Does Urbanization Increase the Risk of Emerging Infectious Diseases in China? A Spatial Econometric Analysis
Abstract
1. Introduction
2. Methodology
2.1. Method
2.2. Spatial Econometric Model
2.3. Variable and Data Source
3. Results
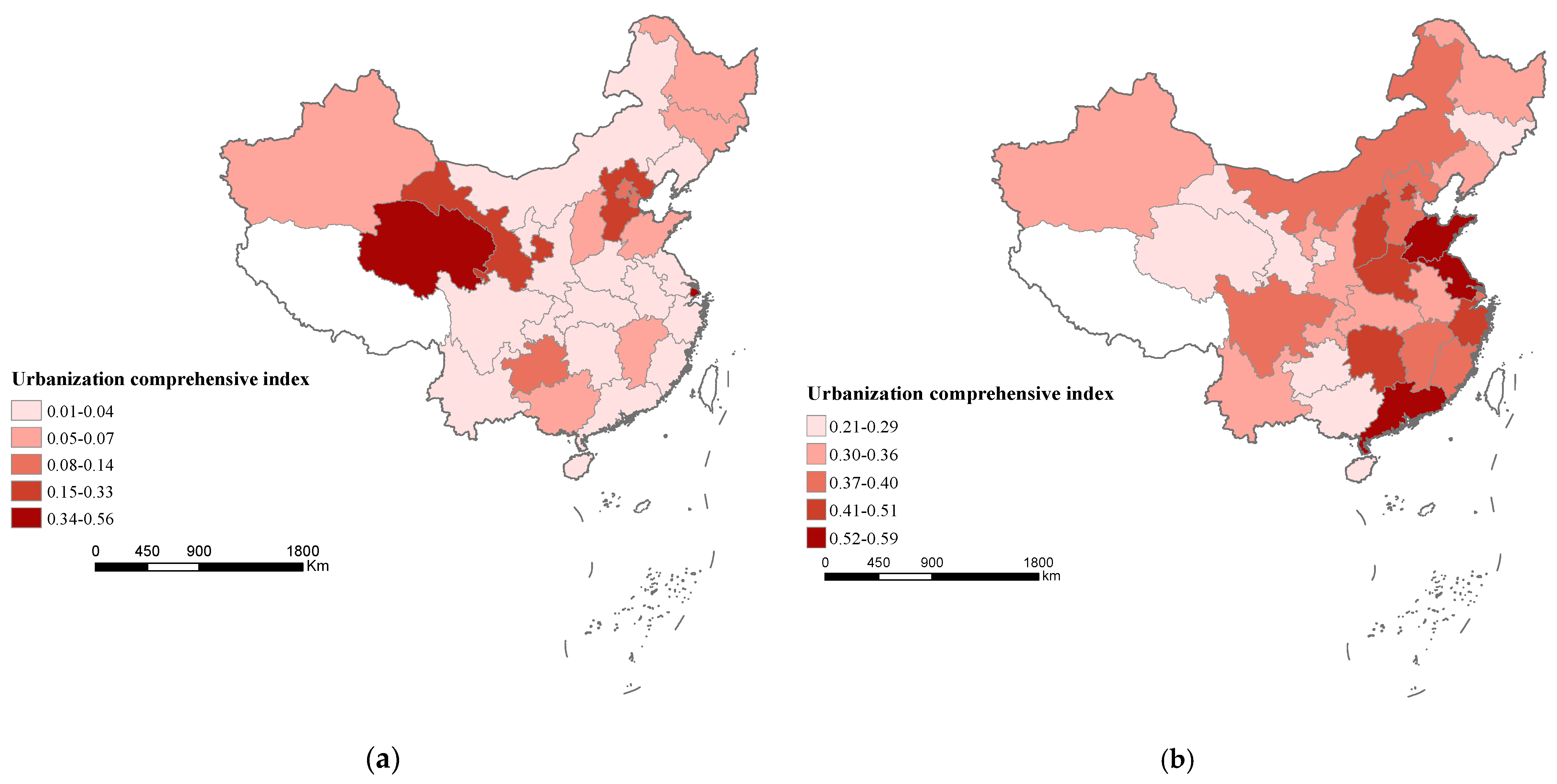
3.1. Spatial Autocorrelation Analysis
3.2. Empirical Analysis
3.3. Robustness Test
3.4. Regional Heterogeneity Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sangar, S.; Thakur, R. Infectious diseases in India: Assessing the role of household amenities and socio-demographic determinants. J. Public Health-UK 2021, 1–9, in press. [Google Scholar] [CrossRef]
- Eckhardt, M.; Hultquist, J.F.; Kaake, R.M.; Hüttenhain, R. A systems approach to infectious disease. Nat. Rev. Genet. 2020, 21, 339–354. [Google Scholar] [CrossRef] [PubMed]
- Morse, S.S. Factors in the emergence of infectious diseases. Emerg. Infect. Dis. 1995, 1, 7–15. [Google Scholar] [CrossRef]
- Wilcox, B.A.; Colwell, R.R. Emerging and reemerging infectious Diseases: Biocomplexity as an interdisciplinary paradigm. EcoHealth 2005, 2, 244–257. [Google Scholar] [CrossRef]
- Wilcox, B.A.; Gubler, D.J. Disease ecology and the global emergence of zoonotic pathogens. Environ. Health Prev. 2005, 10, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Gubler, D.J. Dengue, Urbanization and globalization: The unholy trinity of the 21st century. Int. J. Infect. Dis. 2012, 16, e2. [Google Scholar] [CrossRef]
- Wolf, M. Rethinking urban epidemiology: Natures, networks and materialities. Int. J. Urban Reg. Res. 2016, 40, 958–982. [Google Scholar] [CrossRef] [PubMed]
- Connolly, C.; Keil, R.; Ali, S.H. Extended urbanization and the spatialities of infectious disease: Demographic change, infrastructure and governance. Urban Stud. 2021, 58, 245–263. [Google Scholar] [CrossRef]
- Tong, M.X.; Hansen, A.; Hanson-Easey, S.; Cameron, S.; Xiang, J.; Liu, Q.; Sun, Y.; Weinstein, P.; Han, G.-S.; Williams, C.; et al. Infectious diseases, urbanization and climate change: Challenges in future China. Int. J. Environ. Res. Public Health 2015, 12, 11025–11036. [Google Scholar] [CrossRef]
- Kapan, D.D.; Bennett, S.N.; Ellis, B.N.; Fox, J.; Lewis, N.D.; Spencer, J.H.; Spencer, S.; Wilcox, B.A. Avian influenza (H5N1) and the evolutionary and social ecology of infectious disease emergence. EcoHealth 2006, 3, 187–194. [Google Scholar] [CrossRef]
- Wu, T.; Perrings, C.; Kinzig, A. Economic growth, urbanization, globalization, and the risks of emerging infectious diseases in China: A review. Ambio 2017, 46, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.C.G.; Lacerda, H.G.; Martins, D.R.M.; Barbosa, J.D.A.; Monteiro, G.R.; Quieroz, J.W.; Jeronimo, S.M.B. Changing epidemiology of American cutaneous leishmaniasis (ACL) in Brazil: A disease of the urban–rural interface. Acta Trop. 2004, 90, 155–162. [Google Scholar] [CrossRef]
- Spencer, J.H. The urban health transition hypothesis: Empirical evidence of an avian influenza Kuznets curve in Vietnam? J. Urban Health 2013, 90, 343–357. [Google Scholar] [CrossRef][Green Version]
- Chen, M.; Liu, W.; Lu, D. Challenges and the way forward in China’s new-type urbanization. Land Use Policy 2016, 55, 334–339. [Google Scholar] [CrossRef]
- Gong, P.; Liang, S.; Carlton, E.J.; Jiang, Q.W.; Wu, J.Y.; Wang, L.; Remais, J.V. Urbanization and health in China. Lancet 2012, 379, 843–852. [Google Scholar] [CrossRef]
- World Development Indicators. Available online: https://databank.worldbank.org/source/world-development-indicators (accessed on 20 April 2021).
- World Urbanization Prospects: 2018 Revison. Available online: esa.un.org/unpd/wup/Publications/Files/WUP2018-Report.pdf (accessed on 5 May 2021).
- Statistical Bulletin of China’s Health Development in 2019. Available online: http://www.gov.cn/guoqing/2021-04/09/content_5598657.htm (accessed on 10 May 2021).
- Ali, S.H.; Keil, R. Contagious Cities. Geogr. Compass 2007, 1, 1207–1226. [Google Scholar] [CrossRef]
- Tian, H.; Hu, S.; Cazelles, B.; Chowell, G.; Stenseth, N.C. Urbanization prolongs hantavirus epidemics in cities. Proc. Natl. Acad. Sci. USA 2018, 115, 4707–4712. [Google Scholar] [CrossRef] [PubMed]
- Wilcox, B.A.; Gubler, D. Urbanization and the social ecology of emerging infectious diseases. In The Social Ecology of Infectious Diseases; Mayer, K., Pizer, H., Eds.; Academic Press Inc.: Pittsburgh, PA, USA, 2007; pp. 115–137. [Google Scholar]
- Neiderud, C.J. How urbanization affects the epidemiology of emerging infectious diseases. Infect. Ecol. Epidemiol. 2015, 5, 27060. [Google Scholar] [CrossRef] [PubMed]
- Keiser, J.; Utzinger, J.; Castro, M. Urbanization in sub-Saharan Africa and implication for malaria control. Am. J. Trop. Med. Hyg. 2004, 71, 118–127. [Google Scholar] [CrossRef]
- Saksena, S.; Fox, J.; Epprecht, M.; Tran, C.; Vien, T.D. Role of Urbanization, Land-Use Diversity, and Livestock Intensification in Zoonotic Emerging Infectious Diseases; East-West Center Working Papers; East-West Center: Honolulu, HI, USA, 2014. [Google Scholar]
- Hamidi, S.; Sabouri, S.; Ewing, R. Does density aggravate the COVID-19 pandemic? Early findings and lessons for planners. J. Am. Plann. Assoc. 2020, 86, 495–509. [Google Scholar] [CrossRef]
- Emilie, A.; Laurent, G.; Beat, S.; François, C.; Louis, L. Urbanization and infectious diseases in a globalized world. Lancet Infect. Dis. 2011, 11, 131–141. [Google Scholar]
- Boussaa, S.; Pesson, B.; Boumezzough, A. Phlebotomine sandflies (Diptera: Psychodidae) of Marrakech city, Morocco. Ann. Trop. Med. Parasitol. 2007, 101, 715–724. [Google Scholar] [CrossRef] [PubMed]
- Wood, C.L.; Mcinturff, A.; Young, H.S.; Kim, D.H.; Lafferty, K. Human infectious disease burdens decrease with urbanization but not with biodiversity. Philos. Trans. R. Soc. Lond. B Biol.Sci. 2017, 372, 20160122. [Google Scholar] [CrossRef] [PubMed]
- Qi, Q.; Guerra, C.A.; Moyes, C.L.; Elyazar, I.R.F.; Tatem, A.J. The effects of urbanization on global Plasmodium vivax malaria transmission. Malar. J. 2012, 11, 403. [Google Scholar] [CrossRef] [PubMed]
- Hay, S.I.; Guerra, C.A.; Tatem, A.J.; Atkinson, P.M.; Snow, R.W. Urbanization, malaria transmission and disease burden in Africa. Nat. Rev. Microbiol. 2005, 3, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Moran, P.A.P. Notes on continuous stochastic phenomena. Biometrika 1950, 37, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Sun, X.; Wang, W. Study on the effect of environmental regulations and industrial structure on haze pollution in China from the dual perspective of independence and linkage. J. Clean. Prod. 2020, 256, 120748. [Google Scholar] [CrossRef]
- Elhorst, J.P. Dynamic spatial panels: Models, methods, and inferences. J. Geogr. Syst. 2012, 14, 5–28. [Google Scholar] [CrossRef]
- Vlahov, D.; Galea, S. Urbanization, urbanicity, and health. J. Urban Health 2002, 79, S1–S12. [Google Scholar] [CrossRef]
- Zhang, X.; Song, W.; Wang, J.; Wen, B.; Yang, D.; Jiang, S.; Wu, Y. Analysis on decoupling between urbanization level and urbanization quality in China. Sustainability 2020, 12, 6835. [Google Scholar] [CrossRef]
- Wei, C.; Wang, Z.; Lan, X.; Zhang, H.; Fan, M. The spatial-temporal characteristics and dilemmas of sustainable urbanization in China: A new perspective based on the concept of Five-in-One. Sustainability 2018, 10, 4733. [Google Scholar] [CrossRef]
- Ali, S.H.; Keil, R. Global cities and the spread of infectious disease: The case of Severe Acute Respiratory Syndrome (SARS) in Toronto, Canada. Urban Stud. 2006, 43, 2083–2090. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Ebola virus disease in West Africa: The first 9 months of the epidemic and forward projections. N. Engl. J. Med. 2014, 371, 1481–1495. [Google Scholar] [CrossRef]
- Stein, R.A. Political will and international collaborative frameworks in infectious diseases. Int. J. Clin. Pract. 2015, 69, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Han, H.; Li, H. Coupling Coordination Evaluation between Population and Land Urbanization in Ha-Chang Urban Agglomeration. Sustainability 2020, 12, 357. [Google Scholar] [CrossRef]
- Savard, J.; Clergeau, P.; Mennechez, G. Biodiversity concepts and urban ecosystems. Landsc. Urban Plan. 2000, 48, 131–142. [Google Scholar] [CrossRef]
- McMichael, A.J. The urban environment and health in a world of increasing globalization: Issues for developing countries. Bull. World Health Organ. 2000, 78, 1117–1126. [Google Scholar]
- Kindermann, G.; Domegan, C.; Britton, E.; Carlin, C.; Mashinchi, M.I.; Ojo, A. Understanding the dynamics of green and blue spaces for health and wellbeing outcomes in Ireland: A systemic stakeholder perspective. Sustainability 2021, 13, 9533. [Google Scholar] [CrossRef]
- Liu, B.L.; Zhu, J.F. Urbanization development in New China in the past 70 years: History, problems and prospects. Res. Econ. Manag. 2019, 11, 3–14. (In Chinese) [Google Scholar]
- Mcn, G.; Chenery, H.; Syrquin, M. Patterns of development. Popul. Dev. Rev. 1976, 2, 535. [Google Scholar] [CrossRef]
- Cohen, M. Changing patterns of infectious disease. Nature 2000, 406, 762–767. [Google Scholar] [CrossRef] [PubMed]



| Classification | Index | Meaning |
|---|---|---|
| Population urbanization | Proportion of urban population (%) | Urban population/total population |
| Population density (person/km2) | Urban population/urban area | |
| Economic urbanization | GDP (100,000,000 yuan) | Gross Domestic Product |
| Proportion of urban secondary and tertiary industry output value (%) | Added value of secondary and tertiary industry/GDP | |
| Income (yuan) | The disposable income of residents | |
| Social urbanization | Medical Insurance Coverage (%) | Number of people participating in urban basic medical insurance/urban population |
| Number of doctors owned per 10,000 person (person) | Number of urban doctors/urban population (10,000 person) | |
| Bed number owned per 10,000 person (beds) | Total number of beds in urban area/population in urban area (10,000 person) | |
| Public transport vehicles per 10,000 people | Public transport vehicles/urban population(10,000 person) | |
| Education level (%) | The ration of employed persons with bachelor degree | |
| Land urbanization | Built-up area (km2) | Built-up area in urban |
| Land area requisitioned(km2) | Land area requisitioned each year | |
| Urban road area per capita (m2) | Area of urban roads/urban population | |
| Ecological urbanization | Green area of built-up area (%) | Green land area in urban built-up area/urban built-up area |
| Cleaning area (10,000 km2) | Area of urban cleaning |
| Methods | W1 |
|---|---|
| LM-lag test | 29.016 *** |
| R-LM-lag test | 3.075 |
| LM-err test | 395.534 *** |
| R-LM-err test | 369.593 *** |
| LR-test joint significance spatial fixed effect | 76.87 ** |
| LR-test joint significance time fixed effect | 625.97 *** |
| Hausman test | 38.63 *** |
| lnIIDhep | lnIIDsyp | lnIIDgon | lnIIDhep | lnIIDsyp | lnIIDgon | |
|---|---|---|---|---|---|---|
| lnUCI | 0.112 ** | 1.210 *** | 0.774 *** | 0.840 *** | 3.504 *** | 1.815 *** |
| (0.1089) | (0.1285) | (0.1029) | (0.2375) | (0.2419) | (0.2392) | |
| lnTRA | 0.201 *** | 0.213 *** | 0.0319 * | 0.176 *** | 0.152 *** | 0.044 ** |
| (0.0420) | (0.0477) | (0.0393) | (0.0417) | (0.0440) | (0.0399) | |
| lnHUM | 0.146 | 0.636 *** | −0.0773 | 0.132 | 0.450 ** | 0.0963 |
| (0.1711) | (0.1900) | (0.1622) | (0.1679) | (0.1742) | (0.1608) | |
| lnPOL | 0.0335 | −0.0802 | 0.056 | −0.011 | 0.0177 | 0.0231 |
| (0.0242) | (0.0266) | (0.0222) | (0.0235) | (0.0237) | (0.0221) | |
| λ | 0.0649 *** | 0.0212 ** | 0.0108 ** | 0.0820 *** | 0.0105 * | 0.0428 * |
| (0.0176) | (0.0182) | (0.0159) | (0.0182) | (0.0175) | (0.0181) | |
| Adjust R2 | 0.47 | 0.49 | 0.56 | 0.43 | 0.76 | 0.52 |
| N | 510 | 510 | 510 | 510 | 510 | 510 |
| East | Midwest | |||||
|---|---|---|---|---|---|---|
| lnIIDhep | lnIIDsyp | lnIIDgon | lnIIDhep | lnIIDsyp | lnIIDgon | |
| lnUCI | 0.415 *** | 0.197 ** | 0.524 *** | −0.0432 | 0.0323 | 0.0174 |
| (0.0564) | (0.0648) | (0.0490) | (0.0538) | (0.0620) | (0.0488) | |
| lnTRA | 0.616 *** | 0.572 *** | 0.532 *** | 0.155 ** | 0.0469 | −0.107 * |
| (0.1114) | (0.1266) | (0.0958) | (0.0499) | (0.0655) | (0.0468) | |
| lnPOL | 0.0486 | −0.0853 * | −0.0429 | 0.0263 | 0.063 | 0.0086 |
| (0.0366) | (0.0417) | (0.0313) | (0.0266) | (0.0322) | (0.0251) | |
| lnHUM | 0.0737 | −0.58 | −0.266 | 0.181 | −0.537 | −0.0327 |
| (0.3785) | (0.4354) | (0.3244) | (0.2303) | (0.2822) | (0.2163) | |
| λ | 0.296 *** | 0.276 ** | 0.167 ** | 0.397 *** | 0.128 | −0.137 |
| (0.0759) | (0.0867) | (0.0766) | (0.0927) | (0.0938) | (0.0880) | |
| Adjust R2 | 0.47 | 0.65 | 0.57 | 0.42 | 0.44 | 0.35 |
| N | 154 | 154 | 154 | 266 | 266 | 266 |
| East | Midwest | |||||
|---|---|---|---|---|---|---|
| IIDhep | Actual | Predicted | Error (%) | Actual | Predicted | Error (%) |
| 2017 | 81.9303 | 77.9113 | 4.91% | 103.5716 | 101.4126 | 2.08% |
| 2018 | 78.5464 | 78.5821 | −0.05% | 101.4647 | 100.3163 | 1.13% |
| 2019 | 80.7291 | 85.2425 | −5.59% | 98.1353 | 100.6672 | −2.58% |
| MAPE(%) | 3.4% | 1.9% | ||||
| IIDsyp | Actual | Predicted | Actual | Predicted | ||
| 2017 | 39.6645 | 41.3718 | −4.30% | 37.0868 | 38.1885 | −2.97% |
| 2018 | 38.4109 | 40.2523 | −4.79% | 39.3105 | 39.1963 | 0.29% |
| 2019 | 40.8127 | 41.4433 | −1.55% | 41.8447 | 39.3911 | 5.86% |
| MAPE(%) | 3.5% | 3% | ||||
| IIDgon | Actual | Predicted | Actual | Predicted | ||
| 2017 | 15.3427 | 14.8074 | 3.49% | 6.5784 | 6.3319 | 3.75% |
| 2018 | 13.8536 | 13.1165 | 5.32% | 6.4158 | 6.2412 | 2.72% |
| 2019 | 11.5645 | 12.1061 | −4.68% | 5.8532 | 6.2407 | −6.76% |
| MAPE(%) | 3.7% | 4.4% | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feng, X.; Liu, S.; Wang, C.; Sriboonjit, J.; Liu, J.; Sriboonchitta, S. Does Urbanization Increase the Risk of Emerging Infectious Diseases in China? A Spatial Econometric Analysis. Sustainability 2022, 14, 165. https://doi.org/10.3390/su14010165
Feng X, Liu S, Wang C, Sriboonjit J, Liu J, Sriboonchitta S. Does Urbanization Increase the Risk of Emerging Infectious Diseases in China? A Spatial Econometric Analysis. Sustainability. 2022; 14(1):165. https://doi.org/10.3390/su14010165
Chicago/Turabian StyleFeng, Xiuju, Shutong Liu, Chuanrong Wang, Jittaporn Sriboonjit, Jianxu Liu, and Songsak Sriboonchitta. 2022. "Does Urbanization Increase the Risk of Emerging Infectious Diseases in China? A Spatial Econometric Analysis" Sustainability 14, no. 1: 165. https://doi.org/10.3390/su14010165
APA StyleFeng, X., Liu, S., Wang, C., Sriboonjit, J., Liu, J., & Sriboonchitta, S. (2022). Does Urbanization Increase the Risk of Emerging Infectious Diseases in China? A Spatial Econometric Analysis. Sustainability, 14(1), 165. https://doi.org/10.3390/su14010165






