Abstract
Background and objectives: Quality of life and sleep quality of college students were extensively studied. The present study evaluated sleep quality and quality of life of college students in Taiwan by using the Pittsburgh Sleep Quality Index (PSQI) and Short-Form Health Survey (SF-36), respectively. Materials and Methods: Data of 1756 college students aged 20–24 years were collected in this study. Association rule analysis was also used to provide a graphics-based visualization of the relationships between data, enabling the rapid identification of data correlations. Results: The results showed that the average physical component scale (PCS) and average mental component scale (MCS) scores were 52.9 and 44.1, respectively. Based on their body mass index (BMI), participants were divided into underweight, normal, overweight, and obese groups. The results of one-way analysis of variance showed that the p values for the PSQI, PCS, and MCS scores were 3.5 × 10−5, 1.7 × 10−5, and 0.671, respectively. The normal and overweight groups had the lowest PSQI scores. The PCS score of the obese group was lower than that of normal and overweight groups. The p values of the t-test result among PSQI, BMI, PCS, and MCS groups were 0.002, <2 × 10−16, and <2 × 10−16, respectively. The good sleep quality group had higher PCS and MCS scores. Conclusions: In this study, the results of association rule analysis indicated two distinct groups: Group 1, with the characteristics of good sleep quality as revealed by the high MCS and PCS scores, and Group 2, with the characteristics of poor sleep quality as revealed by low MCS and PCS scores and underweight BMI.
1. Introduction
The advent of modern technologies and the fast-paced lifestyle have led to an increased prevalence of sleep disorders. More than 25% of people in Taiwan have been reported to be affected by insomnia [1]. Similar to air, food, and water, sleep is a necessity of life. Moreover, it is one of the fundamental requirements for physiological well-being, because sleep deprivation and poor sleep quality can substantially affect behavioral cognition and can cause other physiological changes. Long-term insomnia has also been found to increase the risk of emotional disorder; moreover, several studies have identified the correlations between insomnia or sleep deprivation and numerous psychological and physiological diseases [2]. Because sleep constitutes approximately one-third of a person’s lifetime, sleep-related problems affect not only physiological and mental health but also the development of interpersonal relationships and the performance of social functions. Thus, sleep disorder is a complicated problem that involves a wide range of aspects, including but not limited to personal, hereditary, physiological, psychological, mental, genealogical, social, and environmental factors [3]. Without adequate treatment or improvement, sleep disorder may result in serious mental and social problems. Sleep is closely related to physical and mental health problems as well as problem behaviors among adolescents and young adults [4]. In recent years, sleep quality has been widely used as a key indicator in the assessment of sleep in both clinical practice and medical research. However, few studies explore the concept. Sleep quality is highly complicated and thus difficult to define or measure objectively [5,6]. It is influenced by a number of factors, such as social transition, occupational stress, lifestyle, personal mental/health conditions, habits, the environment, diseases, and other physiological conditions [7]. As a basic requirement for health, sleep maintained with high quality is crucial in modern life [8]. Studies have indicated that a high percentage of young people lack quality sleep [9,10], which results in deteriorated academic and athletic performance and even leads to emotional and behavioral problems that eventually develop into mental diseases such as depression.
Advances in technology and social transition have led to a deferred sleep time, the consequences of which are insufficient sleep and poor sleep quality. These phenomena are becoming rapidly prevalent among people. For school-going youths, sleep disorder is often aggravated by study-related stress and electronic media abuse. Because adolescence is the pivotal period for mental and physical development, the influence of sleep cannot be overlooked. Improved sleep quality is known to be beneficial for mental and physical development, academic performance, and personality development. For youths, a lack of sleep or poor sleep quality can lead to fatigue, inattention, and increased daytime dozing, and poor sleep quality also affects their emotional conditions and behaviors in the long term. Furthermore, as they grow older, the situation of deferred sleep becomes more prominent among school-going youths, reducing their duration of sleep; compared with youths in the west, deferred sleep is more acute among youths in Asia [11]. The implication of the present study may be that college students must be made aware of the consequences of inadequate sleep quality and risk factors could be improved if students tried to change their behavior and subjective consciousness [12]. Other than the influence on behaviors, sleep disorder can also cause problems such as developmental retardation and obesity [13]. In addition, insufficient sleep syndrome is known to be associated with suicidal tendencies; youths with long-term sleep deprivation have been demonstrated to exhibit a higher risk of suicide than peers without sleep disorder [14]. Sleep not only controls the efficiency of initial learning but also mediates the subsequent consolidation of memory. During sleep, the biological activities of the neural system at molecular and cellular levels, as well as the remodeling mechanism of the neural network, exert strong effects on the consolidation of long-term memories [15]. Sleep is a requisite for the attainment, maintenance, and restoration of physical and mental health, including physiological function, cognition, and physical recovery [16]. Sleep is also essential for the sustainability of body functions; the cells damaged during the day are repaired during sleep, and the remodeling of cognition and memories in the brain occurs during sleep, which is the reason for higher mental alertness after sufficient sleep. Therefore, the quality of sleep achieved in the nighttime often influences the emotions and behaviors exhibited in the daytime [13]. Sleep is essential for the body, mind, memory, and learning [17]. A substantial portion of college athletes experience poor sleep health and would benefit from interventions aimed at improving sleep [18]. Furthermore, sleep quality has been shown to be closely associated with students’ learning abilities and academic performance; poor learning capacity is often the related to constant sleep loss [19]. Students with poor sleep quality often exhibit poor mental clarity and academic performance in the day, and they are also more prone to depression and negative emotions [20].
Most recent studies on sleep quality have used the Pittsburgh Sleep Quality Index (PSQI) as the assessment tool for sleep quality [21]. The PSQI, which was developed by Buysse et al. [5], consists of seven items: subjective sleep quality, sleep latency (i.e., the length of time required to fall asleep), sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Each of these items is scored 0–3; a higher score denotes poorer sleep quality. The total score ranges from 0 to 21, and a total score of ≤ 5 indicates excellent sleep quality, whereas a total score of > 5 implies poor sleep quality [22]. It is commonly known worldwide that lifestyle can influence personal health. The college stage is the pivotal period during which a youth grows into an adult, and this stage shapes his or her health-related behaviors. Applying assessment tools for college students’ lifestyles and health-related behaviors can help them establish a healthy lifestyle and warn against unhealthy habits or factors. Consequently, adequate health-promoting strategies and interventions can be introduced to help them lead a healthy and positive life. Quality of life is an individual’s perception of well-being in the cultural or value system he or she is in, and this perception is closely associated with personal goals, expectations, standards, and values. Lifestyle is a key factor that governs the life and health of modern people, and it is a key factor that influences the improvement in quality of life. Thus, a positive improvement in lifestyle will increase quality of life. Research has indicated that increased physical activities can lead to changes in lifestyle; thus, exercise is the most straightforward and effective strategy for improving quality of life [23]. Exercise is known to improve peoples’ satisfaction with the physical, psychological, social, and environmental aspects of quality of life; although increasing physical activities can only rectify health-endangering behaviors, it can still improve quality of life [24]. In terms of health, people with intensive physical activities usually have higher quality of life than those who are inactive [25]. Regular physical activities have been proven to exert numerous positive effects that can improve the physiological system, physical fitness, cardiovascular function, immunity, endocrine system, cognitive function, and general health [26]. The positive effects of regular exercise on physical and mental health are positively correlated with life satisfaction. A healthier body and mind contribute to greater life satisfaction and hence higher quality of life.
The Short-Form Health Survey (SF-36) is a self-rated scale consisting of eight multi-item subscales plus one additional item for the perceived change in health [27,28]. The eight subscales can also be divided into two summary measures: the physical component scale (PCS), which combines physical function, role limitations due to physical health problems, bodily pain, and general health perceptions subscales, and the mental component scale (MCS), which combines vitality, social functioning, emotional well-being, and role limitations due to emotional problems subscales. As per the scoring instructions, the scores of these two scales are calculated as follows: the scores of the eight subscales are standardized; thereafter, the standardized scores of each subscale is multiplied by a standardized coefficient derived from factor analysis depending on the scale (PCS or MCS); subsequently, the scores of the same scale are summed up to provide the composite score. The score of each subscale ranges from 0 to 100, with 0 denoting the poorest quality of health and 100 the highest quality of health [29]. The SF-36 has been widely applied to evaluate quality of life, including that of college students [30].
The recent development of big data analytics has benefited studies investigating sleep quality and health. Schatz Bruce applied big data analytics techniques for mobile health monitors and showed that complete baseline records can be acquired by using effective National Surveys of Population Health [31]. Among the numerous big data analytics techniques, link analysis is an information science approach [32] that uses graphics-based visualization methods to present related data, enabling the rapid identification of correlations between the data [33]. Association rule analysis can also be integrated with text analysis; such integration has been proven to be effective for web document analysis [34]. In the present study, link analysis was implemented along with conventional statistical analysis to identify significant factors affecting college students’ sleep quality and quality of life.
2. Materials and Methods
2.1. Participants Information
In this study, 1756 college students aged 20–24 years were recruited as participants. A total of 958 and 798 participants were men and women, respectively. Participants information is listed in Table 1.

Table 1.
Participants information.
2.2. Institutional Review Board Statement
Participants provided written consent and their demographic data. Subsequently, they completed the SF-36 and PSQI surveys. The study protocol was approved by the Institutional Review Board of Asia University (IRB approval No. 10512004).
2.3. Association Rule Analysis and STATISTICS
Assume there are two groups, and X is element in the first group, Y is element in the second group. There are three parameters used in association rule analysis [35] Support: The percentage of union of X and Y to the total number of the data, and m is the total number of the data.
Confidence: The ratio of union of X and Y to the number of either X or Y.
Lift: The ratio of confidence to expected confidence.
The association rule analysis is conducted using PolyAnalyst 6 software (Megaputer Co. Bloomington, IN, USA). The categorized PSQI, PCS, and MCS scores of the BMI groups were imported to PolyAnalyst. A high significance between the variables could be demonstrated and visualized as a link pattern.
2.4. Statistical
Descriptive statistics were calculated for the means, standard deviations, quartiles, and numbers of participants’ BMI, PSQI, PCS, and MCS data. One-way analysis of variance (ANOVA) was applied to evaluate the PCS, MCS, and PSQI data of the four BMI groups, followed by a t test for each group. Because PSQI scores were categorized into only two types (“good sleep quality” and “poor sleep quality”), a t test was applied to examine the differences in BMI, PCS, and MCS data between the PSQI groups. Additionally, a two-way chi-square test was applied to determine differences in the BMI, PSQI, PCS, and MCS data. To determine the R-squared value of the regression line, a regression analysis was implemented to examine the paired PCS, MCS, and PSQI data.
3. Results
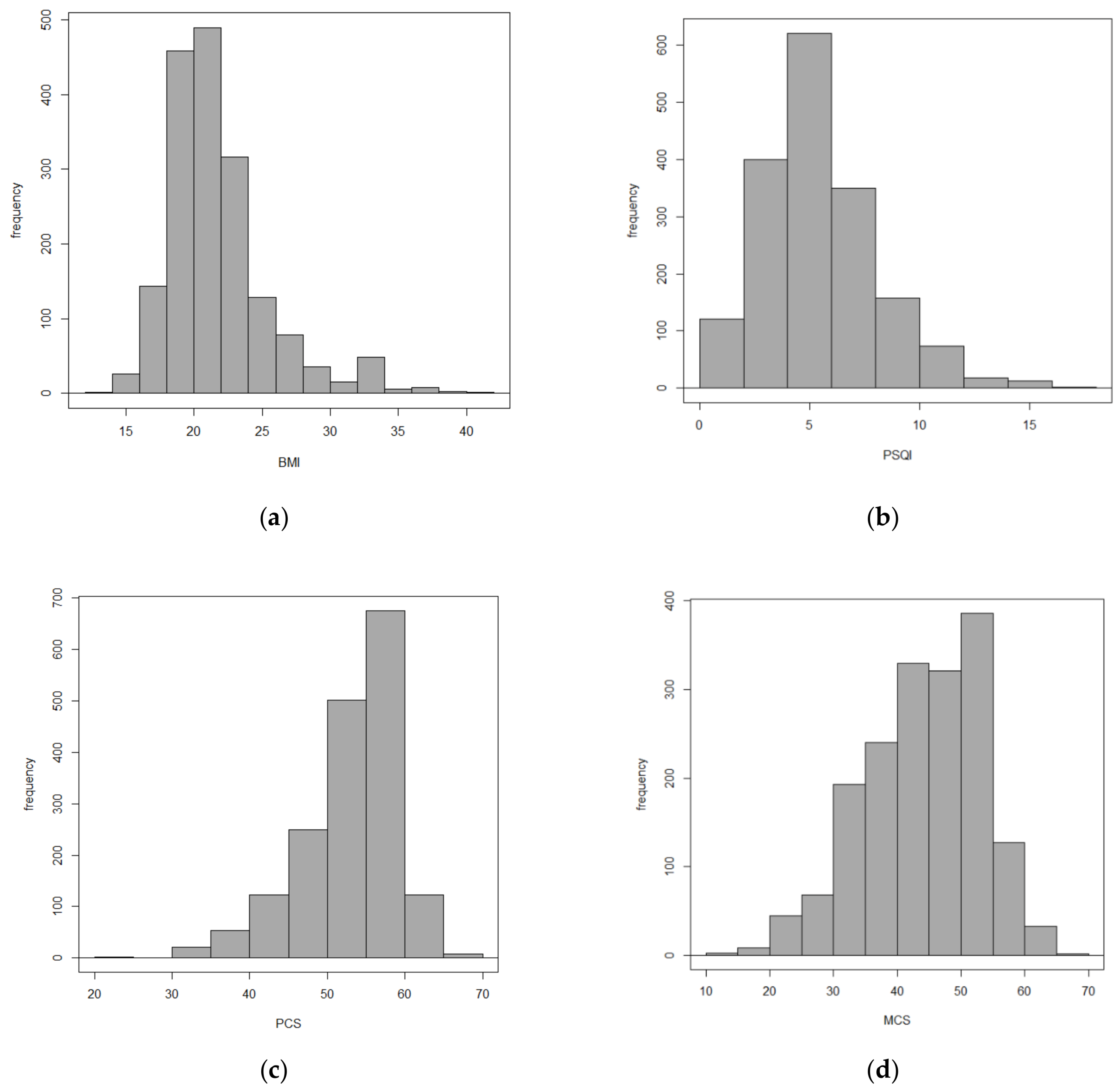
The distributions of participants’ BMI, PSQI, PCS, and MCS are shown in Figure 1a–d, respectively. The bar charts in the figure show that the BMI, PSQI, PCS, and MCS data were all evenly distributed. The quartiles of these data are listed in Table 2.
Figure 1.
Distribution of (a) BMI, (b) PSQI, (c) PCS, and (d) MCS.

Table 2.
Distribution of BMI, PSQI, PCS, MCS.
For PSQI, the mean score was 5. A score of 5 or higher indicated a diagnosis of sleep disorder. The mean PCS and MCS scores were 52.9 and 44.1, respectively. Subsequently, participants were divided into groups based on different parameters. For PSQI, participants with a PSQI score of ≥5 were classified as “good sleep quality” (N = 925), whereas those with a PSQI score of <5 were classified as “poor sleep quality” (N = 831). For PCS and MCS, participants were divided into two groups. Those with a PCS score of <50 were classified as “PCS < 50” (N = 449), and “PCS > 50” group were 1307 subjects. Similarly, “MCS < 50” (N = 1208), and “MCS > 50” (N = 548) were also classified. Participants were divided into four groups based on their BMI: underweight “BMI < 18.5” (N = 238), normal “24 > BMI ≥ 18.5” (N = 1197), overweight “27 > BMI ≥ 24”(N = 165), and obese “BMI ≥ 27” (N = 156). The number of participants in the groups are listed in Table 3. The BMI definition of the four groups is according to the rule by Ministry of Health and Welfare in Taiwan [36].

Table 3.
Number of participants in the groups.
Table 4 shows the results of one-way ANOVA for the PSQI, PCS, and MCS scores of the four BMI groups. Significant differences in PSQI, PCS, and MCS scores were observed among the four BMI groups. Moreover, the results of the paired t test showed that underweight and obese groups exhibited similar PSQI scores (b), with a mean PSQI score ≥ 6. By contrast, the normal and overweight groups exhibited the similar low PSQI scores, with a mean PSQI score of ≤5.7 (a). This finding suggests that both obesity and underweight have negative effects on sleep. The PCS score of the obese and underweight groups was significantly lower than normal and overweight groups. No statistical difference was observed in the MCS score among the BMI groups. This finding suggests that BMI is unrelated with the mental aspect of quality of life.

Table 4.
One-way ANOVA results for BMI group. Superscript Letter a,b,c are label for the same group based on t-test result. The same lettern means the same group. *** denote p value < 0.001.
Table 5 shows the results of t test for the BMI, PCS, and MCS scores of the PSQI groups. The poor Sleep Quality group had lower PCS and MCS scores, whereas the PSQI_better group had higher PCS and MCS scores. This finding suggests that PSQI is highly correlated with PCS and MCS. However, the difference between PSQI and BMI was found to be nonsignificant.

Table 5.
Results of t test for PSQI groups. *** denote p value < 0.001.
Table 6 shows the results of the two-way chi-square test. A statistical difference was observed between the PSQI groups and PCS and MCS (p < 10−16), corroborating the preceding results. Moreover, statistically significant differences were observed among the PSQI, PCS, MCS and BMI groups.

Table 6.
Two-way factor analysis and p values.
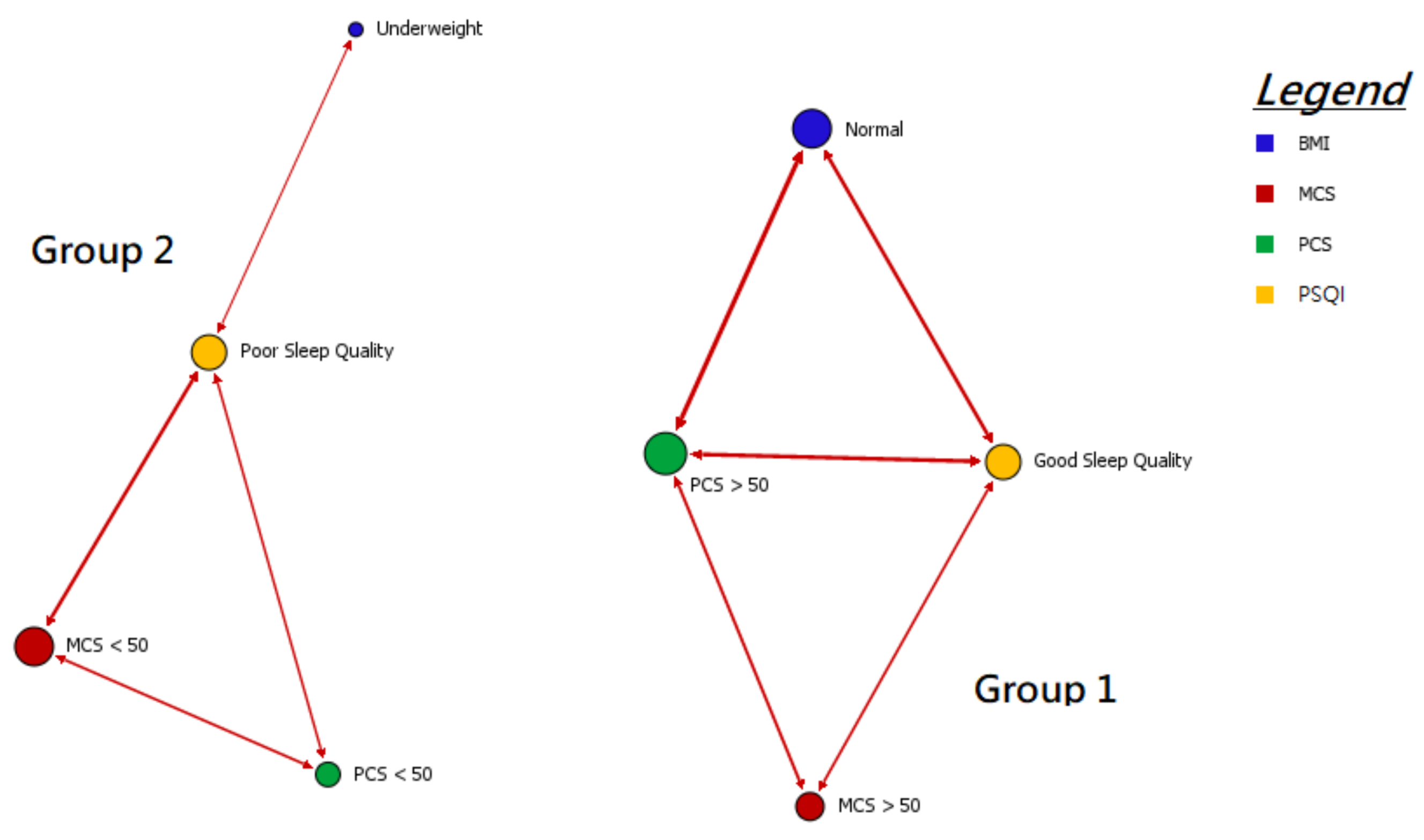
The results of link analysis clearly indicated the existence of two patterns (groups), which are shown in Figure 2, and their parameters are listed in Table 7.
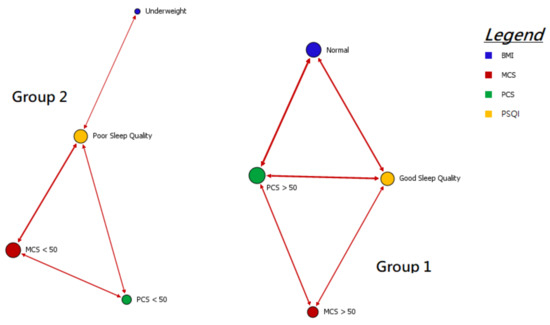
Figure 2.
Links among high support parameters by association rule analysis.

Table 7.
Association rule analysis result of two groups. Table 7a–d are result for union, support, confidence and lifting.
4. Discussion
In this study, two groups were identified through the association rule analysis of the data. One group was the healthier group with the characteristics of good sleep quality, PCS > 50, MCS > 50 and normal BMI level. The other group was the group with poor quality of life and sleep quality, and PCS and MCS both less than 50. The average SF-36 score is 50. Thus, the healthier group had a higher-than-average PCS and MCS score, and the less healthy group had a below average PCS and MCS score, accompanied with underweight BMI level. Furthermore, this study proposed an interesting approach: association rule can be used for clustering statistical data. Each data batch contains numerous parameters; conventional statistical methods can only determine the existence of correlations or significant differences among the parameters, but these methods cannot identify the concurrent characteristics that the groups with parameters exhibiting significant difference possess. Moreover, for a large number of parameters, conventional statistical methods are time consuming for making one-by-one comparisons and still fail to provide a complete result. The association rule can link data batches with the same characteristics, and for a high number of links, a bold line will be shown as an indication. Moreover, association rule can rapidly visualize significant clusters among the data batches. This new approach, along with the visualization effect, is much faster than conventional statistical approaches for sorting data. A high significance value also indicates a statistical difference. For example, in Group 1, the “good sleep quality” group was linked with PCS > 50, MCS > 50 and normal BMI group. In Group 2, the “poor sleep quality” group was linked with PCS < 50, MCS < 50 and underweight BMI group. According to the statistical test results, a statistical difference was observed between the sleep quality groups and the PCS groups and MCS groups (p < 2.2 × 10−16). Therefore, the visualized results of link analysis can provide not only enables the rapid clustering of data, but also identifies parameters with high statistical differences through the visualization of direct links. Another benefit of this approach is the fast computation time, which enables the rapid processing of massive amounts of data. However, for its effectiveness, highly significant clustering should be present in the data. Considering that association rule analysis has never been applied in this type of study, its successful application here can be considered a major contribution of this study.
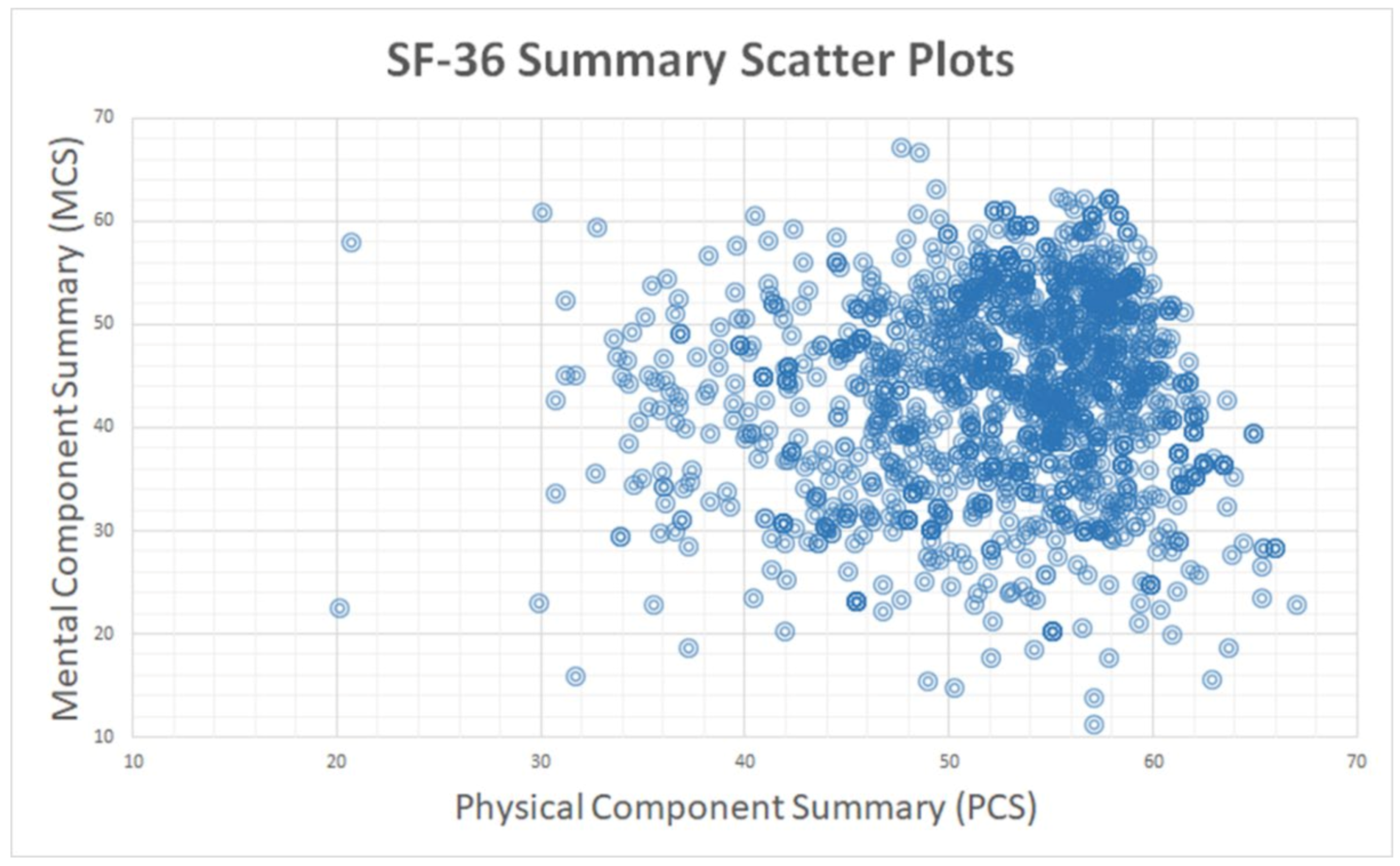
Other commonly used data clustering methods, such as K-means clustering, require advance knowledge on the number of clusters or the distribution of data. However, these methods are ineffective when little difference is present in the data. Moreover, they are ineffective when little difference is present between data dimensions. For example, when the MCS and PCS data, which are of similar dimensions, were converted into an x-y two-dimensional distribution diagram (Figure 3), the two groups could not be distinguished from the diagram. Moreover, because the R-square of linear regression line was 0.0035, MCS and PCS were obviously not positively correlated. Thus, previously applied data analysis methods are unable to show any clearly distinguishable clustering patterns for the data, which is their limitation. Association rule analysis, however, can identify the distinction from the links of sample characteristics and can rapidly visualize the links, which is convenient.
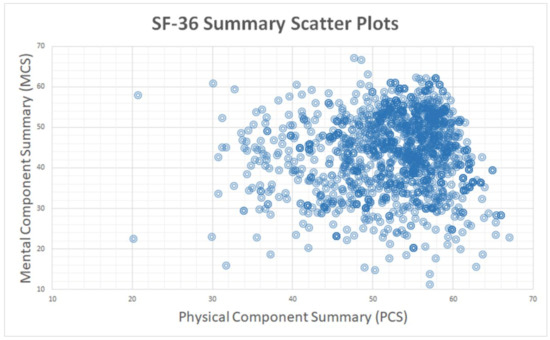
Figure 3.
PCS-MCS distribution map.
There are several limitations to this article. In the data part, the data were only collected from single college school, and the amount of data is not very large. The more schools that can be collected, the better the correlation between the two questionnaires can be presented. In the method part, association rule analysis may be superior to the traditional clustering method, judging by the results of this study. This conclusion is only applied on the correlation between PSQI and Quality of life surveys. If it is applied to other questionnaires, it may not have similar results. More research is needed to verify. In addition, the number of subjects needed to present for association rule analysis to cluster separate data which have no statistical difference is still unknown. This study can be treated as it a pilot study, indicating that association rule analysis may be applicable to the grouping of survey data.
The future direction of this study can be extended from several aspects. The first is to study the relation between two surveys from before and after a specific health promotion program. The association rule analysis results may reflect the improvement of sleep quality and quality of life for college students. The second is to increase the number of data in the set, including total subject numbers and college numbers to verify whether the findings of this study are present in other general college student populations. The third is to apply association rule analysis on other surveys, and to investigate the correlation between the degree of difference of the data and clustering performance by association rule analysis.
5. Conclusions
Although numerous studies have been conducted on quality of life and sleep quality of college students, the application of association rule analysis for the clustering and distribution of a massive sample data is innovative. In this study, this approach enabled the rapid grouping of participants into the healthier and less healthy groups, and then used graphics-based visualization to present the links between their quality of life and sleep quality scores. This is a rapid and effective approach for presenting data and preliminary analytic results.
Author Contributions
Conceptualization, Y.-C.Y., S.-P.C.; methodology, J.-W.L., S.-P.C.; software, K.-M.C.; validation, J.-W.L., C.-P.C.; formal analysis, K.-M.C.; investigation, Y.-C.Y., C.-P.C., K.-M.C.; resources, S.-P.C.; writing—original draft preparation, K.-M.C.; writing—review and editing, S.-P.C.; supervision, J.-W.L.; project administration, C.-P.C.; funding acquisition, Y.-C.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by China Medical University Hospital, grant number ASIA-110-CMUH-09 and Central Taiwan University of Science and Technology, grant number CTU107-PC-003.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kao, C.-C.; Huang, C.-J.; Wang, M.-Y.; Tsai, P.-S. Insomnia: Prevalence and its impact on excessive daytime sleepiness and psychological well-being in the adult Taiwanese population. Qual. Life Res. 2008, 17, 1073–1080. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-H.; Chang, S.-P. Investigation of Relationship between Sleep Duration and Body Mass Index. J. Sport Recreat. Res. 2012, 7, 68–78. [Google Scholar] [CrossRef]
- Pallos, H.; Gergely, V.; Yamada, N.; Miyazaki, S.; Okawa, M. The quality of sleep and factors associated with poor sleep in Japanese graduate students. Sleep Biol. Rhythm. 2007, 5, 234–238. [Google Scholar] [CrossRef]
- Liu, D.; Kahathuduwa, C.; Vazsonyi, A.T. The Pittsburgh Sleep Quality Index (PSQI): Psychometric and clinical risk score applications among college students. Psychol. Assess. 2021, 33, 816. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Tsai, P.-S.; Wang, S.-Y.; Wang, M.-Y.; Su, C.-T.; Yang, T.-T.; Huang, C.-J.; Fang, S.-C. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual. Life Res. 2005, 14, 1943–1952. [Google Scholar] [CrossRef]
- Chen, Y.-H.; Chang, S.-P. Exercise Toward to Sleep Quality improvement. Tai Zhong Xue Yuan Ti Yu 2010, 6, 111–121. [Google Scholar] [CrossRef]
- Chang, S.-P. Relationships among Body Mass Index, Physical Fitness and Sleep Quality in Male University Students. Sport. Res. Rev. 2011, 115, 80–87. [Google Scholar] [CrossRef]
- Ohayon, M.M.; Roberts, R.E.; Zulley, J.; Smirne, S.; Priest, R.G. Prevalence and patterns of problematic sleep among older adolescents. J. Am. Acad. Child Adolesc. Psychiatry 2000, 39, 1549–1556. [Google Scholar] [CrossRef]
- Yang, C.-M.; Wu, C.-H.; Hsieh, M.-H.; Liu, M.-H.; Lu, F.-H. Coping with sleep disturbances among young adults: A survey of first-year college students in Taiwan. Behav. Med. 2003, 29, 133–138. [Google Scholar] [CrossRef]
- Gradisar, M.; Gardner, G.; Dohnt, H. Recent worldwide sleep patterns and problems during adolescence: A review and meta-analysis of age, region, and sleep. Sleep Med. 2011, 12, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Yang, Y.; Shi, T.; Song, Y.; Zhou, Y.; Zhang, Z.; Guo, Y.; Li, X.; Liu, Y.; Xu, G. Prevalence and demographic correlates of poor sleep quality among frontline health professionals in Liaoning Province, China during the COVID-19 outbreak. Front. Psychiatry 2020, 11, 520. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.-N.; Chang, Y.-Y.; Ho, H.-H.; Yen, L.-L. Sleep Problems in Adolescents. Formos. J. Med. 2012, 16, 72–83. [Google Scholar] [CrossRef]
- Lee, Y.J.; Cho, S.-J.; Cho, I.H.; Kim, S.J. Insufficient sleep and suicidality in adolescents. Sleep 2012, 35, 455–460. [Google Scholar] [CrossRef]
- Abel, T.; Havekes, R.; Saletin, J.M.; Walker, M.P. Sleep, plasticity and memory from molecules to whole-brain networks. Curr. Biol. 2013, 23, R774–R788. [Google Scholar] [CrossRef]
- Walsh, N.P.; Halson, S.L.; Sargent, C.; Roach, G.D.; Nédélec, M.; Gupta, L.; Leeder, J.; Fullagar, H.H.; Coutts, A.J.; Edwards, B.J. Sleep and the athlete: Narrative review and 2021 expert consensus recommendations. Br. J. Sport. Med. 2021, 55, 356–368. [Google Scholar] [CrossRef]
- Davey, S.; Davey, A.; Raghav, S.; Singh, J.; Singh, N.; Blanchio, A.; Przepiorkaa, A. Predictors and consequences of “Phubbing” among adolescents and youth in India: An impact evaluation study Sanjeev. J. Fam. Community Med. 2017, 24, 102–105. [Google Scholar] [CrossRef]
- Rabin, J.M.; Mehra, R.; Chen, E.; Ahmadi, R.; Jin, Y.; Day, C. Assessment of sleep health in collegiate athletes using the Athlete Sleep Screening Questionnaire. J. Clin. Sleep Med. 2020, 16, 1349–1356. [Google Scholar] [CrossRef]
- Curcio, G.; Ferrara, M.; De Gennaro, L. Sleep loss, learning capacity and academic performance. Sleep Med. Rev. 2006, 10, 323–337. [Google Scholar] [CrossRef]
- Short, M.A.; Gradisar, M.; Lack, L.C.; Wright, H.R. The impact of sleep on adolescent depressed mood, alertness and academic performance. J. Adolesc. 2013, 36, 1025–1033. [Google Scholar] [CrossRef]
- Chang, W.-L.; Ko, S.-H.; Chang, T.-H.; Hung, L.-C. Effect of Auricular Acupressure on Improving Sleep Quality in Nurses. J. Nurs. Healthc. Res. 2010, 6, 261–270. [Google Scholar] [CrossRef]
- Chiu, H.Y.; Chao, Y. Concept analysis: Sleep quality. Hu Li Za Zhi J. Nurs. 2010, 57, 106–111. [Google Scholar]
- Takano, M.; Matsukura, M.; Harada, K.; Wei, C.-N.; Ohmori, S.; Miyakita, T.; Miike, T.; Ueda, A. Behavior and lifestyle factors related to quality of life in junior high school students. Environ. Health Prev. Med. 2005, 10, 94–102. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wendel-Vos, G.; Schuit, A.J.; Tijhuis, M.; Kromhout, D. Leisure time physical activity and health-related quality of life: Cross-sectional and longitudinal associations. Qual. Life Res. 2004, 13, 667–677. [Google Scholar] [CrossRef]
- Bize, R.; Johnson, J.A.; Plotnikoff, R.C. Physical activity level and health-related quality of life in the general adult population: A systematic review. Prev. Med. 2007, 45, 401–415. [Google Scholar] [CrossRef]
- Prohaska, T.R.; Peters, K.E. Physical activity and cognitive functioning: Translating research to practice with a public health approach. Alzheimer’s Dement. 2007, 3, S58–S64. [Google Scholar] [CrossRef]
- Lu, J.; Tseng, H.; Tsai, Y. Assessment of health-related quality of life in Taiwan (I): Development and psychometric testing of SF-36 Taiwan version. Taiwan J. Public Health 2003, 22, 501–511. [Google Scholar] [CrossRef]
- Tseng, H.; Lu, J.; Tsai, Y. Assessment of health-related quality of life in Taiwan (II): Norming and validation of SF-36 Taiwan version. Taiwan J. Public Health 2003, 22, 512–518. [Google Scholar] [CrossRef][Green Version]
- Wang, H.-H.; Li, G.S.-F. A study of the Stage of Regular Exercise and Health-Related Quality of Life for Adult. Phys. Educ. J. 2004, 36, 1–15. [Google Scholar] [CrossRef]
- Abdel-Khalek, A.M. Quality of life, subjective well-being, and religiosity in Muslim college students. Qual. Life Res. 2010, 19, 1133–1143. [Google Scholar] [CrossRef]
- Schatz, B.R. National Surveys of population health: Big data analytics for mobile health monitors. Big Data 2015, 3, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Thelwall, M. Link Analysis: An Information Science Approach; Emerald Group Publishing Limited: Bradford, UK, 2004. [Google Scholar]
- Borodin, A.; Roberts, G.O.; Rosenthal, J.S.; Tsaparas, P. Link analysis ranking: Algorithms, theory, and experiments. ACM Trans. Internet Technol. (TOIT) 2005, 5, 231–297. [Google Scholar] [CrossRef]
- Almpanidis, G.; Kotropoulos, C.; Pitas, I. Combining text and link analysis for focused crawling—An application for vertical search engines. Inf. Syst. 2007, 32, 886–908. [Google Scholar] [CrossRef]
- Chen, G.; Liu, H.; Yu, L.; Wei, Q.; Zhang, X. A new approach to classification based on association rule mining. Decis. Support Syst. 2006, 42, 674–689. [Google Scholar] [CrossRef]
- Yeh, J.-Z.; Wei, C.-J.; Weng, S.-F.; Tsai, C.-Y.; Shih, J.-H.; Shih, C.-L.; Chiu, C.-H. Disease-specific health literacy, disease knowledge, and adherence behavior among patients with type 2 diabetes in Taiwan. BMC Public Health 2018, 18, 1062. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).