Effects of Functional Strength Training on Functional Movement and Balance in Middle-Aged Adults
Abstract
1. Introduction
2. Materials and Methods
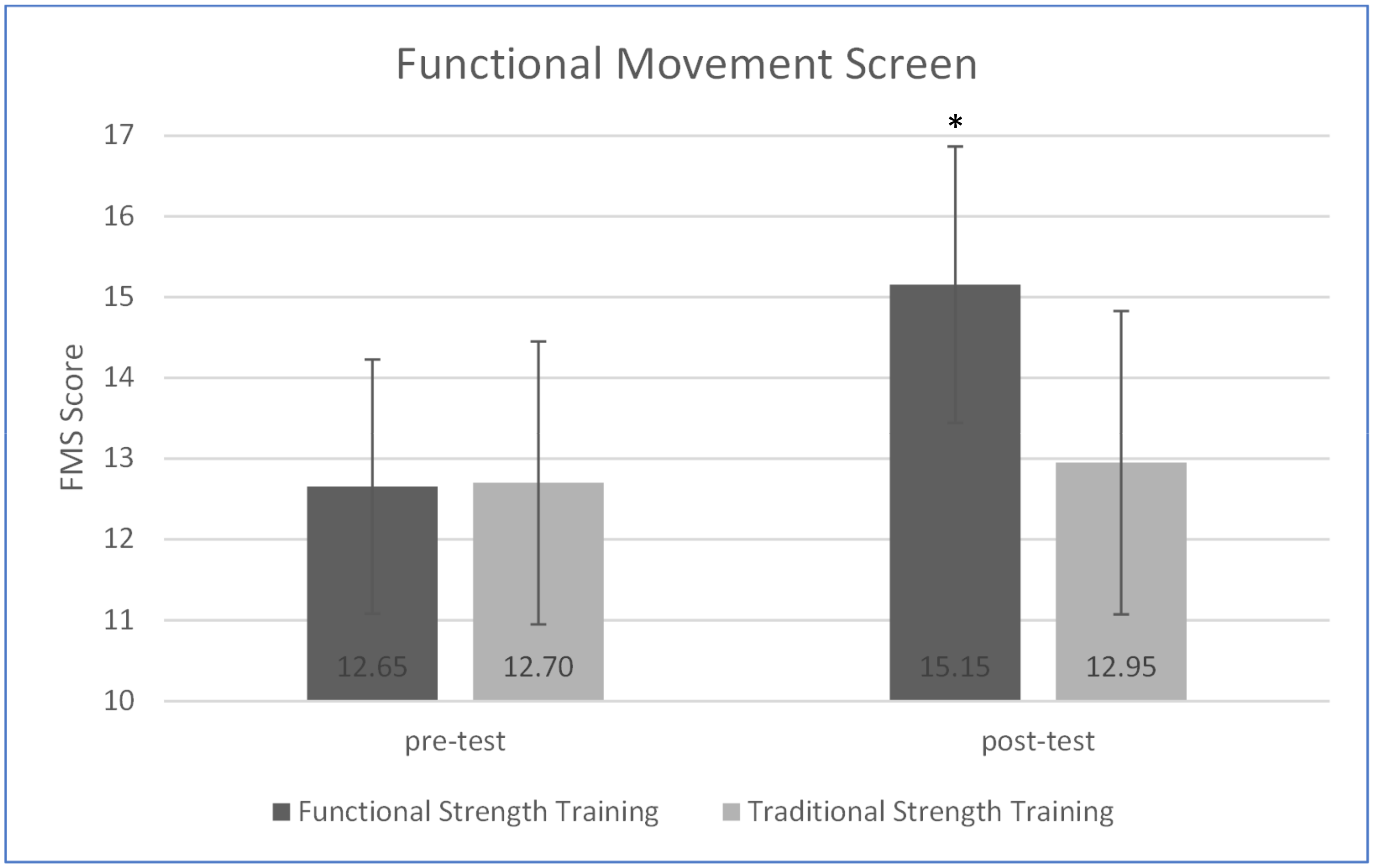
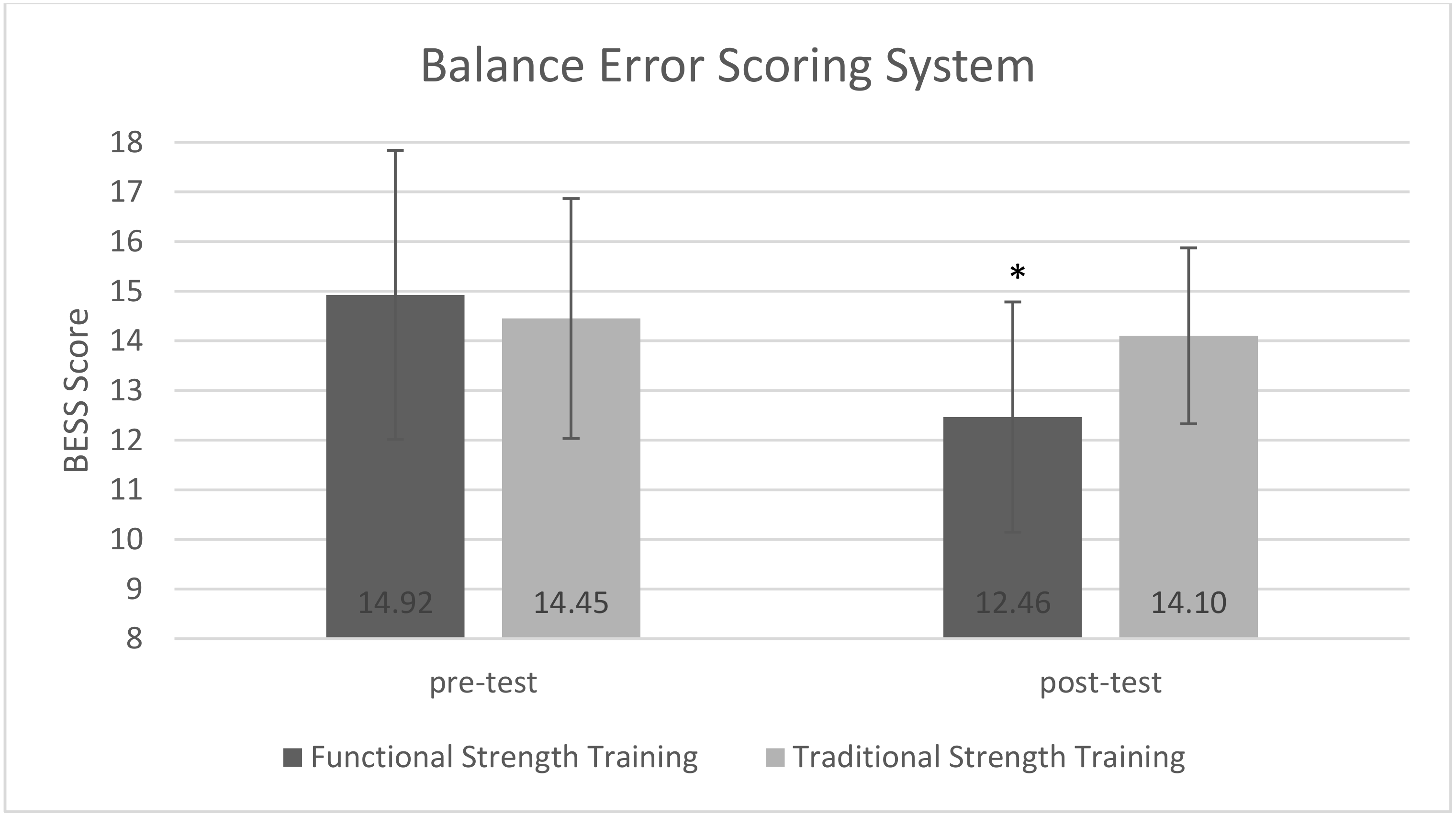
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Melton, L.; Khosla, S.; Crowson, C.S.; O’Connor, M.K.; O’Fallon, W.M.; Riggs, B.L. Epidemiology of sarcopenia. J. Am. Geriatr. Soc. 2000, 48, 625–630. [Google Scholar] [CrossRef]
- Janssen, I.; Heymsfield, S.B.; Wang, Z.; Ross, R. Skeletal muscle mass and distribution in 468 men and women aged 18–88 yr. J. Appl. Physiol. 2000, 89, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, D.; Visser, M.; De Meersman, R.E.; Sepúlveda, D.; Baumgartner, R.N.; Pierson, R.N.; Harris, T.; Heymsfield, S.B. Appendicular skeletal muscle mass: Effects of age, gender, and ethnicity. J. Appl. Physiol. 1997, 83, 229–239. [Google Scholar] [CrossRef]
- Goodpaster, B.H.; Park, S.W.; Harris, T.B.; Kritchevsky, S.B.; Nevitt, M.; Schwartz, A.V.; Simonsick, E.M.; Tylavsky, F.A.; Visser, M.; Newman, A.B. The loss of skeletal muscle strength, mass, and quality in older adults: The health, aging and body composition study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2006, 61, 1059–1064. [Google Scholar] [CrossRef]
- Study, H.A.C. Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am. J. Clin. Nutr. 2009, 90, 1579–1585. [Google Scholar] [CrossRef]
- McLean, R.R.; Shardell, M.D.; Alley, D.E.; Cawthon, P.M.; Fragala, M.S.; Harris, T.B.; Kenny, A.M.; Peters, K.W.; Ferrucci, L.; Guralnik, J.M. Criteria for clinically relevant weakness and low lean mass and their longitudinal association with incident mobility impairment and mortality: The foundation for the National Institutes of Health (FNIH) sarcopenia project. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2014, 69, 576–583. [Google Scholar] [CrossRef] [PubMed]
- Papa, E.V.; Dong, X.; Hassan, M. Skeletal muscle function deficits in the elderly: Current perspectives on resistance training. J. Nat. Sci. 2017, 3, e272. [Google Scholar]
- Visser, M.; Goodpaster, B.H.; Kritchevsky, S.B.; Newman, A.B.; Nevitt, M.; Rubin, S.M.; Simonsick, E.M.; Harris, T.B. Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2005, 60, 324–333. [Google Scholar] [CrossRef]
- Arnold, P.; Bautmans, I. The influence of strength training on muscle activation in elderly persons: A systematic review and meta-analysis. Exp. Gerontol. 2014, 58, 58–68. [Google Scholar] [CrossRef]
- Borde, R.; Hortobágyi, T.; Granacher, U. Dose–response relationships of resistance training in healthy old adults: A systematic review and meta-analysis. Sports Med. 2015, 45, 1693–1720. [Google Scholar] [CrossRef]
- Cadore, E.L.; Casas-Herrero, A.; Zambom-Ferraresi, F.; Idoate, F.; Millor, N.; Gómez, M.; Rodriguez-Mañas, L.; Izquierdo, M. Multicomponent exercises including muscle power training enhance muscle mass, power output, and functional outcomes in institutionalized frail nonagenarians. Age 2014, 36, 773–785. [Google Scholar] [CrossRef] [PubMed]
- Peterson, M.D.; Rhea, M.R.; Sen, A.; Gordon, P.M. Resistance exercise for muscular strength in older adults: A meta-analysis. Ageing Res. Rev. 2010, 9, 226–237. [Google Scholar] [CrossRef]
- Silva, R.B.; Eslick, G.D.; Duque, G. Exercise for falls and fracture prevention in long term care facilities: A systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 2013, 14, 685–689. [Google Scholar] [CrossRef] [PubMed]
- Steib, S.; Schoene, D.; Pfeifer, K. Dose-response relationship of resistance training in older adults: A meta-analysis. Med. Sci. Sports Exerc. 2010, 42, 902–914. [Google Scholar] [CrossRef] [PubMed]
- Arslan, E.; Aras, D. Comparison of body composition, heart rate variability, aerobic and anaerobic performance between competitive cyclists and triathletes. J. Phys. Ther. Sci. 2016, 28, 1325–1329. [Google Scholar] [CrossRef]
- Pereira, P.C.; Medeiros, R.D.; Santos, A.; Oliveira, L.; Aniceto, R.R.; Júnior, A.A.; Nascimento, J.; Sousa, M. Efeitos do treinamento funcional com cargas sobre a composição corporal: Um estudo experimental em mulheres fisicamente inativas. Motricidade 2012, 8, 42–52. [Google Scholar] [CrossRef]
- Pinto, R.S.; Correa, C.S.; Radaelli, R.; Cadore, E.L.; Brown, L.E.; Bottaro, M. Short-term strength training improves muscle quality and functional capacity of elderly women. Age 2014, 36, 365–372. [Google Scholar] [CrossRef]
- Aras, D.; Akalan, C. Sport climbing as a means to improve health-related physical fitness parameters. J. Sports Med. Phys. Fit. 2015, 56, 1304–1310. [Google Scholar]
- Zhao, R.; Zhao, M.; Xu, Z. The effects of differing resistance training modes on the preservation of bone mineral density in postmenopausal women: A meta-analysis. Osteoporos. Int. 2015, 26, 1605–1618. [Google Scholar] [CrossRef]
- Paoli, A.; Gentil, P.; Moro, T.; Marcolin, G.; Bianco, A. Resistance training with single vs. multi-joint exercises at equal total load volume: Effects on body composition, cardiorespiratory fitness, and muscle strength. Front. Physiol. 2017, 8, 1105. [Google Scholar] [CrossRef]
- Pedersen, B.K.; Saltin, B. Exercise as medicine–evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 2015, 25, 1–72. [Google Scholar] [CrossRef] [PubMed]
- Boshuizen, H.C.; Stemmerik, L.; Westhoff, M.H.; Hopman-Rock, M. The effects of physical therapists’ guidance on improvement in a strength-training program for the frail elderly. J. Aging Phys. Act. 2005, 13, 5–22. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.-J.; Latham, N. Can progressive resistance strength training reduce physical disability in older adults? A meta-analysis study. Disabil. Rehabil. 2011, 33, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Gudlaugsson, J.; Gudnason, V.; Aspelund, T.; Siggeirsdottir, K.; Olafsdottir, A.S.; Jonsson, P.V.; Arngrimsson, S.A.; Harris, T.B.; Johannsson, E. Effects of a 6-month multimodal training intervention on retention of functional fitness in older adults: A randomized-controlled cross-over design. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 107. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.A.; You, J.H.; Kim, D.A.; Lee, M.J.; Hwang, P.W.; Lee, N.G.; Park, J.J.; Lee, D.R.; Kim, H.-K. Effects of functional movement strength training on strength, muscle size, kinematics, and motor function in cerebral palsy: A 3-month follow-up. NeuroRehabilitation 2013, 32, 287–295. [Google Scholar] [CrossRef]
- Paoli, A.; Moro, T.; Bianco, A. Lift weights to fight overweight. Clin. Physiol. Funct. Imaging 2015, 35, 1–6. [Google Scholar] [CrossRef]
- Steele, J.; Fisher, J.; Skivington, M.; Dunn, C.; Arnold, J.; Tew, G.; Batterham, A.M.; Nunan, D.; O’Driscoll, J.M.; Mann, S. A higher effort-based paradigm in physical activity and exercise for public health: Making the case for a greater emphasis on resistance training. BMC Public Health 2017, 17, 300. [Google Scholar] [CrossRef]
- De Matos, D.G.; Mazini, F.M.; Moreira, O.C.; De Oliveira, C.E.; De Oliveira, V.G.; Da Silva-Grigoletto, M.E.; Aidar, F.J. Effects of eight weeks of functional training in the functional autonomy of elderly women: A pilot study. J. Sports Med. Phys. Fit. 2017, 57, 272–277. [Google Scholar]
- Do Rosario, J.T.; da Fonseca Martins, N.S.; Peixinho, C.C.; Oliveira, L.F. Effects of functional training and calf stretching on risk of falls in older people: A pilot study. J. Aging Phys. Act. 2017, 25, 228–233. [Google Scholar] [CrossRef]
- Ives, J.C.; Shelley, G.A. Psychophysics in functional strength and power training: Review and implementation framework. J. Strength Cond. Res. 2003, 17, 177–186. [Google Scholar] [CrossRef]
- Weiss, T.; Kreitinger, J.; Wilde, H.; Wiora, C.; Steege, M.; Dalleck, L.; Janot, J. Effect of functional resistance training on muscular fitness outcomes in young adults. J. Exerc. Sci. Fit. 2010, 8, 113–122. [Google Scholar] [CrossRef]
- Beckham, S.G.; Harper, M. Functional training: Fad or here to stay? ACSM’s Health Fit. J. 2010, 14, 24–30. [Google Scholar] [CrossRef]
- Cook, G.; Burton, L.; Hoogenboom, B.J.; Voight, M. Functional movement screening: The use of fundamental movements as an assessment of function-part 1. Int. J. Sports Phys. Ther. 2014, 9, 396–409. [Google Scholar] [PubMed]
- Cook, G.; Burton, L.; Hoogenboom, B.J.; Voight, M. Functional movement screening: The use of fundamental movements as an assessment of function-part 2. Int. J. Sports Phys. Ther. 2014, 9, 549–563. [Google Scholar] [PubMed]
- Bell, D.R.; Guskiewicz, K.M.; Clark, M.A.; Padua, D.A. Systematic review of the balance error scoring system. Sports Health 2011, 3, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Lagally, K.M.; Gallagher, K.I.; Robertson, R.J.; Gearhart, R.; Goss, F.L. Ratings of perceived exertion during low-and high-intensity resistance exercise by young adults. Percept. Mot. Ski. 2002, 94, 723–731. [Google Scholar] [CrossRef]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.-M.; Nieman, D.C.; Swain, D.P. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Fragala, M.S.; Cadore, E.L.; Dorgo, S.; Izquierdo, M.; Kraemer, W.J.; Peterson, M.D.; Ryan, E.D. Resistance training for older adults: Position statement from the national strength and conditioning association. J. Strength Cond. Res. 2019, 33, 2019–2052. [Google Scholar] [CrossRef]
- Yildiz, S.; Pinar, S.; Gelen, E. Effects of 8-week functional vs. Traditional training on athletic performance and functional movement on prepubertal tennis players. J. Strength Cond. Res. 2019, 33, 651–661. [Google Scholar] [CrossRef]
- Liao, T.; Li, L.; Wang, Y.T. Effects of Functional Strength Training Program on Movement Quality and Fitness Performance Among Girls Aged 12–13 Years. J. Strength Cond. Res. 2019, 33, 1534–1541. [Google Scholar] [CrossRef]
- Sawczyn, M. Effects of a periodized functional strength training program (FST) on Functional Movement Screen (FMS) in physical education students. Phys. Educ. Stud. 2020, 24, 162–167. [Google Scholar] [CrossRef]
- Bonazza, N.A.; Smuin, D.; Onks, C.A.; Silvis, M.L.; Dhawan, A. Reliability, validity, and injury predictive value of the functional movement screen: A systematic review and meta-analysis. Am. J. Sports Med. 2017, 45, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos Bunn, P.; Rodrigues, A.I.; da Silva, E.B. The association between the functional movement screen outcome and the incidence of musculoskeletal injuries: A systematic review with meta-analysis. Phys. Ther. Sport 2019, 35, 146–158. [Google Scholar] [CrossRef] [PubMed]
- Nadler, S.F.; Moley, P.; Malanga, G.A.; Rubbani, M.; Prybicien, M.; Feinberg, J.H. Functional deficits in athletes with a history of low back pain: A pilot study. Arch. Phys. Med. Rehabil. 2002, 83, 1753–1758. [Google Scholar] [CrossRef]
- Tomeleri, C.M.; Ribeiro, A.S.; Souza, M.F.; Schiavoni, D.; Schoenfeld, B.J.; Venturini, D.; Barbosa, D.S.; Landucci, K.; Sardinha, L.B.; Cyrino, E.S. Resistance training improves inflammatory level, lipid and glycemic profiles in obese older women: A randomized controlled trial. Exp. Gerontol. 2016, 84, 80–87. [Google Scholar] [CrossRef]
- De Resende-Neto, A.G.; Andrade, B.C.O.; Cyrino, E.S.; Behm, D.G.; De-Santana, J.M.; Da Silva-Grigoletto, M.E. Effects of functional and traditional training in body composition and muscle strength components in older women: A randomized controlled trial. Arch. Gerontol. Geriatr. 2019, 84, 103902. [Google Scholar] [CrossRef]
- Hill, M.W.; Duncan, M.J.; Price, M.J. The emergence of age-related deterioration in dynamic, but not quiet standing balance abilities among healthy middle-aged adults. Exp. Gerontol. 2020, 140, 111076. [Google Scholar] [CrossRef]
- Freund, J.E.; Stetts, D.M.; Oostindie, A.; Shepherd, J.; Vallabhajosula, S. Lower Quarter Y-Balance Test in healthy women 50–79 years old. J. Women Aging 2019, 31, 475–491. [Google Scholar] [CrossRef] [PubMed]
- Roman-Liu, D. Age-related changes in the range and velocity of postural sway. Arch. Gerontol. Geriatr. 2018, 77, 68–80. [Google Scholar] [CrossRef]
- Aras, D.; Kitano, K.; Phipps, A.M.; Enyart, M.R.; Akça, F.; Koceja, D.M.; Ewert, A.W. The Comparison of Postural Balance Level between Advanced Sport Climbers and Sedentary Adults. Int. J. Appl. Exerc. Physiol. 2018, 7, 1–9. [Google Scholar]
- Johansson, J.; Nordström, A.; Gustafson, Y.; Westling, G.; Nordström, P. Increased postural sway during quiet stance as a risk factor for prospective falls in community-dwelling elderly individuals. Age Ageing 2017, 46, 964–970. [Google Scholar] [CrossRef] [PubMed]
- Sipe, C.L.; Ramey, K.D.; Plisky, P.P.; Taylor, J.D. Y-balance test: A valid and reliable assessment in older adults. J. Aging Phys. Act. 2019, 27, 663–669. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, M.M.; Teixeira, L.A.C.; Franchini, E.; Takito, M.Y. Functional vs. strength training in adults: Specific needs define the best intervention. Int. J. Sports Phys. Ther. 2013, 8, 34–43. [Google Scholar]
- De Vreede, P.L.; Samson, M.M.; Van Meeteren, N.L.; Duursma, S.A.; Verhaar, H.J. Functional-task exercise versus resistance strength exercise to improve daily function in older women: A randomized, controlled trial. J. Am. Geriatr. Soc. 2005, 53, 2–10. [Google Scholar] [CrossRef] [PubMed]


| FST (n = 26) | TST (n = 20) | Total Participants (n = 46) | |
|---|---|---|---|
| Age (years) | 51.55 ± 3.73 | 52.85 ± 4.01 | 52.08 ± 3.89 |
| Body height (cm) | 168.69 ± 8.8 | 166.9 ± 9.98 | 167.9 ± 9.27 |
| Body mass (kg) | 75.88 ± 12.18 | 76.15 ± 10.45 | 76.01 ± 11.34 |
| Body mass index (kg × m−2) | 25.52 ± 2.56 | 25.89 ± 6.20 | 26.82 ± 2.08 |
| Body Fat% | 27.61 ± 3.29 | 26.6 ± 3.6 | 27.15 ± 3.43 |
| Within-Group Differences | Between-Group Differences | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| FST (n = 26) | TST (n = 20) | TST | FST (n = 20) | ||||||||
| Pre (Mean SD) | Post (Mean SD) | % | p | Pre (Mean SD) | Post (Mean SD) | % | p | Difference | Difference | p | |
| FMS | 12.65 ± 1.5 | 15.11 ± 1.72 | 19.45 | 0.001 | 12.7 ± 1.75 | 12.95 ± 1.97 | 1.97 | 0.204 | −2.5 ± 1.72 | 0.25 ± 0.85 | 0.001 |
| BESS | 14.92 ± 2.91 | 12.46 ± 2.31 | −16.49 | 0.001 | 14.45 ± 2.41 | 14.1 ± 1.77 | −2.42 | 0.130 | 2.46 ± 1.98 | 0.35 ± 0.98 | 0.001 |
| Body mass | 75.68 ± 12.18 | 73.53 ± 11.95 | −2.84 | 0.001 | 76.15 ± 10.45 | 76.66 ± 10.17 | 0.69 | 0.047 | 2.34 ± 2.27 | 0.5 ± 1.05 | 0.001 |
| BMI | 26.52 ± 2.56 | 25.69 ± 2.55 | −3.12 | 0.001 | 25.89 ± 6.2 | 26.09 ± 6.25 | 0.77 | 0.053 | 0.82 ± 0.79 | 0.25 ± 0.63 | 0.001 |
| Body Fat% | 27.61 ± 3.29 | 23.66 ± 3.45 | −14.3 | 0.001 | 26.6 ± 3.6 | 26.27 ± 3.24 | −1.24 | 0.32 | 3.95 ± 4.1 | 0.32 ± 1.42 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guler, O.; Tuncel, O.; Bianco, A. Effects of Functional Strength Training on Functional Movement and Balance in Middle-Aged Adults. Sustainability 2021, 13, 1074. https://doi.org/10.3390/su13031074
Guler O, Tuncel O, Bianco A. Effects of Functional Strength Training on Functional Movement and Balance in Middle-Aged Adults. Sustainability. 2021; 13(3):1074. https://doi.org/10.3390/su13031074
Chicago/Turabian StyleGuler, Ozkan, Oguzhan Tuncel, and Antonino Bianco. 2021. "Effects of Functional Strength Training on Functional Movement and Balance in Middle-Aged Adults" Sustainability 13, no. 3: 1074. https://doi.org/10.3390/su13031074
APA StyleGuler, O., Tuncel, O., & Bianco, A. (2021). Effects of Functional Strength Training on Functional Movement and Balance in Middle-Aged Adults. Sustainability, 13(3), 1074. https://doi.org/10.3390/su13031074







