Effects of Health Factors on GDP Growth: Empirical Evidence from Saudi Arabia
Abstract
1. Introduction
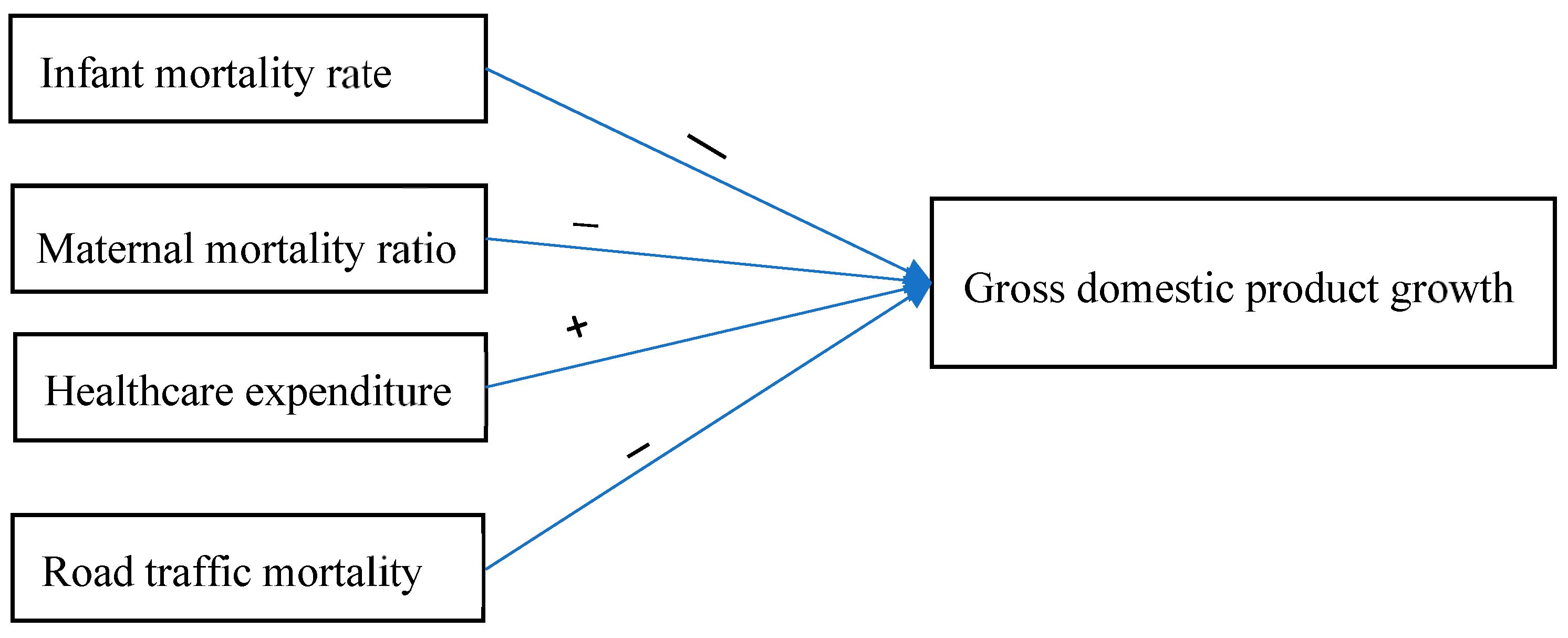
- How are health indicators (such as decreasing IMR, MMR, and RTM and increasing HCE) related to GDP growth in Saudi Arabia in the short and long run, and what is the nature of this impact (positive or negative)?
- Is there a causal relationship between Saudi Arabia’s GDP growth and health factors over time?
- What are the effective policies that should be implemented to address health-related issues and achieve sustainable GDP growth in Saudi Arabia?
2. Literature Review and Hypotheses Development
2.1. Theoretical Framework
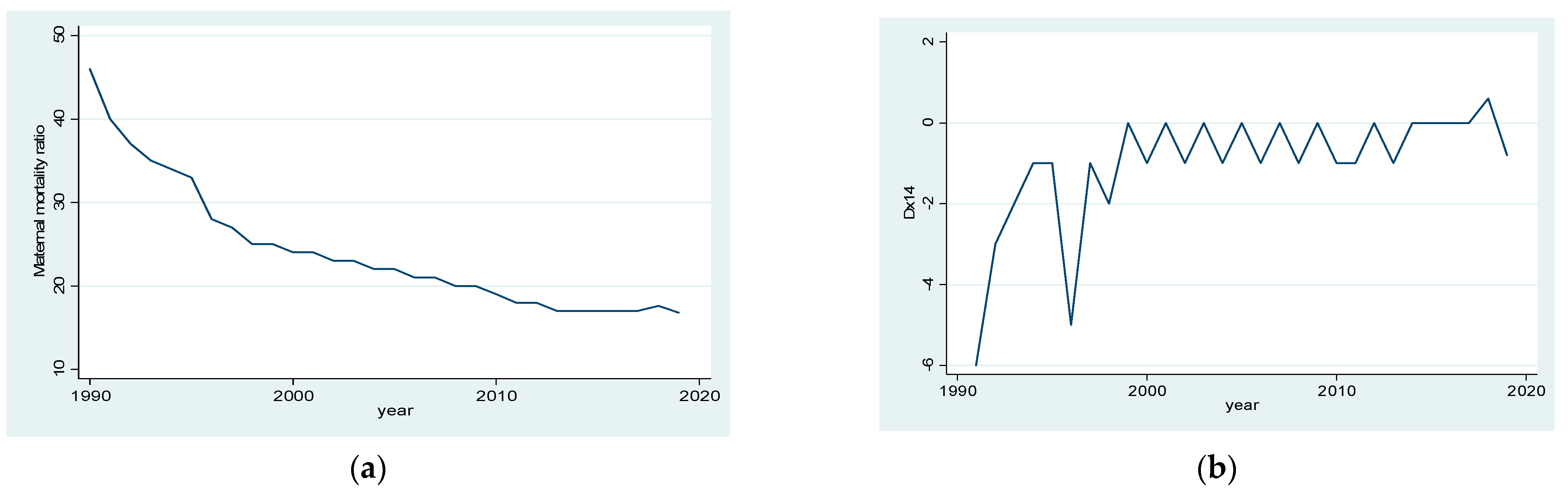
2.2. Relationship between Maternal Mortality Ratio (MMR) and GDP Growth
2.3. Relationship between Infant Mortality Rate (IMR) and GDP Growth
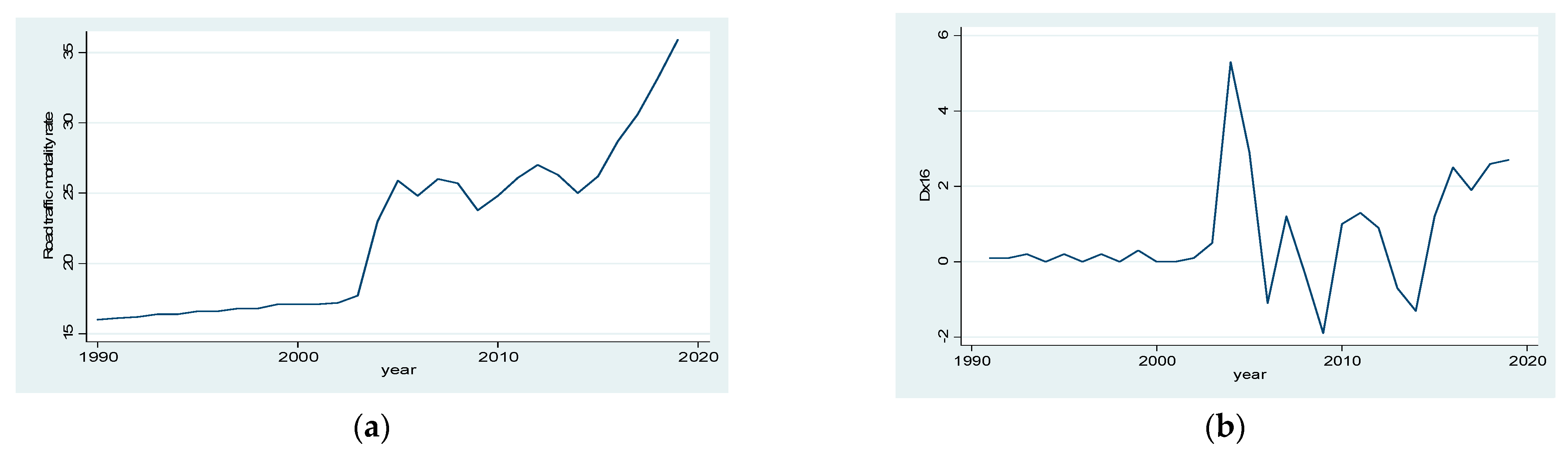
2.4. Relationship between Road Traffic Mortality (RTM) and Economic Growth
2.5. Relationship between Health Care Expenditure (HCE) and GDP Growth
3. Materials and Methods
3.1. Description and Sources of Data
3.2. Model Specification
3.3. Analytical Tools
3.4. Unit Root Test
3.5. Cointegration Test
3.6. Lag Selection Criteria
3.7. Vector Error Correction (VEC) Model
3.8. Granger Causality Test
4. Results Analysis
5. Discussion
6. Practical Implications
7. Conclusions
8. Limitations and Future Directions of the Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ADF | Augmented Dickey–Fuller |
| AIC | Akaike information criterion |
| ARDL | Autoregressive Distributed Lag |
| ECT | Error correction term |
| FPE | Final prediction error |
| GDP | Gross domestic product |
| GDPG | GDP growth |
| HCE | Healthcare expenditure |
| HQIC | Hannan-Quinn information criterion |
| IMR | Infant mortality rate |
| JB | Jarque-Bera |
| LMIC | Low and Middle Income Countries |
| LR | Likelihood ratio |
| MMR | Maternal mortality ratio |
| OLS | Ordinary Least Square |
| PP | Phillips, and Perron |
| RTM | Road traffic mortality |
| SBIC | Schwarz information criterion |
| SD | Standard deviation |
| UN | United Nations |
| USA | United States of America |
| VAR | Vector autoregressive |
| VEC | Vector error correction |
| WB | World Bank |
| WHO | World Health Organization |
References
- Acemoglu, D.; Johnson, S. Disease and development: The effect of life expectancy on economic growth. J. Political Econ. 2007, 115, 925–985. [Google Scholar] [CrossRef]
- Lorentzen, P.; McMillan, J.; Wacziarg, R. Death and development. J. Econ. Growth 2008, 13, 81–124. [Google Scholar] [CrossRef]
- Lucas, R.E., Jr. On the mechanics of economic development. J. Monet. Econ. 1988, 22, 3–42. [Google Scholar] [CrossRef]
- Bloom, D.E.; Canning, D.; Kotschy, R.; Prettner, K.; Schünemann, J.J. Health and Economic Growth: Reconciling the Micro and Macro Evidence; National Bureau of Economic Research: Cambridge, MA, USA, 2019. [Google Scholar]
- Rocco, L.; Fumagalli, E.; Mirelman, A.J.; Suhrcke, M. Mortality, morbidity and economic growth. PLoS ONE 2021, 16, e0251424. [Google Scholar] [CrossRef]
- Bank, W. Current Health Expenditure Per Capita (Current US$); World data bank (WB): Washington, WA, USA, 2022. [Google Scholar]
- OPEC. Saudi Arabia: Organization of the Petroleum Exporting Countries; OPEC: Vienna, Austria, 2019. [Google Scholar]
- Grand, S.; Wolff, K. Assessing Saudi Vision 2030: A 2020 Review; Atlantic Council: Washington, WA, USA, 2020. [Google Scholar]
- Arabia, S. Vision 2030: Kingdom of Saudi Arabia; Riyadh, Saudi Arabia, 2016. Available online: https://vision2030.gov.sa/en (accessed on 12 January 2023).
- Young, Y.; Alharthy, A.; Hosler, A.S. Transformation of Saudi Arabia’s Health System and Its Impact on Population Health: What Can the USA Learn? Saudi J. Health Syst. Res. 2021, 1, 93–102. [Google Scholar] [CrossRef]
- Solow, R. A Contribution to the Theory of Economic Growth. Q. J. Econ. 1956, 70, 65–94. [Google Scholar] [CrossRef]
- Romer, P.M. Increasing Returns and Long Run Growth. J. Political Econ. 1986, 94, 1002–1037. [Google Scholar] [CrossRef]
- Mankiw, G.; Romer, D.; Weil, D. A contribution on the Empirics of Economic Growth. Q. J. Econ. 1992, 107, 407–437. [Google Scholar] [CrossRef]
- Bloom, D.E.; Canning, D.; Sevilla, J. The Effect of Health on Economic Growth: A Production Function Approach. World Dev. 2004, 32, 1–13. [Google Scholar] [CrossRef]
- Ajide, K.B. Determinants of Economic Growth in Nigeria. CBN J. Appl. Stat. 2014, 5, 8. Available online: https://dc.cbn.gov.ng/jas/vol5/iss2/8 (accessed on 12 January 2023).
- Boachie, M.K. Health and Economic Growth in Ghana: An Empirical Investigation. Fudan J. Humanit. Soc. Sci. 2017, 10, 253–265. [Google Scholar] [CrossRef]
- Barro, R. Health and Economic Growth; World Health Organization: Geneva, Switzerland, 1996. [Google Scholar]
- Folland, S.; Goodman, A.; Stano, M. The Economics of Health and Health Care, Pearson New International Edition; Routledge: New York, NY, USA, 2016. [Google Scholar]
- Lopez, C.; Rivera, B.; Currais, L. Health and Economic Growth, Findings and Policy Implication; MIT Press: Cambridge, UK, 2005. [Google Scholar]
- Scheffler, R.M. Health Expenditure and Economic Growth: An International Perspective; Berkeley Public Policy; The Goldman School: Berkeley, CA, USA, 2004. [Google Scholar]
- Islam, M.M.; Alharthi, M. Impact of COVID-19 on the Quality of Life of Households in Saudi Arabia. Int. J. Environ. Res. Public Health 2022, 19, 1538. [Google Scholar] [CrossRef]
- Islam, M.M.; Islam, M.M.; Khoj, H. Coping Mechanisms and Quality of Life of Low-Income Households during the COVID-19 Pandemic: Empirical Evidence from Bangladesh. Sustainability 2022, 14, 16570. [Google Scholar] [CrossRef]
- Messabia, N.; Fomi, P.-R.; Kooli, C. Managing restaurants during the COVID-19 crisis: Innovating to survive and prosper. Innov. Knowl. 2022, 7, 100234. [Google Scholar] [CrossRef]
- Ridhwan, M.M.; Nijkamp, P.; Ismail, A.; Irsyad, L. The effect of health on economic growth: A meta-regression analysis. Empir. Econ. 2022, 63, 3211–3251. [Google Scholar] [CrossRef]
- Barro, R.J.; Lee, J.-W. Sources of Economic Growth. In Carnegie-Rochester Conference series on Public Policy; Elsevier: Amsterdam, The Netherlands, 1994. [Google Scholar]
- Barro, J.; Sala-i-Martin, X. Economic Growth; McGraw-Hill: Boston, MA, USA, 1995. [Google Scholar]
- Trondillo, J. Estimating the effect of maternal and child health outcomes to GDP per Capita. Br. J. Econ. Manag. Trade 2016, 12, 1–12. [Google Scholar] [CrossRef]
- Thompson, E.; Sofo, S. Economic Impact of Maternal Mortality in Africa: A Panel Data Approach. J. Stat. Econom. Methods 2015, 4, 65–78. [Google Scholar]
- Girum, T.; Wasie, A. Correlates of maternal mortality in developing countries: An ecological study in 82 countries. Matern. Health Neonatol. Perinatol. 2017, 3, 1–6. [Google Scholar] [CrossRef]
- Mohamed, H.A. Estimation of socio-economic cost of road accidents in Saudi Arabia: Willingness-to-pay approach (WTP). Adv. Manag. Appl. Econ. 2015, 5, 43. [Google Scholar]
- Frank, O. Maternal Health Outcome and Economic Growth in Sub-Saharan Africa: A Dynamic Panel Analysis. Int. J. Econ. Manag. Eng. 2020, 14, 696–704. [Google Scholar]
- Kirigia, J.M.; Preker, A.; Carrin, G.; Mwikisa, C.; Diarra-Nama, A.J. An overview of health financing patterns and the way forward in the WHO African Region. East Afr. Med. J. 2007, 83, S1–S28. [Google Scholar] [CrossRef]
- Kes, A.; Ogwang, S.; Pande, R.P.; Douglas, Z.; Karuga, R.; O Odhiambo, F.; Laserson, K.F.; Schaffer, K. The economic burden of maternal mortality on households: Evidence from three sub-counties in rural western Kenya. Reprod. Health 2015, 12, S3. [Google Scholar] [CrossRef]
- Amiri, A.; Gerdtham, U.-G. Impact of Maternal and Child Health on Economic Growth: New Evidence Based Granger Causality and DEA Analysis. In Newborn and Child Health, Study Commissioned by the Partnership for Maternal; Lund University: Lund, Sweden, 2013. [Google Scholar]
- Mohamed, E.S. Bounds Test Cointegration Approach to Examine Factors Contributing to Declining Maternal Mortality Ratio in Sudan (1969–2015); Leibniz Information Centre for Economics: Düsternbrooker, Germany, 2018. [Google Scholar]
- Aghion, P.; Howitt, P.; Murtin, F. The relationship between health and growth: When Lucas meets Nelson–Phelps. Rev. Econ. Inst. 2010, 2, 1–24. [Google Scholar]
- Nishiyama, A. Economic growth and infant mortality in developing countries. Eur. J. Dev. Res. 2011, 23, 630–647. [Google Scholar] [CrossRef]
- Baird, S.; Friedman, J.; Schady, N. Aggregate income shocks and infant mortality in the developing world. Rev. Econ. Stat. 2011, 93, 847–856. [Google Scholar] [CrossRef]
- Nevo, A.; Rosen, A.M. Identification with imperfect instruments. Rev. Econ. Stat. 2012, 94, 659–671. [Google Scholar] [CrossRef]
- Khan, M.; Fatima, S.; Zia, S.S.; Hussain, E.; Faraz, T.R.; Khalid, F. Modeling and Forecasting Infant Mortality Rates of Asian Countries in the Perspective of GDP (PPP). Int. J. Sci. Eng. Res. 2019, 10, 18–23. [Google Scholar]
- Hamzat, S.; Ebeh, J.E.; Ali, M. Impact of Health Expenditure on Child Mortality Rate in Nigeria, 1980–2015. Lafia J. Econ. Manag. Sci. 2019, 4, 33. [Google Scholar]
- O’Hare, B.A.-M.; Makuta, I.; Chiwaula, L.; Bar-Zeev, N. Income and child mortality in developing countries: A systematic review and meta-analysis. J. R. Soc. Med. 2013, 106, 408–414. [Google Scholar] [CrossRef]
- Strittmatter, A.; Sunde, U. Health and economic development—Evidence from the introduction of public health care. J. Popul. Econ. 2013, 26, 1549–1584. [Google Scholar] [CrossRef]
- Eboh, I.A.; Aduku, E.B.; Onwughalu, U.B. Health Expenditure, Child Mortality and Economic Growth in Nigeria. Int. J. Econ. Dev. Res. (IJEDR) 2022, 3, 198–216. [Google Scholar] [CrossRef]
- WHO. World Health Statistics 2022: Monitoring Health for the SDGs, Sustainable Development Goals; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Van Lerberghe, W. The World Health Report 2008: Primary Health Care: Now More than Ever; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- WHO. Association for Safe International Road Travel. Faces Behind Igures: Voices of Road Trafic Crash Victims and Their Families; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Dalal, K.; Lin, Z.; Gifford, M.; Svanström, L. Economics of global burden of road traffic injuries and their relationship with health system variables. Int. J. Prev. Med. 2013, 4, 1442–1450. [Google Scholar] [PubMed]
- Al Turki, Y.A. How can Saudi Arabia use the Decade of Action for Road Safety to catalyse road traffic injury prevention policy and interventions? Int. J. Inj. Control. Saf. Promot. 2014, 21, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Jagnoor, J.; Prinja, S.; Lakshmi, P.V.M.; Aggarwal, S.; Gabbe, B.; Ivers, R. The impact of road traffic injury in North India: A mixed-methods study protocol. BMJ Open 2015, 5, e008884. [Google Scholar] [CrossRef]
- Gorea, R. Financial impact of road traffic accidents on the society. Int. J. Ethics Trauma Vict. 2016, 2, 6–9. [Google Scholar] [CrossRef]
- Bhavan, T. The economic impact of road accidents: The case of Sri Lanka. South Asia Econ. J. 2019, 20, 124–137. [Google Scholar] [CrossRef]
- Zeng, L.; Li, H.; Lao, X.; Hu, H.; Wei, Y.; Li, C.; Yuan, X.; Guo, D.; Liu, K. China’s Road Traffic Mortality Rate and Its Empirical Research from Socio-Economic Factors Based on the Tobit Model. Systems 2022, 10, 122. [Google Scholar] [CrossRef]
- Hu, G.; Wen, M.; Baker, T.D.; Baker, S.P. Road-traffic deaths in China, 1985–2005: Threat and opportunity. Inj. Prev. 2008, 14, 149–153. [Google Scholar] [CrossRef]
- Ozturk, S.; Topcu, E. Health Expenditures and Economic Growth: Evidence from G8 Countries. Int. J. Econ. Empir. Res. 2014, 2, 256–261. [Google Scholar]
- Raghupathi, V.; Raghupathi, W. Healthcare expenditure and economic performance: Insights from the United States data. Front. Public Health 2020, 8, 156. [Google Scholar] [CrossRef]
- Agénor, P.-R. Health and infrastructure in a model of endogenous growth. J. Macroecon. 2008, 30, 1407–1422. [Google Scholar] [CrossRef]
- Ke, X.; Saksena, P.; Holly, A. The Determinants of Health Expenditure: A Country-Level Panel Data Analysis; World Health Organization: Geneva, Switzerland, 2011; pp. 1–28. [Google Scholar]
- Ogundipe, M.A.; Lawal, N.A. Health expenditure and Nigerian economic growth. Eur. J. Econ. Financ. Adm. Sci. 2011, 30, 125–129. [Google Scholar]
- Aluko, O.O.; Adeniji, S. Exploring the effect of health on economic growth in Nigeria: A vector error correction model approach. Int. J. Econ. Commer. Manag. 2015, 3, 659–678. [Google Scholar]
- Odior, E.S.O. Government Expenditure on Health, Economic Growth and Long Waves in A CGE Micro-Simulation Analysis: The case of Nigeria. Eur. J. Econ. Financ. Adm. Sci. 2011, 3, 101–113. [Google Scholar]
- Lucian, U.; Oreste, S.; Traian, M.T.; Tudor, B.C. Relationship and causality between economic growth rate and certain diseases in the European Union. Ann. Fac. Econ. 2009, 1, 478–484. [Google Scholar]
- Onisanwa, I.D. The impact of health on economic growth in Nigeria. J. Econ. Sustain. Dev. 2014, 5, 159–166. [Google Scholar]
- Wang, F. More health expenditure, better economic performance? Empirical evidence from OECD countries. Inq. J. Health Care Organ. Provis. Financ. 2015, 52, 0046958015602666. [Google Scholar] [CrossRef]
- Aboubacar, B.; Xu, D. The impact of health expenditure on the economic growth in Sub-Saharan Africa. Theor. Econ. Lett. 2017, 7, 615–622. [Google Scholar] [CrossRef]
- Kurt, S. Government health expenditures and economic growth: A Feder-Ram approach for the case of Turkey. Int. J. Econ. Financ. Issues 2015, 5, 441–447. [Google Scholar]
- Piabuo, S.M.; Tieguhong, J.C. Health expenditure and economic growth-a review of the literature and an analysis between the economic community for central African states (CEMAC) and selected African countries. Health Econ. Rev. 2017, 7, 1–13. [Google Scholar] [CrossRef]
- Sethi, N.; Mohanty, S.; Das, A.; Sahoo, M. Health expenditure and economic growth nexus: Empirical evidence from South Asian countries. Glob. Bus. Rev. 2020, 0972150920963069. [Google Scholar] [CrossRef]
- Weil, D.N. A review of angus deaton’s the great escape: Health, wealth, and the origins of inequality. J. Econ. Lit. 2015, 53, 102–114. [Google Scholar] [CrossRef]
- Pauly, M.V.; Saxena, A. Health employment, medical spending, and long-term health reform. CESifo Econ. Stud. 2012, 58, 49–72. [Google Scholar] [CrossRef]
- Bank, W. Mortality Rate, Infant (Per 1000 Live Births); World Bank (WB): Washington, WA, USA, 2022. [Google Scholar]
- Bank, W. Maternal Mortality Ratio (Modeled Estimate, per 100,000 Live Births); World Bank (WB): Washington, WA, USA, 2022. [Google Scholar]
- Bank, W. Mortality Caused by Road Traffic Injury (per 100,000 Population); World Bank (WB): Washington, WA, USA, 2022. [Google Scholar]
- Cobb, C.W.; Douglas, P.H. A Theory of Production. Am. Econ. Rev. 1928, 18, 139–165. [Google Scholar]
- Ghedabna, L. The Relationship between Government Expenditure and Economic Growth in Algeria: An Empirical Study of the Period 1990–2012. Jordan J. Econ. Sci. 2014, 2, 71–84. [Google Scholar]
- Dickey, D.A.; Fuller, W.A. Likelihood ratio statistics for autoregressive time series with a unit root. Econometrica 1981, 49, 1057. [Google Scholar] [CrossRef]
- Phillips, P.C.; Perron, P. Testing for a unit root in time series regression. Biometrika 1988, 75, 335–346. [Google Scholar] [CrossRef]
- Enders, W. Applied Econometric Time Series, 2nd ed.; University of Alabama: Tuscaloosa, AL, USA, 2004. [Google Scholar]
- Johansen, S. Likelihood-Based Inference in Cointegrated Vector Autoregressive Models; OUP Oxford: Oxford, UK, 1995. [Google Scholar]
- Akaike, H. A new look at the statistical model identification. IEEE Trans. Autom. Control. 1974, 19, 716–723. [Google Scholar] [CrossRef]
- Schwarz, G. Estimating the dimension of a model. Ann. Stat. 1978, 6, 461–464. [Google Scholar] [CrossRef]
- Hannan, E.J.; Quinn, B.G. The determination of the order of an autoregression. J. R. Stat. Soc. Ser. B 1979, 41, 190–195. [Google Scholar] [CrossRef]
- Lütkepohl, H. Introduction to Multiple Time Series Analysis; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Akaike, H. Power Spectrum Estimation through Autoregressive Model Fitting. Ann. Inst. Stat. Math. 1969, 21, 407–419. [Google Scholar] [CrossRef]
- Goldkamp, J. Cointegration for Time Series Analysis. Anal. Vidhya. 10 February 2020. Available online: https://medium.com/analytics-vidhya/cointegration-for-time-series-analysis-1d0a758a20f1 (accessed on 12 January 2023).
- Granger, C.W. Investigating causal relations by econometric models and cross-spectral methods. Econom. J. Econom. Soc. 1969, 37, 424–438. [Google Scholar] [CrossRef]
- Granger, C. Some recent development in a concept of causality. J. Econ. 1988, 39, 199–211. [Google Scholar] [CrossRef]
- Gujarati, D.N. Essentials of Econometrics; SAGE Publications: Thousand Oaks, CA, USA, 2021. [Google Scholar]
- Engle, R.F.; Granger, C.W.J. Co-integration and error correction: Representation, estimation, and testing. Econom. J. Econom. Soc. 1987, 55, 251–276. [Google Scholar] [CrossRef]
- Fraser, J.; Sidebotham, P.; Frederick, J.; Covington, T.; A Mitchell, E. Learning from child death review in the USA, England, Australia, and New Zealand. Lancet 2014, 384, 894–903. [Google Scholar] [CrossRef]
- Gaigbe-Togbe, V.; Bassarsky, L.; Gu, D.; Spoorenberg, T.; Zeifman, L. World Population Prospects 2022; Department of Economic and Social Affairs, Population Division: New York, NY, USA, 2022. [Google Scholar]
- Klobodu, S.; Dawson, J.; Reed, D.; Carpio, C. Do maternal and child health promote economic development? A case study of six sub-Saharan African countries. Afr. J. Food Agric. Nutr. Dev. 2018, 18, 13761–13775. [Google Scholar] [CrossRef]
- Lawal, N.; Osinusi, K.; Bisiriyu, S. Maternal Mortality, Child Mortality, Life Expectancy and Economic Growth: The Nigerian Experience. Jalingo J. Soc. Manag. Sci. 2020, 3, 19. [Google Scholar]
- Ogunjimi, J. Health Expenditure, Health Outcomes and Economic Growth in Nigeria. Health Outcomes and Economic Growth in Nigeria. Asian J. Econ. Empir. Res. 2019, 6, 130–139. [Google Scholar] [CrossRef]
- DeNicola, E.; Aburizaize, O.S.; Siddique, A.; Khwaja, H.; Carpenter, D.O. Road traffic injury as a major public health issue in the Kingdom of Saudi Arabia: A review. Front. Public Health 2016, 4, 215. [Google Scholar] [CrossRef]
- Islam, M.; Alharthi, M.; Alam, M. The impacts of climate change on road traffic accidents in Saudi Arabia. Climate 2019, 7, 103. [Google Scholar] [CrossRef]
- Ghaffar, U.B.; Ahmed, S. A review of road traffic accident in Saudi Arabia: The neglected epidemic. Indian J. Forensic Community Med. 2015, 2, 242. [Google Scholar] [CrossRef]
- Part, D. Highway Safety Manual; American Association of State Highway and Transportation Officials: Washington, WA, USA, 2010; p. 19192. [Google Scholar]
- Isreal, A.I.O.; Kaliappan, S.R.; Hamzah, H.Z. Impact of health capital on total factor productivity in Singapore. J. Ekon. Malays. 2019, 53, 83–98. [Google Scholar]
- Razmi, M.J.; Abbasian, E.; Mohammadi, S. Investigating the effect of government health expenditure on HDI in Iran. J. Knowl. Manag. Econ. Inf. Technol. 2012, 2, 1–8. [Google Scholar]
- Pelizza, L.; Leuci, E.; Landi, G.; Maestri, D.; Paulillo, G.; Ceroni, P.; Soncini, C.; Daolio, M.C.; Quattrone, E.; Pellegrini, P. Personal Health Budget as a new rehabilitation model for severe mental illness within a caring community: An Italian evaluation study of beneficial effects. Aust. N. Z. J. Psychiatry 2020, 55, 602–612. [Google Scholar] [CrossRef]
- Erçelik, G. The relationship between health expenditure and economic growth in Turkey from 1980 to 2015. J. Politics Econ. Manag. 2018, 1, 1–8. [Google Scholar]
- Qehaja, S.S.; Qehaja, D.; Hoti, A.; Marovci, E. The relationship between government health expenditure and economic growth: Evidence from western Balkan countries. Int. J. Appl. Econ. Financ. Account. 2023, 15, 10–20. [Google Scholar] [CrossRef]
- Rana, R.H.; Alam, K.; Gow, J. Health expenditure and gross domestic product: Causality analysis by income level. Int. J. Health Econ. Manag. 2019, 20, 55–77. [Google Scholar] [CrossRef]
- Rahman, M. Causal relationship among education expenditure, health expenditure and GDP: A case study for Bangladesh. Int. J. Econ. Finance 2011, 3, 149. [Google Scholar] [CrossRef]
- Halıcı-Tülüce, N.S.; Doğan, İ.; Dumrul, C. Is income relevant for health expenditure and economic growth nexus? Int. J. Health Econ. Manag. 2016, 16, 23–49. [Google Scholar] [CrossRef]
| Variables | Descriptions | Data Sources |
|---|---|---|
| Gross domestic product growth (GDPG) | GDP per capita is the gross domestic product divided by the midyear population. GDP is the sum of the gross value added by all resident producers in the economy plus any product taxes and minus any subsidies not included in the value of the products. It is calculated without making deductions for the depreciation of fabricated assets or for the depletion and degradation of natural resources. Data are in current U.S. dollars. | [6] |
| Healthcare expenditure (HCE) | Current expenditures on health per capita in current US dollars. Estimates of current health expenditures include healthcare goods and services consumed each year. | [6] |
| Infant mortality rate (IMR) | The mortality rate is the number of infants dying before reaching one year of age per 1000 live births in a given year. | [71] |
| Maternal mortality ratio (MMR) | The mortality ratio is the number of women who die from pregnancy-related causes while pregnant or within 42 days of pregnancy termination per 100,000 live births. The data are estimated with a regression model using information on the proportion of maternal deaths among non-AIDS deaths in women ages 15–49, fertility, birth attendants, and GDP measured using purchasing power parities (PPPs). | [72] |
| Road traffic mortality rate (RTM) | Mortality caused by road traffic injuries is estimated by road traffic fatal injury deaths per 100,000 populations. | [73] |
| Variables | Median | Minimum | Maximum | Skewness | Kurtosis | Jarque-Bera | Prob. | ||
|---|---|---|---|---|---|---|---|---|---|
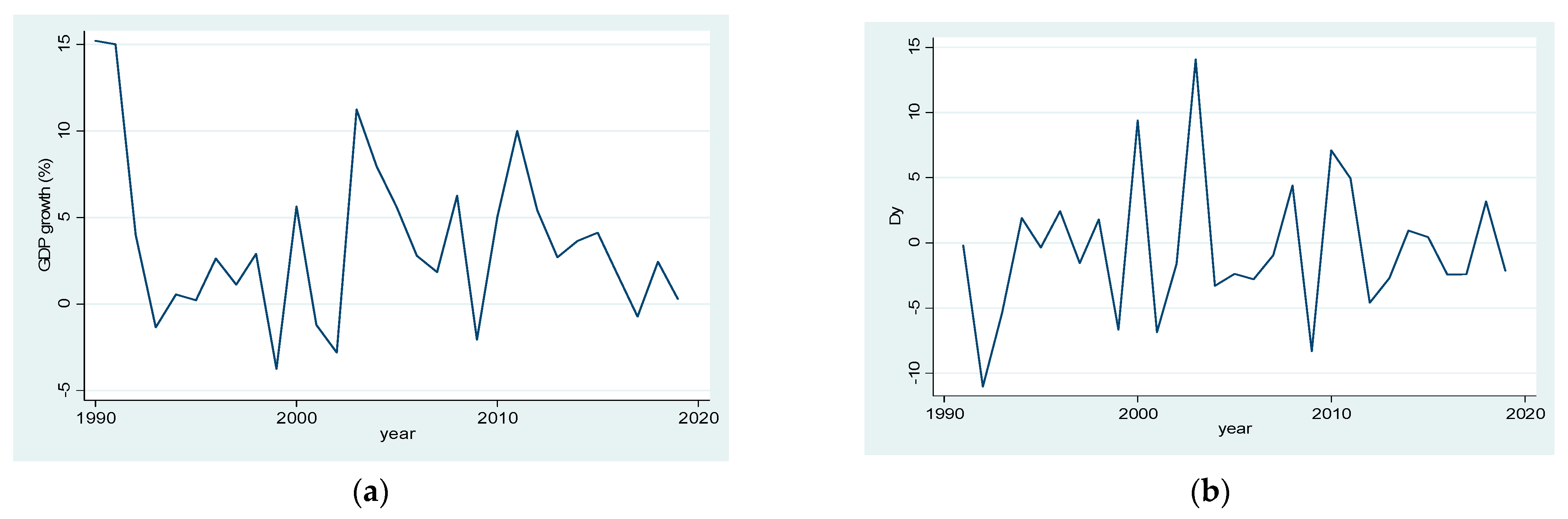
| GDPG | 30 | 3.541 ± 4.72 | 2.744 | −3.76 | 15.19 | 0.899 | 3.497 | 4.344 | 0.114 |
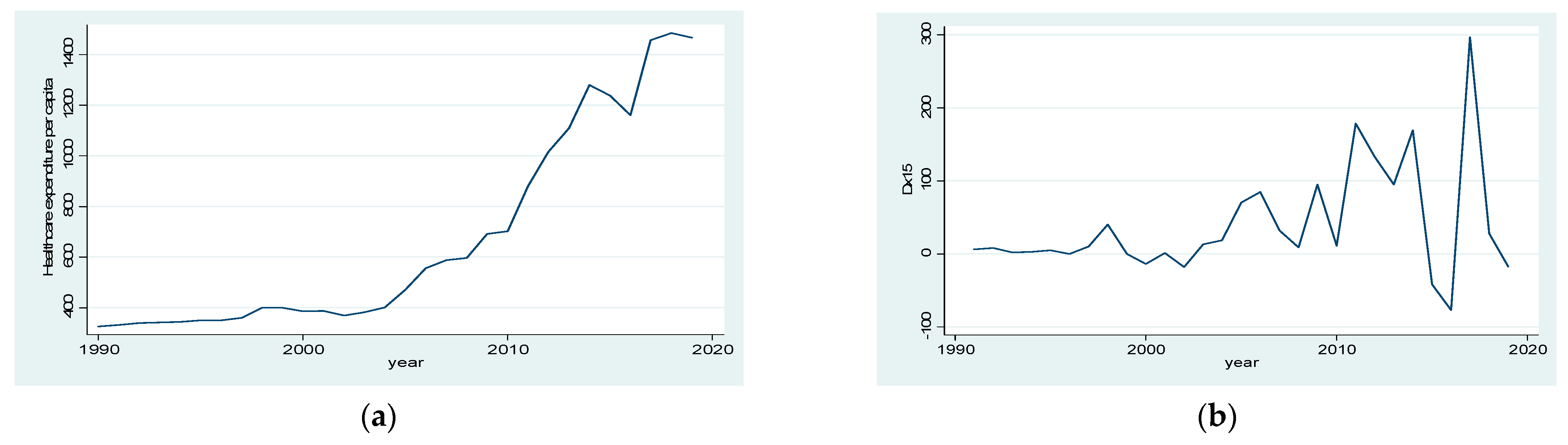
| HCE | 30 | 672.25 ± 401.74 | 435.998 | 326.00 | 1484.59 | 0.929 | 2.329 | 4.88 | 0.0872 |
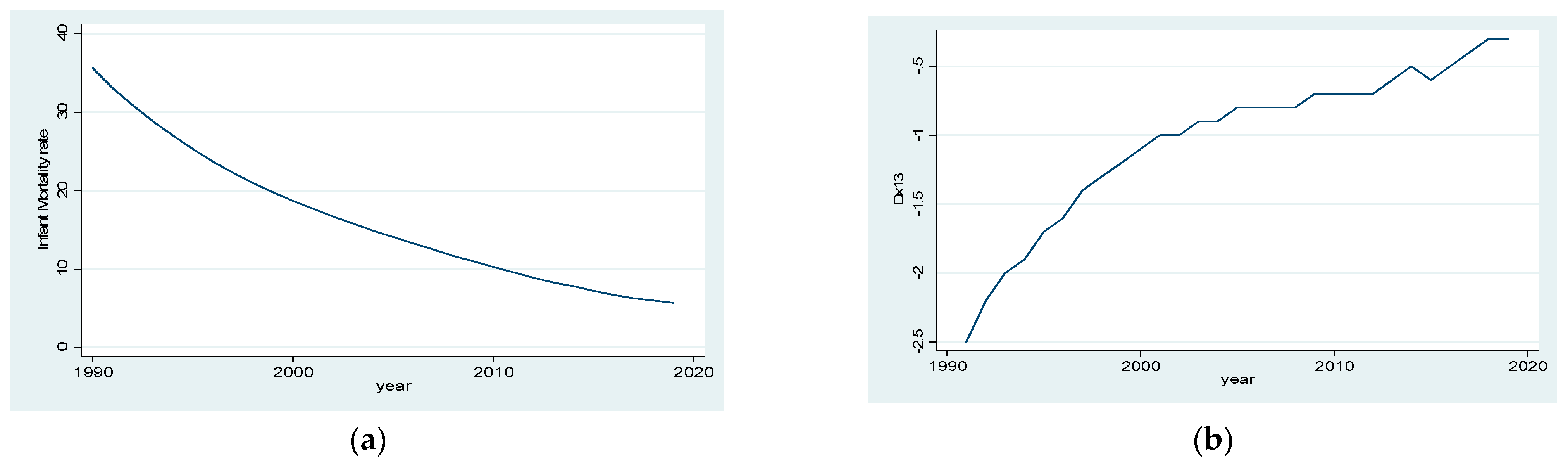
| IMR | 30 | 16.36 ± 8.71 | 14.500 | 5.70 | 35.60 | 0.641 | 2.338 | 2.602 | 0.2723 |
| MMR | 30 | 24.15 ± 7.73 | 22.000 | 16.80 | 46.00 | 1.233 | 3.704 | 8.217 | 0.0164 |
| RTM | 30 | 22.24 ± 5.82 | 23.400 | 16.10 | 35.90 | 0.503 | 2.226 | 2.016 | 0.365 |
| Variables | 1990 | 2019 | Changes (%) |
|---|---|---|---|
| Gross domestic product growth (GDPG) | 15.1934 | 0.300 | −98.0255 |
| Healthcare expenditure (HCE) | 326.00 | 1466.80 | 349.9387 |
| Infant mortality rate (IMR) | 35.60 | 5.70 | −83.9888 |
| Maternal mortality ratio (MMR) | 46.00 | 16.80 | −63.4783 |
| Road traffic mortality rate (RTM) | 16.00 | 35.90 | 124.375 |
| Variables | At Level | At First Difference | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ADF | Prob. a | PP | Prob. a | Decision | ADF | Prob. a | PP | Prob. a | Decision | |
| GDPG | −4.402 | 0.0017 | −4.405 | 0.0017 | I(0) | −5.803 | 0.0001 | −7.274 | 0.0000 | I(1) |
| HCE | 1.193 | 0.9973 | 1.629 | 0.9992 | −0.627 | 0.0455 | −5.035439 | 0.0003 | I(1) | |
| IMR | −4.821 | 0.0009 | −16.820 | 0.0001 | I(0) | −5.436 | 0.0001 | −5.918913 | 0.0000 | I(1) |
| MMR | −2.983 | 0.0493 | −9.576 | 0.0000 | I(0) | −3.699 | 0.0100 | −5.596931 | 0.0001 | I(1) |
| RTM | 1.120 | 0.9967 | 0.796 | 0.9922 | −3.348 | 0.0220 | −3.348 | 0.0220 | I(1) | |
| Lag | LogL | LR | FPE | AIC | SC | HQ |
|---|---|---|---|---|---|---|
| 0 | −436.2063 | NA | 1.07 × 108 | 32.68195 | 32.92192 | 32.75330 |
| 1 | −252.7657 | 285.3521 | 892.4079 | 20.94561 | 22.38542 | 21.37374 |
| 2 | −227.8634 | 29.51386 | 1112.504 | 20.95284 | 23.59251 | 21.73775 |
| 3 | −169.8234 | 47.29183 * | 182.4814 * | 18.50544 * | 22.34495 * | 19.64712 * |
| Hypothesis | Eigenvalue | Trace Statistics | 0.05 Critical Value | Prob. a | Max-Eigen Statistics | 0.05 Critical Value | Prob. a |
|---|---|---|---|---|---|---|---|
| None * | 0.999859 | 358.9761 | 69.81889 | 0.0001 | 230.5754 | 33.87687 | 0.0001 |
| At most 1 * | 0.905974 | 128.4006 | 47.85613 | 0.0000 | 61.46879 | 27.58434 | 0.0000 |
| At most 2 * | 0.723651 | 66.93186 | 29.79707 | 0.0000 | 33.43839 | 21.13162 | 0.0006 |
| At most 3 * | 0.514572 | 33.49347 | 15.49471 | 0.0000 | 18.79086 | 14.26460 | 0.0090 |
| At most 4 * | 0.431915 | 14.70261 | 3.841466 | 0.0001 | 14.70261 | 3.841466 | 0.0001 |
| Cointegrating Equation: | Co-Efficients |
|---|---|
| GDPG(−1) | 1.000000 |
| IMR(−1) | 3.667891 [10.2649] |
| MMR(−1) | −0.408164 [−1.29368] |
| HCE(−1) | 0.016317 [12.3420] |
| RTM(−1) | 0.711331 [4.26702] |
| Constant | −76.66228 |
| Error Correction | Δ(GDPG) | Δ(IMR) | Δ(MMR) | Δ(HCE) | Δ(RTM) |
|---|---|---|---|---|---|
| Cointegration equation | −1.540225 (0.39155) [−3.93369] | −0.003702 (0.00718) [−0.51525] | 0.240182 (0.08459) [2.83938] | −16.20806 (8.72106) [−1.85850] | 0.252136 (0.16557) [1.52281] |
| Δ(GDPG(−1)) | 0.237060 (0.24785) [0.95647] | −0.000529 (0.00455) [−0.11623] | −0.148580 (0.05355) [−2.77484] | 7.241893 (5.52044) [1.31183] | −0.033821 (0.10481) [−0.32270] |
| Δ(GDPG(−2)) | −0.246046 (0.15614) [−1.57580] | −0.000289 (0.00287) [−0.10096] | −0.092157 (0.03373) [−2.73202] | −0.272160 (3.47775) [−0.07826] | −0.001615 (0.06603) [−0.02447] |
| Δ(IMR(−1)) | −12.56020 (14.1171) [−0.88972] | 0.824344 (0.25903) [3.18237] | −4.318597 (3.04984) [−1.41601] | 173.3437 (314.434) [0.55129] | 6.612241 (5.96964) [1.10764] |
| Δ(IMR(−2)) | −34.80565 (16.9289) [−2.05599] | −0.011618 (0.31063) [−0.03740] | 13.43568 (3.65731) [3.67365] | −523.8543 (377.063) [−1.38930] | 2.028268 (7.15868) [0.28333] |
| Δ(MMR(−1)) | 0.051208 (0.87227) [0.05871] | −0.024452 (0.01601) [−1.52775] | −0.165098 (0.18844) [−0.87611] | −37.19748 (19.4283) [−1.91460] | 0.329417 (0.36885) [0.89308] |
| Δ(MMR(−2)) | −0.480208 (0.88821) [−0.54065] | 0.003150 (0.01630) [0.19326] | −0.041692 (0.19189) [−0.21727] | −20.31339 (19.7834) [−1.02679] | 0.181386 (0.37560) [0.48293] |
| Δ(HCE(−1)) | 0.031130 (0.01242) [2.50632] | −3.25 × 10−5 (0.00023) [−0.14247] | −0.003400 (0.00268) [−1.26718] | −0.030118 (0.27665) [−0.10887] | −0.002438 (0.00525) [−0.46415] |
| Δ(HCE(−2)) | 0.022837 (0.01382) [1.65296] | 6.23 × 10−5 (0.00025) [0.24561] | −0.009932 (0.00298) [−3.32775] | 0.071061 (0.30772) [0.23092] | −0.008281 (0.00584) [−1.41747] |
| Δ(RTM(−1)) | 2.060809 (0.72841) [2.82919] | 0.014707 (0.01337) [1.10033] | −0.250197 (0.15737) [−1.58991] | 30.97105 (16.2241) [1.90895] | 0.077495 (0.30802) [0.25159] |
| Δ(RTM(−2)) | −0.350043 (0.66747) [−0.52443] | 0.005031 (0.01225) [0.41082] | −0.150864 (0.14420) [−1.04622] | 19.62198 (14.8668) [1.31985] | −0.561913 (0.28225) [−1.99083] |
| C | −54.42331 (14.7353) [−3.69340] | −0.149121 (0.27038) [−0.55153] | 9.993350 (3.18340) [3.13920] | −434.1424 (328.204) [−1.32278] | 10.72452 (6.23107) [1.72114] |
| R2 | 0.734468 | 0.989232 | 0.723306 | 0.458886 | 0.471737 |
| Log likelihood (LL): −211.8849 Akaike information criterion (AIC): 20.50999 Schwarz criterion (SC): 23.62960 | |||||
| Null Hypothesis | Observations | F-Statistic | Prob. | Decision | Direction of Causality |
|---|---|---|---|---|---|
| IMR does not Granger Cause GDPG | 27 | 0.96736 | 0.4275 | Accept | None |
| GDPG does not Granger Cause IMR | 0.35266 | 0.7877 | Accept | None | |
| MMR does not Granger Cause GDPY | 27 | 0.54904 | 0.6546 | Accept | None |
| GDPG does not Granger Cause MMR | 0.60092 | 0.6219 | Accept | None | |
| HCE does not Granger Cause GDPPG | 27 | 0.41099 | 0.7469 | Accept | None |
| GDPG does not Granger Cause HCE | 1.44223 | 0.2603 | Accept | None | |
| RTM does not Granger Cause GDPG | 27 | 0.78972 | 0.5138 | Accept | None |
| GDPG does not Granger Cause RTM | 1.04253 | 0.3953 | Accept | None | |
| MMR does not Granger Cause IMR | 27 | 1.06395 | 0.3866 | Accept | None |
| IMR does not Granger Cause MMR | 0.56913 | 0.6418 | Accept | None | |
| HCE does not Granger Cause IMR | 27 | 1.44118 | 0.2605 | Accept | None |
| IMR does not Granger Cause HCE | 7.51008 | 0.0015 ** | Reject | IMR to HCE | |
| RTM does not Granger Cause IMR | 27 | 1.57923 | 0.2257 | Accept | None |
| IMR does not Granger Cause RTM | 1.07094 | 0.3838 | Accept | None | |
| HCE does not Granger Cause MMR | 27 | 0.40361 | 0.7520 | Accept | None |
| MMR does not Granger Cause HCE | 1.35554 | 0.2849 | Accept | None | |
| RTM does not Granger Cause MMR | 27 | 0.32052 | 0.8104 | Accept | None |
| MMR does not Granger Cause RTM | 0.39244 | 0.7598 | Accept | None | |
| RTM does not Granger Cause HCE | 27 | 2.70998 | 0.0724 * | Reject | RTM to HCE |
| HCE does not Granger Cause RTM | 0.95854 | 0.4315 | Accept | None |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Islam, M.M.; Mondal, M.N.I.; Khoj, H. Effects of Health Factors on GDP Growth: Empirical Evidence from Saudi Arabia. Sustainability 2023, 15, 8732. https://doi.org/10.3390/su15118732
Islam MM, Mondal MNI, Khoj H. Effects of Health Factors on GDP Growth: Empirical Evidence from Saudi Arabia. Sustainability. 2023; 15(11):8732. https://doi.org/10.3390/su15118732
Chicago/Turabian StyleIslam, Mohammad Mazharul, Mohammad Nazrul Islam Mondal, and Haitham Khoj. 2023. "Effects of Health Factors on GDP Growth: Empirical Evidence from Saudi Arabia" Sustainability 15, no. 11: 8732. https://doi.org/10.3390/su15118732
APA StyleIslam, M. M., Mondal, M. N. I., & Khoj, H. (2023). Effects of Health Factors on GDP Growth: Empirical Evidence from Saudi Arabia. Sustainability, 15(11), 8732. https://doi.org/10.3390/su15118732






