Sustainable Hospital Management by a Cross SWOT Analysis in a Medium-Sized Hospital
Abstract
:1. Introduction
2. Materials and Methods
3. Results
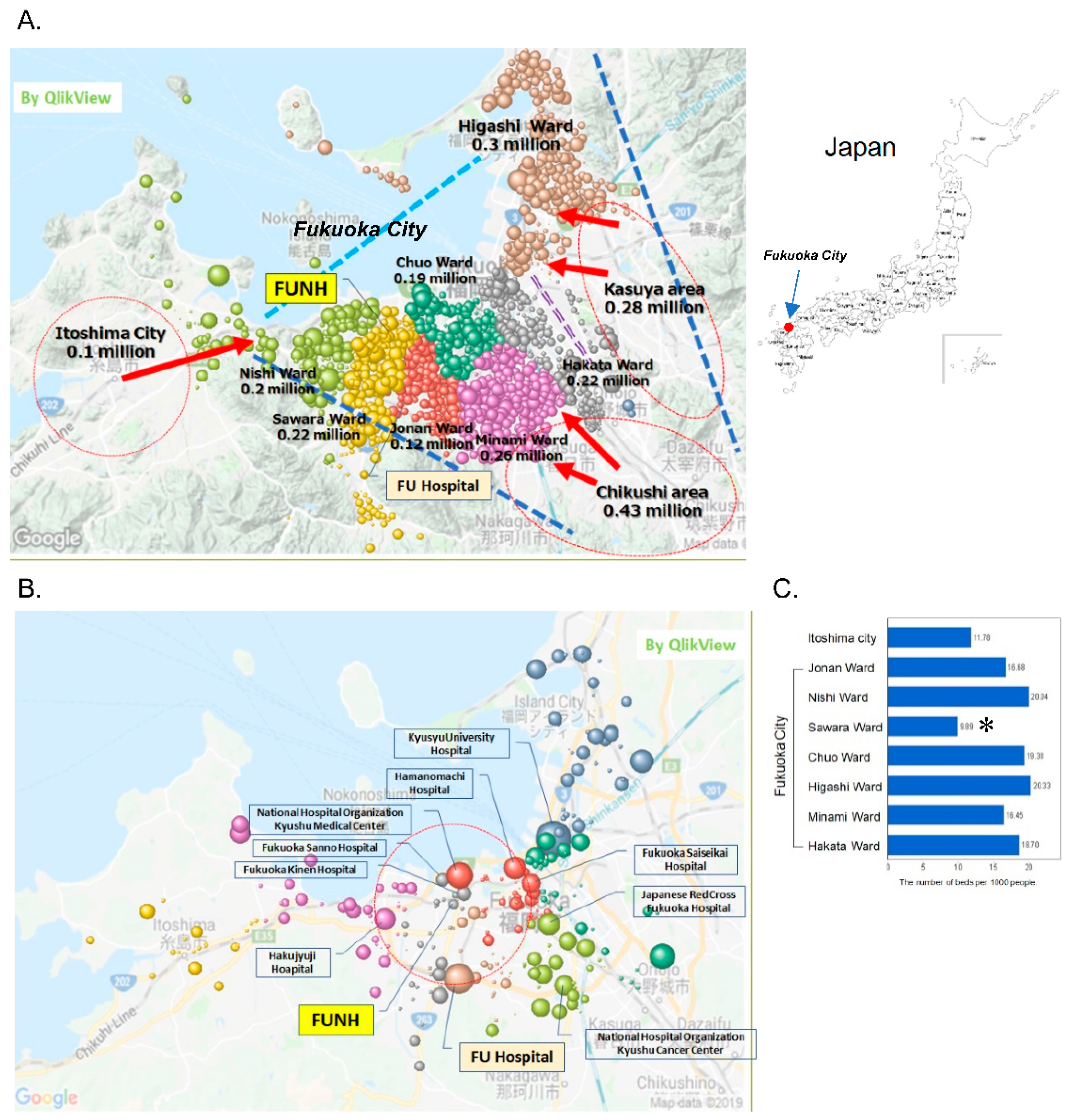
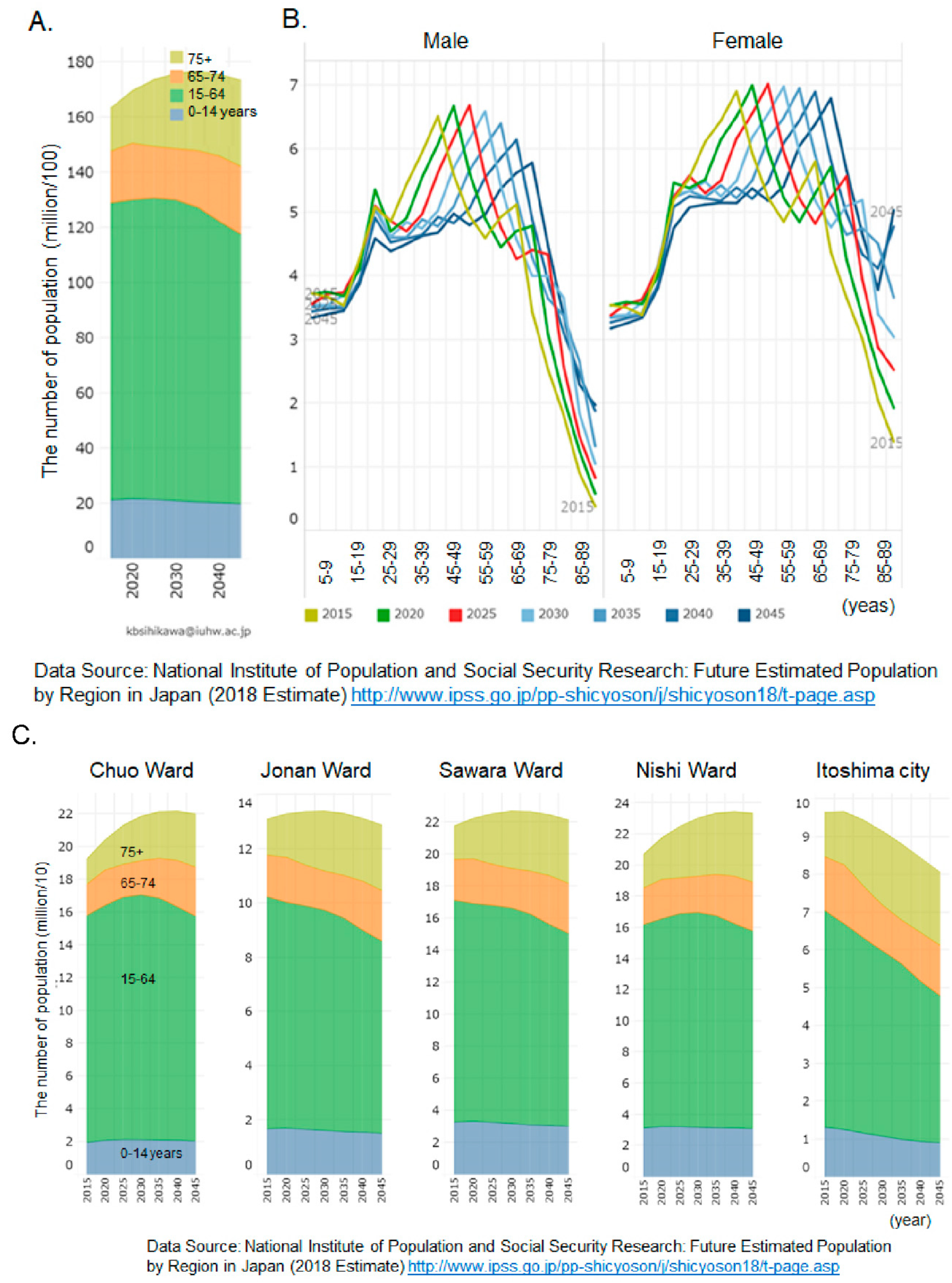
3.1. Vital Statistics of Fukuoka City and Its Suburbs, Distribution of Hospitals, Number of Beds and Population Forecast in Fukuoka-Itoshima Secondary Medical Area
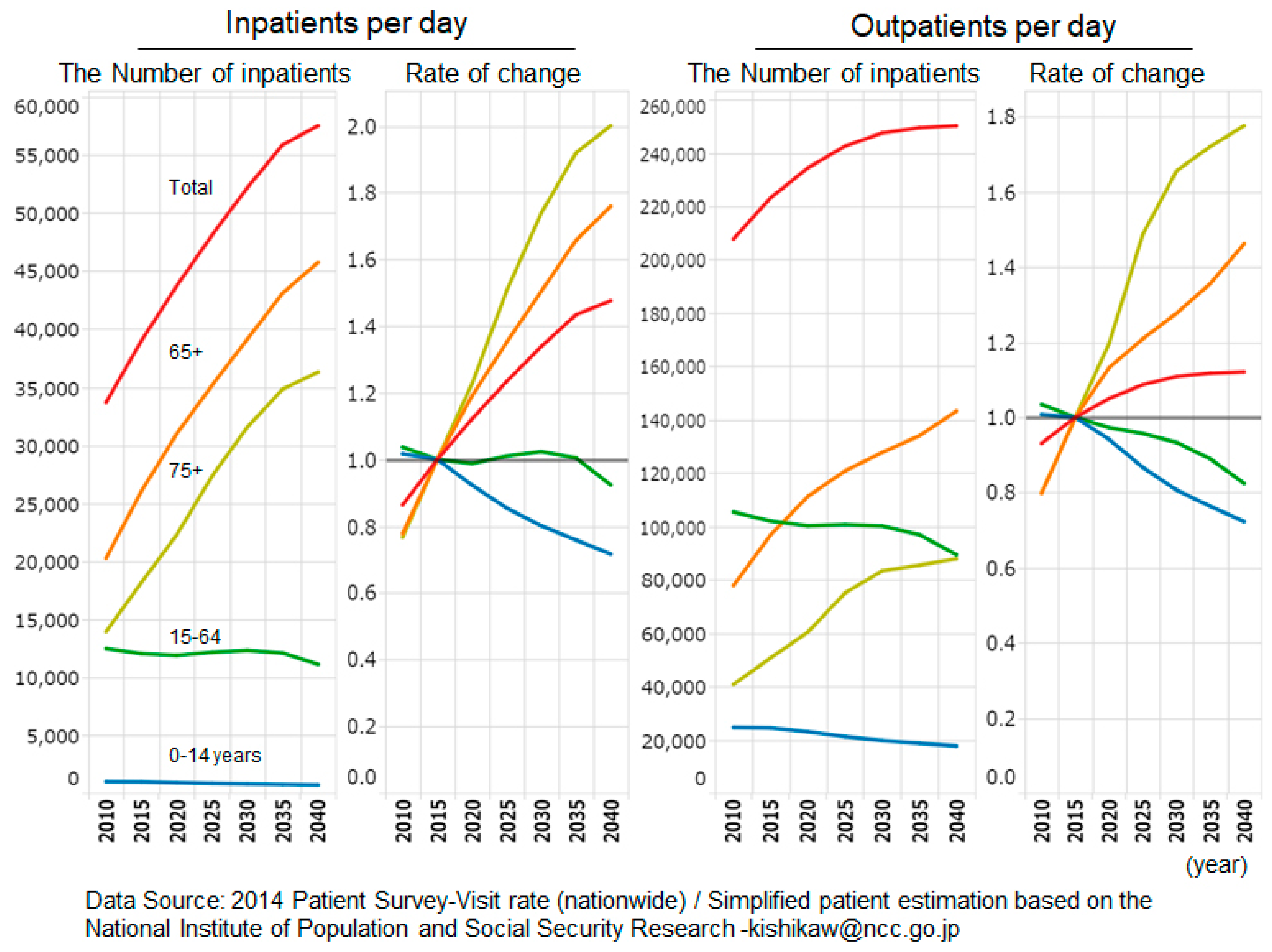
3.2. Medical Dynamics in Fukuoka City and Its Suburbs
3.3. Numbers of Outpatients and Inpatients for All Patients, Males and Females, at FUNH
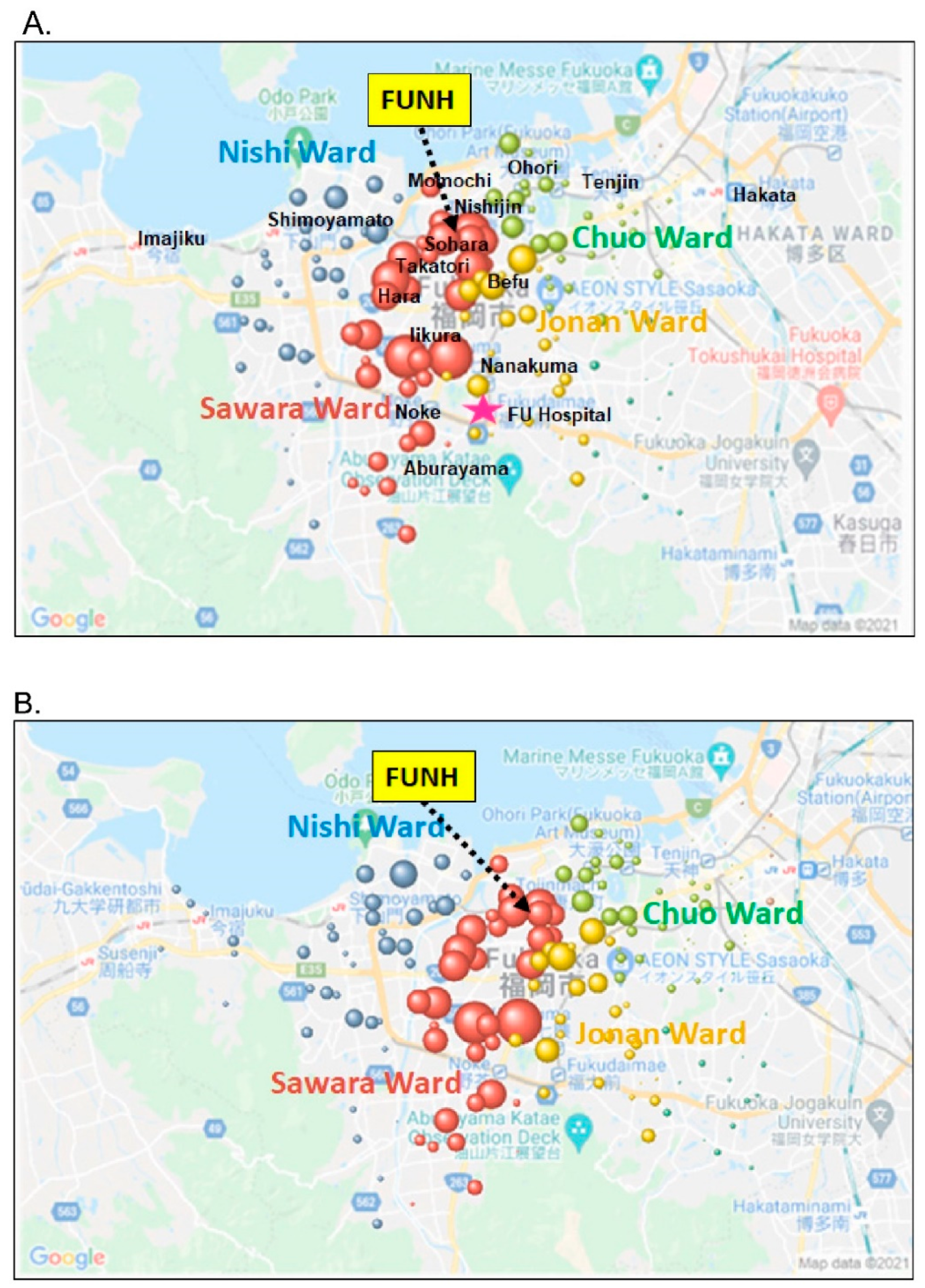
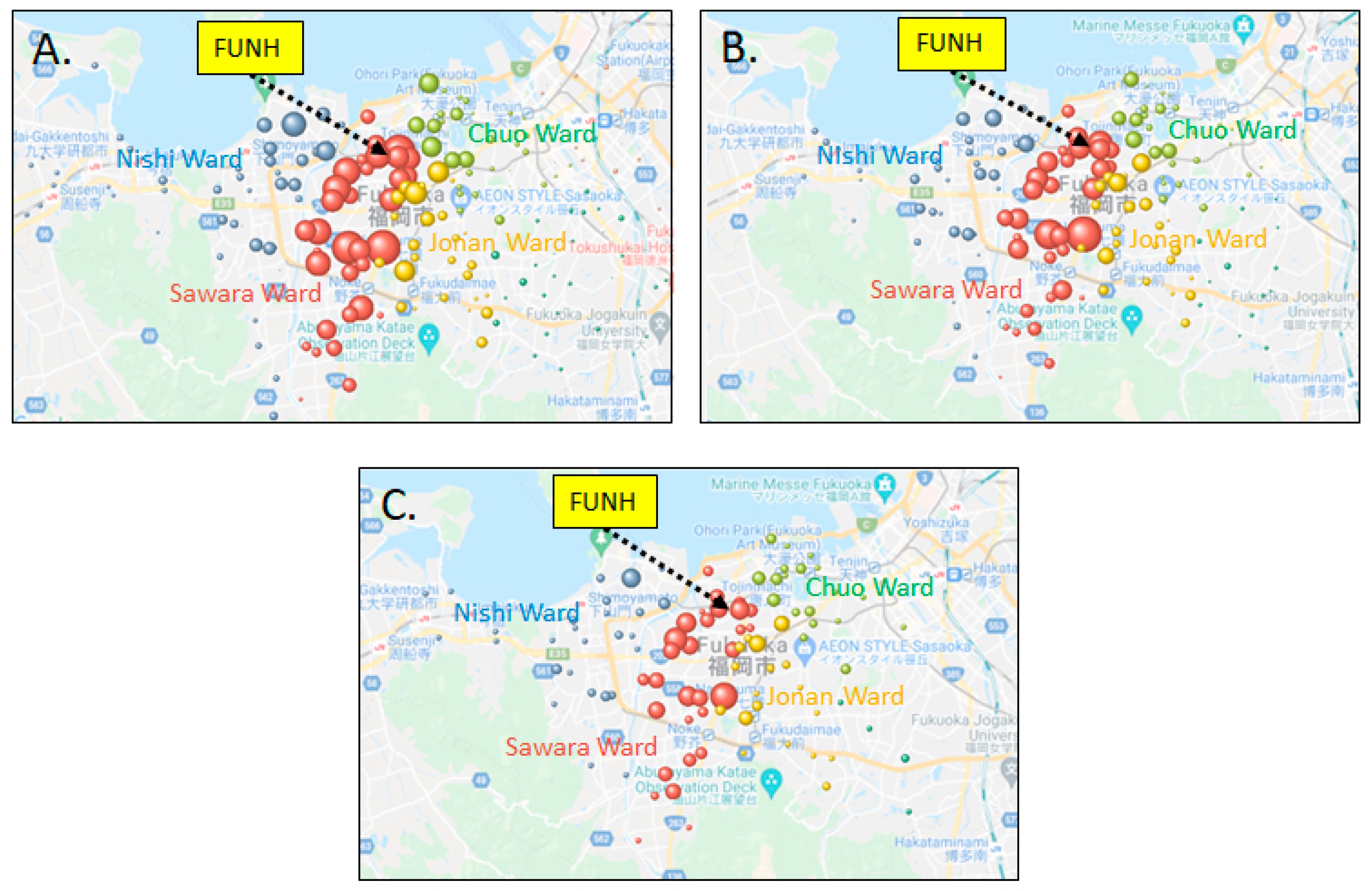
3.4. Regional Distribution of Outpatients and Inpatients at FUNH in 2018–2020
3.5. Regional Distribution of All Outpatients, All Inpatients and Inpatients with Heart Failure at the Division of Cardiology at FUNH in 2018–2020
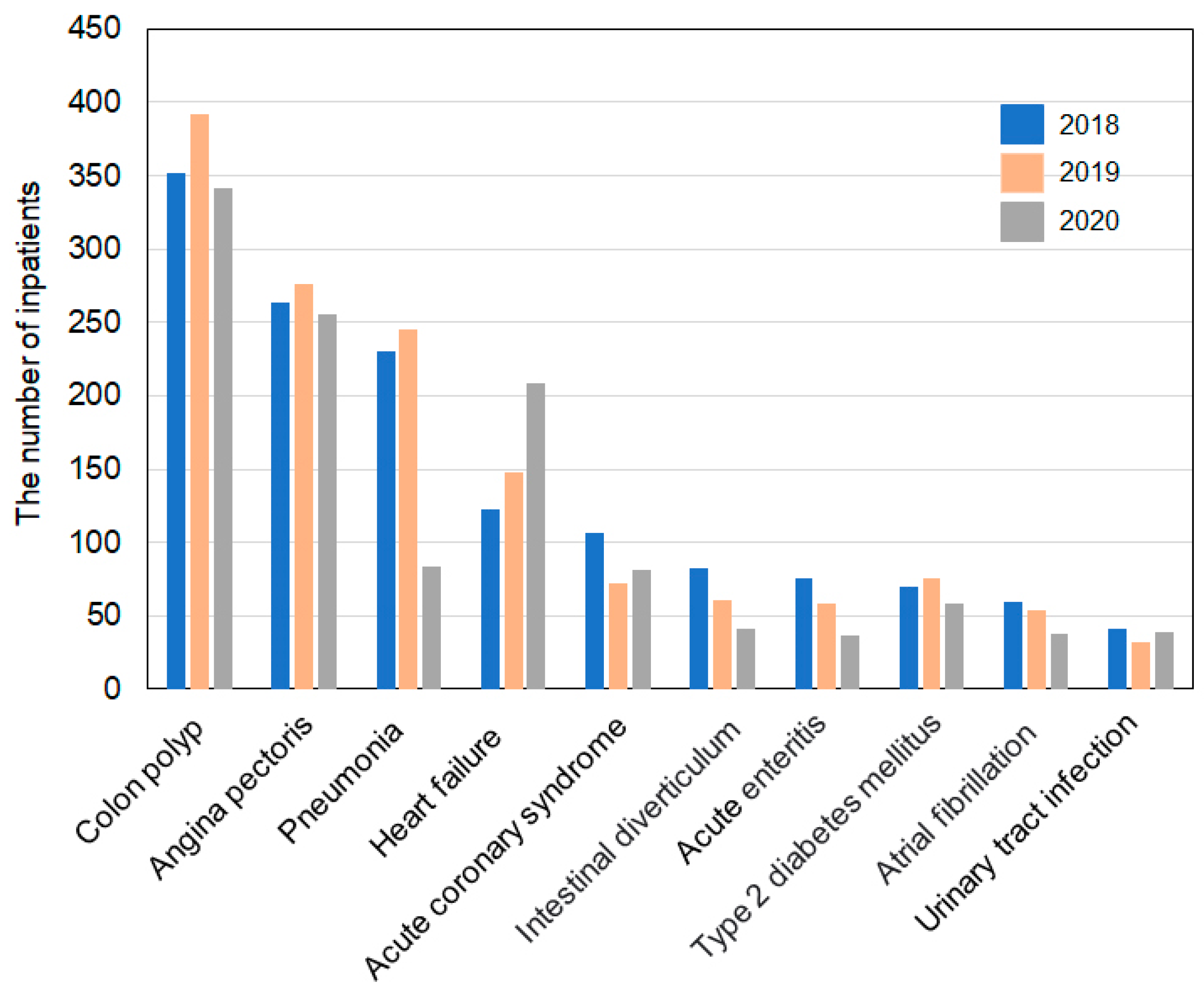
3.6. Three-Year Trends in Major Outpatient and Inpatient Diseases at FUNH
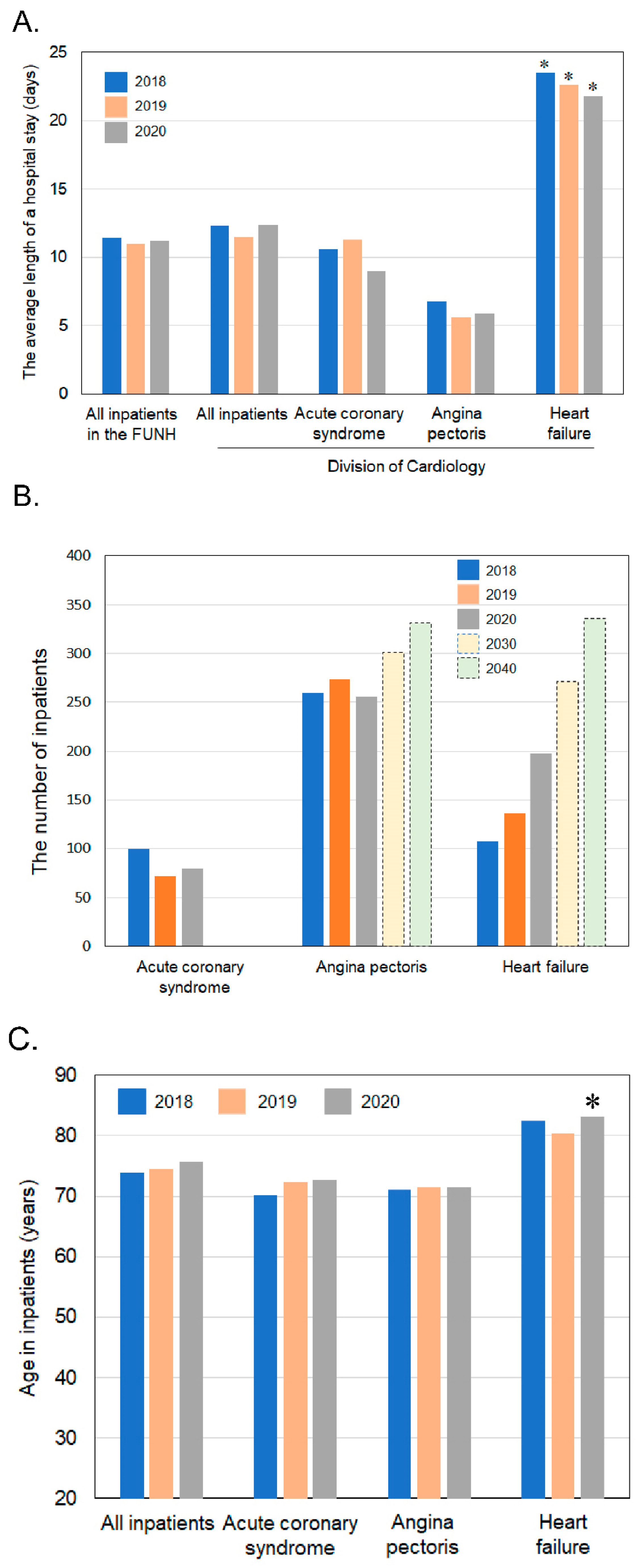
3.7. Changes in the Average Length of Stay and Changes in the Number of Inpatients and Age with Acute Coronary Syndrome, Angina Pectoris and Heart Failure over the Past 3 Years and the Estimated Number of Inpatients with Angina Pectoris and Heart Failure in 2030 and 2040 at the Division of Cardiology at FUNH
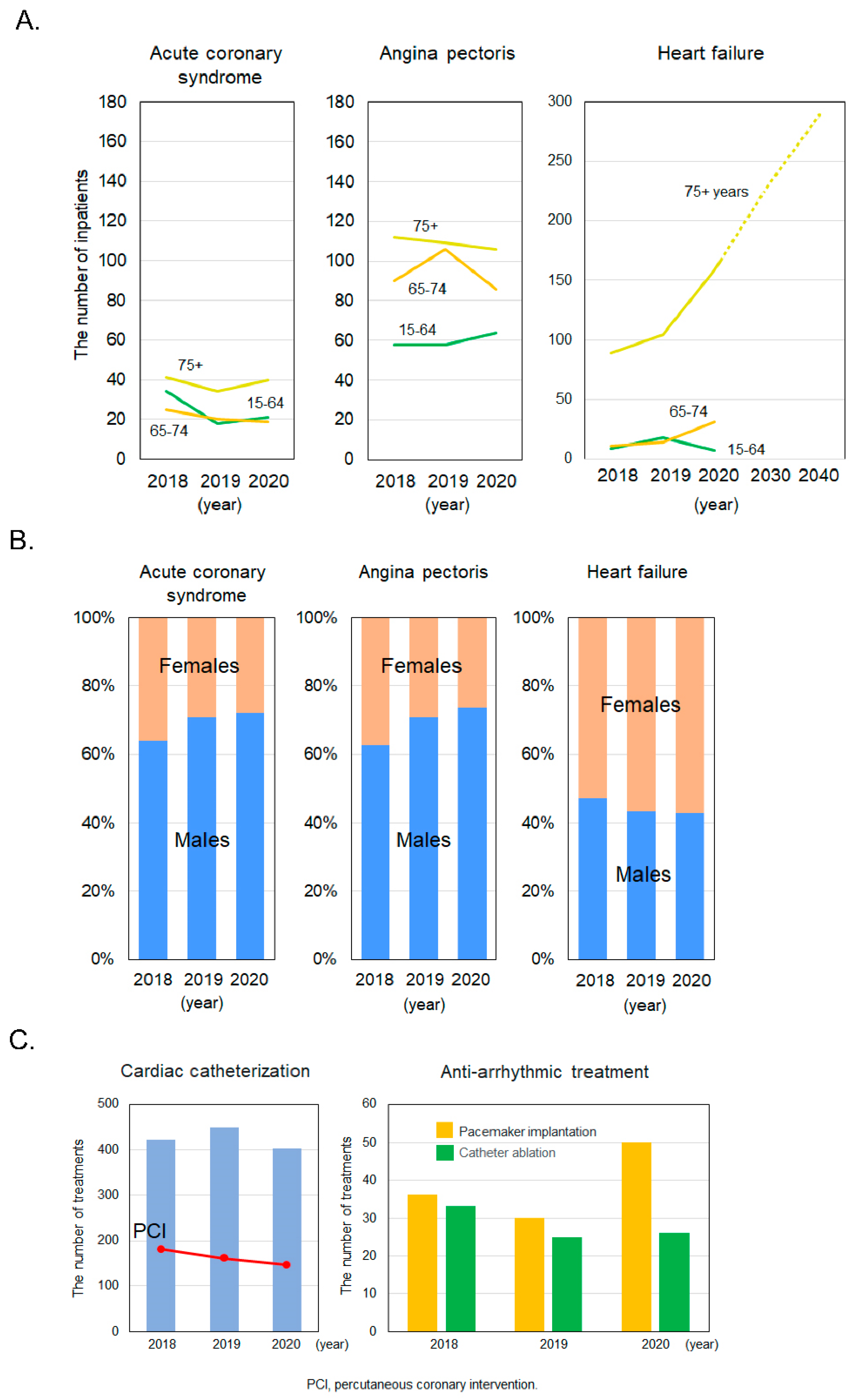
3.8. Changes in the Number of Hospitalized Patients with Acute Coronary Syndrome, Angina Pectoris and Heart Failure by Age and Gender in 2018, 2019 and 2020 and the Estimated Number of Inpatients Aged 75+ with Heart Failure in 2030 and 2040 at the Division of Cardiology at FUNH
3.9. Changes in the Number of Examinations and Treatments at the Division of Cardiology at FUNH for the Past 3 Years
3.10. Working Conditions for Medical Doctors at FUNH
3.11. Countermeasures for COVID-19 Infection
3.12. Results of a SWOT Analysis of the Current Situation at FUNH
3.13. Results of a Cross SWOT Analysis of the Future Direction of FUNH
3.13.1. Offensive Strategy (SO)
3.13.2. Confrontation Strategy (ST)
3.13.3. Strengthening Strategy (WO)
3.13.4. Defense Strategy (WT)
4. Discussion
4.1. A Cross SWOT Analysis
4.1.1. Offensive Strategy (SO)
4.1.2. Confrontation Strategy (ST)
4.1.3. Strengthening Strategy (WO)
4.1.4. Defense Strategy (WT)
4.2. Future Perspective
4.3. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ministry of Justice. Japanese Law. Medical Care Act 1948, Act No. 205 of July 30; Ministry of Justice: Tokyo, Japan, 1948.
- Shiraki, H. The issues of hospital management indicators. Saga Univ. Econ. Rev. 2017, 49, 233–260. (In Japanese) [Google Scholar]
- Tani, Y. Case study on improving management of small and medium-sized hospitals. Shogaku Toukyu 2015, 65, 235–256. (In Japanese) [Google Scholar]
- Haneda, A. Verification of the sources of competitive advantage for hospital management. J. Jpn. So. Health Admin. 2015, 52, 17–24. [Google Scholar]
- Medical Facility Management Stabilization Promotion Project. Small and medium-sized hospital management improvement handbook creation and dissemination project report (March 2003). In 2002 Ministry of Health, Labor and Welfare Medical Affairs Bureau Commissioned; UFJ Research Ins: Tokyo, Japan, 2002. (In Japanese) [Google Scholar]
- Annual Report on the Ageing Society. Vital Statistics of Japan. White Paper on Aging Society in 2019; Cabinet Office: Tokyo, Japan, 2019. (In Japanese)
- Ministry of Health Labour and Welfare. The Japanese National Plan for Promotion of Measures Against Cerebrovascular and Cardiovascular Disease; Ministry of Health Labour and Welfare: Tokyo, Japan, 2020. (In Japanese)
- Kuwabara, M.; Mori, M.; Komoto, S. Japanese National Plan for Promotion of Measures against Cerebrovascular and Cardiovascular Disease. Circulation 2021, 143, 1929–1931. [Google Scholar] [CrossRef]
- Caves, R.W. Encyclopedia of the City; Routledge: London, UK, 2004; p. 653. [Google Scholar]
- Tani, Y. Consideration on hospital management reform in small and medium-sized hospitals. Nippon. Keieigaku Ronsyu 2017, 87, 01-1–01-8. (In Japanese) [Google Scholar]
- Tani, Y. Small and Medium-sized hospitals medical corporations important factors in improving hospital management-considerations from national questionnaire surveys. Nippon. Keieigaku Ronsyu 2018, 88, 01-1–01-8. (In Japanese) [Google Scholar]
- Weihrich, H. The TOWS matrix-A tool for situational analysis. Long Range Plan. 1982, 15, 54–66. [Google Scholar] [CrossRef]
- Available online: https://www.city.fukuoka.lg.jp/soki/tokeichosa/shisei/toukei/jinkou/jinnkousokuhou.html (accessed on 19 March 2021).
- Available online: https://www.city.fukuoka.lg.jp/hofuku/chiikiiryo/health/004.html (accessed on 19 March 2021).
- Available online: https://public.tableau.com/profile/kbishikawa#!/ (accessed on 19 March 2021).
- Shimura, H. Regional revitalization of health and medical care-the role of Fukuoka University Hospital in Fukuoka City. Chiiki Kyosei Kenkyu 2014, 3, 33–50. (In Japanese) [Google Scholar]
- Morita, M. Management strategy of medium-sized community medical support hospital-SWOT analysis and examination by bed reorganization. Shodai Bus. Rev. 2017, 7, 191–218. (In Japanese) [Google Scholar]
- Ministry of Health Labour and Welfare. Fact-Finding Survey on Inpatient Medical Care in 2018; Ministry of Health Labour and Welfare: Tokyo, Japan, 2018; pp. 21–24. (In Japanese)
- Fukuoka Prefecture Community Medical Care Concept. In Proceedings of the Fukuoka Prefecture Health Care Plan Separate Volume, Fukuoka/Itoshima, Japan, March 2017; pp. 34–53. (In Japanese).
- Ohsugi, Y. Training (Senior Residency) program at community hospitals. J. Jpn. So. Intern. Med. 2019, 108, 2007–2009. (In Japanese) [Google Scholar] [CrossRef]
- Meguro, S. The marketing imagination for the health care organization: Strategic approach with the patients’ eyes. Reitaku Keizai Kenkyu. 2007, 15, 135–150. (In Japanese) [Google Scholar]
- Philip, K.; Hayes, T.; Paul, N. Marketing Professional Service in 2002, 2nd ed.; Prentice Hall: Hoboken, NJ, USA, 2002. [Google Scholar]
- Wada, K. A Consideration on ways of the management in a medical institution in an aging society: Focusing on the quality of a medical service from the viewpoint of a service marketing. Shogaku Ronsyu 2016, 85, 25–45. (In Japanese) [Google Scholar]
- Ishii, M. DRG/PPS and DPC/PDPS as prospective payment systems. Jpn. Med Assoc. J. 2012, 55, 279–291. [Google Scholar]
- Iwata, Y. Symbiosis strategy in urban medium-sized hospitals: Example of cardiovascular area. Shodai Bus. Rev. 2013, 3, 167–182. (In Japanese) [Google Scholar]
- Takura, T.; Ebata-Kogure, N.; Goto, Y.; Kohzuki, M.; Nagayama, M.; Oikawa, K.; Koyama, T.; Itoh, H. Cost-effectiveness of cardiac rehabilitation in patients with coronary artery disease: A meta-analysis. Cardiol. Res. Pract. 2019, 2019, 1840894. [Google Scholar] [CrossRef] [Green Version]
- Shields, G.E.; Wells, A.; Doherty, P.; Heagerty, A.; Buck, D.; Davies, L.M. Cost-effectiveness of cardiac rehabilitation: A systematic review. Heart 2018, 104, 1403–1410. [Google Scholar] [CrossRef]
- Owan, T.E.; Hodge, D.O.; Herges, R.M.; Jacobsen, S.J.; Roger, V.L.; Redfield, M.M. Trends in Prevalence and Outcome of Heart Failure with Preserved Ejection Fraction. N. Engl. J. Med. 2006, 355, 251–259. [Google Scholar] [CrossRef] [Green Version]
- Okura, Y.; Ramadan, M.M.; Ohno, Y.; Mitsuma, W.; Tanaka, K.; Ito, M.; Suzuki, K.; Tanabe, N.; Kodama, M.; Aizawa, Y. Impending Epidemic Future Projection of Heart Failure in Japan to the Year 2055. Circ. J. 2008, 72, 489–491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kraal, J.J.; Marle, M.E.V.D.A.-V.; Abu-Hanna, A.; Stut, W.; Peek, N.; Kemps, H.M.C. Clinical and cost-effectiveness of home-based cardiac rehabilitation compared to conventional, centre-based cardiac rehabilitation: Results of the FIT@Home study. Eur. J. Prev. Cardiol. 2017, 24, 1260–1273. [Google Scholar] [CrossRef]
- The Japanese Circulation Society; The Japanese Stroke Society. Second Five-Year Plan to Overcome Stroke and Cardiovascular Disease; The Japanese Circulation Society; The Japanese Stroke Society: Tokyo, Japan, 2021. (In Japanese) [Google Scholar]
- The Japanese Hospital Association; The All Japan Hospital Association; The Japanese Association of Medicalcare Corporations. Survey of Hospital Management Status due to the Spread of Coronavirus Infection, 3rd ed.; Summary Version; The Japanese Hospital Association; The All Japan Hospital Association; The Japanese Association of Medicalcare Corporations: Tokyo, Japan, 2020. (In Japanese) [Google Scholar]
- Financial system subcommittee. In Proceedings of the List of Materials/Ministry of Finance, Tokyo, Japan, 15 April 2021. (In Japanese).
- Maeda, A. Ethical issues experienced by head nurses in small or medium-sized hospitals and measures to solve them. J. Jpn. So. Nurse Ethics. 2018, 10, 16–25. (In Japanese) [Google Scholar]
- Kitzman, D.W.; Whellan, D.J.; Duncan, P.; Pastva, A.M.; Mentz, R.J.; Reeves, G.R.; Nelson, M.B.; Chen, H.; Upadhya, B.; Reed, S.D.; et al. Physical Rehabilitation for Older Patients Hospitalized for Heart Failure. N. Engl. J. Med. 2021, 385, 203–216. [Google Scholar] [CrossRef]
- Social Security and Tax Integrated Reform Draft in 2011. Available online: 230630kettei.pdf (accessed on 17 April 2021). (In Japanese).
- Tyler, L.S.; Cole, S.W.; May, J.R.; Millares, M.; Valentino, M.A.; Vermeulen, L.C., Jr.; Wilson, A.L. ASHP Guidelines on the Pharmacy and Therapeutics Committee and the Formulary System. Am. J. Health-Syst. Pharm. 2008, 65, 1272–1283. [Google Scholar] [CrossRef]
- The 31st Working Group on Community Healthcare Initiative. In Proceedings of the Cabinet Decision on a Bill to Partially Revise the Medical Care Act, etc. to Promote the Securing of a System to Efficiently Provide High-Quality and Appropriate Medical Care, Tokyo, Japan, 12 March 2021. (In Japanese).


| (A) Outpatients | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Total, Except for Children | Division of Cardiology | |||||||
| Year | All Patients | Males | Females | All Patients | Males | Females | All Patients | Males | Females |
| 2018 | 20,971 | 12,201 | 8770 | 20,970 | 12,200 | 8770 | 5098 | 2966 | 2132 |
| 2019 | 21,185 | 11,723 | 9462 | 21,183 | 11,723 | 9460 | 5463 | 3167 | 2296 |
| 2020 | 19,509 | 10,897 | 8612 | 19,501 | 10,894 | 8607 | 5843 | 3380 | 2463 |
| Total | Division of Cardiology | ||||||||
| Year | 75+ Years | 65–74 Years | 15–64 Years | 0–14 Years | 75+ Years | 65–74 Years | 15–64 Years | 0–14 Years | |
| 2018 | 6353 | 5832 | 8728 | 58 | 2055 | 1352 | 1653 | 38 | |
| 2019 | 6621 | 5815 | 8694 | 55 | 2296 | 1359 | 1783 | 25 | |
| 2020 | 6271 | 5510 | 7691 | 37 | 2620 | 1459 | 1743 | 21 | |
| (B) Inpatients | |||||||||
| Total | Total, Except for Children | Division of Cardiology | |||||||
| Year | All Patients | Males | Females | All Patients | Males | Females | All Patients | Males | Females |
| 2018 | 3234 | 1688 | 1546 | 2625 | 1368 | 1257 | 951 | 502 | 449 |
| 2019 | 3049 | 1610 | 1439 | 2383 | 1259 | 1124 | 892 | 477 | 415 |
| 2020 | 2345 | 1271 | 1074 | 1963 | 1076 | 887 | 848 | 461 | 387 |
| Total | Division of Cardiology | ||||||||
| Year | 75+ Years | 65–74 Years | 15–64 Years | 0–14 Years | 75+ Years | 65–74 Years | 15–64 Years | 0–14 Years | |
| 2018 | 1312 | 564 | 748 | 610 | 542 | 210 | 198 | 1 | |
| 2019 | 1229 | 536 | 617 | 667 | 498 | 211 | 183 | 0 | |
| 2020 | 1008 | 480 | 475 | 382 | 501 | 192 | 155 | 0 | |
| Internal factors | ||||
| S (Strengths) | W (Weaknesses) | |||
| S1. A community-based hospital S2. Growing income from the cardiovascular field (heart failure in particular) S3. An established internal medicine emergency system S4. Enhanced endoscopic capabilities S5. Enhanced cardiac rehabilitation S6. Measures against new coronavirus infection | W1. A decreased rate of bed utilization W2. Poor cooperation between physicians and/or medical staff W3. Increased medical material costs and drug costs W4. Old facilities and medical equipment W5. Working on an appropriate work system | |||
| Offensive strategy (SO) S1・S3 & O1-O5 Aiming to establish more community-based and emergency system, community comprehensive care beds and improve patient services through marketing activities. S2・S5 & O1-O4 Increasing the number patients (elderly) with cardiovascular, gastrointestinal and respiratory diseases. | Strengthening strategy (WO) W1 & O1-O5 Improvement of rate of bed utilization by increasing the number of community comprehensive care beds. W2 & O6 Engage in close cooperation between physicians and medical staff by opening a center for multidisciplinary collaboration. W3 & O2-O4 Reduce medical material and drug costs. | O1. An increase in elderly patients O2. An increased in cardiovascular diseases (heart failure in particular) O3. An increased in gastrointestinal diseases O4. An increased in respiratory diseases O5. An increased in community comprehensive care beds O6. Creating a center for multidisciplinary collaboration | O (Opportunities) | External factors |
| Confrontation strategy (ST) S2-S5 & T1 Opening cardiovascular-rhythm center and endoscopy center. Specialized cardiac rehabilitation from acute to maintenance phase of care. Recruiting patients with gastrointestinal diseases that require endoscopy. More useful cardiovascular and internal medicine emergency system S6 & T2 Establishment of strategy for addressing new coronavirus infection. | Defense strategy (WT) W4 & T1 As strategy against the presence of competing hospital, the future direction should need to be relocation and rebuilding to be strongly competitive with other hospitals. W5 & T3・T4 Establishment of an appropriate work system for staff. | T1. Existence of competing hospitals T2. Outbreak of coronavirus infection T3. Securing medical staff and soaring salaries T4. Changing the work habits of physicians | T (Threats) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miura, S.-i.; Nose, D.; Kanamori, K.; Imaizumi, S.; Shimura, H.; Saku, K. Sustainable Hospital Management by a Cross SWOT Analysis in a Medium-Sized Hospital. Sustainability 2021, 13, 13042. https://doi.org/10.3390/su132313042
Miura S-i, Nose D, Kanamori K, Imaizumi S, Shimura H, Saku K. Sustainable Hospital Management by a Cross SWOT Analysis in a Medium-Sized Hospital. Sustainability. 2021; 13(23):13042. https://doi.org/10.3390/su132313042
Chicago/Turabian StyleMiura, Shin-ichiro, Daisuke Nose, Katsutoshi Kanamori, Satoshi Imaizumi, Hideo Shimura, and Keijiro Saku. 2021. "Sustainable Hospital Management by a Cross SWOT Analysis in a Medium-Sized Hospital" Sustainability 13, no. 23: 13042. https://doi.org/10.3390/su132313042
APA StyleMiura, S.-i., Nose, D., Kanamori, K., Imaizumi, S., Shimura, H., & Saku, K. (2021). Sustainable Hospital Management by a Cross SWOT Analysis in a Medium-Sized Hospital. Sustainability, 13(23), 13042. https://doi.org/10.3390/su132313042





