1. Introduction
The 2019 NHS Staff Survey collected data from all National Health Service trusts in the United Kingdom, generating responses from 497,117 employees [
1]. The survey highlighted the prevalent issues for employees working in NHS environments, with “Health and well-being” being observed as a key issue. In total, 39.8% of staff reported feeling unwell due to work-related stress, with only 26.8% feeling that positive action on health and well-being was being taken by their employer; 51.4% considered leaving their current position, with 21% considering leaving the NHS altogether. Whilst these figures cover many roles in the NHS, not solely nurses, they indicate the need for health and well-being-focused initiatives at an organization-wide level, which can improve staff retention and reduce recruitment expenditure.
In recent years, awareness of the importance of nurse health and well-being has increased, as has its relationship with patient care quality and staff retention. It is evident that patients are happier when treated by nurses who themselves are happy and healthy, and that a focus upon staff health and well-being within NHS trusts is linked to improved staff retention [
2]. El-Sharkawy et al. [
3] found that 45% of nurses and doctors in one NHS hospital were dehydrated at the end of their shift and showed signs of cognitive impairment which is linked to dehydration [
4]. Currently, there is no NHS-wide focus on the different facets of health and well-being [
5], just on improving it. Given the lack of standardized well-being solutions available to NHS trusts, there is an opportunity to fill this gap. The behavioral and habitual nature of drinking water and staying hydrated suggests that designing for behavior change can be successful but requires an understanding of the contextual factors and target group [
6]. Given the behavioral nature of consuming water, this study aims to develop a conceptual solution, employing behavioral change theory and user-centered design, to support and develop personal hydration behaviors in NHS hospital ward-based nurses. We aim to achieve this with minimal detriment to the environment and employee health and well-being.
1.1. Related Work
The health and well-being of NHS employees has been widely studied by researchers and policy makers over the last decade. Similarly, the behavior change, management, and habit formation of employees in public sector working environments, including NHS hospital wards, has been explored by public health specialists worldwide.
1.1.1. Health and Well-Being in the NHS
El-Sharkawy et al. [
3] examined the dehydration levels of 88 doctors and nurses in a UK-based NHS hospital. Urine and blood samples were taken at the end of 130 shifts while participant cognition was assessed using multiple tests. At the start of shifts, 36% of participants were dehydrated, while at the end of shifts, 45% were dehydrated. Dehydrated participants were found to be cognitively impaired using short-term memory tests. This study provides evidence to support the existence of a problem relating to hydration within NHS hospital wards and its potential to affect staff cognition, thereby affecting patient care and healthcare delivery. The findings may not be applicable to the entire NHS and international healthcare providers, and the inclusion of doctors means that the data do not wholly support the existence of a dehydration problem for nurses. Further research would be needed to confirm the levels of dehydration in healthcare staff across the NHS. Boorman [
2] discussed the findings of a review of NHS staff health and well-being. They found that organizations that paid significant attention to employee health and well-being performed better, improving patient satisfaction and staff retention levels while lowering the amount of sick days taken. Similarly, stronger quality scores were achieved with better patient outcomes. Boorman [
2] also believed that it would be possible to eliminate a third of staff sickness with well-being improvements, which would save the NHS approximately £555 million per annum or be equivalent to hiring 14,900 more staff. Hydration is a cornerstone of health and well-being, as highlighted by Maslow [
7], giving a financial incentive for the NHS to focus on its improvement. The researchers also compared 2009 staff sickness rates [
8] against 2019 staff sickness rates [
9] and found that there has been no significant change; thus, the prior figures may be considered reliable. Boustead [
10] discussed how hydration stations had been developed and placed in a hospital managed by the West Suffolk NHS Foundation Trust. They comprised accessible enclosed spaces where water bottles, cleared with infection control, could be stored and refilled. Water bottles were provided to all staff and contained a guide to the location of water points within the hospital. This initiative is now also used at a neighboring trust, although the schemes are funded by charities set up to support healthcare staff. It is difficult to identify the efficacy of such solutions, but it is important to consider that individual trusts may already have their own approaches to tackling dehydration. Furthermore, it demonstrates that it is possible to implement hydration stations on wards.
1.1.2. Water, Hydration and Health
Armstrong and Johnson [
4] proposed a new method for measuring hydration levels using neuroendocrine responses detectable in blood plasma. They highlighted that there is no existing consensus on the recommended daily water intake for men, women and children. They proposed a new research approach for defining these recommended levels, but this has not yet been undertaken. Further, it is stated that indications of dehydration in blood plasma are likely linked to multiple chronic diseases and a decrease in cognitive brain function. From this, the authors concluded that there is currently no means for accurately determining daily water intake or monitoring hydration levels without analysis of bodily fluids, which is considered an intrusive procedure. This led to the authors avoiding the tracking of water intake levels. The researchers also suggest that the findings of El-Sharkawy et al. [
3], who linked dehydration to cognitive impairment, are valid. Elmadfa and Meyer [
11] discussed hydration data taken from a European-wide sample. Daily water intake ranged from 1500 to 2000 mL and it was found that there is no “healthy figure” as fluid is absorbed through the food people eat, and the amount required is dependent on physical characteristics. A conclusion drawn is that regular fluid intake, consisting mainly of water, promotes a healthy fluid balance. This suggested that the current research should avoid specific consumption levels in potential solutions, indicating that increasing hydration regularity and focusing on promoting water as a main hydration source may be more successful. It should be noted that this study does not examine the diet and lifestyle of nurses in maintaining a healthy fluid balance and there may be other factors at play here.
1.1.3. Behavior Change and Habit Formation
Michie et al. [
12] discussed the creation of a Behavior Change Technique (BCT) taxonomy. Experts rated labels and definitions of 124 BCTs from six classification systems. Another group of experts categorized the BCTs, based on method similarities, resulting in 93 BCTs (duplicates and non-applicable BCTs were eliminated) in 16 groups. The research, however, does not provide guidance on how to select appropriate BCTs but was useful for ensuring that the techniques selected are accepted and valued and led to other areas of investigation. Fernandez et al. [
6] outlined a theory and evidence-guided six-step model for developing health-promotion interventions. It was stated that identifying and understanding environmental and contextual factors is vital, alongside an understanding of the health issues to be addressed and the desired outcomes of the intervention. A further review of relevant literature, an understanding of theory and identification of the correct Behavior Change Interventions (BCIs) are also required. The involvement of stakeholders in the development process is stated as leading to more successful outcomes. Whilst this six-step model draws parallels with the user-centered design approach, and held valuable guidance for this study, it was more relevant to projects of a larger scope. Thus, the authors used aspects of this model to inform their process but did not wholly rely on it.
Yardley et al. [
13] summarized research questions into Digital Behavior Change Intervention (DBCI) engagement. DBCIs are defined as “interventions that employ digital technologies such as the Internet, telephones and mobile and environmental sensors”. Engagement levels with DBCIs were linked to user knowledge, skills, behavior motivations, culture and context, all aspects intrinsic to a user-centered design. Researchers agreed that the DBCI market is novel while investigation into factors that affect the success of DBCIs is limited. This article indicated that there is an opportunity for developing solutions that can contribute to knowledge surrounding DBCIs. Gardner and Rebar [
14] discussed the psychological definition of habits, their formation and how they can be used in BCIs. They stated that for a habit to form, a behavior must be performed repeatedly in the presence of cues or in a specific context. The habit is formed when the behavior becomes triggered by an impulse, rather than a reflective and deliberative process. Four requirements for habit formation were listed—a person must decide to act, then they must act, and must do so repeatedly, in a manner conducive to developing cue-behavior associations. It was also stated that cues of high salience, frequency and consistency quicken the rate of habit formation.
Lally et al. [
15] presented findings from a 12-week study into habit formation with 96 participants. They were asked to focus on one activity, once a day and associated with a cue (i.e., breakfast), with 31 participants focusing on hydrating. For participants to reach behavioral automaticity (habit formation), the median time taken was 66 days with a range of 18–254 days. The effectiveness of the habit formation was shown to correlate with the consistency of behavior performance. This research was valuable in indicating how long it can take to form habits and the factors that contribute to this. It also highlighted the need for participants to have the motivation to interact effectively with BCIs. Foster et al. [
16] studied asthma medication adherence, using a device that prompted users when they needed to take medication. The purpose of their research was to investigate whether behaviors changed and how users perceived a tool that can help. This was found to encourage habit formation, behavior changes and attitude changes. Users who formed a routine found that this aided sustained behavior change, as well as experiencing the “reward” of their asthma improving. Users who deemed their medication less necessary or that only took it when symptomatic, considered the prompts to be a less acceptable interruption. It was registered that some users’ adherence improved within one month, with most users liking the idea that it was a training program. This study confirmed the importance of a desire to engage with BCIs and to form new habits and routines, and the importance of noticing a positive outcome through doing so.
Klöckner and Blöbaum [
17] discussed a “comprehensive action determination model” and explained the four types of influencer that affect behaviors: intentional, normative, situational and habitual. It is stated that these are not mutually exclusive, but that normative processes (social norms, personal norms, awareness of need and awareness of consequences) influence habitual and intentional processes. These are, in turn, restricted by situational influences, and these factors combined result in a behavioral outcome. The authors further stated that norms are less respectful of time, and thus establishing them may be a stable way to influence behaviors. This article highlighted the primary factors that influence behaviors, which is pivotal to the design process for this research.
1.1.4. User Interface Design
Alzahrani and Alnanih [
18] discussed the effects of the user experience approach on user interface design quality, with specific reference to the use of personas to characterize different user group requirements in healthcare scenarios. It was found that different personas highlighted different priorities when making design decisions and that it was essential to be aware of existing user behaviors. It was concluded that the design of a “friendly” User Interface (UI) can save time, improve usability and access, and reduce stress. In our research, personas were developed using their recommendations, which were used to ensure the usability of the developed user interface. Norman [
19] discussed the importance of mental models, affordances, signifiers and natural mappings. These are elements that contribute to the design of effective interfaces. For example, combining the affordance for a button to be pressed with a signifier (such as a symbol or icon) that this button relates to an action on a screen is likely to result in the intended outcome for the user. Applying the correct mental models of how a system functions also helps users to interpret the affordances and signifiers correctly. Furthermore, mapping interface controls in a layout that is visually relevant to the item being controlled reduces the learning users must undergo before correct and efficient interactions can take place. In line with this, Yardley et al. [
13] agreed that an easy to use interface is related to motivating effective BCI engagement, which is important for ensuring success.
1.1.5. Summary
Extant research has found that a high proportion of nurses are dehydrated at the end of their shifts and that this can cause cognitive impairment [
3]. Further, it has been shown that a focus on health and well-being within NHS trusts improves staff retention and reduces staff sickness rates [
2]. A reduction in sickness could save the NHS approximately £555 million—an incentive for a program that focuses on nurse hydration. It has been highlighted that there is currently no NHS-wide initiative that targets specific aspects of health and well-being [
5] and that proper hydration provides a foundation for this [
7]. Not much is known about the optimum level of daily water intake [
4], but increased frequency of water intake benefits health and hydration [
11]. Thus, reinforcing regular hydration may minimize the risk of cognitive impairment. At present, there is not a large body of knowledge on DBCIs, although it is known that user-centered design principles can ensure successful engagement [
13]. There is, however, comprehensive understanding about how to effectively achieve habit formation [
15], with emphasis being placed on user desire to engage with BCIs [
16]. Ensuring that people engage with BCIs is largely dependent on norms, habits and contextual factors [
17], while regular salient prompts and cues are vital to ensure successful habit development [
14]. In uncontrolled environments, habits have been shown to form between one month [
16] and upwards of 66 days [
15], with improved results from consistent engagement with BCIs. Given that these periods relate to once-daily actions, it may be appropriate to expect a shorter period with increased frequency [
14]. An easy to use UI is important for ensuring that people engage with devices and benefit from their use [
18]. This can be achieved by using correct mental models, affordances, signifiers and natural mappings [
19]. The findings of this review guide the decisions taken during the design and development of the proposed solution.
2. Methods
The Double-Diamond Model for innovation and design development [
20] was deemed an appropriate methodology for the design of the conceptual solution. The first half of the model focuses on discovery and definition of the problem and context. Hence, this model was used, although during the second half of the model it was discovered that there was another narrowing stage. The authors coined this “The Triple Diamond Model”, as illustrated in
Figure 1, which contains notable project stages. This is similar to the Double-Diamond Model, as it does state that the diamonds can and should be repeated iteratively, but in the context of this research, the triple variation illustrates the process more clearly.
Before choosing appropriate method(s) for investigating the problems experienced by nurses, the first author viewed and analyzed the documentary “The Big Hospital Experiment” [
21], which details the testing of a volunteer healthcare assistant program, covering many of the usual duties that nurses undertake. This was used to learn more about contextual factors that might influence hydration behaviors in hospital ward environments, and to reinforce the authors’ understanding of ward-based nursing. Hand-written notes were taken during the documenting process, focusing on the general daily routines of nurses, the activities they undertake and how and when breaks were taken. After analyzing the notes taken, a user persona for nurses operating on NHS wards (
Figure 2) was developed to provide inspiration and guidance for design decisions, which gave an understanding of the ward environment and nurses’ responsibilities. Further insights were taken from a Royal College of Nursing report on Hydration in Nursing [
22]. The Nursing and Midwifery Council registry data [
23], on the profile of its members, were also consulted to help define the user group; however, this did not include data from private organizations, midwives and nursing associates. The persona was created using recommendations made by Van Boeijen et al. [
24] and based on the personas used by Alzahrani and Alnanih [
18].
Then, the analyzed notes were organized into a list of summative points that were aligned to research findings to formulate questions that could be answered through interview and observations of nurses at the collaborating NHS trust, confirming that the appropriate methods were selected. The list of key research questions is shown in
Table 1, together with supporting literature. The completion of this qualitative research also contributed to the planning of the research methods used.
First, a 30-min audio-recorded telephone interview was conducted with a long-serving, highly skilled and knowledgeable midwife who had previously worked as a senior nurse in hospital wards in the NHS. The in-depth interview focused on the participant’s experiences, daily routines and activities while working on the ward, both as a nurse and midwife. Further, questions were narrowed to focus on hydration, specifically examining what made it easy or difficult to drink water during shifts. The audio recording was transcribed using Otter.ai, an automatic transcription program, and was later edited by the first author to correct inaccuracies. Key sections were highlighted and annotated based on insights given and the key research questions they related to. Key insights were then summarized, alongside key quotes, to allow the authors to refer at a later stage.
Second, an observation study was conducted in the “Patience” Urology ward in Guy’s Hospital, which was closed to the public. The sample of those observed included all present nurses and the nurse management team of any age. The observation was completed using a “fly on the wall” approach. It took place in the ward on the morning of Wednesday, 4 March 2020, from 10:20 to 11:50 a.m., during a period when nurse tea-breaks were being organized. This was deemed an appropriate observation period by the authors, given the variety of activities undertaken by nurses during this length of time, and the insights gained from speaking with nurse management staff. Prior to the observation, the Guy’s Hospital uniform guide was reviewed, so that the author was aware of whom to include in the study. At the beginning of the observation, the author made a request to be taken around the ward and to be shown where nurses typically drank and took their breaks. During this tour, the author had the opportunity to ask questions about normal behaviors regarding hydration (i.e., hydration frequency and chosen drink) and what the preferred behaviors were from a nurse management perspective. The author then sat next to the Nurses’ Station (NS), out of the main area of the walkway, and took tallies and hand-written notes on aspects related to the key research questions, which included: (1) number of bottles being kept at the NS; (2) number of nurses that had a drink of water at the NS; (3) number of nurses wearing fob watches; (4) typical uniform characteristics; (5) commonalities in uniform adornment; (6) reasons for returning to the NS; (7) information points; (8) the different stimuli; (9) how breaks were arranged and taken; (10) routine activities. Immediately following the observation, the first author interpreted and summarized the notes in a list of key insights pertinent to the identified key research questions.
The inclusion of the observational study further inspired the creation of a single event case study that employed the in-depth findings of the observation study conducted at the Guy’s and St Thomas’ Patient ward, a 17-bed Urology hospital ward. The case study aimed to assist the understanding of the phenomena of nurses’ hydration habits in hospital wards and to determine how the proposed device and BCI program could be embedded into real-world hospital ward environments. The case study also allowed for the data captured from the in-depth nurse interview to be cross-validated to enhance the study’s reliability.
Development of Conceptual Ideas
Brainstorming techniques, suggested by the Design Council [
20] and IDEO [
25], a human-centered design community, were used to identify a range of potential solutions. These were narrowed down to five solutions based on viability and achievability: (1) education materials; (2) prompting devices; (3) workflow analysis service; (4) water bottle cleaning and filling service; (5) future-focused ward redesign for staff well-being. It was decided, in collaboration with an NHS Clinical Champion that the interview and observational study would be used to discover whether the development of education materials or prompting devices would be most effective, as the other solutions were either outside the scope of the project or not financially viable. Whilst analysis of nurse workflow, to inform managerial and organizational adjustments, could improve the health and well-being of nurses, it was discounted due to the predicted need for extended research access to hospital wards and the costs that this could incur. Similarly, the investigation of all factors that influence nurse health and well-being for the purpose of informing future ward designs has also been discounted, primarily due to the extended period that this research was predicted to require being outside of the study’s scope. The use of hydration-focused education materials, to initiate behavior change, could have been combined with a diary tool for personal development—both methods are found in the taxonomy developed by Michie et al. [
12]—and the authors agreed that this was a feasible approach, especially if the focus was on nurse education environments which can be easier to access for study. This would have identified how much nurses know about hydration and how to build it into their workflow. If the main issue was discovered to be that nurses are overworked, ward-based nurses might not have had the required attention to focus on creating new routines. As a result, such an approach was thought to more likely help nurses in education become healthier in the future, rather than help the existing workforce.
The alternative conceptual solution envisioned using devices that prompted users to drink, based on their location and the time since their last water consumption. It was suggested that these could be integrated into devices already in use or into clothing. They were seen to offer the potential to be used as a training program which could be workshopped for short periods with ward management teams. This would aim to develop behaviors within short timeframes and enable the device to be reused in different wards, reducing overall costs and reducing the cost to the environment through minimization of resource consumption and transportation. By doing this, it would allow for iterative development between different wards or trusts to refine the solution, making it less of a financial commitment. The authors agreed that this solution would be a viable approach and it was suggested that combining this with education materials might ensure success and motivate individuals to engage with the device.
4. The Proposed System
From this point, the paper reports the development of a behavioral change intervention system to support the hydration habits of nurses, using a fob watch-integrated BCI device that prompts nurses when to drink, as shown in
Figure 6. This was chosen as the checking of a watch for the time was perceived as a habitual action—an opportunity to form a new habit of checking the time and hydration levels simultaneously. Using a habit-based BCI would provide an opportunity for the devices to only be required for the short period that habits take to form and would thereby offer an environmental and financial benefit. For the context of this study, hydration habits were defined as “the regularity with which one considers whether they need to drink, and the regularity with which one chooses to drink”. This decision was based on the findings of Elmadfa and Meyer [
11]. Given this definition, hydration habits would be considered to have improved if the frequency of both actions had increased in a manner that would not impede the completion of other normal actions or duties. The idea of a smartwatch is not foreign to nurses, as many health trackers already take this form—conceptually making a new BCI device understandable and easy to motivate interaction with. A fob watch is usually worn in plain view of others—an opportunity to create a visual indication of a nurse’s hydration level and an opportunity for staff to support each other if they require water. This idea was prompted by the verbal arrangement of breaks, an opening to help staff gauge who needs relieving. The use of this prompting device was proposed as part of a habit formation program, whereby the device would be used for 8–12 weeks, based on the findings of Lally et al. [
15] and Foster et al. [
16]. This period would be confirmed during the trial phase of the device development and could be adjusted over time as data are collected. Data collection capabilities were proposed to enable iterative development as the program grows; data analysis may provide insights into why behaviors exist and how they change. These data could also expand the limited research into nurse hydration, potentially informing future decisions on how staff welfare is managed. In this way the BCI device could also lead to larger scale developments in the future.
The associated training program would be run as a service, similar to the NHS Improvement’s 90-day staff health and well-being workshops [
5]. The service would include the setting up of devices, the provision of a means to charge them, and a temporary water bottle storage point. In addition, it may be necessary to provide hygiene-assured bottles, although this would have cost implications. The fob watch user guide would include information on best hydration practices; creating this would require a more comprehensive review of existing literature and guidelines. At the closing of the program, nurses would return the devices, and would be either encouraged to purchase their own fob watches for daily use or would be provided with them depending on the service budget. This concept direction was agreed as a viable approach, with the deliverables being set as: (1) identification of suitable technologies; (2) development of a UI; (3) a fully visualized fob watch design; (4) device computer logic development; (5) service parameter identification.
4.1. Technology Selection
The focus of the proposed deliverable was hydration regularity and prompting users when they had not consumed a drink for a certain time period. At a basic interaction level, this meant that the device would need to register when users drink, preferably automatically to place this burden on the system. Given the suggestion of providing a bottle storage point as part of the service, it was appropriate to explore the fob watch and water bottle communicating wirelessly. If a water bottle acted as a wireless ID tag, the watch could then register when a nurse drank from it, using proximity or motion detection. Another option was considered—if users spent a defined amount of time at wirelessly tagged water points, such as the bottle storage station or break room, although this would be open to increased error, a nurse may not always have had a drink when visiting the station. The last option was that nurses record their own drinks on the device, though this could lead to lower compliance rates. Due to the wireless nature of the interactions, the authors researched different wireless technologies and defined six key interaction points: (1) wireless communication and sensing; (2) interface/watch control; (3) prompts/cues; (4) attachment to uniform; (5) watch identification so that nurses could use the same watch each time; (6) the watch’s display.
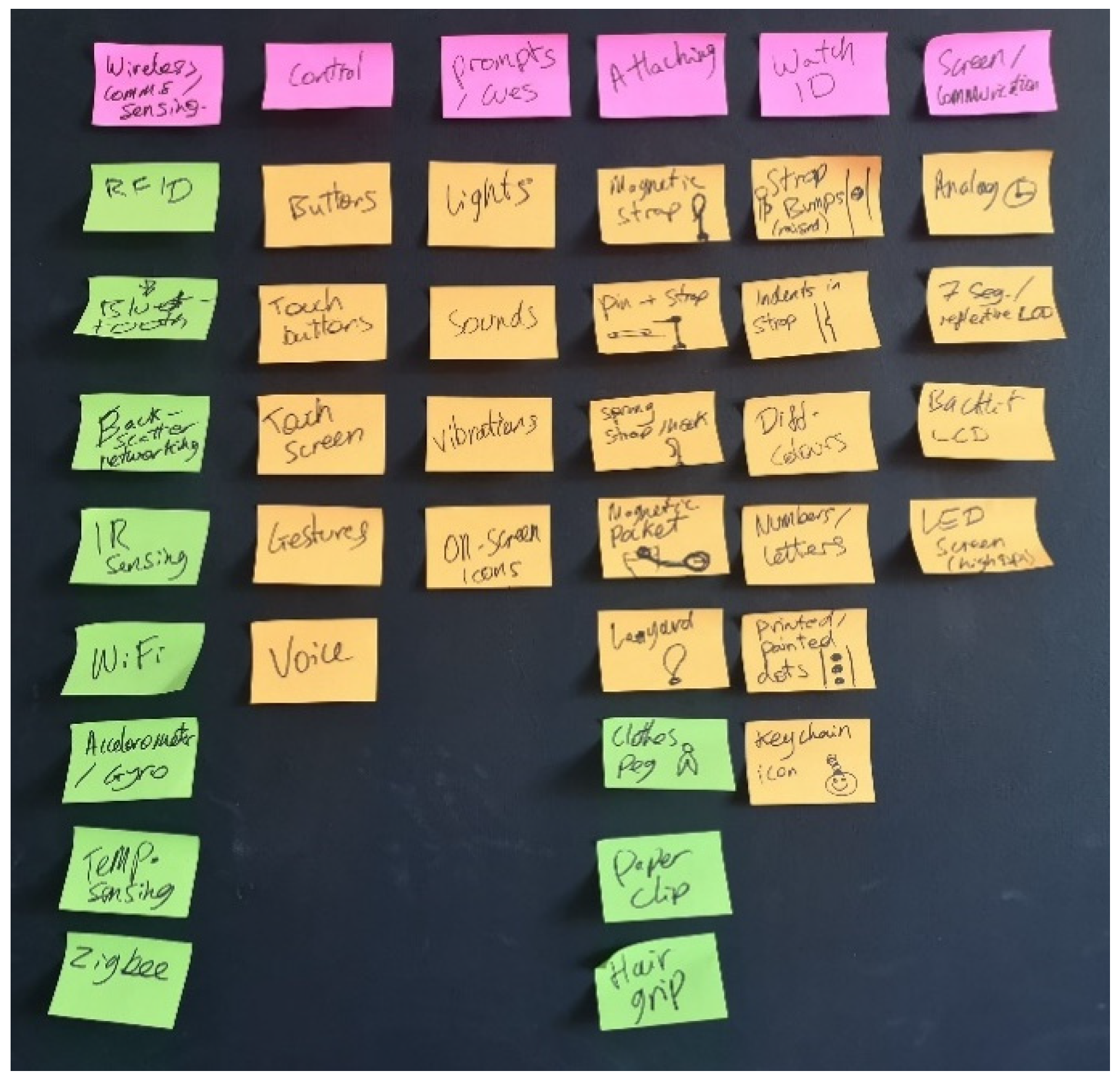
This identification led to a second brainstorming stage, the results of which are shown in
Figure 7. This stage explored the available options for each category. Wireless communications were narrowed down to Bluetooth Low Energy (BLE), a form of communication designed for lower-fidelity data and low-power devices [
28]. BLE does, however, require active tags, meaning that all data points must have a power source, though with low power consumption these could last for months or even years with a small battery; this is demonstrated by the Tile Sticker [
29], a 27-mm wide BLE tracking device that that has a battery life of two years.
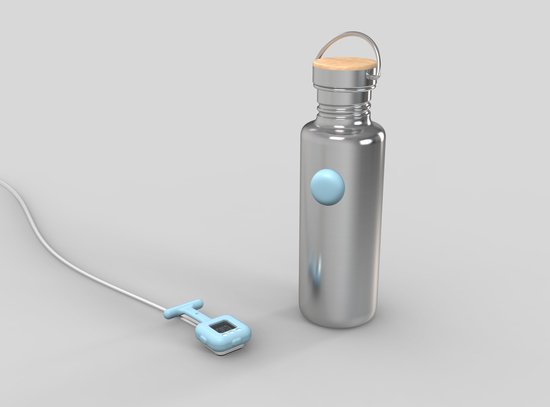
Two BLE enabled Arduino Nano boards were used to test the wireless communication. The BLE boards can pair with each other, with one board being set as a central device, similar to a Wi-Fi router, and the other being set as a peripheral device, similar to a device connected to a Wi-Fi router. The devices can then pair, meaning that they remember each other’s identity and can be set to only be connected to that device. Giving the water bottle gyroscopic and acceleration sensing capabilities would allow it to automatically detect a drinking motion (i.e., the water bottle is raised and tipped to horizontal for over a second), and to register if a drink was taken in close proximity with the paired device; this can be detected using the BLE signal strength, linked to the Received Signal Strength Indication (RSSI) [
30]. The bottle can then send a data packet to the watch device, which will register that a drink has been taken and will reset the hydration tracker. This would mean that each nurse would need a bottle with this capability, which would be expensive if the technology was embedded into the bottles, not mentioning the challenge of waterproofing the contained electronics. To avoid this expense, it was decided that the technology would be embedded into a small housing that could be temporarily attached to the water bottles, the Bottle Device (BD). If the BD was required to be waterproof, enclosing it in silicone using over-molding would be a cost-effective way to achieve this on a batch production scale [
31]. This would mean the devices would become single-use, having an environmental impact, as the batteries could not be charged or replaced. In using BLE, this would be possible, though may add expense if the devices were disposed of at the closing of each program. A more expensive manufacturing method would be to have a charging port covered by a seal to allow device reuse, but a cost-benefit analysis would be required during future development to establish the optimum method in terms of sustainability and expense. This research progressed by using disposable sealed BDs. Given the service nature of the solution, the devices could be disposed of and recycled in a cradle-to-cradle system to mitigate any environmental impacts.
4.2. Fob Watch Interface, Prompts and Display
Whilst the interactions were to be mainly automatic, users would need to communicate with the device. The ward environment contains many stimuli so the watch interface could not add distractions or be affected by external stimuli, ruling out voice control. Gesture control has been used in many modern devices, though it can be unreliable and less efficient than using a simple button press. For the watch control, this left only mechanical buttons, which can be very low profile (i.e., smartphone volume buttons), and touch buttons or a touch screen. To determine the most appropriate communication methods, it was necessary to identify the types of information that would need to be communicated. The authors split these into two categories: the “Tracker” and the “Watch”. The Tracker element would communicate the added functionality of the fob watch, such as the length of time since the user’s last drink (the prompt), and the BLE connection status. The Watch element would communicate the usual elements, such as the time and use of a stopwatch function. This was broken down further to determine the required communications: time since last drink; drink registered successfully; BLE pairing/connection successful; battery level; time of day; stopwatch; system error occurred; factory reset successful.
Sound was eliminated for the prompting method due to potential conflicts with other auditory stimuli and the variety of prompts that would be required in the hospital ward environment. Vibration was eliminated due to the physical nature of nursing. This would make vibrations hard to identify, especially given Phantom Vibration Syndrome where users believe a device has vibrated when it has not [
32]. This left either indicator lights on the watch body, or on-screen icons, depending on the type of display chosen.
One display option was to use an analogue watch mechanism to display the time and rely on another feature for the remaining communications. The authors decided against this, given the interviewee’s comment that digital fob watches are more convenient. Another option was to use a reflective seven-segment Liquid Crystal Display (LCD), as used by many modern digital watches. This would be inexpensive if a standard display were used, although it would be possible to manufacture a custom display that could show more relevant information at a slightly higher cost. These displays are also low powered, another positive for a sustainable wireless device. Another option would be to use a backlit LCD, akin to many computer monitors, or a Light-Emitting Diode (LED) display. This would have required added expense and been power intensive but would have been able to show a higher information fidelity. The last option was a dot-LED display, seen in recent fitness trackers; this would have been a low-power and inexpensive solution, but would have been limited in terms of the information it could display. Ultimately, it was decided to use a combination of a seven-segment reflective LCD screen and LEDs placed on the body of the watch for the Tracker. This decision was made in part to separate the Tracker and Watch displays to make it easier to see them at a glance but to also provide the Tracker prompts with a higher salience, a requirement for habit formation [
14]. This approach would also minimize cost and power consumption. Furthermore, it was determined that three LEDs would be sufficient for the Tracker’s display, based on the number of available combinations and that white LEDs would be the safest option. It should be noted that white LEDs are more expensive than red, green, or blue LEDs. They can also show a range of other colors, leaving the tracker display open to expansion, if required. White LED combinations were also considered to avoid potential color associations from confusing the interpretations of the messages being shown. These associations can vary in meaning between cultures [
33] and could be unpredictable for a multicultural target group. Given these decisions, it was decided to use mechanical buttons as the main interface.
4.3. Form, Attaching and Identifying
Forms were ideated using thumbnail sketches on paper, as shown in
Figure 8. The form covers three key elements: overall shape, how the device is attached to clothing and how nurses identify the correct watch at the start of a shift. Many different forms were considered, including a device that would attach onto a fob watch, but this was discounted due to infection control reasons. Fob watches are available in several variations, such as in silicone housings, attached to a metal chain, or attached to a clip. The silicone and chain watches use a lockable safety pin to attach to clothing, with the silicone watch being more common during the observation study at Guy’s Hospital, possibly due to its ease of cleaning, clinical appearance and low price. For these reasons, a silicone housing style solution was chosen, ensuring user familiarity with the device. Two main forms were identified—circular or a rounded square. The rounded square was chosen, as the authors found it difficult to apply pressure to a circular silicone watch (
Figure 9) as though buttons were being pressed.
Different methods for attaching the watch device to clothing were also considered, with the locking pin chosen in this case. Whilst attaching using a pin could be more time consuming than something that clipped directly onto a pocket, it was selected as it would be inexpensive to produce and provided the least complex manufacture process; further, it would be easy to repair or replace if broken or lost, and would not require uniform modification and could be placed anywhere on nurses’ clothing. Using options such as a hairgrip style fastener or a magnetic attachment would limit this placement. Removing this freedom from the experience could lead to lower participant engagement, especially if the watch could not be placed in the most convenient position, which may vary between users. The above decisions led to the form shown in
Figure 10, with several options for LED placement.
Attaching the correct device at the start of shifts would be vital. For this, nurses would need to easily identify their own watch at a glance. The most obvious answer to this was color, something that is easily imbued into silicone. This can also be changed whilst using the same production mold, which lowers the cost of production. To test how many colors could be used, the authors created a palette of nine colors which would be suitable for the environment and easy to distinguish between, based on Boynton’s 11 colors “that are almost never confused”, as shown in
Figure 11 [
34].
It was found difficult to create a larger palette without encountering similar colors. This was an issue, as hospital wards are likely to have more than nine nurses in a team and may have more than this on shift at one time. A range of solutions were considered, such as placing stickers on the watch straps, which could rub off, or keychain-like tags with names or icons on, which may fall off. Whilst acting out the attaching of a fob watch, the first author found that they held the strap. This provided an opportunity for a physical indication that could not only be seen but felt. If the strap had bumps on its surface, the user would become used to the feeling of attaching their watch. If they picked up a watch with a different number of bumps, they would have a chance to see this but also feel it—a form of fail-safe. Whilst using symbols or letters in place of bumps would have provided a larger range, these would not be easy to feel and could be visually problematic at a small scale.
Attaching the BD was intrinsic to its form. Following ideation, two solutions were reviewed: (1) use an adhesive to temporarily attach the BD or (2) use a watch-like strap. It was realized that some nurses may not want to provide water bottles for reasons of expense, while other nurses may already have their own water bottle and want to continue using it. This meant the attaching method had to be universal. The device would also have to withstand the interactions that a bottle undergoes, such as being jostled in a rucksack or washed with hot water. Furthermore, the BD could not pose an issue for infection control and must be easy to clean and not have parts that might trap bacteria. For these reasons, the adhesive attachment was chosen. The form of the BD was also a focus of ideation, though the most appropriate was again the simplest—either circular or a rounded square. The rounded square, whilst in line with the fob watch design, posed an issue—the corners could make it likely to get caught and dislodged.
4.4. Summary of Design Decisions
In summary, the design decisions taken for the development of the conceptual design were to: create a digital fob watch device with LCD and mechanical buttons; indicate “hydration tracking” times through use of LEDs; have all in a separable silicone housing; attach to clothing using a lockable safety pin; utilize BLE communication capabilities; pair with a single-use “bottle device”; have an enclosed (waterproof) silicone housing; attach to bottles using an adhesive; register drinks using gyroscopic and acceleration sensing; communicate this to the watch using BLE.
4.5. User Interface Development
To test using three LEDs for the Tracker communication, UI tables were created that detailed the messages that the LEDs would need to show, in six categories: (1) general UI (device has turned on etc.); (2) tracker display (drink timing); (3) tracker display interrupts (system error etc.); (4) battery display; (5) charging display (when connected to charger); (6) BLE pairing (connecting devices).
LED flash patterns were designed for the different messages and tested using an Arduino board and LEDs wired on a breadboard. The flashes were kept below 5 Hz in frequency, as going above 5 Hz created a small likelihood of triggering a seizure in someone with photosensitive epilepsy [
35]. This was deemed an unacceptable risk, especially given the medical context of the research. Light flashes above 65 Hz become safer [
35], though are not usable for LED flash messages, discovered during Arduino testing.
The flash patterns were designed based on the findings of Harrison et al. [
36], who discussed the most successful pattern types for an LED indicator on a mobile phone. It was found that three LEDs were sufficient and, therefore, it was decided to use this number for the final design. Alongside the LED flash tables, tables were created for the button press interactions, relating to the BLE pairing, battery display and LCD display. This proved that the watch device would only require three main buttons for the major interactions, with three different button press lengths. At this stage, the user journey was updated with the identified service interactions, as shown in
Figure 12.
4.6. Form Development
Given that the physical elements of the device had been confirmed, the form was iterated further, in this instance, using digital illustrations followed by three-dimensional computer-aided design models. To find the correct scale and button placement, physical models were created (
Figure 13) and tested with two users with different hand sizes. This identified a comfortable size for the device to be gripped in one hand, although in future this would need to be confirmed using anthropometric data sampled from UK citizens, which could not be accessed at the time. Two different button arrangements were tested, with the easiest arrangement for all three buttons to be pressed with one hand being to place a button on each open edge of the watch body. The LCD display was developed with a battery display and an icon to indicate whether the watch was in Clock or Stopwatch mode, with a focus on keeping the LCD uncluttered and easy to read at a glance. The LED shape, size and placement were then ideated. The chosen solution was selected for reasons of visual balance and aesthetic quality, as well as ease of viewing whilst checking the time and observing other users’ watches.
The ID bump shape and placement were also experimented with, with the discovery that visual balance could not be achieved with more than three bumps. Physical prototyping of the watch could not be carried out during the study, though this would be required to confirm the appropriate form elements. The above elements were combined into a final design, shown in
Figure 14, which was then 3D modelled using Solidworks software. The three-dimensional aspects were modelled around the inclusion of a clear plastic window, an LCD, a printed circuit board, a 3 V rechargeable lithium battery, a rear battery contact, three LED lightguides and three mechanical buttons. The dimensions were estimated using comparable components in the first author’s possession or from manufacturer specifications. This was contained within a half-plastic (most likely injection-molded ABS), half-aluminum alloy casing. This would allow the back of the casing to function as a contact for charging. The watch strap bumps were experimented with, with the design changing to indents rather than raised bumps; this was completed for aesthetic reasons, but also because it was realized that repeated use may produce small protrusions over time.
The BD model was developed with the assumption that the silicone housing need only contain a CR2032 3 V battery and a Printed Circuit Board (PCB) with a button mounted on top. These preliminary models allowed for the visualization of the final design but would not be appropriate for production. A charging dock, shown in
Figure 15, was also created for the purpose of visualization and to explain the interaction of charging.
4.7. Service Provision
Preliminary service parameters were identified for the purpose of contextualizing the developed devices and to explain their integration into the service. This was carried out with a focus on creating a user experience that makes the service accessible and encourages high participant engagement. The service would require further development before being trialed.
The service would involve the provision of a water point where bottles can be stored, and watches can be charged. The fob watches would arrive one or two days before program commencement and would be set up by a Program Liaison. This would involve pairing the watches with BDs, checking for faults and placing them on charge. Each nurse would be assigned a watch color, ideally by preference, to add to the quality of the user experience, and a number (1–3) relating to the indents on the watch strap. The Liaison would establish the importance of the nurse handover—when watches must be removed from their charging points and attached to uniforms at the start of shifts and replaced on charging points at the end of shifts. Nurses would be encouraged to remind each other at this point, as it may be easy to forget to attach or remove a watch. The guide would explain that nurses can drink from the bottle to which they attach their BD, and that the watch will register this automatically. If they are not drinking from this bottle, drinks can be registered by pressing the Tracker UI button. The bottles would need to be approved in relation to infection control and may need to be provided as part of the service.
At the beginning of shifts, when the watches are removed from the charging points, they will begin tracking at zero. This means that an internal circuit will begin timing the period between drinks, lighting up an LED as each hour passes. When the fourth hour without drink registry is reached, the LEDs will begin flashing. These time periods are preliminary only and would require validation during trials. During the shifts, watches will collect data on how frequently drinks are registered and how they are registered. When the watches are placed on charge, they will transfer these data to the water point. This would be completed either through the charging points or using BLE communications and would be confirmed during later development. The data would not be personalized to assure nurses that they are not being tracked in any way and that the data are used to provide insights only. The data would then be processed at the closing of the program with regard to the following questions:
Has hydration frequency improved during the program?
At what level do prompts become most effective?
Have hydration types changed (bottle vs. manual registering)?
Does one nurse drinking remind other nurses to drink?
Are there good or bad times of day, or activities, for hydration frequency?
How does the program effectiveness vary between wards?
Data analysis can then be completed over time to refine the service and adapt it to different hospital ward environments. It can also inform future decision makers and industrial designers about ward design, with respect to nurse health and well-being, and decisions relating to staff and workflow management, especially with regard to times of day or activities where it is particularly difficult to remain hydrated. At the closing of the hydration program, the liaison can discuss with the nursing team the overall improvements that have been made and any points for further development. This creates an opportunity for nurses to view the progress they have made and to celebrate. It would also allow nurses to discuss if they have noticed any changes in their health and well-being; in future research, it is worth considering whether a survey could be used to collect data on these changes. The technological water point components would be removed, leaving behind a simple water storage area. This would provide nurses with continued ease of access to water on the ward, without sacrificing technological components that can be reused in the interest of reduced cost and added sustainability. Nurses would be encouraged to continue using fob watches where possible and it may be possible to provide these at the closing of the program. These provisions would help with the maintenance of new hydration habits but would have financial implications and may be dependent on the level of service provision requested by the NHS trust.
4.8. Case Study
To clarify how the service would be implemented, a case study has been presented in the context of Guy’s and St Thomas’ Patient ward—a 17-bed Urology hospital ward. For the purpose of this case study, a number of assumptions have been made: (1) the water point design and water bottles have been cleared for use by infection control teams; (2) the methods have been validated by a trial stage using hydration and cognition tests; (3) the ward operates on a 12.5-h shift roster with five nurses per shift and 20 nurses on the roster in total; (4) nurses wear a pre-COVID-19 level of Personal Protective Equipment (PPE); (5) ward/hospital management have requested the implementation of the service. To begin, the Program Liaison completes an analysis of the ward, primarily to determine where the water point will be located in the nurse station (dependent on minor rearrangements, power supply availability and proximity to electrical equipment) and how large it needs to be, dependent on the number of required water bottles and fob watches. Then, the Program Liaison will install the water point and charge the fob watches, within a timeframe agreed with the hospital management team. Nurses on the ward will be informed of the intention to carry out the optional program and will be provided with informational material to explain its purpose and the benefits of taking part (i.e., improved health and well-being, and improved ability to provide healthcare).
The 12-week program will begin with an introductory session wherein the Liaison explains the use of the fob watches, BDs and the water station to participating nurses. It will be necessary to schedule such sessions with ward management to avoid interruption of healthcare practices. During these sessions, the nurses will be encouraged to use the connected water bottles (nurses own bottle or bottles provided by the program) to supplement their usual hydration habits and will be provided with informational materials covering the fluids most appropriate for hydration, and the impacts that different drinks can have during a shift (i.e., high sugar or caffeinated drinks). There will also be a focus on drinking from reusable bottles to reduce the environmental impact of consuming water from disposable containers, especially single-use plastic containers. The Program Liaison will then express the importance of avoiding peer pressure or coercion regarding the drinks nurses choose to consume and will stress the freedom of choice that nurses will continue to have throughout the program. This will act as a measure to avoid any ethical or legal issues that could be encountered by a lack of clarity as to whether the employer is forcing the consumption of water upon their staff, and the reduction in productivity that this perception could cause through a disruption of workplace harmony. Nurses will be reminded that the Tracker UI button can be used at any time to register any drink not taken from their connected bottle.
Nurses will then begin to use their fob watches, which will record data anonymously and transfer them to the water point when charging. The water point can then either upload these data to a remote server using an available internet connection or store it, depending on connection availability. This can enable an analysis software to monitor the use of the watches and flag any issues that may arise involving improper use. It may be necessary for the Program Liaison to return to the ward if any issues of misuse or poor device functionality arise. At the close of the 12-week period, the Program Liaison will return to the ward and collect all fob watches and BDs, and then remove the charging and data storage components of the water point. This would leave behind a dedicated bottle storage area in the nurse station and allow for the reuse of the technological elements of the service to reduce environmental impact and reduce NHS costs. A survey will be administered to participating nurses to record qualitative data regarding whether they perceive their health and well-being to have changed and their perceptions of the service quality.
This case study brings to light several potential limitations. Firstly, a Urology ward does not typically require extensive use of PPE, although developments in PPE usage throughout the Coronavirus pandemic have highlighted that a fob watch may not be visible or usable whilst wearing gowns over uniforms. For the proposed solution to be effective while using such PPE, the device design and location would need to be further considered in later stages of development. This may address the limitations of the BCI device in environments where extensive PPE is typically worn (e.g., operating theatres). Secondly, the service procurement may depend on whether employers perceive it as a necessary expense, for which preliminary hydration and cognition testing of staff may be required. Thirdly, this approach is limited by the lack of inclusion of the employers as participants in the process and would be improved by giving access to data for managerial insights. They may also benefit from using an adapted version of the service tailored to office environments, which could adjust employer perceptions of the need for improving hydration.
4.9. Discussion
Insights from both the in-depth interview and video observation suggested that the best approach for implementation would be to provide a sanitary water bottle storage area, i.e., the water point, and to integrate a BCI within a device that is both familiar and visible—i.e., the fob watch. The workshop nature of the solution allows for resources to be reused, rather than equipping each nurse with a smart water bottle which inflates costs and decreases the sustainability of the solution (i.e., increased transport, resource extraction and consumption). Due to the limited capacity for trialing and testing during this study, the solution proposed is conceptual only.
Due to the above points, the authors believe that the proposed solution can be an effective short-term and low-cost approach, with the potential to inform longer-term environmental adjustments (e.g., improved ward designs) that may require larger investment. Given that hospitals require constant development and improvement in pursuit of the highest quality healthcare, pairing data collection with well-being improvements has the capacity to improve hospital wards and healthcare provision in both the short and long term. A key component of this is to develop understanding of nurses’ behaviors to enable the improvement of future hospital wards in a staff-centered and user-centered manner. This study confirms that the issues faced with regard to personal hydration in nursing, and the prioritization of healthcare provision over nurse personal welfare, have roots in behavioral psychology. In order to limit the potential impact this has on patient well-being, an approach that can create healthy habits while providing more detailed insights into existing behaviors was developed. However, this does not conclusively mean that the device designed is the best approach, especially given the extensive PPE now worn in hospital wards; further development is therefore required before the proposed solution can be made effective in the current environment.
The proposed solution may also be more effective than other hydration station solutions, as discussed by Boustead [
10], due to its focus on behavior change and habit formation. At the time of the study, no studies exist that propose alternative solutions to combat the issue of nurse hydration.
5. Conclusions
This paper reports the design development of a behavior change intervention device and service provision aimed at supporting the health and well-being of personal hydration habits for NHS ward-based nurses. Whilst further development of the device and program is required, the authors believe that the relevant aspects of the solution have been well defined. Further practical development should be conducted to explore form development and testing, a key component of the user experience. More stakeholders should also be incorporated, as the design process followed has not been wholly user-centered. Further, this research requires greater user testing to confirm that the applied theories work. The ramifications of COVID-19 have limited participant engagement and the physical prototyping of elements in the design, though it is believed that the solution can progress into a trial stage after additional development of the service, the water point and the design for manufacture.
Further developmental work should focus on how disinfecting can be incorporated into the process, especially with the reuse of devices. The more stringent infection control standards of the current healthcare climate may have implications for the use of a water point, and this should be a focus for future development. Concerns were raised by management at Guy’s and St Thomas NHS Foundation trust on how the system would work given the required PPE during the COVID-19 pandemic. Further exploration is required to make prompts salient under this PPE, and to consider whether an alternative device may be more effective. Another concern was whether nurses drinking could appear unprofessional. It may be worth surveying healthcare service users to gain a view of public opinion on this. This would help to develop approaches to dispel concerns, given the importance of hydration and improved patient care. Something that might benefit the solution would be the incorporation of cognitive testing before and after the program, to identify if any changes take place. This would be time costly and may only be relevant to the trial stage of development to prove efficacy. Another aspect of development that should be focused on is the user experience for the differently abled, as the communications chosen may not be appropriate for all users. This solution could be transitioned into other sectors with similar workflows, such as factory production lines. It could also be used to track aspects of staff behavior, but it should be noted that this could easily become invasive. In a later study the solution could also be used to investigate whether transitioning to a more flexible time management approach—for instance, taking more regular and shorter breaks—could improve staff health and well-being. This could avoid the complications of the proposed solution caused by infection control and disruption of professional image.