Does Postural Feedback Reduce Musculoskeletal Risk?: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
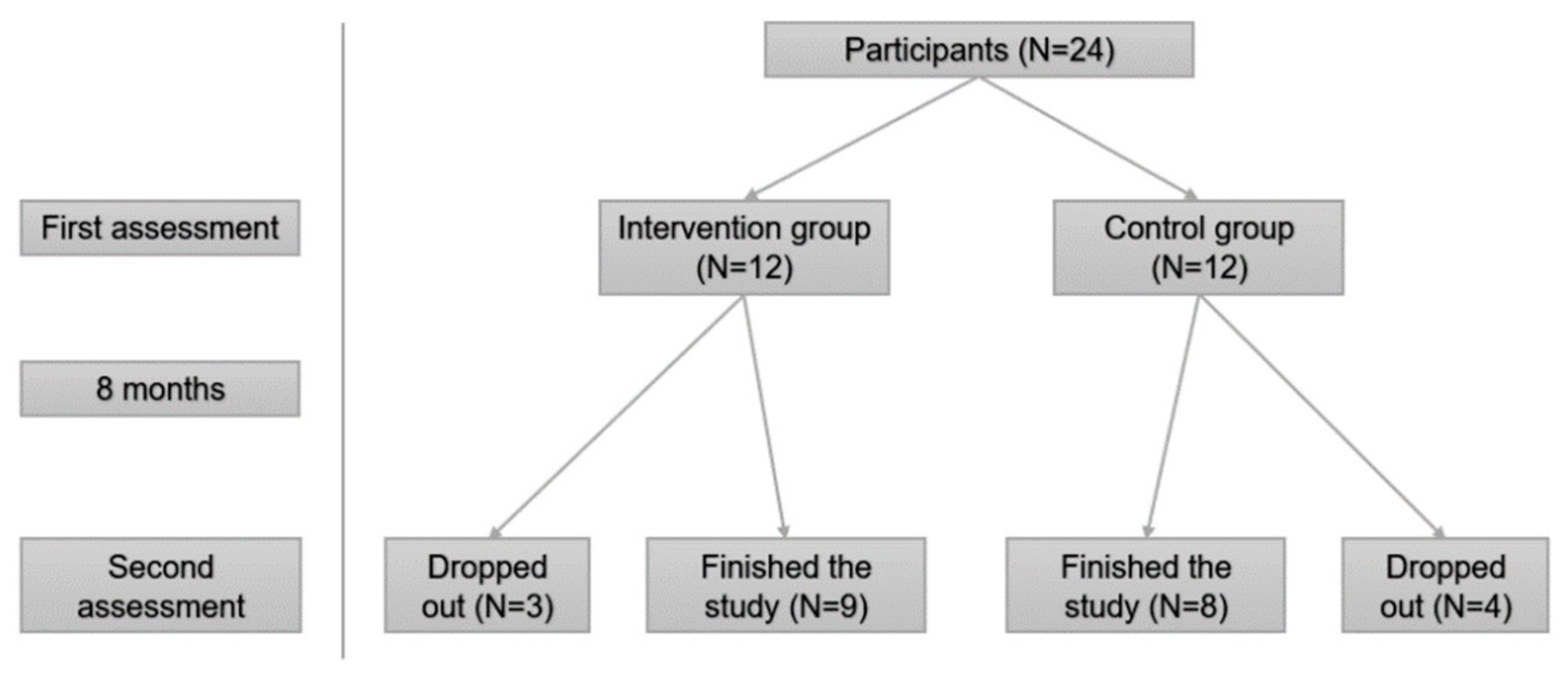
2.1. Settings and Design
2.2. Participants
- (a)
- Professional category is nursing assistant or orderly.
- (b)
- The main daily tasks involve patient handling.
- (c)
- Be on duty on the date of data collection and intervention.
- With temporary contracts of less than eight months.
- Participating in other intervention projects simultaneously.
- Not working on evaluation and intervention days, sick leave, or vacation.
2.3. Variables and Instruments
- (a)
- Sociodemographic variables
- (b) Variables on musculoskeletal risk
2.4. Intervention Program
2.5. Data Collection Procedure
2.6. Ethical Approval
2.7. Data Analysis
3. Results
3.1. The Sociodemographic Characteristics
3.2. Per-Protocol (PP) Analysis
3.3. Intention-to-Treat (ITT) Analysis
4. Discussion
Advantages and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Coluci, M.Z.O.; Alexandre, N.M.C. Job factors related to musculoskeletal symptoms among nursing personnel—A review. Work 2012, 41, 2516–2520. [Google Scholar] [CrossRef]
- El-Sallamy, R.M.; Zayed, H.; Saied, S.; Shehata, W. Work-Related Musculoskeletal Disorders among Nursing Staff of Tanta University Hospitals: Pattern, Risk Factors, and Coping Strategies. Community Med. 2019, 37, 51–61. [Google Scholar]
- Occupational Health and Safety Risks in the Healthcare Sector. Publications Office of the EU. 2014. Available online: https://op.europa.eu/en/publication-detail/-/publication/b29abb0a-f41e-4cb4-b787-4538ac5f0238 (accessed on 20 October 2020).
- Guan, J.; Wu, D.; Xie, X.; Duan, L.; Yuan, D.; Lin, H.; Liu, L.; Li, J. Occupational Factors Causing Pain among Nurses in Mainland China. Med. Sci. Monit. 2019, 25, 1071–1077. [Google Scholar] [CrossRef] [PubMed]
- Viester, L.; Verhagen, E.A.; Hengel, K.M.O.; Koppes, L.L.; Van Der Beek, A.J.; Bongers, P.M. The Relation between Body Mass Index and Musculoskeletal Symptoms in the Working Population. BMC Musculoskelet. Disord. 2013, 14, 238. [Google Scholar] [CrossRef] [PubMed]
- Bernal, D.; Campos-Serna, J.; Tobias, A.; Vargas-Prada, S.; Benavides, F.G.; Serra, C. Work-Related Psychosocial Risk Factors and Musculoskeletal Disorders in Hospital Nurses and Nursing Aides: A Systematic Review and Meta-Analysis. Int. J. Nurs. Stud. 2015, 52, 635–648. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Faucett, J.; Gillen, M.; Krause, N.; Landry, L. Factors Associated with Safe Patient Handling Behaviors among Critical Care Nurses. Am. J. Ind. Med. 2010, 53, 886–897. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Musculoskeletal Conditions. Available online: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions (accessed on 2 January 2022).
- Lezin, N.; Walkins Castillo, S. The Burden of Musculoskeletal Disorders on Americans—Opportunities for Action; The United States Bone and Joint Initiative (USBJI): Rosemont, IL, USA, 2016. [Google Scholar]
- De Kok, J.; Vroonhof, P.; Snijders, J.; Roullis, G.; Clarke, M.; Peereboom, K.; van Dorst, P.; Isusi, I. Work-Related Musculoskeletal Disorders: Prevalence, Costs and Demographics in the EU; European Agency for Safety and Health at Work: Bilbao, Spain, 2019. [Google Scholar]
- Davis, K.G.; Kotowski, S.E. Prevalence of Musculoskeletal Disorders for Nurses in Hospitals, Long-Term Care Facilities, and Home Health Care: A Comprehensive Review. Hum. Factors 2015, 57, 754–792. [Google Scholar] [CrossRef] [PubMed]
- Carugno, M.; Pesatori, A.C.; Ferrario, M.M.; Ferrari, A.L.; da Silva, F.J.; Martins, A.C.; Felli, V.E.A.; Coggon, D.; Bonzini, M. Physical and Psychosocial Risk Factors for Musculoskeletal Disorders in Brazilian and Italian Nurse. Cad. De Saude Publica 2012, 28, 1632–1642. [Google Scholar] [CrossRef]
- Nützi, M.; Koch, P.; Baur, H.; Elfering, A. Work-Family Conflict, Task Interruptions, and Influence at Work Predict Musculoskeletal Pain in Operating Room Nurses. Saf. Health Work 2015, 6, 329–337. [Google Scholar] [CrossRef]
- Harcombe, H.; Herbison, G.P.; McBride, D.; Derrett, S. Musculoskeletal Disorders among Nurses Compared with Two Other Occupational Groups. Occup. Med. 2014, 64, 601–607. [Google Scholar] [CrossRef]
- Akbari, H.; Akbari, H.; Bagheri Hossein Abadi, M.; Gholami Fesharaki, M.; Ghasemi, M. Assessing the Risk of Manual Handling of Patients and Its Relationship with the Prevalence of Musculoskeletal Disorders among Nursing Staff: Performance Evaluation of the MAPO and PTAI Methods. Iran. Red Crescent Med. J. 2017, 19, 8. [Google Scholar] [CrossRef]
- Serranheira, F.; Sousa-Uva, M.; Sousa-Uva, A. Hospital Nurses Tasks and Work-Related Musculoskeletal Disorders Symptoms: A Detailed Analysis. Work 2015, 51, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Heidari, M.; Borujeni, M.G.; Rezaei, P.; Abyaneh, S.K. Work-Related Musculoskeletal Disorders and Their Associated Factors in Nurses: A Cross-Sectional Study in Iran. Malays. J. Med. Sci. 2019, 26, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Sezgin, D.; Esin, M.N. Predisposing Factors for Musculoskeletal Symptoms in Intensive Care Unit Nurses. Int. Nurs. Rev. 2015, 62, 92–101. [Google Scholar] [CrossRef]
- European Agency for Safety and Health at Work (EU-OSHA). Work-Related Musculoskeletal Disorders: Facts and Figures—Synthesis Report of 10 EU Member States Reports, 2020 (AT, DE, DK, ES, FI, FR, HU, IT, NL and SE); European Agency for Safety and Health at Work: Bilbao, Spain, 2020. [Google Scholar]
- Ergonomics and Musculoskeletal Disorders.The National Institute for Occupational Safety and Health (NIOSH) CDC. 2018. Available online: https://www.cdc.gov/niosh/topics/ergonomics (accessed on 3 November 2020).
- Nourollahi, M.; Afshari, D.; Dianat, I. Awkward Trunk Postures and Their Relationship with Low Back Pain in Hospital Nurses. Work 2018, 59, 317–323. [Google Scholar] [CrossRef]
- Freitag, S.; Fincke-Junod, I.; Seddouki, R.; Dulon, M.; Hermanns, I.; Kersten, J.F.; Larsson, T.J.; Nienhaus, A. Frequent Bending—An Underestimated Burden in Nursing Professions. Ann. Occup. Hyg. 2012, 56, 697–707. [Google Scholar] [CrossRef] [PubMed]
- Caponecchia, C.; Coman, R.L.; Gopaldasani, V.; Mayland, E.C.; Campbell, L. Musculoskeletal Disorders in Aged Care Workers: A Systematic Review of Contributing Factors and Interventions. Int. J. Nurs. Stud. 2020, 110, 103715. [Google Scholar] [CrossRef]
- Da Costa, B.R.; Vieira, E.R. Risk Factors for Work-Related Musculoskeletal Disorders: A Systematic Review of Recent Longitudinal Studies. Am. J. Ind. Med. 2009, 53, 285–323. [Google Scholar] [CrossRef] [PubMed]
- Warren, G. Moving and Handling: Reducing Risk through Assessment. Nurs. Stand. 2016, 30, 49–58. [Google Scholar] [CrossRef]
- Samaei, S.E.; Mostafaee, M.; Jafarpoor, H.; Hosseinabadi, M.B. Effects of Patient-Handling and Individual Factors on the Prevalence of Low Back Pain among Nursing Personnel. Work 2017, 56, 551–561. [Google Scholar] [CrossRef] [PubMed]
- Rypicz, Ł.; Karniej, P.; Witczak, I.; Kołcz, A. Evaluation of the Occurrence of Work-Related Musculoskeletal Pain among Anesthesiology, Intensive Care, and Surgical Nurses: An Observational and Descriptive Study. Nurs. Health Sci. 2020, 22, 1056–1064. [Google Scholar] [CrossRef] [PubMed]
- Kucera, K.L.; Schoenfisch, A.L.; McIlvaine, J.; Becherer, L.; James, T.; Yeung, Y.L.; Avent, S.; Lipscomb, H.J. Factors Associated with Lift Equipment Use during Patient Lifts and Transfers by Hospital Nurses and Nursing Care Assistants: A Prospective Observational Cohort Study. Int. J. Nurs. Stud. 2019, 91, 35–46. [Google Scholar] [CrossRef]
- Petit, A.; Mairiaux, P.; Desarmenien, A.; Meyer, J.-P.; Roquelaure, Y. French Good Practice Guidelines for Management of the Risk of Low Back Pain among Workers Exposed to Manual Material Handling: Hierarchical Strategy of Risk Assessment of Work Situations. Work 2016, 53, 845–850. [Google Scholar] [CrossRef]
- Hegewald, J.; Berge, W.; Heinrich, P.; Staudte, R.; Freiberg, A.; Scharfe, J.; Girbig, M.; Nienhaus, A.; Seidler, A. Do Technical Aids for Patient Handling Prevent Musculoskeletal Complaints in Health Care Workers?—A Systematic Review of Intervention Studies. Int. J. Environ. Res. Public Health 2018, 15, 476. [Google Scholar] [CrossRef] [PubMed]
- Freiberg, A.; Euler, U.; Girbig, M.; Nienhaus, A.; Freitag, S.; Seidler, A. Does the Use of Small Aids during Patient Handling Activities Lead to a Decreased Occurrence of Musculoskeletal Complaints and Diseases? A Systematic Review. Int. Arch. Occup. Environ. Health 2016, 89, 547–559. [Google Scholar] [CrossRef]
- Stock, S.R.; Nicolakakis, N.; Vézina, N.; Vézina, M.; Gilbert, L.; Turcot, A.; Sultan-Taïeb, H.; Sinden, K.; Denis, M.A.; Delga, C.; et al. Are Work Organization Interventions Effective in Preventing or Reducing Work-Related Musculoskeletal Disorders? A Systematic Review of the Literature. Scand. J. Work Environ. Health 2018, 44, 113–133. [Google Scholar] [CrossRef]
- Gasibat, Q.; bin Simbak, N.; Abd Aziz, A. Stretching Exercises to Prevent Work-Related Musculoskeletal Disorders—A Review Article. Am. J. Sports Sci. Med. 2017, 5, 27–37. [Google Scholar] [CrossRef]
- Chanchai, W.; Songkham, W.; Ketsomporn, P.; Sappakitchanchai, P.; Siriwong, W.; Robson, M.G. The Impact of an Ergonomics Intervention on Psychosocial Factors and Musculoskeletal Symptoms among Thai Hospital Orderlies. Int. J. Environ. Res. Public Health 2016, 13, 464. [Google Scholar] [CrossRef] [PubMed]
- Savarise, M.T.; Savarise, Y.; Buhavac, M.; Blumhagen, J.; Glasgow, R.E.; Marcus, R.; Magel, J.S. Structured Postural Education Program to Improve Ergonomics and Reduce Work-Related Musculoskeletal Disorders among Surgeons. J. Am. Coll. Surg. 2020, 231, e51–e52. [Google Scholar] [CrossRef]
- Dennerlein, J.T.; Hopcia, K.; Sembajwe, G.; Kenwood, C.; Stoddard, A.M.; Tveito, T.H.; Hashimoto, D.M.; Sorensen, G. Ergonomic Practices within Patient Care Units Are Associated with Musculoskeletal Pain and Limitations. Am. J. Ind. Med. 2012, 55, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Garg, A.; Kapellusch, J.M. Long-Term Efficacy of an Ergonomics Program That Includes Patient-Handling Devices on Reducing Musculoskeletal Injuries to Nursing Personnel. Hum. Factors 2012, 54, 608–625. [Google Scholar] [CrossRef] [PubMed]
- Hoe, V.C.; Urquhart, D.M.; Kelsall, H.L.; Zamri, E.N.; Sim, M.R. Ergonomic Interventions for Preventing Work-Related Musculoskeletal Disorders of the Upper Limb and Neck among Office Workers. Cochrane Database Syst. Rev. 2018, 10, 1–135. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues Ferreira Faisting, A.L.; de Oliveira Sato, T. Effectiveness of Ergonomic Training to Reduce Physical Demands and Musculoskeletal Symptoms—An Overview of Systematic Reviews. Int. J. Ind. Ergon. 2019, 74, 102845. [Google Scholar] [CrossRef]
- Andersen, L.L.; Burdorf, A.; Fallentin, N.; Persson, R.; Jakobsen, M.D.; Mortensen, O.S.; Clausen, T.; Holtermann, A. Patient Transfers and Assistive Devices: Prospective Cohort Study on the Risk for Occupational Back Injury among Healthcare Workers. Scand. J. Work Environ. Health 2014, 40, 74–81. [Google Scholar] [CrossRef][Green Version]
- Tullar, J.M.; Brewer, S.; Amick, B.C.; Irvin, E.; Mahood, Q.; Pompeii, L.A.; Wang, A.; van Eerd, D.; Gimeno, D.; Evanoff, B. Occupational Safety and Health Interventions to Reduce Musculoskeletal Symptoms in the Health Care Sector. J. Occup. Rehabil. 2010, 20, 199–219. [Google Scholar] [CrossRef]
- Risør, B.W.; Casper, S.D.; Andersen, L.L.; Sørensen, J. A Multi-Component Patient-Handling Intervention Improves Attitudes and Behaviors for Safe Patient Handling and Reduces Aggression Experienced by Nursing Staff: A Controlled before-after Study. Appl. Ergon. 2017, 60, 74–82. [Google Scholar] [CrossRef]
- Nelson, A.; Matz, M.; Chen, F.; Siddharthan, K.; Lloyd, J.; Fragala, G. Development and Evaluation of a Multifaceted Ergonomics Program to Prevent Injuries Associated with Patient Handling Tasks. Int. J. Nurs. Stud. 2006, 43, 717–733. [Google Scholar] [CrossRef]
- Ratzon, N.Z.; Bar-Niv, N.A.; Froom, P. The Effect of a Structured Personalized Ergonomic Intervention Program for Hospital Nurses with Reported Musculoskeletal Pain: An Assigned Randomized Control Trial. Work 2016, 54, 367–377. [Google Scholar] [CrossRef]
- Martimo, K.-P.; Shiri, R.; Miranda, H.; Ketola, R.; Varonen, H.; Viikari-Juntura, E. Effectiveness of an Ergonomic Intervention on the Productivity of Workers with Upper-Extremity Disorders—A Randomized Controlled Trial. Scand. J. Work Environ. Health 2010, 36, 25–33. [Google Scholar] [CrossRef][Green Version]
- Olinski, C.; Norton, C.E. Implementation of a Safe Patient Handling Program in a Multihospital Health System from Inception to Sustainability: Successes over 8 Years and Ongoing Challenges. Workplace Heal. Saf. 2017, 65, 546–559. [Google Scholar] [CrossRef]
- Yang, S.; Li, L.; Wang, L.; Zeng, J.; Yan, B.; Li, Y. Effectiveness of a Multidimensional Intervention Program in Improving Occupational Musculoskeletal Disorders among Intensive Care Unit Nurses: A Cluster-Controlled Trial with Follow-up at 3 and 6 Months. BMC Nurs. 2021, 20, 46. [Google Scholar] [CrossRef] [PubMed]
- Richardson, A.; McNoe, B.; Derrett, S.; Harcombe, H. Interventions to Prevent and Reduce the Impact of Musculoskeletal Injuries among Nurses: A Systematic Review. Int. J. Nurs. Stud. 2018, 82, 58–67. [Google Scholar] [CrossRef]
- Van Hoof, W.; O’Sullivan, K.; O’Keeffe, M.; Verschueren, S.; O’Sullivan, P.; Dankaerts, W. The Efficacy of Interventions for Low Back Pain in Nurses: A Systematic Review. Int. J. Nurs. Stud. 2018, 77, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Weir, C.B.; Jan, A. BMI Classification Percentile and Cut Off Points; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Hignett, S.; McAtamney, L. Rapid Entire Body Assessment (REBA). Appl. Ergon. 2000, 31, 201–205. [Google Scholar] [CrossRef]
- Schwartz, A.H.; Albin, T.J.; Gerberich, S.G. Intra-Rater and Inter-Rater Reliability of the Rapid Entire Body Assessment (REBA) Tool. Int. J. Ind. Ergon. 2019, 71, 111. [Google Scholar] [CrossRef]
- Diego, J.A. Postural Evaluation Using the REBA Method. Ergonauts, Polytechnic University of Valencia. 2015. Available online: http://www.ergonautas.upv.es/metodos/reba/reba-ayuda.php (accessed on 2 January 2022).
- Al Madani, D.; Dababneh, A. Rapid Entire Body Assessment: A Literature Review. Am. J. Eng. Appl. Sci. 2016, 9, 107–118. [Google Scholar] [CrossRef]
- Khan, R.; Scaffidi, M.A.; Satchwell, J.; Gimpaya, N.; Lee, W.; Genis, S.; Tham, D.; Saperia, J.; Al-Mazroui, A.; Walsh, C.M.; et al. Impact of a Simulation-Based Ergonomic Training Curriculum on Work-Related Musculoskeletal Injury Risk in Colonoscopy. Gastrointest. Endosc. 2020, 92, 1070–1080. [Google Scholar] [CrossRef] [PubMed]
- Hita-Gutiérrez, M.; Gómez-Galán, M.; Díaz-Pérez, M.; Callejón-Ferre, Á.J. An Overview of Reba Method Applications in the World. Int. J. Environ. Res. Public Health 2020, 17, 2635. [Google Scholar] [CrossRef]
- Beyan, A.C.; Dilek, B.; Demiral, Y. The Effects of Multifaceted Ergonomic Interventions on Musculoskeletal Complaints in Intensive Care Units. Int. J. Environ. Res. Public Health 2020, 17, 3719. [Google Scholar] [CrossRef]
- Moreira, R.F.C.; Moriguchi, C.S.; Carnaz, L.; Foltran, F.A.; Silva, L.C.C.B.; Coury, H.J.C.G. Effects of a Workplace Exercise Program on Physical Capacity and Lower Back Symptoms in Hospital Nursing Assistants: A Randomized Controlled Trial. Int. Arch. Occup. Environ. Health 2021, 94, 275–284. [Google Scholar] [CrossRef]
- Jakobsen, M.D.; Sundstrup, E.; Brandt, M.; Jay, K.; Aagaard, P.; Andersen, L.L. Physical Exercise at the Workplace Reduces Perceived Physical Exertion during Healthcare Work: Cluster Randomized Controlled Trial. Scand. J. Public Health 2015, 43, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Chae, D.; Cho, S.; Kim, J.; Yoo, R. Influence of a Community-Based Stretching Intervention on the Health Outcomes among Korean-Chinese Female Migrant Workers in South Korea: A Randomized Prospective Trial. Jpn. J. Nurs. Sci. 2017, 14, 277–287. [Google Scholar] [CrossRef]
- Lee, E.W.C.; Fok, J.P.C.; Lam, A.T.; Law, R.K.Y.; Szeto, G.P.Y.; Li, P.P.K. The Application of Participatory Ergonomics in a Healthcare Setting in Hong Kong. Work 2014, 48, 511–519. [Google Scholar] [CrossRef]
- Soler-Font, M.; Ramada, J.M.; van Zon, S.K.R.; Almansa, J.; Bültmann, U.; Serra, C.; Merelles, A.; Peña, P.; Vargas-Prada, S. Multifaceted Intervention for the Prevention and Management of Musculoskeletal Pain in Nursing Staff: Results of a Cluster Randomized Controlled Trial. PLoS ONE 2019, 14, e0225198. [Google Scholar] [CrossRef]
- Serra, C.; Soler-Font, M.; García, A.M.; Peña, P.; Vargas-Prada, S.; Ramada, J.M. Prevention and Management of Musculoskeletal Pain in Nursing Staff by a Multifaceted Intervention in the Workplace: Design of a Cluster Randomized Controlled Trial with Effectiveness, Process and Economic Evaluation (INTEVAL_Spain). BMC Public Health 2019, 19, 348. [Google Scholar] [CrossRef] [PubMed]
- Shojaei, S.; Tavafian, S.S.; Jamshidi, A.R.; Wagner, J. A Multidisciplinary Workplace Intervention for Chronic Low Back Pain among Nursing Assistants in Iran. Asian Spine J. 2017, 11, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Carta, A.; Parmigiani, F.; Roversi, A.; Rossato, R.; Milini, C.; Parrinello, G.; Apostoli, P.; Alessio, L.; Porru, S. Training in Safer and Healthier Patient Handling Techniques. Br. J. Nurs. 2010, 19, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Abdollahi, T.; Razi, S.P.; Pahlevan, D.; Yekaninejad, M.S.; Amaniyan, S.; Sieloff, C.L.; Vaismoradi, M. Effect of an Ergonomics Educational Program on Musculoskeletal Disorders in Nursing Staff Working in the Operating Room: A Quasi-Randomized Controlled Clinical Trial. Int. J. Environ. Res. Public Health 2020, 17, 7333. [Google Scholar] [CrossRef]
- Ziam, S.; Laroche, E.; Lakhal, S.; Alderson, M.; Gagné, C. Application of MSD Prevention Practices by Nursing Staff Working in Healthcare Settings. Int. J. Ind. Ergon. 2020, 77, 102959. [Google Scholar] [CrossRef]
- Owlia, M.; Kamachi, M.; Dutta, T. Reducing Lumbar Spine Flexion Using Real-Time Biofeedback during Patient Handling Tasks. Work 2020, 66, 41–51. [Google Scholar] [CrossRef]
- Koningsveld, E.; de Looze, M. Approaches to Work Design—OSHWiki. 2017. Available online: https://oshwiki.eu/wiki/Approaches_to_work_design#Participatory_ergonomics (accessed on 12 August 2021).
- Burgess-Limerick, R. Participatory Ergonomics: Evidence and Implementation Lessons. Appl. Ergon. 2018, 68, 289–293. [Google Scholar] [CrossRef] [PubMed]


| Pre-Assessment | Post-Assessment | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable a | Group | N b | Mean | SD c | p-Value d | Group | N b | Mean | SDc | p-Value d | ||
| Age (years) | Intervention | 12 | 52.67 | 8.424 | 0.927 | Intervention | 9 | 53.67 | 6.1 | 0.537 | ||
| Control | 12 | 52.42 | 4.122 | Control | 8 | 51.38 | 8.77 | |||||
| Work Experience (years) | Intervention | 12 | 16.67 | 3.798 | 0.819 | Intervention | 9 | 15.78 | 8.04 | 0.975 | ||
| Control | 12 | 16.08 | 7.81 | Control | 8 | 15.88 | 3.72 | |||||
| Height (cm) | Intervention | 12 | 161.42 | 7.179 | 0.686 | Intervention | 9 | 163.22 | 13.56 | 0.89 | ||
| Control | 12 | 163.08 | 12.124 | Control | 8 | 162.5 | 5.4 | |||||
| Weight (kg) | Intervention | 12 | 67.33 | 9.884 | 0.648 | Intervention | 9 | 66.44 | 10.93 | 0.474 | ||
| Control | 12 | 65.33 | 11.236 | Control | 8 | 70 | 8.7 | |||||
| BMI (weight/height2) | Intervention | 12 | 25.81 | 3.20565 | 0.385 | Intervention | 9 | 25.14 | 4.2 | 0.452 | ||
| Control | 12 | 24.61 | 3.40255 | Control | 8 | 26.48 | 2.7 | |||||
| Control Group (n%) | Intervention Group (n%) | p-Value e | Control Group (n%) | Intervention Group (n%) | p-Value e | |||||||
| Gender | Male | 2 | 16.67% | 3 | 25.00% | 0.5 | Male | 1 | 10.00% | 3 | 28.57% | 0.312 |
| Female | 10 | 83.33% | 9 | 75.00% | Female | 7 | 90.00% | 6 | 71.43% | |||
| Professional Category | Orderly | 4 | 33.33% | 4 | 33.33% | 0.667 | Orderly | 2 | 20.00% | 4 | 42.86% | 0.402 |
| Nursing assistants | 8 | 66.67% | 8 | 66.67% | Nursing assistants | 6 | 80.00% | 5 | 57.14% | |||
| Service Unit | Internal Medicine | 5 | 41.67% | 5 | 41.67% | 0.660 | Internal Medicine | 3 | 40.00% | 4 | 42.86% | 0.772 |
| Neurology | 7 | 58.33% | 7 | 58.33% | Neurology | 5 | 60.00% | 5 | 57.14% | |||
| Pre-Assessment | Post-Assessment | Pre vs. Post | |||||||
|---|---|---|---|---|---|---|---|---|---|
| GROUP | N a | REBA Score | Mean | SD b | N a | REBA Score | Mean | SD b | p-Value c |
| Control | 21 | Global before | 7.24 | 2.844 | 19 | Global after | 6.68 | 1.003 | 0.212 |
| 21 | A before | 6.38 | 2.312 | 19 | A after | 5.74 | 0.872 | 0.182 | |
| 21 | B before | 4.9 | 1.044 | 19 | B after | 4.68 | 0.749 | 0.141 | |
| Intervention | 35 | Global before | 8.54 | 2.381 | 27 | Global after | 5.44 | 1.05 | 0.000 ** |
| 35 | A before | 7.06 | 1.714 | 27 | A after | 4.81 | 0.736 | 0.000 ** | |
| 35 | B before | 5.26 | 1.4 | 27 | B after | 4.56 | 0.577 | 0.023 * | |
| Pre-Assessment | ||||||||
|---|---|---|---|---|---|---|---|---|
| Control | Intervention | IG vs. CG (pre) | ||||||
| N a | REBA Score | Mean | SD b | N a | REBA Score | Mean | SD b | p-Value c |
| 21 | Global before | 7.24 | 2.844 | 35 | Global before | 8.54 | 2.381 | 0.12 |
| 21 | A before | 6.38 | 2.312 | 35 | A before | 7.06 | 1.714 | 0.202 |
| 21 | B before | 4.9 | 1.044 | 35 | B before | 5.26 | 1.4 | 0.343 |
| Post-Assessment | ||||||||
| Control | Intervention | IG vs. CG (post) | ||||||
| N a | REBA Score | Mean | SD b | N a | REBA Score | Mean | SD b | p-Value c |
| 19 | Global after | 6.68 | 1.003 | 27 | Global after | 5.44 | 1.05 | 0.000 ** |
| 19 | A after | 5.74 | 0.872 | 27 | A after | 4.81 | 0.736 | 0.000 ** |
| 19 | B after | 4.68 | 0.749 | 27 | B after | 4.56 | 0.577 | 0.655 |
| 19 | Improvement | 0.62 | 0.489 | 27 | Improvement | 2.22 | 3.098 | 0.014 * |
| Pre-Assessment | Post-Assessment | Pre- vs. Post- | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| GROUP | N a | REBA Score | Mean | SD b | N a | REBA Score | Mean | SD b | p-Value c | p-Value d |
| Control | 21 | Global before | 7.24 | 2.844 | 21 | Global after | 6.43 | 1.248 | 0.212 | 0.212 |
| 21 | A before | 6.38 | 2.312 | 21 | A after | 5.48 | 0.981 | 0.141 | 0.141 | |
| 21 | B before | 4.9 | 1.044 | 21 | B after | 4.62 | 0.669 | 0.179 | 0.179 | |
| Intervention | 35 | Global before | 8.54 | 2.381 | 35 | Global after | 6.11 | 1.937 | 0.000 ** | 0.000 ** |
| 35 | A before | 7.06 | 1.714 | 35 | A after | 5.23 | 1.352 | 0.000 ** | 0.000 ** | |
| 35 | B before | 5.26 | 1.4 | 35 | B after | 4.74 | 0.852 | 0.035 * | 0.023 * | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliver Hernández, C.; Li, S.; Merino Rivera, M.D.; Mateo Rodríguez, I. Does Postural Feedback Reduce Musculoskeletal Risk?: A Randomized Controlled Trial. Sustainability 2022, 14, 583. https://doi.org/10.3390/su14010583
Oliver Hernández C, Li S, Merino Rivera MD, Mateo Rodríguez I. Does Postural Feedback Reduce Musculoskeletal Risk?: A Randomized Controlled Trial. Sustainability. 2022; 14(1):583. https://doi.org/10.3390/su14010583
Chicago/Turabian StyleOliver Hernández, Coral, Shimeng Li, María Dolores Merino Rivera, and Inmaculada Mateo Rodríguez. 2022. "Does Postural Feedback Reduce Musculoskeletal Risk?: A Randomized Controlled Trial" Sustainability 14, no. 1: 583. https://doi.org/10.3390/su14010583
APA StyleOliver Hernández, C., Li, S., Merino Rivera, M. D., & Mateo Rodríguez, I. (2022). Does Postural Feedback Reduce Musculoskeletal Risk?: A Randomized Controlled Trial. Sustainability, 14(1), 583. https://doi.org/10.3390/su14010583







