HVAC Control Systems for a Negative Air Pressure Isolation Room and Its Performance
Abstract
:1. Introduction
- An anteroom that operates as an airlock with interlocking doors; both doors must not open at the one time; the anteroom must be large enough to permit bed movement in and out of the isolation room if direct doors from the corridor to the isolation room are not provided.
- An alarm to be activated on the loss of differential pressure; time delay may be required to permit entry/exit from the isolation room.
- A clinical handwash basin with ‘hands free’ operation in the isolation room and the anteroom.
- An ensuite shower and toilet.
- Self-closing doors with interlocking doors to the anteroom
- 100% outside air ventilation (i.e., no return air permitted), with low-level exhaust ducts approximately 200 mm above floor level to discharge vertically to the outside air.
- Supply air ducts are to be independent of the building supply air system.
- For immunosuppressed and infectious patients, a high-efficiency particulate absorbing (HEPA) filtration system should be provided on the supply air ducting to protect the patient from unfiltered air.
- Exhaust air should be HEPA filtered and provided with UV irradiation.
- Provision of a pan/utensil sanitizer is optional. If provided, it should be located within the ensuite. Alternatively, disposables can be considered.
2. Materials and Methods
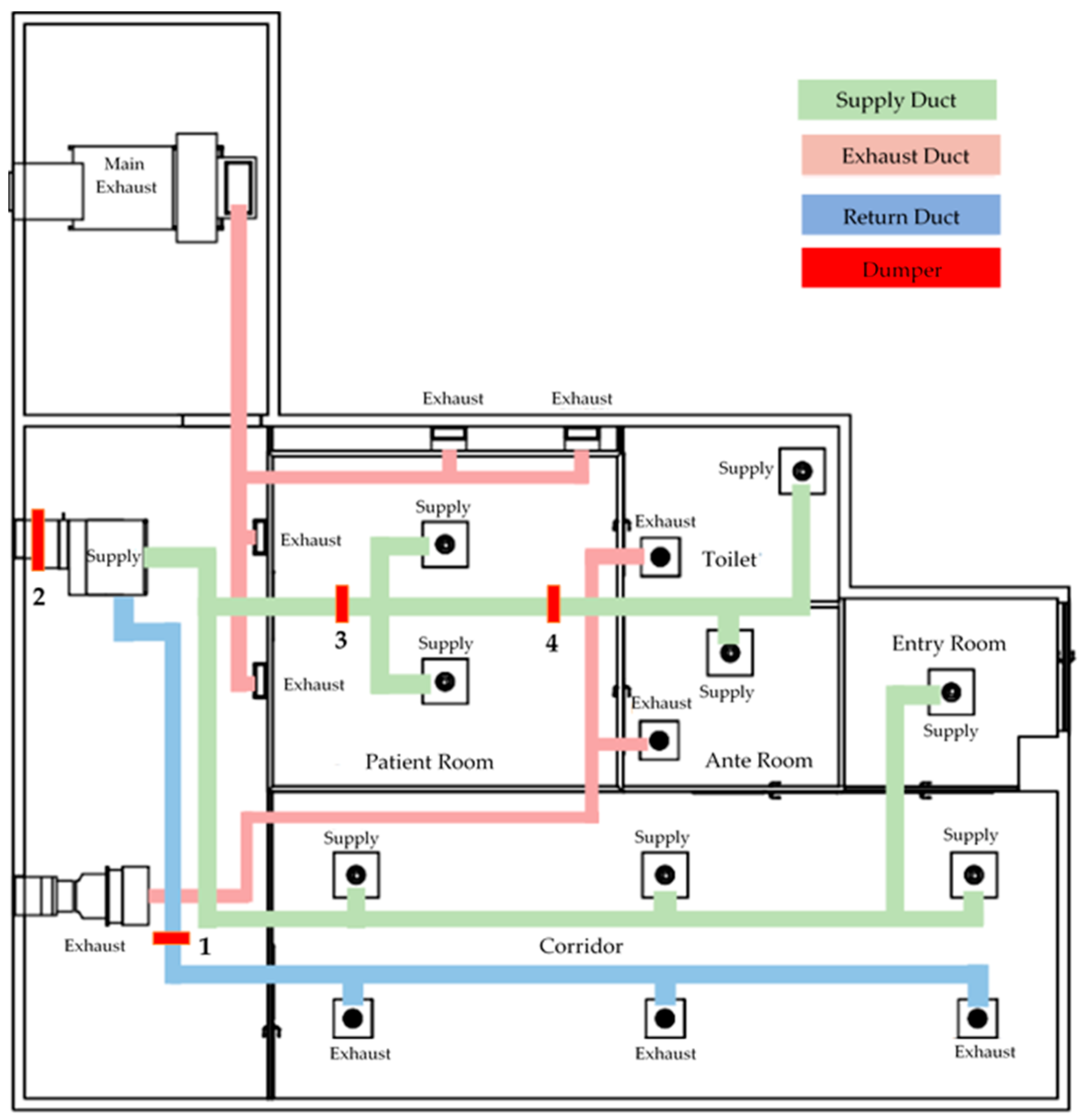
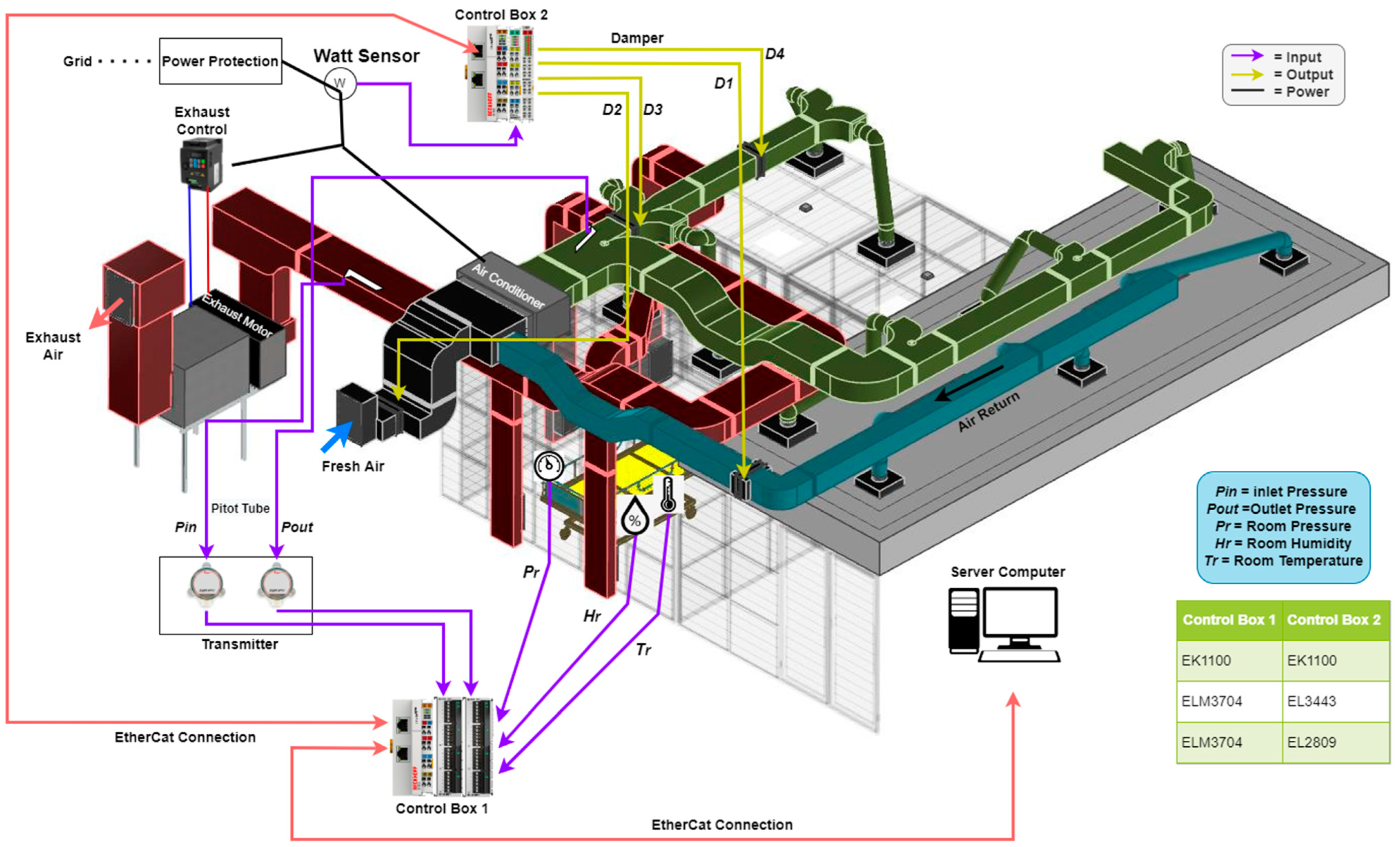
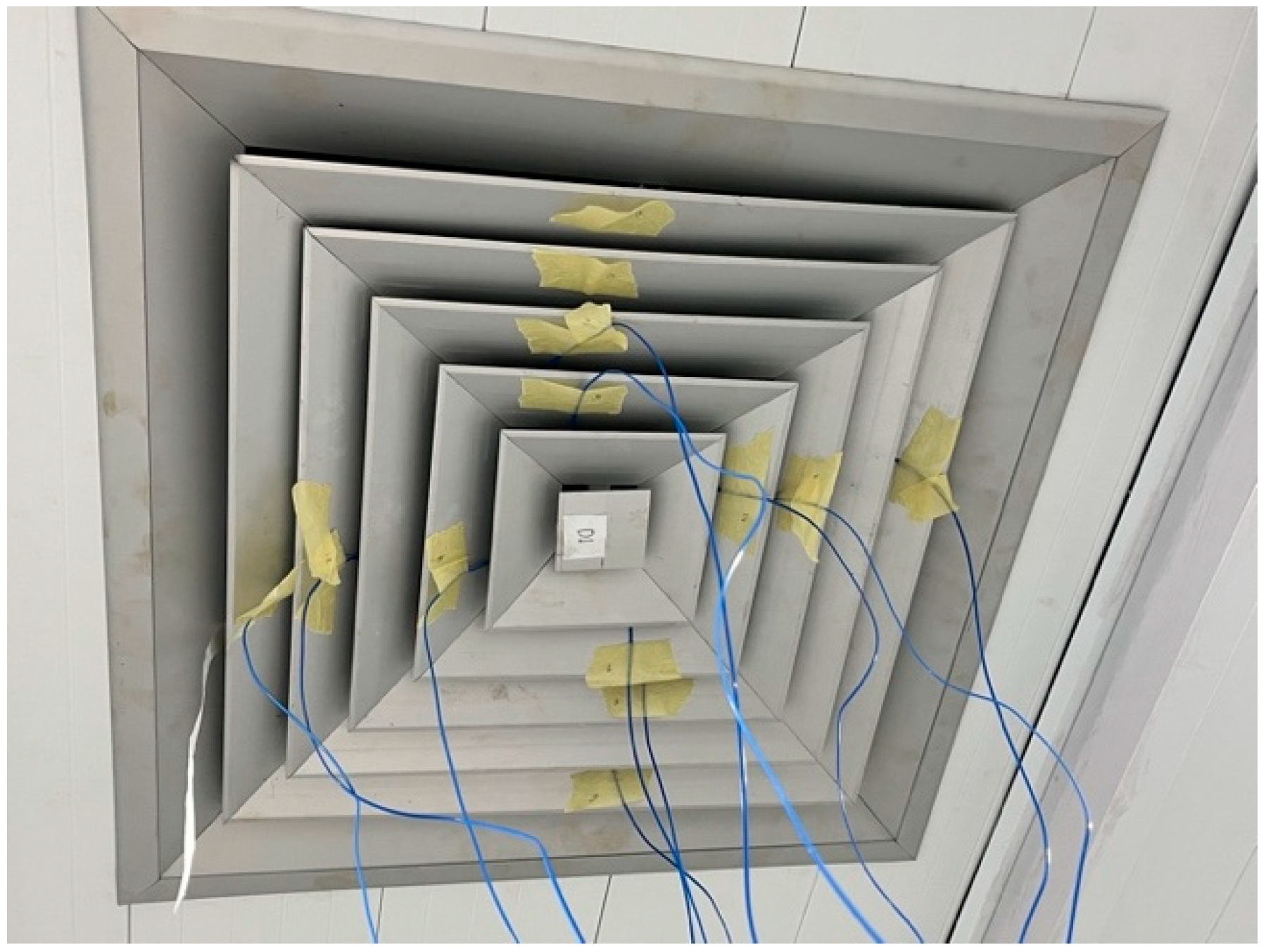
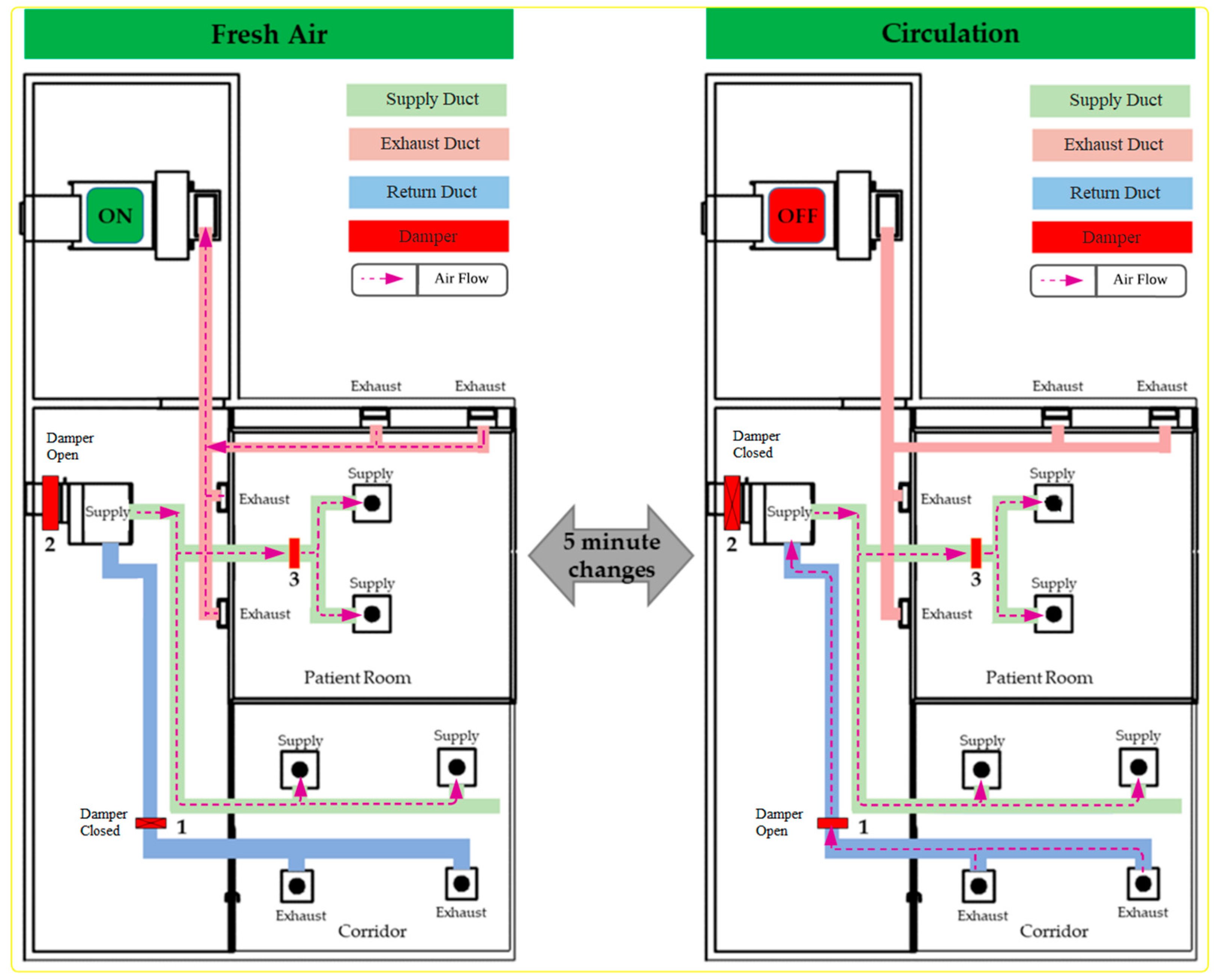
2.1. System Overview
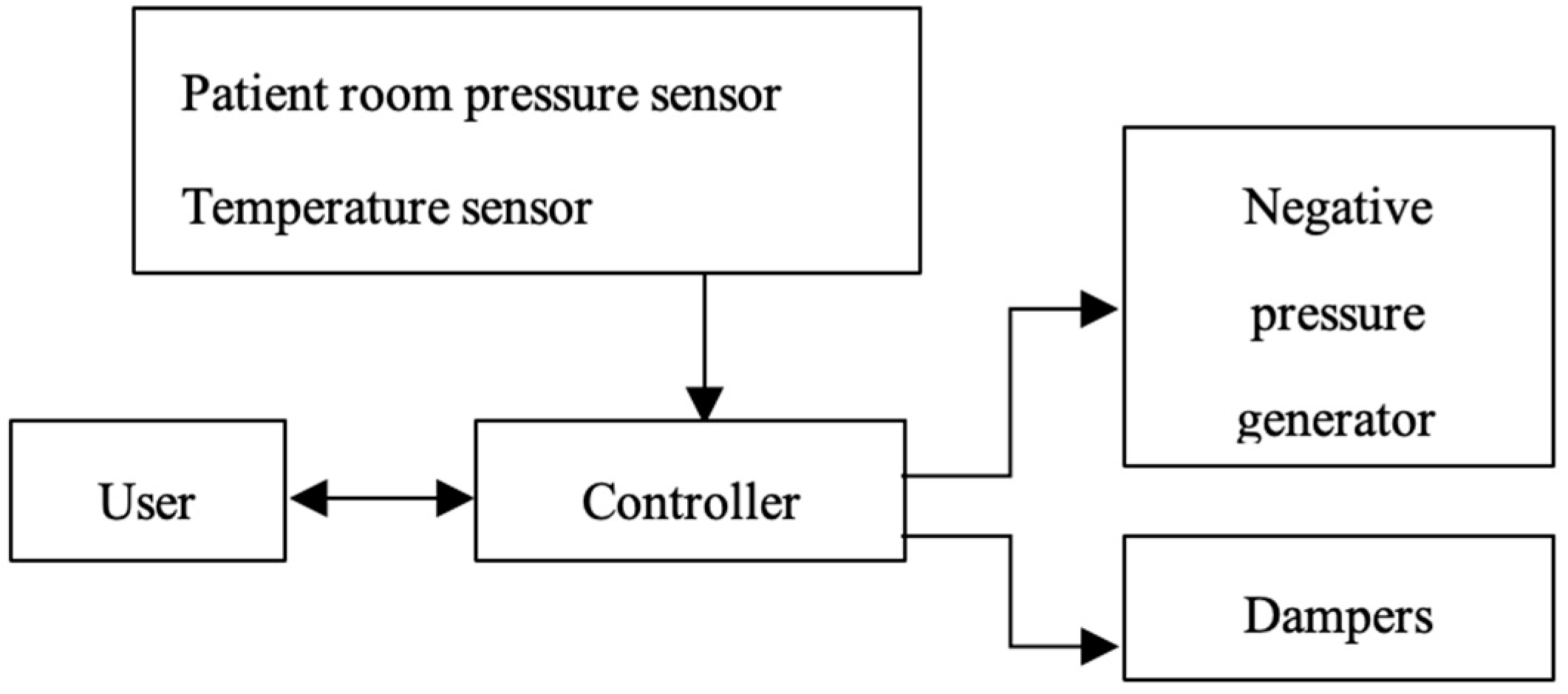
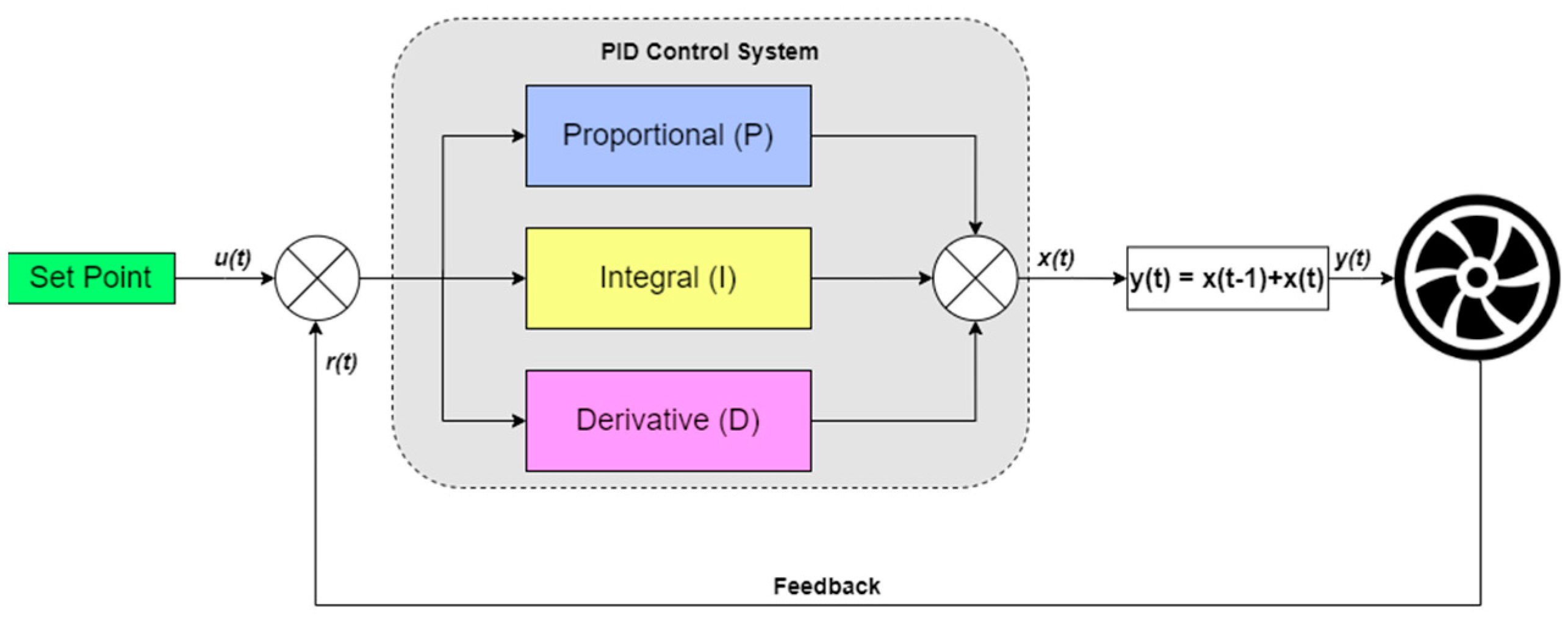
2.2. Control Strategy
3. Results and Discussion
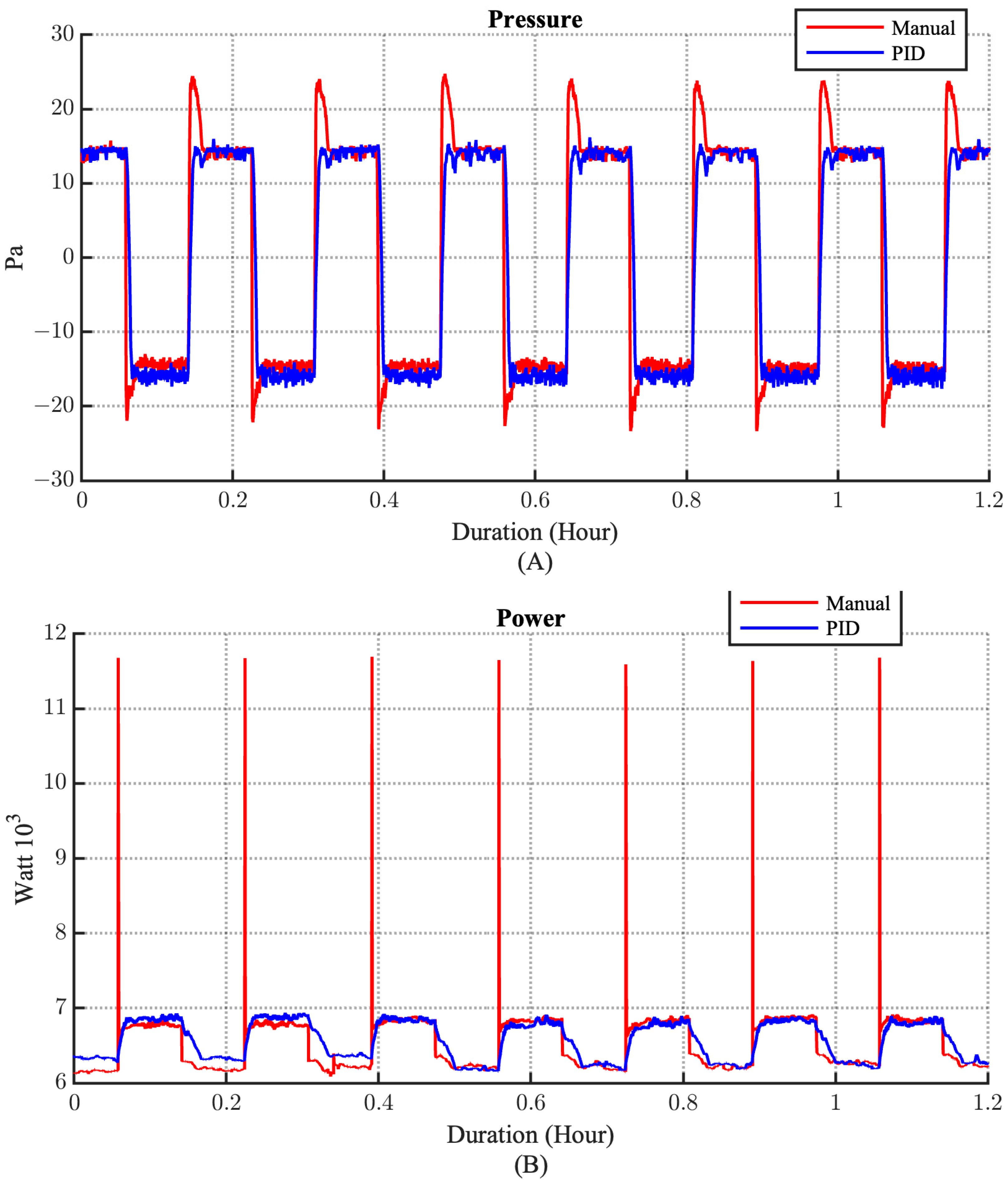
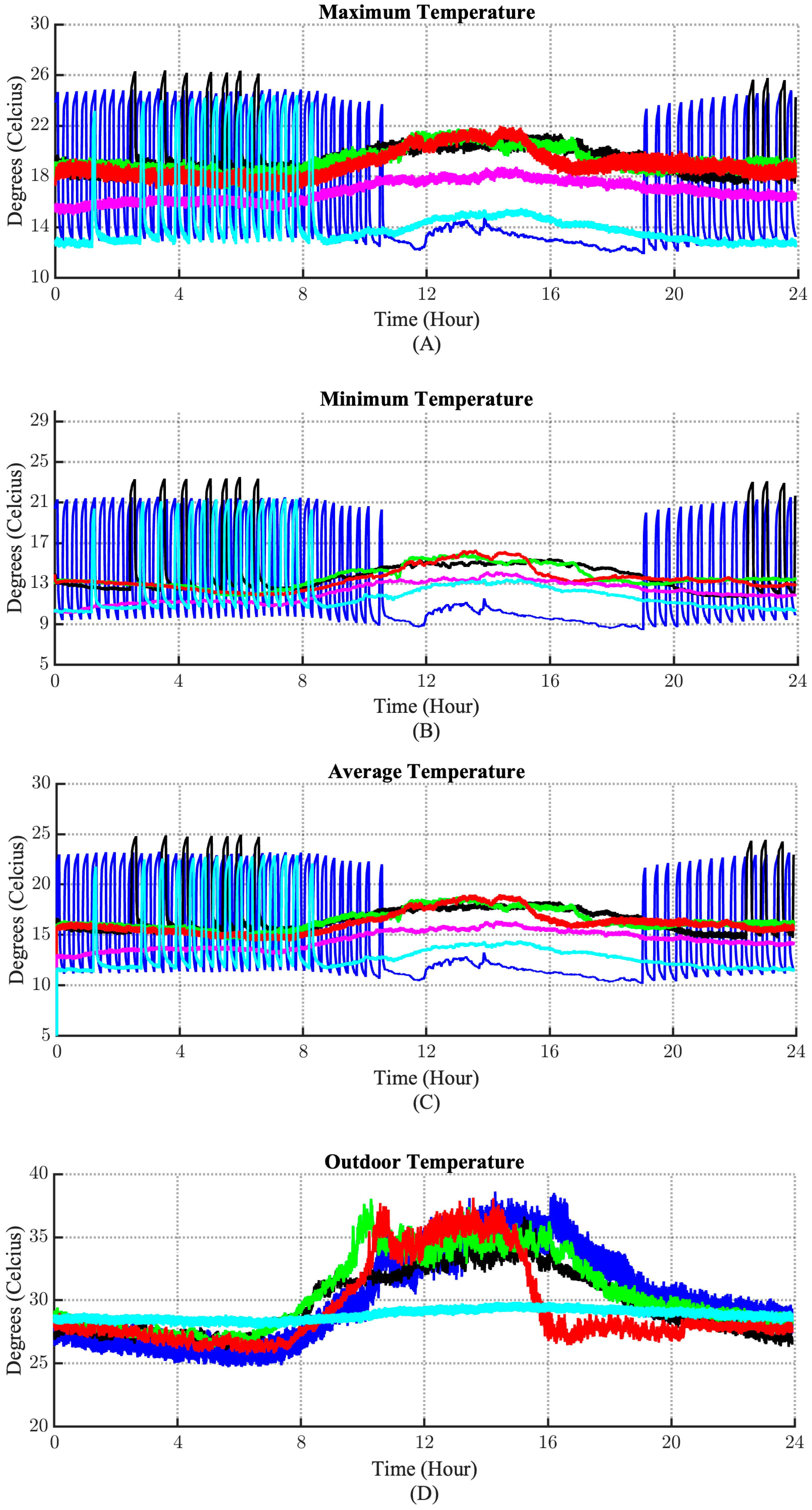
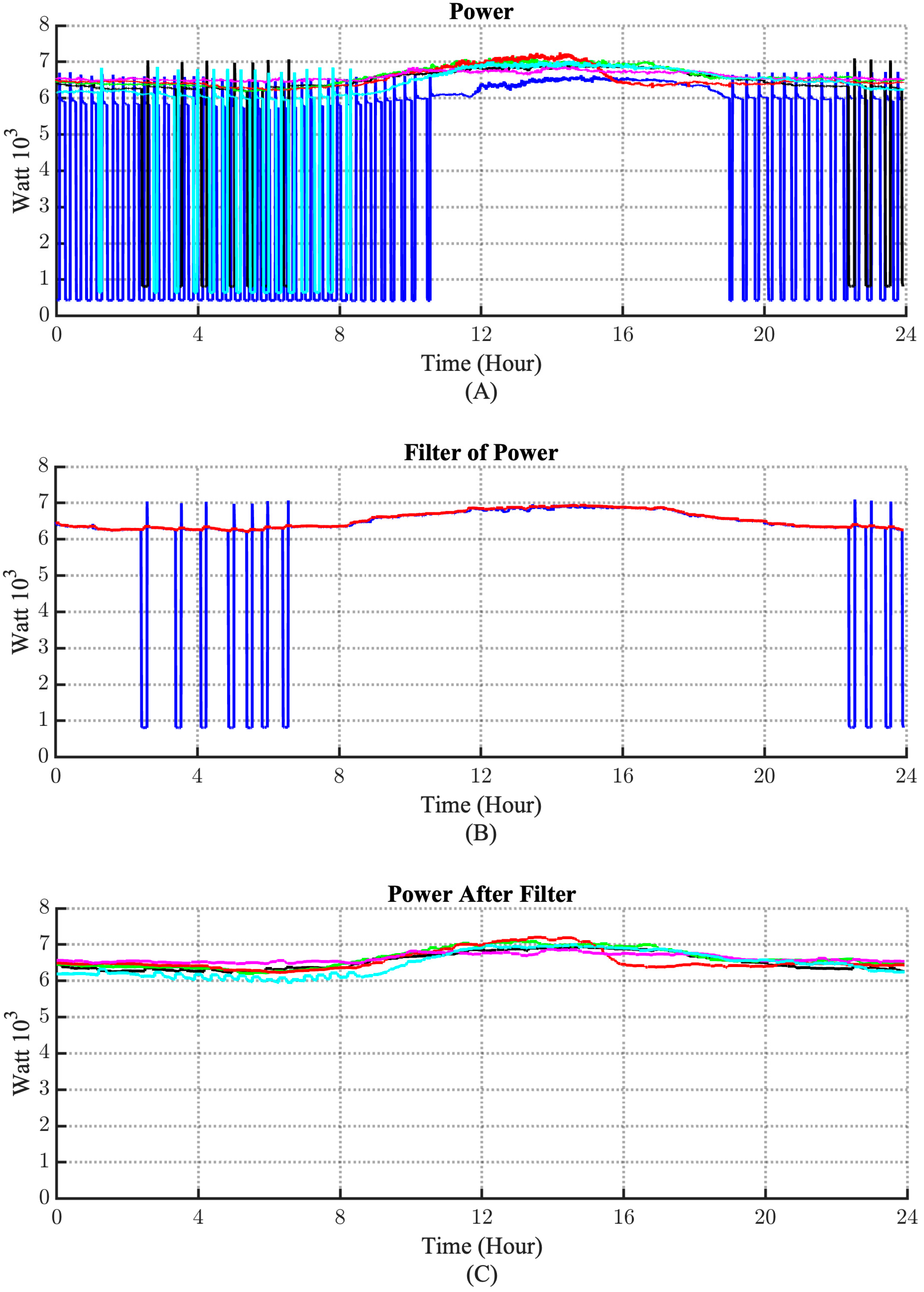
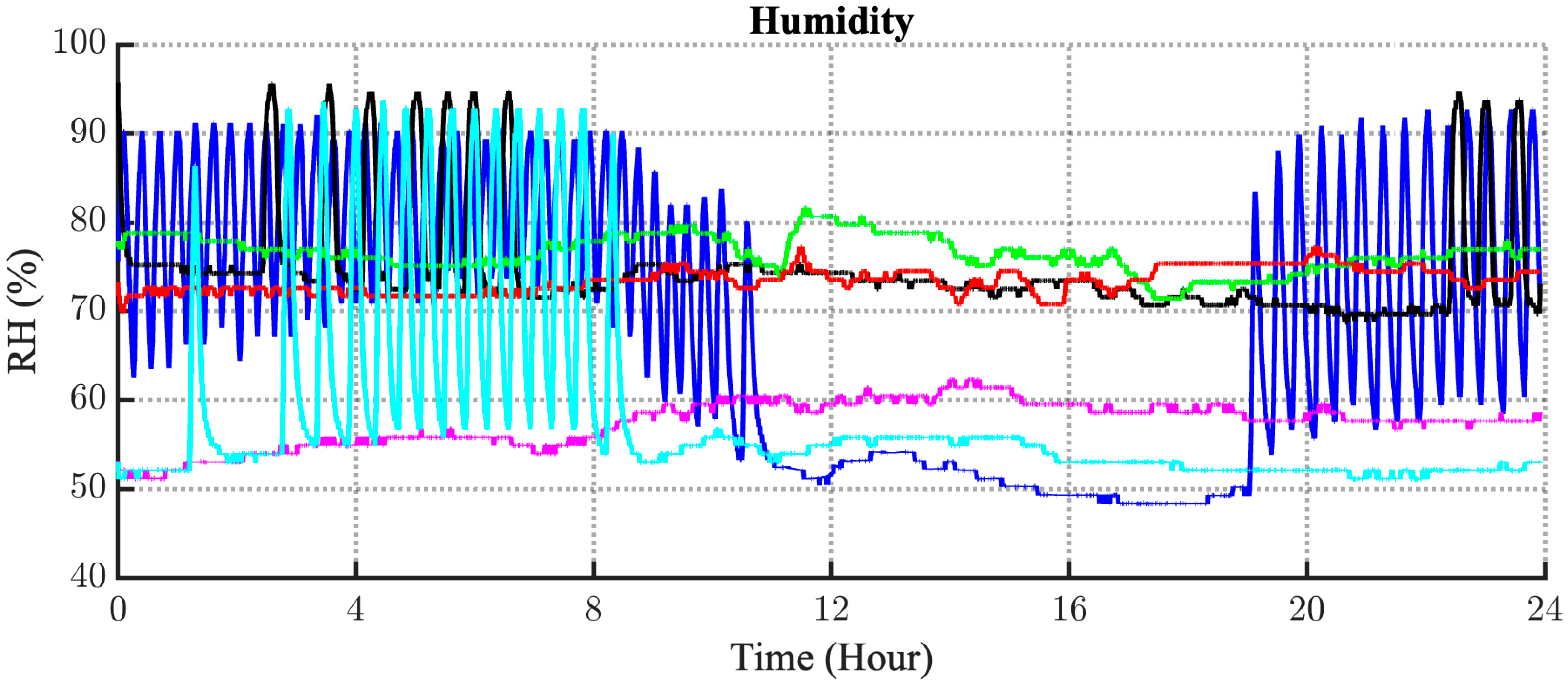
3.1. The Comparison of Control Strategy
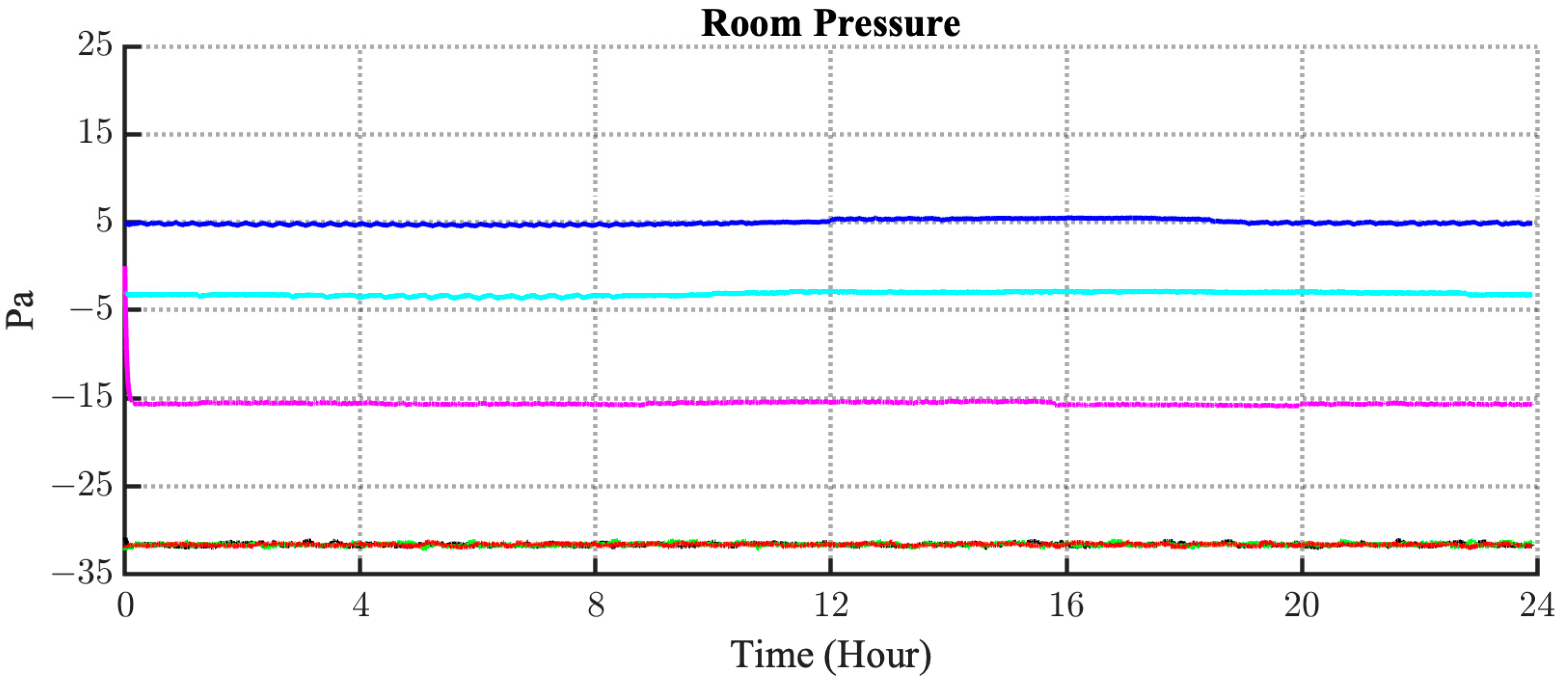
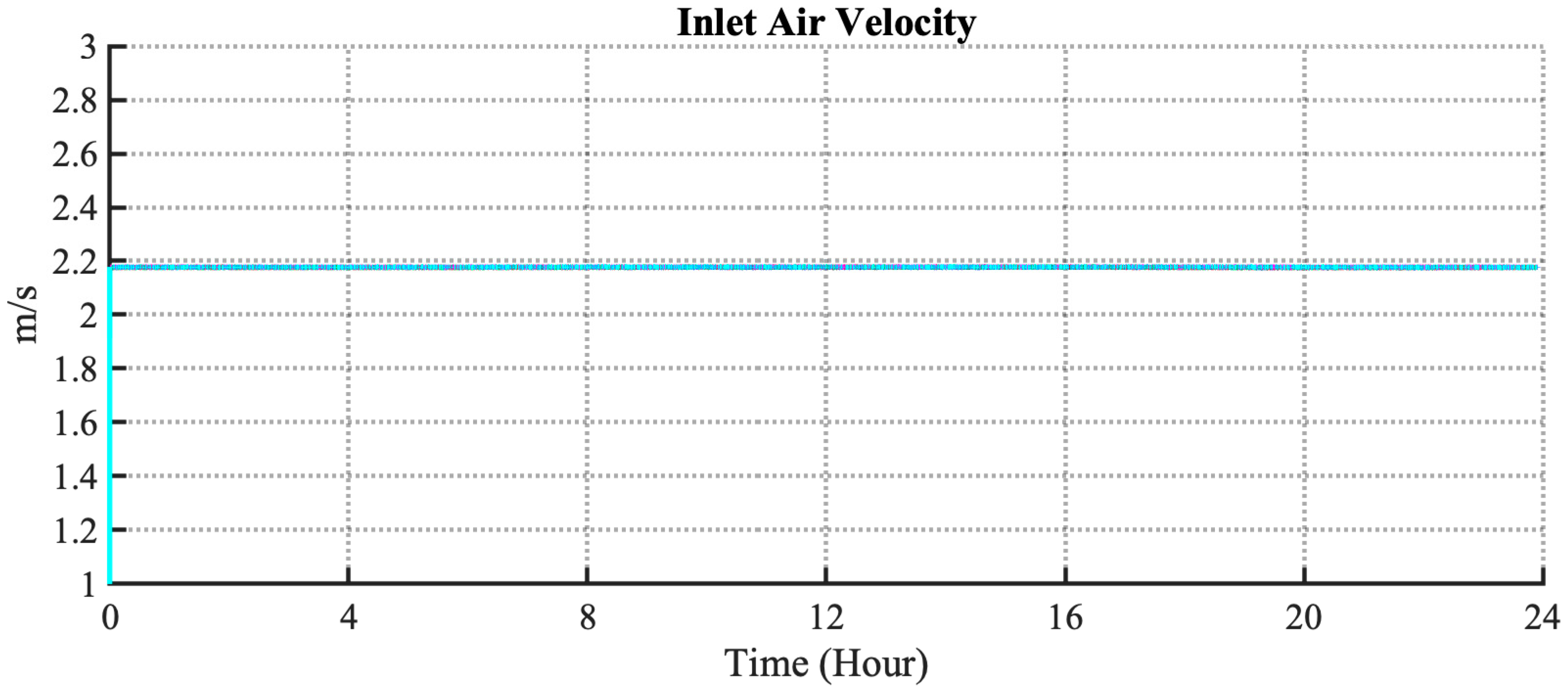
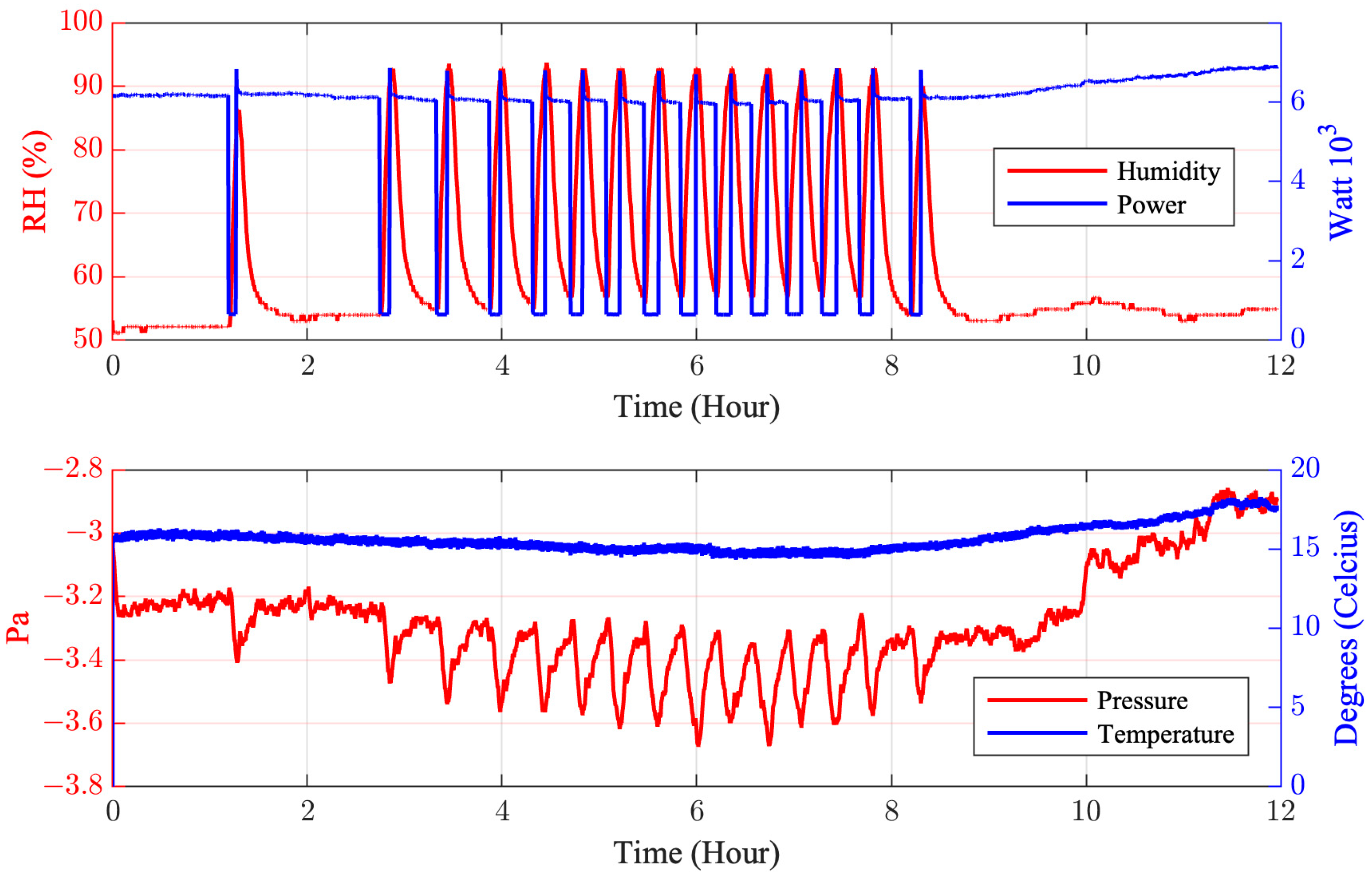
3.2. Performance Measurement of the Isolation Room
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Qian, H.; Zheng, X. Ventilation control for airborne transmission of human exhaled bio-aerosols in buildings. J. Thorac. Dis. 2018, 10, S2295–S2304. [Google Scholar] [CrossRef] [PubMed]
- Nourmohammadi, M.; Mirzaei, R.; Taban, E.; Yari, S. Effect of Ventilation System on Spread and Control of Infections (COVID-19) in Indoor Environments: Based on Current Studies. Asian Pac. J. Environ. Cancer 2020, 3, 55–58. [Google Scholar] [CrossRef]
- Heating, Ventilation and Air-Conditioning Systems in the Context of COVID-19: First Update. Available online: https://www.ecdc.europa.eu/en/publications-data/heating-ventilation-air-conditioning-systems-covid-19 (accessed on 3 August 2022).
- Santos, A.F.; Gaspar, P.D.; Hamandosh, A.; de Aguiar, E.B.; Filho, A.C.G.; de Souza, H.J.L. Best Practices on HVAC Design to Minimize the Risk of COVID-19 Infection within Indoor Environments. Braz. Arch. Biol. Technol. 2020, 63, 1–11. [Google Scholar] [CrossRef]
- Korea, S.; Byungseon, S.; Kim, P.D. Improved Ventilation System for Removal of Airborne Contamination in Airborne Infectious Isolation Rooms. 2019. Available online: www.ashrae.org (accessed on 3 August 2022).
- Kementerian kesehatan Republik Indonesia, Panduan Teknis Pelayanan Rumah Sakit Pada Masa Adaptasi. Kebiasaan Baru Pustaka, Badan Mutu Pelayanan Kesehatan. Available online: http://badanmutu.or.id/pustaka/ (accessed on 3 August 2022).
- Tahpi, Isolation Rooms. International Health Facility Guidelines. Available online: https://www.healthfacilityguidelines.com/GuidelineIndex/Index/Infection-Control (accessed on 3 August 2022).
- Weng, C.L.; Kau, L.J. Planning and design of a full-outer-air-intake natural air-conditioning system for medical negative pressure isolation wards. J. Healthc. Eng. 2021, 2021, 8872167. [Google Scholar] [CrossRef] [PubMed]
- Saran, S.; Gurjar, M. Baronia, A.; Sivapurapu, V.; Ghosh, P.S.; Raju, G.M.; Maurya, I. Heating, ventilation and air conditioning (HVAC) in intensive care unit. Crit. Care 2020, 24, 194. [Google Scholar] [CrossRef] [PubMed]
- Zheng, W.; Hu, J.; Wang, Z.; Li, J.; Fu, Z.; Li, H.; Jurasz, J.; Chou, S.K.; Yan, J. COVID-19 Impact on Operation and Energy Consumption of Heating, Ventilation and Air-Conditioning (HVAC) Systems. Adv. Appl. Energy 2021, 3, 100040. [Google Scholar] [CrossRef]
- Sporr, A.; Zucker, G.; Hofmann, R. Automated HVAC Control Creation Based on Building Information Modeling (BIM): Ventilation System. IEEE Access 2019, 7, 74747–74758. [Google Scholar] [CrossRef]
- Anuntasethakul, C.; Banjerdpongchai, D. Design of Supervisory Model Predictive Control for Building HVAC System with Consideration of Peak-Load Shaving and Thermal Comfort. IEEE Access 2021, 9, 41066–41081. [Google Scholar] [CrossRef]
- Jacob, S.; Yadav, S.S.; Sikarwar, B.S. Design and simulation of isolation room for a hospital. In Lecture Notes in Mechanical Engineering; Springer: Singapore, 2019; pp. 75–93. [Google Scholar] [CrossRef]
- Khankari, K. Technical Feature Patient Room HVAC. 2016. Available online: www.ashrae.org (accessed on 3 August 2022).
- Cho, J. Investigation on the contaminant distribution with improved ventilation system in hospital isolation rooms: Effect of supply and exhaust air diffuser configurations. Appl. Therm. Eng. 2019, 148, 208–218. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Chaerasari, C.; Rakshit, D.; Permana, I. Kusnandar, Performance Improvement of a Negative-Pressurized Isolation Room for Infection Control. Healthcare 2021, 9, 1081. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharya, A.; Ghahramani, A.; Mousavi, E. The effect of door opening on air-mixing in a positively pressurized room: Implications for operating room air management during the COVID outbreak. J. Build. Eng. 2021, 44, 102900. [Google Scholar] [CrossRef]
- Ezzeddine, W.; Schutz, J.; Rezg, N. Pitot sensor air flow measurement accuracy: Causal modelling and failure risk analysis. Flow Meas. Instrum. 2019, 65, 7–15. [Google Scholar] [CrossRef]
- Escobar, L.M.; Aguilar, J.; Garces-Jimenez, A.; de Mesa, J.A.G.; Gomez-Pulido, J.M. Advanced fuzzy-logic-based context-driven control for HVAC management systems in buildings. IEEE Access 2020, 8, 16111–16126. [Google Scholar] [CrossRef]
- Tamburrano, P.; de Palma, P.; Plummer, A.R.; Distaso, E.; Amirante, R. Simulink Modelling for Simulating Intensive Care Mechanical Ventilators. E3S Web Conf. 2020, 197, 07007. [Google Scholar] [CrossRef]
- Khalid, W.; Zaki, S.A.; Rijal, H.B.; Yakub, F. Investigation of comfort temperature and thermal adaptation for patients and visitors in Malaysian hospitals. Energy Build 2019, 183, 484–499. [Google Scholar] [CrossRef]
- Moving Mean-MATLAB Movmean. Available online: https://www.mathworks.com/help/matlab/ref/movmean.html#d123e948000 (accessed on 25 August 2022).
- Moving Maximum-MATLAB Movmax. Available online: https://www.mathworks.com/help/matlab/ref/movmax.html#d123e947144 (accessed on 25 August 2022).


| Pressure Differential | Country |
|---|---|
| More than 2.5 Pa | USA, Hongkong, South Korea |
| More than 5 Pa | United Kingdom, Norway |
| More than 15 Pa | Australia |
| 15 Pa | Indonesia |
| S1 | S2 | S3 | S4 | S5 | S6 | |
|---|---|---|---|---|---|---|
| Date (2022) | 18.06 | 19.06 | 20.06 | 21.06 | 5.07 | 7.07 |
| Regulated room pressure (Pa) | Negative pressure regulator is not activated | −30 | −15 | −3 | ||
| AC temperature (°C) | 24 ± 2 | |||||
| AC fan speed | Auto | |||||
| Bed head exhaust | Open | Open | Closed | Open | ||
| Bed foot exhaust | Closed | Open | ||||
| Damper 1, Damper 2, Damper 3, Damper 4 | Open | |||||
| S1 | S2 | S3 | S4 | S5 | S6 | |
|---|---|---|---|---|---|---|
| kWh (before filter) | 105.29 | 147.17 | 157.99 | 156.39 | 158.02 | 143.49 |
| Difference (%) (before filter) | Baseline | 39.78 | 50.05 | 48.53 | 50.07 | 36.27 |
| kWh (after filter) | 156.41 | 158.54 | 156.96 | 158.53 | 154.86 | |
| Difference (%) (after filter) | Not applicable | Baseline | 1.36 | 0.35 | 1.35 | 0.99 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hamdani, H.; Sabri, F.S.; Harapan, H.; Syukri, M.; Razali, R.; Kurniawan, R.; Irwansyah, I.; Sofyan, S.E.; Mahlia, T.M.I.; Rizal, S. HVAC Control Systems for a Negative Air Pressure Isolation Room and Its Performance. Sustainability 2022, 14, 11537. https://doi.org/10.3390/su141811537
Hamdani H, Sabri FS, Harapan H, Syukri M, Razali R, Kurniawan R, Irwansyah I, Sofyan SE, Mahlia TMI, Rizal S. HVAC Control Systems for a Negative Air Pressure Isolation Room and Its Performance. Sustainability. 2022; 14(18):11537. https://doi.org/10.3390/su141811537
Chicago/Turabian StyleHamdani, Hamdani, Fajar Salamul Sabri, Harapan Harapan, Maimun Syukri, Razali Razali, Rudi Kurniawan, Irwansyah Irwansyah, Sarwo Edhy Sofyan, Teuku Meurah Indra Mahlia, and Samsul Rizal. 2022. "HVAC Control Systems for a Negative Air Pressure Isolation Room and Its Performance" Sustainability 14, no. 18: 11537. https://doi.org/10.3390/su141811537
APA StyleHamdani, H., Sabri, F. S., Harapan, H., Syukri, M., Razali, R., Kurniawan, R., Irwansyah, I., Sofyan, S. E., Mahlia, T. M. I., & Rizal, S. (2022). HVAC Control Systems for a Negative Air Pressure Isolation Room and Its Performance. Sustainability, 14(18), 11537. https://doi.org/10.3390/su141811537









