Enhancing the Sustainable Goal of Access to Healthcare: Findings from a Literature Review on Telemedicine Employment in Rural Areas
Abstract
1. Introduction
2. Background
- Reducing healthcare cost/Increasing healthcare efficiency (C/E);
- Enhancing healthcare utilization (U);
- Improving healthcare quality (Q).
- (1)
- “moving” patients to hospital;
- (2)
- “moving” hospital to patients.
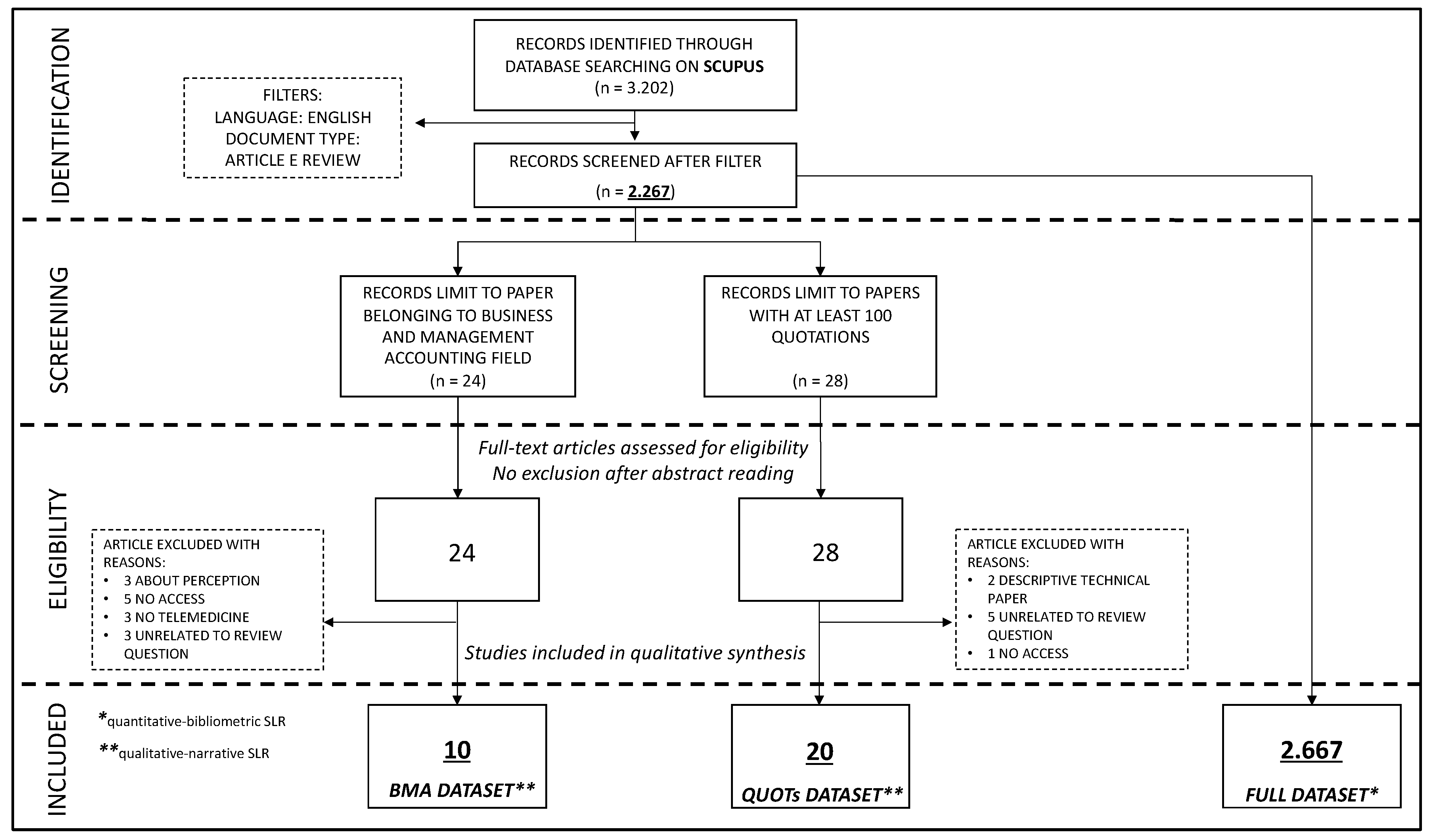
3. Materials and Methods
- Language: only studies published in English were selected;
- Document type: only peer-reviewed articles and reviews were considered. The other categories of study from Scopus as conference papers, editorials, book chapters, articles in press, conference proceedings, and letters were excluded.
3.1. Stage One
- Papers/years;
- Journals;
- Countries;
- Research areas;
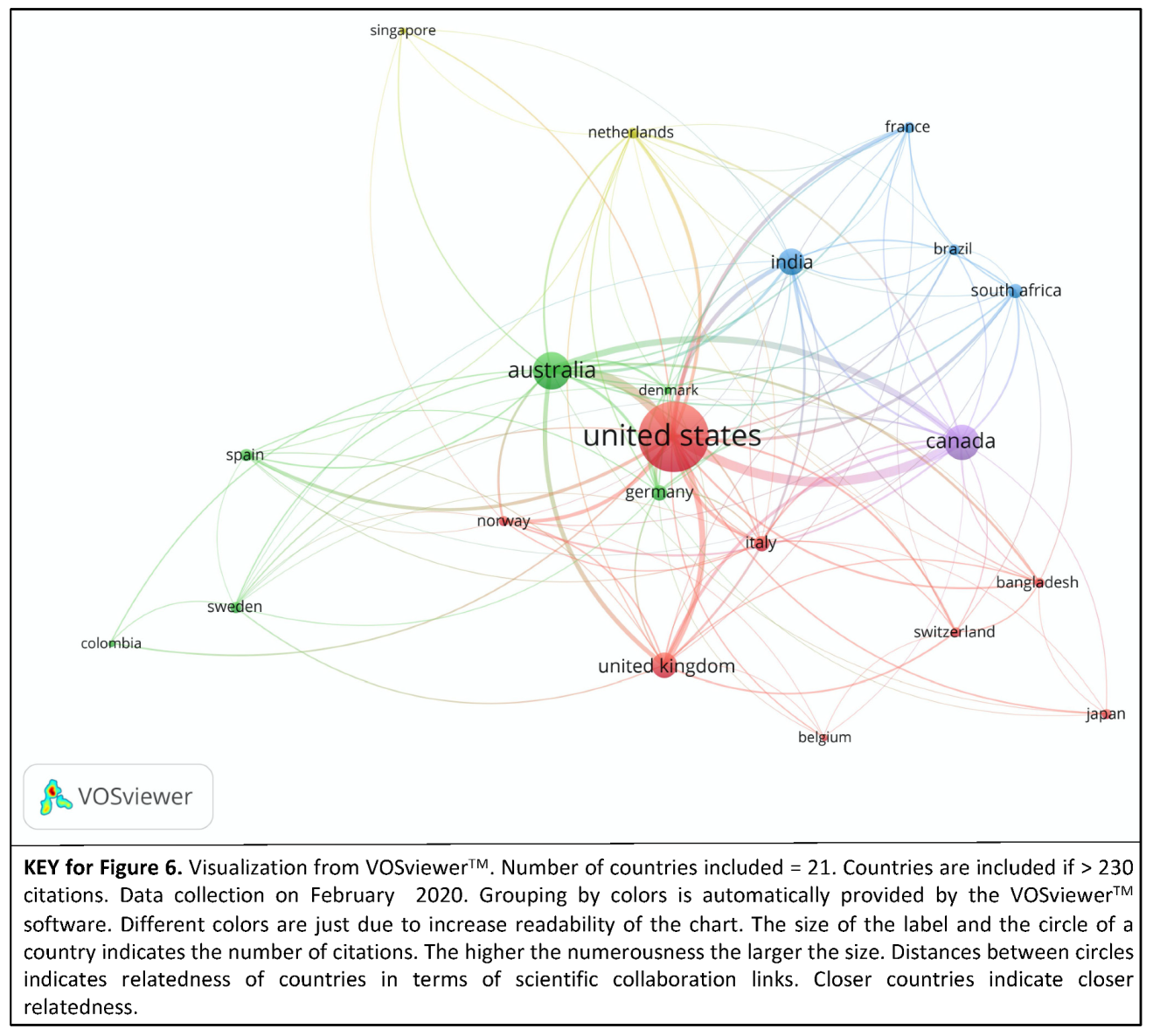
- Collaboration among countries;
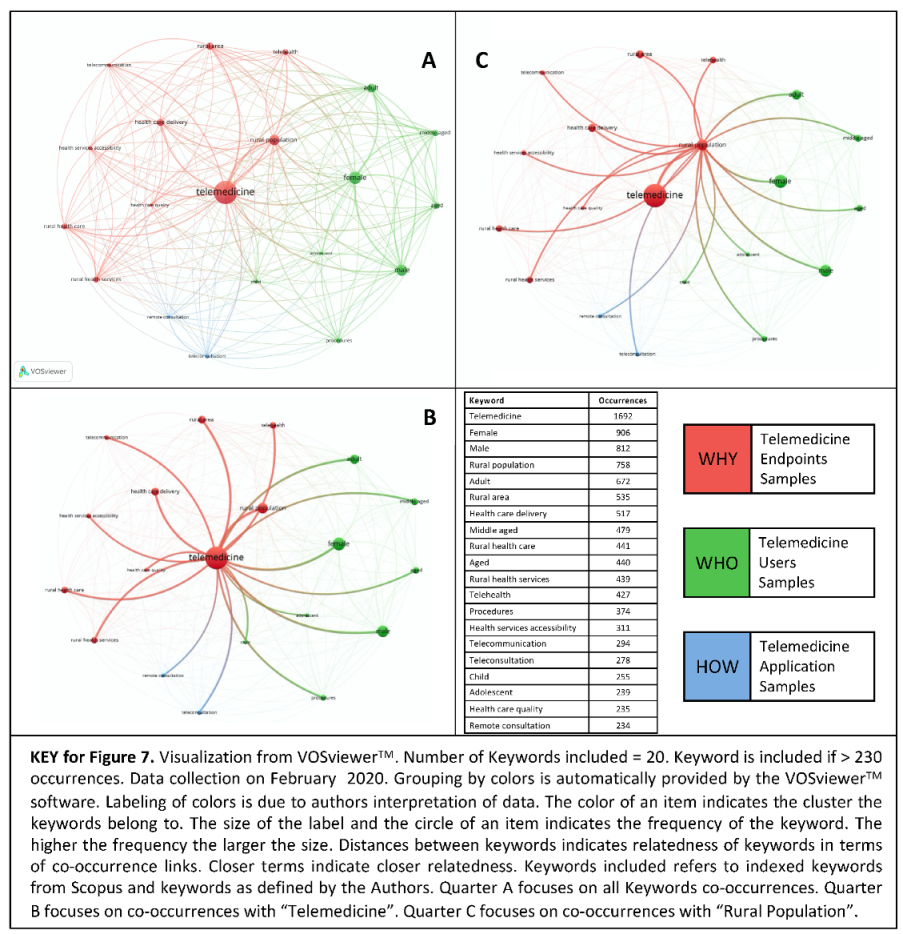
- Co-occurrence of keywords;
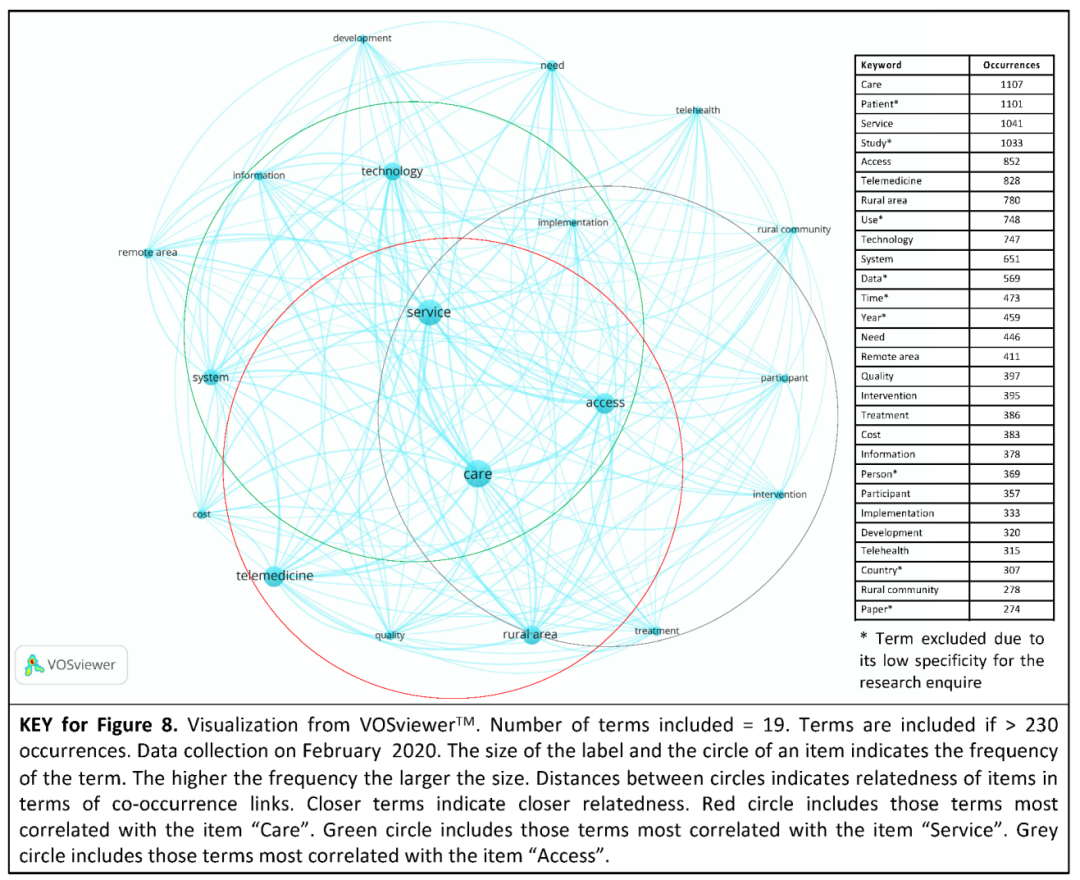
- Co-occurrence of terms within titles and abstracts.
3.2. Stage Two
4. Results
- FULL dataset;
- BMA dataset;
- QUOTs dataset.
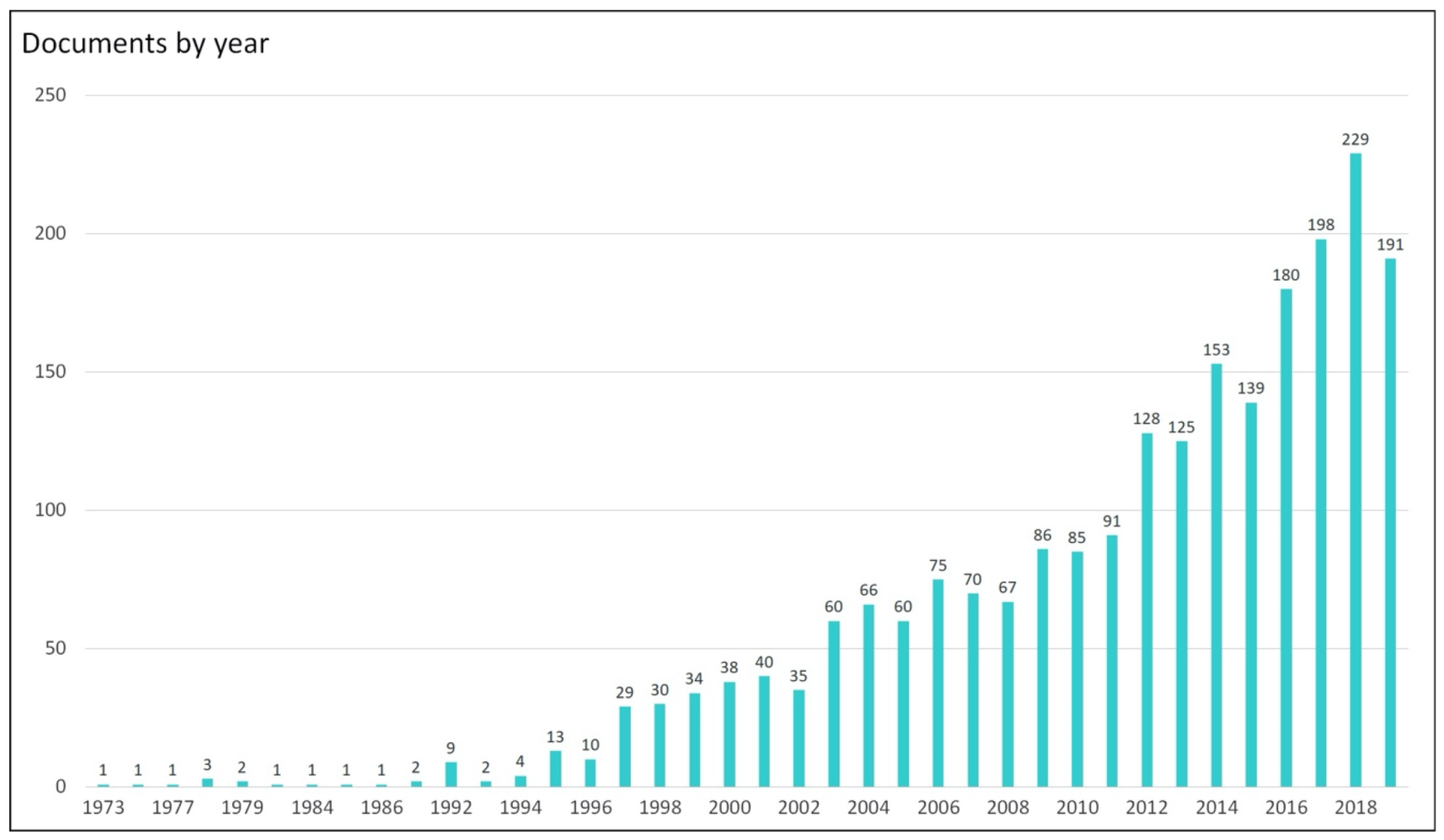
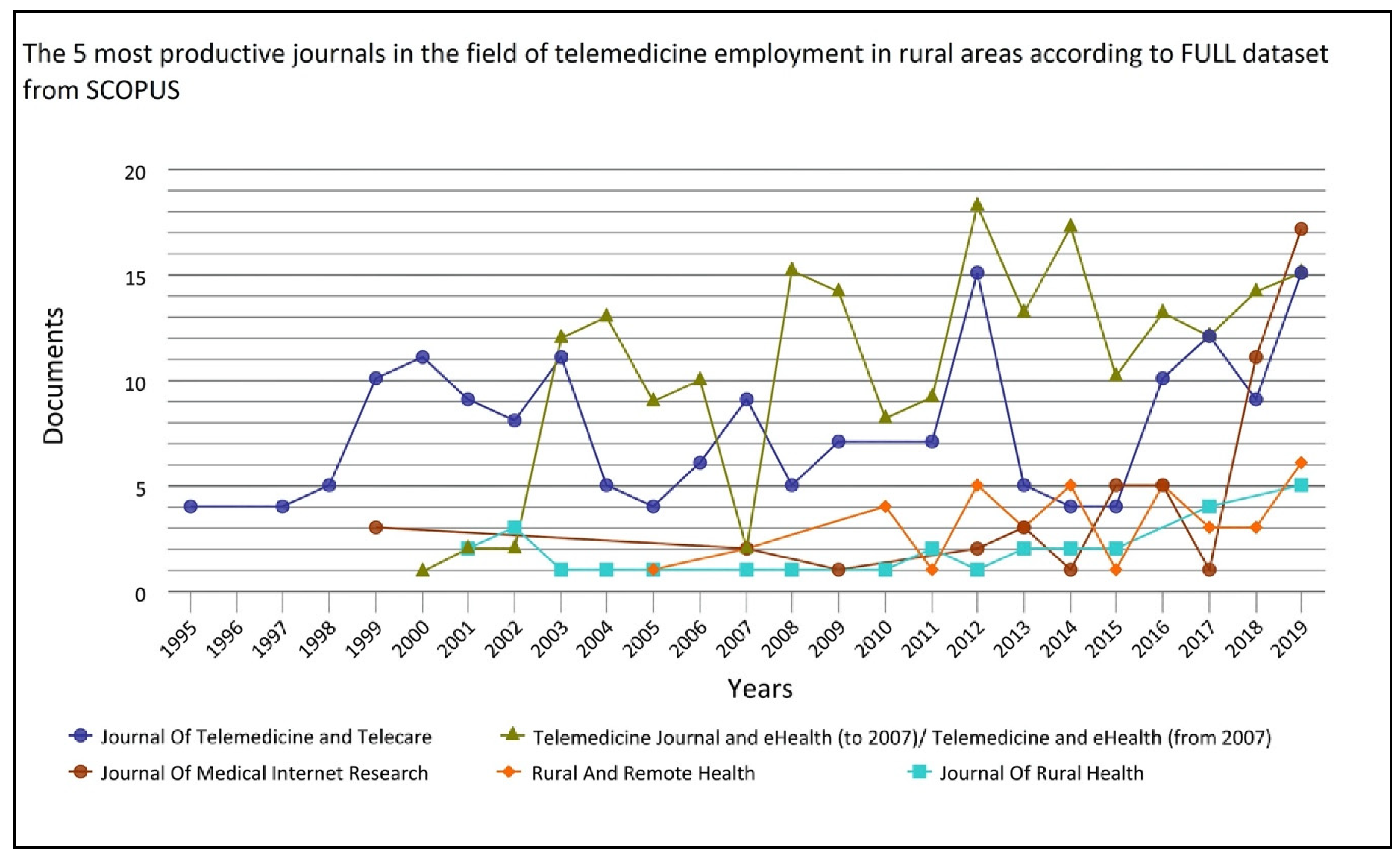
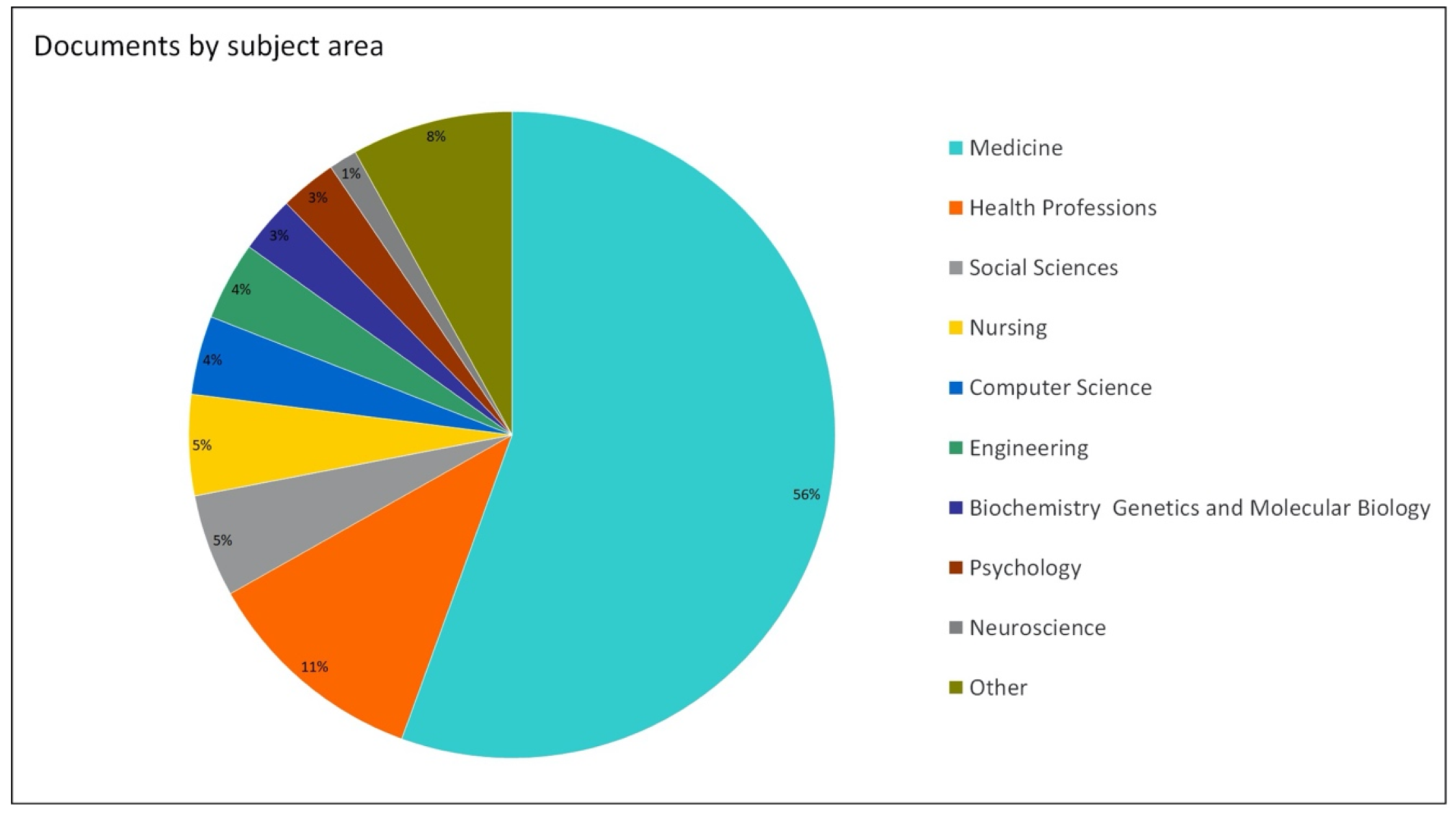
4.1. Qantitative-Descriptive and Bibliometric Analyses of the FULL Dataset
- the greater the circle representing the variable, the higher the recurrence of that variable in the sample of papers;
- the thicker the connection line among two variables, the stronger the relationship among those variables in the sample of papers;
- the closer the circles representing two variables, the higher the correlation among the two variables.
4.2. Qualitative Analysis of the BMA Dataset: Papers Belonging to Business Management and Accounting Field
4.3. Qualitative Analysis of the QUOTs Dataset: Papers Quoted at Least 100 Times
5. Discussion
5.1. Quantitative and Bibliometric Analyses of the FULL Dataset
- countries aimed at providing universal coverage of healthcare at the point of service [82] (United Kingdom [83], Germany [84], Italy [85], South Africa [86], and Spain [87]), which, due to financial restrictions and necessities, are looking for strategies and new technologies to decrease the costs of healthcare.
- “Telemedicine” is a “barycentric” term within the others; it seems to be an all-embracing item that generally connects the sphere of kind of users (e.g., terms: “female”, “adult”, “child”) with the sphere of healthcare expected outcomes and applications (e.g., terms “health care quality”, “health care delivery”, “heath service accessibility”) through the use of remote service delivery tools (e.g., terms: “remote consultation”, “teleconsultation”). Accordingly, in the authors’ opinion, the keyword “Telemedicine” is well linked with those terms that represent the demographic features (green-labeled terms) and socio-helpful needs and expectations (red-labeled terms) of rural habitants.
- “Rural Population” instead, is a term more connected with those words regarding the demographic/epidemiologic features of specific clusters of people (e.g., terms “female”, “adult”, “middle aged”), whose healthcare necessities (ref. “rural penalties” [69]) could be satisfied by the employment of innovative strategies in health service delivery (e.g., terms: “telemedicine”, “telehealth”, “health care delivery”). Accordingly, in the authors’ opinion, the keyword “Rural Population” is prevalently connected to those terms that call for new technologies and applications (red-labeled terms) as a solution for healthcare needs, particularly common in groups of people (green-labeled terms) in unserved areas.
5.2. Qualitative Analysis of the BMA Dataset
5.3. Qualitative Analysis of the QUOTs Dataset
- early diagnosis and emergency cares (6 empirical studies);
- biomedical parameter monitoring and long-term cares (5 empirical studies).
6. Conclusions
- Increasing healthcare cost/Improving healthcare efficiency (C/E);
- Enhancing healthcare utilization (U);
- Improving healthcare quality (Q).
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Martin Health. Reduce Inequality within and among Countries. 2015. Available online: https://www.un.org/sustainabledevelopment/inequality/ (accessed on 21 February 2020).
- Hess, C. Mapping the New Commons. 2008. Available online: https://ssrn.com/abstract=1356835 (accessed on 21 February 2020).
- World Health Organization. Constitution. Available online: https://www.who.int/about/who-we-are/constitution (accessed on 21 February 2020).
- Martin Health. Ensure Healthy Lives and Promote Well-Being for All at All Ages. 2015. Available online: https://www.un.org/sustainabledevelopment/health/ (accessed on 21 February 2020).
- Demography—Elderly Population—OECD Data. Available online: http://data.oecd.org/pop/elderly-population.htm (accessed on 21 February 2020).
- Yang, Y.; Peng, F.; Wang, R.; Guan, K.; Jiang, T.; Xu, G.; Sun, J.; Chang, C. The deadly coronaviruses: The 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. J. Autoimmun. 2020, 109, 102434. [Google Scholar] [CrossRef] [PubMed]
- Osborne, S.P. The New Public Governance 1; Taylor & Francis: Abingdon, UK, 2006. [Google Scholar]
- Porter, M.E. What is value in health care? N. Engl. J. Med. 2010, 363, 2477–2481. [Google Scholar] [CrossRef] [PubMed]
- du Toit, M.; Malau-Aduli, B.; Vangaveti, V.; Sabesan, S.; Ray, R.A. Use of telehealth in the management of non-critical emergencies in rural or remote emergency departments: A systematic review. J. Telemed. Telecare 2019, 25, 3–16. [Google Scholar] [CrossRef] [PubMed]
- Moffatt, J.J.; Eley, D.S. The reported benefits of telehealth for rural Australians. Aust. Health Rev. 2010, 34, 276. [Google Scholar] [CrossRef]
- Fatehi, F.; Wootton, R. Telemedicine, telehealth or e-health? A bibliometric analysis of the trends in the use of these terms. J. Telemed. Telecare 2012, 18, 460–464. [Google Scholar] [CrossRef]
- Huberfeld, N. The Universality of Medicaid at Fifty. 2015. Available online: https://uknowledge.uky.edu/cgi/viewcontent.cgi?referer=https://www.google.com/&httpsredir=1&article=1495&context=law_facpub (accessed on 21 February 2020).
- Rosenberg, C.N.; Peele, P.; Keyser, D.; McAnallen, S.; Holder, D. Results from a patient-centered medical home pilot at UPMC Health Plan hold lessons for broader adoption of the model. Health Aff. (Millwood) 2012, 31, 2423–2431. [Google Scholar] [CrossRef][Green Version]
- Roine, R.; Ohinmaa, A.; Hailey, D. Assessing Telemedicine: A Systematic Review of the Literature. 2001. Available online: https://www.cmaj.ca/content/165/6/765.full (accessed on 21 February 2020).
- Italian Ministry of Health. Telemedicina. Available online: http://www.salute.gov.it/portale/temi/p2_6.jsp?lingua=italiano&id=2515&area=eHealth&menu=vuoto (accessed on 21 February 2020).
- Sampietro Colom, L.; Lach, K.; Haro, I.E.; Sroka, S.; Cicchetti, A.; Marchetti, M.; Iacopino, V.; Kidholm, K.; Ølholm, A.M.; Birk Olsen, M.; et al. The AdHopHTA Handbook: A Handbook of Hospital-Based Health Technology Assessment (HB-HTA). 2015. Available online: https://iris.luiss.it/retrieve/handle/11385/186174/78225/adhophta_handbook%202015.pdf (accessed on 21 February 2020).
- Hess, C.; Ostrom, E. Understanding Knowledge as A Commons; The MIT Press: Cambridge, MA, USA, 2007. [Google Scholar]
- Ostrom, E.; Burger, J.; Field, C.B.; Norgaard, R.B.; Policansky, D. Revisiting the commons: Local lessons, global challenges. Science 1999, 284, 278–282. [Google Scholar] [CrossRef]
- Basu, S.; Jongerden, J.; Ruivenkamp, G. Development of the drought tolerant variety Sahbhagi Dhan: Exploring the concepts commons and community building. Int. J. Commons 2017, 11. [Google Scholar] [CrossRef]
- Human Rights and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/human-rights-and-health (accessed on 23 March 2020).
- Fulop, N.; Allen, P.; Clarke, A.; Black, N. From health technology assessment to research on the Organization and delivery of health services: Addressing the balance. Health Policy 2003, 63, 155–165. [Google Scholar] [CrossRef]
- Porter, M.E. Towards a dynamic theory of strategy. Strateg. Manag. J. 1991, 12, 95–117. [Google Scholar] [CrossRef]
- Porter, M.E. Competitive strategy. Meas. Bus. Excel. 1997, 1, 12–17. [Google Scholar] [CrossRef]
- Kaplan, R.S.; Porter, M.E. How to solve the cost crisis in health care. Harv. Bus. Rev. 2011, 89, 46–52. [Google Scholar] [PubMed]
- Otley, D. Performance management: A framework for management control systems research. Manag. Account. Res. 1999, 10, 363–382. [Google Scholar] [CrossRef]
- Ferreira, A.; Otley, D. The design and use of performance management systems: An extended framework for analysis. Manag. Account. Res. 2009, 20, 263–282. [Google Scholar] [CrossRef]
- Aidemark, L.-G. The meaning of balanced scorecards in the health care organization. Financ. Account. Manag. 2001, 17, 23–40. [Google Scholar] [CrossRef]
- Kaplan, R.S.; Norton, D.P. The Balanced Scorecard—Measures that Drive Performance. 1992. Available online: https://hbr.org/1992/01/the-balanced-scorecard-measures-that-drive-performance-2 (accessed on 23 March 2020).
- Kaplan, R.S.; Norton, D. Why Does Business Need a Balanced Scorecard? Part II. 1997. Available online: https://www.hbs.edu/faculty/Pages/item.aspx?num=9985 (accessed on 23 March 2020).
- Lock, K. Health impact assessment. BMJ 2000, 320, 1395–1398. [Google Scholar] [CrossRef]
- Kemm, J.; Parry, J.; Palmer, S. (Eds.) Health Impact Assessment; Oxford University Press: Oxford, NY, USA, 2004; ISBN 978-0-19-852629-2. [Google Scholar]
- World Health Organization. Monitoring and Evaluating Digital Health Interventions: A Practical Guide to Conducting Research and Assessment. 2016. Available online: https://apps.who.int/iris/bitstream/handle/10665/252183/9789241511766-eng.pdf;jsessionid=7CA23CDA61BFD376A7BC28ECAD93A555?sequence=1 (accessed on 4 April 2020).
- World Health Organization. A Health Telematics Policy in Support of WHO’s Health-for-All Strategy for Global Health Development. 1998. Available online: https://apps.who.int/iris/bitstream/handle/10665/63857/WHO_DGO_98.1.pdf?sequence=1&isAllowed=y (accessed on 23 March 2020).
- Garshnek, V.; Logan, J.S.; Hassell, L.H. The telemedicine frontier: Going the extra mile. Space Policy 1997, 13, 37–46. [Google Scholar] [CrossRef]
- Burri, H.; Heidbüchel, H.; Jung, W.; Brugada, P. Remote monitoring: A cost or an investment? Europace 2011, 13, ii44–ii48. [Google Scholar] [CrossRef]
- Calò, L.; Gargaro, A.; De Ruvo, E.; Palozzi, G.; Sciarra, L.; Rebecchi, M.; Guarracini, F.; Fagagnini, A.; Piroli, E.; Lioy, E. Economic impact of remote monitoring on ordinary follow-up of implantable cardioverter defibrillators as compared with conventional in-hospital visits. A single-center prospective and randomized study. J. Interv. Card. Electrophysiol. 2013, 37, 69–78. [Google Scholar] [CrossRef]
- Hasan, A.; Paul, V. Telemonitoring in chronic heart failure. Eur. Heart J. 2011, 32, 1457–1464. [Google Scholar] [CrossRef]
- Norton, S.A.; Burdick, A.E.; Phillips, C.M.; Berman, B. Teledermatology and underserved populations. Arch. Dermatol. 1997, 133, 197–200. [Google Scholar] [CrossRef] [PubMed]
- Bradford, N.; Caffery, L.; Smith, A. Telehealth Services in Rural and Remote Australia: A Systematic Review of Models of Care and Factors Influencing Success and Sustainability. 2016. Available online: www.rrh.org.au/journal/article/3808 (accessed on 21 February 2020).
- Diodato, V.P.; Gellatly, P. Dictionary of Bibliometrics; Routledge, Taylor & Francis Group: New York, NY, USA, 2013. [Google Scholar]
- Aria, M.; Cuccurullo, C. bibliometrix: An R-tool for comprehensive science mapping analysis. J. Informetr. 2017, 11, 959–975. [Google Scholar] [CrossRef]
- Durieux, V.; Gevenois, P.A. Bibliometric indicators: Quality measurements of scientific publication. Radiology 2010, 255, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Whittemore, R.; Chao, A.; Jang, M.; Minges, K.E.; Park, C. Methods for knowledge synthesis: An overview. Heart Lung 2014, 43, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Tranfield, D.; Denyer, D.; Smart, P. Towards a methodology for developing evidence-informed management knowledge by means of systematic review. Br. J. Manag. 2003, 14, 207–222. [Google Scholar] [CrossRef]
- Thorpe, R.; Holt, R.; Macpherson, A.; Pittaway, L. Using knowledge within small and medium-sized firms: A systematic review of the evidence. Int. J. Manag. Rev. 2005, 7, 257–281. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Lawal, I.A.; Klink, M.; Ndungu, P.; Moodley, B. Brief bibliometric analysis of “ionic liquid” applications and its review as a substitute for common adsorbent modifier for the adsorption of organic pollutants. Environ. Res. 2019, 175, 34–51. [Google Scholar] [CrossRef]
- Dhillon, H.S.; Doermann, A.C.; Walcoff, P. Telemedicine and rural primary health care: An analysis of the impact of telecommunications technology. Socio Econ. Plann. Sci. 1978, 12, 37–48. [Google Scholar] [CrossRef]
- Whitacre, B.E. Estimating the economic impact of telemedicine in a rural community. Agric. Resour. Econ. Rev. 2011, 40, 172–183. [Google Scholar] [CrossRef]
- Ishfaq, R.; Raja, U. Bridging the healthcare access divide: A strategic planning model for rural telemedicine network: Bridging the healthcare access divide. Decis. Sci. 2015, 46, 755–790. [Google Scholar] [CrossRef]
- Venkatesh, V.; Rai, A.; Sykes, T.A.; Aljafari, R. Combating infant mortality in rural India: Evidence from a field study of eHealth kiosk implementations. MIS Q 2016, 40, 353–380. [Google Scholar] [CrossRef]
- Tiwari, A.; Bhanu, Y.; Prasad, B.R.R. The telemedicine experience of care hospitals. Int. J. Serv. Technol. Manag. 2005, 6, 467. [Google Scholar] [CrossRef]
- Paris, H.E.C.; Srivastava, S.C.; Shainesh, G.; Indian Institute of Management Bangalore. Bridging the service divide through digitally enabled service innovations: Evidence from Indian healthcare service providers. MIS Q 2015, 39, 245–267. [Google Scholar]
- Anil, A.; Jayakumar, M.S. Improving rural health care services using ICT: Telemedicine facility in Kerala. Int. J. Sci. Technol. Res. 2019, 8, 7. [Google Scholar]
- Zishan, S.R.; Hossain, C.A.; Mohamed, M.A.; Sharun, M. The Scenario of e-Health Systems in Developing Countries (Bangladesh and Malaysia). 2019. Available online: https://www.ijrte.org/wp-content/uploads/papers/v8i1C2/A12000581C219.pdf (accessed on 23 March 2020).
- Barjis, J.; Kolfschoten, G.; Maritz, J. A sustainable and affordable support system for rural healthcare delivery. Decis. Support Syst. 2013, 56, 223–233. [Google Scholar] [CrossRef]
- Arora, S.; Kalishman, S.; Thornton, K.; Dion, D.; Murata, G.; Deming, P.; Parish, B.; Brown, J.; Komaromy, M.; Colleran, K.; et al. Expanding access to hepatitis C virus treatment-Extension for Community Healthcare Outcomes (ECHO) project: Disruptive innovation in specialty care. Hepatology 2010, 52, 1124–1133. [Google Scholar] [CrossRef]
- Wade, V.A.; Karnon, J.; Elshaug, A.G.; Hiller, J.E. A systematic review of economic analyses of telehealth services using real time video communication. BMC Health Serv. Res. 2010, 10, 233. [Google Scholar] [CrossRef]
- Ricketts, T.C. The changing nature of rural health care. Annu. Rev. Public Health 2000, 21, 639–657. [Google Scholar] [CrossRef]
- Preston, J.; Brown, F.W.; Hartley, B. Using telemedicine to improve health care in distant areas. Psychiatr. Serv. 1992, 43, 25–32. [Google Scholar] [CrossRef]
- Dávalos, M.E.; French, M.T.; Burdick, A.E.; Simmons, S.C. Economic evaluation of telemedicine: Review of the literature and research guidelines for benefit–cost analysis. Telemed. E-Health 2009, 15, 933–948. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Theobald, D.; Wu, J.; Norton, K.; Morrison, G.; Carpenter, J.; Tu, W. Effect of telecare management on pain and depression in patients with cancer: A randomized trial. JAMA 2010, 304, 163. [Google Scholar] [CrossRef] [PubMed]
- Morland, L.A.; Greene, C.J.; Rosen, C.S.; Foy, D.; Reilly, P.; Shore, J.; He, Q.; Frueh, C. Telemedicine for anger management therapy in a rural population of combat veterans with posttraumatic stress disorder: A randomized noninferiority trial. J. Clin. Psychiatry 2010, 71, 855–863. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, K.M.; Christensen, H. Internet-based mental health programs: A powerful tool in the rural medical kit. Aust. J. Rural Health 2007, 15, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, J.E.; Crosby, R.D.; Wonderlich, S.A.; Crow, S.; Lancaster, K.; Simonich, H.; Swan-Kremeier, L.; Lysne, C.; Cook Myers, T. A randomized trial comparing the efficacy of cognitive–behavioral therapy for bulimia nervosa delivered via telemedicine versus face-to-face. Behav. Res. Ther. 2008, 46, 581–592. [Google Scholar] [CrossRef] [PubMed]
- Marcin, J.P.; Ellis, J.; Mawis, R.; Nagrampa, E.; Nesbitt, T.S.; Dimand, R.J. Using telemedicine to provide pediatric subspecialty care to children with special health care needs in an underserved rural community. Pediatrics 2004, 113, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Audebert, H.J.; Schenkel, J.; Heuschmann, P.U.; Bogdahn, U.; Haberl, R.L. Effects of the implementation of a telemedical stroke network: The telemedic pilot project for integrative stroke care (TEMPiS) in Bavaria, Germany. Lancet Neurol. 2006, 5, 742–748. [Google Scholar] [CrossRef]
- Wang, S.; Lee, S.B.; Pardue, C.; Ramsingh, D.; Waller, J.; Gross, H.; Nichols, F.T.; Hess, D.C.; Adams, R.J. Remote evaluation of acute ischemic stroke: Reliability of national institutes of health stroke scale via telestroke. Stroke 2003, 34. [Google Scholar] [CrossRef]
- Hess, D.C.; Wang, S.; Hamilton, W.; Lee, S.; Pardue, C.; Waller, J.L.; Gross, H.; Nichols, F.; Hall, C.; Adams, R.J. REACH: Clinical feasibility of a rural telestroke network. Stroke 2005, 36, 2018–2020. [Google Scholar] [CrossRef]
- Wiborg, A.; Widder, B. Teleneurology to improve stroke care in rural areas: The telemedicine in stroke in Swabia (TESS) project. Stroke 2003, 34, 2951–2956. [Google Scholar] [CrossRef]
- Burdea, G.C. Virtual rehabilitation—Benefits and challenges. Methods Inf. Med. 2003, 42, 519–523. [Google Scholar] [PubMed]
- Russell, T.G.; Buttrum, P.; Wootton, R.; Jull, G.A. Internet-based outpatient telerehabilitation for patients following total knee arthroplasty: A randomized controlled trial. J. Bone Jt. Surg. Am. Vol. 2011, 93, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, J.T.; Terkelsen, C.J.; Norgaard, B.L.; Trautner, S.; Hansen, T.M.; Botker, H.E.; Lassen, J.F.; Andersen, H.R. Urban and rural implementation of pre-hospital diagnosis and direct referral for primary percutaneous coronary intervention in patients with acute ST-elevation myocardial infarction. Eur. Heart J. 2011, 32, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Sable, C.A.; Cummings, S.D.; Pearson, G.D.; Schratz, L.M.; Cross, R.C.; Quivers, E.S.; Rudra, H.; Martin, G.R. Impact of telemedicine on the practice of pediatric cardiology in community hospitals. Pediatrics 2002, 109, e3. [Google Scholar] [CrossRef] [PubMed]
- Wootton, R. Multicentre randomised control trial comparing real time teledermatology with conventional outpatient dermatological care: Societal cost-benefit analysis. BMJ 2000, 320, 1252–1256. [Google Scholar] [CrossRef]
- Pramanik, M.I.; Lau, R.Y.K.; Demirkan, H.; Azad, M.D.A.K. Smart health: Big data enabled health paradigm within smart cities. Expert Syst. Appl. 2017, 87, 370–383. [Google Scholar] [CrossRef]
- Social Security Programs throughout the World: The Americas, 2019—United States of America. Available online: https://www.ssa.gov/policy/docs/progdesc/ssptw/2018-2019/americas/united-states.html (accessed on 23 March 2020).
- Social Security Programs throughout the World: Asia and the Pacific, 2018—Australia. Available online: https://www.ssa.gov/policy/docs/progdesc/ssptw/2018-2019/asia/australia.html (accessed on 23 March 2020).
- Social Security Programs throughout the World: The Americas, 2019—Canada. Available online: https://www.ssa.gov/policy/docs/progdesc/ssptw/2018-2019/americas/canada.html (accessed on 23 March 2020).
- Social Security Programs throughout the World: Asia and the Pacific, 2018—India. Available online: https://www.ssa.gov/policy/docs/progdesc/ssptw/2018-2019/asia/india.html (accessed on 23 March 2020).
- Social Security Programs throughout the World: Asia and the Pacific, 2018—China. Available online: https://www.ssa.gov/policy/docs/progdesc/ssptw/2018-2019/asia/china.html (accessed on 23 March 2020).
- Spano, A.; Aroni, A. Organizational Performance in the Italian Health Care Sector. In Outcome-Based Performance Management in the Public Sector; Borgonovi, E., Anessi-Pessina, E., Bianchi, C., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 25–43. ISBN 978-3-319-57018-1. [Google Scholar]
- Social Security Programs throughout the World: Europe, 2018—United Kingdom. Available online: https://www.ssa.gov/policy/docs/progdesc/ssptw/2018-2019/europe/united-kingdom.html (accessed on 23 March 2020).
- Social Security Programs throughout the World: Europe, 2018—Germany. Available online: https://www.ssa.gov/policy/docs/progdesc/ssptw/2018-2019/europe/germany.html (accessed on 23 March 2020).
- Social Security Programs throughout the World: Europe, 2018—Italy. Available online: https://www.ssa.gov/policy/docs/progdesc/ssptw/2018-2019/europe/italy.html (accessed on 23 March 2020).
- Social Security Programs throughout the World: Africa, 2019—South Africa. Available online: https://www.ssa.gov/policy/docs/progdesc/ssptw/2018-2019/africa/south-africa.html (accessed on 23 March 2020).
- Social Security Programs throughout the World: Europe, 2018—Spain. Available online: https://www.ssa.gov/policy/docs/progdesc/ssptw/2018-2019/europe/spain.html (accessed on 23 March 2020).
- EvaluateMedTech World Preview 2018, Outlook to 2024. Available online: https://www.evaluate.com/thought-leadership/medtech/evaluatemedtech-world-preview-2018-outlook-2024 (accessed on 21 February 2020).
- Palozzi, G.; Chirico, A.; Gabbrielli, F. Cost Analysis of Telemedicine Implementation in the Lens of Healthcare Sustainability: A Review of the Literature. 2018. Available online: https://link.springer.com/chapter/10.1007/978-3-030-30911-4_32 (accessed on 4 April 2020).
- WHO. Global Action Plan for the Prevention and Control of NCDs 2013–2020. Available online: https://www.who.int/nmh/publications/ncd-action-plan/en/ (accessed on 21 February 2020).
- Terry, N.P. Will the internet of things transform healthcare. Vanderbilt J. Entertain. Technol. Law 2016, 19, 327. [Google Scholar]
- Guagliardo, M.F. Spatial accessibility of primary care: Concepts, methods and challenges. Int. J. Health Geogr. 2004, 3, 3. [Google Scholar] [CrossRef]
- Mueller, K.J.; Potter, A.J.; MacKinney, A.C.; Ward, M.M. Lessons from tele-emergency: Improving care quality and health outcomes by expanding support for rural care systems. Health Aff. (Millwood) 2014, 33, 228–234. [Google Scholar] [CrossRef]
- Mathews, K.A.; Elcock, M.S.; Furyk, J.S. The use of telemedicine to aid in assessing patients prior to aeromedical retrieval to a tertiary referral centre. J. Telemed. Telecare 2008, 14, 309–314. [Google Scholar] [CrossRef]
- Kyle, E.; Aitken, P.; Elcock, M.; Barneveld, M. Use of telehealth for patients referred to a retrieval service: Timing, destination, mode of transport, escort level and patient care. J. Telemed. Telecare 2012, 18, 147–150. [Google Scholar] [CrossRef] [PubMed]
- Kleindorfer, D.; Xu, Y.; Moomaw, C.J.; Khatri, P.; Adeoye, O.; Hornung, R. US geographic distribution of rt-PA utilization by hospital for acute ischemic stroke. Stroke 2009, 40, 3580–3584. [Google Scholar] [CrossRef] [PubMed]
- Garlatti, A.; Fedele, P.; Ianniello, M. The iron law of unintended effects, again? Outcome measures and blame-avoidance. In Outcome-Based Performance Management in the Public Sector; Borgonovi, E., Anessi-Pessina, E., Bianchi, C., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 45–62. ISBN 978-3-319-57018-1. [Google Scholar]
- Bivona, E.; Cosenz, F. Designing outcome-based performance management systems to assess policies impacting on caesarean section rate: An analysis of the sicilian maternity pathway. In Outcome-Based Performance Management in the Public Sector; Borgonovi, E., Anessi-Pessina, E., Bianchi, C., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 63–77. ISBN 978-3-319-57018-1. [Google Scholar]
- Bouckaert, G.; Halligan, J. Managing Performance: International Comparisons; Routledge, Taylor & Francis Group: New York, NY, USA, 2007. [Google Scholar]
- Mackie, B. The Scottish Government’s System of Outcome-Based Performance Management: A Case Study of the National Performance Framework and Scotland Performs. In Outcome-Based Performance Management in the Public Sector; Borgonovi, E., Anessi-Pessina, E., Bianchi, C., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 81–105. ISBN 978-3-319-57018-1. [Google Scholar]


| Value-Based Healthcare Variables (as derived by Porter, 2010 [8]) | Sustainability Pillars for Healthcare (as derived by UN-SDGs 3 and 10, 2015 [1,4]) | Metrics for Digital Health Intervention (as derived by WHO, 2016 [32]) |
|---|---|---|
| Profitability | Reducing Healthcare Cost Increasing Healthcare Efficiency | Cost |
| Cost | Efficiency | |
| Access to Services | Enhancing Healthcare Utilization; | Utilization |
| Patient-Centeredness | ||
| Quality | Improving Healthcare Quality | Quality |
| Safety | ||
| Patient Satisfaction |
| 1st Keyword | AND | 2nd Keyword |
| “e-health” or “ehealth” or “telecare” or “telemedicine” or “telehealth” or “telemonitoring” or “telepractice” or “telenursing” | “rural areas” or “rural communities” or “rural population” or “remote areas” or “remote population” or “remote communities” or “province” |
| Country | Authors | Aim | Findings | Sust. Var. |
|---|---|---|---|---|
| USA | **Dhillon H.S. et al. [48] | Describing procedures used for estimating the impacts of telemedicine-based technological alternatives for delivering primary care in rural areas. | The use of telemedicine: - expands the role of physician in rural areas; - lowers costs; - enhances access to primary healthcare. | C/E U |
| **Garshnek V. et al. [34] | Discussing the new frontier of telemedicine beyond its current and common use. | Telemedicine makes real both the vision of an enhanced accessibility of medical expertise and a global network of healthcare available in any situation. | U | |
| *Whitacre B.E. [49] | Examining the benefits of telemedicine for hospitals and their surrounding communities. | Each community recognizes an impact of at least $20,000/year in cost-savings or other economic opportunities generated by the telemedicine employment. Estimated average annual impact is about $522,000 with a maximum over $1,300,000. | C/E | |
| *Ishfaq R., Raja U. [50] | Planning model that incorporates different operational and service elements of the rural telemedicine healthcare network. | It is economical to operate more small-service area telemedicine centers than fewer large telemedicine healthcare centers. | C/E U | |
| *Venkatesh V. et al. [51] | Examining how the use of eHealth kiosks can alleviate the problem of high infant mortality in rural India. | Infant mortality in rural India can be effectively combatted with an ICT intervention by disseminating authenticated health information about infant healthcare, positively altering infant healthcare practices and promoting the utilization of professional medical care. | C/E U | |
| INDIA | *Tiwari A. et al. [52] | Analyzing the application of telemedicine technology towards benefiting the rural people. | The telemedicine is the best example of the ICT helping the poor in improving the standards of their lives and making them live better lives, although the critical factors of the process are making people understand the process and the use of it. | C/E U Q |
| *Srivastava S.C., Shainesh G. [53] | Understanding how orchestrate an innovative assembly of ICT and No-ICT resources in use telemedicine. | Innovative ICT tools have the potential to be significant service levelers and hence to contribute to balanced growth in the developing world | U | |
| *Anil A., Jayakumar M.S. [54] | Assessing how far the use of ICT has resulted in strengthening rural health care services and the key issues being faced by its utilization. | Telemedicine is a potential tool that can give technical support to bridge the rural–urban disparity. It allows to saving time and cost of travelling along by bringing high quality specialist diagnosis to the rural area. | C/E U | |
| BANGLADESH–MALAYSIA | **Zishan M.S.R. et al. [55] | Discussing the current scenario of e-Health system in Bangladesh and Malaysia. | Telemedicine/e-health can: - reduce the cost of treatment of the villagers; - provide emergency medical treatment for patients that take a lot of time to reach in the urban areas to get proper medical treatment; - be a solution for the health care budget of the developing countries; - virtually bring the urban hospitals in rural areas. | C/E U |
| NETHERLANDS–SOUTH-AFRICA | *Barjis J. et al. [56] | Proposing a patient monitoring system for supporting the model using Unstructured Supplementary Service Data (USSD) technology. | The use of telemonitoring shows that the perceived value was high for both patients and caregiver. This creates a path to a more sustainable solution, as it is in the interest of the caregivers to sustain the use of the DSS. | U Q |
| Discipline | No. Qs | Authors | Country | Aim | Findings | Sust. Var. |
|---|---|---|---|---|---|---|
| Health Policy | 152 | **Arora S. et al. [57] | USA | Assessing the impact of the Extension for Community Healthcare Outcomes (ECHO) model to delivering specialist medical care in rural areas. | Thanks to the ECHO model, HCV cares delivered in rural areas are safer and more effective, as provided by specialists belonging to an academic medical center. | U |
| 142 | **Wade V.A. et al. [58] | Australia | The economic evaluation of synchronous or real-time video communication in telehealth delivery. | Video communication offers value to healthcare. Patients’ health outcomes were equal (and in some cases better) than conventional care. | C/E U | |
| 140 | **Ricketts T.C. [59] | USA | The characteristic of rural health care system in America. | The healthcare conditions of rural areas are unfavorably with the rest of nation. | U | |
| 120 | **Moffatt J.J., Eley D.S. [10] | Australia | Identifying benefits attributable to telehealth for both people living and professionals working in remote locations of Australia. | Patients living in remote locations of Australia get benefit from telehealth by increasing access to services and high-skilled health professionals. | U | |
| 115 | **Preston J. et al. [60] | USA | The cost of telemedicine and the improvement of health care in rural areas using telemedicine. | Telemedicine cuts the cost of healthcare and improve its quality. | C/E Q | |
| 105 | **Dávalos M.E. et al. [61] | USA | Tracing guidelines for conducting cost-benefit analysis of telemedicine programs. | Identified general outcomes of telemedicine programs that can be converted into dollar values. | C/E | |
| Psychiatry | 182 | *Kroenke K., et al. [62] | USA | Determining whether centralized telephone-based care management coupled with automated symptom monitoring could improve pain and depression rate in rural patient with cancer. | Telecare improves outcomes of life quality domains (vitality, anxiety, physical symptom). It also improves secondary depression- outcomes of Mental Health Inventory (depression severity and diagnostic status). | Q |
| 159 | *Morland L.A., et al. [63] | USA | Demonstrating the non-inferiority of telemedicine strategies compared to traditional cares in person service for rural combat veterans with post-traumatic stress disorder. | Providing tele-psychotherapy is feasible and produces outcomes as good as in-person treatment | Q | |
| 140 | **Griffiths K.M., Christensen H. [64] | Australia | Discussing the usefulness of internet-based depression information and AI automated therapy programs in rural regions. | The programs are cost-effective self-help tools as adjunct to GP treatment for rural residents with depression. | C/E U | |
| 105 | *Mitchell J.E. et al. [65] | USA | Comparing efficacy and acceptability of a “cognitive-behavioral” therapy delivered in-person to a therapy delivered via telemedicine. | Telemedicine therapy is acceptable for participants and roughly equivalent in outcome to in-person therapy. | U | |
| 104 | *Marcin J.P. et al. [66] | USA | Reporting the satisfaction of a telemedicine program regarding a medical need assessment of parents/caregivers of children with special health care needs in rural areas. | Telemedicine pediatric subspecialty consultations to rural and underserved community are feasible. They are considerable as highly satisfactory by both the parents/caregivers and rural healthcare providers. | U Q | |
| Neurology | 206 | *Audebert H.J. et al. [67] | Germany | Estimating the effects of a rural stroke network with telemedicine support from Germany on the quality of cares. | Telemedicine networks, empowered by international academic stroke centers, offer new and innovative approaches to improve acute stroke care for patients living in suburban areas. | Q |
| 144 | *Wang S. et al. [68] | USA | Assessing the employment of remote evaluation of acute ischemic stroke (REACH) and the comparison between values of bedside and remote evaluators. | The REACH system is a suitable tele-stroke tool to delivering consultations to rural and “underserved” areas. It may also provide opportunities for rural hospitals in TPA management. | U | |
| 127 | *Hess D.C. et al. [69] | USA | The development of stroke network to bringing guideline driven stroke care to rural, unserved areas. | The REACH strategy suggests that patients can be treated rapidly, safely, and effectively with TPA in rural community hospitals. | U Q | |
| 118 | *Wiborg A., Widder B. [70] | Germany | The opportunity to improve stroke care in rural areas by using a conventional videoconference system. | Videoconference system improves stroke care in rural areas where management in a stroke unit is hindered by long transportation distances | Q | |
| Rehabilitation | 190 | **Burdea G.C. [71] | USA | Reviewing the benefits brought by virtual reality-enhanced and virtual reality-based rehabilitation to groups of patients. | Virtual Rehabilitation is: - economy of scale; - interactivity and patient motivation; - beneficial in reducing healthcare costs; - promoter of high-quality healthcare in rural areas. | U Q |
| 117 | *Russell T.G. et al. [72] | Australia | Evaluating the equivalence of an Internet-based tele-rehabilitation program compared with conventional outpatient physical therapy for patients who have had a total knee arthroplasty. | Patients reported a high level of satisfaction and the outcomes achieved were comparable with in person rehabilitation | Q | |
| Cardiology | 116 | *Sørensen J.T. et al. [73] | Denmark | Evaluating the impact of pre-hospital diagnosis on time from emergency medical services in cohort of patients with STEMI. | Pre-hospital diagnosis on time: -can be successfully implemented; - allow to offer the treatment for patient that live in rural areas; -reduce long term mortality. | U Q |
| 105 | *Sable C.A. et al. [74] | USA | Evaluating the impact of telemedicine on delivering pediatric cardiac cares in community hospitals. | The methodology improves patient care: it enhances echocardiogram quality, aids sonographer education. Telemedicine positively impacts on referral patterns, time management without increasing the echocardiography utilization. | Q | |
| Dermatology | 209 | *Wootton R. et al. [75] | United Kingdom | Comparison real time tele-dermatology with outpatient dermatology. | If the equipment were purchased at current prices and the travelling distances greater, tele-dermatology could be considered as a cost-effective alternative to conventional care. | C/E U |
| Rank (no. Papers Published) | Journal | No. Papers in BMA Dataset | No. Papers in QUOTs Dataset |
|---|---|---|---|
| 1 (208) | Telemedicine Journal and eHealth (to 2007)/Telemedicine and eHealth (from 2007) | 0 | 1 |
| 2 (177) | Journal of Telemedicine and Telecare | 0 | 0 |
| 3 (48) | Journal of Medical Internet Research | 0 | 0 |
| 4 (39) | Rural and Remote Health | 0 | 0 |
| 5 (28) | Journal of Rural Health | 0 | 0 |
| Rank (% of Publishing) | Discipline | No. Papers in BMA Dataset | No. Papers in QUOTs Dataset |
|---|---|---|---|
| 1 (56%) | Medicine | 0 | 20 |
| 2 (11%) | Health Professionals | 0 | 0 |
| 3 (5%) | Social Sciences | 0 | 0 |
| 4 (5%) | Nursing | 0 | 0 |
| 5 (4%) | Computer Science | 0 | 0 |
| 6 (4%) | Engineering | 0 | 0 |
| 7 (3%) | Biochemistry, Genetics, and Molecular Biology | 0 | 0 |
| 8 (3%) | Psychology | 0 | 0 |
| 9 (1%) | Neuroscience | 0 | 0 |
| 10 (8%) | Other | 10 | 0 |
| Strategic Objectives | Operating Objectives | Source |
|---|---|---|
| Sustainability Pillars for Healthcare (as Derived by UN-SDGs 3 and 10, 2015 and WHO, 2016) | Sustainability Variables (as Derived by the Literature Review on BMA Dataset) | |
| Reducing Healthcare Cost Improving Healthcare Efficiency | - reducing travelling expenses both for patients and clinical staff | [49,50,52,54] |
| - increasing clinical staff productivity | [49,54,55] | |
| - increasing the cost-effectiveness of clinical resources involved in healthcare | [52,54] | |
| - reducing losses for missed work for both patients and their caregivers | [49] | |
| - reduces costs for potential subsequent examinations or emergency cares | [51] | |
| - reducing patients’ referrals | [48] | |
| Enhancing Healthcare Utilization | - improving early interventions | [34,50,55] |
| - fostering access to new technologies and interventional strategies | [52] | |
| - increasing the coverage of services, including emergency cares | [50,52,53,55] | |
| - improving information available for patients/caregivers | [51] | |
| - enhancing better communication among patients and clinicians | [55] | |
| - expanding roles of non-physicians | [48] | |
| Improving Healthcare Quality | - improvement of communication exchange among patient and physician | [55,56] |
| - enhancing the efficacy of specialist diagnosis | [54] | |
| - improving healthcare practices and the skilling-up of local practitioners | [34,51,52] |
| Strategic Objectives | Operating Objectives | Source |
|---|---|---|
| Sustainability Pillars for Healthcare (as Derived by UN-SDGs 3 and 10, 2015 and WHO, 2016) | Sustainability Variables (as Derived by the Literature Review on QUOTs Dataset) | |
| Reducing Healthcare Cost Improving Healthcare Efficiency | - reducing visit length | [75] |
| - reducing time for examination | [71] | |
| Enhancing Healthcare Utilization | - reducing drop-out | [63] |
| - fostering access to specialist cares | [65,71] | |
| - providing treatments that are not otherwise available | [58] | |
| - improving specialist second-opinion consultations | [66] | |
| - skilling-up of local practitioners | [10] | |
| - improving early clinical assessment | [10,74] | |
| - enhancing the continuity of care | [10,72] | |
| Improving Healthcare Quality | - reducing mortality rate | [67,73] |
| - reducing severe disability rate | [67] | |
| - improving patients’ motivation to healthcare participation | [71] | |
| - enhancing better outcomes | [62] | |
| - expanding Evidence Based best practices | [57] | |
| - enhancing high-quality healthcare | [70] | |
| - fostering delivering “right” specialist care to “right” patient | [60,69] | |
| - enhancing better diagnosis | [74] | |
| - improving healthcare coordination | [66] | |
| - improving more immediate treatments | [58,64] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palozzi, G.; Schettini, I.; Chirico, A. Enhancing the Sustainable Goal of Access to Healthcare: Findings from a Literature Review on Telemedicine Employment in Rural Areas. Sustainability 2020, 12, 3318. https://doi.org/10.3390/su12083318
Palozzi G, Schettini I, Chirico A. Enhancing the Sustainable Goal of Access to Healthcare: Findings from a Literature Review on Telemedicine Employment in Rural Areas. Sustainability. 2020; 12(8):3318. https://doi.org/10.3390/su12083318
Chicago/Turabian StylePalozzi, Gabriele, Irene Schettini, and Antonio Chirico. 2020. "Enhancing the Sustainable Goal of Access to Healthcare: Findings from a Literature Review on Telemedicine Employment in Rural Areas" Sustainability 12, no. 8: 3318. https://doi.org/10.3390/su12083318
APA StylePalozzi, G., Schettini, I., & Chirico, A. (2020). Enhancing the Sustainable Goal of Access to Healthcare: Findings from a Literature Review on Telemedicine Employment in Rural Areas. Sustainability, 12(8), 3318. https://doi.org/10.3390/su12083318





