The Protective Role of Emotional Intelligence in Self-Stigma and Emotional Exhaustion of Family Members of People with Mental Disorders
Abstract
:1. Introduction
2. Method
2.1. Participants
2.2. Measurements
2.2.1. Emotional Intelligence
2.2.2. Family Self-Stigma Scale
2.2.3. Burnout
2.3. Procedure
3. Data Analysis
4. Results
4.1. Preliminary Analysis
4.2. Structural Equation Modeling
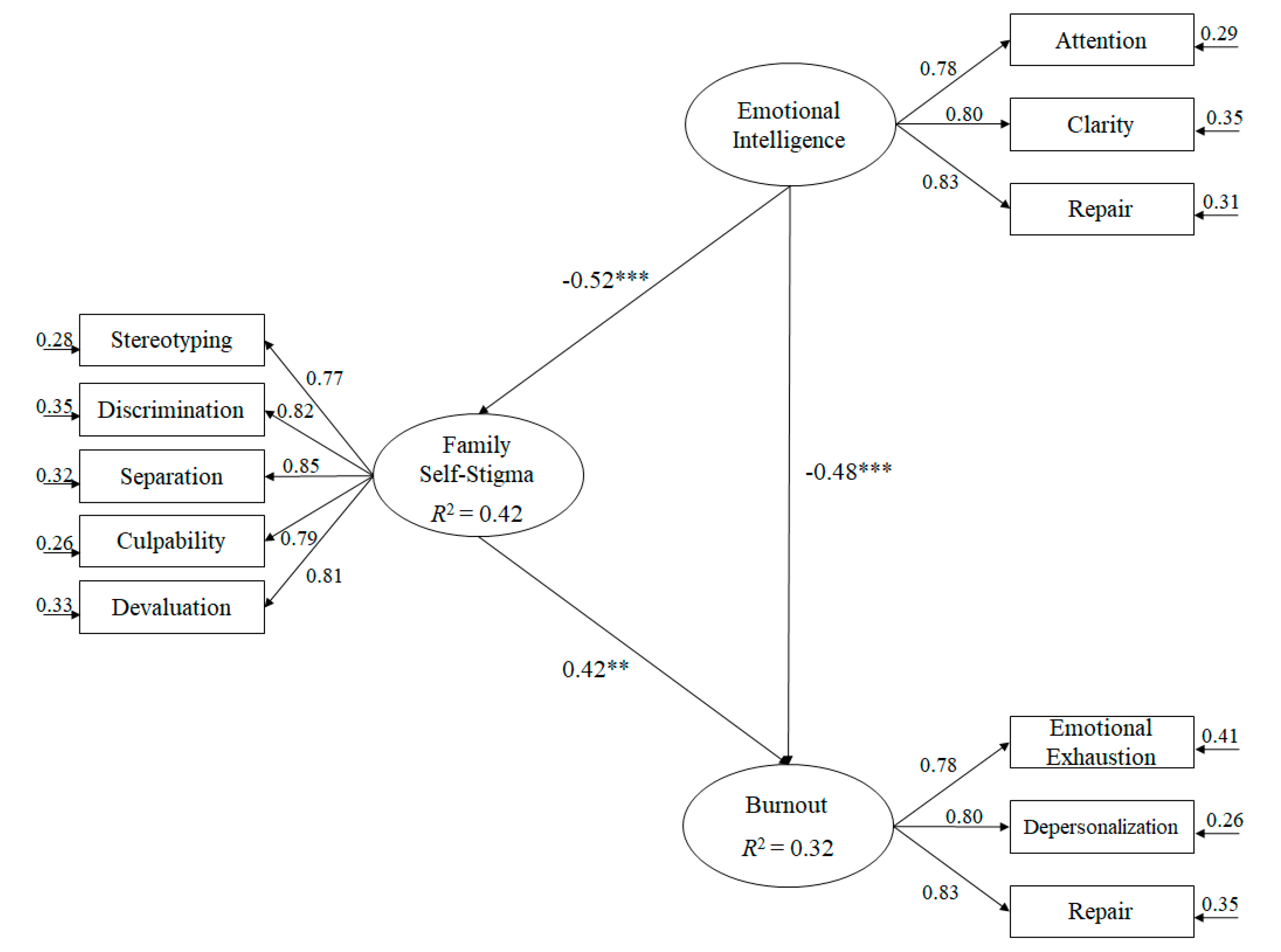
- (a)
- Emotional intelligence negatively predicted family self-stigma (β = −0.52, p < 0.001).
- (b)
- Family self-stigma positively predicted burnout (β = 0.42, p < 0.001).
- (c)
- Emotional intelligence predicted burnout negatively (β = −0.48, p < 0.001).
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Engelberg, E.; Sjöberg, L. Internet use, social skills, and adjustment. Cyberpsychol. Behav. 2004, 1, 41–47. [Google Scholar] [CrossRef] [Green Version]
- El-Khodary, B.; Samara, M. The mediating role of trait emotional intelligence, prosocial behaviour, parental support and parental psychological control on the relationship between war trauma, and PTSD and depression. J. Res. Personal. 2019, 81, 246–256. [Google Scholar] [CrossRef]
- Cheung, R.Y.; Leung, M.C.; Chung, K.K.H.; Cheung, H.Y. Family risks and adolescent adjustment in Chinese contexts: Testing the mediating role of emotional intelligence. J. Child Fam. Stud. 2018, 12, 3887–3896. [Google Scholar] [CrossRef]
- Extremera, N.; Mérida-López, S.; Sánchez-Álvarez, N.; Quintana-Orts, C.; Rey, L. A friend is a treasure: Emotional intelligence, workplace social support and teacher engagement. Prax. Saber 2019, 24, 69–92. [Google Scholar] [CrossRef] [Green Version]
- Salovey, P.; Stroud, L.R.; Woolery, A.; Epel, E.S. Perceived emotional intelligence, stress reactivity, and symptom reports: Further explorations using the trait meta-mood scale. Psychol. Health 2002, 5, 611–627. [Google Scholar] [CrossRef]
- Fink, K.; Cohen, J.; Slade, S. Integrating Prosocial Learning with Education Standards: School Climate Reform Initiatives; Routledge: New York, NY, USA, 2015. [Google Scholar]
- Ashknasy, N.M.; Dasborough, M.T. Emotional Awareness and Emotional Intelligence in Leadership Teaching. J. Educ. Bus. 2003, 79, 18–22. [Google Scholar] [CrossRef]
- Garg, R.; Levin, E.; Tremblay, L. Emotional intelligence: Impact on post-secondary academic achievement. Soc. Psychol. Educ. 2016, 3, 627–642. [Google Scholar] [CrossRef]
- MacCann, C.; Jiang, Y.; Brown, L.E.; Double, K.S.; Bucich, M.; Minbashian, A. Emotional intelligence predicts academic performance: A meta-analysis. Psychol. Bull. 2020, 2, 150. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.L.; Cassady, J.C.; Heller, M.L. The influence of emotional intelligence, cognitive test anxiety, and coping strategies on undergraduate academic performance. Learn. Individ. Differ. 2017, 55, 40–48. [Google Scholar] [CrossRef]
- Mestre, J.M.; Guil, R.; Martínez-Cabañas, F.; Larrán, C.; González, G. Validación de una prueba para evaluar la capacidad de percibir, expresar y valorar emociones en niños de la etapa infantil. Rev. Electrónica Interuniv. Form. Profr. 2011, 3, 37–54. [Google Scholar]
- Cladellas, R.; Clariana, M.; Gotzens, C.; Badía, M.; Dezcallar, T. Patrones de descanso, actividades físico-deportivas extraescolares y rendimiento académico en niños y niñas de primaria. Rev. Psicol. Deporte 2015, 1, 0053–0059. [Google Scholar]
- Goleman, D. Liderazgo. El Poder de la Inteligencia Emocional; B de Bolsillo: Barcelona, Spain, 2014. [Google Scholar]
- Koole, S.L. The psychology of emotion regulation: An integrative review. Cogn. Emot. 2009, 1, 4–41. [Google Scholar] [CrossRef]
- Mayer, J.D.; Salovey, P.; Caruso, D.R. Emotional Intelligence as Zeigeist, as Personality, and as Mental Ability. In The Handbook of Emotional Intelligence. Theory, Development, Assessment, and Application at Home, School, and in the Workplace; Bar-On, R., Parker, J.D.A., Eds.; Jossey-Bass: San Francisco, CA, USA, 2000; pp. 92–117. [Google Scholar]
- Guerrero-Barona, E.; Sánchez-Herrera, S.; Moreno-Manso, J.M.; Sosa-Baltasar, D.; Durán-Vinagre, M.Á. El autoconcepto y su relación con la inteligencia emocional y la ansiedad. Behav. Psychol. 2019, 3, 455–476. [Google Scholar]
- Corrigan, P.W.; Bink, A.B.; Schmidt, A. Reducing Physical Illness Stigma: Insights from the Mental Illness Arena. In The Oxford Handbook of Stigma, Discrimination, and Health; Major, B., Dovidio, J.F., Link, B., Eds.; Oxford University Press: Oxford, UK, 2018. [Google Scholar]
- Livingston, J.D.; Boyd, J.E. Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Soc. Sci. Med. 2010, 12, 2150–2161. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, M.; Sanz, M.; Pérez-Santos, E. Estado del conocimiento sobre el estigma internalizado desde el modelo socio-cognitivo comportamental. Anu. Psicol. Clínica Salud. Annu. Clin. Health Psychol. 2011, 7, 41–50. [Google Scholar]
- López, M.; Laviana, M.; Fernández, L.; López, A.; Rodríguez, A.M.; Aparicio, A. La lucha contra el estigma y la discriminación en salud mental: Una estrategia compleja basada en la información disponible. Rev. Asoc. Española Neuropsiquiatría 2008, 1, 48–83. [Google Scholar] [CrossRef] [Green Version]
- Gentile, A.; Servidio, R.; Caci, B.; Boca, S. Social stigma and self-esteem as mediators of the relationship between Body Mass Index and Internet addiction disorder. An exploratory study. Curr. Psychol. 2018, 1–9. [Google Scholar] [CrossRef]
- Evans-Lacko, S.; Henderson, C.; Thornicroft, G.; McCrone, P. Economic evaluation of the anti-stigma social marketing campaign in England 2009–2011. Br. J. Psychiatry 2013, 55, s95–s101. [Google Scholar] [CrossRef] [Green Version]
- Oexle, N.; Waldmann, T.; Staiger, T.; Xu, Z.; Ruesch, N. Mental illness stigma and suicidality: The role of public and individual stigma. Epidemiol. Psychiatr. Sci. 2018, 2, 169–175. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Nieweglowski, K. How does familiarity impact the stigma of mental illness? Clin. Psychol. Rev. 2019, 70, 40–50. [Google Scholar] [CrossRef]
- Rüsch, N.; Zlati, A.; Black, G.; Thornicroft, G. Does the stigma of mental illness contribute to suicidality? Br. J. Psychiatry 2014, 4, 257–259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Persson, P.; Rossin-Slater, M. Family ruptures, stress, and the mental health of the next generation. Am. Econ. Rev. 2018, 4–5, 1214–1252. [Google Scholar] [CrossRef] [Green Version]
- Thornicroft, G.; Mehta, N.; Clement, S.; Evans-Lacko, S.; Doherty, M.; Rose, D.; Koschorke, M.; Shidhaye, R.; O’Reilly, C.; Henderson, C. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet 2016, 10023, 1123–1132. [Google Scholar] [CrossRef]
- Muñoz, M.; Pérez Santos, E.; Crespo, M.; Guillen, A.I. Estigma y Enfermedad Mental. Available online: Biblioteca.ucm.es/ecsa/9788474919806.pdf (accessed on 8 April 2020).
- Gabrielian, S.; Young, A.S.; Greenberg, J.M.; Bromley, E. Social support and housing transitions among homeless adults with serious mental illness and substance use disorders. Psychiatr. Rehabil. J. 2018, 3, 208. [Google Scholar] [CrossRef] [PubMed]
- Maguire, R.; Egan, A.; Hyland, P.; Maguire, P. Engaging students emotionally: The role of emotional intelligence in predicting cognitive and affective engagement in higher education. High. Educ. Res. Dev. 2017, 2, 343–357. [Google Scholar] [CrossRef] [Green Version]
- Extremera, N.; Durán, A.; Rey, L. Perceived emotional intelligence and dispositional optimism–pessimism: Analyzing their role in predicting psychological adjustment among adolescents. Personal. Individ. Differ. 2007, 6, 1069–1079. [Google Scholar] [CrossRef]
- Carvalho, V.S.; Guerrero, E.; Chambel, M.J. Emotional intelligence and health students’ well-being: A two-wave study with students of medicine, physiotherapy and nursing. Nurse Educ. Today 2018, 63, 35–42. [Google Scholar] [CrossRef]
- De Alba, U.R.; Colorado, Y.S. Relación entre inteligencia emocional, depresión y rendimiento académico en estudiantes de psicología. Psicogente 2012, 28, 348–359. [Google Scholar]
- Salovey, P.; Mayer, J.D. Emotional intelligence. Imagin. Cogn. Personal. 1990, 3, 185–211. [Google Scholar] [CrossRef]
- Salovey, P.; Woolery, A.; Mayer, J.D. Emotional intelligence: Conceptualization and measurement. In Blackwell Handbook of Social Psychology: Interpersonal Processes; John Wiley & Sons: Hoboken, NJ, USA, 2001; pp. 279–307. [Google Scholar]
- Veytia, M.; Fajardo, R.; Guadarrama, R.; Escutia, N. Inteligencia Emocional: Factor positivo ante la depresión en adolescentes de bachillerato. Rev. Inf. Psicológicos 2016, 1, 35–50. [Google Scholar] [CrossRef]
- Balluerka, N.; Aritzeta, A.; Gorostiaga, A.; Gartzia, L.; Soroa, G. Emotional intelligence and depressed mood in adolescence: A multilevel approach. Int. J. Clin. Health Psychol. 2013, 2, 110–117. [Google Scholar] [CrossRef] [Green Version]
- Reever, K.E.; Mathieu, E.; Dennis, M.P.; Gitlin, L.N. Adult day services plus: Augmenting adult day centers with systematic care management for family caregivers. Alzheimer’s Care Today 2004, 4, 332–339. [Google Scholar]
- Ross, S.G.; Bruggeman, B.; Maldonado, M.; Deiling, M. Examining personal, perceived, treatment, and self-stigma in college students: The role of Parent beliefs and mental health literacy. J. Coll. Stud. Psychother. 2019, 1, 1–15. [Google Scholar] [CrossRef]
- Lysaker, P.H.; Vohs, J.; Hasson-Ohayon, I.; Kukla, M.; Wierwille, J.; Dimaggio, G. Depression and insight in schizophrenia: Comparisons of levels of deficits in social cognition and metacognition and internalized stigma across three profiles. Schizophr. Res. 2013, 3, 18–23. [Google Scholar] [CrossRef]
- Kamaradova, D.; Latalova, K.; Prasko, J.; Kubinek, R.; Vrbova, K.; Mainerova, B.; Tichackova, A. Connection between self-stigma, adherence to treatment, and discontinuation of medication. Patient Prefer. Adherence 2016, 10, 1289. [Google Scholar] [CrossRef] [Green Version]
- European Federation of Associations of Families of People with Mental Illness, (EUFAMI); Annual Report; EUFAMI: De Haan, Bélgica, 2014; Available online: http://eufami.org/wp-content/uploads/2018/03/eufami-annual-report-2014-lr.pdf (accessed on 8 April 2020).
- Freudenberger, H.J. Staff burnout. J. Soc. Issues 1974, 7, 159–164. [Google Scholar] [CrossRef]
- Briones, C. Teorías performativas de la identidad y performatividad de las teorías. Tabula Rasa 2007, 6, 55–83. [Google Scholar] [CrossRef]
- Valério, F.J.; Amorim, C.; Moser, A.M. A síndrome de Burnout em professores de Educação Física. Rev. Psicol. IMED 2009, 1, 127–136. [Google Scholar] [CrossRef]
- WHO. Informe Sobre la Salud en el Mundo: 2000. Mejorar el Desempeño de los Sistemas de Salud; Organización Mundial de la Salud: Ginebra, Switzerland, 2000. [Google Scholar]
- Aceves, G.A. Síndrome de burnout. Arch. Neurocienc. 2006, 4, 305–309. [Google Scholar]
- Laschinger, H.; Grau, A. The Influence of Personal Dispositional Factors and Organizational Resources on Workplace Violence, Burnout, and Health Outcomes in New Graduate Nurses: A Cross-Sectional Study. Int. J. Nurs. Stud. 2012, 49, 282–291. [Google Scholar] [CrossRef]
- Alarcon, G.; Eschleman, K.J.; Bowling, N.A. Relationship between Personality Variables and Burnout A Meta-Analysis. Work Stress 2009, 23, 244–263. [Google Scholar] [CrossRef]
- Schaufeli, W.; Enzmann, D. The Burnout Companion to Study and Practice: A Critical Analysis; CRC Press: Boca Raton, FL, USA, 1998. [Google Scholar]
- Son, J.; Erno, A.; Shea, D.G.; Femia, E.E.; Zarit, S.H.; Parris Stephens, M.A. The caregiver stress process and health outcomes. J. Aging Health 2007, 6, 871–887. [Google Scholar] [CrossRef] [PubMed]
- Morris, E.; Hippman, C.; Murray, G.; Michalak, E.E.; Boyd, J.E.; Livingston, J.; Inglis, A.; Carrion, P.; Austin, J. Self-Stigma in Relatives of people with Mental Illness scale: Development and validation. Br. J. Psychiatry 2018, 212, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trigueros, R.; Navarro, N.; Cangas, A.J.; Aguilar-Parra, J.M.; Ortiz, L. Adaptation and validation to the spanish context of the scale of self-stigma in relatives of people with mental illness. Ann. Psychol. 2019, 35, 371–377. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Seisdedos, N. Inventario de Burnout de Maslach; TEA Ediciones: Madrid, Spain, 1997. [Google Scholar]
- Hair, J.; Black, W.; Babin, B.; Anderson, R.; Tatham, R. Multivariate Data Analysis; Pearson/Prentice Hall: Upper Saddle River, NJ, USA, 2006. [Google Scholar]
- Marsh, H.W.; Hau, K.T.; Wen, Z. In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Struct. Equ. Model. 2004, 11, 320–341. [Google Scholar] [CrossRef]
- McDonald, R.P.; Ho, M.H.R. Principles and practice in reporting structural equation analyses. Psychol. Methods 2002, 7, 64. [Google Scholar] [CrossRef]
- James, C. Law student wellbeing: Benefits of promoting psychological literacy and self-awareness using mindfulness, strengths theory and emotional intelligence. Legal Educ. Rev. 2011, 21, 217. [Google Scholar]
- Checa, P.; Fernández-Berrocal, P. The Role of Intelligence Quotient and Emotional Intelligence in Cognitive Control Processes. Front. Psychol. 2015, 6, 1853. [Google Scholar] [CrossRef] [Green Version]
- Armstrong, A.R.; Galligan, R.F.; Critchley, C.R. Emotional intelligence and psychological resilience to negative life events. Personal. Individ. Differ. 2011, 51, 331–336. [Google Scholar] [CrossRef]
- Mayer, J.D.; Salovey, P. What is emotional intelligence? In Emotional Development and Emotional Intelligence: Educational Implications; Salovey, P., Sluyter, D.J., Eds.; Basic Books: New York, NY, USA, 1997; pp. 3–34. [Google Scholar]
- Kircaburun, K.; Griffiths, M.D.; Billieux, J. Trait emotional intelligence and problematic online behaviors among adolescents: The mediating role of mindfulness, rumination, and depression. Personal. Individ. Differ. 2019, 139, 208–213. [Google Scholar] [CrossRef]
- Martínez-Monteagudo, M.C.; Inglés, C.J.; Granados, L.; Aparisi, D.; García-Fernández, J.M. Trait emotional intelligence profiles, burnout, anxiety, depression, and stress in secondary education teachers. Personal. Individ. Differ. 2019, 142, 53–61. [Google Scholar] [CrossRef]
- Barraza, R.; Muñoz, N.; Alfaro, M.; Álvarez, A.; Araya, V.; Villagra, J.; Contreras, A.M. Ansiedad, depresión, estrés y organización de la personalidad en estudiantes novatos de medicina y enfermería. Rev. Chil. Neuro-Psiquiatr. 2015, 4, 251–260. [Google Scholar] [CrossRef] [Green Version]
- Soares, J.J.; Grossi, G.; Sundin, Ö. Burnout among women: Associations with demographic/socio-economic, work, life-style and health factors. Arch. Women’s Ment. Health 2007, 2, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Eaton, K.; Stritzke, W.G.; Corrigan, P.W.; Ohan, J.L. Pathways to Self-Stigma in Parents of Children with a Mental Health Disorder. J. Child Fam. Stud. 2019, 29, 1732–1744. [Google Scholar] [CrossRef]
- Díaz, T. El desarrollo de competencias socioemocionales y su evaluación como elementos clave en los planes de formación docente. Algunas conclusiones derivadas de la evaluación SIMCE 2011. Rev. Iberoam. Educ. 2014, 64, 73–98. [Google Scholar] [CrossRef]
- Caruso, D.R. Emotional intelligence. In Encyclopedia of Industrial/Organizational Psychology; Rogelberg, S., Ed.; Sage: Thousand Oaks, CA, USA, 2006; pp. 180–182. [Google Scholar]
| Factors | M | SD | Range | α | 1 | 2 | 3 |
|---|---|---|---|---|---|---|---|
| 1. Emotional Intelligence | 3.82 | 0.86 | 1–5 | 0.79 | −0.40 *** | −0.31 ** | |
| 2. Family Self-Stigma | 2.07 | 1.12 | 1–5 | 0.84 | 0.53 *** | ||
| 3. Burnout | 2.57 | 1.34 | 0–6 | 0.82 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trigueros, R.; Navarro, N.; Cangas, A.J.; Mercader, I.; Aguilar-Parra, J.M.; González-Santos, J.; González-Bernal, J.J.; Soto-Cámara, R. The Protective Role of Emotional Intelligence in Self-Stigma and Emotional Exhaustion of Family Members of People with Mental Disorders. Sustainability 2020, 12, 4862. https://doi.org/10.3390/su12124862
Trigueros R, Navarro N, Cangas AJ, Mercader I, Aguilar-Parra JM, González-Santos J, González-Bernal JJ, Soto-Cámara R. The Protective Role of Emotional Intelligence in Self-Stigma and Emotional Exhaustion of Family Members of People with Mental Disorders. Sustainability. 2020; 12(12):4862. https://doi.org/10.3390/su12124862
Chicago/Turabian StyleTrigueros, Rubén, Noelia Navarro, Adolfo J. Cangas, Isabel Mercader, José M. Aguilar-Parra, Josefa González-Santos, Jerónimo J. González-Bernal, and Raúl Soto-Cámara. 2020. "The Protective Role of Emotional Intelligence in Self-Stigma and Emotional Exhaustion of Family Members of People with Mental Disorders" Sustainability 12, no. 12: 4862. https://doi.org/10.3390/su12124862
APA StyleTrigueros, R., Navarro, N., Cangas, A. J., Mercader, I., Aguilar-Parra, J. M., González-Santos, J., González-Bernal, J. J., & Soto-Cámara, R. (2020). The Protective Role of Emotional Intelligence in Self-Stigma and Emotional Exhaustion of Family Members of People with Mental Disorders. Sustainability, 12(12), 4862. https://doi.org/10.3390/su12124862










