Google Scholar]
- Griffith, J.R. Understanding High-Reliability Organizations: Are Baldrige Recipients Models? J. Healthc. Manag. 2015, 60, 44–61. [Google Scholar] [CrossRef]
- Clench-Aas, J.; Holte, A. The Financial Crisis in Europe: Impact on Satisfaction with Life. Scand. J. Public Health 2017, 45, 30–40. [Google Scholar] [CrossRef]
- Eurofound. Living and Working in Europe 2017; Publications Office of the European Union; Eurofound: Dublin, Ireland, 2017. [Google Scholar]
- Gudmundsdottir, D.G. The Impact of Economic Crisis on Happiness. Soc. Indic. Res. 2013, 110, 1083–1101. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 Pandemic and Mental Health Consequences: Systematic Review of the Current Evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Wilson, J.M.; Lee, J.; Fitzgerald, H.N.; Oosterhoff, B.; Sevi, B.; Shook, N.J. Job Insecurity and Financial Concern during the COVID-19 Pandemic Are Associated with Worse Mental Health. J. Occup. Environ. Med. 2020, 62, 686–691. [Google Scholar] [CrossRef]
- Carli, L.L. Women, Gender Equality and COVID-19. Gend. Manag. Int. J. 2020, 35, 647–655. [Google Scholar] [CrossRef]
- Collins, C.; Landivar, L.C.; Ruppanner, L.; Scarborough, W.J. COVID-19 and the Gender Gap in Work Hours. Gend. Work Organ. 2021, 28, 101–112. [Google Scholar] [CrossRef]
- Gaspar, T.; Cabrita, T.; Rebelo, A.; Matos, M. Psychological and Social Factors That Influence Quality of Life: Gender, Age and Professional Status Differences. Psychol. Res. 2017, 7, 489–498. [Google Scholar] [CrossRef]
- OECD. Tackling the Mental Health Impact of the COVID-19 Crisis: An Integrated, Whole-of-Society Response; OECD Publishing: Paris, France, 2021; Available online: https://read.oecd-ilibrary.org/ (accessed on 1 May 2023).
- Reichelt, M.; Makovi, K.; Sargsyan, A. The Impact of COVID-19 on Gender Inequality in the Labor Market and Gender-Role Attitudes. Eur. Soc. 2021, 23, S228–S245. [Google Scholar] [CrossRef]
- Saqib, M.A.N.; Siddiqui, S.; Qasim, M.; Jamil, M.A.; Rafique, I.; Awan, U.A.; Ahmad, H.; Afzal, M.S. Effect of COVID-19 Lockdown on Patients with Chronic Diseases. Diabetes Metab. Syndr. 2020, 14, 1621–1623. [Google Scholar] [CrossRef]
- Giménez-Espert, M.D.C.; Prado-Gascó, V.; Soto-Rubio, A. Psychosocial Risks, Work Engagement, and Job Satisfaction of Nurses during COVID-19 Pandemic. Front. Public Health 2020, 8, 566896. [Google Scholar] [CrossRef] [PubMed]
- Steidtmann, D.; McBride, S.; Mishkind, M.C. Experiences of Mental Health Clinicians and Staff in Rapidly Converting to Full-Time Telemental Health and Work from Home during the COVID-19 Pandemic. Telemed. e-Health 2021, 27, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Bartram, T.; Stanton, P.; Bamber, G.J.; Leggat, S.G.; Ballardie, R.; Gough, R. Engaging Professionals in Sustainable Workplace Innovation: Medical Doctors and Institutional Work: Workplace Innovation for Medical Doctors. Br. J. Manag. 2020, 31, 42–55. [Google Scholar] [CrossRef]
- Fladerer, M.P.; Braun, S. Managers’ Resources for Authentic Leadership–A Multi-study Exploration of Positive Psychological Capacities and Ethical Organizational Climates. Br. J. Manag. 2020, 31, 325–343. [Google Scholar] [CrossRef]
- Kash, B.A.; Spaulding, A.; Johnson, C.E.; Gamm, L. Success Factors for Strategic Change Initiatives: A Qualitative Study of Healthcare Administrators’ Perspectives. J. Healthc. Manag. 2014, 59, 65–81. [Google Scholar] [CrossRef]
- Spaulding, A.; Kash, B.A.; Johnson, C.E.; Gamm, L. Organizational Capacity for Change in Health Care: Development and Validation of a Scale. Health Care Manag. Rev. 2017, 42, 151–161. [Google Scholar] [CrossRef]
- Gaspar, T.; Salado, V.; do Céu Machado, M.; Guedes, F.B.; Faia-Correia, M.; Coelho, A. Impact of COVID-19 on Management, Quality and Satisfaction of Health Organizations: A Case Study in a Portuguese Hospital. Int. J. Environ. Res. 2023, 17, 21. [Google Scholar] [CrossRef]
- Slavković, M.; Sretenović, S.; Bugarčić, M. Remote Working for Sustainability of Organization during the COVID-19 Pandemic: The Mediator-Moderator Role of Social Support. Sustainability 2021, 14, 70. [Google Scholar] [CrossRef]
- OECD. Recommendation of the Council on Integrated Mental Health, Skills and Work Policy; OECD Publishing: Paris, France, 2022; Available online: https://legalinstruments.oecd.org/public/doc/334/334.en.pdf (accessed on 29 April 2023).
- United Nations. The Sustainable Development Goals Report; United Nations: New York, NY, USA, 2022; Available online: https://unstats.un.org/sdgs/report/2022/ (accessed on 27 April 2023).
- Butterick, M.; Charlwood, A. HRM and the COVID-19 Pandemic: How Can We Stop Making a Bad Situation Worse? Hum. Resour. Manag. J. 2021, 31, 847–856. [Google Scholar] [CrossRef]
- Gonçalves, S.P.; dos Santos, J.V.; Silva, I.S.; Veloso, A.; Brandão, C.; Moura, R. COVID-19 and People Management: The View of Human Resource Managers. Adm. Sci. 2021, 11, 69. [Google Scholar] [CrossRef]
- United Nations. Progress on the Sustainable Development Goals: The Gender Snapshot 2022; United Nations: New York, NY, USA, 2022; Available online: https://www.unwomen.org/en/digital-library/publications/2022/09/progress-on-the-sustainable-development-goals-the-gender-snapshot-2022 (accessed on 27 April 2023).
- Wenham, C.; Smith, J.; Morgan, R. Gender and COVID-19 Working Group. COVID-19: The Gendered Impacts of the Outbreak. Lancet 2020, 395, 846–848. [Google Scholar] [CrossRef]
- Rožman, M.; Sternad Zabukovšek, S.; Bobek, S.; Tominc, P. Gender Differences in Work Satisfaction, Work Engagement and Work Efficiency of Employees during the COVID-19 Pandemic: The Case in Slovenia. Sustainability 2021, 13, 8791. [Google Scholar] [CrossRef]
- Gaspar, T.; Faia-Correia, M.; Machado, M.C.; Xavier, M.; Guedes, F.B.; Pais-Ribeiro, J.; Matos, M.G. Ecossistemas Dos Ambientes de Trabalho Saudáveis (EATS): Instrumento de Avaliação Dos Healthy Workplaces. Rev. Psicol. Saúde Doenças Doenças 2022, 23, 253–269. [Google Scholar] [CrossRef]
- Cohen, J. The Effect Size. Statistical Power Analysis for the Behavioral Sciences; Taylor and Francis: Abingdon, UK, 1988; pp. 77–83. [Google Scholar]
- Pais-Ribeiro, J.; Marques, T. A avaliação do stresse: A propósito de um estudo de adaptação da escala de percepção de stresse. Psicol. Saúde E Doenças 2009, 10, 237–248. [Google Scholar]
- Peterson, R.A.; Brown, S.P. On the Use of Beta Coefficients in Meta-Analysis. J. Appl. Psychol. 2005, 90, 175–181. [Google Scholar] [CrossRef]
- Cheung, G.W.; Rensvold, R.B. Evaluating Goodness-of-Fit Indexes for Testing Measurement Invariance. Struct. Equ. Model. 2002, 9, 233–255. [Google Scholar] [CrossRef]
- McNeish, D.; An, J.; Hancock, G.R. The Thorny Relation between Measurement Quality and Fit Index Cutoffs in Latent Variable Models. J. Pers. Assess. 2018, 100, 43–52. [Google Scholar] [CrossRef]
- Brown, T. Confirmatory Factor Analysis for Applied Research; Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- Kline, R.B. Response to Leslie Hayduk’s Review of Principles and Practice of Structural Equation Modeling, 4th Edition. Can. Stud. Popul. 2018, 45, 188. [Google Scholar] [CrossRef]
- Lai, K. Fit Difference between Nonnested Models given Categorical Data: Measures and Estimation. Struct. Equ. Modeling 2021, 28, 99–120. [Google Scholar] [CrossRef]
- SA Health. A Workplace Health and Wellbeing Toolkit: Step by Step Guide to Developing a Successful Workplace Program; SA Health Government of South Australia: Adelaide, Australia, 2012.
- Žižek, S.Š.; Mulej, M.; Potočnik, A. The Sustainable Socially Responsible Society: Well-Being Society 6.0. Sustainability 2021, 13, 9186. [Google Scholar] [CrossRef]
- OECD. OECD Guidelines on Measuring the Quality of the Working Environment; OECD: Paris, France, 2017; ISBN 9789264278233. [Google Scholar]
- World Health Organization (WHO). Healthy Workplaces: A Model for Action: For Employers, Workers, Policymakers and Practitioners; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Park, S.; Jeong, S.; Chai, D.S. Remote E-Workers’ Psychological Well-Being and Career Development in the Era of COVID-19: Challenges, Success Factors, and the Roles of HRD Professionals. Adv. Dev. Hum. Resour. 2021, 23, 222–236. [Google Scholar] [CrossRef]
- Pulido-Martos, M.; Cortés-Denia, D.; Lopez-Zafra, E. Teleworking in Times of COVID-19: Effects on the Acquisition of Personal Resources. Front. Psychol. 2021, 12, 685275. [Google Scholar] [CrossRef]
- Niu, Q.; Nagata, T.; Fukutani, N.; Tezuka, M.; Shimoura, K.; Nagai-Tanima, M.; Aoyama, T. Health Effects of Immediate Telework Introduction during the COVID-19 Era in Japan: A Cross-Sectional Study. PLoS ONE 2021, 16, e0256530. [Google Scholar] [CrossRef]
- World Health Organization (WHO). W.H. Considerations for Public Health and Social Measures in the Workplace in the Context of COVID-19. 2023. Available online: https://www.who.int/publications/i/item/considerations-for-public-health-and-social-measures-in-the-workplace-in-the-context-of-covid-19 (accessed on 2 May 2023).
- World Health Organization (WHO). COVID-19: Occupational Health and Safety for Health Workers: Interim Guidance; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Yoshida, M.; Gordon, B.S.; James, J.D. Social Capital and Consumer Happiness: Toward an Alternative Explanation of Consumer-Brand Identification. J. Brand Manag. 2021, 28, 481–494. [Google Scholar] [CrossRef]
- Cuesta-Valiño, P.; Gutiérrez-Rodríguez, P.; Sierra-Fernández, M.-P.; Aguirre García, M.-B. Measuring a Multidimensional Green Brand Equity: A Tool for Entrepreneurship Development. Br. Food J. 2021, 123, 3326–3343. [Google Scholar] [CrossRef]
- García-Sánchez, I.-M.; Hussain, N.; Khan, S.-A.; Martínez-Ferrero, J. Assurance of Corporate Social Responsibility Reports: Examining the Role of Internal and External Corporate Governance Mechanisms. Corp. Soc. Responsib. Environ. Manag. 2022, 29, 89–106. [Google Scholar] [CrossRef]
- Rela, I.Z.; Awang, A.H.; Ramli, Z.; Md Sum, S.; Meisanti, M. Effects of Environmental Corporate Social Responsibility on Environmentalwell-beingperception and the Mediation Role of Community Resilience. Corp. Soc. Responsib. Environ. Manag. 2020, 27, 2176–2187. [Google Scholar] [CrossRef]
- Macassa, G.; McGrath, C.; Tomaselli, G.; Buttigieg, S.C. Corporate Social Responsibility and Internal Stakeholders’ Health and Well-Being in Europe: A Systematic Descriptive Review. Health Promot. Int. 2021, 36, 866–883. [Google Scholar] [CrossRef]
- Kalaitzaki, A.E.; Tsouvelas, G.; Tamiolaki, A.; Konstantakopoulos, G. Post-Traumatic Stress Symptoms during the First and Second COVID-19 Lockdown in Greece: Rates, Risk, and Protective Factors. Int. J. Ment. Health Nurs. 2022, 31, 153–166. [Google Scholar] [CrossRef]
- Lahav, Y. Psychological Distress Related to COVID-19-The Contribution of Continuous Traumatic Stress. J. Affect. Disord. 2020, 277, 129–137. [Google Scholar] [CrossRef]
- Feng, Z.; Savani, K. COVID-19 Created a Gender Gap in Perceived Work Productivity and Job Satisfaction: Implications for Dual-Career Parents Working from Home. Gend. Manag. Int. J. 2020, 35, 719–736. [Google Scholar] [CrossRef]
- Krukowski, R.A.; Jagsi, R.; Cardel, M.I. Academic Productivity Differences by Gender and Child Age in Science, Technology, Engineering, Mathematics, and Medicine Faculty during the COVID-19 Pandemic. J. Womens Health (Larchmt) 2021, 30, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Tronco Hernandez, Y.A. Remote Workers during the COVID-19 Lockdown. What Are We Missing and Why Is Important. J. Occup. Environ. Med. 2020, 62, e669–e672. [Google Scholar] [CrossRef] [PubMed]
- Zinn, I.; Hofmeister, H. The gender order in action: Consistent evidence from two distinct workplace settings. J. Gend. Stud. 2022, 31, 941–955. [Google Scholar] [CrossRef]
- Davis, O.; Quinby, L.; Rutledge, M.; Wettstein, G. How did COVID-19 affect the labor force participation of older workers in the first year of the pandemic? J. Pension Econ. Financ. 2023, 1–15. [Google Scholar] [CrossRef]
- OECD. The Unequal Impact of COVID-19: A Spotlight on Frontline Workers, Migrants and Racial/Ethnic Minorities. 2022. Available online: https://www.oecd.org/coronavirus/policy-responses/the-unequal-impact-of-covid-19-a-spotlight-on-frontline-workers-migrants-and-racial-ethnic-minorities-f36e931e/ (accessed on 2 May 2023).
- Sigahi, T.F.A.C.; Kawasaki, B.C.; Bolis, I.; Morioka, S.N. A systematic review on the impacts of COVID-19 on work: Contributions and a path forward from the perspectives of ergonomics and psychodynamics of work. Hum. Factors Ergon. Manuf. 2021, 31, 375–388. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).