Abstract
Immunization is one of the most cost-effective interventions in global health and has a crucial role in achieving 14 of the 17 sustainable development goals (SDGs). The issue of sustainable financing for new vaccines is particularly pertinent as Indonesia transitions away from extensive Gavi support towards a self-financing immunization system. As the current immunization system transitions, practical solutions must be found and applied to provide more flexibility in the budget for financing immunizations without sacrificing the current healthcare system’s needs. Despite the fact that economic evaluation studies are essential as an initial step to ensure financial readiness, the lack of reliable data is the first barrier to Indonesia’s journey toward a self-financing immunization system. To overcome this problem, standardization of data collection strategies and methodologies are required. In particular, Indonesia may have to explore other options to increase revenue for its immunization system, such as through general revenue from the central government, a sector-wide approach to financing, and a national trust fund. To deal with the tight immunization budget and its consequences, Indonesia also has to restructure its immunization system, which can be implemented through province block grants, insurance mandate and subsidy. Taking the potential of a COVID-19 vaccine into account, the Indonesian government should consider a number of costs and issues beyond the development and procurement of vaccines. The costs of delivering vaccines to the remote parts of Indonesia, implementing the necessary infrastructure, and modifying vaccine delivery are also important in this time of transition. These constraints must be addressed in the new self-financing system and other public health efforts must be increased to decrease the burden of infectious disease as Indonesia develops a stronger immunization system.
1. Introduction
A decreased fear of contracting contagious diseases in the last decade has been significantly correlated to prevention strategies, such as vaccinations. A vaccine, as defined by the World Health Organization (WHO) [1], is a biological preparation that improves immunity to a particular disease. Vaccines typically contain an agent, resembling a disease-causing microorganism, that is in a weakened or killed form of the microbe, its toxins, or its surface proteins. Currently, vaccinations are typically recommended from childbirth to protect a child’s weak immune system. Vaccinations continue into adolescence, building and strengthening the immune system’s response to infectious disease agents. While this usage of vaccines has increased worldwide, preventing the contraction and spread of many infectious diseases, there are some diseases that still persist. Developing regions are disproportionately affected by this problem. The total number of healthy life years lost per capita was 15-times greater in developing countries than in developed countries [2]. Although the burden of infectious diseases is markedly high in low-income countries (LICs), the WHO reported that the majority of vaccine-preventable diseases (VPDs) actually occur in middle-income countries (MICs) [3].
As one of the most cost-effective medical interventions, vaccinations are considered to be a critical tool to reduce health inequality, ensure the greatest possible protection of health and wellbeing, promote peaceful and inclusive societies, and strengthen the means of implementation for the Sustainable Development Goals (SDGs) [4,5]. Therefore, sustainable financing for new vaccines is critical to ensure immunization systems can reach every targeted population with the vaccinations they deserve. This article aimed to discuss the challenges and proposed strategies on sustainable financing for new vaccines in MICs by using Indonesia as a reference case.
2. Importance of Sustainable Financing for New Vaccines
There are numerous costs involved in the financing of new vaccines. These costs include, but are not limited to: (i) research and development (R&D) costs; (ii) costs related to the regulatory approval process; (iii) ongoing regulatory costs; (iv) plant costs, including depreciation; (v) marketing costs; (vi) variable costs (i.e., labor, production, equipment, and supplies); and (vii) liability costs [6]. During the 1970s, the overall cost was relatively low. However, in the 1980s through to the early 1990s, the price for vaccines sharply increased before stabilizing later in the 1990s [6]. While the price of older vaccines remains stable, new vaccines tend to garner increasingly higher market prices. Experts estimate the cost for a new vaccine entering the market to be approximately USD 700 million [6]. The WHO has emphasized that new vaccines are now high in demand in all countries [7], thus requiring more efficient funding of their production.
The staggering amount of money required to maintain and develop an immunization system evokes the following questions related to the source of financing for immunization services and its sustainability. The answers to these questions depend on the country. For example, the United States is a self-financing country. Due to its high income, the federal and state governments share the responsibility of financing vaccines. Indonesia, however, is new to self-financing since the extensive support from Gavi, a global vaccine alliance, has ended [8]. In the context of sustainability, this situation pushed the government of Indonesia to find a capacious, substantial, and reliable way to finance the immunization programs. With the current budget and the number of new vaccines to be financed, this would be difficult because Indonesia’s previous reliance on Gavi assistance provided a sizeable amount of support to the country’s health financing system [8]. At the end of extensive support from Gavi, Indonesia received USD 47.6 million in the period of 2017–2018, with the majority of the budget being used for the measles-rubella vaccine (58.30%), inactivated polio virus vaccine (31.03%), and vaccine introduction grants (8.43%) [9]. As the current immunization system transitions, practical solutions must be found and applied to provide more flexibility in the budget for financing immunizations without sacrificing the current healthcare system’s needs. Given this information, it is necessary to explore several strategies to finance the implementation of new vaccines in addition to fortifying the availability of vaccines in routine immunization programs. The following sections will present and discuss three steps to fund and implement new vaccines, such as conducting economic evaluation studies, increasing national revenues, and restructuring the immunization system.
2.1. Economic Evaluations of New Vaccines
Up to now, countries have been encouraged to implement economic evaluation studies as the first step to determine whether the presumed benefits of adding a new vaccine in a country are worth the costs at a certain point in time. Performing an economic evaluation study before choosing to introduce a vaccine to a national immunization system is essential to ensure financial readiness. Previous studies highlighted three key issues for evaluation studies to review when establishing a national vaccine demand [10,11]. The first matter is determining the public health priority of a disease by estimating the magnitude of the disease burden and the presence or lack of effective strategies to prevent and control the disease [10,11]. The second matter is establishing the vaccine’s safety, performance, availability, and other characteristics, such as economic and financial attributes [10,11]. Lastly, the third matter is taking into consideration the country’s ability to successfully introduce and deliver the vaccine long-term [10,11]. The combination of data from these three focus areas is indispensable when working to convince policy makers on the necessity and urgency of a new vaccine introduction.
Learning from the experience of rotavirus, pneumococcal conjugate vaccine (PCV), dengue, and hepatitis A vaccines, several economic evaluation studies have been conducted in Indonesia to assist the government on the potential introduction of these new vaccines [12,13,14,15,16,17]. Several studies recommended that new vaccines can be considered as cost-effective interventions to be implemented in Indonesia. These comprehensive assessments have proven to be effective to assist the stakeholder in including new vaccines into the national immunization programs. As we can determine from this example, economic evaluation studies mark a pivotal point in the process of financing and implementing new vaccines. They provide policy makers with the evidence required to make decisions that can positively impact the immunization system. The biggest challenge to conduct economic evaluation studies in Indonesia is the lack of reliable data and information on the burden of disease, as occurring in other countries in Southeast Asia [18]. Even with sufficient data on disease burdens, policy makers also need information on economic benefits and the cost effectiveness of a new vaccine [18]. Indonesia has had particular difficulty in obtaining such information. The country lacks a standardized method for data collection and analysis [19]. This is largely due to the fact that the majority of patient data is recorded on paper and there is no standardized platform to document and upload information [19]. This lack of reliable data availability is the first barrier to Indonesia’s journey toward a self-financing immunization system. Indonesia must begin with standardization of data collection strategies and methodologies. An increase in quality data from economic evaluation studies will allow healthcare officials to better convince policy makers on the importance of providing ample revenue to the immunization budget.
2.2. Increasing National Revenue
Next to economic evaluation studies, with the termination of extensive Gavi support, Indonesia may have to explore other options to increase revenue for its immunization system. WHO in collaboration with Gavi developed a resource for policy makers titled “Immunization Financing Options” that presents multiple solutions for financing immunizations in countries with limited resources [20]. In the context of Indonesia, there are three strategies from several published studies that may be valuable and practical to be implemented. Firstly, it is by far the most common practice to use general revenue from the central government, that is, funds from national general tax or public revenues, as the main source of funds for national immunization programs around the world [20]. Increasing the amount of general funds from the central government allocated to Indonesia’s immunization program would be the simplest option to increase the programs’ revenue. Reallocation of general revenues has been particularly useful in MICs. Applying this strategy, several MICs in Latin America have been able to successfully reorganize their central government general revenues to provide sufficient funding for their immunization programs [20]. Although this is a simple approach, there are some pros and cons to consider.
Secondly, the sector-wide approach (SWAp) is a method used by donor and recipient countries to organize support for a developing country’s healthcare system [20]. The donor and recipient countries discuss targets of the health care system in order to improve its services and enhance equity. This may be a beneficial opportunity for Indonesia to redefine the national immunization system during the shift to self-financing in order to better meet immunization goals. Donor organizations provide funding for the external framework of the vision set forth by the recipient country [20], leaving the recipient country with the responsibility to make sufficient use of the funds. SWAp is a new development, but has been implemented in countries such as Zambia, Ghana, and Bangladesh. The World Bank sees this practice as a move in the right direction to funding and developing health sectors, but the method requires monitoring and refinement to ensure countries are able to meet their healthcare goals [21].
Thirdly, a national trust fund to generate income for a particular purpose, with specific rules about how the proceeds can be used [20]. The financing of this fund can be domestic or external. In the establishment of the fund, there must be a memorandum of understanding to define the responsibilities, rights, and obligations of the founding partners and contributors, the goals to be attained, organizations to be created, operations envisaged, reporting required, and when and how results are to be reviewed based on performance and achievement criteria [20]. Once this is established, it is the responsibility of the governing board to control the trust fund’s development and use. This is a beneficial option for Indonesia to cultivate a source for long-term financing of the national immunization program as it transitions to self-financing. The long and successful story of Bhutan on running national trust funds for healthcare can be used as a reference case. The goal of the Bhutan Health Trust Fund is to help sustain and achieve self-reliance in the primary health care sector by eliminating financing uncertainties through income generated out of capital investments [22]. The country began to build its trust with public donations from a movement called Move for Health Walk. In 2015, the walk alone raised more than three times the amount the country spent on vaccinations that year, which has proven that trust funds can be an important contributor to immunization financing in Bhutan. More detailed information about the pros and cons of the strategies to increase national revenue can be seen in Table 1.

Table 1.
Strategies to increase the national revenue.
2.3. Restructuring the Immunization System
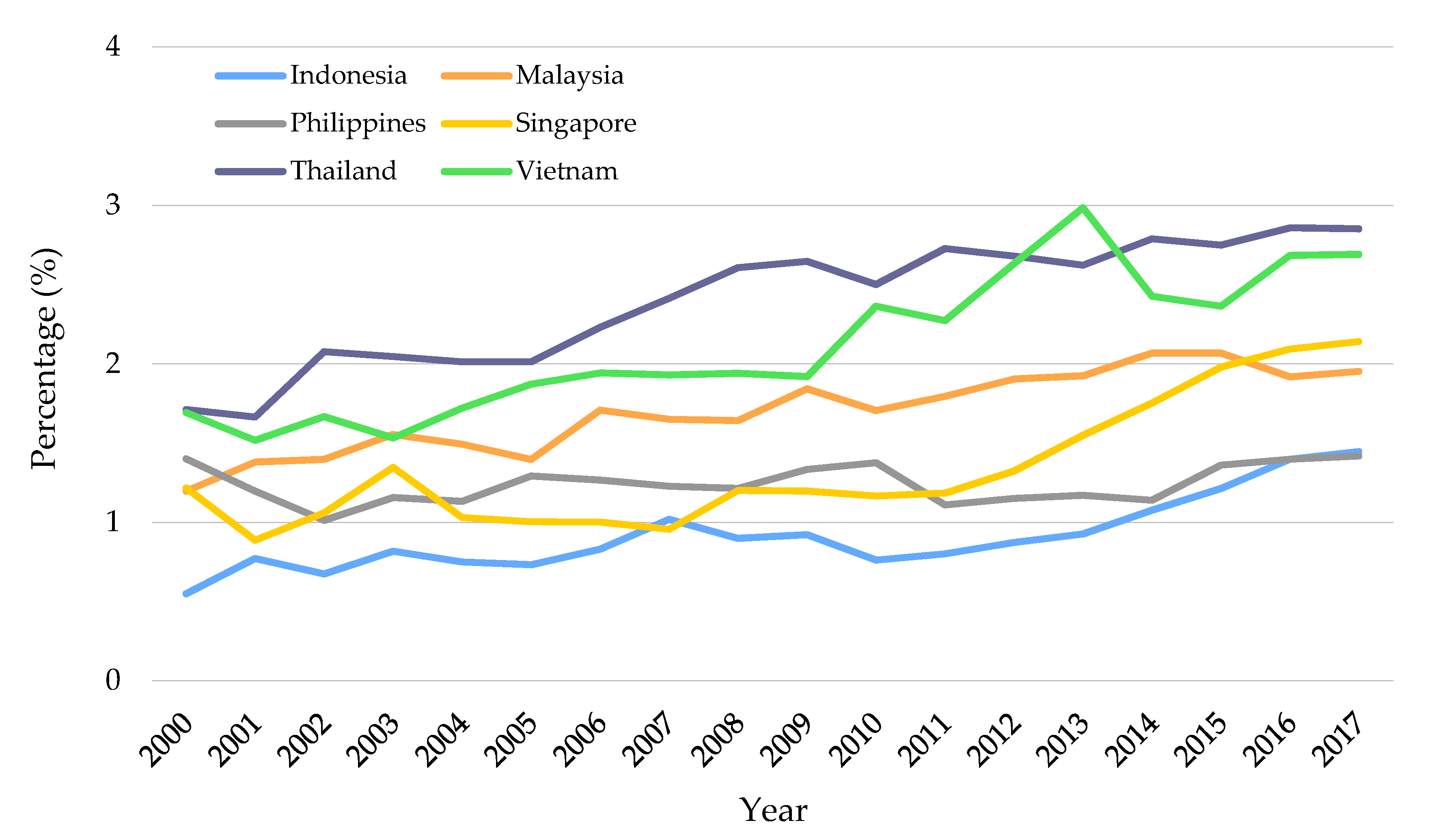
Despite the fact that Indonesia’s Gross National Income rose from USD 1390 in 2006 to USD 3650 in 2014, the government share of total routine immunization expenditures dropped from 95% to 64% during this period [23]. In addition, Indonesia health spending per capita has increased rapidly since 2010 [24]. Nevertheless, the relative value as a proportion of Gross Domestic Product (GDP) remains lower than the average of MICs and neighboring countries in Southeast Asia, such as Thailand (2.8%), Malaysia (1.9%), Singapore (2.1%), and Vietnam (2.7%) [25].
Figure 1 presents a comparison of healthcare spending in Southeast Asian countries in the period of 2000–2017. Comparing with other countries in this region, Indonesia’s health expenditure was reported to be relatively low, which might produce significant strain on the immunization system. The tight budget results in some obstacles to proper system financing and structuring, such as lack of funds to procure vaccines, unreliable vaccine availability, under-developed infrastructure (e.g., vaccine cold chain), and the possibility of subnational governments to use central government revenue for financing other health initiatives [8,19].
Figure 1.
Domestic general government health expenditure as the percentage of GDP [25].
To deal with the tight budget and its consequences, Indonesia has to restructure its immunization system. In this case, there are two alternative strategies that can be implemented in Indonesia. The first strategy is through province block grants. In order to meet the specific financial needs of each province, the central government would provide province block grants to each province based on a formula that estimates its needs. The allocation of these funds to different immunization-related activities, such as vaccine procurement and infrastructure, is at the province’s discretion. This grant would also require the province to meet their immunization objectives. The second strategy is through insurance mandate and subsidy. Establishing an insurance mandate would require Indonesia’s national social insurance plan and all private insurances to cover the costs of all vaccination fees for vulnerable populations—children and adults over the age of 65. The mandate would be geared, particularly, to cover vaccines that have high societal benefits, meaning the vaccine has the ability to prevent the spread of a highly contagious disease [6]. This mandate sanctions an obligation on the public and private healthcare system to ensure vaccines are available to all of its insured. The subsidy amount given would be determined by the societal benefits for new vaccines as well as current market price for established vaccines. With the provision of a subsidy, social and private insurances have a greater ability to procure and administer vaccines in order to increase immunization rates, while the central government plays the role of enforcer. The central government has the responsibility of reimbursing public and private insurance plans for the mandated vaccine costs and associated vaccine administration fees [6]. More detailed information about the pros and cons of the strategies to restructure the immunization system can be seen in Table 2.

Table 2.
Strategies to restructure the immunization system.
3. Financial Barriers in Indonesia: Considering the Potential of COVID-19 Vaccine
As a country with the highest fatal cases due to the novel coronavirus disease 2019 (COVID-19) in Southeast Asia, the health crisis has urged the government of Indonesia to mitigate the pandemic through several strategies, such as COVID-19 vaccination. Next to mitigating the pandemic, maintaining the performance of routine immunization program is also critical to prevent further outbreaks of VPDs. Taking the potential of a COVID-19 vaccine into account, there are several financial barriers that must be considered for financing new vaccines in Indonesia.
3.1. Regional Disparities and Geographical Barriers
The role of the subnational government in Indonesia became more important since the political transition from authoritarian regime into democratic and decentralization reforms in 1999 [26]. Although decentralization has successfully enhanced local government capacities to be more responsive to local needs, this transition also has increased the variation levels of development between regions due to heterogeneity of resources [24]. It should be noted that regional disparities have been widely known as the major problem and the determinant factor of health inequality in emerging countries [27]. A previous study reported that Indonesia had inequalities in health expenditure, access and quality of health services, and public health development index [28,29,30,31]. This situation might lead into inequalities in life expectancy. Indonesian life expectancy was reported to be 69.44 and 73.33 for males and females, respectively. Life expectancy of the population in Java (male: 70.79; female: 74.56) was reported to be higher than in non-Java islands (male: 67.42; female: 71.26) [32]. These disparities are essential to be addressed in improving Indonesia’s immunization system.
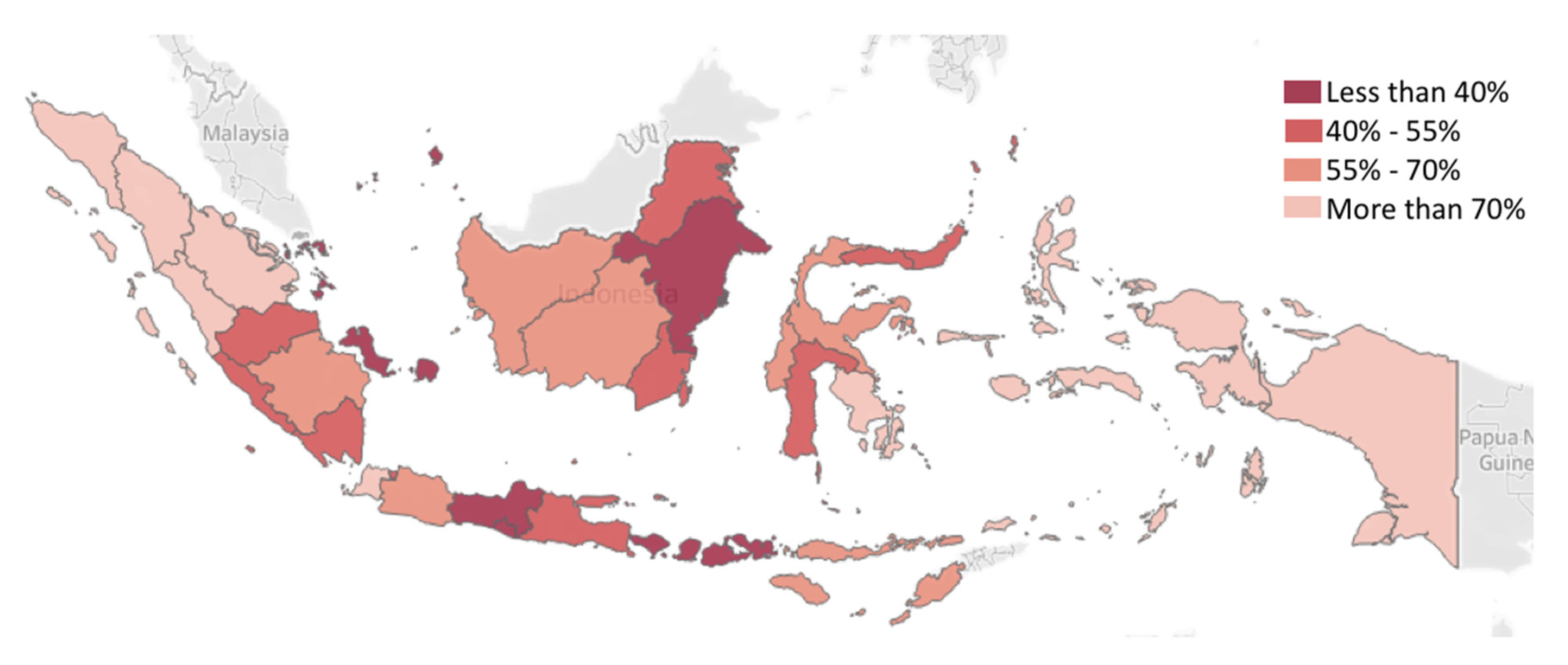
Figure 2 presents the regional differences in terms of basic immunization rates among children from poor households (i.e., below 40 percentile of welfare rate). On average, only 55.5% of children from the poorest households in Indonesia received complete basic immunization in 2018 [33]. Taking regional analysis into account, it can be seen that immunization rate differences are significant. For example, the poorest households in Java were reported to have better access to basic immunization than in other islands. The current pandemic will likely further enhance variability between regional and local priorities and economic differences. In these subnational variabilities, regional disparities and geographical barriers are critical factors for mitigating the pandemic.
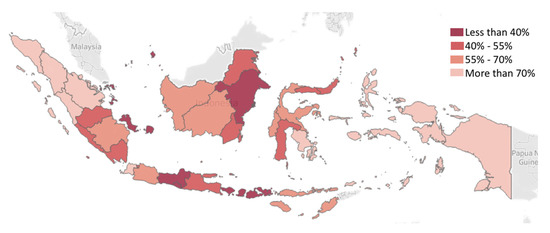
Figure 2.
Spatial map of the percentage of children (<2 years old) from the poorest households (lowest 40% of welfare rate) receiving complete basic immunization in Indonesia [33].
3.2. Lack of Infrastructure
As one of the most populous countries in the world with approximately 14,750 islands [34], ensuring access to immunization for all targeted population remains one of the biggest challenges. In particular, providing access to immunizations in remote regions has been problematic due to the high costs of transporting vaccines and other medical supplies to these regions. To deal with this problem, supporting infrastructures are required. For instance, the availability of vaccine cold chains, since a vaccine is a sensitive compound that must be properly stored at a specific temperature to maintain its viability. In the context of Indonesia, the availability and maintenance of cold chains in remote regions are critical factors to distribute vaccines across the country [19]. An important factor in maintaining cold chain products is the correct treatment in each of the main distribution points in the cold chain so that the right distribution channels will provide a good quality of cold chain products. The application of cold chains requires the provision of several facilities, both in the storage and distribution process. It has been highlighted that failure to provide good cold chains causes damage to almost 50% of vaccines worldwide every year [35]. Using the introduction of a COVID-19 vaccine as an opportunity to strengthen the infrastructure, cold chain procurement should be prioritized by the stakeholder to prevent changes and damages to chemical structure that can cause potential loss. Several factors should be considered in choosing the cold chain, such as the number of targets, the volume of vaccines to be loaded, the available energy sources, the nature of storage facilities (function and temperature stability), and the WHO’s recommendations.
3.3. Challenges in Vaccine Delivery
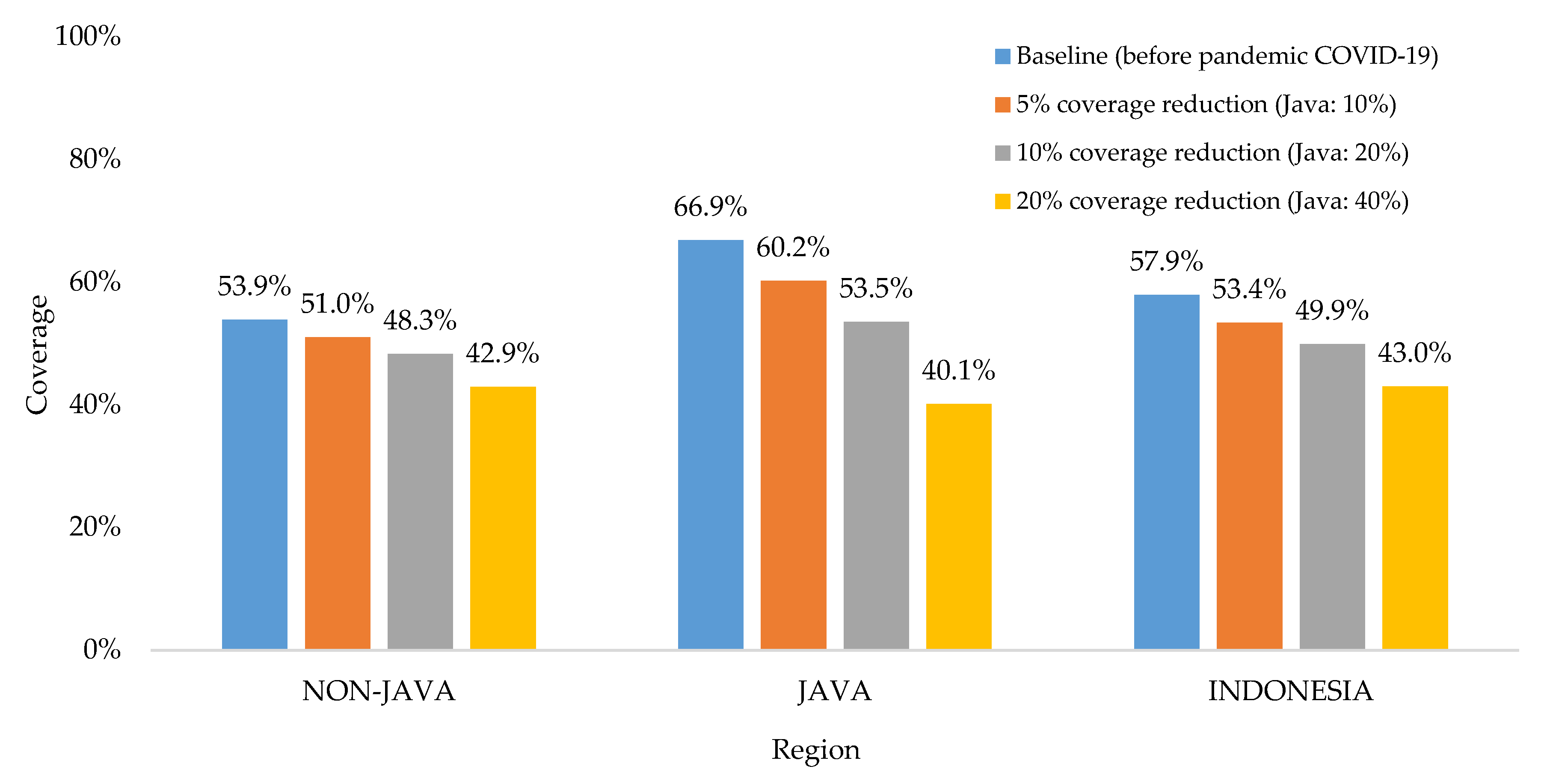
Basic childhood immunization coverage in Indonesia has fluctuated in the last decade, but currently appears to be declining [8]. The latest survey reported that the proportion of fully immunized children at the age of 12–23-months-old was only 58%, which was lower than the targeted coverage by the government at 93% [8]. Due to the impact of the COVID-19 pandemic, a recent study estimated the basic childhood immunization coverage would be 53%, 50%, and 43% for the respective scenarios of immunization coverage reductions at 5%, 10%, and 20% [36]. The study considered the impact of the pandemic in reducing immunization coverage would be doubled in all provinces of Java, since this island is the epicenter of the COVID-19 pandemic in Indonesia (see Figure 3).
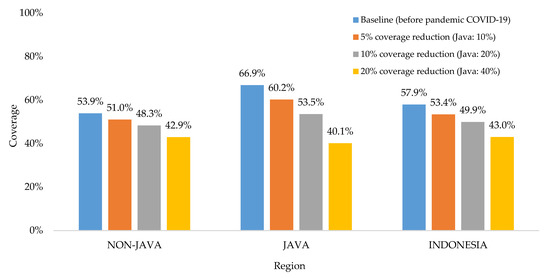
Figure 3.
The impact of the COVID-19 pandemic on basic childhood immunization coverage [36].
Reductions in immunization coverage were associated with school closures and parents’ concern on taking their children to healthcare facilities during the pandemic. To prevent disruptions to immunization services during the COVID-19 pandemic, the healthcare facilities must be adequately equipped to provide safe services for healthcare workers and communities. The disruption to immunization services due to the additional burden in the healthcare system might lead to a potential reduction in demand for vaccination by the community. This situation can increase the risk of outbreaks of VPDs. Hence, immunization services should be maintained whenever these can be conducted safely. Providing routine immunization services in a safe manner requires the program to be adequately resourced to ensure the safety of healthcare workers, minimize the transmission of virus in the community, and adapt the way immunization is delivered during the pandemic situation. Modifications to vaccine delivery can potentially increase the cost of conducting immunization services. To optimize service delivery and minimize the risks of virus transmission at the same time, WHO recommends countries to explore innovative methods for vaccine delivery by improving infection prevention and control (IPC) measures, training staff on IPC, supplying facilities with IPC equipment, screening at the entrance of the vaccination area, reducing the session size, and reducing waiting time [37]. For outreach and mobile services, WHO recommends countries to work together with communities to identify alternative outdoor sites that allow physical distancing [37].
4. Discussion
As one of the MICs, Indonesia is designated to explore internal co-financing of vaccines since financial assistance has been gradually phased out. With economic decline due to the COVID-19 pandemic and the country starting to transition to fully self-financing its immunization program, extra sources are required to replace about 10–15% of the externally financed share of the immunization program budget [38]. This causes immense tension within the healthcare system and an incredible strain on the immunization program. In the context of sustainable financing, this situation prompted the stakeholder to find an innovative way to finance the introduction of new vaccines, including a COVID-19 vaccine. Up to now, Indonesia has rather expressed strong interest in resource tracking and efficiency gains rather than a push for revenue generation, which would potentially endanger the financial sustainability of the immunization program in Indonesia. A realistic approach to expand fiscal space is needed through efficiency gains both in all public sectors and new innovative interventions for financing the implementation of routine immunization programs and the introduction of new vaccines. There is no single solution that tackles every obstacle and answers every element of this major issue, but using the framework of the solutions presented through increasing the national revenue and structuring the immunization system, a tailored plan to finance immunization can be developed.
It has been known that immunization is one of the most cost-effective interventions in global health and has a crucial role in achieving 14 of the 17 SDGs [38]. Sustainable financing for new vaccines closely reflects the ethos of the SDGs: leaving no one behind. Table 3 presents the impact of financing immunization on SDGs.

Table 3.
Impact of financing immunization on sustainable development goals (SDGs) [38].
As Indonesia works to develop a substantial way to finance new vaccines, other public health interventions to prevent infectious diseases can be employed or can eventually be used in cooperation with immunization to decrease costs. Education in communities on the following topics are essential to achieve SDGs through public health efforts. Several prevention interventions can be taken into account, such as exclusive breastfeeding, good hygiene, and water sanitation. Exclusive breastfeeding is when an infant receives only breast milk for their nutrition. No other sources of nutrition including water, other milks or juices, or solid foods are consumed during this time. WHO recommends that new mothers breastfeed their child for at least 6 months to ensure optimal growth and development [39]. This is essential because children are born with weak immune systems that must be fortified after birth. Breast milk from mothers provides a child with all the antibodies and nutrients critical for this period of life. Exclusive breastfeeding has been shown to protect children from common childhood diseases like diarrhea and pneumonia, which are responsible with approximately 25,000 and 8551 annual deaths in Indonesian children under 5 years old, respectively [40]. Therefore, exclusive breastfeeding practices could have a positive impact on morbidity and mortality from this disease until vaccines for diarrhea and pneumonia can be introduced in Indonesia. However, only 37% of children younger than six months are exclusively breastfed [41]. Thus, efforts must be made to educate parents around the world on the importance of exclusive breastfeeding and the duration for which it should be done. Research studies have shown that firstly, exclusive breastfeeding does in fact decrease risk of infectious diseases, but also signify that there is a correlation in length of time of exclusive breastfeeding and level of risk for respiratory and gastrointestinal infections. One study found that exclusive breastfeeding until 4 months of age followed by partial breastfeeding was associated with a significant reduction in respiratory and gastrointestinal infectious diseases, but breastfeeding until 6 months of age tended to be more protective [42]. There is extensive data supporting this notion, but children are still not being breastfed. Therefore, it is important that educational efforts and public health interventions are increased to inform parents on the importance of breastfeeding. This can be done through events in communities to educate and respond to parental concerns or requiring doctors to take the time to discuss the importance of breastfeeding with new mothers. If breastfeeding efforts are increased, this could relieve the large morbidity and mortality of VPDs, specifically in children under 5 years old.
In particular, good hygiene is similarly as important as exclusive breastfeeding in the fight against infectious diseases and in the efforts to achieve SDGs. Taking extra caution and increasing hand washing can decrease the spread of infectious diseases [17]. The Centers for Disease Control and Prevention (CDC) states that washing hands with clean water and soap is one of the most important methods for infectious disease prevention. Some recommendations include washing hands before preparation and consumption of food, after using the toilet, and after touching a pet or the garbage [43]. The education of people on the importance of good hygiene and hand washing is not necessarily an expensive intervention; therefore, it is a reasonable solution for Indonesia to encourage during this time of transition to a self-financing immunization system. However, the major concern here is the availability of clean water. The availability of clean water and appropriate septic systems and sanitation facilities has a significant impact on the spread of infectious diseases in Indonesia. About 27 million Indonesians lack clean and safe water and 51 million lack access to improved sanitation facilities [44]. UNICEF estimates that roughly, 1 in 8 Indonesian households do not have access to safe drinking water sources and in rural areas, access to piped water is still below 10 per cent [44]. Subsequently, less than 50% of people practice hand washing at critical times [44]. It has also been discovered that 88% of deaths due to diarrhea are linked to incomplete water, sanitation, and hygiene provision [44]. These statistics highlight the significance that water sanitation and appropriate sanitation facilities has in the spread of infectious diseases. International organizations (i.e., UNICEF, USAID, and water.org) have provided a bit of relief to the Indonesian government through their public health efforts to provide Indonesians with adequate water supplies. This aid will continue to be an important factor in the upcoming years. In combination with the other two practices mentioned above, these alternative prevention methods have the ability to decrease infectious diseases while Indonesia works on ways to better finance their immunization system.
In a five-year view, the Indonesian government should consider a number of costs and issues beyond the development and procurement of vaccines [13,14]. The costs of delivering vaccines to the remote parts of Indonesia, implementing the necessary infrastructure, and adequately staffing healthcare facilities for efficient vaccine delivery are also important in this time of transition [45]. These constraints must be addressed and mitigated in the new self-financing system [45]. Understandably, it will take some time to increase funds to resolve all the concerns involved in the maintenance of Indonesia’s immunization system and the introduction of new vaccines. Therefore, public health efforts must be increased to, in turn, decrease the burden of infectious disease as Indonesia develops a stronger immunization system. Increasing the dispersal of information on the importance of breastfeeding and good hygiene is paramount. Public health officials, medical providers, and news media outlets should work cohesively on educating Indonesians from Sabang (the most western point) to Merauke (the most eastern point). These focuses have the ability to make a major impact on the reduction of infectious diseases in Indonesia at a lower cost. Henceforth, increasing these public health efforts will be incredibly important in helping children in Indonesia live past the age of 5 while Indonesia works toward providing a sound, well-financed immunization system for its citizens.
5. Conclusions
As the most cost-effective medical intervention, vaccinations have the potential to strengthen the means of implementation for the SDGs. To ensure immunization systems can reach every targeted population with the vaccinations they deserve, sustainable financing for new vaccines is critical and the issue of financing is particularly pertinent as Indonesia transitions away from extensive Gavi support towards a self-financing immunization system. Therefore, substantial financing solutions and system structuring strategies are vital during this critical period. Despite the fact that economic evaluation studies are essential as an initial step to ensure financial readiness, the lack of reliable data is the first barrier to Indonesia’s journey toward a self-financing immunization system. To deal with this problem, standardization of data collection strategies and methodologies are required. An increase in quality data from economic evaluation studies will allow healthcare officials to better convince policy makers on the importance of providing ample revenue to the immunization budget. Next to economic evaluation studies, Indonesia may have to explore other options to increase revenue for its immunization system. There are three strategies from several published studies that may be valuable and practical to be implemented, such as through general revenue from the central government, a sector-wide approach to financing, and a national trust fund. To deal with the tight budget and its consequences, Indonesia has to restructure its immunization system. Learning from the experience of other countries, there are two alternative strategies that can be implemented in Indonesia, such as through province block grants, insurance mandate and subsidy. Furthermore, taking the potential of a COVID-19 vaccine into account, the Indonesian government should consider a number of costs and issues beyond the development and procurement of vaccines. The costs of delivering vaccines to the remote parts of Indonesia, implementing the necessary infrastructure, and modifying vaccine delivery are also important in this time of transition. These constraints must be addressed in the new self-financing system and other public health efforts must be increased to decrease the burden of infectious disease as Indonesia develops a stronger immunization system.
Author Contributions
Conceptualization, D.B. and R.A.; methodology, F.F. and A.A.S.; software, A.S.W.K.; validation, F.F. and M.Y.P.; formal analysis, F.F. and A.A.S.; investigation, F.F. and A.D.; resources, R.A. and A.S.W.K.; writing—original draft preparation, F.F. and M.Y.P.; writing—review and editing, R.A. and A.A.S.; supervision, D.B. and A.D.; project administration, A.S.W.K.; All authors have read and agreed to the published version of the manuscript.
Funding
This research was partially funded by the Indonesian Ministry of Research and Technology/National Agency for Research and Innovation, and Indonesia Ministry of Education and Culture, under World Class University Program managed by Institut Teknologi Bandung for R.A.
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO. Vaccines and Immunization. Available online: https://www.who.int/health-topics/vaccines-and-immunization#tab=tab_1 (accessed on 30 March 2020).
- Prüss-Üstün, A.; Corvalán, C. Preventing Disease through Healthy Environments: Towards an Estimate of the Environmental Burden of Disease; WHO: Geneva, Switzerland, 2006; pp. 65–70. [Google Scholar]
- WHO. Immunization, Vaccines, and Biologicals: The Middle-Income Country Strategy. Available online: http://www.who.int/immunization/programmes_systems/sustainability/mic_strategy/en/ (accessed on 24 December 2019).
- WHO. WHO’s Vision and Mission in Immunization and Vaccines 2015–2030. Available online: http://www.who.int/immunization/documents/general/WHO_Mission_VIsion_Immunization_Vaccines_2015_2030.pdf?ua=1 (accessed on 15 August 2019).
- WHO. Global Vaccine Action Plan 2011–2020. Available online: http://www.who.int/immunization/global_vaccine_action_plan/GVAP_doc_2011_2020/en/ (accessed on 19 August 2019).
- Committee on the Evaluation of Vaccine Purchase Financing in the United States and Board on Health Care Services. Financing Vaccines in the 21st Century: Assuring Access and Availability; The National Academies Press: Washington, DC, USA, 2004. [Google Scholar]
- WHO. Vaccine Market. Available online: http://www.who.int/immunization/programmes_systems/procurement/market/individual_vaccine/en/ (accessed on 30 March 2020).
- Immunization Financing. Indonesia: The Challenge of Protecting Immunization in the Transition to Universal Health Coverage. Available online: https://www.immunizationfinancing.org/en/country-case-studies/indonesia-the-challenge-of-protecting-immunization-in-the-transition-to-universal-health-coverage# (accessed on 30 March 2020).
- Gavi. Indonesia. Available online: https://www.gavi.org/programmes-impact/country-hub/south-east-asia/indonesia (accessed on 1 October 2020).
- WHO. Expanded Programme on Immunization of the Department of Immunization of the Department of Immunization, Vaccines and Biologicals, Vaccine Introduction Guidelines: Adding a Vaccine to a National Immunization Programme, Decision and Implementation; WHO: Geneva, Swizterland, 2005. [Google Scholar]
- DeRoeck, D.; Wang, A. Principles and Considerations for Adding a Vaccine to a National Immunization Programme: From Decision to Implementation and Monitoring; WHO: Geneva, Swizterland, 2014. [Google Scholar]
- Suwantika, A.A.; Postma, M.J. Effect of breastfeeding promotion interventions on cost-effectiveness of rotavirus immunization in Indonesia. BMC Public Health 2013, 13, 1106. [Google Scholar] [CrossRef] [PubMed]
- Suwantika, A.A.; Zakiyah, N.; Lestari, K.; Postma, M.J. Accelerating the introduction of rotavirus immunization in Indonesia. Expert Rev. Vaccines 2014, 13, 463–472. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Suwantika, A.A.; Zakiyah, N.; Kusuma, A.S.W.; Abdulah, R.; Postma, M.J. Impact of switch options on the economics of pneumococcal conjugate vaccine (PCV) introduction in Indonesia. Vaccines 2020, 8, 233. [Google Scholar] [CrossRef] [PubMed]
- Supadmi, W.; Suwantika, A.A.; Perwitasari, D.A.; Abdulah, R. Economic Evaluations of Dengue Vaccination in the Southeast Asia Region: Evidence from a Systematic Review. Value Health Reg. Issues 2019, 18, 132–144. [Google Scholar] [CrossRef] [PubMed]
- Suwantika, A.A.; Kautsar, A.P.; Supadmi, W.; Zakiyah, N.; Abdulah, R.; Ali, M.; Postma, M.J. Cost-effectiveness of dengue vaccination in Indonesia: Considering integrated programs with wolbachia-infected mosquitos and health education. Int. J. Environ. Res. Public Health 2020, 17, 4217. [Google Scholar] [CrossRef] [PubMed]
- Suwantika, A.A.; Beutels, P.; Postma, M.J. Cost-effectiveness of hepatitis a vaccination in Indonesia. Hum. Vaccines Immunother. 2014, 10, 2342–2349. [Google Scholar] [CrossRef]
- WHO. South-East Asia Regional Vaccine Action Plan 2016–2020. Available online: http://www.searo.who.int/indonesia/topics/immunization/south_east_asia_regional_vaccine_action_plan_2016_2020.pdf (accessed on 10 March 2020).
- Milken Institute. New Models for Financing Vaccination Programs in Southeast Asia. Available online: https://assets1c.milkeninstitute.org/assets/Publication/InnovationLab/PDF/VaxPrgrmsSEAsia4WEB.pdf (accessed on 10 March 2020).
- Results for Development. Immunizing Financing Options: A Resource Guide for Advocates, Policymakers, and Program Managers. Available online: https://www.gavi.org/sites/default/files/document/support/Immunization%20financing%20resource%20guide.pdf (accessed on 10 February 2020).
- Garner, P.; Flores, W.; Tang, S. Sector-wide approaches in developing countries: The aid given must make the most impact. BMJ 2000, 321, 129–130. [Google Scholar] [CrossRef]
- Immunization Financing. Bhutan: A National Trust Fund for Immunization. Available online: https://www.immunizationfinancing.org/en/country-case-studies/bhutan-a-national-trust-fund-for-immunization# (accessed on 10 February 2020).
- Sabin Vaccine Institute. Indonesia. Available online: https://www.sabin.org/programs/sustainable-immunization-financing/indonesia (accessed on 11 July 2020).
- WHO. State of Health Inequality: Indonesia; WHO: Geneva, Swizterland, 2017. [Google Scholar]
- World Bank. World Development Indicators. Available online: https://data.worldbank.org/indicator/SH.XPD.GHED.GD.ZS (accessed on 11 July 2020).
- Fang, P.; Dong, S.; Xiao, J.; Liu, C.; Feng, X.; Wang, Y. Regional inequality in health and its determinants: Evidence from China. Health Policy 2010, 94, 14–25. [Google Scholar] [CrossRef]
- Holzhacker, R.L.; Wittek, R.; Woltjer, J. (Eds.) Decentralization and Governance in Indonesia; Springer International Publishing: Cham, Swizterland, 2016. [Google Scholar]
- Heywood, P.; Harahap, N.P. Public funding of health at the district level in Indonesia after decentralization—Sources, flows and contradictions. Health Res. Policy Syst. 2009, 7, 5. [Google Scholar] [CrossRef]
- Sparrow, R.; Budiyati, S.; Yumna, A.; Warda, N.; Suryahadi, A.; Bedi, A.S. Sub-national health care financing reforms in Indonesia. Health Policy Plan. 2017, 32, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Hodge, A.; Firth, S.; Jimenez-Soto, E.; Trisnantoro, L. Linkages between decentralisation and inequalities in neonatal health: Evidence from Indonesia. J. Dev. Stud. 2015, 51, 1634–1652. [Google Scholar] [CrossRef]
- Suparmi; Kusumawardani, N.; Nambiar, D.; Trihono; Hosseinpoor, A.R. Subnational regional inequality in the public health development index in Indonesia. Glob. Health Action 2018, 11 (Suppl. 1), 1500133. [Google Scholar] [CrossRef] [PubMed]
- Statistics Indonesia. Life Expectancy. Available online: https://www.bps.go.id/linkTableDinamis/view/id/1114 (accessed on 1 October 2020).
- Statistics Indonesia. Percentage of Children 12–23 Months Who Received Complete Basic Immunization with the Lowest 40% Welfare Rate, by Province. Available online: https://www.bps.go.id/dynamictable/2019/10/04%2010:20:19.764125/1658/persentase-anak-umur-12-23-bulan-yang-menerima-imunisasi-dasar-lengkap-dengan-tingkat-kesejahteraan-40-terendah-menurut-provinsi-2015–2018.html (accessed on 25 August 2020).
- World Atlas. World Facts. Available online: https://www.worldatlas.com/articles/how-many-islands-does-indonesia-have.html (accessed on 19 February 2020).
- WHO. Cold Chain, Vaccines and Safe-Injection Equipment Management. Available online: https://www.who.int/immunization/documents/MLM_module1.pdf?ua=1 (accessed on 1 October 2020).
- Suwantika, A.A.; Boersma, C.; Postma, M.J. The potential impact of COVID-19 pandemic on the immunization performance in Indonesia. Expert Rev. Vaccines 2020, 19, 687–690. [Google Scholar] [PubMed]
- WHO. Framework for Decision-Making: Implementation of Mass Vaccination Campaigns in the Context of COVID-19. Available online: https://apps.who.int/iris/bitstream/handle/10665/332159/WHO-2019-nCoV-Framework_Mass_Vaccination-2020.1-eng.pdf?sequence=1&isAllowed=y (accessed on 1 October 2020).
- Gavi. Sustainable Development Goals. Available online: https://www.gavi.org/our-alliance/global-health-development/sustainable-development-goals (accessed on 1 October 2020).
- WHO. Exclusive Breastfeeding for Optimal Growth, Development and Health of Infants. Available online: http://www.who.int/elena/titles/exclusive_breastfeeding/en/ (accessed on 1 March 2020).
- WHO. Monitoring Progress in Averting Pneumonia and Diarrhoea Deaths. Available online: https://www.who.int/test/others/gappd/# (accessed on 1 October 2020).
- NCD Alliance. Breastfeeding—Transforming Global Health One Baby at a Time. Available online: https://ncdalliance.org/news-events/blog/breastfeeding-transforming-global-health-one-baby-at-a-time (accessed on 30 July 2020).
- Duijts, L.; Jaddoe, V.W.V.; Hofman, A.; Moll, H.A. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics 2010, 126, e18–e25. [Google Scholar] [CrossRef] [PubMed]
- CDC. Water, Sanitation & Environmentally-Related Hygiene. Available online: https://www.cdc.gov/healthywater/hygiene/ldc/index.html (accessed on 24 June 2020).
- Unicef Indonesia. Water and Sanitation: Challenges. Available online: https://www.unicef.org/indonesia/wes.html (accessed on 24 June 2020).
- Unicef. Immunization Financing in MENA Middle Income Countries. Available online: https://www.unicef.org/mena/sites/unicef.org.mena/files/2018-04/immunization%20financing%20Web_0.pdf (accessed on 24 June 2020).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).