1. Introduction
The transformative impact of new technologies on the health system has become increasingly concrete in recent decades. Technological devices connect the patient and healthcare professionals, even remotely. Using these devices allows the development of a health system model based on “connected care” paths which assume the idea of a “connected” health ecosystem based on the centrality of people [
1]. Continuous technology improvement allows users to release feedback that has an immediate impact on system design. In this way, quality data are obtained that can support healthcare professionals in defining more accurate and effective diagnosis.
The close connection between the use of technology, the enhancement of the actor and the creation of new value is also central in the service theories, particularly in the service-dominant logic (S-D logic) [
2,
3], and service science, management, engineering, and design (Service Science or SSMED) [
4,
5]. Based on a systems view, S-D logic defines businesses as networks of relationships [
2], in which value is collaboratively created as a result of interaction between consumers and providers. In this theory, the importance of a social dimension and a multi-stakeholder vision is highlighted [
3]. SSMED focuses on the role of technology, especially Information and Communication Technologies (ICT), considered the main levers that enhance resource integration and value co-creation [
4].
The developments of the two theories lead to the formulation of the concept of “service ecosystem”, intended as an organizational layout to foster a complex set of actors to exchange resources through ICT mediated interactions based on pre-existing social norms (institutions) and finally producing value co-creation.
Despite the rapid technological processes in the medical field, the level of use of Digital Health or electronic health (eHealth) technologies is still limited [
6]. The main obstacle to the adoption of these technologies is the area of use, characterized by a complex multi-stakeholder environment, with a multi-fragmented decision-making process, with different needs and requirements to be satisfied, for different segments and classes of users [
7].
A possible solution is to approach digital health through the lens of service theories, which adopt a holistic view to the service management and identify the “service ecosystem” as the most appropriate organizational model to support the emergence of value.
Therefore, this paper aims to re-read the eHealth sector as a service ecosystem, within which the main elements are explored and identified, in order to map the elements necessary for the formation of new value. This approach allows us to create a theoretical framework that identifies the main elements of the service ecosystems (actors, technology, institutions, resources integration), whose integration leads to value co-creation and innovation in the short term, and sustainable value co-creation in long term. The model is tested through a case study represented by digital healthcare in the Autonomous Province of Trento, which represents a best practice in this sector.
The proposed model is characterized by a reticular configuration, within which the development of collaborative logics, resulting from continuous processes of cooperation between patient networks and service provider networks, allows to multiply moments of value creation. Synergistic interactions between players are facilitated by the constant search for user engagement, which represent fundamental partners in the production and improvement of the service and in the value co-creation process.
2. Theoretical Background
2.1. Service-Dominant Logic and Service Science: Two Service-Oriented Theories
2.1.1. Service-Dominant Logic
Service-dominant logic [
2,
8,
9] is one of the most relevant services theories that, based on network theory assumption, conceptualizes markets as networks of co-creating actors [
10,
11].
S-D logic [
2,
8,
12] reinterprets theoretically: (1) the notions of value, (2) the relationship between customer and provider, (3) the concept of service. In contrast with other theoretical frameworks, S-D logic states that value is no longer created exclusively by firms [
13]. Value is co-created collaboratively by each stakeholder, intended as active participants. In this view, customers are active participants in a co-creation process which stems from the experience and knowledge exchanged through the mutual efforts of each stakeholder [
2,
8,
14,
15]. In line with this idea, the service is intended as a process in which two or more entities exchange resources [
2] and in which users can apply their competencies, producing mutual benefits for all the actors [
8].
In summary, the key concept of this theory is value co-creation that is the joint production of value among all the actors engaged in service provision. It also represents the result of transformations occurring in contemporary markets, which involve actors and relationship among actors [
8,
14,
16].
2.1.2. Service Science
While S-D logic constitutes a theoretical basis of cultural and philosophical matrix for the analysis of services, service science represents a practical application of the S-D logic [
5]. SSMED is a multidisciplinary theory that studies the implications of adopting new management approaches to services [
17]. The founders of SSMED considered the service as a system of interacting and interdependent parts that includes people, technologies, and organizations [
4]. The purpose of the theory is to practically address the question of the most suitable organizational model to support the emergence of value. For this reason, it proposes a unitary framework for the study of the design, provision and evaluation of services. It is the “service system”, a dynamic value co-creation configuration of people, technology, organizations, and shared information [
4,
18].
The theory focuses on the active role of the players involved in the service system (customers are not merely participants but active actors in the service production process) and on the knowledge shared (shared information) through the main role of the technologies. Knowledge and technology are essential factors to accomplish value co-creation.
2.2. From Service System to Service Ecosystem
Broadening the concept of service systems [
5], the founders of S-D logic proposed the concept of the “service ecosystem” [
3,
12,
19,
20]. Vargo and Lusch [
9] (p. 176) defined the service ecosystem as a “relatively self-contained, self-adjusting system of resource-integrating actors connected by shared institutional logics and mutual value creation through service exchange”. The self-regeneration of the systems is an indispensable process for reconfiguring and remodelling the service over time, contrasting the scenario changes. This process can only take place through learning, or rather co-learning, which helps users to overcome environmental turbulences, enrich provider skills, anticipate market demands, react proactively, and survive any changes. Knowledge sharing brings advantages in terms of effectiveness and efficiency of the service; in fact, it allows access to resources owned by other actors and an understanding of how to best integrate these resources [
3]. This generates a “win-win” logic in which the enrichment of each participant is exactly balanced with that of the others.
2.3. The Dimensions of Service Ecosystem
Although the service ecosystems have been studied in different sectors [
21,
22] in the literature, there is no agreement on its main dimensions.
In the first conceptualizations of service ecosystems, Vargo and Lusch [
9,
12] emphasized the importance of social norms and common symbols as prerequisites for collaboration and the creation of innovation. In these studies, there is a pre-eminence of the social dimension, based on the key roles of institutions, including social rules, guidelines in terms of law, values, symbolic meaning and language [
12].
Over time, a series of studies on service ecosystem emphasized the centrality of technological feature [
23,
24]. In this view, technology and ICT are considered as key levers of value co-creation [
25]. In fact, since they are involved in all the phases of service delivery, technology and ICT can be considered bridge elements, creating connections with and between the other elements of ecosystems. Recent studies proposed the existence of a bidirectional relationship between technology and institutions, both considered as levers for fostering value co-creation [
26].
Finally, in service ecosystems, the human component is also extremely relevant [
27]. Not only customers and providers, but each actor is actively involved in service-for-service exchange as part of a network in a multi-stakeholder vision. In this view, each actor can be a resource integrator then a potential co-creator. The term consumer-supplier is overcome in favor of the actor-to-actor (A2A) view.
Matching the main dimensions taken in consideration from the main scholars of service ecosystems, Polese et al. [
28] summarized the main elements of service ecosystem as: (1) actors, (2) technology, (3) institutions, (4) resource integration.
- (1)
Actors are all the stakeholders involved in the service exchange of services. They are “resource integrators” in an A2A reticular approach [
3] in which everyone can share resources to obtain mutual benefits for each.
- (2)
Technology is one of the main dimensions of service ecosystems [
3,
21,
29,
30,
31] because it accelerates the passage of shared information and allows the creation of new institutions [
32].
- (3)
Institutions are social rules, norms, shared practices regulating exchanges and acting as prerequisites for resource integration.
- (4)
Resource integration occurs during actor interactions. It allows for the co-learning of the actors which can turn into value co-creation. The resources are divided into: operand, represented by the usually tangible and static natural or economic resources that require manipulations to take on values, and operant, i.e., human knowledge and skills, cultural or social resources, usually intangible and dynamic, which have the task of acting on operands and other operants to create value.
2.4. The Sustainable Value Co-Creation in Service Ecosystem
The four elements of the service ecosystem represent the drivers of value co-creation (at a potential level). Only their integration, allowing the actors to exchange resources through technology and following common rules, allows the value co-creation process to activate (dynamic level).
In the single service exchange, value co-creation is intended as a joint value for all the actors of the transition (all the actors of the transition create and receive value).
The sum of the value obtained in every single transition from the actors’ resources exchange (value co-creation), such as consumer feedback, generate new elements (innovation), which allow managers to improve the entire service.
From value co-creation, innovation can be generated when [
33,
34]: the integration of the resources exchanged between the actors creates new resources (new knowledge, new experiences); the strategic use of technology creates new ways of interacting; the sharing of the same goal and the same rules creates new practices and new institutions (new habits).
If the novelty elements, caused by the interaction of the supplier network and the customer network, generate product (or service) improvement or redesign, sustainable value co-creation is obtained [
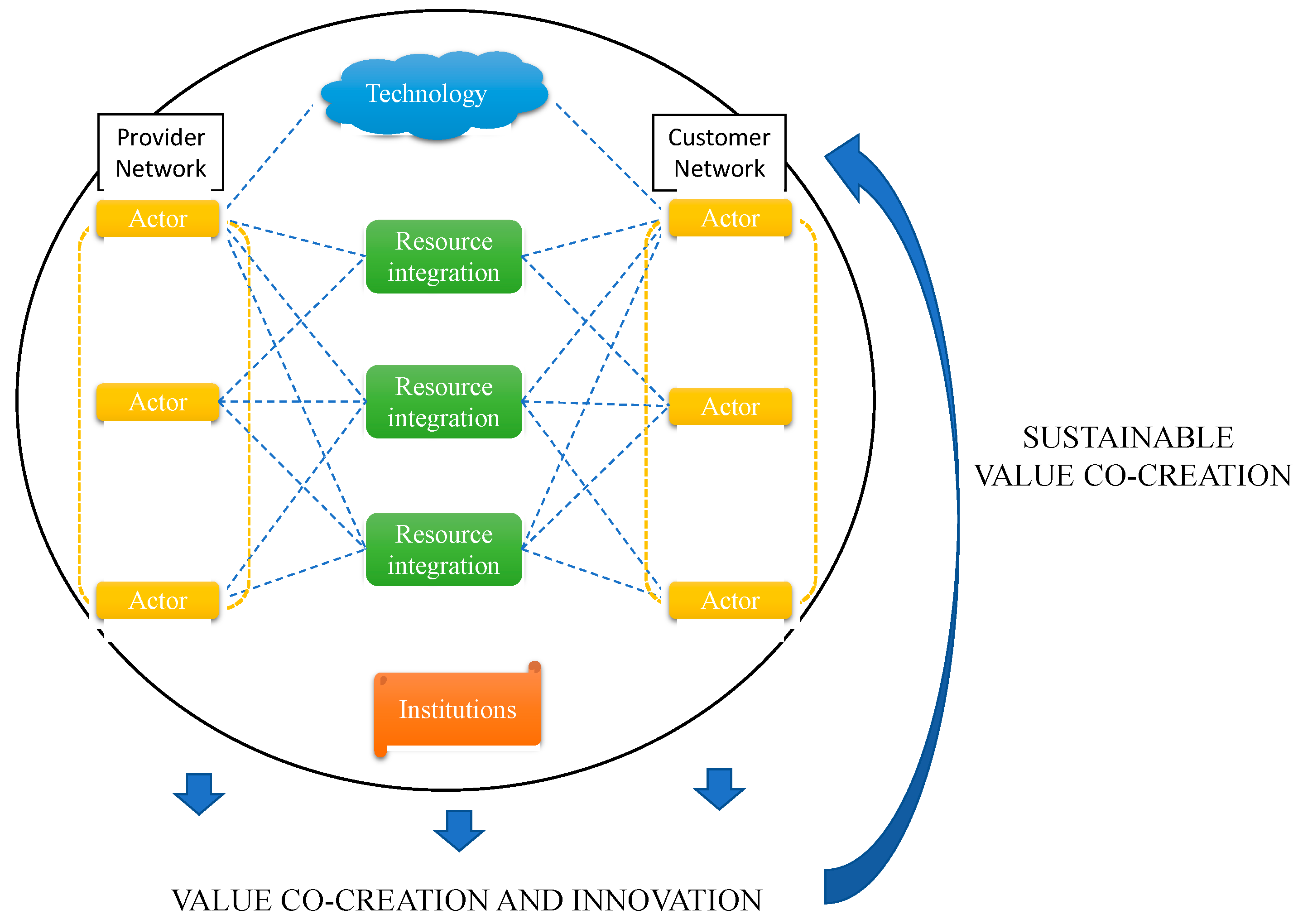
35]. This process is graphically described in
Figure 1.
The relationship between value co-creation, innovation and sustainability, maintained over time, brings advantages in terms of [
28]: (1) economic advantage; (2) social well-being; (3) environmental benefit.
In this vision, sustainable value co-creation is intended as creation in the long run of new solutions set up with and for end-users to guarantee a better service for the whole society. In this sense, the concept of sustainable value co-creation implies the desire for social well-being and therefore is a concept close to the notion of social innovation.
3. Digital Health: New Digital Technologies to Support Healthcare
Digitalization is considered one of the most important instruments to develop health care systems. The use of modern technologies produces many advantages for the healthcare sector [
36,
37]. One of the most advantages is the collection and processing of large quantities of data from health information systems [
38,
39], from medical devices, from patients/family members and from external applications (internet of things, social platforms, telemedicine). The ability to acquire a lot of data in a real context allows a greater probability of drawing up accurate diagnoses, a greater probability of opting for effective treatments and, more generally, an increase in the overall capacity of health systems to provide good assistance [
40]. In sum, it favours the effectiveness and efficiency of drug therapies [
41,
42].
However, digitization in the healthcare sector also entails many disadvantages. The main obstacle to the adoption of these technologies is the clinical environment, characterized by a complex multi-stakeholder environment, with a multi-fragmented decision-making process, with different needs and requirements to be met for different segments and classes of users [
7]. Users can be [
7]:
The government and regulatory authorities, which approve and deliberate the use of these solutions;
Healthcare professionals, who must select the solution and buy it;
Doctors and healthcare personnel, who evaluate and choose the solution;
Patients, caregivers and community associations, who influence and determine the success or otherwise of the use of these solutions;
Technology providers and medical device suppliers, who market and distribute the solution.
Another obstacle is the limited digitization of health information systems in relation to the rapid evolution of technologies applied to the domain of health.
Further limits concern data security and privacy. Digital solutions are often based on data coming from databases created for other purposes. This generates problems in terms of [
43]: (1) the guarantee of the data source; (2) the correct “representation” of an entire population; (3) the quality of the algorithms; (4) the validity and correct use of data.
Digital health technologies introduce problems for the respect of privacy in the sharing and transmission of patient data. Patients think that some personal information is not known by those who are not authorized. However, this is not always true. The growing availability and exchange of health information supports advances in individual care and public health, but also facilitates invasive marketing practices and discrimination outside the law.
The effectiveness of medical services is obtained by overcoming old paradigms that relegated the patient to a position of absolute dependence on the knowledge of the doctor. Over the past few decades, and with the application of digital technologies, the health system appears to be an increasingly complex, fluid, multi-faceted, multi-stakeholder environment, in which the patient has an increasingly active and central role. For this reason, the desirable healthcare system model is based on “connected care” paths which presuppose the idea of a “connected” healthcare ecosystem governed by the principle of the centrality of the person (patient-centred) [
44]. In this ecosystem, telemedicine, the use of wearable devices and monitoring apps allow the patient to be in control of their daily care, increasing the patient’s ability to think critically and make autonomous and informed decisions (patient empowerment).
Today, the recent developments in technology allow users to release real-time feedback on the provision of the service, promoting the collection of unlimited quality data (big data). User feedback becomes an indispensable source of knowledge for improving the health system. In this scenario, the patient-user is increasingly oriented towards sharing lifestyle data with the doctor. The active participation of patients involves a mutual exchange of resources and knowledge between doctors and users, triggering co-learning, which involves the sharing of resources and feedback [
45,
46,
47]. The exchange of mutual knowledge and the wise use of such knowledge translates into value acquired by both actors of the healthcare system, which can allow for sustainable value co-creation [
48,
49].
On the basis of the considerations made, the following research questions arise:
RQ1: which elements make up a service ecosystem in the eHealth sector?
RQ2: does the integration of such elements lead to the sustainable value co-creation in the eHealth ecosystem?
To answer these RQs, we investigate the case of the Trentino digital health system, re-reading it as a service ecosystem.
4. Research Methodology
The research adopts a qualitative approach, based on the case study methodology [
50,
51]. We chose this methodology as it serves exploratory, descriptive and explanatory purposes [
52]. However, case study research is more than a first exploratory step [
53]—“the richness and contextualization of a case study are a source of theoretical insight” [
54,
55]. In this research, in line with the approach proposed by Yin [
52], we formulate theoretical proposals before engaging in data collection and analysis. So, the mode of using theory is theory testing, in which case study analysis is mainly driven by theoretical deduction.
The case study aims to take into account as much as possible the complexity of the concrete situation in which events occur. Since in a situation to be analyzed there are many factors that can be considered, the case study aims to conduct research according to a holistic approach [
56,
57,
58]. Therefore, this methodology is suitable for examining the dynamics underlying a complex context such as the digital health system, in which a multiplicity of stakeholders is involved. Indeed, in health services, well-being can only be achieved through joint agreements between health professionals and patients. For this reason and because of its progressive development, the eHealth sector is chosen as a case study in this work. Specifically, we chose a representative case, as it is an Italian digital health best practice: the case of digital healthcare in Trentino.
Data collection was carried out using different sources so that the validity of the statements produced by the research was confirmed through data triangulation processes [
59]. We used multiple data sources: secondary and primary data.
Secondary data that yielded insights into the sustainable value co-creation were collected through online (reports, websites, app description) and official documentation. Official websites of the main players of eHealth in Trentino (Trentino Salute 4.0 website—trentinosalutedigitale.com, Autonomous Province of Trento website—provincia.tn.it, the Provincial Health Services website—apss.tn.it, TreC platform—trec.trentinosalute.net, Bruno Kessler Foundation website - fbk.eu) were checked in detail, as were relevant news and press releases on, for example, new projects and the expected benefits. The researchers were allowed to attend and document meetings and seminars relevant to the present study.
Primary data were collected through the semi-structured interview technique, based on the administration of some predefined topics to key informants. In our case, they correspond to public employees, operating in the governance of health services in Italy. In line with this methodology, the subjects of the sample are selected on the basis of their direct experience and knowledge of the phenomenon studied. Therefore, we chose purposive sampling, preferred over random sampling [
52]. Each actor was considered a peculiar individual, influenced by the context in which he lives; for this reason, the previous experiences, knowledge, attitudes of the interviewees should be preserved by the researchers in the transcription of the interviews [
60,
61,
62].
In line with the main research objectives, the interview was structured with the main macro-areas to be discussed during the interviews. In particular, in this research, the objective of the interviews is to investigate the digital health ecosystem, trying to demonstrate the ways in which the integration of the actors, technology, institutions and resource integration can lead to the co-creation of value.
Since this study can be considered as a pilot case study, we administered one interview to a public employee, who has an executive role in a virtuous health administration: Provincial Company for Healthcare Services.
The interview was conducted in March 2020 and lasted about 30 min; it was recorded, transcribed and analyzed on the basis of the main hypotheses deriving from the theoretical background and from the research questions. We called for having transcripts and drafts reviewed by key informants and three peers—a methodologist and two value co-creation experts [
63]. In addition, authors called for having the collaboration of two researchers to analyze the results separately and only subsequently did they collaborate and triangulate their observations [
58]. Different types of triangulation contribute to the increased robustness of the findings and construct validity [
58,
63]. Piekkari and Welch [
53] contended that different types of triangulation contribute to a better understanding of the different ways in which cases are seen and interpreted.
Since our research aims at the in-depth understanding of the sustainable value co-creation, we found it useful to iterate data/observations and analyses/interpretations [
53,
58]. To keep track and organize all these data/observations along with preliminary analyses/interpretations, researchers used a digitized case study database [
52]. It allowed us to increase the reliability of the study [
63].
5. Results
5.1. The Case of Digital Healthcare in Trentino
The Autonomous Province of Trento represents a best practice of Italian digital health. It plays the role of a pioneer for the intelligent implementation of health apps and technologies, useful for improving citizens’ lives.
The city is working to implement an integrated digital health management model to cope with changes linked to demographic evolution and new health needs of the population. Over the years, in fact, life expectancy has increased, and also chronic diseases have increased in the elderly.
To cope with social and demographic changes, Trentino has adapted its health policies. From an organizational and structural point of view, the network of services has been redesigned for a digital transformation. New technologies represent a useful opportunity to review the processes and treatment paths, experiment with new clinical and organizational models and redesign the infrastructure of services.
For this reason, the “TrentinoSalute4.0” was set up. It is the competence centre on digital health and represents the heart of all information technology activities applied to healthcare. TrentinoSalute4.0 has the objective of creating a shared space and a joint laboratory in the Trentino area, capable of supporting the development of digital healthcare in the Autonomous Province of Trento, through a system approach. The innovation policies of Trentino Health Service led to the development of various digital tools and products that facilitate access to health services and care for Trentino citizens; i.e., the digital medical prescription has replaced the paper recipe, giving way to the “dematerialization” of pharmaceutical prescriptions.
The most significant innovation is represented by a digital health services platform (the so-called TreC) consisting of an ecosystem of web and mobile applications through which, on the one hand, citizens can find support for the management of their health and communicating with healthcare professionals and, on the other, healthcare professionals can activate “customized” remote monitoring models for their patients.
The TreC platform has several functions:
- -
to allow access to the Electronic Health Record, enabling citizens to consult their health documentation produced by the Provincial Health Service structures (e.g., reports, laboratory tests, discharge letters, health and pharmaceutical prescriptions);
- -
to book and pay for visits and change their doctor;
- -
to offer the possibility of having a real health diary where citizens can keep track of their personal and family clinical history (e.g., drugs, therapies, allergies, intolerances, vaccinations, etc.);
- -
to record personal observations about health (e.g., weight, pressure, lifestyles);
- -
to use the services also through the smartphone thanks to a mobile app (App Trec_FSE).
A faster and complementary solution to the TreC platform is another digital service (FastTreC) which allows users to view laboratory reports, book blood samples and check vaccination status for children under 16 years of age.
Furthermore, especially for home-assisted chronically ill patients, home telemonitoring models based on mobile technologies are being tested, with the aim of guaranteeing continuity in care and more timely and effective assistance for chronically ill patients. An @Home project has been developed for these patients. The goal is to share information, coordinate doctors and nurses and communications between family and caregivers involved in the treatment process.
Finally, the Trentino health service also works to promote healthy lifestyles. For this reason, a new application (TrentinoSalute+) has been launched which promotes health and healthy lifestyles through a system of incentives (social and personal).
5.2. The Analysis of the Interview
The interview track is divided into four subdimensions, corresponding to the ecosystems’ key concepts arising from the theoretical background. For this reason, the results are reported by commenting on each dimension separately.
5.2.1. Actor
The main actors of Trentino eHealth ecosystem belong to the patient network - patient, patient’s family, formal and informal caregiver - and the provider network - health workers, other healthcare organization, etc. (the classification “patient network—provider network” is taken from Patrício et al. [
64]). In the provider network, there are different actors with organizational roles, such as the Autonomous Province of Trento (PAT) (including the health department or innovation and research department), the Provincial Agency for Health Services (APSS) and the Bruno Kessler Foundation (FBK). Since the Trentino eHealth ecosystem is populated by a series of actors who plan health policies in a shared way, we asked the interviewee if the multi-stakeholder dimension is seen as an advantage or a disadvantage. The interviewee states that the planning of health policies in a shared way, through the involvement of different stakeholders, represents an extraordinary work tool that enables combining the multiple experiences and dividing the responsibilities that each actor has in the programming of the service. With reference to the multi-stakeholder dimension of the digital health ecosystem, the interviewee states:
“We consider a great opportunity the possibility of aggregating subjects who have different responsibilities: such as the responsibility of conducting services on the territory, the responsibility of government and the responsibility of programming. All together, by making available our skills and knowledge, we believe that absolutely good work can be done, remembering that our goal is to provide services, adapting them to the challenges that digital healthcare will give us. So, it is a great opportunity for us, it is a great opportunity for professional growth by comparing skills within the system.”
5.2.2. Technology
Regarding the technology element, we asked what the role of technology is in the ecosystem. The interviewee considers technology a lever for the innovation of health services. He argues that, in addition to innovating health services, the use of technologies and information technology can be useful to citizens mainly for two reasons: (1) flattening the differences between the levels of assistance provided to citizens, (2) improving the management of visits. Regarding the first point, the interviewee states:
“The Italian health system has many differences because it is a federated system in which, despite the guidelines of the Ministry of Health, the implementation of the policies on the territory is entrusted to the Regions. In this sense, there are Regions that manage their mission better and others that manage their mission worse. However, all Italian citizens have the right to the same levels of assistance and in this (sense) the ICT, or in general the information systems, can certainly represent support to improve health care and lead the Ministry towards uniformity of assistance.”
Regarding the better management of visits (the second point), the interviewee refers to recent digital methods and procedures related to telemedicine. The use of tele-visits would allow citizens to receive medical services remotely, allowing the doctor to provide more facilitated management of the volume of visits. The idea is to refer to the model adopted by some foreign countries, in which only some of the visits are carried out in the presence of the doctor, while the rest is carried out remotely. In this regard, the interviewee says:
“There are some foreign experiences in which 50% of the assessments for a first diagnosis are carried out thanks to automatic systems, such as chatbot systems (Artificial Intelligence), to a subsequent level, 20% (of the visits are carried out) with a tele-visit. Finally, only 30% physically show up for a visit. This should be the development and future of public health.”
5.2.3. Institution
Regarding the institution, we asked what has changed in terms of rules, social norms with the introduction of the digitization of health care.
The interviewee states that the participatory governance model, implemented in Trentino, in which multiple actors participate in the planning of health services, has favoured the digitization of healthcare. The participatory governance model allowed the introduction of new technologies that led to new habits and new institutions. For example, the introduction of tele-visits or the telemonitoring of chronic patients is favouring the development of the patient’s self-management of the disease. The interviewee says:
“We are developing web IT systems to support customers and families through self-management, as long as the family can withstand them. (We mean) A self-management of the pathology, resorting to the specialist, the general practitioner or epidemiologist nurse, only where necessary.”
5.2.4. Resource Integration
The resources exchanged between the provider network and patient network, as mentioned above, can be divided into operand and operant resources. Regarding operand resource (material resources) [
2], digital tools and devices can be considered. The interviewee mentions some “pedometer bracelets” for the elderly, which were provided to citizens participating in a program to promote healthy lifestyles (TrentinoSalute+). This involves “Geo cashing”, which is a treasure hunt with pedometer bracelets connected to a geolocation app to hide or find real or virtual objects.
Regarding operant resources (immaterial resources) [
2], knowledge and data can be considered. These resources are more in number than the first ones, as the “dematerialization” of material resources (e.g., digitized health recipe, electronic health record, etc.) allows us to acquire countless data (big data) and information that represent “the result of a co-creation made with end-users.”
Regarding the result of the resource integration, the interviewee states:
“The Autonomous Province of Trento organized a Competence Center on Digital Health, called Trentinosalute4.0, to give value and collect value through citizens’ data. These data are collected by the various Trentino entities for health activities. It is not just a matter of giving value to the individual health service but of creating added value, through the processing of big data, for the whole community. At the same time, entities that develop this approach must protect citizen data. So, (it is necessary) to give value to the data, to allow this value to be distributed to citizens and, at the same time, to make it safer to use the data.”
6. The Service Ecosystem in Digital Health Sector
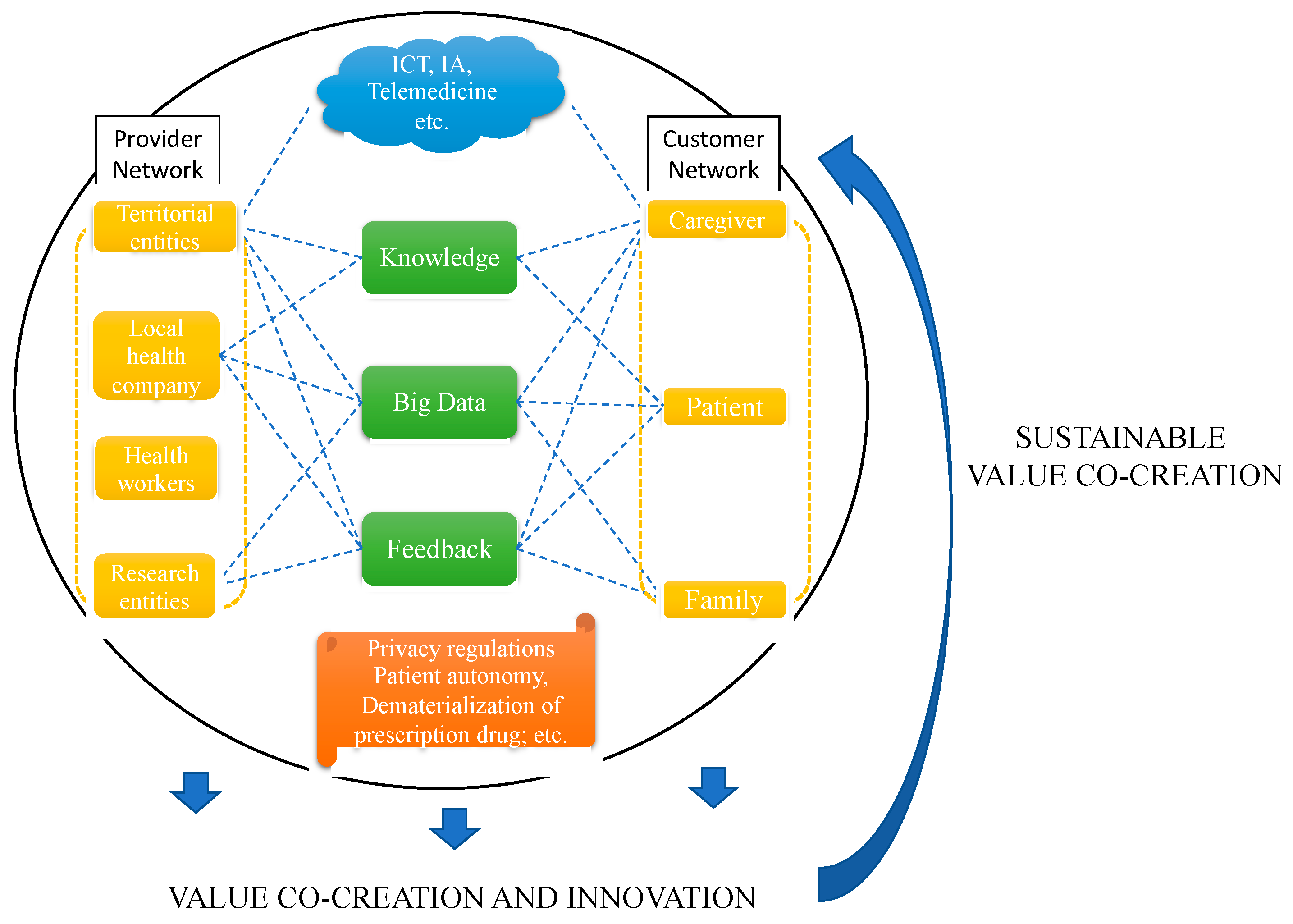
This work re-reads the digital health sector as a service ecosystem, through the lens of service theories, applying a case study methodology. Specifically, the analysis of the Trentino digital health system allows us to test a framework which pinpoints: (1) the main actors of an eHealth ecosystem; (2) the kind of resources exchanged; (3) innovations brought by technologies to health services; (4) new institutions (social rules). According to a system view of value co-creation, the framework assumes that the four elements of the service ecosystem influence value co-creation.
Regarding the actors, in line with Vargo and Lusch’s [
3] assumption, in the Trentino e-health ecosystem there is a multi-stakeholder vision in which actors have equal power and comprise interconnected systems. The analyzed ecosystem is considered as a complex set of stakeholder groups, in which the actors belong to the patient network or provider network. In the Trentino e-health ecosystem, participatory governance exists, which entails a series of advantages, especially in terms of service co-design [
65] and the division of responsibility.
Regarding the dimension of technology, many studies stated [
66,
67] that ICT plays an active role in reshaping the user’s co-creation experiences. In line with this view, in the Trentino e-health ecosystem, technology is a crucial element for the introduction of innovation in health services. Since it allows everyone to provide the service in the same way, technology favours the elimination of differences in the assistance of citizens (democratization of service provision). In addition, the introduction of telemedicine allows the improvement in the management of visits, which are carried out in the physical presence if urgent or remotely if less urgent.
Together with technology, the institutions (rules, norms, practices, etc.) are also considered as facilitators of value co-creation [
68]. Regarding the dimension of the institution, in the Trentino eHealth ecosystem, the continuous digitalization development of health services allowed the establishment of new social norms that were added to the existing ones. New institutions can be categorized as formal rules (such as the need to have the health card to access some services, having the credentials to access the electronic files, respecting visit times and general rules, accept privacy regulations) and informal rules (such as the creation of new norms and practices). Among the new informal rules, the following are fundamental for the value co-creation: patient self-management, dematerialization of pharmaceutical prescriptions; remote monitoring; access to own health records in real-time through technology and patient empowerment through feedback sharing.
Finally, resource integration refers to the exchange of operand (tangible elements) and operant resources (intangible elements) between the players of the ecosystem [
2]. In the Trentino eHealth ecosystem, the operand resources are represented by digital devices and digital tools that allow the patient to record data and communicate with healthcare professionals; operant resources are information, know-how, competencies knowledge, personal experience, feedback, but above all patient data.
The integration of the four elements into the service ecosystem of Trentino brings value for all the players in the system and produces innovation, in terms of new resources, new uses of technology, and new institutions (see
Table 1).
The new elements created by the integration of the provider network and the patient network allow the improvement of the service, bringing about value co-creation and innovation in the short term and sustainable value co-creation in the long term.
Specifically, resource dematerialization allows to collect a large quantity of data. Data processing provides valuable information that improves the diagnoses and brings benefits not only to the individual patient but to the entire community. Therefore, while patient data represent the main value provided by the patient network, knowledge provided by those who process and interpret the data represents the main value provided by the provider network. Data and knowledge exchange between the actors enable the exchange of value between the ecosystem players. The integration of these resources (data and knowledge), the strategic use of eHealth technologies and the pursuit of common rules among the players of the system foster the creation of new resources, new uses of technology and new institutions that support a more effective and efficient service, then a mutual benefit that leads to sustainable value co-creation (as shown in
Figure 2).
7. Conclusions
Recent service theories, S-D logic [
8] and SSMED [
5], foresee the adoption of a holistic vision of the process of service exchange and a systemic perspective, which led to the conceptualization of the ecosystem service, intended as the most appropriate business asset to favour the emergence of value.
By applying the system perspective to the healthcare sector [
21,
48,
64], the work aims to configure the service ecosystem as the most suitable organizational model for obtaining the value co-creation in the digital health sector.
Through the case study of the Trentino eHealth ecosystem, this work demonstrates that the eHealth ecosystem is a system of actors in which all the players are potential value co-creators that, through the use of technologies and the creation of new practices and social rules (institution), can exchange operand and operant resources, allowing the integration of resources, which leads to value co-creation. The multi-stakeholder reality, which is considered to be the main obstacle to the adoption of digital technologies in the healthcare field [
7], is instead an advantage according to the holistic view of the theories of the service.
These theories consider that the interaction of supplier network actors and patient network actors produce resource integration which can turn into value co-creation and innovation if new resources, new uses of technology and new institutions are created. When such innovation persists over time, giving rise to the improvement of the service in its entirety, sustainable value co-creation is generated.
Sustainable value co-creation brings advantages in terms of: (1) economic advantage (digital health can increase the economic sustainability of the health system and extend access to care in the population, both in terms of economic accessibility and capillarity); (2) social well-being (the use of digital tools allows citizens to have direct contact with health professionals and constant monitoring of their health, bringing advantage in terms of health to the entire community); (3) environmental benefit (eHealth systems involve the development of the entire territory and encourage healthy and sustainable lifestyles, e.g., walking on foot, respecting the environment).
These conclusions are in line with the recent literature, in which we have increasingly witnessed the development of theories that try to reconcile these three aspects: economic, social, environmental. Starting from the triple bottom line (TBL) model of sustainability [
69], this trend has affected the area of service management but also other areas (such as entrepreneurship, where new entrepreneurial theories require increasingly human entrepreneurship) [
70,
71]. This evolution suggests that the application of these theoretical models allows entrepreneurs, public decision-makers and policymakers to have the theoretical foundations for improving not only individual services but the whole society.
The main limitation of this work is in the methodology. In fact, case studies are never generalizable to the population. Moreover, the number of interviews should be increased in order to enhance data validity. Other qualitative research techniques such as observations or content analysis (e.g., of online reviews) can be also integrated into the methodology in order to perform more in-depth data analysis and to gain richer data. Furthermore, empirical research only takes into account the providers’ points of view. Therefore, further empirical research should be conducted on patients to make comparisons between providers and users’ point of view. It could also be interesting to investigate the acceptance and use of technology.
8. Implications
The work entails both theoretical and practical implications.
From a theoretical point of view, the present work contributes to advancements in service research by bridging the existing gap in the literature between theory and practice. The present study provides empirical proofs regarding service ecosystem functioning as it is an empirical study on value co-creation that differs from previous research [
72,
73]. In line with recent studies [
74,
75], the literature on value co-creation has been expanded, particularly by providing the service provider’s point of view. Moreover, in light of the importance of technology in value co-creation activities, it is possible to consider eHealth as a mean of integrating and optimizing the resources exchanged and of creating new institutions. In order to increase patient engagement, eHealth must not simply focus on providing technical infrastructures but must also consider the social aspects connected with the development of new practices that allow patient autonomy. Lastly, the paper provides a theoretical framework for pinpointing the main elements of eHealth ecosystems and the main conditions fostering value co-creation.
From a practical point of view, the elements of the service ecosystem can be understood as antecedents of value co-creation. In this sense, the results of the study can address public decision-makers to focus on these elements by seeking: to stimulate active citizenship through actor engagement and to lay out the conditions for a participatory governance model (actors); to overcome technological barriers and to defend the privacy of citizens’ data (technology); to define new social norms (institutions) that are patient-centred, such as: the democratization of the health service, the dematerialization of pharmaceutical prescriptions, remote monitoring, the access to health documentation through technology.
In this frame, digital technology is fundamental, as its strategic use allows organizations to make decisions on objective facts, and not on personal sensations. These data-driven approaches are increasingly widespread, especially in marketing [
76,
77], and allow the improvement of services through a greater personalization of the offer.
Specifically, in the health sector, decision-makers can be encouraged to manage better ICT platforms in order to strive towards the creation of a competence centre on digital healthcare with the aim of creating a digital space shared among all the actors of the ecosystem to support the development of digital healthcare and value co-creation. The generation of sustainable value co-creation translates into a general improvement of the service that can affect the entire society. Specifically, in the healthcare sector, the encounter with digital health and attention to the patient generated digital systems for monitoring wellness parameters and mobile apps dedicated to specific pathological situations that allow the collection of personalized data relating to the health status of each patient. In the future, increasingly sophisticated algorithms that analyze data from sensors or mobile apps will allow researchers to create real “digital biomarkers” of the health status, able to keep all the critical parameters for disease progression under control. This will represent a fundamental step towards the emergence of precision medicine based on the stratification of patients into homogeneous groups based on symptoms. Digital health and the centrality of the patient can be considered a step forward towards personalized medicine, which proposes the personalization of health, with decisions, practices and/or medical products being tailored to the patient. Finally, this study anticipates some problems emerging in current times for the management of the Covid-19 pandemic. In particular, the use of ICT platforms is proving to be fundamental both in the treatment phase and in the prevention phase. In the treatment phase, the need to isolate the patient makes the ICT platforms a fundamental tool for communicating with doctors and for keeping in touch with family members. For prevention, ICT platforms are the main tool for tracking the movements of people to rebuild, if necessary, the chain of contacts.