Gaps in Reporting Greenhouse Gas Emissions by German Hospitals—A Systematic Grey Literature Review
Abstract
1. Introduction
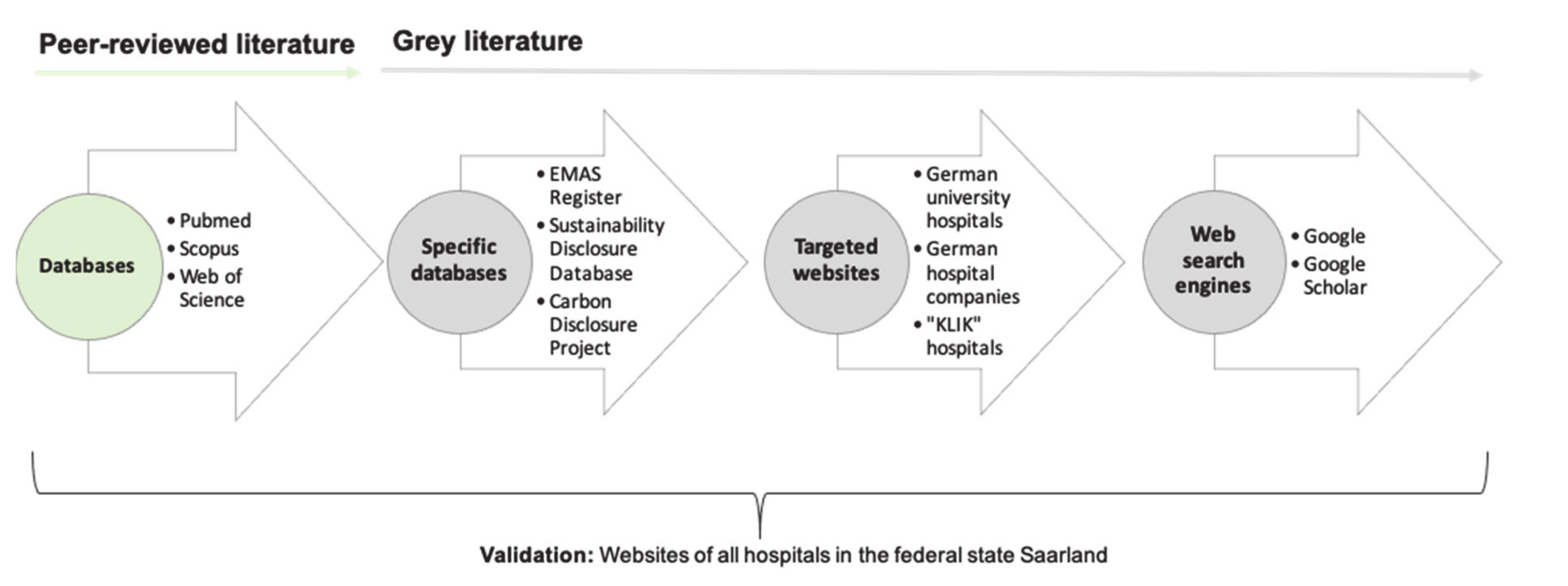
2. Materials and Methods
3. Results
3.1. All German Hospitals with GHG Emissions Reports
3.2. Further Analysis of 62 Hospitals with GHG Emission Reports Meeting the Inclusion Criteria
3.2.1. Size of Hospitals
3.2.2. Location of Hospitals
3.2.3. Reporting Framework
3.2.4. Reported Greenhouse Gases
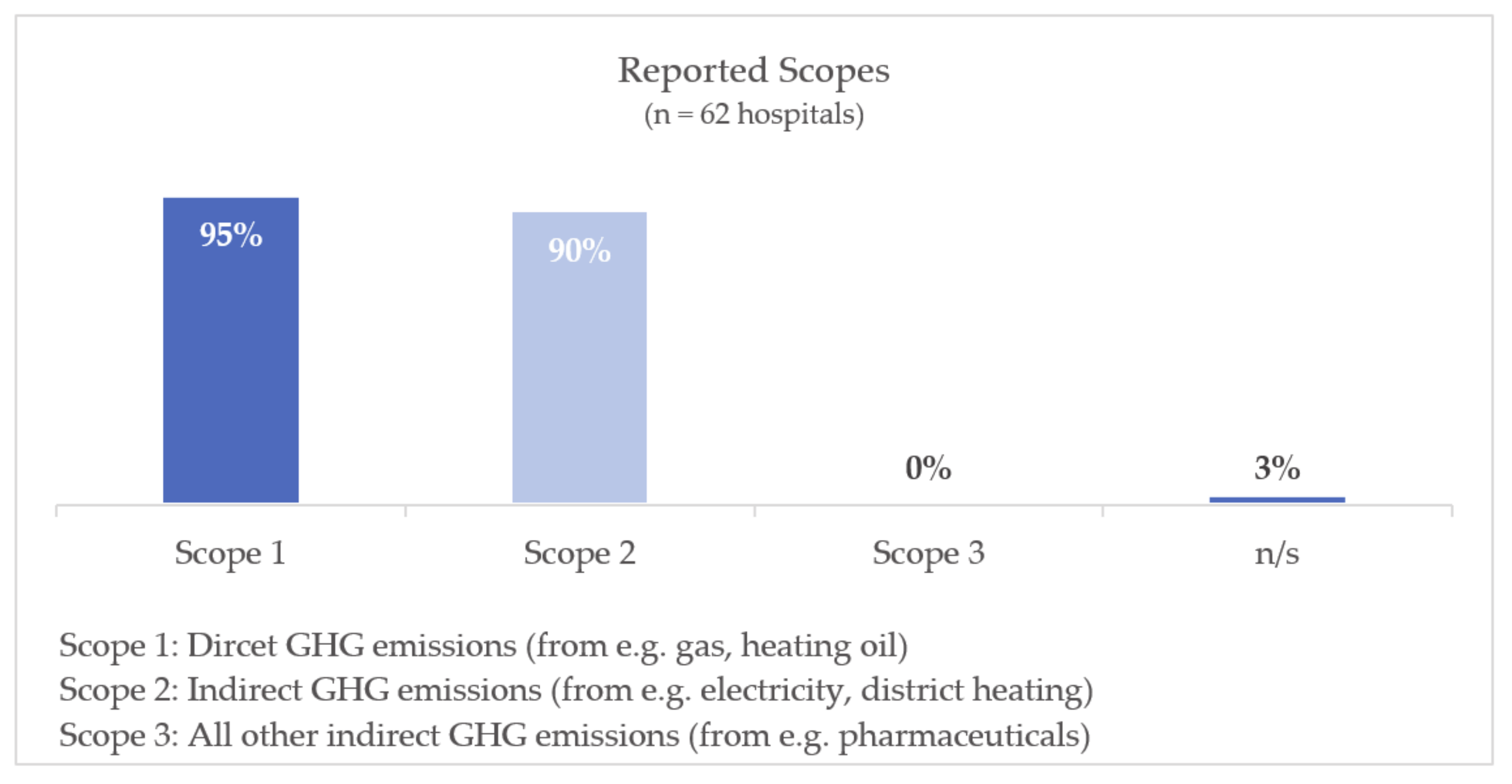
3.2.5. Reported Scopes
- Scope 1 comprises direct GHG emissions from sources that are owned or controlled by the company, e.g., emissions from combustion in owned or controlled boilers or vehicles.
- Scope 2 comprises indirect GHG emissions from purchased electricity, steam, heating and cooling consumed by the company.
- Scope 3 comprises all other indirect emissions due to activities of the company not included in Scope 2. These emissions occur from sources not owned or controlled by the company, e.g., upstream (extraction and production) and downstream (disposal) of purchased materials.
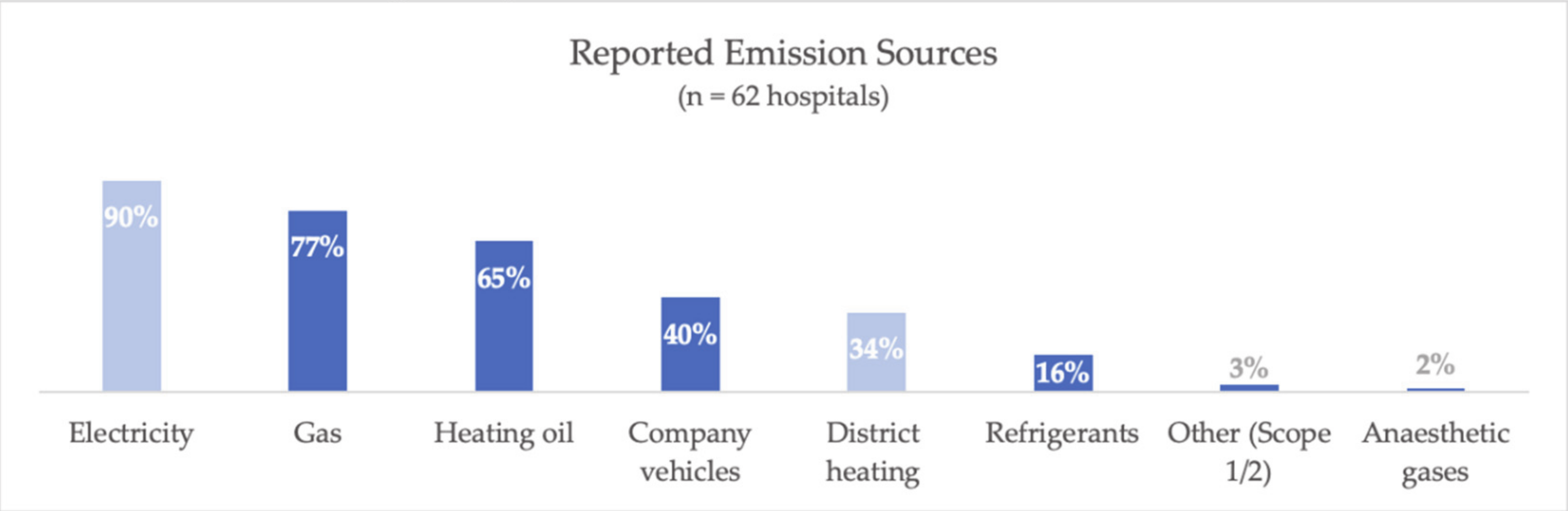
3.2.6. Reported Emissions Sources
4. Discussion
4.1. Gaps in GHG Emissions Reporting
- Small proportion of hospitals with GHG emissions reporting
- Incomplete reporting on Scope 1 and 2 emission sources
- No reporting on Scope 3 emission
- Frequent omission of GHG other than CO2
- (Gap 1) Small proportion of hospitals with GHG emissions reporting
- (Gap 2) Incomplete reporting on Scope 1 and 2 emission sources
- (Gap 3) No reporting on Scope 3 emissions
- (Gap 4) Frequent omission of GHG other than CO2
4.2. Discussion of Reasons for the Existing Gaps
4.3. Policy Recommendations
- (1)
- A legal obligation for German hospitals to report GHG emissions should be introduced (addressing gap 1).
- (2)
- A standardized methodology for GHG emissions reporting of hospitals should be provided (addressing gaps 2 to 4)
4.4. Research Recommendations
4.5. Strengths and Limitations
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Database | Search Terms | Relevant Hits |
|---|---|---|
| Web of Science | TS = ((“hospital”) OR (“health care facility”) OR (“healthcare facility”) OR (“infirmary”)) AND TS = ((“carbon footprint”) OR (“CO2 emission”) OR (“climate footprint”) OR (“greenhouse gas”) OR (“greenhouse gas inventory”) OR (“greenhouse gas emission”) OR (“greenhouse gas protocol”)) | 0 |
| PubMed | ((“hospital”) OR (“health care facility”) OR (“healthcare facility”) OR (“infirmary”)) AND ((“carbon footprint”) OR (“CO2 emission”) OR (“climate footprint”) OR (“greenhouse gas”) OR (“greenhouse gas inventory”) OR (“greenhouse gas emission”) OR (“greenhouse gas protocol”)) | 0 |
| Scopus | TITLE-ABS-KEY(((“hospital”) OR (“health care facility”) OR (“healthcare facility”) OR (“infirmary”)) AND ((“carbon footprint”) OR (“CO2 emission”) OR (“climate footprint”) OR (“greenhouse gas”) OR (“greenhouse gas inventory”) OR (“greenhouse gas emission”) OR (“greenhouse gas protocol”))) | 0 |
Appendix B
| Name | Filters | Hits | Relevant Hits | URL |
|---|---|---|---|---|
| Sustainability Disclosure Database |
| 0 | 0 | https://database.globalreporting.org/search/ |
| Eco Management and Audit Scheme (EMAS) |
| 33 | 28 (some hits comprise several hospitals → 49 EMAS certified hospitals included) | https://webgate.ec.europa.eu/emas2/public/registration/list |
| Carbon Disclosure Project (CDP) |
| 12 | 0 | https://www.cdp.net/en/responses?utf8=%E2%9C%93&queries%5Bname%5D= |
Appendix C
| Website Category | Search Terms | Relevant Hits |
|---|---|---|
| Websites of the 35 German University Hospitals |
| 2 |
| Websites of 10 hospital companies (with >150,000 cases/year) |
| 5 |
| Websites of hospitals that participated in the project “KLIK–Klimamanager für Kliniken” |
| 0 (after excluding EMAS-certified hospitals, university hospitals and hospital companies) |
Appendix D
| Web Search Engine | Search Terms | Relevant Hits |
|---|---|---|
| Google German |
| 6 (after excluding EMAS-certified hospitals, university hospitals and hospital companies) |
| Google English |
| 0 |
| Google Scholar |
| 0 |
Appendix E
|
Appendix F
| Names of the Hospitals Meeting the Inclusion Criteria |
|---|
| Bezirkskrankenhaus Günzburg [54] |
| Bezirkskrankenhaus Kaufbeuren [55] |
| Charité Berlin [56] |
| DIAKO Bremen [57] |
| DRK Klinikservicegesellschaft Sachsen mbH (Standort: DRK Krankenhaus Chemnitz-Rabenstein) [58] |
| DRK Klinikservicegesellschaft Sachsen mbH (Standort: DRK Krankenhaus Lichtenstein) [58] |
| Evangelische Krankenhaus Köln-Weyertal [59] |
| Fachklinik Heiligenfeld [60] |
| Klinikum Idar-Oberstein–SHG-Kliniken [61] |
| Katholische Kliniken Emscher-Lippe: St. Antonius-Krankenhaus [62] |
| Katholische Kliniken Emscher-Lippe: St. Barbara-Hospital [62] |
| Katholische Kliniken Emscher-Lippe: St. Josef-Hospital [62] |
| Klinik Heiligenfeld Standort Uffenheim [60] |
| Klinik Heiligenfeld Standort Waldmünchen [60] |
| Kliniken Landkreis Heidenheim gGmbH [63] |
| Klinikum Bremen Mitte [64] |
| Klinikum Chemnitz gGmbH [65] |
| Klinikum Kulmbach [66] |
| Klinikum Landsberg am Lech [67] |
| Klinikum Oldenburg [68] |
| Klinikum Penzberg [69] |
| Klinikum Saarbrücken [70] |
| Klinikum Seefeld [69] |
| Klinikum Starnberg [69] |
| Klinikverbund Kempten –Oberallgäu Standort: Klinik Immenstadt [71] |
| Klinikverbund Kempten –Oberallgäu Standort: Klinik Oberstdorf [71] |
| Klinikverbund Kempten –Oberallgäu Standort: Klinik Sonthofen [71] |
| Klinikverbund Kempten –Oberallgäu Standort: Klinikum-Kempten [71] |
| Krankenhaus Rotthalmünster [72] |
| Krankenhaus Vilshofen [72] |
| Krankenhaus Wegscheid [72] |
| Kreisklinik Wolfratshausen gGmbH [73] |
| Luitpoldklinik Heiligenfeld [60] |
| LVR Klinik Bedburg-Hau [74] |
| LVR Klinik Bedburg-Hau Außenstelle: Sternbuschklinik Kleve [74] |
| LVR Klinik Bonn [75] |
| LVR Klinik Düren [76] |
| LVR Klinik Düsseldorf [77] |
| LVR Klinik Köln [78] |
| LVR Klinik Langenfeld [79] |
| LVR Klinik Viersen [80] |
| LVR Klinik Mönchengladbach [81] |
| LWL Klinik Lengerich [82] |
| LWL Klinik Münster [83] |
| München Klinik Standort Bogenhausen [84] |
| München Klinik Standort Harlaching [84] |
| München Klinik Standort Neuperlach [84] |
| München Klinik Standort Schwabing [84] |
| München Klinik Standort Thalkircher Straße [84] |
| Orthopädische Universitätsklinik Friedrichsheim [85] |
| Parkklinik Heiligenfeld [60] |
| Rhön-Klinikum AG: Universitätsklinikum Gießen und Marburg, Standort Gießen [86] |
| Rhön-Klinikum AG: Universitätsklinikum Gießen und Marburg, Standort Marburg [86] |
| Rhön-Klinikum AG: Campus Bad Neustadt [86] |
| Rhön-Klinikum AG: Klinikum Frankfurt (Oder) GmbH [86] |
| Rhön-Klinikum AG: Zentralklinik Bad Berka GmbH [86] |
| Rosengarten Klinik Heiligenfeld [60] |
| Sankt Josef-Hospital Xanten [87] |
| St. Barbara-Klinik Hamm-Heessen GmbH [88] |
| Städtisches Klinikum Karlsruhe [89] |
| Städtisches Klinikum Karlsruhe: Psychiatrische Kliniken [89] |
| Universitätsklinikum Jena [90] |
References
- Haines, A.; Ebi, K. The Imperative for Climate Action to Protect Health. New Engl. J. Med. 2019, 380, 263–273. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The World Health Report 2000: Health Systems: Improving Performance; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Herrmann, A.; de Jong, L.; Kowalski, C.; Sauerborn, R. Health Co-benefits of climate change mitigation measures-how households and policy makers can benefit. Bundesgesundheitsblatt Gesundh. Gesundh. 2019, 62, 556–564. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Operational Framework for Building Climate Resilient Health Systems; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Pichler, P.P.; Jaccard, I.S.; Weisz, U.; Weisz, H. International comparison of health care carbon footprints. Environ. Res. Lett. 2019, 14, 064004. [Google Scholar] [CrossRef]
- Health Care Without Harm. Appendix C Health Care Emissions National Snapshot. In Health Care’s Climate Footprint—How the Health Sector Contributes to the Global Climate Crisis and Opportunities for Action; ARUP: London, UK, 2019; Available online: https://noharm-global.org/sites/default/files/documents-files/5959/Apendix%20C%20National%20Emissions%20Snapshots.pdf (accessed on 9 November 2020).
- United Nations. Paris Agreement. In Report of the Conference of the Parties to the United Nations Framework Convention on Climate Change (21st Session, 2015: Paris); HeinOnline: Getzville, NY, USA, 2015. [Google Scholar]
- European Commission. The European Green Deal; Europäische Komission: Brussels, Belgium, 2019. [Google Scholar]
- Bundes-Klimaschutzgesetz. Bundes-Klimaschutzgesetz vom 12. Dezember 2019 (BGBl. I S. 2513); BGBl. I: Berlin, Germany, 2019; p. 2513. [Google Scholar]
- WBGU. Welt im Wandel: Gesellschaftsvertrag für eine Große Transformation. 2011. Available online: https://web.archive.org/web/20130122222145/http://www.bmbf.de/de/16204.php. (accessed on 9 November 2020).
- World Health Organization; Health Care Without Harm. Healthy Hospitals, Healthy Planet, Healthy People—Addressing Climate Change in Health Care Settings: Discussion Draft; WHO: Geneva, Switzerland, 2009. [Google Scholar]
- Weisz, U.; Pichler, P.-P.; Jaccard, I.S.; Haas, W.; Matej, S.; Bachner, F.; Nowak, P.; Weisz, H. Carbon emission trends and sustainability options in Austrian health care. Resour. Conserv. Recycl. 2020, 160, 104862. [Google Scholar] [CrossRef]
- Statistisches Bundesamt (Destatis). Gesundheitsausgaben nach Einrichtungen (2018). 2020. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Gesundheitsausgaben/Tabellen/einrichtungen.html. (accessed on 27 November 2020).
- Lyeonov, S.; Pimonenko, T.; Bilan, Y.; Mentel, G.; Štreimikienė, D. Assessment of green investments’ impact on sustainable development: Linking gross domestic product per capita, greenhouse gas emissions and renewable energy. Energies 2019, 12, 3891. [Google Scholar] [CrossRef]
- CLIRE. Simple Steps to Reduce the Climate Impact of Healthcare. 2016. Available online: https://ec.europa.eu/environment/life/project/Projects/index.cfm?fuseaction=home.showFile&rep=file&fil=CLIRE_Guide_Reduction_Impact_Climate_Healthcare.pdf (accessed on 27 November 2020).
- Godin, K.; Stapleton, J.; Kirkpatrick, S.i.; Hanning, R.M.; Leatherdale, S.T. Applying systematic review search methods to the grey literature: A case study examining guidelines for school-based breakfast programs in Canada. Syst. Rev. 2015, 4, 138. [Google Scholar] [CrossRef] [PubMed]
- BUND. KLIK von 2014 Bis 2016. 2020. Available online: https://www.klik-krankenhaus.de/das-projekt/klik-von-2014-bis-2016 (accessed on 28 August 2020).
- Verband der Universitätsklinika Deutschlands. Übersicht der Universitätsklinika in Deutschland. 2020. Available online: https://www.uniklinika.de/die-deutschen-universitaetsklinika/uebersicht-der-universitaetsklinika/ (accessed on 16 September 2020).
- A & S-Aktuell. Ranking der 20 Größten Klinik-Unternehmen in Deutschland nach Anzahl der Stationären Fälle im Jahr 2012. Available online: https://de.statista.com/statistik/daten/studie/433300/umfrage/ranking-der-20-groessten-klinik-unternehmen-in-deutschland-nach-fallzahl/ (accessed on 15 September 2020).
- BUND. Teilnehmende Krankenhäuser KLIK 2014 bis 2016. 2020. Available online: https://umap.openstreetmap.fr/de/map/klik-green_333681#3/48.98/34.89 (accessed on 6 November 2020).
- Ellen Bates, M. Is Google Hiding My News? Online Medford 2011, 35, 64. [Google Scholar]
- Deutsche Krankenhaus TrustCenter und Informationsverarbeitung GmbH. Deutsches Krankenhausverzeichnis. 2020. Available online: https://www.deutsches-krankenhaus-verzeichnis.de/app/suche (accessed on 1 September 2020).
- Statistisches Bundesamt (Destatis). Anzahl der Deutschen Krankenhäuser nach Trägerschaft in den Jahren 2000 bis 2018. 2020. Available online: https://de.statista.com/statistik/daten/studie/157072/umfrage/anzahl-der-krankenhaeuser-nach-traegerschaft/ (accessed on 15 September 2020).
- Helios Kliniken. Nachhaltigkeitsbericht 2019 (Helios Kliniken, Sustainability Report 2019). 2020. Available online: https://www.helios-gesundheit.de/fileadmin/UWS_Unternehmen/Nachhaltigkeit/Helios_Nachhaltigkeitsbericht2019.pdf (accessed on 7 August 2020).
- Asklepios. Nachhaltigkeitsbericht 2019 (Sustainability Report 2019). 2020. Available online: https://www.asklepios.com/konzern/unternehmen/investors/nachhaltigkeitsbericht/ (accessed on 25 August 2020).
- Bundesministerium für Umwelt Naturschutz und Nukleare Sicherheit and Umweltbundesamt. Umweltkennzahlen in der Praxis—Ein Leitfaden zur Anwendung von Umweltkennzahlen in Umweltmanagementsystemen mit dem Schwerpunkt auf EMAS. 2013. Available online: https://www.umweltbundesamt.de/sites/default/files/medien/376/publikationen/umweltkennzahlen_in_der_praxis_leitfaden_barrierefrei.pdf (accessed on 14 August 2020).
- EMAS. Sectoral Reference Documents. 2020. Available online: https://ec.europa.eu/environment/emas/emas_publications/sectoral_reference_documents_en.htm (accessed on 14 October 2020).
- Health Care Without Harm. Health Care’s Climate Footprint—How the Health Sector Contributes to the Global Climate Crisis and Opportunities for Action; ARUP: London, UK, 2019; Available online: https://noharm-global.org/sites/default/files/documents-files/5961/HealthCaresClimateFootprint_092319.pdf (accessed on 9 November 2020).
- World Business Council for Sustainable Development; World Resources Institute. The Greenhouse Gas Protocol—A Corporate Accounting and Reporting Standard, Revised Edition; WBCSD: Washington, DC, USA, 2004. [Google Scholar]
- National Health Service and Sustainable Development Unit. Reducing the Use of Natural Resources in Health and Social Care—2018 Report; National Health Service and Sustainable Development Unit: Cambridge, UK, 2018. [Google Scholar]
- Malik, A.; Lenzen, M.; McAlister, S.; McGain, F. The carbon footprint of Australian health care. Lancet Planet Health 2018, 2, e27–e35. [Google Scholar] [CrossRef]
- Wu, R. The carbon footprint of the Chinese health-care system: An environmentally extended input-output and structural path analysis study. Lancet Planet Health 2019, 3, e413–e419. [Google Scholar] [CrossRef]
- Umweltbundesamt. Anteil von CO2 an den Treibhausgasemissionen in Deutschland in den Jahren 1990 bis 2018. 2020. Available online: https://de.statista.com/statistik/daten/studie/312536/umfrage/anteil-von-co2-an-den-treibhausgasemissionen-in-deutschland/ (accessed on 4 September 2020).
- Sulbaek, A.; Nielsen, O.J.; Wallington, T.J.; Karpichev, B.; Sander, S.P. Medical intelligence article: Assessing the impact on global climate from general anesthetic gases. Anesth. Analg. 2012, 114, 1081–1085. [Google Scholar]
- Allen, M.W.; Craig, C.A. Rethinking corporate social responsibility in the age of climate change: A communication perspective. Int. J. Corp. Soc. Responsib. 2016, 1, 1–11. [Google Scholar] [CrossRef]
- Health Care Without Harm. Health Care Climate Footprint Report. Available online: https://noharm-europe.org/ClimateFootprintReport (accessed on 20 January 2021).
- Seifert, C. The Barriers for Voluntary Environmental Management Systems—The Case of EMAS in Hospitals. Sustainability 2018, 10, 1420. [Google Scholar] [CrossRef]
- Jameton, A.; McGuire, C. Toward sustainable health-care services: Principles, challenges, and a process. Int. J. Sustain. High. Educ. 2002, 3, 113–127. [Google Scholar] [CrossRef]
- Dunphy, J.L. Healthcare professionals’ perspectives on environmental sustainability. Nurs. Ethics 2014, 21, 414–425. [Google Scholar] [PubMed]
- Pencheon, D. Making health care more sustainable: The case of the English NHS. Public Health 2015, 129, 1335–1343. [Google Scholar] [CrossRef] [PubMed]
- Corina, R. Closing the Scope 3 Reporting Gap. 2020. Available online: https://avieco.com/news-insights/closing-the-scope-3-reporting-gap/ (accessed on 30 September 2020).
- République Francaise. Décret no 2011-829 du 11 Juillet 2011 Relatif au Bilan des Émissions de Gaz à Effet de Serre et au Plan Climat-Énergie Territorial. 2011. Available online: https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000024353784&categorieLien=id (accessed on 15 July 2020).
- Agence de la Transition Écologique. Réalisation d’un Bilan D’émissions de Gaz à Effet de Serre—Guide Sectoriel Établissements Sanitaires et Médico-Sociaux (Agency for Ecological Transition, Greenhouse Gas Emissions Assessment—Sector Guide for Health and Medico-Social Institutions). 2020. Available online: https://www.ademe.fr/sites/default/files/assets/documents/guide-sectoriel-etablissements-sanitaires-et-medico-sociaux-2020-010896.pdf (accessed on 27 November 2020).
- NHS England. NHS England Carbon Emissions Carbon Footprinting Report, September 2008 (Updated August 2009); Sustainable Development Commission: London, UK, 2009. [Google Scholar]
- Gesundheitsministerkonferenz. Beschlüsse der 93. GMK (2020) TOP: 5.1 Der Klimawandel—Eine Herausforderung für das Deutsche Gesundheitswesen (Conference of Health Ministers, Resolutions of the 93rd Conference of Health Ministers (2020) Agenda Item: 5.1 Climate change—A Challenge for the German Health Care System). 2020. Available online: https://www.gmkonline.de/Beschluesse.html?id=1018&jahr= (accessed on 27 November 2020).
- Agora Energiewende. Die Energiewende im Corona-Jahr: Stand der Dinge 2020. Rückblick auf die Wesentlichen Entwicklungen Sowie Ausblick auf 2021. (Agora Energy Transition, The Energy Transition in the Corona Year: State of Affairs in 2020. Review of the Main Developments and Outlook for 2021.). Available online: https://static.agora-energiewende.de/fileadmin2/Projekte/2021/2020_01_Jahresauswertung_2020/200_A-EW_Jahresauswertung_2020_WEB.pdf (accessed on 14 January 2021).
- NHS England. Delivering a “Net Zero” National Health Service. 2020. Available online: https://www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2020/10/delivering-a-net-zero-national-health-service.pdf (accessed on 27 November 2020).
- Council of the European Union. Intended Nationally Determined Contribution of the EU and its Member States. 2015. Available online: https://www4.unfccc.int/sites/ndcstaging/PublishedDocuments/Germany%20First/LV-03-06-EU%20INDC.pdf (accessed on 11 January 2021).
- Bundesministerium für Umwelt Naturschutz und nukleare Sicherheit. Klimaschutzplan 2050—Klimaschutzpolitische Grundsätze und Ziele der Bundesregierung. 2016. Available online: https://www.bmu.de/fileadmin/Daten_BMU/Download_PDF/Klimaschutz/klimaschutzplan_2050_bf.pdf (accessed on 27 November 2020).
- European Commission. Regulation (EU) 2019/631 of the European Parliament and of the Council of 17 April 2019 Setting CO2 Emission Performance Standards for New Passenger Cars and for New Light Commercial Vehicles, and Repealing REGULATIONS (EC) No 443/2009 and (EU) No 510/2011. 2019. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32019R0631&from=EN (accessed on 27 November 2020).
- Behrens, G.; Gredner, T.; Stock, C.; Leitzmann, M.F.; Brenner, H.; Mons, U. Cancers Due to Excess Weight, Low Physical Activity, and Unhealthy Diet. Dtsch. Aerzteblatt Int. 2018, 115, 578–585. [Google Scholar]
- World Health Organization. Q & A on the Carcinogenicity of the Consumption of Red Meat and Processed Meat. 2015. Available online: https://www.who.int/news-room/q-a-detail/cancer-carcinogenicity-of-the-consumption-of-red-meat-and-processed-meat (accessed on 11 January 2021).
- Northumbria Healthcare NHS Foundation Trust. Shine 2012 Final Report—A Clinico-Ethical Framework for Multidisciplinary Review of Medication in Nursing Homes. 2014. Available online: https://www.health.org.uk/sites/default/files/Shine2012_NorthumbriaHealthcareNHSFoundationTrust_report.pdf (accessed on 27 November 2020).
- Bezirkskrankenhaus Günzburg. Umwelterklärung 2014 (Community Hospital Günzburg, Environmental Declaration 2014). Available online: https://www.bkh-guenzburg.de/fileadmin/Daten_haeuser/Daten_guenzburg/PDF/pdf/Umwelterkl%C3%A4rung_2014.pdf (accessed on 11 January 2021).
- Bezirkskrankenhaus Kaufbeuren. Umwelterklärung 2012 (Community Hospital Kaufbeuren, Environmental Declaration 2012). 2012. Available online: https://www.bezirkskrankenhaus-kaufbeuren.de/fileadmin/Daten_haeuser/Daten_kaufbeuren/Pdfs/Umwelterkl%C3%A4rung_2012_neu.pdf (accessed on 11 January 2021).
- Günther, R.; Einhäupl, K.M. Klimaschutzvereinbarung zwischen dem Land Berlin Senatsverwaltung für Umwelt, Verkehr und Klimaschutz und der Charité—Universitätsmedizin Berlin. 2019. Available online: https://www.berlin.de/sen/uvk/_assets/klimaschutz/klimaschutz-in-der-umsetzung/vorbildrolle-oeffentliche-hand/klimaschutzvereinbarung_charite_2019-2028.pdf (accessed on 11 January 2021).
- DIAKO-Diakonissenanstalt Evangelisches Diakonie Krankenhaus. Evangelisches Diakonie-Krankenhaus. Umwelterklärung 2018 mit den Umweltbilanzen des Jahres 2017 (DIAKO Protestant Diakonie Hospital, Environmental Statement 2018 with the Environmental Balances of the Year 2017). 2018. Available online: https://diako.1kcloud.com/ep1vyZJg/#22 (accessed on 11 January 2021).
- DRK-Deutsches Rotes Kreuz. Klinikservicegesellschaft Sachsen mbH. Aktualisierte Umwelterklärung 2020 Standorte Chemnitz und Lichtenstein (DRK Clinic Service Company Saxony, Updated Environmental Statement 2020 Chemnitz and Lichtenstein Sites). Available online: https://rab.drk-khs.de/fileadmin/user_upload/Umwelterklaerung_2019_Rev.pdf (accessed on 11 January 2021).
- Evangelische Krankenhaus Köln-Weyertal. Umwelterklärung 2011 (Protestant Hospital Köln-Weyertal, Environmental Declaration 2011). Available online: http://www.evk-koeln.de/fileadmin/user_upload/KHKW/Dokumente/umwelterklaerung_2011_internet_12042012.pdf (accessed on 11 January 2021).
- Heiligenfeld GmbH. Umwelterklärung 2018 nach Eco-Management and Audit Scheme (EMAS) der Europäischen Union (Environmental Statement 2018 According to Eco-Management and Audit Scheme (EMAS) of the European Union). 2018. Available online: https://www.heiligenfeld.de/fileadmin/user_upload/Ueber_uns/Auszeichnungen/Umwelterklaerung_Heiligenfeld_Kliniken_181_JKOE.pdf (accessed on 11 January 2021).
- Klinikum Idar-Oberstein GmbH. Nachhaltigkeitsbericht 2014 (Hospital Idar-Oberstein, Sustainability Report 2014). 2014. Available online: https://docplayer.org/64192817-Klinikum-idar-oberstein-gmbh.html (accessed on 18 August 2020).
- Katholische Kliniken Emscher-Lippe. Erste Umwelterklärung 2017 (Catholic Hospitals, First Environmental Declaration 2017). 2017. Available online: https://www.kkel.de/fileadmin/user_upload/Erste_Umwelterklaerung_KKEL_final_22.12.207.pdf (accessed on 10 August 2020).
- Klinken Landkreis Heidenheim gGmbH. Umweltbericht 2018 (Clinics Heidenheim Administrative District, Environemtal Declaration 2018). Available online: https://kliniken-heidenheim.de/2019_04-UE-Umweltbericht_2018.pdf (accessed on 10 August 2020).
- Klinikum Bremen Mitte. Umwelterklärung 2014 (Bremen Center Hospital, Environmental Declaration 2014). 2014. Available online: https://www.gesundheitnord.de/fileadmin/daten/kbm_pdf/oekologie/Umwelterkl%C3%A4rung_2014.pdf (accessed on 11 January 2021).
- Klinikum Chemnitz gGmbH. Umweltbericht 2018 (Hospital Chemnitz, Environmental Report 2018). Available online: https://www.klinikumchemnitz.de/fileadmin/user_upload/Institute_Abteilungen/Hygiene/Umweltbericht_Klinikum_Chemnitz_2018.pdf (accessed on 11 January 2021).
- Klinikum Kulmbach. Umwelterklärung 2017 (Hospital Kulmbach, Environmental Declaration 2017). Available online: https://www.klinikum-kulmbach.de/fileadmin/user_upload/Rubriken/Qualitaetsmanagement/Umwelterkl%C3%A4rung%202017%20blau%20Stand%2009.04.2018.pdf (accessed on 11 January 2021).
- Klinikum Landsberg am Lech. Umwelterklärung 2019 (Hospital Landsberg am Lech, Environmental Declaration 2019). 2019. Available online: https://www.klinikum-landsberg.de/wp-content/uploads/Umwelterklarung_Klinikum_Landsberg_2019.pdf (accessed on 11 January 2021).
- Klinikum Oldenburg. Umwelterklärung 2015 (Oldenburg Hospital, Environmental Declaration 2015). 2015. Available online: https://www.klinikum-oldenburg.de/files/kol_qmh_umwelterklaerung_2015.pdf (accessed on 18 August 2020).
- Starnberger Klinken GmbH. Umwelterklärung (Starnberg Hospitals, Environmental Declaration). 2019. Available online: https://www.klinikum-seefeld.de/files/2019-STA-PDFs/Umwelterklrung-2019.pdf#page=16&zoom=auto,-278,593 (accessed on 11 January 2021).
- Klinikum Saarbrücken. Team Blau Zeigt Grünes Engagement und Halbiert CO2-Ausstoß (Hospital Saarbrücken, Team Blue Shows Green Commitment and Halves CO2 Emissions). 2020. Available online: https://www.klinikum-saarbruecken.de/pressemitteilung/news/team-blau-zeigt-gruenes-engagement-und-halbiert-co2-ausstoss/?tx_news_pi1%5Bday%5D=24&tx_news_pi1%5Bmonth%5D=7&tx_news_pi1%5Byear%5D=2020&cHash=8fd02739e49a84111d3d7b4a8d3067f9 (accessed on 2 September 2020).
- Klinikverbund Kempten Oberallgäu gGmbH. Aktualisierte Umwelterklärung 2018 (Hospital Association Kempten Oberallgäu, Updated Environmental Declaration 2019). Available online: https://www.emas.de/fileadmin/user_upload/ue/reg/DE-104-00061_Klinikverbund-OA.pdf (accessed on 5 August 2020).
- Alfred Schmatz and Landkreis Passau Krankenhaus GmbH. Aktualisierte Umwelterklärung 2019. 2019. Available online: https://ge-passau.de/wp-content/uploads/2019/06/190227-akt.-Umwelterkl%C3%A4rung-2019.pdf (accessed on 11 January 2021).
- Kreisklinik Wolfratshausen gGmbH. Umwelterklärung 2019 (Community Hospital Wolfratshausen, Environmental Declaration 2019). 2019. Available online: https://www.kreisklinik-wolfratshausen.de/downloads/qm/Umwelterklaerung%202019%20KK%20Wolfratshausen.pdf (accessed on 11 January 2021).
- LVR-Klinik Bedburg-Hau. Aktualisierte Umwelterklärung 2020 (LVR-Hospital Bedburg-Hau, Updated Environmental Declaration 2020). 2020. Available online: https://klinik-bedburg-hau.lvr.de/media/lvr_klinik_bedburg_hau/dokumente/aktuelles/veroeffentlichungen/umwelt/Umwelterklaerung_LVR-Klinik_Bedburg-Hau_2020.pdf (accessed on 5 August 2020).
- LVR-Klinik Bonn. Aktualisierte Umwelterklärung 2019 (LVR-Hospital Bonn, Updated Environmental Declaration 2019). Available online: https://klinik-bonn.lvr.de/media/lvr_klinik_bonn/ueber_uns/qualitaetsmanagement/dokumente/umwelterklaerung-lvr-klinik-bonn.pdf (accessed on 11 January 2021).
- LVR Klinik Düren. Aktualisierte Umwelterklärung 2019 (LVR-Hospital Düren, Updated Environmental Declaration 2019). 2019. Available online: https://klinik-dueren.lvr.de/media/lvr_klinik_dueren/dokumente/pdf/umweltmanagement/LVR-Klinik_Dueren_Umwelterklaerung_2019.pdf (accessed on 11 August 2020).
- LVR-Klinikums Düsseldorf. Aktualisierte Umwelterklärung 2019 (LVR-hospital Düsseldorf, Updated Environmental Declaration 2019). 2019. Available online: https://klinikum-duesseldorf.lvr.de/media/lvr_klinik_duesseldorf/pdf_download/2019_3/Umwelterklaerung_2019x.pdf (accessed on 18 August 2020).
- LVR Klinik Köln. Aktualisierte Umwelterklärung 2020 (LVR-Hospital Köln, Updated Environmental Declaration 2020). 2020. Available online: https://klinik-koeln.lvr.de/media/lvr_klinik_koeln/downloaddateien/Umwelterklaerung_2017-LVR-Klinik-Koeln.pdf (accessed on 5 August 2020).
- LVR-Klinik Langenfeld. Konsolidierte EMAS-Umwelterklärung 2020 (LVR-Hospital Langenfeld, Consolidated EMAS Environmental Declaration 2020). 2020. Available online: https://klinik-langenfeld.lvr.de/media/lvr_klinik_langenfeld/first_spirit/ueberuns/1.5_qualitaetsmanagement_1/Umwerlterklaerung_2019.pdf (accessed on 11 August 2020).
- LVR-Klinik Viersen. Konsolidierte Umwelterklärung 2018 (LVR-Hospital Viersen, Consolidated Environmental Declaration 2019). 2018. Available online: https://klinik-viersen.lvr.de/media/lvr_klinik_viersen/klinik/qualitaetsmanagement/umwelterklaerung/Umwelterklaerung_2018.pdf (accessed on 5 August 2020).
- LVR-Klinik Mönchengladbach. Aktualisierte Umwelterklärung 2019 (LVR-Hospital Mönchengladbach, Updated Environmental Declaration 2019). 2019. Available online: https://klinik-moenchengladbach.lvr.de/media/lvr_klinik_moenchengladbach/ueber_uns/umweltmanagement/LVR_Moenchengladbach_Umwelterklaerung_2019.pdf (accessed on 5 August 2020).
- LWL-Klinik Lengerich. Aktualisierte Umwelterklärung 2019 (LWL-Hospital Lengerich, Updated Environmental Declaration 2019. Available online: https://www.lwl-klinik-lengerich.de/media/filer_public/b1/b1/b1b18fb6-c4ac-4628-93fe-111066ec2a58/umwelterklaerung_le_2019.pdf (accessed on 11 January 2021).
- LWL-Klinik Münster. Umwelterklärung 2017 (LWL-Hospital Münster, Environmental Declaration 2017). 2017. Available online: https://www.emas.de/fileadmin/user_upload/ue/reg/DE-156-00070_LWL-Klinik-Muenster.pdf (accessed on 11 January 2021).
- Axel, F.; Susanne, D.; Dietmar, P. Gemeinsame Aktualisierte Umwelterklärung 2019 der München Klinik (MüK) Standorte: Bogenhausen Harlaching Neuperlach Schwabing Thalkirchner Straße Akademie; (Joint updated Environmental Statement 2019 of München Klinik (MüK) Locations: Bogenhausen, Harlaching, Neuperlach, Schwabing, Thalkirchner Straße Akademie); München Klinik: Munich, Germany, 2019. [Google Scholar]
- Orthopädische Universitätsklinik Friedrichsheim. Umwelterklärung 2019 (Orthopedic University Hospital Friedrichsheim, Environmental Declaration 2019). 2019. Available online: https://orthopaedische-universitaetsklinik.de/fileadmin/pdf/Umwelterklaerung_OUF_2019.pdf (accessed on 11 August 2020).
- Rhön Klinikum, AG. Umwelt—Effizientes Umweltmanagement (Rhön Hospital Corporation, Environment—Efficient Environmental Management). 2020. Available online: https://www.rhoen-klinikum-ag.com/konzern/verantwortung/fortschrittsberichte/fortschrittsbericht-2015/umwelt.html (accessed on 18 August 2020).
- Sankt Josef-Hospital Xanten. Umwelterklärung 2018 des Sankt Josef-Hospital Xanten (Environmental Declaration 2018 of the Sankt Josef-Hospital Xanten). 2018. Available online: https://www.sankt-josef-hospital.de/umwelterklaerung/ (accessed on 5 August 2020).
- St.Barbara-Klinik Hamm-Heessen GmbH. Umwelterklärung 2008 (St. Barbara Hospital Hamm-Heessen GmbH, Environmental Declaration 2008). Available online: https://www.barbaraklinik.de/fileadmin/daten/mandanten/sbh/wir-ueber-uns/dateien/Umwelterkl%C3%A4rung_2008_Brosch%C3%BCre.pdf (accessed on 1 November 2020).
- Städtisches Klinikum Karlsruhe. Konsolidierte Umwelterklärung 2019 (Municipal Hospital Karlsruhe, Consolidated Environmental Declaration 2019). 2019. Available online: https://www.klinikum-karlsruhe.de/fileadmin/Redaktion/UEber_uns/Zertifikate_und_Auszeichnungen/2019_11_13__EMAS-Umwelterkaerung_2019_komplett.pdf (accessed on 11 January 2021).
- Universitätsklinikum Jena. Umweltschutzbericht 2018 (University Hospital Jena, Environmental Protection Report 2018). 2019. Available online: https://www.uniklinikum-jena.de/MedWeb_media/Corporate+Design+Bilder/Sonstige+Bilder+und+Dateien/Umweltbericht+2018.pdf (accessed on 11 January 2021).
| Source | Hospitals with GHG Emission Reports | Hospitals for Detailed Analysis | |
|---|---|---|---|
| Peer-reviewed literature | Scopus | 0 | 0 |
| PubMed | 0 | 0 | |
| Web of Science | 0 | 0 | |
| Specific databases | Eco Management and Audit Scheme register | 49 | 49 |
| Sustainability Disclosure Database | 0 | 0 | |
| Carbon Disclosure Project | 0 | 0 | |
| Targeted websites | Websites of all full members of “Verband der Universitätsklinika Deutschlands e.V.” | 2 | 2 |
| Websites of hospital companies with more than 150,000 cases/year | 175 | 5 | |
| Websites of hospitals that participated in “KLIK–Klimamanager für Kliniken” | 0 | 0 | |
| Web search engines | 6 | 6 | |
| Google Scholar | 0 | 0 | |
| Total | 232 | 62 | |
| Category | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Type of Facility |
|
|
| Country |
|
|
| Language |
|
|
| Presented numbers |
|
|
| Year of reporting |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quitmann, C.; Sauerborn, R.; Herrmann, A. Gaps in Reporting Greenhouse Gas Emissions by German Hospitals—A Systematic Grey Literature Review. Sustainability 2021, 13, 1430. https://doi.org/10.3390/su13031430
Quitmann C, Sauerborn R, Herrmann A. Gaps in Reporting Greenhouse Gas Emissions by German Hospitals—A Systematic Grey Literature Review. Sustainability. 2021; 13(3):1430. https://doi.org/10.3390/su13031430
Chicago/Turabian StyleQuitmann, Claudia, Rainer Sauerborn, and Alina Herrmann. 2021. "Gaps in Reporting Greenhouse Gas Emissions by German Hospitals—A Systematic Grey Literature Review" Sustainability 13, no. 3: 1430. https://doi.org/10.3390/su13031430
APA StyleQuitmann, C., Sauerborn, R., & Herrmann, A. (2021). Gaps in Reporting Greenhouse Gas Emissions by German Hospitals—A Systematic Grey Literature Review. Sustainability, 13(3), 1430. https://doi.org/10.3390/su13031430







