Analysis of Hospital’s Emergency and Disaster Preparedness Using Hospital Safety Index in Indonesia
Abstract
1. Introduction
2. Literature Review
2.1. Overview of Study Area
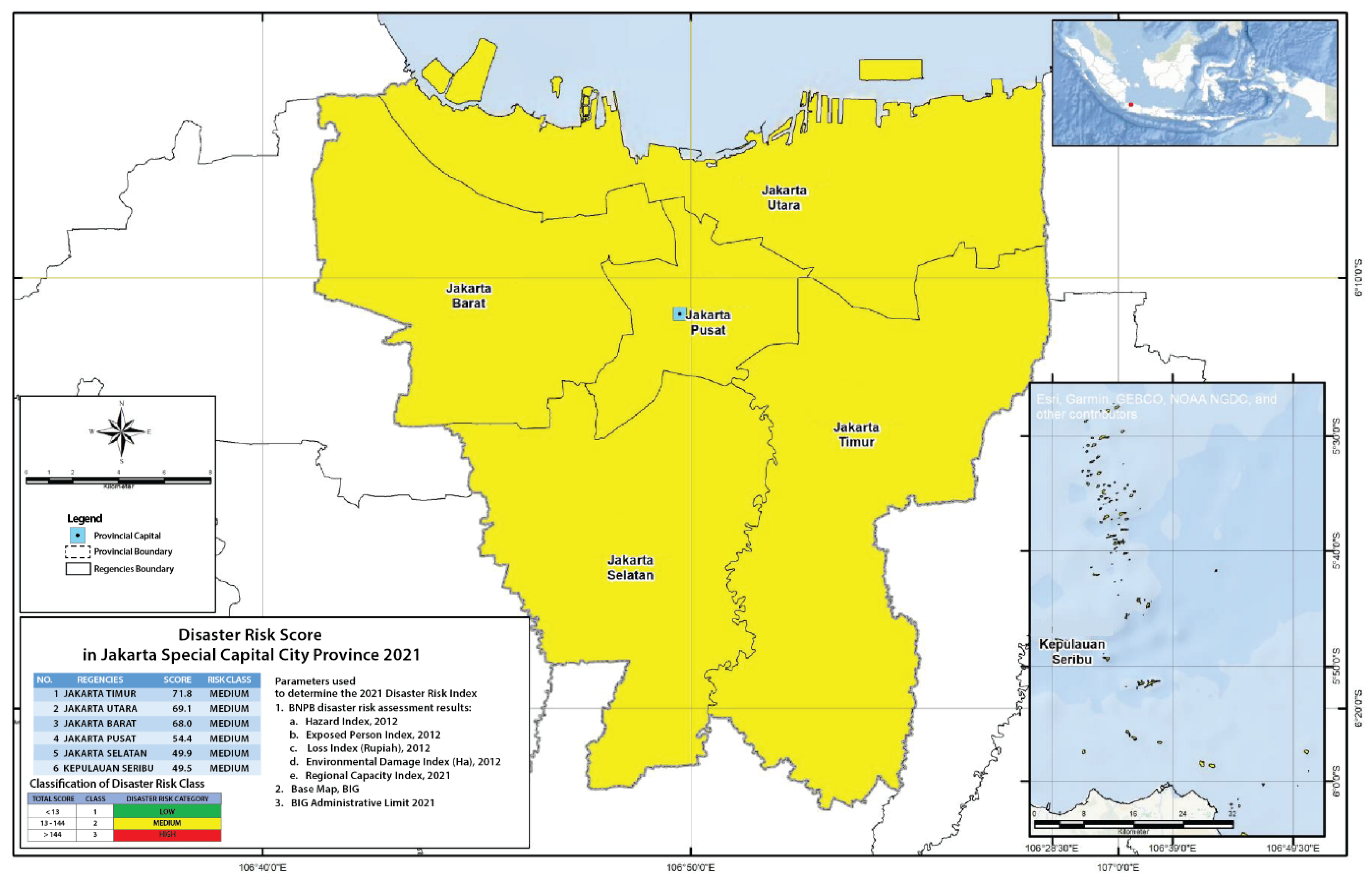
2.1.1. DKI Jakarta Province
2.1.2. West Java Province
2.1.3. Yogyakarta Special Regions Province
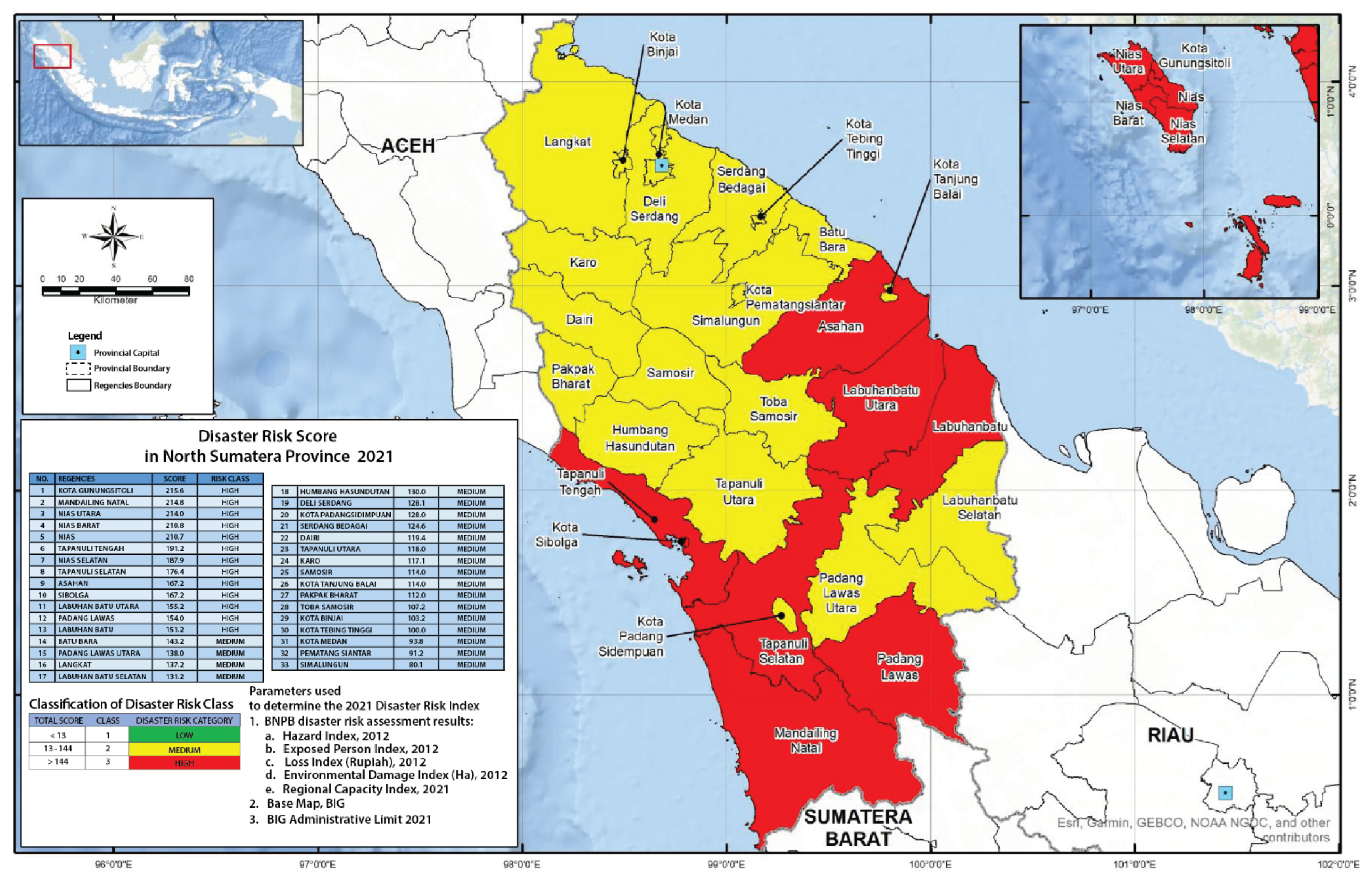
2.1.4. North Sumatera Province
2.2. Hospital Safety Index for Evaluating Hospital Preparedness
2.2.1. Module 1 (Potential Hazard and Disaster)
2.2.2. Module 2 (Structural Safety)
2.2.3. Module 3 (Non-Structural Safety)
2.2.4. Module 4 (Emergency and Disaster Management)
3. Materials and Methods
3.1. Data Collection and Sampling
3.2. Data Analysis, Weighting, and Score Calculation
- Category A (hospital safety index of 0.66–1.00)
- Category B (hospital safety index is 0.36–0.65)
- Category C (hospital safety index is 0.00–0.35)
4. Results
4.1. Potential Hazards
4.2. Structural Safety Assessment
4.3. Non-Structural Safety Assessment
4.4. Disaster and Emergency Management
4.5. Overall Hospital Safety Index (HSI)
4.6. Comparison of HSI Scores in All Provinces
5. Discussion
5.1. Potential Hazards
5.2. Structural Safety
5.3. Non-Structural Safety
5.4. Disaster and Emergency Management
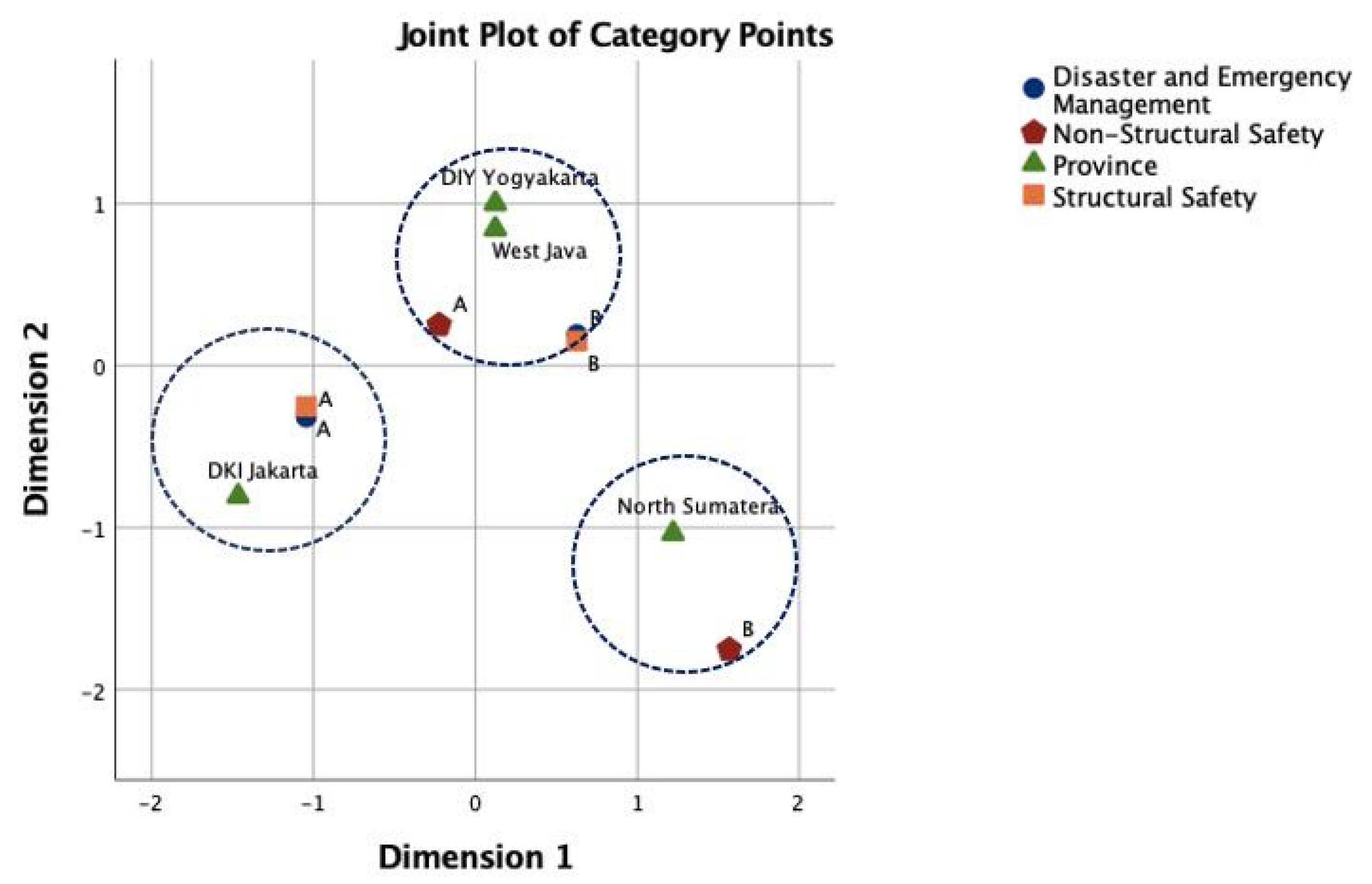
5.5. Multiple Correspondence Analysis
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Badan Pusat Statistik. Berita Resmi Statistik. Available online: https://www.bps.go.id/brs.html (accessed on 20 September 2021).
- BNPB. IRBI Indeks Risiko Bencana Indonesia Tahun 2020. Available online: https://inarisk.bnpb.go.id/pdf/BUKU%20IRBI%202020%20KP.pdf (accessed on 15 September 2021).
- UNDRR. Disaster Risk Reduction in Indonesia: Status Report 2020. Available online: https://reliefweb.int/report/indonesia/disaster-risk-reduction-indonesia-status-report-2020 (accessed on 17 September 2021).
- BNPB. IRBI Indeks Risiko Bencana Indonesia Tahun 2021. Available online: https://inarisk.bnpb.go.id/pdf/BUKU%20IRBI%202021%20(PDF).pdf (accessed on 15 September 2021).
- BNPB. Bencana Indonesia 2020. Available online: https://bnpb.go.id/infografis/infografis-bencana-indonesia-2020 (accessed on 1 November 2021).
- Lestari, F.; Hasbullah, T.; Haryanto, B.; Ronoatmodjo, S.; Purwana, R.; Trihandini, I.; Utomo, B.; Pratomo, H.; Wiweko, B.; Kasali, R.; et al. Indonesia’s Experience in COVID-19 Control Period January–July 2020; BNPB: Jakarta, Indonesia, 2020. [Google Scholar]
- COVID19.go.id. Peta Sebaran COVID-19 di Indonesia. Available online: https://covid19.go.id/peta-sebaran (accessed on 16 September 2021).
- World Health Organization & Pan American Health Organization. Hospital Safety Index: Guide for Evaluators, 2nd ed.; World Health Organization: Geneva, Switzerland, 2015; Available online: Https://Apps.Who.Int/Iris/Handle/10665/258966 (accessed on 1 February 2022).
- UNISDR. Hyogo Framework for Action 2005–2015. Encycl. Earth Sci. Ser. 2005, 508–516. [Google Scholar] [CrossRef]
- UNISDR. Sendai Framework for Disaster Risk Reduction 2015–2030. 2015. Available online: https://www.undrr.org/publication/sendai-framework-disaster-risk-reduction-2015-2030 (accessed on 27 September 2021).
- Sunindijo, R.Y.; Lestari, F.; Wijaya, O. Hospital safety index: Assessing the readiness and resiliency of hospitals in Indonesia. Facilities 2019, 38, 39–51. [Google Scholar] [CrossRef]
- Firdausi, N.; Lestari, F.; Ismiyati, A. Disaster Preparedness Analysis of Public Health Centers in DKI Jakarta Province in 2020. Int. J. Saf. Secur. Eng. 2021, 11, 91–99. [Google Scholar] [CrossRef]
- Kompas. Gempa Majene, RS Mitra Manakkara Ambruk, 6 Pasien dan Keluarganya Terjebak di Reruntuhan. Available online: https://regional.kompas.com/read/2021/01/15/08304201/gempa-majene-rs-mitra-manakkara-ambruk-6-pasien-dan-keluarganya-terjebak-di?page=all (accessed on 12 November 2021).
- Djalante, R.; Lassa, J.; Setiamarga, D.; Sudjatma, A.; Indrawan, M.; Haryanto, B.; Mahfud, C.; Sinapoy, M.S.; Djalante, S.; Rafliana, I.; et al. Review and analysis of current responses to COVID-19 in Indonesia: Period of January to March 2020. Prog. Disaster Sci. 2020, 6, 100091. [Google Scholar] [CrossRef] [PubMed]
- Mahayana, F.S.; Suryawati, C.; Agushybana, F. Penanganan Pasien COVID-19 Pada Rumah Sakit di Indonesia. J. Kesehat. 2020, 8, 162–170. [Google Scholar] [CrossRef]
- Kompas. Rumah Sakit Penuh, RSD Wisma Atlet Pun Harus Antre untuk Rujuk Pasien COVID-19 Gejala Berat. Available online: https://megapolitan.kompas.com/read/2021/01/04/15562311/rumah-sakit-penuh-rsd-wisma-atlet-pun-harus-antre-untuk-rujuk-pasien (accessed on 10 September 2021).
- COVID-19 Satgas. Presiden Jokowi Doring APT Cipatakan Resilensi Pandemi COVID-19. Available online: https://covid19.go.id/artikel/2020/04/14/presiden-jokowi-dorong-apt-ciptakan-resiliensi-pandemi-covid-19-dan-resiliensi-untuk-penguatan-ekonomi (accessed on 16 September 2021).
- Paramitasari, D. Public Health and Disaster Risk Reduction: Understanding Similarities and Divergences in Jakarta, Indonesia; The University of Auckland: Auckland, New Zealand, 2019. [Google Scholar]
- Laily, M. Hospital Readiness Assessment for Disasters Using the Hospital Safety Index in Severalc Accredited Hospitals in Yogyakarta Province. J. Med. Dan Manaj. Rumah Sakit 2020, 9, 135–145. [Google Scholar] [CrossRef]
- Aiello, A.; Pecce, M.; di Sarno, L.; Perrone, D.; Rossi, F. A Safety Index for Hospital Buildings. Disaster Adv. 2012, 5, 4. [Google Scholar]
- Adini, B.; Goldberg, A.; Laor, D.; Cohen, R.; Zadok, R.; Bar-Dayan, Y. Assessing Levels of Hospital Emergency Preparedness. Prehosp. Disaster Med. 2006, 21, 451–457. [Google Scholar] [CrossRef]
- Lazar, E.J.; Cagliuso, N.V.; Gebbie, K.M. Are We Ready and How Do We Know? The Urgent Need for Performance Metrics in Hospital Emergency Management. Disaster Med. Public Health Prep. 2009, 3, 57–60. [Google Scholar] [CrossRef]
- Top, M.; Gider, Ö.; Tas, Y. An Investigation of Hospital Disaster Preparedness in Turkey. J. Homel. Secur. Emerg. Manag. 2011, 7, 15. [Google Scholar] [CrossRef]
- Higgins, W.; Wainright, C.; Lu, N.; Carrico, R. Assessing hospital preparedness using an instrument based on the Mass Casualty Disaster Plan Checklist: Results of a statewide survey. Am. J. Infect. Control 2004, 32, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Kaji, A.H.; Lewis, R.J. Hospital Disaster Preparedness in Los Angeles County. Acad. Emerg. Med. 2006, 13, 1198–1203. [Google Scholar] [CrossRef] [PubMed]
- Kaji, A.H.; Langford, V.; Lewis, R.J. Assessing Hospital Disaster Preparedness: A Comparison of an On-Site Survey, Directly Observed Drill Performance, and Video Analysis of Teamwork. Ann. Emerg. Med. 2008, 52, 195–201.e12. [Google Scholar] [CrossRef]
- Kollek, D.; Cwinn, A.A. Hospital Emergency Readiness Overview Study. Prehosp. Disaster Med. 2011, 26, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Ismiyati, A.; Lestari, F. Analysis on Emergency and Disaster Preparedness Level of Hospitality Industry in Palu and Gorontalo Cities. Int. J. Saf. Secur. Eng. 2020, 10, 671–677. [Google Scholar] [CrossRef]
- Mulyasari, F.; Inoue, S.; Prashar, S.; Isayama, K.; Basu, M.; Srivastava, N.; Shaw, R. Disaster preparedness: Looking through the lens of hospitals in Japan. Int. J. Disaster Risk Sci. 2013, 4, 89–100. [Google Scholar] [CrossRef]
- Zoraster, R.M. Barriers to Disaster Coordination: Health Sector Coordination in Banda Aceh following the South Asia Tsunami. Prehosp. Disaster Med. 2006, 21, S13–S18. [Google Scholar] [CrossRef]
- Mojtahedi, M.; Sunindijo, R.; Lestari, F.; Suparni; Wijaya, O. Developing Hospital Emergency and Disaster Management Index Using TOPSIS Method. Sustainability 2021, 13, 5213. [Google Scholar] [CrossRef]
- Suparni; Lestari, F.; Darmawan, E.S.; Modjo, R.; Dane, S. Are Indonesian Hospitals Ready to Response to Disaster? Hospital Disaster Preparedness in West Java Province. J. Res. Med. Dent. Sci. 2020, 8, 4. [Google Scholar]
- Alkhalil, N.A.; Evaluation, S.M. Analysis of Hospital Disaster Preparedness in Jeddah. Health 2014, 6, 2668–2687. [Google Scholar] [CrossRef]
- Lestari, F.; Paramitasari, D.; Kadir, A.; Firdausi, N.A.; Fatmah; Yani Hamid, A.; Suparni; EL-Matury, H.J.; Wijaya, O.; Ismiyati, A. The Application of Hospital Safety Index for Analyzing Primary Healthcare Center (PHC) Disaster and Emergency Preparedness. Sustainability 2022, 14, 1488. [Google Scholar] [CrossRef]
- Yazdani, M.; Mojtahedi, M.; Loosemore, M.; Sanderson, D.; Dixit, V. Hospital Evacuation Modelling: A Critical Literature Review on Current Knowledge and Research Gaps. Int. J. Disaster Risk Reduct. 2021, 66, 102627. [Google Scholar] [CrossRef]
- Aghapour, A.H.; Yazdani, M.; Jolai, F.; Mojtahedi, M. Capacity Planning and Reconfiguration for Disaster-Resilient Health Infrastructure. J. Build. Eng. 2019, 26, 100853. [Google Scholar] [CrossRef]
- BBC. Iraq Hospital Fire: Protests as COVID Ward Blaze Kills at Least 92. BBC. July 2021. Available online: https://www.bbc.com/news/world-middle-east-57814954 (accessed on 11 September 2021).
- Rasheed, A.; Al-Saih, M. Anger Mounts after 92 Die in Fire on Iraq COVID Ward. Reuters 2021. 2021. Available online: https://www.reuters.com/world/middle-east/deaths-iraqs-coronavirus-hospital-fire-rise-64-ina-2021-07-13/ (accessed on 12 November 2021).
- Indonesia National Standard Hospital Accreditation. Indonesia National Standard Hospital Accreditation (Standar Nasional Akreditasi Rumah Sakit Indonesia), SNARS Edition 1.1. 2022. Available online: https://repository.dinus.ac.id/docs/ajar/KARS_2017.pdf (accessed on 27 August 2021).
- Haryanto, B.; Lestari, F.; Nurlambang, T. Extreme Events, Disasters, and Health Impacts in Indonesia. In Extreme Weather Events and Human Health; Springer Nature Switzerland AG: Cham, Switzerland, 2020; Available online: Https://www.Springerprofes-Sional.de/En/Extreme-Events-Disasters-and-Health-Impacts-in-Indonesia/17394024 (accessed on 26 September 2021).
- UNDRR. Disaster Risk Reduction in The Republic of Indonesia. Status Rep. 2020, 2020, 40. [Google Scholar]
- Lin, M.M.; Hidayat, R. Jakarta, the Fastest-Sinking City in the World. Available online: https://www.bbc.com/news/world-asia-44636934 (accessed on 15 November 2021).
- Erwanti, M.O. Istana soal Aksi 212: Demo Hak Konstitusional, Selama Bersubstansi. Available online: https://news.detik.com/berita/d-4908815/istana-soal-aksi-212-demo-hak-konstitusional-selama-bersubstansi (accessed on 17 September 2021).
- Wicaksono, A. 97 Orang Ditangkap Saat Demo Hari Buruh di Jakarta. Available online: https://www.cnnindonesia.com/nasional/20210501201715-12-637390/97-orang-ditangkap-saat-demo-hari-buruh-di-jakarta (accessed on 20 September 2021).
- Satgas COVID-19. Cases Per Province. Available online: https://data.covid19.go.id/public/index.html (accessed on 12 September 2021).
- Ahmad, F. Sejak 1829 Gunung Tangkuban Parahu Meletus 13 Kali. Available online: https://tekno.tempo.co/read/1231396/sejak-1829-gunung-tangkuban-parahu-meletus-13-kali (accessed on 20 September 2021).
- Arnani, M. Melihat Letusan Besar Gunung Merapi 10 Tahun. Available online: https://www.kompas.com/tren/read/2020/10/26/150300365/melihat-letusan-besar-gunung-merapi-10-tahun-lalu?page=all (accessed on 12 September 2021).
- Warsini, S.; Usher, K.; Buettner, P.; Mills, J.; West, C. Psychosocial and Environmental Distress Resulting from a Volcanic Eruption: Study Protocol. Collegian 2015, 22, 325–331. [Google Scholar] [CrossRef]
- Tempo.co. Pantai Cermin, Sumatera Utara Porak Poranda Disapu Tsunami. Available online: https://nasional.tempo.co/read/53734/pantai-cermin-sumatera-utaraporak-poranda-disapu-tsunami (accessed on 24 September 2021).
- Sinaga, N. Sinabung Meletus 3.500 Meter, Hujan Abu Pekat Melanda Empat Desa. Available online: https://www.kompas.id/baca/nusantara/2021/05/19/sinabung-meletus-3-500-meter-hujan-abu-pekat-melanda-empat-desa (accessed on 23 September 2021).
- WHO. Health Facility Seismic Health Facility Seismic Vulnerability Evaluation. 2006. Available online: https://www.who.int/publications/i/item/health-facility-seismic-vulnerability-evaluation (accessed on 24 September 2021).
- Barbera, J.A.; Yeatts, D.J.; Macintyre, A.G. Challenge of Hospital Emergency Preparedness: Analysis and Recommendations. Disaster Med. Public Health Prep. 2009, 3 (Suppl. 1), S74–S82. [Google Scholar] [CrossRef]
- Pemprov Jawa Barat. Korban Gempa 6,9 SR dan Kerusakan Bangunan Bertambah. Available online: https://jabarprov.go.id/index.php/news/26521/2017/12/16/Korban-Gempa-69-SR-dan-Kerusakan-Bangunan-Bertambah (accessed on 10 September 2021).
- Agung Supriyanto. Mount Merapi Volcano Erupts, Spews Red-Hot Lava. Available online: https://www.thejakartapost.com/news/2021/02/19/mount-merapi-volcano-erupts-spews-red-hot-lava-.html (accessed on 20 September 2021).
- BNPB. West Java Landslides Kill 11, Injure 18. Available online: https://www.thejakartapost.com/news/2021/01/10/west-java-landslides-kill-11-injure-18-.html (accessed on 11 May 2021).
- Indonesia Investments. Massive Electricity Blackouts in Java; A Look at Indonesia’s Electrification Ratio & PLN’s Performance. 2019. Available online: https://www.indonesia-investments.com/id/news/news-columns/massive-electricity-blackouts-in-java-a-look-at-indonesia-s-electrification-ratio-pln-s-performance/item9179 (accessed on 24 September 2021).
- Warta Nias. Sejarah Berdirinya RSUD Gunung Sitoli. Available online: https://www.wartanias.com/2021/01/sejarah-berdirinya-rsud-gunungsitoli.html (accessed on 12 September 2021).
- Kaban, M.A.B.; Achmad, N. Health and Illnes Concept in Elderly Age in Munte Village, Munte District, Karo Regency. Indones. J. Med. Anthropol. 2021, 2, 48–52. [Google Scholar] [CrossRef]
- Dwianto, A.R. Banjir Genangi Rumah Sakit di Jakarta. Available online: https://health.detik.com/berita-detikhealth/d-4914588/banjir-genangi-rumah-sakit-di-jakarta (accessed on 13 September 2021).
- Hadi, S. Learning from The Legacy of Post-Disaster Recovery in Indonesia for The Acceleration of Post-Disaster Recovery in Lombok. J. Perenc. Pembang. Indones. J. Dev. Plan. 2019, 3, 14–31. [Google Scholar] [CrossRef]
- James, E. Getting Ahead of the next Disaster: Recent Preparedness Efforts in Indonesia. Dev. Pract. 2008. [Google Scholar] [CrossRef]
- UNDP. 150,000 People in Quake-Hit Lombok Will Benefit from New Vocational Schools and Health Facilities with UNDP’s Support. 2021. Available online: https://www.id.undp.org/content/indonesia/en/home/presscenter/pressreleases/2021/People-in-quake-hit-Lombok.html (accessed on 12 October 2021).
- Aljazeera. ‘Everything Is Broken’: Healthcare after the Palu Disaster. 2018. Available online: https://www.aljazeera.com/news/2018/10/28/everything-is-broken-healthcare-after-the-palu-disaster (accessed on 13 December 2021).
- Radovic, V.; Vitale, K.; Tchounwou, P.B. Health Facilities Safety in Natural Disasters: Experiences and Challenges from South East Europe. Int. J. Environ. Res. Public Health 2012, 9, 1677–1686. [Google Scholar] [CrossRef]
- World Bank Group. Urban Fire Regulatory Assessment & Mitigation Evaluation Diagnostic; World Bank Group: Washington, DC, USA, 2020. [Google Scholar]
- Samsuddin, N.M.; Takim, R.; Nawawi, A.H.; Rosman, M.R.; SyedAlwee, S.N. A Non-Structural Components Influencing Hospital Disaster Preparedness in Malaysia. IOP Conf. Ser. Earth Environ. Sci. 2018, 140, 012007. [Google Scholar] [CrossRef]
- Lapčević, Z.; Mandić-Rajčević, S.; Lepić, M.; Jovanović, M. Evaluating a Primary Healthcare Center’s Preparedness for Disasters Using the Hospital Safety Index: Lessons Learned from the 2014 Floods in Obrenovac, Serbia. Int. J. Disaster Risk Reduct. 2019, 34, 436–442. [Google Scholar] [CrossRef]
- Yari, A.; Zarezadeh, Y.; Fatemi, F.; Ardalan, A.; Vahedi, S.; Yousefi-Khoshsabeghe, H.; Boubakran, M.S.; Bidarpoor, F.; Motlagh, M.E. Disaster Safety Assessment of Primary Healthcare Facilities: A Cross-Sectional Study in Kurdistan Province of Iran. BMC Emerg. Med. 2021, 21, 23. [Google Scholar] [CrossRef] [PubMed]
- Djalali, A.; Ardalan, A.; Ohlen, G.; Ingrassia, P.L.; Corte, F.D.; Castren, M.; Kurland, L. Nonstructural Safety of Hospitals for Disasters: A Comparison Between Two Capital Cities. Disaster Med. Public Health Prep. 2014. [Google Scholar] [CrossRef]
- Lapčević, Z.; Mandić-Rajčević, S.; Lepić, M.; Jovanović, M. Evaluating a Primary Healthcare Center’s Preparedness for Disasters Using the Hospital Safety Index: Lessons Learned from the 2014 Floods in Obrenovac, Serbia. bioRxiv 2018. [Google Scholar] [CrossRef]
- Mani, G.; Danasekaran, R.; Annadurai, K. Disaster-Resilient Hospitals: The Noah’S Ark. Public Health Indones. 2016, 2, 172–176. [Google Scholar] [CrossRef][Green Version]
- UNDRR. Indonesia Pledges Safety of Over 3,000 Schools and 100-plus Hospitals. Available online: https://www.undrr.org/news/indonesia-pledges-safety-over-3000-schools-and-100-plus-hospitals (accessed on 1 March 2022).


| No | Item | Max Score | Average Score | Ratio |
|---|---|---|---|---|
| 1 | Prior events affecting hospital safety | 3 | 2.125 | 0.708 |
| 2 | Building integrity | 15 | 9.438 | 0.629 |
| Total Score | 18 | 11.563 | 0.642 | |
| No | Item | Max Score | Average Score | Ratio |
|---|---|---|---|---|
| 1 | Architectural safety | 15 | 10.688 | 0.713 |
| 2 | Infrastructure protection, access, andphysical security | 4 | 3.000 | 0.750 |
| Critical systems | ||||
| a. Electrical system | 10 | 6.813 | 0.681 | |
| b. Telecommunication system | 8 | 5.750 | 0.719 | |
| c. Water supply system | 6 | 3.875 | 0.646 | |
| d. Fire protection system | 5 | 3.000 | 0.600 | |
| e. Waste management system | 5 | 4.500 | 0.900 | |
| f. Fuel storage system | 5 | 3.125 | 0.625 | |
| g. Medical gas system | 6 | 4.438 | 0.740 | |
| h. Heating, ventilation, and air conditioning | 8 | 6.000 | 0.750 | |
| 3 | Equipment and supplies | |||
| a. Office and storeroom furnishings and equipment | 2 | 0.938 | 0.469 | |
| b. Medical and laboratory equipment and supplies used for diagnosis and treatment | 19 | 13.750 | 0.724 | |
| Total Score | 93 | 65.875 | 0.732 | |
| No | Item | Max Score | Average Score | Ratio |
|---|---|---|---|---|
| 1. | Coordination of emergency and disaster management activities | 8 | 4938 | 0.617 |
| 2. | Hospital emergency and disaster response and recovery planning | 5 | 2688 | 0.538 |
| 3. | Communication and information management | 4 | 2375 | 0.594 |
| 4. | Human resources | 5 | 2938 | 0.588 |
| 5. | Logistics and finance | 4 | 2938 | 0.734 |
| 6. | Patient care and support services | 9 | 6375 | 0.708 |
| 7. | Evacuation, decontamination, and security | 5 | 3563 | 0.713 |
| Total | 40 | 25,813 | 0.645 |
| No | Module | Score | Index |
|---|---|---|---|
| 1 | Structural Safety | 11.563 | 0.642 |
| 2 | Non-structural Safety | 65.875 | 0.732 |
| 3 | Disaster and Emergency Management | 25.813 | 0.645 |
| Overall Safety Index | 0.673 | ||
| Dimension | Cronbach’s Alpha | Total Eigenvalue | Inertia | % of Variance |
|---|---|---|---|---|
| 1 | 0.816 | 2.578 | 0.644 | 64.442 |
| 2 | 0.378 | 1.396 | 0.349 | 34.889 |
| Total | 3.973 | 0.993 | ||
| Mean | 0.662 | 1.987 | 0.497 | 49.665 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lestari, F.; Paramitasari, D.; Fatmah; Yani Hamid, A.; Suparni; EL-Matury, H.J.; Wijaya, O.; Rahmadani, M.; Ismiyati, A.; Firdausi, R.A.; et al. Analysis of Hospital’s Emergency and Disaster Preparedness Using Hospital Safety Index in Indonesia. Sustainability 2022, 14, 5879. https://doi.org/10.3390/su14105879
Lestari F, Paramitasari D, Fatmah, Yani Hamid A, Suparni, EL-Matury HJ, Wijaya O, Rahmadani M, Ismiyati A, Firdausi RA, et al. Analysis of Hospital’s Emergency and Disaster Preparedness Using Hospital Safety Index in Indonesia. Sustainability. 2022; 14(10):5879. https://doi.org/10.3390/su14105879
Chicago/Turabian StyleLestari, Fatma, Debby Paramitasari, Fatmah, Achir Yani Hamid, Suparni, Herlina J. EL-Matury, Oktomi Wijaya, Meilisa Rahmadani, Avinia Ismiyati, Rizka Asshafaa Firdausi, and et al. 2022. "Analysis of Hospital’s Emergency and Disaster Preparedness Using Hospital Safety Index in Indonesia" Sustainability 14, no. 10: 5879. https://doi.org/10.3390/su14105879
APA StyleLestari, F., Paramitasari, D., Fatmah, Yani Hamid, A., Suparni, EL-Matury, H. J., Wijaya, O., Rahmadani, M., Ismiyati, A., Firdausi, R. A., & Kadir, A. (2022). Analysis of Hospital’s Emergency and Disaster Preparedness Using Hospital Safety Index in Indonesia. Sustainability, 14(10), 5879. https://doi.org/10.3390/su14105879











