Environmental Management in German Hospitals—A Classification of Approaches
Abstract
1. Introduction
- What is the organizational environmental performance of hospitals?
- Based on the hospitals’ organizational environmental performance, what classifications of EM approaches exist?
- What determines the EM approach?
2. Review of the Literature
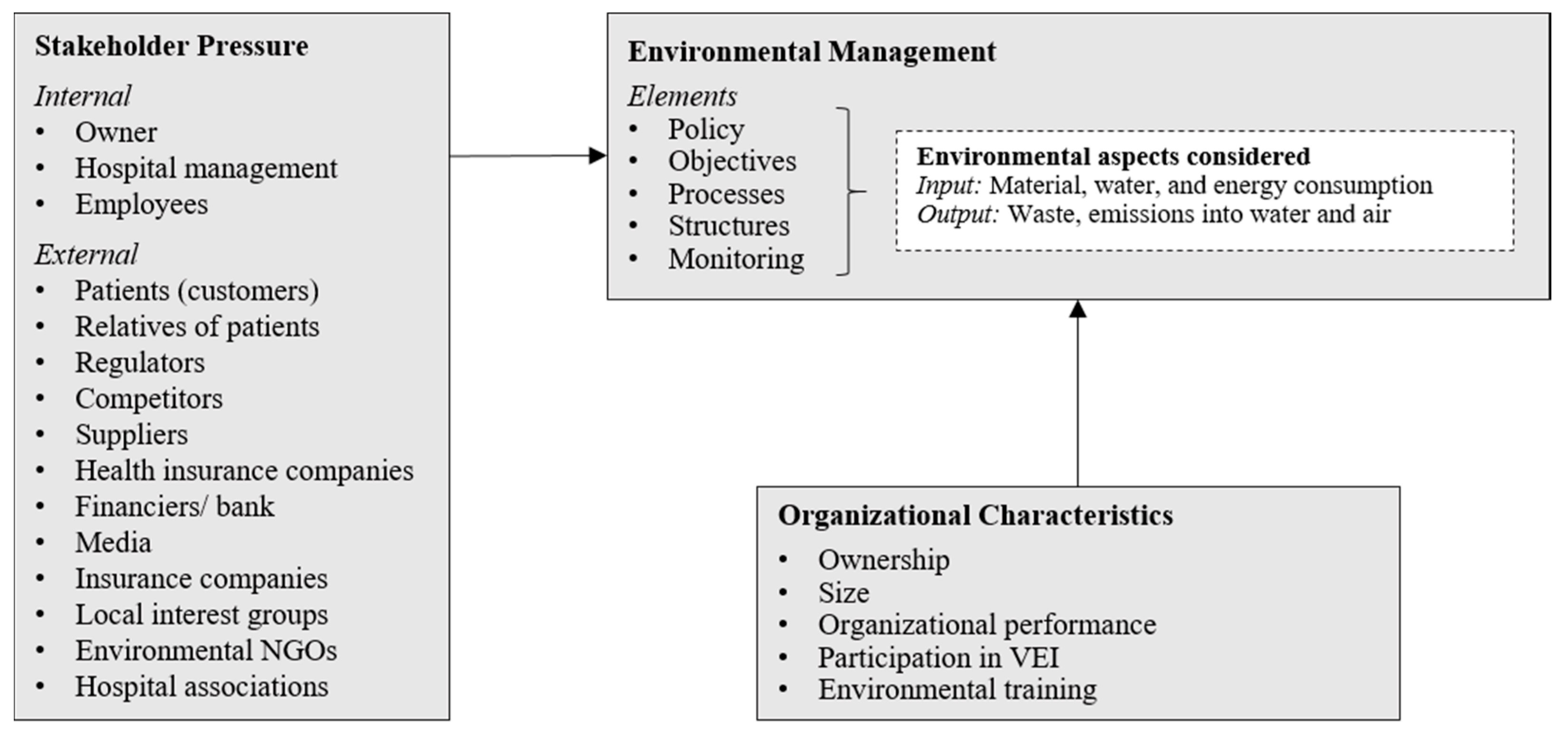
2.1. Organizational Environmental Management
2.2. Existing Environmental Management Approaches in Organizations
2.3. Practical Background: The German Hospital Sector and Its Stakeholders
3. Research Design
3.1. Measurement and Survey Development
3.2. Data Collection and Sampling
3.3. Data Analysis
4. Results and Discussion
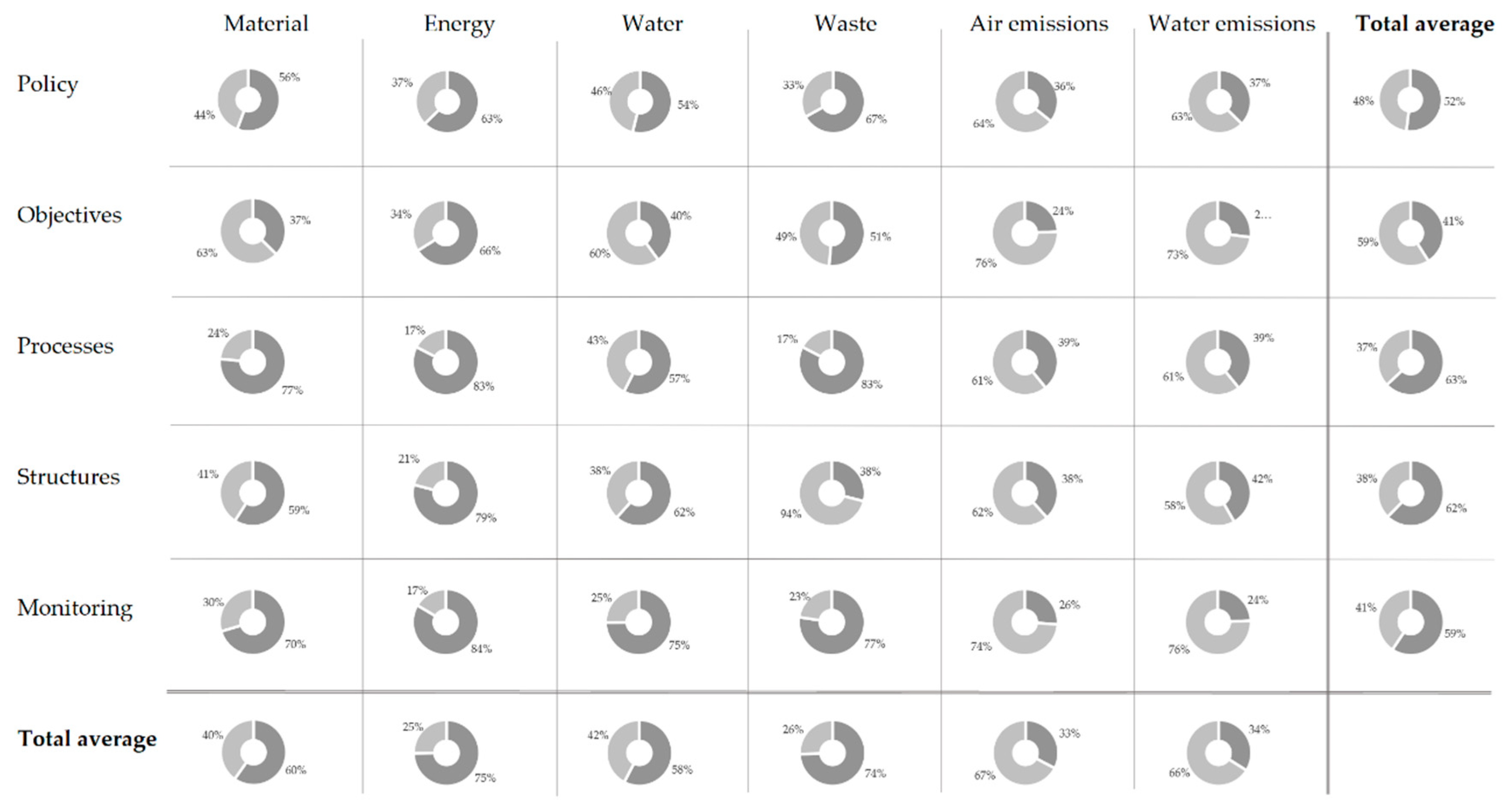
4.1. Descriptive Statistics
4.2. Cluster Analysis
4.2.1. Traditionalists
4.2.2. Pragmatists
4.2.3. Environmentalists
4.3. Potential Determinants of Environmental Management Approaches
4.3.1. Stakeholder Pressure
4.3.2. Ownership
4.3.3. Organizational Performance and Size
4.3.4. Participation in VEI
4.3.5. Environmental Training
5. Implications
6. Limitations and Future Research
Author Contributions
Funding
Conflicts of Interest
Appendix A
- Material consumption
- Energy consumption
- Water consumption
- Wastes
- Air emissions
- Emissions into water
- Material consumption
- Energy consumption
- Water consumption
- Wastes
- Air emissions
- Emissions into water
- Material consumption
- Energy consumption
- Water consumption
- Wastes
- Air emissions
- Emissions into water
- Material consumption
- Energy consumption
- Water consumption
- Wastes
- Air emissions
- Emissions into water
- Material consumption
- Energy consumption
- Water consumption
- Wastes
- Air emissions
- Emissions into water
- Owner
- Hospital management
- Employees
- Patients
- Relatives of patients
- Regulators
- Competitors
- Suppliers
- Health insurance companies
- Financiers/ banks
- Media
- Insurance companies
- Local interest groups
- Environmental NGOs
- Hospital associations
- Others (specify)
- Material consumption
- Energy consumption
- Water consumption
- Wastes
- Air emissions
- Emissions into water
- Yes, and we will continue to have it in the future.
- Yes, but we won’t have it in the future.
- No, but we are currently planning it for the future.
- No, and we are not currently planning it for the future.
- I do not know.
- Return on assets
- Return on sales
- Employee growth
- Sales growth
- Asset growth
- Debt-to-equity
- Innovation performance
- Overall organizational performance
- Bed occupancy rate
References
- Ambec, S.; Lanoie, P. Does it pay to be green? A systematic overview. Acad. Manag. Perspect. 2008, 22, 45–62. [Google Scholar] [CrossRef]
- Endrikat, J.; Guenther, E.; Hoppe, H. Making sense of conflicting empirical findings: A meta-analytic review of the relationship between corporate environmental and financial performance. Eur. Manag. J. 2014, 32, 735–751. [Google Scholar] [CrossRef]
- Heras-Saizarbitoria, I.A.; German, A.; Boiral, O. Exploring the dissemination of environmental certifications in high and low polluting industries. J. Clean. Prod. 2015, 89, 50–58. [Google Scholar] [CrossRef]
- Carballo-Penela, A.; Castromán-Diz, J.L. Environmental policies for sustainable development: An analysis of the drivers of proactive environmental strategies in the service sector: Environmental policies for sustainable development. Bus. Strategy Environ. 2015, 24, 802–818. [Google Scholar] [CrossRef]
- Céspedes-Lorente, J.; de Burgos-Jiménez, J.; Álvarez-Gil, M.J. Stakeholders’ environmental influence. An empirical analysis in the Spanish hotel industry. Scand. J. Manag. 2003, 19, 333–358. [Google Scholar] [CrossRef]
- Sánchez-Medina, P.S.; Díaz-Pichardo, R.; Cruz-Bautista, M. Stakeholder influence on the implementation of environmental management practices in the hotel industry: Stakeholders and EMPs in the hotel industry. Int. J. Tour. Res. 2016, 18, 387–398. [Google Scholar] [CrossRef]
- McGain, F.; Naylor, C. Environmental sustainability in hospitals—A systematic review and research agenda. J. Health Serv. Res. Policy 2014, 19, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Pinzone, M.; Lettieri, E.; Masella, C. Proactive environmental strategies in healthcare organisations: Drivers and barriers in Italy. J. Bus. Ethics 2015, 131, 183–197. [Google Scholar] [CrossRef]
- Jameton, A.; McGuire, C. Toward sustainable health-care services: Principles, challenges, and a process. Int. J. Sustain. High. Educ. 2002, 3, 113–127. [Google Scholar] [CrossRef]
- Ulhøi, J.; Ulhøi, B. Beyond climate focus and disciplinary myopia. The roles and responsibilities of hospitals and healthcare professionals. Int. J. Environ. Res. Public Health 2009, 6, 1204–1214. [Google Scholar] [CrossRef]
- Karlsson, M.; Öhman, D.P. Material consumption in the healthcare sector: Strategies to reduce its impact on climate change—The case of Region Scania in South Sweden. J. Clean. Prod. 2005, 13, 1071–1081. [Google Scholar] [CrossRef]
- Unger, S.; Landis, A. Assessing the environmental, human health, and economic impacts of reprocessed medical devices in a Phoenix hospital’s supply chain. J. Clean. Prod. 2016, 112, 1995–2003. [Google Scholar] [CrossRef]
- González, A.G.; García-Sanz-Calcedo, J.; Salgado, D.R.; Mena, A. A quantitative analysis of cold water for human consumption in hospitals in Spain. J. Healthc. Eng. 2016, 2016, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Čongradac, V.; Prebiračević, B.; Petrovački, N. Methods for assessing energy savings in hospitals using various control techniques. Energy Build. 2014, 69, 85–92. [Google Scholar] [CrossRef]
- Diaz, L.F.; Eggerth, L.L.; Enkhtsetseg, S.; Savage, G.M. Characteristics of healthcare wastes. Waste Manag. 2008, 28, 1219–1226. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.S.; Santhanam, A.; Norulaini, N.A.N.; Omar, A.K.M. Clinical solid waste management practices and its impact on human health and environment—A review. Waste Manag. 2011, 31, 754–766. [Google Scholar] [CrossRef] [PubMed]
- Vidal, R.; Moliner, E.; Pikula, A.; Mena-Nieto, A.; Ortega, A. Comparison of the carbon footprint of different patient diets in a Spanish hospital. J. Health Serv. Res. Policy 2015, 20, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Verlicchi, P.; Aukidy, M.A.; Zambello, E. What have we learned from worldwide experiences on the management and treatment of hospital effluent?—An overview and a discussion on perspectives. Sci. Total Environ. 2015, 514, 467–491. [Google Scholar] [CrossRef]
- Trumpp, C.; Endrikat, J.; Zopf, C.; Guenther, E. Definition, conceptualization, and measurement of corporate environmental performance: A critical examination of a multidimensional construct. J. Bus. Ethics 2015, 126, 185–204. [Google Scholar] [CrossRef]
- Seifert, C.; Guenther, E. Prevention is better than cure-environmental management measures in hospitals. Corp. Soc. Responsib. Environ. Manag. 2019, 26, 781–790. [Google Scholar] [CrossRef]
- Lizzi, G.D.; Collazzo, R.; Capra, E.; Lazzarini, R.; Goi, D. The environmental management system in a health structure: The case study of ORC-Aviano (Italy). Open Waste Manag. J. 2017, 10, 1–12. [Google Scholar] [CrossRef]
- Ryan-Fogarty, Y.; O’Regan, B.; Moles, R. Greening healthcare: Systematic implementation of environmental programmes in a university teaching hospital. J. Clean. Prod. 2016, 126, 248–259. [Google Scholar] [CrossRef]
- Dettenkofer, M.; Kümmerer, K.; Schuster, A.; Mühlich, M.; Scherrer, M.; Daschner, F.D. Environmental auditing in hospitals: Approach and implementation in an university hospital. J. Hosp. Infect. 1997, 36, 17–22. [Google Scholar] [CrossRef]
- Dettenkofer, K.K.; Armin, M.; Kuemmerer, K.; Schuster, A.; Mueller, W.; Muehlich, M.; Scherrer, M.; Daschner, F.D. Environmental auditing in hospitals: First results in a university hospital. Environ. Manag. 2000, 25, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Seifert, C. The barriers for voluntary environmental management systems—The case of EMAS in hospitals. Sustainability 2018, 10, 1420. [Google Scholar] [CrossRef]
- Seifert, C.; Guenther, E. Who cares?—Stakeholder relevance for voluntary environmental management in hospitals. Corp. Soc. Responsib. Environ. Manag. 2020. [Google Scholar] [CrossRef]
- Lega, F.; Prenestini, A.; Spurgeon, P. Is management essential to improving the performance and sustainability of health care systems and organizations? A systematic review and a roadmap for future studies. Value Health 2013, 16, S46–S51. [Google Scholar] [CrossRef] [PubMed]
- Seifert, C.; Koep, L.; Wolf, P.; Guenther, E. Life cycle assessment as decision support tool for environmental management in hospitals: A literature review. Health Care Manag. Rev. 2019, 1. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Blanco, J.; Inaba, A.; Quiros, A.; Valdivia, S.; Milà-i-Canals, L.; Finkbeiner, M. Organizational LCA: The new member of the LCA family—Introducing the UNEP/SETAC Life Cycle Initiative guidance document. Int. J. Life Cycle Assess. 2015, 20, 1045–1047. [Google Scholar] [CrossRef]
- Guinee, J.B.; Heijungs, R.; Huppes, G.; Zamagni, A.; Masoni, P.; Buonamici, R.; Ekvall, T.; Rydberg, T. Life cycle assessment: Past, present, and future. Environ. Sci. Technol. 2010, 45, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Rimano, M.; Simboli, A.; Taddeo, R.; Raggi, A. Life cycle approaches for the environmental impact assessment of organizations: Defining the state of the art. Adm. Sci. 2019, 9, 94. [Google Scholar] [CrossRef]
- EMAS III. Regulation (EC) No 1221/2009 of the European Parliament and of the Council. Available online: http://eur-lex.europa.eu/legal-content/EN/TXT/HTML/?uri=CELEX:32009R1221&from=en (accessed on 6 March 2020).
- Testa, F.; Rizzi, F.; Daddi, T.; Gusmerotti, N.M.; Frey, M.; Iraldo, F. EMAS and ISO 14001: The differences in effectively improving environmental performance. J. Clean. Prod. 2014, 68, 165–173. [Google Scholar] [CrossRef]
- Tourais, P.; Videira, N. Why, how and what do organizations achieve with the implementation of environmental management systems?—Lessons from a comprehensive review on the eco-management and audit scheme. Sustainability 2016, 8, 283. [Google Scholar] [CrossRef]
- Morrow, D.; Rondinelli, D. Adopting corporate environmental management systems: Motivations and results of ISO 14001 and EMAS certification. Eur. Manag. J. 2002, 20, 159–171. [Google Scholar] [CrossRef]
- Boiral, O.; Guillaumie, L.; Heras-Saizarbitoria, I.; Tene, C.V.T. Adoption and outcomes of ISO 14001: A systematic review. Int. J. Manag. Rev. 2017. [Google Scholar] [CrossRef]
- Wenk, M.S. EU’s eco-management and audit scheme. Environ. Qual. Manag. 2004, 14, 59–70. [Google Scholar] [CrossRef]
- Nawrocka, D.; Parker, T. Finding the connection: Environmental management systems and environmental performance. J. Clean. Prod. 2009, 17, 601–607. [Google Scholar] [CrossRef]
- Tschiggerl, K.; Wolf, P. Innovative CP networks: The case of the ÖKOPROFIT® network promoting innovative clean production solutions for 20 years. Clean Technol. Environ. Policy 2012, 14, 1029–1035. [Google Scholar] [CrossRef]
- Dixon, R.; Mousa, G.A.; Woodhead, A. The role of environmental initiatives in encouraging companies to engage in environmental reporting. Eur. Manag. J. 2005, 23, 702–716. [Google Scholar] [CrossRef]
- Bednárová, M.; Klimko, R.; Rievajová, E. From environmental reporting to environmental performance. Sustainability 2019, 11, 2549. [Google Scholar] [CrossRef]
- Hart, S.L.; Dowell, G. Invited editorial: A natural-resource-based view of the firm: Fifteen years after. J. Manag. 2011, 37, 1464–1479. [Google Scholar] [CrossRef]
- Roome, N. Developing environmental management strategies. Bus. Strategy Environ. 1992, 1, 11–24. [Google Scholar] [CrossRef]
- Aragon-Correa, J.A. Research notes. Strategic proactivity and firm approach to the natural environment. Acad. Manag. J. 1998, 41, 556–567. [Google Scholar] [CrossRef]
- Buysse, K.; Verbeke, A. Proactive environmental strategies: A stakeholder management perspective. Strategy Manag. J. 2003, 24, 453–470. [Google Scholar] [CrossRef]
- Henriques, I.; Sadorsky, P. The relationship between environmental commitment and managerial perceptions of stakeholder importance. Acad. Manag. J. 1999, 42, 87–99. [Google Scholar] [CrossRef]
- Kolk, A.; Mauser, A. The evolution of environmental management: From stage models to performance evaluation. Bus. Strategy Environ. 2002, 11, 14–31. [Google Scholar] [CrossRef]
- Garcés-Ayerbe, C.; Rivera-Torres, P.; Murillo-Luna, J.L. Stakeholder pressure and environmental proactivity: Moderating effect of competitive advantage expectations. Manag. Decis. 2012, 50, 189–206. [Google Scholar] [CrossRef]
- Ormazabal, M.; Sarriegi, J.M.; Barkemeyer, R.; Viles, E.; McAnulla, F. Evolutionary pathways of environmental management in UK companies. Corp. Soc. Responsib. Environ. Manag. 2015, 22, 169–181. [Google Scholar] [CrossRef]
- Hart, S.L. A natural-resource-based view of the firm. Acad. Manag. Rev. 1995, 20, 986–1014. [Google Scholar] [CrossRef]
- Kallio, T.J.; Nordberg, P. The evolution of organizations and natural environment discourse: Some critical remarks. Organ. Environ. 2006, 19, 439–457. [Google Scholar] [CrossRef]
- Mardani, A.; Streimikiene, D.; Zavadskas, E.; Cavallaro, F.; Nilashi, M.; Jusoh, A.; Zare, H. Application of Structural Equation Modeling (SEM) to solve environmental sustainability problems: A comprehensive review and meta-analysis. Sustainability 2017, 9, 1814. [Google Scholar] [CrossRef]
- González-Benito, J.; González-Benito, Ó. A review of determinant factors of environmental proactivity. Bus. Strategy Environ. 2006, 15, 87–102. [Google Scholar] [CrossRef]
- Freeman, R.E. Strategic Management: A Stakeholder Approach (Pitman Series in Business and Public Policy); Pitman: Boston, MA, USA, 1984; ISBN 978-0-273-01913-8. [Google Scholar]
- Mitchell, R.K.; Agle, B.R.; Wood, D.J. Toward a theory of stakeholder identification and salience: Defining the principle of who and what really counts. Acad. Manag. Rev. 1997, 22, 853–886. [Google Scholar] [CrossRef]
- Murillo-Luna, J.L.; Garcés-Ayerbe, C.; Rivera-Torres, P. Why do patterns of environmental response differ? A stakeholders’ pressure approach. Strategy Manag. J. 2008, 29, 1225–1240. [Google Scholar] [CrossRef]
- Sharma, S. Managerial interpretations and organizational context as predictors of corporate choice of environmental strategy. Acad. Manag. J. 2000, 43, 681–697. [Google Scholar] [CrossRef]
- Berman, S.L.; Wicks, A.C.; Kotha, S.; Jones, T.M. Does stakeholder orientation matter? The relationship between stakeholder management models and firm financial performance. Acad. Manag. J. 1999, 42, 488–506. [Google Scholar] [CrossRef]
- Banerjee, S.B.; Iyer, E.S.; Kashyap, R.K. Corporate environmentalism: Antecedents and influence of industry type. J. Mark. 2003, 67, 106–122. [Google Scholar] [CrossRef]
- Betts, T.K.; Wiengarten, F.; Tadisina, S.K. Exploring the impact of stakeholder pressure on environmental management strategies at the plant level: What does industry have to do with it? J. Clean. Prod. 2015, 92, 282–294. [Google Scholar] [CrossRef]
- Rueda-Manzanares, A.; Aragón-Correa, J.A.; Sharma, S. The Influence of stakeholders on the environmental strategy of service firms: The moderating effects of complexity, uncertainty and munificence. Br. J. Manag. 2008, 19, 185–203. [Google Scholar] [CrossRef]
- Destatis–Germany’s Federal Statistical Office Grunddaten der Krankenhäuser 2017. Fachserie 12: Gesundh. Reihe 6.1.1.; Statistisches Bundesamt (Destatis): Wiesbaden, Germany, 2018. [Google Scholar]
- Augurzky, B.; Engel, D.; Schmidt, C.M.; Schwierz, C. Ownership and financial sustainability of german acute care hospitals. Health Econ. 2012, 21, 811–824. [Google Scholar] [CrossRef]
- Klenk, T. Ownership change and the rise of a for-profit hospital industry in Germany. Policy Stud. 2011, 32, 263–275. [Google Scholar] [CrossRef]
- Berry, L.L.; Bendapudi, N. Health care: A fertile field for service research. J. Serv. Res. 2007, 10, 111–122. [Google Scholar] [CrossRef]
- Kuntz, L.; Pulm, J.; Wittland, M. Hospital ownership, decisions on supervisory board characteristics, and financial performance. Health Care Manag. Rev. 2016, 41, 165–176. [Google Scholar] [CrossRef]
- Hyatt, D.G.; Berente, N. Substantive or symbolic environmental strategies? Effects of external and internal normative stakeholder pressures: Stakeholder pressure and environmental strategies. Bus. Strategy Environ. 2017, 26, 1212–1234. [Google Scholar] [CrossRef]
- Henriques, I.; Sadorsky, P. The determinants of an environmentally responsive firm: An empirical approach. J. Environ. Econ. Manag. 1996, 30, 381–395. [Google Scholar] [CrossRef]
- Delmas, M.; Toffel, M.W. Stakeholders and environmental management practices: An institutional framework. Bus. Strategy Environ. 2004, 13, 209–222. [Google Scholar] [CrossRef]
- Bolton, R.N. Pretesting questionnaires: Content analyses of respondents concurrent verbal protocols. Mark. Sci. 1993, 12, 280–303. [Google Scholar] [CrossRef]
- Ericsson, K.A.; Simon, H.A. Protocol Analysis: Verbal Reports as Data; The MIT Press: Cambridge, MA, USA, 1984. [Google Scholar]
- Sprengel, D.C.; Busch, T. Stakeholder engagement and environmental strategy—The case of climate change. Bus. Strategy Environ. 2011, 20, 351–364. [Google Scholar] [CrossRef]
- Saunders, M.N.K.; Lewis, P.; Thornhill, A. Research Methods for Business Students, 7th ed.; Pearson Education: New York, NY, USA, 2015; ISBN 978-1-292-01662-7. [Google Scholar]
- Armstrong, J.S.; Overton, T.S. Estimating nonresponse bias in mail surveys. J. Mark. Res. 1977, 14, 396–402. [Google Scholar] [CrossRef]
- Walesiak, M.; Dudek, A. Finding groups in ordinal data: An examination of some clustering procedures. In Classification as a Tool for Research; Locarek-Junge, H., Weihs, C., Eds.; Springer: Berlin/Heidelberg, Germany, 2010; pp. 185–192. ISBN 978-3-642-10744-3. [Google Scholar]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson New Internat, Ed.; Pearson: Harlow, UK, 2014; ISBN 978-1-292-02190-4. [Google Scholar]
- Ramus, C.A.; Montiel, I. When are corporate environmental policies a form of greenwashing? Bus. Soc. 2005, 44, 377–414. [Google Scholar] [CrossRef]
- Delmas, M.A.; Burbano, V.C. The drivers of greenwashing. Calif. Manag. Rev. 2011, 54, 64–87. [Google Scholar] [CrossRef]
- Lyon, T.P.; Maxwell, J.W. Greenwash: Corporate environmental disclosure under threat of audit. J. Econ. Manag. Strategy 2011, 20, 3–41. [Google Scholar] [CrossRef]
- Walker, K.; Wan, F. The harm of symbolic actions and green-washing: Corporate actions and communications on environmental performance and their financial implications. J. Bus. Ethics 2011, 109, 227–242. [Google Scholar] [CrossRef]
- Seifert, C.; Krannich, T.; Guenther, E. Gearing up sustainability thinking and reducing the bystander effect —A case study of wastewater treatment plants. J. Environ. Manag. 2019, 231, 155–165. [Google Scholar] [CrossRef] [PubMed]
| Environmental Management Performance | |
| Environmental policy | Any overarching organizational philosophy or principle regarding environmental issues |
| Environmental objectives | Any organizational targets or objectives regarding environmental issues |
| Environmental processes | Considering environmental issues within operations, e.g., applying environmental criteria or life-cycle assessment |
| Organizational structures | Allocation of responsibilities and tasks, employee education/training, ISO 14001 or EMAS certification |
| Environmental monitoring | Collection and analysis of environmental indicators |
| Environmental Operational Performance | |
| Material consumption | Any material that is utilized |
| Energy consumption | Any energy that is utilized |
| Water consumption | Any freshwater that is utilized |
| Wastes | Any undesired outputs emerging |
| Emission into air | Any releases into air, such as smell or CO2 |
| Emission into water | Any releases into water, esp. after wastewater treatment |
| Author(s) | Categories of Organizational EM Approaches | Derived From | Empirical Context | EM Elements Considered in Empirical Analysis | ||
|---|---|---|---|---|---|---|
| Theory | Empirical Data | |||||
| Roome [43] |
| X | - | - | ||
| Hart [50] |
| X | - | - | ||
| Aragón-Correa [44] |
| x | 105 Spanish companies from various sectors |
| ||
| Henriques and Sadorsky [46] |
| x | 750 Canadian firms from various sectors |
| ||
| Buysse and Verbeke [45] |
| x | 450 Belgian companies from various sectors |
| ||
| Hart and Dowell [42] |
| X | - | - | ||
| Job Position | Number | Percentage |
|---|---|---|
| Managing director/assistance | 66/6 | 62.6% |
| Environmental or sustainability manager | 16 | 13.9% |
| Waste manager | 4 | 3.5% |
| Energy manager | 4 | 3.5% |
| Facility or technical manager | 9 | 7.8% |
| Quality manager | 4 | 3.5% |
| Others | 6 | 5.2% |
| Average years of experience in… | ||
| this hospital | 12.2 | |
| this position (this and other hospitals) | 11.6 | |
| this hospital and this position | 8.2 | |
| Educational background | ||
| Business and management | 48 | 41.7% |
| Engineering/natural sciences | 32 | 27.8% |
| Medicine | 4 | 3.5% |
| Others | 12 | 10.5% |
| No answer | 19 | 16.5% |
| Sex | ||
| Male | 76 | 66.1% |
| Female | 29 | 25.2% |
| No answer | 10 | 8.7% |
| Age | ||
| 20–29 | 3 | 2.6% |
| 30–39 | 16 | 13.9% |
| 40–49 | 29 | 25.2% |
| 50–59 | 50 | 43.5% |
| >60 | 12 | 10.4% |
| No answer | 5 | 4.4% |
| Clusters | Total Average | Chi-Square | |||
|---|---|---|---|---|---|
| 1 Traditionalists | 2 Pragmatists | 3 Environmentalists | |||
| EM element | |||||
| Policy | 1.81 [3] | 1.31 [3] | 5.29 [1,2] | 3.12 | 74.92 *** |
| Objectives | 0.52 [2,3] | 1.72 [1,3] | 4.12 [1,2] | 2.46 | 55.69 *** |
| Processes | 1.59 [2,3] | 4.08 [1,3] | 4.73 [1,2] | 3.77 | 46.99 *** |
| Structures | 1.59 [2,3] | 4.10 [1] | 4.63 [1] | 3.74 | 47.81 *** |
| Monitoring | 1.33 [2,3] | 3.69 [1,3] | 4.69 [1,2] | 3.57 | 57.04 *** |
| Average | 1.37 | 2.98 | 4.69 | ||
| Number of cases (% of sample) | 27 (23.5 %) | 39 (33.9 %) | 49 (42.6 %) | ||
| Stakeholder Group | Clusters | Total Average | Chi-Square | ||
|---|---|---|---|---|---|
| 1 Traditionalists | 2 Pragmatists | 3 Environmentalists | |||
| Internal | |||||
| Hospital management | 3.33 [3] | 3.69 [3] | 4.20 [1,2] | 3.83 | 8.17 * |
| Employees | 3.41 | 3.46 | 3.43 | 3.43 | 0.06 |
| Owner | 2.89 [3] | 2.92 [3] | 3.73 [1,2] | 3.26 | 8.73 * |
| External | |||||
| Regulators | 3.70 | 3.56 | 3.96 | 3.77 | 1.74 |
| Patients | 2.81 | 2.87 | 2.67 | 2.77 | 0.65 |
| Media | 2.37 | 2.38 | 2.78 | 2.55 | 2.48 |
| Relatives of patients | 2.63 | 2.49 | 2.43 | 2.50 | 0.37 |
| Local interest groups | 2.11 | 2.23 | 2.73 | 2.42 | 4.81 |
| Environmental NGOs | 1.81 [3] | 2.15 | 2.63 [1] | 2.28 | 4.56 |
| Hospital associations | 1.96 [3] | 2.05 [3] | 2.61 [1,2] | 2.27 | 7.32 * |
| Insurance companies | 2.15 | 2.03 | 2.51 | 2.26 | 2.46 |
| Suppliers | 2.04 | 1.95 | 2.31 | 2.12 | 3.50 |
| Competitors | 1.70 | 1.90 | 2.10 | 1.94 | 0.94 |
| Health insurance companies | 1.89 | 1.56 | 1.98 | 1.82 | 3.11 |
| Banks | 1.48 | 1.41 | 1.78 | 1.58 | 2.46 |
| Average | 2.42 | 2.44 | 2.79 | 2.59 | |
| Characteristics | Clusters | Total Avg. | F Statistic | Chi- Square | ||
|---|---|---|---|---|---|---|
| 1 Traditionalists | 2 Pragmatists | 3 Environmentalists | ||||
| Ownership | ||||||
| Public (n = 49) | 10.2 % | 36.7 % | 53.1 % | |||
| Voluntary charitable hospitals (n = 41) | 24.4 % | 39.0 % | 36.6 % | |||
| Private (n = 25) | 20.0 % | 48.0 % | 32.0 % | |||
| Size | ||||||
| Average number of employees | 999 | 1696 | 1806 | 1579 | 1.06 | |
| Performance † | ||||||
| Return on assets (n = 73) | 3.13 | 3.04 | 3.45 | 3.23 | 2.32 | |
| Return on sales (n = 73) | 3.07 | 3.07 | 3.43 | 3.22 | 2.01 | |
| Employee growth (n = 83) | 2.89 | 3.22 | 3.45 | 3.24 | 3.62 | |
| Sales growth (n = 78) | 3.00 | 3.13 | 3.38 | 3.21 | 1.52 | |
| Asset growth (n = 70) | 2.67 [3] | 3.08 | 3.33 [1] | 3.10 | 4.74 | |
| Debt-to-equity (n = 73) | 2.29 | 2.50 | 2.07 | 2.27 | 1.66 | |
| Innovation performance (n = 77) | 2.76 [2,3] | 3.41 [1] | 3.71 [1] | 3.39 | 14.59 ** | |
| Overall organizational performance (n = 77) | 3.67 | 3.55 | 4.00 | 3.75 | 3.16 | |
| Bed occupancy rate (n = 82) | 3.78 | 3.31 [3] | 3.94 [2] | 3.68 | 8.96 * | |
| Average performance | 3.03 | 3.15 | 3.42 | 3.23 | ||
| VEI | ||||||
| None (n = 86) | 31.4 % | 39.5 % | 29.1 % | |||
| ISO (n = 5) | 0.0 % | 0.0 % | 100.0 % | |||
| EMAS (n = 16) | 0.0 % | 6.3 % | 93.7 % | |||
| Others (n = 18) | 5.6 % | 22.2 % | 72.2 % | |||
| Environmental training | ||||||
| Number of included environmental issues | 0.67 [2,3] | 1.87 [1,3] | 3.29 [1,2] | 39.46 *** | ||
| No. of cases (% of sample) | 27 (23.5 %) | 39 (33.9 %) | 49 (42.6 %) | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seifert, C.; Damert, M.; Guenther, E. Environmental Management in German Hospitals—A Classification of Approaches. Sustainability 2020, 12, 4428. https://doi.org/10.3390/su12114428
Seifert C, Damert M, Guenther E. Environmental Management in German Hospitals—A Classification of Approaches. Sustainability. 2020; 12(11):4428. https://doi.org/10.3390/su12114428
Chicago/Turabian StyleSeifert, Christin, Matthias Damert, and Edeltraud Guenther. 2020. "Environmental Management in German Hospitals—A Classification of Approaches" Sustainability 12, no. 11: 4428. https://doi.org/10.3390/su12114428
APA StyleSeifert, C., Damert, M., & Guenther, E. (2020). Environmental Management in German Hospitals—A Classification of Approaches. Sustainability, 12(11), 4428. https://doi.org/10.3390/su12114428





