Abstract
The concept of resilience has been used extensively across the sciences in engineering and the humanities. It is applied to ecology, medicine, economics, and psychology. The novel coronavirus disease (COVID-19) has posed an extraordinary challenge to the resilience of healthcare systems, communities, and nations and has profoundly altered our previous day-to-day operations. This paper presents a discussion of the definitions and characteristics of resilient systems. Scenarios are utilized to qualitatively explore key relationships, responses, and paths for recovery across different system types. The purpose is to develop an integrated approach that can accommodate simultaneous threats to system resilience, in particular, impacts from a natural hazard in conjunction with COVID-19. This manuscript is the first to advocate for more in-depth and quantitative research utilizing transdisciplinary approaches that can accommodate considerations across our built environment and healthcare system infrastructures in pursuit of designing systems that are resilient to both natural hazards and pandemic impacts.
1. Introduction
Resilience is defined, in general terms, as the capacity of a system, community, or society potentially exposed to hazards to adapt, by resisting or changing in order to reach and maintain an acceptable level of function and structure [1,2,3]. This could be in response to a natural hazard (e.g., earthquake or flood), a human-made threat (e.g., cyber-attack or terrorism), or a biological hazard (e.g., pandemic). Presidential Policy Directive 21 [4] defines the term resilience as “a structure’s ability to prepare for and adapt to changing conditions while simultaneously being able to withstand and recover rapidly from functionality disruptions”. Hazards have the potential to cause significant disruption to the functions provided by the built environment and healthcare systems if they are not capable of adapting to or resisting the impacts of the hazards.
The concept of resilience has evolved across diverse fields, including ecological systems [1], psychology [5], environmental science [6], and other social sciences [7], as well as applied to the design and operations of the built environment [8]. Multiple publications discuss how to increase the resilience of structures, infrastructure systems, and communities to natural hazards, climate change [9], earthquakes [10], and floods [11]. However, there are only a few documented pandemic-resilient communities [12,13,14]. In addition, some researchers have discussed various intervention scenarios to reduce the pandemic risk, and thus, increase the resilience of the society [15,16].
In December 2019, the novel coronavirus, known as COVID-19, emerged from Wuhan, China [17] and resulted in a global pandemic. COVID-19 is a zoonotic disease [18,19] with a low to moderate mortality rate when compared to other deadly contagions, such as Ebola. Person-to-person transmission may occur through aerosolized droplets or direct contact [20], and, therefore, interventions such as isolation and contact tracing are essential to controlling COVID-19 outbreaks. However, the probability of successfully controlling an outbreak typically decreases as the number of initial cases increases [21].
COVID-19 surprised many nations and demonstrated a lack of preparedness and willingness to act quickly in order to prevent adverse impacts across many sectors and systems. However, prominent public figures provide evidence that such an outbreak was predictable. In December 2014, President Barack Obama warned that the U.S. needed to prepare for an upcoming https://www.youtube.com/watch?v=w50tZonOgoU, accessed on 30 May 2020 pandemic (President George W. Bush https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1283304/, accessed on 30 May 2020 and Bill Gates https://www.npr.org/sections/coronavirus-live-updates/2020/04/09/831174885/bill-gates-who-has-warned-about-pandemics-for-years-on-the-response-so-far, accessed on 30 May 2020 were also concerned about a pandemic):
“There may and likely will come a time in which we have both an airborne disease that is deadly, and in order for us to deal with that effectively, we have to put in place an infrastructure - not just here at home, but globally - that allows us to see it quickly, isolate it quickly, respond to it quickly, so that if and when a new strain of flu like the Spanish flu crops up five years from now or a decade from now, we’ve made the investment and we’re further along to be able to catch it”.
The occurrence of a pandemic has been anticipated among public health and medical officials for some time [22,23]. Similarly, projections for future natural hazards, including climate change [24], and “the big one” (i.e., a large earthquake in the Pacific Northwest) [25] have been key topics among environmental and climate science, geology, and engineering professionals for many years. The Sendai Framework for Disaster Risk Reduction (SFDRR) 2015–2030 [26] recognizes the connection between health risks and hazards, including those that are geophysical, hydrological, climatological, and meteorological [27], but it does not distinguish how biological hazards are similar or different from natural hazards. There have been some attempts to understand the interrelationships between the pandemic and the built environment or climate change [28,29,30]. In this paper, the authors build upon this work to better conceptualize and visualize implications of the intersection of geo-, hydro- and climatological hazards and an infectious disease outbreak.
This paper provides a review of similarities and differences of the concept of resilience to natural hazards (conventionally used for assets of the built environment) and pandemics (conventionally used for healthcare systems [31]). It proposes an integrated approach that can help bridge the two and encourage transdisciplinary efforts towards an integrated systems design approach to address the co-occurrence of both types of hazards. The importance of such a transdisciplinary study has been addressed already [32]. The objective of this paper is not to present modeling or simulation results, but instead provide insights on how those working at the intersection of natural hazards and pandemics can identify and express unique research questions. More generic bibliometric analyses of the publications on risk and resilience on COVID-19 was reported by Merad [33].
Section 2 summarizes recent worldwide experiences of natural hazards and pandemics. The underlying theories relevant to conventional multi-hazard resilience are reviewed in Section 3. Section 4 reviews the literature on the relationship between resilience and pandemics. A proposal for a unified resilience approach that addresses the co-occurrence of a natural hazard and a pandemic, and their potential interactions, is presented in Section 5. Finally, Section 6 identifies the limitations of this study and provides recommendations for research questions in this area.
2. Worldwide Experience on Natural Hazards and Pandemic
2.1. Comparison of Historical Natural Hazard and Pandemic Mortality Statistics
Since the focus of this paper is multi-hazard resilience during a pandemic, it is important to examine the relative impacts of natural and biological hazards on loss of life. Figure 1 provides the distribution of human losses due to disasters worldwide over the period 1989–2019. The data is normalized by millions of people to allow for comparisons across different countries.
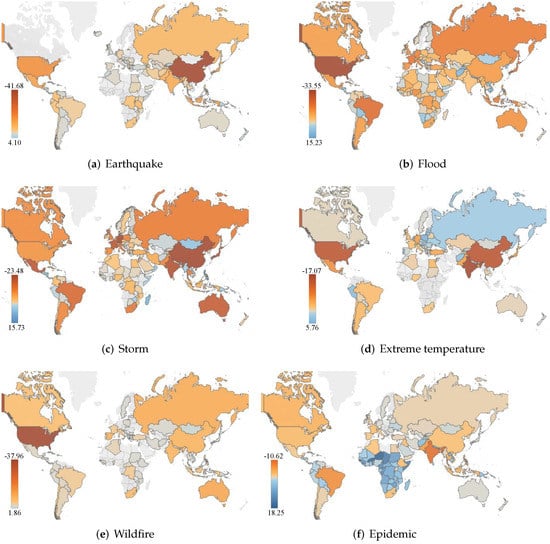
Figure 1.
Average number of deaths normalized per million people during 1989–2019 worldwide, data are in base-10 logarithmic scale (blue shows more deaths); data source from EM-DAT (International Disaster Database) and visualized by A. Martinez.
2.2. Recent Natural Hazards in the COVID-19 Era
Since January 2020, when the COVID-19 outbreak was initially identified, several national and domestic natural hazard events have been reported. The National Oceanic and Atmospheric Administration (NOAA) reported 2020 as a record breaking year, with 22 independent weather-related events, each causing at least USD 1B in damage in the US alone. Some of these events are briefly reviewed in this section. The reported events are among those for which hazard intensity was significant (e.g., exceeded design level event), a large amount of the population was affected in the region where the event took place, there was a considerable loss to the built environment, and/or those for which the co-occurrence of the pandemic and natural hazard was qualitatively or quantitatively evaluated by other researchers.
- Cyclones/Hurricanes:
- –
- Between 1–6 April 2020, the Southwest Pacific Ocean islands (i.e., Solomon Islands, Vanuatu, Fiji, Tonga) were hit by tropical cyclone Harold [34]. In Sanma (Vanuatu), about 85% of the population lost their homes, and 20% of healthcare facilities were damaged. At the time Harold hit Vanuatu, it was Category 5. Harold impacted the Solomon Islands with devastating winds accompanied by heavy rains, river flooding, very rough seas, high ocean waves, and coastal flooding, including storm surge. About 59,000 people were affected, with 27 people reported missing at sea. Harold hit Fiji as a Category 4 on the night of 7 April. More than 1541 were sheltered across 52 evacuation centers as of 14 April. Social gathering restrictions and other COVID-19 protocols remained in force. In Tonga, significant damage to the water supply and food crops were reported.
- –
- Tropical Storm Amanda, the first of the Eastern Pacific Ocean hurricane season, formed on Sunday 31 May 2020 along the coast of Guatemala and quickly moved inland. According to USAToday, it killed at least 17 people in El Salvador and Guatemala, where heavy rains produced flooding and landslides. A World Food Program (WFP) rapid food security assessment in El Salvador estimated that over 336,000 people could be pushed into severe food insecurity. WFP also requested USD 19 million to support the government of El Salvador in its response to COVID-19.
- –
- On 2 June 2020, tropical storm Cristobal formed off the coast of Mexico, and moved towards Texas, Louisiana, and the Florida Panhandle. Cristobal moved over southeastern Louisiana on 7 June, and impacted southern Wisconsin by 10 June. The governor of Texas announced that the COVID-19 pandemic and tropical storm Cristobal combined for a unique challenge. He encouraged local officials to adopt evacuation strategies that take into account COVID-19; for example, (1) using more vehicles for evacuations to allow for more spacing between people, or (2) using hotels for the displaced population instead of convention center-type settings. Frausto-Martínez et al. [35] tracked the potential interaction of tropical storm Cristobal in the Western Yucatan Peninsula, Mexico with an increase in the number of COVID-19 positive cases. A numerical analysis was first conducted to identify the tropical storm’s extreme characteristics. Second, an analysis was performed using the reported flooding and rainfall information. Third, data on the confirmed positive cases of COVID-19 was post-processed. They reported no direct evidence for an increase in number of infectious cases in 10 out of 11 municipal areas. However, in one case, there was a sudden increase in the number of positive cases.
- –
- On 22 August 2020, tropical storm Laura brought heavy rainfall to Haiti and the Dominican Republic (with some locations recording about 300 mm of rain in one day). At least 11 fatalities have been reported. Several rivers broke their banks, and several floods were reported in Greater Santo Domingo. Civil Protection urged residents near the Artibonite River to evacuate their homes after flood gates of the Peligre Dam were opened [36]. The Haiti government placed an overnight curfew in an effort to stem the spread of COVID-19. The effects of Hurricane Laura in the United States were also destructive. It made landfall in Louisiana on August 27 as a Category 4 hurricane and caused around USD 17.5 billion damage and 33 fatalities. State emergencies were declared in Louisiana and Mississippi, and the Louisiana Department of Health tweeted “If evacuating: In addition to standard supplies like adequate meds and pet supplies, be sure to include items that help protect you and others from COVID-19 in your go kit, such as hand sanitizer with at least 60% alcohol, soap, disinfectant wipes and 2 masks for each person”. Laura caused disruption to testing centers, as well as disruption of water supplies. Non-congregate sheltering was recommended due to high rates of community spread. Shelters for evacuees were opened with cots set farther apart to maintain social distancing. Moreover, disrupted evacuations put many at shelter-in-place at risk from natural hazards. A number of agencies, including FEMA, pulled back their typical field response due to the pandemic, which may hamper relief efforts and delay distribution of post-disaster financial assistance.
- –
- On 16 September 2020, Hurricane Sally made its way inland, and killed at least one person in Alabama, U.S. According to the National Weather Service (NWS), the storm dumped ~760 mm and 630 mm of rain in Alabama and Florida, respectively. Nearly 500,000 homes and businesses lost power. Hurricane Sally put a pause on COVID-19 testing, because the sites were shut down for a week [36].
- –
- On 17 and 18 September 2020, cyclone Ianos (also known as Medicane Ianos) impacted Greece. It caused severe damage to the structures and infrastructures comprising health facilities including health centers and hospitals. Flooding was reported in several cities, resulting in four fatalities. Mavroulis et al. [37] tracked the number of affected people for one week before and three weeks after the event for 16 regional units of Greece. They reported 16%, 21% and 83% increase in the number of positive cases in three successive weeks after Medicane Ianos compared to a week before event.
- Droughts:
- –
- According to Mishra et al. [38], the co-occurrence of drought and the COVID-19 pandemic occurred across many countries to different degrees. The western U.S., southeastern Australia, southeast Asia, and south America, Africa, and Europe experienced both hazards. Populations at-risk were similar for drought and COVID-19 (e.g., older adults, those with lower socioeconomic status, those with pre-existing conditions, migrant workers, etc.). The COVID-19 outbreak limited access of millions of people to clean water. It increased the hardship of those in the farming sector to sell their produce. Moreover, COVID-19 disrupted food distribution and demand. Several reports have been published about the potential interaction of COVID-19 and drought, for example, in Zimbabwe (See FEWS NET), U.S., Italy (See The-Local), and others. In Madagascar, three years of drought combined with COVID-19 and brought the people to crisis point. According to WaterAid, nearly half of the 25 million people who live in Madagascar already had no access to clean water, and a staggering three-quarters lived in poverty.
- Earthquakes:
- –
- On 21 March 2020, a magnitude 5.6 earthquake hit west-central Epirus [39]. Mavroulis et al. [37] post-processed publicly-available data on the daily reported laboratory-confirmed COVID-19 number of cases in Greece and correlated them with the Epirus earthquake. They concluded that the impact of this earthquake on the pandemic evolution in northwestern Greece was negligible (only 2 out of 5 positive cases during the post-earthquake period could be attributed to this event).
- –
- On 22 March 2020, a magnitude 5.3 earthquake hit the city of Zagreb, Croatia [40]. This resulted in one fatality, 27 injured, ~6200 damaged buildings, and over 1900 buildings becoming uninhabitable. COVID-19 testing was disrupted for hours in hospitals. The earthquake caused widespread unrest, causing people to leave their homes and compromising social distancing measures [41]. Svetina et al. [42] proposed a resilience framework with a case study of earthquake in Zagreb during pandemic.
- –
- On 7 May 2020, an early morning magnitude 5.1 earthquake hit Tehran, Iran. At least two people died and about 38 were injured, but no other major damage was observed. According to Reuters, officials urged people to observe mandated social distancing measures to prevent the spread of COVID-19, even as some slept outdoors for fear of aftershocks.
- –
- On 30 October 2020, a magnitude 6.9 earthquake struck the eastern part of Greece and the western part of Turkey (the epicenter was located in the northern Samos Island) [43]. A total of 119 deaths and over 1030 injuries were reported in both Turkey and Samos Island, nearly all of them due to partial or total collapse of structures and the subsequent tsunami. By comparing the number of positive cases pre- and post-earthquake, [37] concluded that the impact of the Samos earthquake on COVID-19 in the eastern part of Greece was low (with only 12 reported positive cases compared to a previous 7 cases).
- Floods:
- –
- On 1 May 2020, after a long rainy week, part of an earth-fill dam broke along the Sardoba Reservoir in Uzbekistan, leading to flooding. Four people died, ~50 were injured, and 70,000 were evacuated from 22 villages. The reservoir was 29 m deep and completed in 2017 (capacity 922 Mm) [44]. While there is no solid information on the regional COVID-19 spread, the number of fatalities does not show any change (only one death is reported) for three weeks after the dam break in the whole of Uzbekistan (based on WHO data). At the time of the dam break, Uzbekistan was at the initial stage of virus spread (the main peak started mid-June) and therefore, there was no significant connection observed between flooding and pandemic. It is noteworthy that in the highly affected regions, the mass movement due to dam failure may increase the spread of virus.
- –
- On 19 May 2020, following heavy rains, the Edenville Dam was breached, and the Sanford Dam downstream overflowed, causing a major flood in Midland County, Michigan, United States. Sanford Dam is an 11 m concrete dam completed in 1925 (capacity of 18.5 Mm). Edenville Dam is a 16.5 m earthfill dam completed in 1924 (capacity of 81.6 Mm). Both dams are categorized as high hazards by the National Inventory of Dams [45]. These dam failures forced the evacuation of 11,000 people, including patients in the Midland Hospital. It was fortunate that both dams had emergency action plans (EAPs) in place. An EAP is a document that identifies (1) potential incidents around the dam, (2) the affected areas by the less of reservoir, and (3) pre-planned actions to be followed to minimize loss of life and property damage.
- –
- Several weeks of torrential monsoon rains during June and July 2020 caused flooding and landslides in Bangladesh, Bhutan, India, and Nepal, and killed over 700 people. According to UNICEF, over 4 million children were estimated to be impacted and in urgent need of life-saving support. The COVID-19 pandemic made the situation complicated as the number of positive cases accelerated in some of the affected areas.
- –
- On 9 August 2020, a large amount of rain (300 mm within 8 h) was recorded in Steni station and intense lightning activity was reported in Evia Island, Greece. Several rivers overflowed their banks, and the flooding caused eight fatalities and extensive damage to buildings and infrastructure [46], water supply, and electricity networks. There were water and electricity shut-offs in several villages. While the flooding occurred in the beginning of the second wave of the pandemic in Greece, tracking the number of COVID-19 positive cases one week before and three weeks after the event showed no relation between the pandemic and flooding [37].
- Tornado:
- –
- Between 12 and 13 April of 2020, dozens of tornadoes impacted a number of southeastern United States. Homes were obliterated and 36 fatalities were reported. Many had to move to shelters, which were attempting to implement social distancing and other COVID-19 precautions, and some were turned away due to a shortage of face masks [47].
- Wildfire:
- –
- Since 21 March 2020, more than 374 wildfires were reported through the forests in Iran’s Zagros Mountains. Wildfires raged across five provinces and burned more than 50,000 hectares of forests [48].
- –
- Lightning strikes in August 2020 sparked a number of fires in western U.S. states, notably California, Oregon, and Washington. Warm temperatures and dry conditions fueled additional fires. These wildfires expanded quickly, resulting in more than 40 deaths, destroying more than 7000 structures, scorching more than five million acres across the three states, and forcing tens of thousands of residents to evacuate [49]. The wildfires caused significant air quality degradation, contributing to hazardous conditions that may have adverse effects for those infected with, recovering from, or vulnerable to COVID-19.
- –
- Between 12 and 20 October of 2020, multiple fall wildfires occurred in Colorado, including near major population centers like Fort Collins, Boulder, and Estes Park (as reported by inciweb). This led to evacuation orders for thousands of residents, raising concerns about COVID-19 transmission, especially when an outbreak was reported at a Colorado Springs fire station in El Paso County.
- Extreme weather:
- –
- In February of 2021, a series of winter storms brought significant amounts of sleet and ice, as well as subfreezing temperatures, across the southern United States [50]. The storms resulted in vast power outages in Texas, largely attributed to a failure to winterize the Texas electric grid [51]. At the peak of the outages, nearly 4.5 million Texas homes and businesses were without power. Dozens of Texans filed lawsuits against the Electric Reliability Council of Texas (ERCOT) and local power companies. In addition to the devastating impacts on millions of residents and businesses, the power outages impacted recovering COVID-19 patients at home who were dependent on plug-in breathing machines and portable oxygen tanks [52]. The lack of reliable oxygen, in combination with extreme cold at home, forced many patients to return to already overwhelmed hospitals. Moreover, dangerous travel conditions, distribution delays, and the power outages resulted in vaccine delays [53]. As of 31 March 2021, the power outages resulted in 3123 vaccine doses being wasted [54].
3. Resilience to Natural Hazards
Resilience can be a broad and general concept, or it can be domain-specific, and applied at various levels to physical, ecological, and social systems. Improving resilience to natural hazard events, such as hurricanes, earthquakes, and hazards affected by climate change, such as extreme heat and drought, requires the operationalization of resilience across all three of these systems. This involves coordinated efforts across multiple fields of expertise ranging from geoscience (to understand hazards and their impacts) to risk and emergency communications (informing people and promoting behavioral change). Acknowledging other literature that provides a more comprehensive classification of resilience categories and typologies, such as Davidson et al. [55], the focus here is on identifying core concepts across three resilience domains: components of the built environment (e.g., structures and infrastructure systems), socio-ecological systems adaptation (e.g., environment and society), and holistic community planning (e.g., ability to withstand perturbations). The purpose of this discussion is to provide an overview of several key features of resilience across domains that are relevant to understanding impacts from natural hazards and pandemics and important for discussion in later sections of this paper.
3.1. Resilience of Structures and Infrastructure Systems
Resilience for structures and infrastructure systems subjected to extreme events has been studied by many researchers, among them [56,57,58,59,60,61]. A general conceptual representation of resilience for structures or infrastructure systems is illustrated in Figure 2 [62]. This figure shows a system’s regular performance and expected rate of degradation (i.e., aging) over time until an incident (e.g., a natural hazard) occurs. The event degrades the performance of the system (i.e., damage or failure), and the figure shows five alternate recovery trajectories to a performance state that can range from “worse than the original aged state” to “better than new”. This graphical representation actually shows the loss of resilience of the system as a relationship of functionality (or serviceability) over time after an impact occurs and the system is recovered [58]. Defining these relationships this way, the often described “resilience triangle” [3], enables the quantification and numerical analysis of a system, the system’s components, and their recovery. This approach describes different recovery paths (e.g., exponential, sigmoid) depending upon the system conditions and repair and recovery interventions.
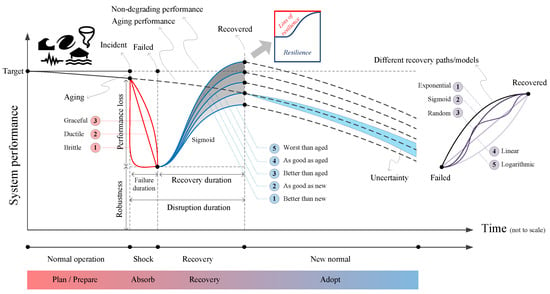
Figure 2.
Concept of resilience of the built environment to natural hazards.
Ayyub [63] defines resilience metrics for use in modeling hazard impacts and recovery that enable operationalization of abstract notions of resilience and their measurement. Two key areas of the resilience triangle illustrate where efforts can be placed to achieve higher levels of resilience for structures and infrastructure systems. The first is to improve the anticipated performance of an asset, such as a building, to the hazard. In Figure 2, this is exemplified by alternate paths for performance loss: brittle, ductile, and graceful. These three terms describe the performance states of buildings when subjected to an earthquake. A brittle building may crumble easily while a building that is designed to be more flexible has the ability to withstand some level of earthquake shaking. Achieving more robust performance requires planning and design at the time a structure is built, and later retrofitted. An alternative approach is to focus on speeding repairs to structures and lifeline systems after a hazard event occurs, to enable quicker return to function. To perform the needed repairs, multiple elements are required, such as: (1) budget, (2) crew, (3) material and equipment, (4) expertise, and (5) stakeholder approval. The availability and accessibility of these elements are key to resilience in the recovery process.
Decision-making processes related to strengthening or speeding repairs to structures and infrastructure systems is complex and involves the weighing of priorities and identification of factors that may constrain resilience planning. These priorities and factors include those described in Bruneau et al. [3], which categorizes eleven aspects of resilience into three groups: (1) the desired results from the resilience effort, (2) the properties of each resilience project, and (3) the dimensions of resilience decision making [58].
- Three desired results:
- –
- More reliable: since it has a lower probability of reaching limit states.
- –
- Fast recovery: the rapidity of functionality restoration during a disaster is paramount to resilient systems.
- –
- Low socio-economic consequences: the reduced probability of significant service reductions and fast recovery decreases the impact of extreme events on a society.
- Four properties:
- –
- Robustness: the ability to withstand a given extreme event and still deliver a service.
- –
- Rapidity: the speed with which a structure recovers from such an event to reach a high functionality level.
- –
- Redundancy: the extent to which components of the system are substitutable.
- –
- Resourcefulness: the capacity to make the appropriate budget available, identify problems, establish priorities, and mobilize resources after an extreme event.
- Four dimensions:
- –
- Technical: includes all the technological aspects associated with construction.
- –
- Organizational: includes all the management activities and plans, maintenance, and response to emergencies.
- –
- Social: includes societal effects and impacts of mitigation actions.
- –
- Economic: includes all the direct and indirect costs due to the loss of functionality and the subsequent restoration.
Improving the resilience of structural or infrastructure systems constitutes an integral part of its risk management [64]. For a given structure or infrastructure system, engineers, architects, and other designers can identify an appropriate performance target or may have one set for them by codes and standards. These specifications delineate the hazard type and performance level required. Modeling of structural and infrastructure systems enables the quantification of their performance. This allows for scenario analyses to examine consequences of the intensity of the hazard impact, the ability of the system to withstand impacts, changes to recovery time, and an examination of estimated costs of alternative solutions. Current practice for addressing natural hazards through building design focuses on life safety by reducing the likelihood of significant damage or structural collapse. This life safety objective may be less focused on fast recovery and lowering socio-economic consequences of damage or failure at a societal level [65,66].
There are multiple efforts ongoing to enable community-level planning that increases the capacity of the built environment to provide services and maintain functionality through and after natural hazard events. These are discussed in Section 3.3.
3.2. Resilience of Socio-Ecological Systems
The concept of the socio-ecological system (SES) has evolved from earlier work to study and understand ecological systems. The conceptual framing of an SES can be particularly useful to understand the interactions between individuals and groups and the elements of the built environment and natural environment. SES can be defined at a range of spatial scales and may include a mix of natural, technological, and social systems. For example, one can view a small town and its surrounding agricultural fields as a SES, or apply the concept to an entire watershed, including all developed and natural areas. Holling [1] first applied resilience theory to ecological systems. Instead of focusing on a rigid state of equilibrium within an ecological system, Holling [1] shifted focus to describe the ability of systems to absorb change and for relationships to persist across the system [67,68,69,70]. This influenced conceptualization of the natural environment, but it also changed thinking about complex systems that include humans-in-nature, called socio-ecological systems [71]. Within an SES, these complex systems can be both rigid and adaptive, recognizing their ability to evolve into new states or collapse. In relation to the built environment and the ability of individuals and organizations within the system to respond to shocks or stressors, an SES describes how individuals can respond to and direct the adaptation of a system’s state (e.g., improved engineering design) [67].
The concept of an SES is particularly useful when examining or attempting to describe how to influence various states of resilience of a community, organization, or institution, when they are under stress or shock caused by natural hazards or epidemics. Rather than focusing on specifically how to “bounce back” to an existing steady-state equilibrium (or status quo), influencing the resilience of an SES requires examining the overall system and the role and function of individual components of the system. Two approaches to describing the resilience of an SES include: (1) generalized resilience, which refers to the health of the overall system; and (2) specified resilience, which refers to the resilience of important system components [72]. Challenges have been observed when only focusing on one type of SES resilience, including difficulties characterizing system feedback interactions, emergent processes, non-linear dynamics, and uncertainty, which can cause unforeseen consequences [73].
This is an issue particularly relevant to COVID-19 impacts, as components of the built environment may have emergent properties that are not present in prior states of operation. Within the context of a SES, COVID-19 presents a unique set of stressors that may not be observed in other natural hazards. For example, stressors on parts of an SES, including individuals and elements of the built environment, take place over a different temporal scale than most natural hazards. The impacts of the event are related to both individual and group-level dynamics (e.g., adoption of mitigation measures), and social and economic factors, which greatly affect the ability of a system to function. SESs that are adaptive are able to absorb these changes and transition to a new operational state (or equilibrium). However, planning to ensure a system can adapt is challenging. Memory and existing knowledge can be detrimental for resilient outcomes in light of unexpected events, so socio-ecological research recommends that managers assist in the development of participatory processes that promote holistic systems perspectives to avoid rigid system design and configuration. With this approach, achieving system-level resilience requires not returning to an original system state, but rather transitioning to a new state. Resilience planning, described further in the next section, provides a structured process for enabling individuals and organizations to build resilience capacity by increasing adaptability and robustness of their systems.
3.3. Planning for Resilient Communities
Presidential Policy Directive 21 (PPD-21) (The White House, 2013) defines resilience as: “The ability to prepare for and adapt to changing conditions and to withstand and recover rapidly from disruptions. Resilience includes the ability to withstand and recover from deliberate attacks, accidents, or naturally occurring threats or incidents”. Planning for and adapting to natural hazards (e.g., earthquakes, floods, hurricanes, tornadoes) can help to reduce deaths and injuries, as well as other social and economic costs to communities [74]. For example, structural failure and damage can lead to interruption or complete disruption of building occupancy. Similarly, power, water, communications, or transportation network damage or failure can lead to serious deficiencies in these essential services. These kinds of impacts can have serious consequences in terms of the health and safety of community residents and can be difficult to repair or replace in the needed recovery timeframes. Of particular importance is access to and rapid restoration of clean running water, power, and essential facilities such as hospitals and other emergency service providers. Furthermore, cascading consequences over a longer term include business disruption and failure, food insecurity, and population out-migration [75,76,77].
A key concept of community resilience is interdependency among various systems including both human and environmental systems and the supporting built environment. The built environment (including both buildings and infrastructure systems) helps sustain basic human needs for water, food, and shelter. It also provides spaces and resources that enable social development and growth of individuals, families, and communities by enabling activities like education, healthcare, security, governance, and the functioning of the economy, among many others (See Thriving Together). Restoring key community functions and ensuring the continuity or resumption of social and economic activities is imperative to minimize disastrous consequences across communities affected by a natural hazard. To prevent these interruptions, actions taken to ensure the functionality of structures (residential, commercial, or industrial) and infrastructure systems (e.g., electric, water, transportation) can reduce adverse outcomes from natural hazards.
The National Institute of Standards and Technology (NIST) has created a practical and flexible planning guide, the NIST Community Resilience Planning Guide for Buildings and Infrastructure Systems (CRPG), that can help communities identify and develop actions that will enhance their resilience to natural (as well as other) hazards [78,79]. This six-step planning process for community resilience is shown in Figure 3 and revolves around establishing collaboratively determined performance goals that connect social functions of a community to pre-specified recovery time frames for the built environment. Via the CRPG, communities can decide which hazards are of greatest concern to them, articulate performance goals for their built environment to ensure restoration of social and economic functions, and prioritize solutions to achieve these goals. In addition, communities are urged to make resilience planning part of their routine activities, in order to revisit and revise their resilience needs as condition changes. The CRPG enables holistic community and resilience planning, which allows community leaders the ability to establish resilience goals, prioritize solutions based on the community’s social and economic functions, and more ably recover from hazard events.

Figure 3.
A six-step process for communities planning for enhanced resilience to natural and other hazards; adapted from [78]. Color spectrum corresponds to evolution of different planning stages.
4. Pandemic-Centered Resilience
The application of the resilience concept across sectors increased as the COVID-19 pandemic continued. Many articles address aspects of medical resilience [80,81,82], mental health resilience [83,84,85,86], tourism resilience [87], food system resilience [88,89], supply chain resilience [90,91,92], educational system resilience [93], socioeconomic resilience [94,95,96,97], risk, hazard, and uncertainty science [98,99,100,101,102,103,104], and welfare resilience [105]. All provide valuable information, but our approach will build knowledge on cross-sector resilience thinking.
Putting the concept of resilience within a broader context, as applied to aspects and phases of pandemic progression, is an essential task. Figure 4 illustrates the World Health Organization’s (WHO) “Continuum of Pandemic Phases”, as a distribution curve of the hypothetical global average of pandemic cases over time.
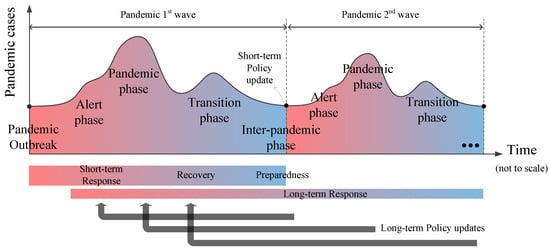
Figure 4.
Representation of pandemic phases in the context of emergency management plan; adopted and modified from [106]. Color spectrum red-to-blue corresponds to starting and ending point of individual phase (or in the case of long-term response, the entire pandemic occurrence).
The four phases include: alert, pandemic, transition, and inter-pandemic. These phases overlap with three risk assessment stages: preparedness, response, and recovery. The alert phase refers to when a novel pathogen has been identified in humans. The pandemic phase corresponds to a period of global spread of the disease. The inter-pandemic transition phase is the time between pandemics. Pandemics come in multiple waves. Since each pandemic has unique characteristics, the policy approach applied to one pandemic cannot necessarily be generalized. At various stages, policies and protocols will likely need revision to reflect new information and minimize negative consequences. The iterative requirement of pandemic recovery planning is a key characteristic of event progression where community and system resilience can be taken into account. Through the long-term recovery of a pandemic, it is important to minimize the loss of functionality in healthcare system through operational and design changes, and ensure continual updating of protocols informed by “lessons learned” to improve outcomes [12,21,107,108,109,110,111,112].
While “resilience” in the context of a pandemic often prioritizes long-term benefits (e.g., reduced mortality), this perspective may sometimes conflict with short-term efficiency and profitability objectives [113]. Response to pandemics should therefore incorporate short-term and long-term considerations to address emerging risks to individuals and institutions. In the short-term, healthcare decision-makers should seek to address the immediate concerns (e.g., identify the affected groups, provides basic needs for the affected population), and in the long-term, develop and revise effective guidelines and treatments based on new scientific findings and lessons learned. COVID-19 is a multi-pronged hazard causing demonstrated disruptions to: (1) public health systems, (2) socioeconomic activity, (3) global trade, and (4) sometimes even political challenges. A pandemic-resilient system should effectively incorporate all aspects of human life and manage trade-offs between efficiency and resilience of various system components. Decisions to ensure continuous performance of systems should be considered by provisioning extra resources and introducing redundancy into the system. For a systematic risk (such as the COVID-19 pandemic), the International Risk Governance Center (IRGC) [114] provides a seven-step guide to mitigate risks and reduce consequences; see Figure 5. A sample application of these guidelines on a disease epidemic can be found in Massaro et al. [115].
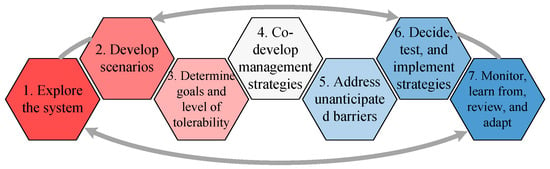
Figure 5.
Seven steps recommended by International Risk Governance Center [114] to handle the complex systemic risks. Color variation means that not all these steps will happen at a same level. A semi-linear trend shows the flexible sequence and the inherent nonlinearity. Arrows present the interaction among all steps.
This paper utilizes the concept of resilience to assess the healthcare system, including components that support medical functions to respond to the COVID-19 outbreak [116]. This includes, (a) physical structures (e.g., hospitals, out-patient facilities) and infrastructure systems (e.g., power [117] and water); (b) sufficient equipment, supplies, treatments, and medicines; (c) resources for communication and transportation where needed; and (d) qualified and proficient staff at all levels.
A healthcare system is considered to be resilient if it can provide patients with sufficient and timely treatment that minimizes deaths, injuries, and sickness—ideally to the maximum extent possible. This description of a healthcare system’s generalized resilience can be delineated into two specified resilience components: (1) the demand for healthcare services (this component is particularly critical because the demand can rapidly increase during a pandemic), and (2) the capacity of the healthcare system to provide patients with adequate treatment. Together, these two components can be used to describe the capacity of the healthcare system to meet demand.
Figure 6 illustrates the application of the concept of resilience for a healthcare system. When compared to Figure 2, the resilience models have notable similarities and differences. First of all, the vertical axis is the “level of demand satisfied” in the pandemic application, measured as the percentage of the demand that receives medical treatment from the healthcare system. In Figure 2, the vertical axis is a system’s performance under the natural hazard setting, which implies that for the healthcare system, we measure the performance as the level of demand satisfied and that emergency managers have the goal of achieving 100% performance so that all patients receive adequate and timely medical treatment.
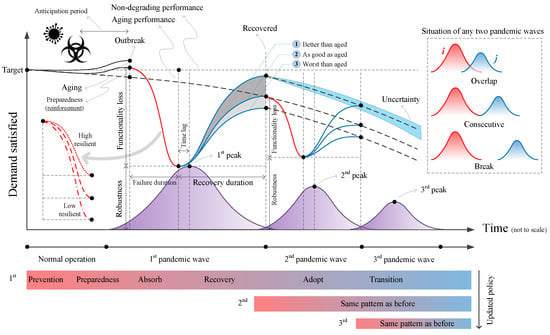
Figure 6.
Concept of resilience to pandemic. It shows three hypothetical pandemic phases and two recovery phases. Color bar variation presents the evolution pandemic occurrence similar to Figure 2. Icons on the top left illustrate pandemic/epidemic.
As in Figure 2, the baseline is a measure of the system working normally to provide its standard pre-pandemic or pre-hazard services. Ideally, the existing healthcare system capacity would be meeting 100% of the demand when functioning effectively. For example, the hospital system may have sufficient supplies of mechanical ventilators to treat the regular flow of patients with chronic respiratory diseases in an entire city. A pandemic is usually associated with a period of anticipation, unlike some natural hazards. Depending on the infectious disease outbreak’s location and propagation speed, the healthcare system can reinforce itself (i.e., become prepared) to satisfy the forthcoming demand surge, thus increasing capacity before the disease significantly impacts a region.
If key medical resources are not sufficiently stockpiled or cannot be acquired through alternative means, the level (percentage) of demand satisfied can rapidly decrease as an outbreak spreads, due to the rise in the number of patients requiring treatment. For pandemics, the rise in demand is rapid and overwhelming as a result of its exponential growth. Thus, it can quickly exceed the existing capacity of the healthcare system [118,119,120,121]. For example, during COVID-19, shortages of mechanical ventilators, oxygen tanks, effective drugs and medication, and medical personnel were reported worldwide [122,123,124,125]. Patients who cannot receive timely treatment due to these shortages can rapidly deteriorate and face a higher mortality risk.
Moreover, we must consider several pandemic scenarios to adequately plan for healthcare system resilience. The time at which the level of demand reaches its minimum value may or may not precisely match the pandemic peak, and there might be a time lag. Next, the system starts to recover, and usually, the recovery duration takes until the end, or after, the pandemic. Depending on the available resources, the recovered system can be better, worse, or as good as the system without a pandemic outbreak. Depending on the level of demand satisfied throughout the disease’s spread, the healthcare system can be categorized as a high-, normal- or low-resilience system.
Pandemics, including COVID-19, have been described as affecting populations in multiple waves (i.e., resurgence of pandemic). The second wave of the Spanish flu pandemic in 1918–1920 was particularly devastating in the United States and Europe. Tracking variation of the daily confirmed COVID-19 cases in different countries shows that some experienced a third COVID-19 wave (e.g., United States and Canada), some had four waves (e.g., Japan) and some may experience a fifth (e.g., Iran). Therefore, one can categorize multiple pandemic waves depending on the situation of the daily transmission graphs as shown in the top right corner of Figure 6:
- They might highly overlap (e.g., Iran COVID-19 confirmed cases);
- They may just touch each other (e.g., Italy, Spain, and Japan COVID-19 confirmed cases);
- There might be a gap/break between waves (e.g., Spanish flu pandemic).
The third case is clearly more favorable for the healthcare systems as they will recover more efficiently. Figure 6 also shows the second and third waves of the pandemic and the associated reductions in level of demand satisfied and potential recovery scenarios. Cross-referencing this figure with Figure 4, it is clear that the phases “recovery” and “adopt” for wave is based on the information and experience gained from previous waves, . Finally, one should not forget the presence of uncertainty during all steps, from preparedness to recovery and adopt [99].
One of the most effective methods to reduce the number of infected people, the number of deaths, and increase the healthcare system’s resilience is to flatten the transmission curves, as illustrated in Figure 7. In this scenario, the curve’s peak value is compressed, and subsequently, its arrival time is delayed. The initial reduction in the demand satisfied is less steep and allows emergency managers more time for the system to recover from the surge of initial patients. Another reason to flatten the transmission curve is to give scientists more time to find a treatment or cure (e.g., vaccine) for COVID-19. Moreover, each country’s healthcare system has a specific capacity (e.g., ICU rooms, ventilators) and cannot provide sufficient service if the capacity is significantly exceeded during pandemics. Therefore, the flattened transmission curves can help to unload an overwhelmed healthcare system, and alter demands so their peak is equal or smaller than the healthcare system’s capacity. If the level of demand met in the system reaches a critical lower level, the system may not recover at all [116]. The pandemic curves can be flattened by increasing the testing centers, contact tracing, non-pharmaceutical interventions (NPIs) such as face masks, more strict social distancing, and finally accelerating the public vaccination.
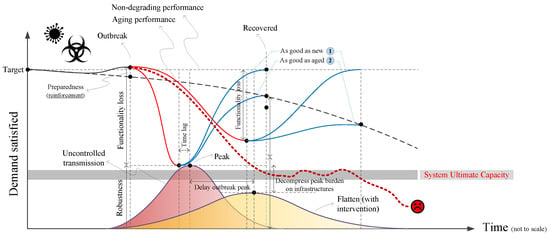
Figure 7.
Concept of healthcare system resilience under pandemic. Icons on the top left illustrate pandemic/epidemic. Two pandemic phases (narrow and wide) with corresponding recovery paths are shown. Each recovery can upgrade the system performance to either aging or non-degrading situations. System’s ultimate capacity presents a threshold for failure.
Finally, we must acknowledge a number of related considerations. It is important to note that the concept of resilience during a pandemic is not limited to the demand met by the healthcare system, yet this is among the most important elements. Other social, economic, industrial, and political factors should also be considered. Figure 8 schematically presents the multi-target performance loss in three key elements which affect the daily life of community members: healthcare, social, and economic activities. For each of those three, a hypothetical resilience curve is plotted for controlled and uncontrolled transmission cases. While flattening the curve has benefits in decreasing mortality and increasing the resilience of the healthcare system, it does have potential adverse impacts on social and economic systems. Longer stay-at-home orders can increase the rate of unemployment (for example, the U.S. unemployment rate increased to about 14% during April and May 2020 (from 4% in March), and reduced to about 8% again as of August 2020). Moreover, the impacts of interventions such as lockdowns tend to be widespread as they propagate through the supply chain [126,127]. According to Djalante et al. [128], the economic fallout from COVID-19 may exceed the 2008–2009 recession [128]. According to the IMF’s April 2021 World Economic Outlook, the global economy contracted by 3.5% in 2020, and the impacts are likely to persist for several years, especially in emerging and developing countries.
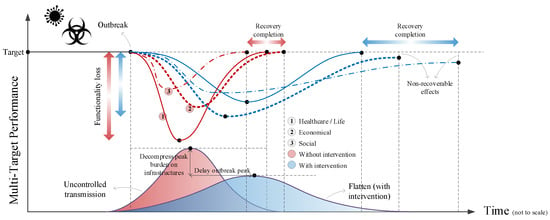
Figure 8.
Concept of intervention in multi-target resilience to pandemic. Icons on the top left illustrate pandemic/epidemic. Two pandemic phases (narrow and wide) with corresponding recovery paths are shown. Three recovery objectives of life, economy, and social are shown for each case. This figure also illustrates the uncertainty in recovery compilation conditioned on objectives.
Mental health [129] is an important concern during pandemic outbreaks, and has close ties to the availability and function of social activities. Restrictive public health measures may have adverse effects on individuals with existing mental health disorders or create new stress-related disruptions. This may adversely affect individual responses to a natural hazard, and their decisions during a pandemic [130]. Such public health measures may have negative consequences for other elements of social health and physical health [131]. For instance, Ravindran and Shah [132] document how social distancing measures due to COVID-19 in India have coincided with a “shadow pandemic” of increased domestic violence. In addition, pandemic impacts are unlikely to be distributed equally across a population, and will potentially exacerbate existing economic and social inequities [133,134,135].
Finally, in some cases, it may be possible that the performance of the considered system will never, or within a reasonable time frame, fully recover from hazard impacts. Natural hazards have been shown to result in permanent out-migration at the county-level [136] and in long-term declines in incomes at the national level [137]. According to Jordà et al. [138], while the short-run impacts of pandemics are similar to the impacts of other economic disasters such as natural hazard events, the medium- and long-term impacts are very different, with significant macroeconomic declines persisting for decades. Moreover, the countries with the highest economic risk from both natural hazards and pandemics tend to be less affluent (e.g., countries in Sub-Saharan Africa, South Asia, and Central Asia) [139]. Notably, social cohesion has been shown to be a significant mitigating factor for reducing economic risk from natural hazards [140].
5. Perspectives into Resilience during Pandemic and Natural Hazard
Here, we raise the question: “What to do in the case of concurrence of pandemic with a natural hazard (i.e., combined multi-hazard situation)?” Before exploring this question more fully, note that the combined effects of a natural hazard and pandemic may be discussed in two different sequences:
- Natural hazard prior to pandemic: In this scenario, a natural hazard (e.g., flood, earthquake, or hurricane) occurs and affects the fundamentals of a healthcare system and consequently contributes to an outbreak. The 2004 South Asian tsunami, which hit sixteen countries and caused 250,000 fatalities, is an example of this dynamic [141]. The impacts of the tsunami contributed to factors leading to an acute respiratory infection outbreak in Indonesia [142]. In another case, a 2010 magnitude 7.0 earthquake in Haiti caused about 200,000 fatalities [143]. About nine months later, a cholera outbreak began to spread across the country, killing about 8000 people. Prior to the 2010 earthquake, no history of cholera in Haiti was reported. Other examples of pandemic after earthquake or flooding can be found in [144,145].
- Natural hazard during a pandemic: In this scenario, a design level natural hazard (e.g., flood, earthquake, and hurricane) occurs during an ongoing pandemic outbreak. This will have an adverse effect on capacity of the healthcare system. Examples of this scenario have been presented in Section 2.2 for the current COVID-19 outbreak. This case may even be worsen by sequential/cascading natural hazards during a pandemic. Two notable examples of compound hazards are post-earthquake fire [146] and flooding into nuclear power plants (e.g., in 2020, the Midland dam failure prompted an emergency notification at a nearby nuclear research reactor [147]).
While the first sequence was already discussed by multiple researchers [148,149,150], our paper highlights the second sequence: natural hazard during a pandemic. Spiegel et al. [151] studied all the large natural hazards, complex emergencies (CE), and epidemic events during the period 1995–2004. They reported that 63% of the largest CEs included more than one epidemic compared with 23% of the largest natural disasters. While natural hazards can have an acute onset (e.g., tsunamis and hurricanes), or slow onset (e.g., drought), the CEs are defined as a humanitarian crisis in a country, region, or society with total or considerable breakdown of authority resulting from internal or external conflict that requires an international response [152]. In CEs, mortality among the civilian population substantially increases above the population baseline mortality, either as a result of the direct effects of war, or indirectly through the increased prevalence of malnutrition and/or transmission of communicable diseases, especially if the latter result from deliberate political and military policies and strategies [153]. In addition, Hariri-Ardebili [154] discussed the impact of pandemics on recent CEs associated with protests (e.g., black lives matter).
Multiple concerns are associated with concurrently managing a natural hazard and a pandemic (the following examples are specific to COVID-19 but could be applied to any pandemic):
- Most importantly, an ongoing pandemic overloads the healthcare system and reduces the system’s ability to provide appropriate and timely emergency medical services and thus may increase fatalities due to the occurrence of a natural hazard.
- Filling up the remaining capacity of the healthcare system with victims from the natural hazard decreases the capacity to test for infectious disease, and can therefore contribute to an increase in transmission.
- At the same time, both the pandemic and the natural hazard may lead to a decline in elective medical services, with negative public health consequences as well consequences for healthcare providers [155].
- An improper response to a natural hazard may increase the spread of an infectious disease and ultimately fatalities [156]. Response activities without precautions such as distancing measures may spread the virus, and extreme measures taken to lessen virus disease consequences could lead to inadequate responses to natural hazard management, causing other negative effects [154]. For example, extreme caution in evacuating high-rise buildings after an earthquake may put occupants at greater risk from building failure.
- Mass evacuation and sheltering in communal centers, without appropriate face covering and social distancing, increases the spread of an infectious disease.
- Evacuation capacity may be limited, because the occupancies of emergency shelter facilities are reduced during a pandemic when compared to preexisting emergency plans [157].
- Those infected (or even those without proper infectious disease protections) might be turned away from important services due to fear of viral spread. For example, during the April 2020 tornado in Crossville, Alabama, a family was not allowed to stay at a tornado shelter because the they did not have enough face masks for every family member [47].
- Locally specific context of the multi-hazard scenario is also very important. According to Dincer and Gillanders [158], in communities with high corruption, observing the social distancing during sheltering and also implementation of the mitigation strategies is difficult. They used two primary measures for corruption, one based on corruption convictions and the other based on news stories related to corruption. A measure of compliance based on cell phone activity constructed by SafeGraph is also used. In order to evaluate the robustness of the adopted metrics, they also tested a new metric, the corruption reflections index (CRI), which uses corruption stories covered in Associated Press (AP) news wires, which are electronically available online via LexisNexis.
- Under the stress of a massive natural hazard, governments often rely on non-local aid (e.g., international help) to increase the capacity of the local healthcare system [159,160,161].
- During a pandemic, travel restrictions between and within countries drastically reduce international and non-local agencies’ ability to deploy medical teams to the most affected regions of the world.
Policies for emergency management during natural hazards and pandemics are different [162]. The risk assessment sequential phases (i.e., response, absorb, recovery, and adopt), as illustrated in Figure 2, are essentially linear in natural hazards. However, the response and recovery phases for pandemics are nonlinear [162], as shown in Figure 6.
Since the concept of resilience is applied differently to cases of natural hazard and pandemic, their combined impact should be studied from two different perspectives. In both scenarios, we assume that a natural hazard is coincident with a pandemic:
- In the first scenario, illustrated by Figure 9, the objective is to examine the resilience of the built environment under a natural hazard, and the way it is affected by presence of a pandemic.
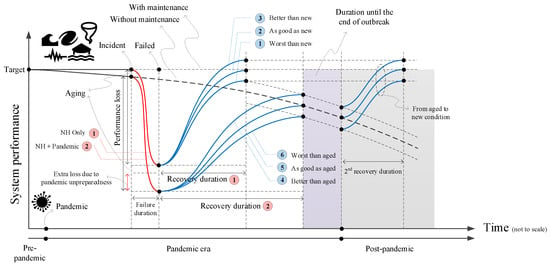 Figure 9. Concept of infrastructural resilience to natural hazards at the pandemic era. Icons on the top left illustrate different natural hazard. Icon on the bottom left illustrates pandemic. Two scenarios are compared (i.e., only natural hazard and pandemic plus natural hazard) with red lines. For each scenario, three recovery paths are assumed (blue lines).
Figure 9. Concept of infrastructural resilience to natural hazards at the pandemic era. Icons on the top left illustrate different natural hazard. Icon on the bottom left illustrates pandemic. Two scenarios are compared (i.e., only natural hazard and pandemic plus natural hazard) with red lines. For each scenario, three recovery paths are assumed (blue lines). - In the second scenario, illustrated by Figure 10, the objective is to focus on the resilience of healthcare systems during pandemic, and the way it may be affected by a sudden shock (i.e., a natural hazard).
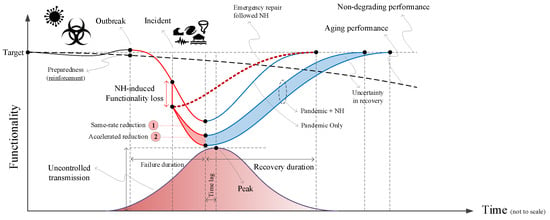 Figure 10. Concept of pandemic resilience with an external natural hazard. Icons on the top left illustrate pandemic/epidemic. Icons on the center illustrate different natural hazard. Vertical drop presents the natural hazard induced functionality loss.
Figure 10. Concept of pandemic resilience with an external natural hazard. Icons on the top left illustrate pandemic/epidemic. Icons on the center illustrate different natural hazard. Vertical drop presents the natural hazard induced functionality loss.
5.1. First Scenario: Resilience of Built-Environment Systems in a Natural Hazard and Pandemic
In Figure 9, two cases are compared: (1) natural hazard only (already discussed in Figure 2), and (2) natural hazard (NH) + pandemic. For the combined case, at the time of incident (i.e., a natural hazard), there might exist some performance loss (not because of the incident but due to lack of sufficient maintenance caused by the pandemic). After the incident (at the time of a theoretical failure), the overall performance loss for the NH + pandemic case can be higher than the NH only case. This is not only because of the initial aging effect, but also due to lack of preparedness during (and right after) the incident due to the ongoing pandemic, which limits the emergency response and limits the ability to prevent further compound impacts. For example, it may be possible to stop leakage of damaged oil reservoir tanks with enough crew in place. If not, the leak can cause compounding consequences (i.e., environmental pollution).
The next step is recovery from this adverse effect. Since the system performance loss is expected to be higher for the NH + pandemic case, time for recovery is expected to be greater than the NH only case. This becomes even more critical when we consider community-scale recovery. Three elements should be present during any repair/recovery activities, including: crew member availability, sufficient repair budget, and availability of material and equipment. A pandemic directly and negatively influences the ability to recover by adversely affecting the population levels through death, illness, and quarantine. A budget shortage is also a secondary consequence, which results from pandemic expenditures, business discontinuity, and transportation interruption. These secondary consequences may prohibit availability of sufficient repair budgets and accessibility of the materials and equipment required to perform necessary repairs. The pandemic also caused supply chain disruptions that drove up prices for materials due to shortages.
Finally, system operators (or community leaders) may decide to repair an affected system up to a below-normal performance level (because of the above-mentioned reasons) to provide basic services during a pandemic. However, full or complete recovery activities can be implemented later (for example, at the post-pandemic era or whenever a cure is found). The extra recovery duration is shown in Figure 9 via a second recovery period.
5.2. Second Scenario: Healthcare System Resilience in a Pandemic with Addition of Natural Hazard Shock
Now, we present the scenario in which natural hazards interrupt the functionality of a healthcare system during a pandemic; Figure 10. This figure is, in fact, the modified version of Figure 7 by incorporating a natural hazard that occurs some time before the pandemic reaches its peak. Clearly, any such intrusion causes a sudden functionality reduction in the system [163,164], which was experiencing overload due to pandemic impacts. One may note the sharp, nearly vertical nature of the NH-induced reduction in demand satisfied compared to the pandemic. This is due to the fact that the time scale in a natural hazard event is much faster than that of a pandemic. While COVID-19 took about two months to reach its first peak (from a nearly zero value), it may take a few minutes for an earthquake to cause damage (or a few days in the case of a hurricane or flooding).
The sudden loss of functionality across a critical system can lead to catastrophic outcomes due to reduced capacity; thus, planning for these potential scenarios should be incorporated within an effective emergency repair/recovery strategy. The emergency recovery will need extra resources (e.g., monetary interventions) to ensure the system’s safe operation during and after the pandemic. On the other hand, the community may decide to continue regular operations until they reach the pandemic’s peak. The rate of the reduction in the level of demand satisfied during this period might be equal to the non-NH case (recovery path 1 in Figure 10), or the loss of function may be accelerated (recovery path 2).
An accelerated reduction in demand satisfied is the likely outcome since demand increases while capacity decreases. This problem can be exacerbated if the NH causes an additional surge of patients. For example, large earthquakes can cause thousands of injured people to require medical treatment from the already overloaded system [165,166]. Moreover, an NH may reduce the capacity by disruption of power, water system, or built infrastructure. The pandemic+NH scenario’s recovery time is also longer than the non-NH case because the system is at its minimum robustness in the former case with multiple uncertainties and delays in recovery duration.
While Figure 10 discusses only one scenario for the natural hazard occurrence, there is large aleatory uncertainty (due to natural randomness in the process) in the time and space of the impacts and consequences of such hazard events. Typically, it is better for the system if a natural hazard occurs towards the end of the pandemic. Moreover, it is essential to note that if a devastating natural hazard occurs at the peak of the pandemic, the combined effect of reductions in functionality and the demand shock might trigger a total failure of the system with severe social consequences such as the permanent dislocation of a population. Perhaps most importantly, we should emphasize that all hybrid scenarios defined here utilize a single-wave pandemic, and that the importance of the subsequent pandemic waves should not be ignored or underestimated.
6. Conclusions and Future Direction
This paper discusses aspects of resilient systems that are important for mitigating negative outcomes and enhancing recovery after hazard and pandemic impacts. Detailed consideration of the potential interactions and interdependencies between pandemic and natural hazards is needed to improve resilience planning. The paper demonstrates how co-occurrence of natural hazards and pandemics can increase recovery time across the built environment and healthcare systems. In some cases, the systems may not recover pre-hazard functionality for an extended period. Two scenarios illustrate different dimensions of operationalized resilience: (1) resilience of built environment systems in a natural hazard and pandemic, and (2) healthcare system resilience in a pandemic under an acute natural hazard shock. A more holistic view is provided by simultaneous consideration of the hazards. Moreover, this perspective positions resilience across systems, as opposed to only within them. It is a first step towards more robust resilience planning to strengthen infrastructure across both the built environment and healthcare system. Key lessons learned from this effort that can be applied to future resilience planning include:
- The post-hazard performance and functionality of the built environment is dependent upon considerations of design, flow of materials, and operational requirements of restoration and maintenance; for example, whether materials, skilled personnel, and labor nearby are accessible to begin rapid repair.
- Economic impacts significantly affect the ability of local, state, and tribal governments to raise revenue that supports the operation, maintenance, and restoration of structures and infrastructure systems and other elements of the built environment. As the pandemic continues over time, potential accumulation of deferred maintenance activities could result in unexpected reductions in functionality under hazard conditions or some other unforeseen loading event.
- Economic impacts from both natural hazard events and pandemics can persist into the medium- and long-term, with the impacts of pandemics potentially persisting far longer than the impacts of natural hazards, for developed counties, depending on the magnitude of the event(s). For developing counties the impact from devastating natural hazards persists for decades.
- Combined social and economic impacts may shift expectation for demands on the built environment and expectations for restoration of functionality. The COVID-19 pandemic is a hazard event that has a long time horizon, requires dramatically different uses of some elements of the built environment, and may change how those elements function to serve the needs of occupants or users. Changes in regional or national cultural norms may also influence expectations for functionality and maintenance of systems.
- Disaster preparedness may help with response to a pandemic. For example, in a survey of small businesses, 23% of respondents that have implemented natural hazard planning in the past reported that such planning was helpful for coping with COVID-19 [167].
- Data availability and data analytics play an important role in increasing the resilience of society to natural hazards [168,169]. Therefore, exploring the capabilities and limitations of social networks is important as a potential tool to indirectly increase disaster preparedness. Multiple studies have been dedicated to investigating the role of the social network during the pandemic and its connection to a resilient society [170,171,172]. However, there is limited research that investigates the role of social media in the prevention and preparedness of events at the intersection of pandemic and natural hazards [173,174]. Eyre et al. [175] discussed the role of social media during the recovery stage from the pandemic (See Figure 4).
Additional research is needed to better assess how disaster resilience and pandemic resilience interact, and to ensure that these findings are useful for researchers and practitioners engaging across disciplines [176]. As a result of this paper, key questions for future research include:
- How can we effectively collect and use data associated with co-occurrence of pandemic and natural hazard (e.g., social media data) at the regional and national levels with minimum potential bias (due to the objective nature of multi-hazards)?
- How to quantify the imposed risk to critical infrastructures (i.e., healthcare, energy [177] and power, information and cyber-technology, transportation, communications, water and wastewater, nuclear reactors, dams, etc.) due to combined pandemic and natural hazards?
- How to prioritize the risk reduction elements on the structures and critical infrastructures under a multi-objective (e.g., health, social, economical) and multi-constraint (e.g., political) condition?
- How to make sure all the resilience-centered tasks on operating, maintaining, and repairing critical infrastructure will continue in a reliable way, while the majority of the crew work remotely?
- How to quantify the importance of redundancy in both personnel (if they become sick) and infrastructures (if they are damaged) and their interaction during the pandemic plus natural hazards.
- How can we quantify the uncertainties in the observed vs. expected societal impacts, which affect the resilience of the healthcare system in response to the pandemic and natural hazards?
- How do we map Bruneau et al.’s [3] aspects of resilience to the co-occurrence of a natural hazard and a pandemic? For instance, in terms of desired results, do we prioritize restoring functionality of the healthcare system at the expense of recovery of the transportation network?
- What are the losses to society from natural hazard-induced disruptions to testing and treatment of infected populations during a pandemic? For example, can we quantify the excess cases or deaths associated with the inability to test, trace, and treat due to a disruption to the built infrastructure? While a few small studies found no correlation between a natural hazard event and COVID-19 cases or deaths, it is difficult to draw conclusions without a deeper investigations into the counterfactual (e.g., through an event study).
- On the other hand, can we quantify the impact of a pandemic on response and recovery to an acute natural hazard, such as an earthquake or flood? For instance, some of the cases cited in this paper suggest the policy response to the COVID-19 pandemic presented challenges for evacuations. Can we quantify excess losses from natural hazards that are due to the pandemic? Are they negligible? Moreover, several studies have shown the effectiveness of GIS-based data in evacuation planning during natural hazards [178]. Similar studies have been conducted on evacuation and transportation during pandemic [179,180]. Rajabifard et al. [181] discussed the connection between pandemic, geospatial information, and community resilience. Therefore, we need to quantify how GIS-based data can be combined with information about infected populations to reduce the spread of the virus during natural hazard-induced evacuations [182,183,184].
- While most of this paper has focused on the co-occurrence of an acute natural hazard event (e.g., earthquake, hurricane) during a pandemic, it is also important to consider the intersection of chronic and persistent hazard events (e.g., drought, extreme weather) during a pandemic. For instance, extreme cold in February of 2021 led to a failure of the electric grid in Texas. How much of the failure was driven by the excess demand for power by people at home? On the other hand, if vaccines had not been available, how costly would this disruption have been to testing and treating patients? What are the different challenges of a chronic vs. acute hazard occurring during a pandemic?
- Much of natural hazard resilience focus to-date has addressed system failure and restoration, functionality, and independencies of a range of designed and engineered systems. The COVID-19 pandemic raises questions about how we reflect the simultaneous impacts of natural and pandemic hazards on social and economic systems in traditional planning and design approaches?
- How can the level of function or service of social and economic systems, which are disrupted by pandemic, social, or economic disruptions, be quantitively linked to the performance of elements of the built and natural environment?
- While this paper presented a unified framework to combine the natural hazards and pandemic, it is also important to quantify the impact of different types of natural hazards when they are combined with pandemic scenario. For example, an earthquake typically occurs without any prior warning in a short period of time (e.g., few minutes) [42]. However, a flood is typically predictable (except sudden dam break [185]) and may last for few hours to days [186]. This requires slightly different strategies to address the compound natural hazard-pandemic resilience scenario. A detailed discussion for hurricane-pandemic hazards can be found in [187,188].
Author Contributions
Conceptualization, M.A.H.-A., S.S. and K.J.; methodology, M.A.H.-A., S.S., K.J., C.C., J.F. and L.C. investigation, M.A.H.-A., S.S., K.J., C.C., J.F. and L.C.; writing—original draft preparation, M.A.H.-A.; writing—review and editing, M.A.H.-A., S.S., K.J., C.C., J.F. and L.C.; visualization, M.A.H.-A.; supervision, M.A.H.-A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Holling, C.S. Resilience and stability of ecological systems. Annu. Rev. Ecol. Syst. 1973, 4, 1–23. [Google Scholar] [CrossRef] [Green Version]
- Waller, M.A. Resilience in ecosystemic context: Evolution of the concept. Am. J. Orthopsychiatry 2001, 71, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Bruneau, M.; Chang, S.E.; Eguchi, R.T.; Lee, G.C.; O’Rourke, T.D.; Reinhorn, A.M.; Shinozuka, M.; Tierney, K.; Wallace, W.A.; Von Winterfeldt, D. A framework to quantitatively assess and enhance the seismic resilience of communities. Earthq. Spectra 2003, 19, 733–752. [Google Scholar] [CrossRef] [Green Version]
- Presidential Policy Directive 21. Presidential Policy Directive—Critical Infrastructure Security and Resilience. 2013. Available online: https://obamawhitehouse.archives.gov/the-press-office/2013/02/12/presidential-policy-directive-critical-infrastructure-security-and-resil (accessed on 30 January 2018).
- Johnson, J.L.; Wiechelt, S.A. Introduction to the special issue on resilience. Subst. Use Misuse 2004, 39, 657–670. [Google Scholar] [CrossRef]
- Van der Leeuw, S.E.; Aschan-Leygonie, C. A long-term perspective on resilience in socio-natural systems. In Micro-Meso-Macro: Addressing Complex Systems Couplings; World Scientific: London, UK, 2005; pp. 227–264. [Google Scholar]
- Magis, K. Community resilience: An indicator of social sustainability. Soc. Nat. Resour. 2010, 23, 401–416. [Google Scholar] [CrossRef]
- Labaka, L.; Hernantes, J.; Sarriegi, J.M. A holistic framework for building critical infrastructure resilience. Technol. Forecast. Soc. Chang. 2016, 103, 21–33. [Google Scholar] [CrossRef]
- Vallejo, L.; Mullan, M. Climate-Resilient Infrastructure: Getting the Policies Right. Environment Working Papers No. 121. 2017. Available online: https://dx.doi.org/10.1787/02f74d61-en (accessed on 14 February 2022).
- Nikolaou, S.; Kourkoulis, R.; Diaz-Fanas, G. Earthquake-Resilient Infrastructure: The Missing Link. In Geotechnical Earthquake Engineering and Soil Dynamics V: Seismic Hazard Analysis, Earthquake Ground Motions, and Regional-Scale Assessment; American Society of Civil Engineers: Reston, VA, USA, 2018; pp. 79–90. [Google Scholar]
- Lhomme, S.; Serre, D.; Diab, Y.; Laganier, R. Analyzing resilience of urban networks: A preliminary step towards more flood resilient cities. Nat. Hazards Earth Syst. Sci. 2013, 13, 221. [Google Scholar] [CrossRef] [Green Version]
- Litman, T. Pandemic-Resilient Community Planning: Practical Ways to Help Communities Prepare for, Respond to, and Recover from Pandemics and Other Economic, Social and Environmental Shocks. 2020. Available online: https://www.vtpi.org/PRCP.pdf (accessed on 14 February 2022).
- Carvalhaes, T.; Markolf, S.; Helmich, A.; Kim, Y.; Li, R.; Natarajan, M.; Bondank, E.; Ahmad, N.; Chester, M. COVID-19 as a Harbinger of Transforming Infrastructure Resilience. Front. Built Environ. 2020, 6, 148. [Google Scholar] [CrossRef]
- United Nations ESCAP. Resilience in a Riskier World: Managing Systemic Risks from Biological and Other Natural Hazards. 2021. Available online: https://hdl.handle.net/20.500.12870/3811 (accessed on 14 February 2022).
- Lai, S.; Ruktanonchai, N.W.; Zhou, L.; Prosper, O.; Luo, W.; Floyd, J.R.; Wesolowski, A.; Santillana, M.; Zhang, C.; Du, X.; et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature 2020, 585, 410–413. [Google Scholar] [CrossRef]
- Masrur, A.; Yu, M.; Luo, W.; Dewan, A. Space-time patterns, change, and propagation of COVID-19 risk relative to the intervention scenarios in Bangladesh. Int. J. Environ. Res. Public Health 2020, 17, 5911. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report, 80. 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200409-sitrep-80-covid-19.pdf (accessed on 30 April 2020).
- Mackenzie, J.S.; Smith, D.W. COVID-19: A novel zoonotic disease caused by a coronavirus from China: What we know and what we don’t. Microbiol. Aust. 2020, 41, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Mazinani, M.; Rude, B. The novel zoonotic Coronavirus disease 2019 (COVID-19) pandemic: Health perspective on the outbreak. J. Healthc. Qual. Res. 2021, 36, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.C.; Chen, C.S.; Chan, Y.J. The outbreak of COVID-19: An overview. J. Chin. Med. Assoc. 2020, 83, 217. [Google Scholar] [CrossRef] [PubMed]
- Hellewell, J.; Abbott, S.; Gimma, A.; Bosse, N.I.; Jarvis, C.I.; Russell, T.W.; Munday, J.D.; Kucharski, A.J.; Edmunds, W.J.; Sun, F.; et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob. Health 2020, 8, e488–e496. [Google Scholar] [CrossRef] [Green Version]
- Yang, Y.; Peng, F.; Wang, R.; Guan, K.; Jiang, T.; Xu, G.; Sun, J.; Chang, C. The deadly coronaviruses: The 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. J. Autoimmun. 2020, 109, 102434. [Google Scholar] [CrossRef]
- Kleinman, A.; Watson, J.L. SARS in China: Prelude to Pandemic? Stanford University Press: Redwood City, CA, USA, 2006. [Google Scholar]
- Brysse, K.; Oreskes, N.; O’Reilly, J.; Oppenheimer, M. Climate change prediction: Erring on the side of least drama? Glob. Environ. Chang. 2013, 23, 327–337. [Google Scholar] [CrossRef]
- Kircher, C.A.; Seligson, H.A.; Bouabid, J.; Morrow, G.C. When the big one strikes again—Estimated losses due to a repeat of the 1906 San Francisco earthquake. Earthq. Spectra 2006, 22, 297–339. [Google Scholar] [CrossRef] [Green Version]
- UNISDR (United Nations International Strategy for Disaster Reduction) Sendai framework for disaster risk reduction 2015–2030. In Proceedings of the 3rd United Nations World Conference on DRR, Sendai, Japan, 14–18 March 2015; pp. 14–18.
- Maini, R.; Clarke, L.; Blanchard, K.; Murray, V. The Sendai Framework for Disaster Risk Reduction and its indicators-where does health fit in? Int. J. Disaster Risk Sci. 2017, 8, 150–155. [Google Scholar] [CrossRef] [Green Version]
- Semenza, J.C.; Menne, B. Climate change and infectious diseases in Europe. Lancet Infect. Dis. 2009, 9, 365–375. [Google Scholar] [CrossRef]
- Caminade, C.; McIntyre, K.M.; Jones, A.E. Impact of recent and future climate change on vector-borne diseases. Ann. N. Y. Acad. Sci. 2019, 1436, 157. [Google Scholar] [CrossRef] [Green Version]
- Hulme, M.; Lidskog, R.; White, J.M.; Standring, A. Social scientific knowledge in times of crisis: What climate change can learn from coronavirus (and vice versa). Wiley Interdiscip. Rev. Clim. Chang. 2020, 11, e656. [Google Scholar] [CrossRef] [PubMed]
- Hassan, E.M.; Mahmoud, H.N. Orchestrating performance of healthcare networks subjected to the compound events of natural disasters and pandemic. Nat. Commun. 2021, 12, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Shi, W.; Hall, B.J. What can we do for people exposed to multiple traumatic events during the coronavirus pandemic? Asian J. Psychiatry 2020, 51, 102065. [Google Scholar] [CrossRef] [PubMed]
- Merad, M. Some Elements of Analysis of the Bibliography on Risk and Resilience on COVID-19. In COVID-19: Systemic Risk and Resilience; Springer: Cham, Switzerland, 2021; pp. 17–34. [Google Scholar]
- World Meteorological Organization. Tropical Cyclone Harold Challenges Disaster and Public Health Management. 2020. Available online: https://public.wmo.int/en/media/news/tropical-cyclone-harold-challenges-disaster-and-public-health-management (accessed on 30 April 2020).
- Frausto-Martínez, O.; Aguilar-Becerra, C.D.; Colín-Olivares, O.; Sánchez-Rivera, G.; Hafsi, A.; Contreras-Tax, A.F.; Uhu-Yam, W.D. COVID-19, Storms, and Floods: Impacts of Tropical Storm Cristobal in the Western Sector of the Yucatan Peninsula, Mexico. Sustainability 2020, 12, 9925. [Google Scholar] [CrossRef]
- Copernicus. Flood List. 2020. Available online: http://floodlist.com/america (accessed on 30 September 2020).
- Mavroulis, S.; Mavrouli, M.; Lekkas, E. Geological and hydrometeorological hazards and related disasters amid COVID-19 pandemic in Greece: Post-disaster trends and factors affecting the COVID-19 evolution in affected areas. Saf. Sci. 2021, 138, 105236. [Google Scholar] [CrossRef]
- Mishra, A.; Bruno, E.; Zilberman, D. Compound natural and human disasters: Managing drought and COVID-19 to sustain global agriculture and food sectors. Sci. Total Environ. 2020, 754, 142210. [Google Scholar] [CrossRef]
- Valkaniotis, S.; Briole, P.; Ganas, A.; Elias, P.; Kapetanidis, V.; Tsironi, V.; Fokaefs, A.; Partheniou, H.; Paschos, P. The Mw = 5.6 Kanallaki Earthquake of 21 March 2020 in West Epirus, Greece: Reverse Fault Model from InSAR Data and Seismotectonic Implications for Apulia-Eurasia Collision. Geosciences 2020, 10, 454. [Google Scholar] [CrossRef]
- Čivljak, R.; Markotić, A.; Capak, K. Earthquake in the time of COVID-19: The story from Croatia (CroVID-20). J. Glob. Health 2020, 10, e010349. [Google Scholar] [CrossRef]
- Peitl, V.; Golubić Zatezalo, V.; Karlović, D. Mental Health Issues and Psychological Crisis Interventions during the COVID-19 Pandemic and Earthquakes in Croatia. Arch. Psychiatry Res. Int. J. Psychiatry Relat. Sci. 2020, 56, 193–198. [Google Scholar]
- Svetina, L.; Kosec, A.; Curkovic, M.; Iskra, A.N. A case study of complex disasters within the resilience framework in Zagreb, Croatia: Two earthquakes in one pandemic. Environ. Res. 2022, 204, 112079. [Google Scholar] [CrossRef]
- Papadimitriou, P.; Kapetanidis, V.; Karakonstantis, A.; Spingos, I.; Kassaras, I.; Sakkas, V.; Kouskouna, V.; Karatzetzou, A.; Pavlou, K.; Kaviris, G.; et al. First Results on the Mw= 6.9 Samos Earthquake of 30 October 2020. Bull. Geol. Soc. Greece 2020, 56, 251–279. [Google Scholar] [CrossRef]
- Putz, C. 70,000 Evacuated After Breach in Uzbek Dam, Investigation Into Failure Launched. The Diplomat, 2020. [Google Scholar]
- NID. National Inventory of Dams. 2019. Available online: https://nid-test.sec.usace.army.mil/ords/f?p=105:22:13023978711032::NO::: (accessed on 30 May 2020).
- Lekkas, E.; Mavroulis, S.; Gogou, M.; Papadopoulos, G.; Triantafyllou, I.; Katsetsiadou, K.; Kranis, H.; Skourtsos, E.; Carydis, P.; Voulgaris, N.; et al. The October 30, 2020 M w 6.9 Samos (Greece) earthquake. Newsl. Environ. Disaster Cris. Manag. Strateg. Dep. Dyn. Tecton. Appl. Geol. Fac. Geol. Geoenviron. Natl. Kapodistr. Univ. Athens Athens Greece 2020, 21, 156. [Google Scholar]
- Andrews, R. What Happens If a ’Big One’ Strikes during the Pandemic? 2020. Available online: https://www.preventionweb.net/news/what-happens-if-big-one-strikes-during-pandemic (accessed on 30 May 2020).
- Kheshti, M. Protect Iran’s Zagros forests from wildfires. Science 2020, 369, 1066. [Google Scholar] [CrossRef] [PubMed]
- BBC News. US West Coast Fires in Maps, Graphics and Images. 2020. Available online: https://www.bbc.com/news/world-us-canada-54180049 (accessed on 30 September 2020).
- Doss-Gollin, J.; Farnham, D.J.; Lall, U.; Modi, V. How unprecedented was the February 2021 Texas cold snap? Environ. Res. Lett. 2021, 16, 064056. [Google Scholar] [CrossRef]
- Price, A.; Schler, B. Winter storm blackouts plagued Texas in 2011, too. Recommendations made afterward went unenforced. USA Today. 2021. Available online: https://www.usatoday.com/story/news/nation/2021/02/18/state-energy-winter-protections-lacking-reports-have-suggested/4490501001/ (accessed on 13 July 2021).
- Hixenbauh, M.; Trevizo, P. Texans recovering from COVID-19 relied on machines to help them breathe. Then the power went out. The Texas Tribune. 2021. Available online: https://www.texastribune.org/2021/03/09/texas-covid-power-outages/ (accessed on 12 July 2021).
- Harper, K.B. Hundreds of thousands of COVID-19 vaccine deliveries, injections delayed by winter storm. The Texas Tribune. 2021. Available online: https://www.texastribune.org/2021/02/16/texas-coronavirus-vaccine-winter-storm/ (accessed on 12 July 2021).
- Cobler, N. Spoiled vaccines from Texas winter storms top 3,000. Austin American-Statesman. Available online: https://www.statesman.com/story/news/coronavirus/2021/03/31/spoiled-covid-vaccines-texas-winter-storms-february-top-3-000/4807780001/ (accessed on 13 July 2021).
- Davidson, J.L.; Jacobson, C.; Lyth, A.; Dedekorkut-Howes, A.; Baldwin, C.L.; Ellison, J.C.; Holbrook, N.J.; Howes, M.J.; Serrao-Neumann, S.; Singh-Peterson, L.; et al. Interrogating resilience: Toward a typology to improve its operationalization. Ecol. Soc. 2016, 21. [Google Scholar] [CrossRef] [Green Version]
- Bruneau, M.; Reinhorn, A. Exploring the concept of seismic resilience for acute care facilities. Earthq. Spectra 2007, 23, 41–62. [Google Scholar] [CrossRef] [Green Version]
- Cimellaro, G.P.; Reinhorn, A.M.; Bruneau, M. Framework for analytical quantification of disaster resilience. Eng. Struct. 2010, 32, 3639–3649. [Google Scholar] [CrossRef]
- Bocchini, P.; Frangopol, D.; Ummenhofer, T.; Zinke, T. Resilience and sustainability of civil infrastructure: Toward a unified approach. J. Infrastruct. Syst. 2013, 20, 04014004. [Google Scholar] [CrossRef]
- Deodatis, G.; Ellingwood, B.; Frangopol, D. Safety, Reliability, Risk and Life-Cycle Performance of Structures and Infrastructures; CRC Press: Boca Raton, FL, USA, 2014. [Google Scholar]
- Sharma, N.; Tabandeh, A.; Gardoni, P. Resilience analysis: A mathematical formulation to model resilience of engineering systems. Sustain. Resilient Infrastruct. 2017, 3, 49–67. [Google Scholar] [CrossRef] [Green Version]
- Clavin, C.T.; Dabreau, A.M.; Walpole, E.H. Resilience, Adaptation, and Sustainability Plan Assessment Methodology: An Annotated Bibliography, Technical Note 2117; Technical Report; National Institute of Standards and Technology: Gaithersburg, MD, USA, 2020.
- Ayyub, B.M. Systems resilience for multihazard environments: Definition, metrics, and valuation for decision making. Risk Anal. 2014, 34, 340–355. [Google Scholar] [CrossRef] [PubMed]
- Ayyub, B.M. Resilience metrics for multi-hazard environments. In Vulnerability, Uncertainty, and Risk: Quantification, Mitigation, and Management; American Society of Civil Engineers: Reston, VA, USA, 2014; pp. 925–936. [Google Scholar]
- Haimes, Y.Y. On the definition of resilience in systems. Risk Anal. 2009, 29, 498–501. [Google Scholar] [CrossRef] [PubMed]
- Sattar, S.; McAllister, T.; Johnson, K.; Clavin, C.; Segura, C.; McCabe, S.; Fung, J.; Abrahams, L.; Sylak-Glassman, E.; Levitan, M.; et al. Research Needs to Support Immediate Occupancy Building Performance Objective Following Natural Hazard Events, NIST Special Publication 1224; Technical Report; National Institute of Standards and Technology: Gaithersburg, MD, USA, 2018.
- NIST-FEMA. Recommended Options for Improving the Built Environment for Post-Earthquake Reoccupancy and Functional Recovery Time, FEMA P-2090/NIST SP-1254; Technical Report; Federal Emergency Management Agency: Washington, DC, USA; National Institute of Standards and Technology: Gaithersburg, MD, USA, 2020.
- Folke, C. Resilience: The emergence of a perspective for social–ecological systems analyses. Glob. Environ. Chang. 2006, 16, 253–267. [Google Scholar] [CrossRef]
- Gunderson, L.H. Ecological resilience—In theory and application. Annu. Rev. Ecol. Syst. 2000, 31, 425–439. [Google Scholar] [CrossRef] [Green Version]
- Holling, C.S. Engineering resilience versus ecological resilience. Eng. Ecol. Constraints 1996, 31, 32. [Google Scholar]
- Scheffer, M. Critical Transitions in Nature and Society; Princeton University Press: Princeton, NJ, USA, 2009; Volume 16. [Google Scholar]
- Folke, C.; Carpenter, S.R.; Walker, B.; Scheffer, M.; Chapin, T.; Rockström, J. Resilience thinking: Integrating resilience, adaptability and transformability. Ecol. Soc. 2010, 15. [Google Scholar] [CrossRef]
- Walker, B.; Salt, D. Resilience Practice: Building Capacity to Absorb Disturbance and Maintain Function; Island Press: Washington, DC, USA, 2012. [Google Scholar]
- Leenhardt, P.; Teneva, L.; Kininmonth, S.; Darling, E.; Cooley, S.; Claudet, J. Challenges, insights and perspectives associated with using social-ecological science for marine conservation. Ocean Coast. Manag. 2015, 115, 49–60. [Google Scholar] [CrossRef]
- Cutter, S.L.; Ahearn, J.A.; Amadei, B.; Crawford, P.; Eide, E.A.; Galloway, G.E.; Goodchild, M.F.; Kunreuther, H.C.; Li-Vollmer, M.; Schoch-Spana, M.; et al. Disaster resilience: A national imperative. Environ. Sci. Policy Sustain. Dev. 2013, 55, 25–29. [Google Scholar] [CrossRef]
- Cutter, S.L. Linkages between vulnerability and resilience. In Vulnerability and Resilience to Natural Hazards; Cambridge University Press: Cambridge, UK, 2018; pp. 257–270. [Google Scholar]
- Koliou, M.; van de Lindt, J.W.; McAllister, T.P.; Ellingwood, B.; Dillard, M.; Cutler, H. State of the research in community resilience: Progress and challenges. Sustain. Resilient Infrastruct. 2020, 5, 131–151. [Google Scholar] [CrossRef]
- Farokhnia, K.; van de Lindt, J.W.; Koliou, M. Selection of Residential Building Design Requirements to Achieve Community Functionality Goals under Tornado Loading. Pract. Period. Struct. Des. Constr. 2020, 25, 04019035. [Google Scholar] [CrossRef]
- C.R.P. NIST. Community Resilience Planning Guide for Buildings and Infrastructure Systems, Volume I, Special Publication 1190; Technical Report; National Institute of Standards and Technology: Gaithersburg, MD, USA, 2016.
- C.R.P. NIST. Community Resilience Planning Guide for Buildings and Infrastructure Systems, Volume II, Special Publication 1190; Technical Report; National Institute of Standards and Technology: Gaithersburg, MD, USA, 2016.
- Legido-Quigley, H.; Asgari, N.; Teo, Y.Y.; Leung, G.M.; Oshitani, H.; Fukuda, K.; Cook, A.R.; Hsu, L.Y.; Shibuya, K.; Heymann, D. Are high-performing health systems resilient against the COVID-19 epidemic? Lancet 2020, 395, 848–850. [Google Scholar] [CrossRef] [Green Version]
- Wister, A.; Speechley, M. COVID-19: Pandemic risk, resilience and possibilities for aging research. Can. J. Aging/Rev. Can. Vieil. 2020, 39, 344–347. [Google Scholar] [CrossRef] [PubMed]
- Legido-Quigley, H.; Mateos-García, J.T.; Campos, V.R.; Gea-Sánchez, M.; Muntaner, C.; McKee, M. The resilience of the Spanish health system against the COVID-19 pandemic. Lancet Public Health 2020, 5, e251–e252. [Google Scholar] [CrossRef] [Green Version]
- Santarone, K.; McKenney, M.; Elkbuli, A. Preserving mental health and resilience in frontline healthcare workers during COVID-19. Am. J. Emerg. Med. 2020, 38, 1530–1531. [Google Scholar] [CrossRef]
- Plomecka, M.B.; Gobbi, S.; Neckels, R.; Radziński, P.; Skórko, B.; Lazerri, S.; Almazidou, K.; Dedić, A.; Bakalović, A.; Hrustić, L.; et al. Mental Health Impact of COVID-19: A global study of risk and resilience factors. medRxiv 2020. [Google Scholar] [CrossRef]
- Prime, H.; Wade, M.; Browne, D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. 2020, 75, 631. [Google Scholar] [CrossRef]
- Rahman, M.; Chowdhury, M.; Garcia-Ballestas, E.; Florez, W.; Agrawal, A.; Moscote-Salazar, L.R. COVID 19 and Resilience: Neurosurgical perspectives. World Neurosurg. 2020. [Google Scholar] [CrossRef]
- D’Orazio, M.; Bernardini, G.; Quagliarini, E. Sustainable and resilient strategies for touristic cities against COVID-19: An agent-based approach. arXiv 2020, arXiv:2005.12547. [Google Scholar] [CrossRef]
- Worstell, J. Ecological resilience of food systems in response to the COVID-19 crisis. J. Agric. Food Syst. Community Dev. 2020, 9, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Hobbs, J.E. Food supply chains during the COVID-19 pandemic. Can. J. Agric. Econ. Can. D’agroecon. 2020, 68, 171–176. [Google Scholar] [CrossRef] [Green Version]
- Golan, M.S.; Jernegan, L.H.; Linkov, I. Trends and applications of resilience analytics in supply chain modeling: Systematic literature review in the context of the COVID-19 pandemic. Environ. Syst. Decis. 2020, 40, 222–243. [Google Scholar] [CrossRef] [PubMed]
- Ivanov, D. Viable supply chain model: Integrating agility, resilience and sustainability perspectives—Lessons from and thinking beyond the COVID-19 pandemic. Ann. Oper. Res. 2020, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Palin, P.J. Supply Chain Resilience: Push and Pull in Catastrophes. J. Crit. Infrastruct. Policy 2020, 1, 17–35. [Google Scholar] [CrossRef]
- Hart, C.; Nash, F. Teacher Resilience during COVID: Burnout and Trauma. 2020. Available online: https://www.rti.org/insights/coaching-teacher-resilience-during-covid-19-burnout-and-trauma (accessed on 30 May 2020).
- Baker, S.R.; Bloom, N.; Davis, S.J.; Terry, S.J. COVID-Induced Economic Uncertainty; Technical Report; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- Baldwin, R.; Evenett, S. COVID-19 and Trade Policy: Why Turning Inward Won’t Work. 2020. Available online: https://voxeu.org/system/files/epublication/Covid-19_and_Trade_Policy.pdf (accessed on 30 December 2020).
- Amekudzi-Kennedy, A.; Labi, S.; Woodall, B.; Marsden, G.; Grubert, E. Role of Socially-Equitable Economic Development in Creating Resilient and Sustainable Systems: COVID-19-Related Reflections. Preprints 2020, 2020040336. [Google Scholar] [CrossRef]
- Hynes, W.; Trump, B.; Kirman, A.; Latini, C.; Linkov, I. Complexity, Interconnectedness and Resilience: Why a Paradigm Shift in Economics is Needed to Deal with Covid 19 and Future Shocks. In COVID-19: Systemic Risk and Resilience; Springer: Amsterdam, The Netherlands, 2021; pp. 61–73. [Google Scholar]
- Bostrom, A.; Bohm, G.; OConnor, R.E.; Hanss, D.; Bodi-Fernandez, O.; Halder, P. Comparative risk science for the coronavirus pandemic. J. Risk Res. 2020, 23, 902–911. [Google Scholar] [CrossRef]
- Bryce, C.; Ring, P.; Ashby, S.; Wardman, J. Resilience in the face of uncertainty: Early lessons from the COVID-19 pandemic. J. Risk Res. 2020, 23, 880–887. [Google Scholar] [CrossRef]
- Barton, M.A.; Christianson, M.; Myers, C.G.; Sutcliffe, K. Resilience in action: Leading for resilience in response to COVID-19. BMJ Leader 2020, 000260. [Google Scholar] [CrossRef]
- Sadati, A.K.; MH, B.L.; Bagheri Lankarani, K. Risk Society, Global Vulnerability and Fragile Resilience; Sociological View on the Coronavirus Outbreak. Shiraz E-Med. J. 2020, 21, e102263. [Google Scholar] [CrossRef] [Green Version]
- Collins, A.; Florin, M.V.; Renn, O. COVID-19 risk governance: Drivers, responses and lessons to be learned. J. Risk Res. 2020, 23, 1073–1082. [Google Scholar] [CrossRef]
- Aven, T.; Bouder, F. The COVID-19 pandemic: How can risk science help? J. Risk Res. 2020, 23, 849–854. [Google Scholar] [CrossRef] [Green Version]
- Dryhurst, S.; Schneider, C.R.; Kerr, J.; Freeman, A.L.; Recchia, G.; Van Der Bles, A.M.; Spiegelhalter, D.; van der Linden, S. Risk perceptions of COVID-19 around the world. J. Risk Res. 2020, 23, 994–1006. [Google Scholar] [CrossRef]
- Figari, F.; Fiorio, C.V. Welfare Resilience in the Immediate Aftermath of the COVID-19 Outbreak in Italy. Available online: https://cepr.org/content/covid-economics-vetted-and-real-time-papers-0#block-block-9 (accessed on 31 May 2020).
- CDC. The Continuum of Pandemic Phases. 2016. Available online: https://www.cdc.gov/flu/pandemic-resources/planning-preparedness/global-planning-508.html (accessed on 31 May 2020).
- Menoni, S.; Schwarze, R. Recovery during a crisis: Facing the challenges of risk assessment and resilience management of COVID-19. Environ. Syst. Decis. 2020, 40, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Hynes, W.; Trump, B.; Love, P.; Linkov, I. Bouncing forward: A resilience approach to dealing with COVID-19 and future systemic shocks. Environ. Syst. Decis. 2020, 40, 174–184. [Google Scholar] [CrossRef] [PubMed]
- Keenan, J.M. COVID, resilience, and the built environment. Environ. Syst. Decis. 2020, 40, 216–221. [Google Scholar] [CrossRef]
- Anderson, R.M.; Heesterbeek, H.; Klinkenberg, D.; Hollingsworth, T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet 2020, 395, 931–934. [Google Scholar] [CrossRef]
- San Lau, L.; Samari, G.; Moresky, R.T.; Casey, S.E.; Kachur, S.P.; Roberts, L.F.; Zard, M. COVID-19 in humanitarian settings and lessons learned from past epidemics. Nat. Med. 2020, 26, 647–648. [Google Scholar]
- Van Bavel, J.J.; Baicker, K.; Boggio, P.S.; Capraro, V.; Cichocka, A.; Cikara, M.; Crockett, M.J.; Crum, A.J.; Douglas, K.M.; Druckman, J.N.; et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020, 4, 460–471. [Google Scholar] [CrossRef]
- Aubin, J.P. Une approche viabiliste du couplage des systèmes climatique et économique. Nat. Sci. Sociétés 2010, 18, 277–286. [Google Scholar] [CrossRef] [Green Version]
- International Risk Governance Center. Guidelines for the Governance of Systemic Risks: In Systems and Organisations in the Context of Transitions; International Risk Governance Center: Lausanne, Switzerland, 2018. [Google Scholar]
- Massaro, E.; Ganin, A.; Perra, N.; Linkov, I.; Vespignani, A. Resilience management during large-scale epidemic outbreaks. Sci. Rep. 2018, 8, 1859. [Google Scholar] [CrossRef] [Green Version]
- Jovanović, A.; Klimek, P.; Renn, O.; Schneider, R.; Øien, K.; Brown, J.; DiGennaro, M.; Liu, Y.; Pfau, V.; Jelić, M.; et al. Assessing resilience of healthcare infrastructure exposed to COVID-19: Emerging risks, resilience indicators, interdependencies and international standards. Environ. Syst. Decis. 2020, 40, 252–286. [Google Scholar] [CrossRef]
- Sell, T.; Lien, O.; Toner, E. A Framework for Healthcare Resilience during Widespread Electrical Power Loss. J. Crit. Infrastruct. Policy 2020, 1, 13–26. [Google Scholar] [CrossRef]
- Mills, C.E.; Robins, J.M.; Lipsitch, M. Transmissibility of 1918 pandemic influenza. Nature 2004, 432, 904–906. [Google Scholar] [CrossRef] [PubMed]
- Sanche, S.; Lin, Y.T.; Xu, C.; Romero-Severson, E.; Hengartner, N.; Ke, R. High Contagiousness and Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2. Emerg. Infect. Dis. 2020, 26, 1470–1477. [Google Scholar] [CrossRef] [PubMed]
- Dehning, J.; Zierenberg, J.; Spitzner, F.P.; Wibral, M.; Neto, J.P.; Wilczek, M.; Priesemann, V. Inferring change points in the spread of COVID-19 reveals the effectiveness of interventions. Science 2020, 369, eabb9789. [Google Scholar] [CrossRef]
- Khachfe, H.H.; Chahrour, M.; Sammouri, J.; Salhab, H.A.; Makki, B.E.; Fares, M.Y. An Epidemiological Study on COVID-19: A Rapidly Spreading Disease. Cureus 2020, 12, e7313. [Google Scholar] [CrossRef] [Green Version]
- Lurie, N. Engla, Journal-2010-New engla nd journal. N. Engl. J. Med. 2020, 41, 1969–1973. [Google Scholar] [CrossRef]
- Goldfarb, D.S.; Benstein, J.A.; Zhdanova, O.; Hammer, E.; Block, C.A.; Caplin, N.J.; Thompson, N.; Charytan, D.M. Impending shortages of kidney replacement therapy for covid-19 patients. Clin. J. Am. Soc. Nephrol. 2020, 15, 880–882. [Google Scholar] [CrossRef]
- Rasmussen, S.; Sperling, P.; Poulsen, M.S.; Emmersen, J.; Andersen, S. Medical students for health-care staff shortages during the COVID-19 pandemic. Lancet 2020, 395, e79–e80. [Google Scholar] [CrossRef]
- Badreldin, H.A.; Atallah, B. Global drug shortages due to COVID-19: Impact on patient care and mitigation strategies. Res. Soc. Adm. Pharm. 2020, 17, 1946–1949. [Google Scholar] [CrossRef]
- Inoue, H.; Todo, Y. The propagation of economic impacts through supply chains: The case of a mega-city lockdown to prevent the spread of COVID-19. PLoS ONE 2020, 15, e0239251. [Google Scholar] [CrossRef]
- Guan, D.; Wang, D.; Hallegatte, S.; Davis, S.J.; Huo, J.; Li, S.; Bai, Y.; Lei, T.; Xue, Q.; Coffman, D.; et al. Global supply-chain effects of COVID-19 control measures. Nat. Hum. Behav. 2020, 4, 577–587. [Google Scholar] [CrossRef] [PubMed]
- Djalante, R.; Shaw, R.; DeWit, A. Building resilience against biological hazards and pandemics: COVID-19 and its implications for the Sendai Framework. Prog. Disaster Sci. 2020, 6, 100080. [Google Scholar] [CrossRef] [PubMed]
- Panchal, N.; Kamal, R.; Orgera, K.; Cox, C.; Garfield, R.; Hamel, L.; Chidambaram, P. The implications of COVID-19 for mental health and substance use. Kais. Fam. Found. 2020, 21, 1–16. [Google Scholar]
- Marko, C.; Andro, K.; Petrana, B. Stay home while going out–possible impacts of earthquake co-occurring with COVID-19 pandemic on mental health and vice versa. Brain Behav. Immun. 2020, 87, 82. [Google Scholar] [CrossRef]
- Ma, L.; Shapira, G.; De Walque, D.; Do, Q.T.; Friedman, J.; Levchenko, A.A. The Intergenerational Mortality Tradeoff of COVID-19 Lockdown Policies; Technical Report; National Bureau of Economic Research: Cambridge, MA, USA, 2021. [Google Scholar]
- Ravindran, S.; Shah, M. Unintended Consequences of Lockdowns: COVID-19 and the Shadow Pandemic; Working Paper 27562; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- Brown, C.S.; Ravallion, M. Inequality and the Coronavirus: Socioeconomic Covariates of Behavioral Responses and Viral Outcomes Across US Counties; Working Paper 27549; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- Benitez, J.A.; Courtemanche, C.J.; Yelowitz, A. Racial and Ethnic Disparities in COVID-19: Evidence from Six Large Cities; Working Paper 27592; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- Helgeson, J.F.; Aminpour, P.; Fung, J.F.; Henriquez, A.R.; Zycherman, A.; Butry, D.; Nierenberg, C.; Zhang, Y. Natural hazards compound COVID-19 impacts on small businesses disproportionately for historically underrepresented group operators. Int. J. Disaster Risk Reduct. 2022, 72, 102845. [Google Scholar] [CrossRef]
- Boustan, L.P.; Kahn, M.E.; Rhode, P.W.; Yanguas, M.L. The Effect of Natural Disasters on Economic Activity in US Counties: A Century of Data; Working Paper 23410; National Bureau of Economic Research: Cambridge, MA, USA, 2017. [Google Scholar]
- Hsiang, S.M.; Jina, A.S. The Causal Effect of Environmental Catastrophe on Long-Run Economic Growth: Evidence From 6700 Cyclones; Working Paper 20352; National Bureau of Economic Research: Cambridge, MA, USA, 2014. [Google Scholar]
- Jordà, s.; Singh, S.R.; Taylor, A.M. Longer-Run Economic Consequences of Pandemics; Working Paper 26934; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- Noy, I.; Doan, N.; Ferrarini, B.; Park, D. Measuring the Economic Risk of COVID-19. Glob. Policy 2020, 11, 413–423. [Google Scholar] [CrossRef]
- Cavallo, E.; Galiani, S.; Noy, I.; Pantano, J. Catastrophic natural disasters and economic growth. Rev. Econ. Stat. 2013, 95, 1549–1561. [Google Scholar] [CrossRef] [Green Version]
- Ramalanjaona, G. Impact of 2004 tsunami in the islands of Indian ocean: Lessons learned. Emerg. Med. Int. 2011, 2011, 920813. [Google Scholar] [CrossRef] [PubMed]
- Guha-Sapir, D.; van Panhuis, W.G. Health impact of the 2004 Andaman Nicobar earthquake and tsunami in Indonesia. Prehospital Disaster Med. 2009, 24, 493–499. [Google Scholar] [CrossRef] [Green Version]
- Doocy, S.; Cherewick, M.; Kirsch, T. Mortality following the Haitian earthquake of 2010: A stratified cluster survey. Popul. Health Metr. 2013, 11, 5. [Google Scholar] [CrossRef] [Green Version]
- Miyagawa, S.; Satoh, M.; Furuya, S.; Yamada, Y.; Shaw, R. External Support and Community Cooperation during Long-Term Sheltering—From the Case of the Great East Japan Earthquake. In Public Health and Disasters; Springer: Berlin/Heidelberg, Germany, 2020; pp. 201–219. [Google Scholar]
- Kondo, H.; Seo, N.; Yasuda, T.; Hasizume, M.; Koido, Y.; Ninomiya, N.; Yamamoto, Y. Post-flood—Infectious diseases in Mozambique. Prehospital Disaster Med. 2002, 17, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Mousavi, S.; Bagchi, A.; Kodur, V.K. Review of post-earthquake fire hazard to building structures. Can. J. Civ. Eng. 2008, 35, 689–698. [Google Scholar] [CrossRef]
- Gunter, P. U.S. Unprepared for Nuclear Accident during Pandemic. 2020. Available online: https://www.commondreams.org/newswire/2020/05/22/us-unprepared-nuclear-accident-during-pandemic (accessed on 31 May 2020).
- Watson, J.T.; Gayer, M.; Connolly, M.A. Epidemics after natural disasters. Emerg. Infect. Dis. 2007, 13, 1–5. [Google Scholar] [CrossRef]
- Lemonick, D.M. Epidemics after natural disasters. Am. J. Clin. Med. 2011, 8, 144–152. [Google Scholar]
- Kouadio, I.K.; Aljunid, S.; Kamigaki, T.; Hammad, K.; Oshitani, H. Infectious diseases following natural disasters: Prevention and control measures. Expert Rev. Anti-Infect. Ther. 2012, 10, 95–104. [Google Scholar] [CrossRef]
- Spiegel, P.B.; Le, P.; Ververs, M.T.; Salama, P. Occurrence and overlap of natural disasters, complex emergencies and epidemics during the past decade (1995–2004). Confl. Health 2007, 1, 2. [Google Scholar] [CrossRef] [Green Version]
- IASC Working Group XVI-th Meeting. Definition of Complex Emergencies; Technical Report; Inter-Agency Standing Committee: New York, NY, USA, 1994. [Google Scholar]
- Salama, P.; Spiegel, P.; Talley, L.; Waldman, R. Lessons learned from complex emergencies over past decade. Lancet 2004, 364, 1801–1813. [Google Scholar] [CrossRef]
- Hariri-Ardebili, M.A. Living in a multi-risk chaotic condition: Pandemic, natural hazards and complex emergencies. Int. J. Environ. Res. Public Health 2020, 17, 5635. [Google Scholar] [CrossRef]
- Deryugina, T.; Gruber, J.; Sabety, A. Natural Disasters and Elective Medical Services: How Big is the Bounce-Back? Working Paper 27505; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- Ishiwatari, M.; Koike, T.; Hiroki, K.; Toda, T.; Katsube, T. Managing disasters amid COVID-19 pandemic: Approaches of response to flood disasters. Prog. Disaster Sci. 2020, 6, 100096. [Google Scholar] [CrossRef]
- Ebrahim, S.H.; Memish, Z.A. COVID-19–the role of mass gatherings. Travel Med. Infect. Dis. 2020, 34, 101617. [Google Scholar] [CrossRef]
- Dincer, O.; Gillanders, R. Shelter in place? Depends on the place: Corruption and social distancing in American states. Soc. Sci. Med. 2021, 269, 113569. [Google Scholar] [CrossRef]
- Bambarén, C. Legal issues of humanitarian assistance after the 2007 earthquake in Pisco, Peru. Prehospital Disaster Med. 2010, 25, 203–206. [Google Scholar] [CrossRef] [PubMed]
- Li, X.H.; Zheng, J.C. Efficient post-disaster patient transportation and transfer: Experiences and lessons learned in emergency medical rescue in Aceh after the 2004 Asian tsunami. Mil. Med. 2014, 179, 913–919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Minimum Technical Standards and Recommendations for Rehabilitation—Emergency Medical Teams; Technical Report; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Fakhruddin, B.; Blanchard, K.; Ragupathy, D. Are we there yet? The transition from response to recovery for the COVID-19 pandemic. Prog. Disaster Sci. 2020, 7, 100102. [Google Scholar] [CrossRef] [PubMed]
- Kirsch, T.D.; Mitrani-Reiser, J.; Bissell, R.; Sauer, L.M.; Mahoney, M.; Holmes, W.T.; Santa Cruz, N.; De La Maza, F. Impact on hospital functions following the 2010 Chilean earthquake. Disaster Med. Public Health Prep. 2010, 4, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Yavari, S.; Chang, S.E.; Elwood, K.J. Modeling post-earthquake functionality of regional health care facilities. Earthq. Spectra 2010, 26, 869–892. [Google Scholar] [CrossRef]
- Ceferino, L.; Kiremidjian, A.S.; Deierlein, G.G. Probabilistic Model for Regional Multiseverity Casualty Estimation due to Building Damage Following an Earthquake. Spec. Collect. ASCE-ASME J. Risk Uncertain. Eng. Syst. Part A Civ. Eng. 2018, 4, 04018023. [Google Scholar] [CrossRef]
- Ceferino, L.; Mitrani-Reiser, J.; Kiremidjian, A.; Deierlein, G.; Bambarén, C. Effective plans for hospital system response to earthquake emergencies. Nat. Commun. 2020, 11, 1–12. [Google Scholar] [CrossRef]
- Helgeson, J.F.; Fung, J.F.; Roa-Henriques, A.; Zhang, Y.; Zycherman, A.; Nierenberg, C.; Butry, D.T.; Ramkissoon, D. Complex Event Resilience of Small- and Medium-Sized Enterprises: Natural Disaster Planning during the COVID-19 Pandemic; Special Publication Forthcoming; National Institute of Standards and Technology: Gaithersburg, MD, USA, 2020.
- Wang, Z.; Ye, X. Social media analytics for natural disaster management. Int. J. Geogr. Inf. Sci. 2018, 32, 49–72. [Google Scholar] [CrossRef]
- Li, Z.; Wang, C.; Emrich, C.T.; Guo, D. A novel approach to leveraging social media for rapid flood mapping: A case study of the 2015 South Carolina floods. Cartogr. Geogr. Inf. Sci. 2018, 45, 97–110. [Google Scholar] [CrossRef]
- Fearnley, C.J.; Dixon, D. Early warning systems for pandemics: Lessons learned from natural hazards. Int. J. Disaster Risk Reduct. 2020, 49, 101674. [Google Scholar] [CrossRef] [PubMed]
- AI-Youbi, A.O.; Al-Hayani, A.; Bardesi, H.J.; Basheri, M.; Lytras, M.D.; Aljohani, N.R. The King Abdulaziz University (KAU) pandemic framework: A methodological approach to leverage social media for the sustainable management of higher education in crisis. Sustainability 2020, 12, 4367. [Google Scholar] [CrossRef]
- Zhou, S. Impact of pandemic proximity and media use on risk perception during COVID-19 in China. Geomat. Nat. Hazards Risk 2022, 13, 591–609. [Google Scholar] [CrossRef]
- Mirbabaie, M.; Bunker, D.; Stieglitz, S.; Marx, J.; Ehnis, C. Social media in times of crisis: Learning from Hurricane Harvey for the coronavirus disease 2019 pandemic response. J. Inf. Technol. 2020, 35, 195–213. [Google Scholar] [CrossRef]
- Mukherjee, S.; Kumar, R.; Bala, P.K. Managing a natural disaster: Actionable insights from microblog data. J. Decis. Syst. 2022, 31, 134–149. [Google Scholar] [CrossRef]
- Eyre, R.; De Luca, F.; Simini, F. Social media usage reveals recovery of small businesses after natural hazard events. Nat. Commun. 2020, 11, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Bostick, T.P. Ten Strategies for Leadership during COVID-19: A Plan of Action for Decision Makers in Times of Critical Change. In COVID-19: Systemic Risk and Resilience; Springer: Cham, Switzerland, 2021; pp. 11–16. [Google Scholar]
- Gilbert, A.Q.; Bazilian, M.D. The COVID-19 Pandemic: Energy Market Disruptions and Resilience. J. Crit. Infrastruct. Policy 2020, 1, 73–83. [Google Scholar] [CrossRef]
- Kawamura, Y.; Dewan, A.M.; Veenendaal, B.; Hayashi, M.; Shibuya, T.; Kitahara, I.; Nobuhara, H.; Ishii, K. Using GIS to develop a mobile communications network for disaster-damaged areas. Int. J. Digit. Earth 2014, 7, 279–293. [Google Scholar] [CrossRef]
- Shah, P.; Patel, C.R. Prevention is better than cure: An application of big data and geospatial technology in mitigating pandemic. Trans. Indian Natl. Acad. Eng. 2020, 5, 187–192. [Google Scholar] [CrossRef]
- Hill, S.; Hutton, N.S.; Whytlaw, J.L.; Yusuf, J.E.; Behr, J.G.; Landaeta, E.; Diaz, R. Changing Logistics of Evacuation Transportation in Hazardous Settings during COVID-19. Nat. Hazards Rev. 2021, 22, 04021029. [Google Scholar] [CrossRef]
- Rajabifard, A.; Paez, D.; Foliente, G. COVID-19 Pandemic, Geospatial Information, and Community Resilience: Global Applications and Lessons; Taylor & Francis: Abingdon, UK, 2021. [Google Scholar]
- Nakai, H.; Itatani, T.; Horiike, R. Construction of an evacuee placement model for tsunami shelters considering physical distancing to prevent COVID-19 infection. Prog. Disaster Sci. 2021, 11, 100183. [Google Scholar] [CrossRef]
- Ghorbanzadeh, M. Accessibility-Based Assessment and Modeling of Evacuations and Sheltering for Hurricanes and Pandemics. Ph.D. Thesis, The Florida State University, Tallahassee, FL, USA, 2021. [Google Scholar]
- Page-Tan, C.; Fraser, T. CoViD-19 to go? The role of disasters and evacuation in the CoViD-19 pandemic. Glob. Environ. Chang. 2022, 73, 102471. [Google Scholar] [CrossRef] [PubMed]
- Hariri-Ardebili, M.A.; Lall, U. Superposed natural hazards and pandemics: Breaking dams, floods, and COVID-19. Sustainability 2021, 13, 8713. [Google Scholar] [CrossRef]
- Tripathy, S.S.; Bhatia, U.; Mohanty, M.; Karmakar, S.; Ghosh, S. Flood evacuation during pandemic: A multi-objective framework to handle compound hazard. Environ. Res. Lett. 2021, 16, 034034. [Google Scholar] [CrossRef]
- Hutton, N.S.; Mumford, S.W.; Saitgalina, M.; Yusuf, J.E.; Behr, J.G.; Diaz, R.; Kiefer, J.J. Nonprofit capacity to manage hurricane-pandemic threat: Local and national perspectives on resilience during COVID-19. Int. J. Public Adm. 2021, 44, 984–993. [Google Scholar] [CrossRef]
- Dargin, J.S.; Li, Q.; Jawer, G.; Xiao, X.; Mostafavi, A. Compound hazards: An examination of how hurricane protective actions could increase transmission risk of COVID-19. Int. J. Disaster Risk Reduct. 2021, 65, 102560. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).