Effects of Changing Air Temperature at Different Sleep Stages on the Subjective Evaluation of Sleep Quality
Abstract
1. Introduction
2. Methods
2.1. IoT Sensors
2.2. Transition of Setpoint Temperatures
2.3. Study Experiment
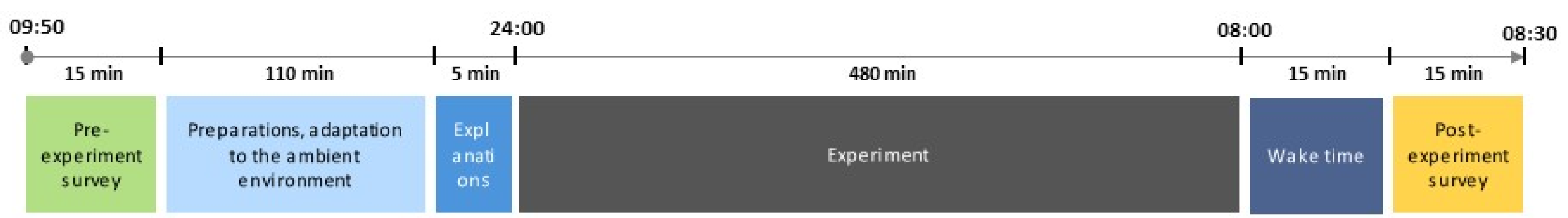
2.3.1. Experimental Conditions and Procedures
2.3.2. Subjects and Clothing
2.4. Subjective Questionnaires
2.5. Statistical Analysis
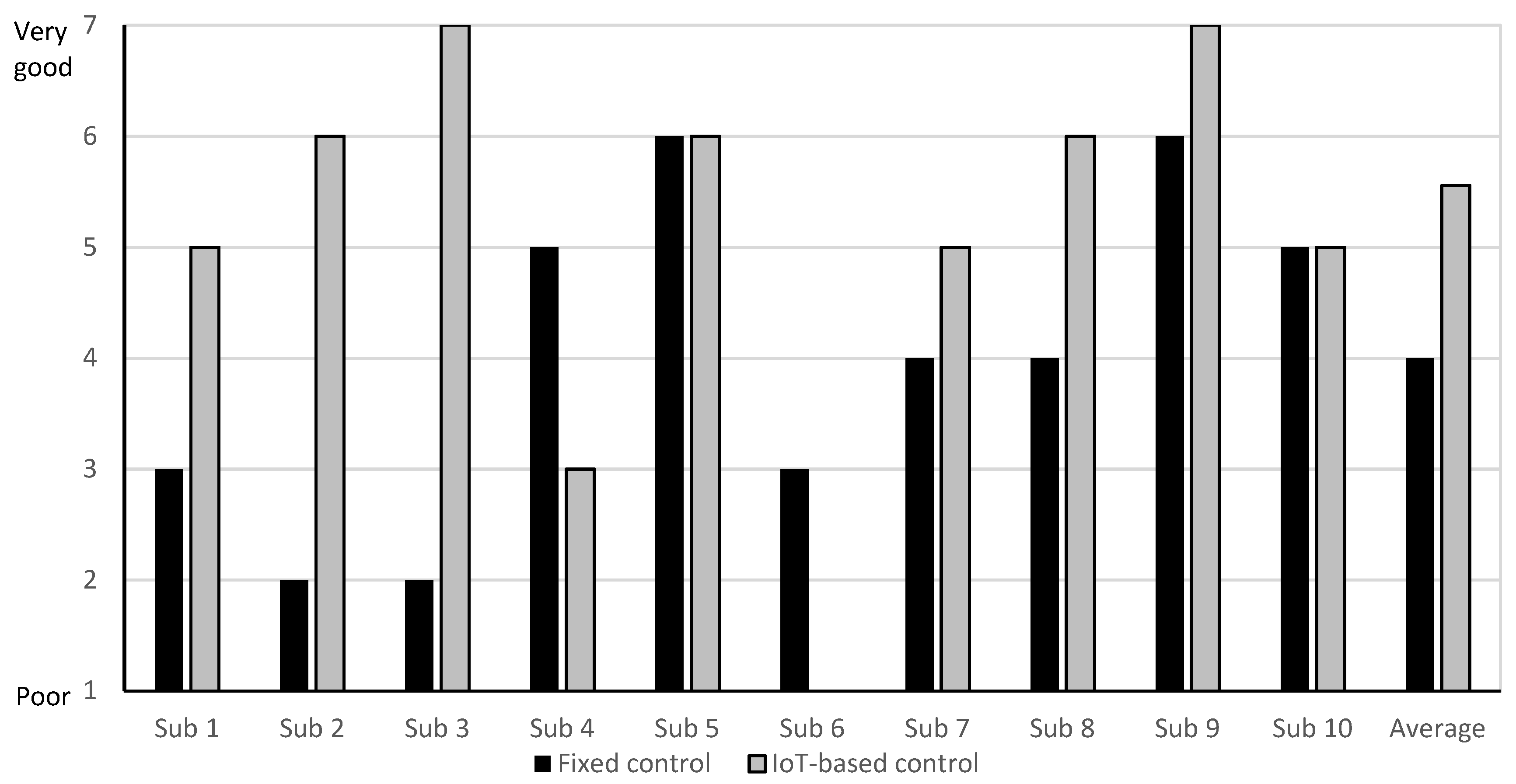
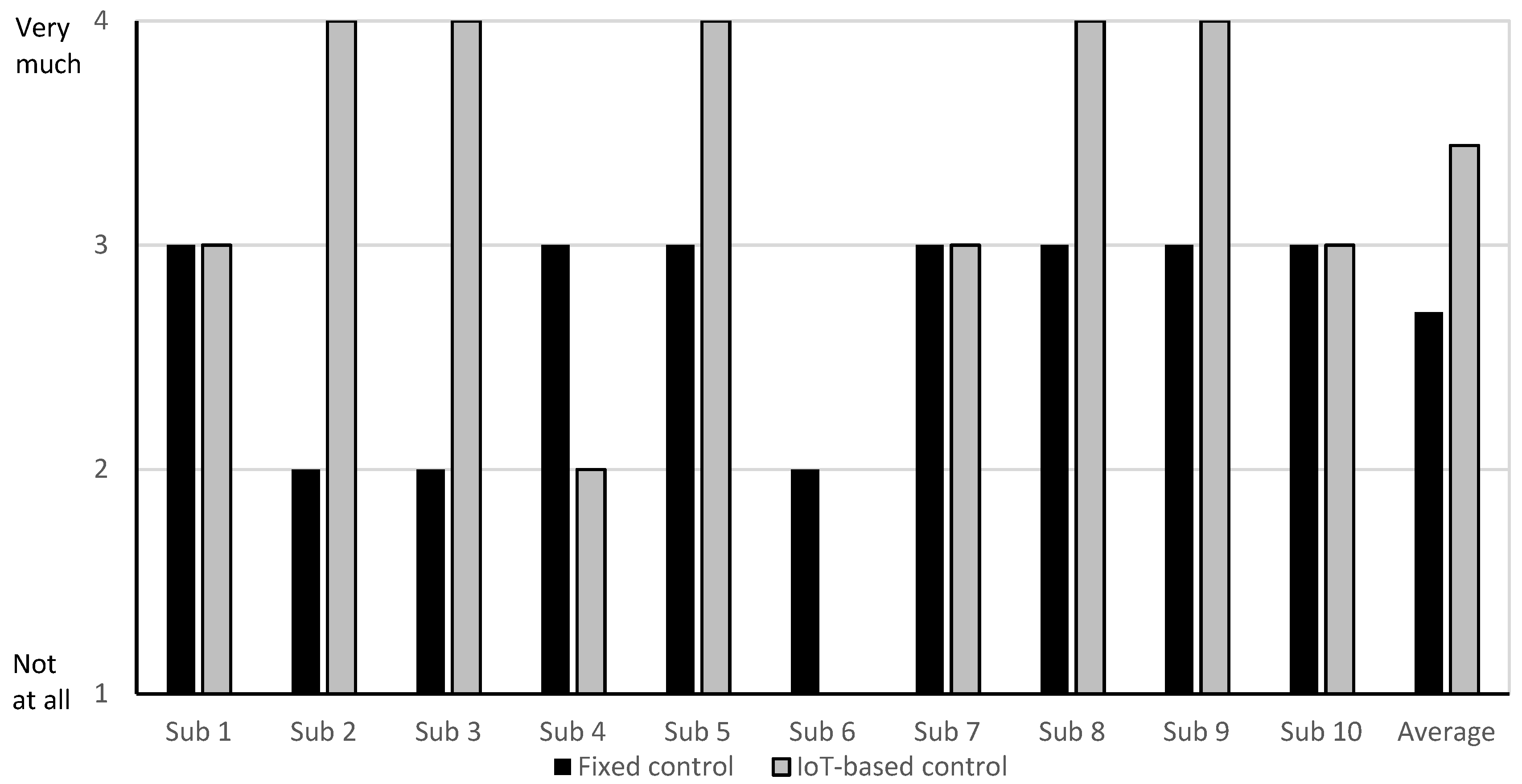
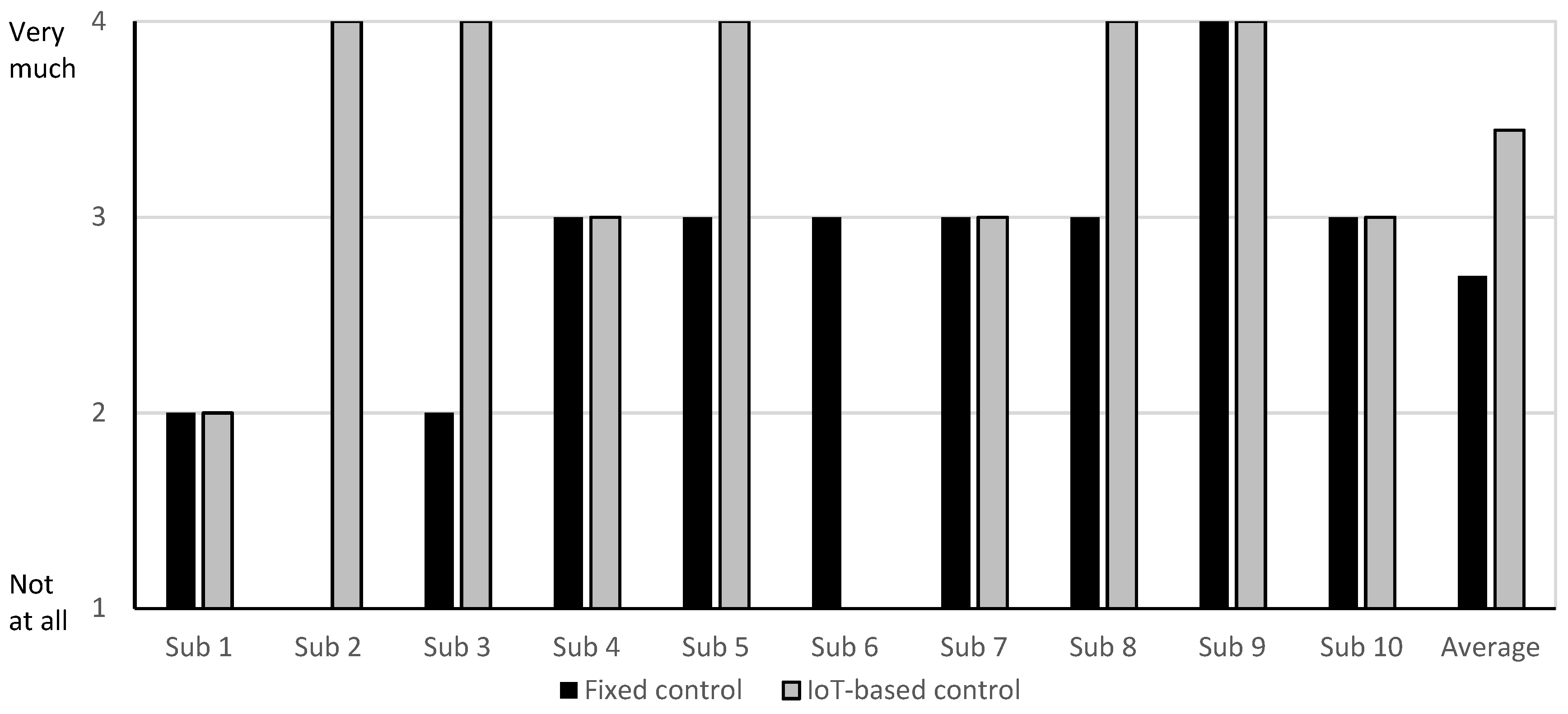
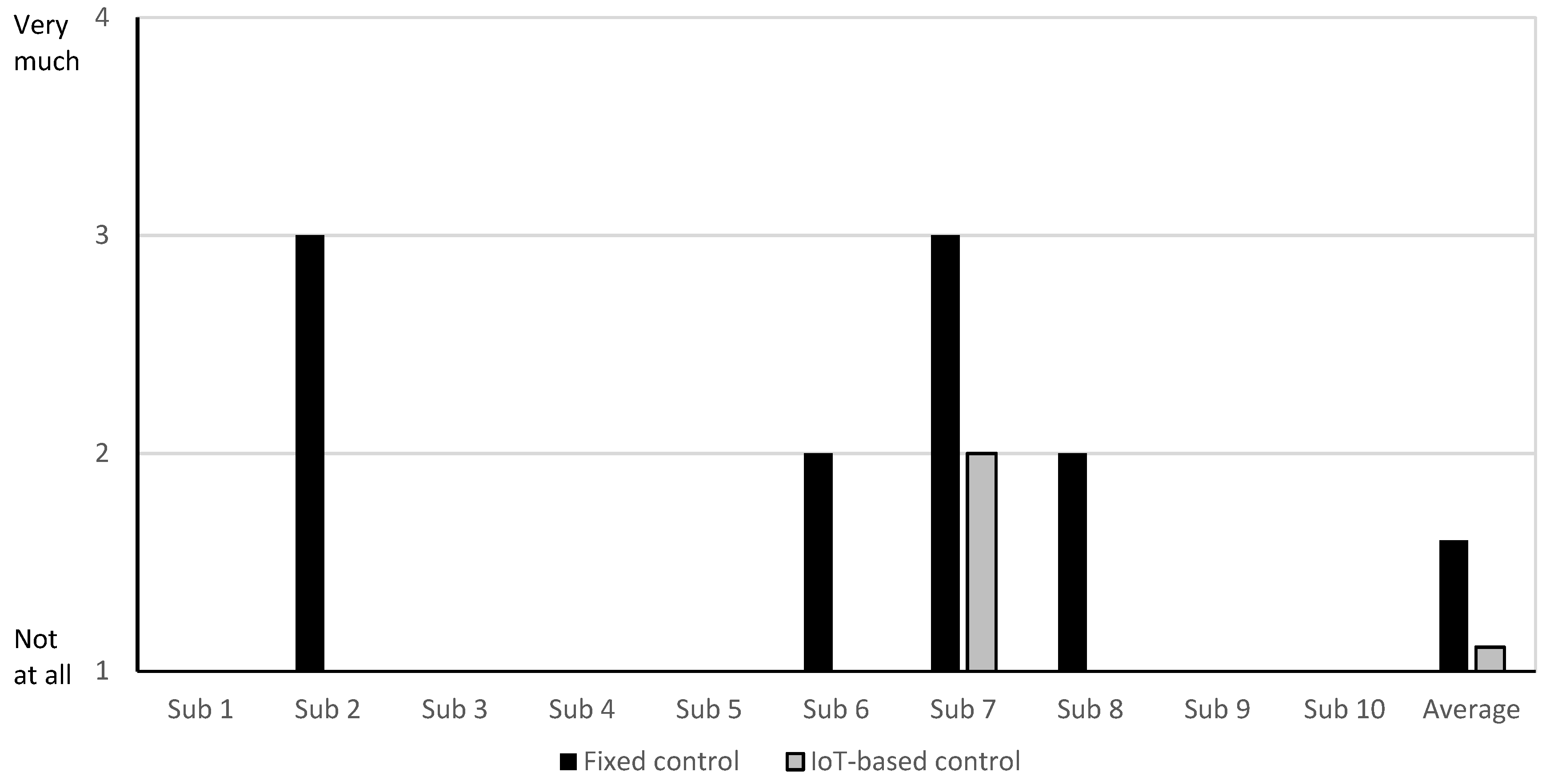
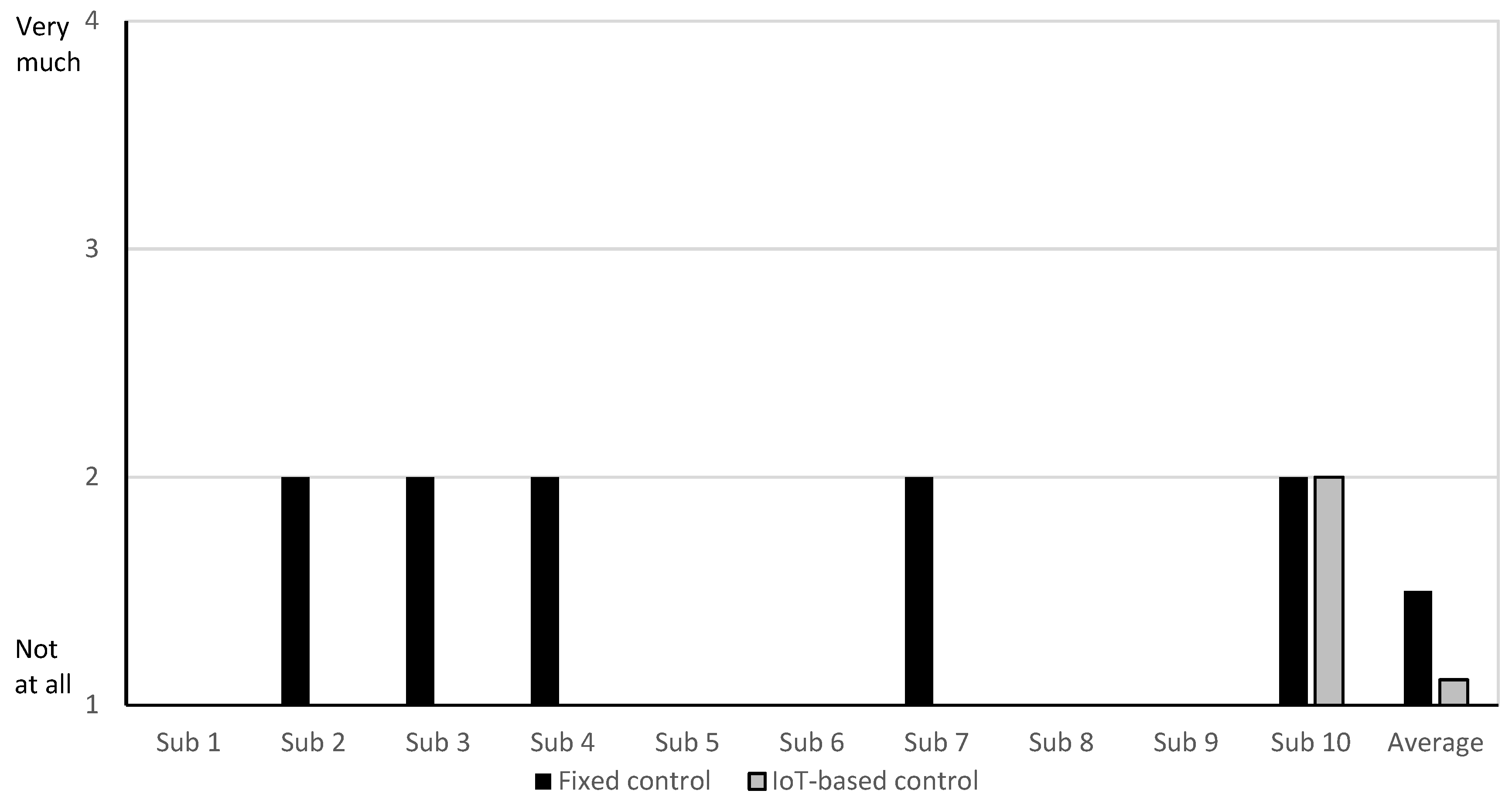
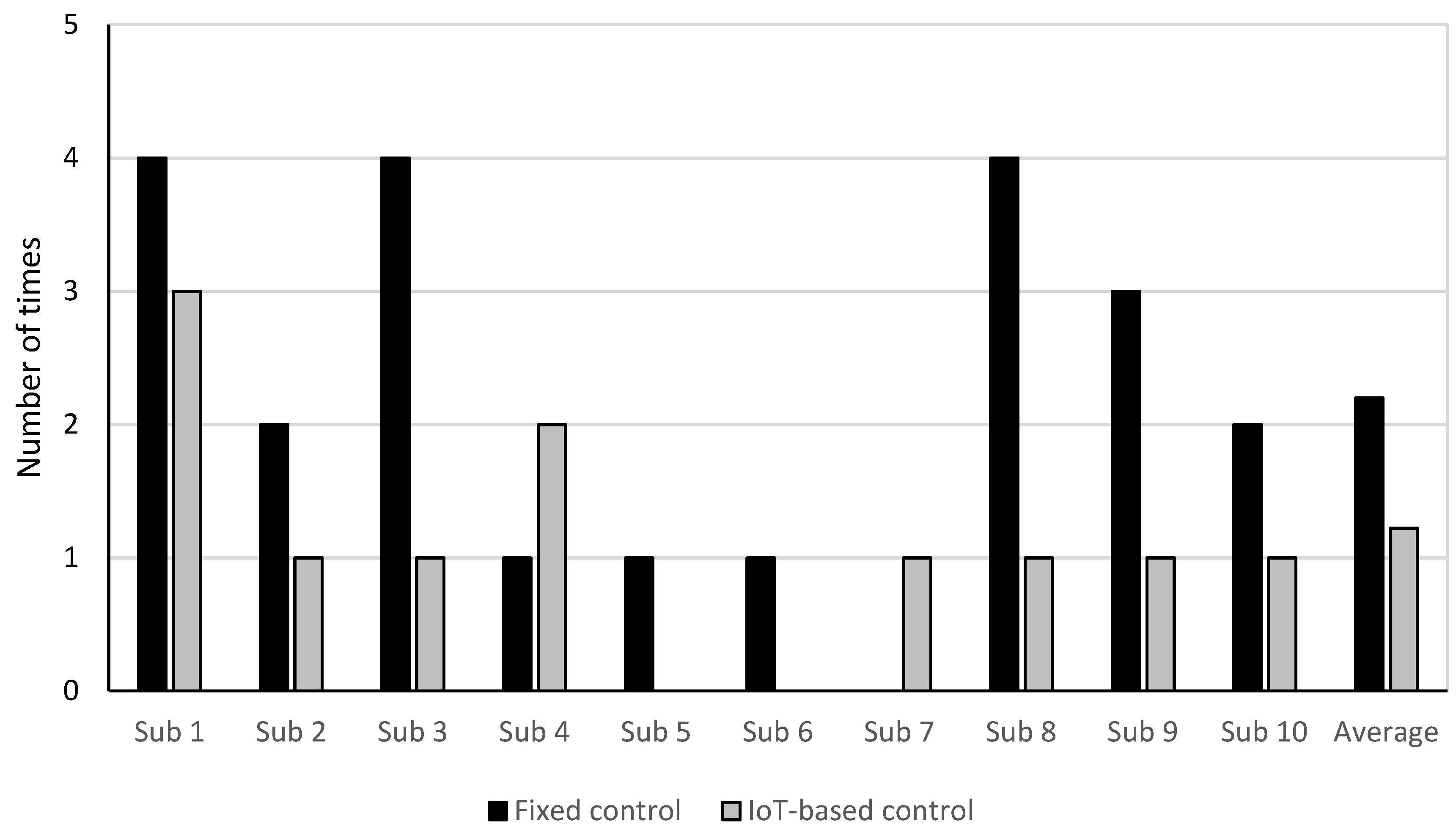
3. Results
4. Discussion and Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- João, K.A.; de Jesus, S.N.; Carmo, C.; Pinto, P. The impact of sleep quality on the mental health of a non-clinical population. Sleep Med. 2018, 46, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Edéll-Gustafsson, U.M.; Kritz, E.I.; Bogren, I.K. Self-reported sleep quality, strain and health in relation to perceived working conditions in females. Scand. J. Caring Sci. 2002, 16, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Bryant, P.A.; Trinder, J.; Curtis, N. Sick and tired: Does sleep have a vital role in the immune system? Nat. Rev. Immunol. 2004, 4, 457–467. [Google Scholar] [CrossRef] [PubMed]
- Telzer, E.H.; Fuligni, A.J.; Lieberman, M.D.; Galván, A. The effects of poor quality sleep on brain function and risk-taking in adolescence. Neuroimage 2013, 71, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Leger, D.; Poursain, B.; Neubauer, D.; Uchiyama, M. An international survey of sleeping problems in the general population. Curr. Med Res. Opin. 2008, 24, 307–317. [Google Scholar] [CrossRef] [PubMed]
- Carskadon, M.A.; Dement, W.C. Normal human sleep: An overview. Princ. Pract. Sleep Med. 2005, 4, 13–23. [Google Scholar]
- Potter, G.D.; Skene, D.J.; Arendt, J.; Cade, J.E.; Grant, P.J.; Hardie, L.J. Circadian rhythm and sleep disruption: Causes, metabolic consequences, and countermeasures. Endocr. Rev. 2016, 37, 584–608. [Google Scholar] [CrossRef] [PubMed]
- Refinetti, R.; Menaker, M. The circadian rhythm of body temperature. Physiol. Behav. 1992, 51, 613–637. [Google Scholar] [CrossRef]
- Parmeggiani, P.L. Interaction between sleep and thermoregulation: An aspect of the control of behavioral states. Sleep 1986, 10, 426–435. [Google Scholar] [CrossRef]
- Liu, Y.; Song, C.; Wang, Y.; Wang, D.; Liu, J. Experimental study and evaluation of the thermal environment for sleeping. Build. Environ. 2014, 82, 546–555. [Google Scholar] [CrossRef]
- CIBSE. Guide A. Environmental Design; The Chartered Institution of Building Services Engineers: London, UK, 2006. [Google Scholar]
- British Standards Institution. Indoor Environmental Input Parameters for Design and Assessment of Energy Performance of Buildings Addressing Indoor Air Quality, Thermal Environment, Lighting and Acoustics; CEN: Brussels, Belgium, 2012. [Google Scholar]
- Lin, Z.; Deng, S. A questionnaire survey on sleeping thermal environment and bedroom air conditioning in high-rise residences in Hong Kong. Energy Build. 2006, 38, 1302–1307. [Google Scholar] [CrossRef]
- Ekasiwi, S.N.N.; Majid, N.H.A.; Hokoi, S.; Oka, D.; Takagi, N.; Uno, T. Field survey of air conditioner temperature settings in hot, humid climates, part 1: Questionnaire results on use of air conditioners in houses during sleep. J. Asian Archit. Build. Eng. 2013, 12, 141–148. [Google Scholar] [CrossRef]
- Lan, L.; Tsuzuki, K.; Liu, Y.F.; Lian, Z.W. Thermal environment and sleep quality: A review. Energy Build. 2017, 149, 101–113. [Google Scholar] [CrossRef]
- Kushida, C.A.; Littner, M.R.; Morgenthaler, T.; Alessi, C.A.; Bailey, D.; Coleman, J., Jr.; Friedman, L.; Hirshkowitz, M.; Kapen, S.; Kramer, M.; et al. Practice parameters for the indications for polysomnography and related procedures: An update for 2005. Sleep 2005, 28, 499–523. [Google Scholar] [CrossRef] [PubMed]
- Morgenthaler, T.; Alessi, C.; Friedman, L.; Owens, J.; Kapur, V.; Boehlecke, B.; Brown, T.; Chesson, A., Jr.; Coleman, J.; Lee-Chiong, T.; et al. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: An update for 2007. Sleep 2007, 30, 519–529. [Google Scholar] [CrossRef] [PubMed]
- Keenan, S.; Hirshkowitz, M. Monitoring and staging human sleep. Princ. Pract. Sleep Med. 2011, 5, 1602–1609. [Google Scholar]
- Stojkoska, B.L.; Trivodaliev, K.V. A review of Internet of Things for smart home: Challenges and solutions. J. Clean. Prod. 2017, 140, 1454–1464. [Google Scholar] [CrossRef]
- Fanger, P.O. Thermal comfort. Analysis and applications in environmental engineering. In Thermal Comfort. Analysis and Applications in Environmental Engineering; McGrew-Hill: New York, NY, USA, 1970. [Google Scholar]
- Alfano, F.R.D.A.; Olesen, B.W.; Palella, B.I. Povl Ole Fanger’s impact ten years later. Energy Build. 2017, 152, 243–249. [Google Scholar] [CrossRef]
- Schmidt, C.; Wölki, D.; Grün, G.; van Treeck, C. Accuracy of mean skin temperature calculations and measurements in thermal comfort-related assessment. In Proceedings of the Windsor Conference, London, UK, 12–15 April 2012. [Google Scholar]
- Lan, L.; Pan, L.; Lian, Z.; Huang, H.; Lin, Y. Experimental study on thermal comfort of sleeping people at different air temperatures. Build. Environ. 2014, 73, 24–31. [Google Scholar] [CrossRef]
- Lin, Z.; Deng, S. A study on the thermal comfort in sleeping environments in the subtropics—Developing a thermal comfort model for sleeping environments. Build. Environ. 2008, 43, 70–81. [Google Scholar] [CrossRef]
- Karacan, I.; Thornby, J.I.; Anch, A.M.; Williams, R.L.; Perkins, H.M. Effects of high ambient temperature on sleep in young men. Aviat. Spaceand Environ. Med. 1978, 49, 855–860. [Google Scholar]
- Sewitch, D.E.; Kittrell, E.M.W.; Kupfer, D.J.; Reynolds, C.F., III. Body temperature and sleep architecture in response to a mild cold stress in women. Physiol. Behav. 1986, 36, 951–957. [Google Scholar] [CrossRef]
- Macpherson, R.K. Thermal stress and thermal comfort. Ergonomics 1973, 16, 611–622. [Google Scholar] [CrossRef] [PubMed]
- Di Nisi, J.; Ehrhart, J.; Galeou, M.; Libert, J.P. Influence of repeated passive body heating on subsequent night sleep in humans. Eur. J. Appl. Physiol. Occup. Physiol. 1989, 59, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Dewasmes, G.; Signoret, P.; Nicolas, A.; Ehrhart, J.; Muzet, A. Advances of human core temperature minimum and maximal paradoxical sleep propensity by ambient thermal transients. Neurosci. Lett. 1996, 215, 25–28. [Google Scholar] [CrossRef]
- Palca, J.W.; Walker, J.M.; Berger, R.J. Thermoregulation, metabolism, and stages of sleep in cold-exposed men. J. Appl. Physiol. 1986, 61, 940–947. [Google Scholar] [CrossRef] [PubMed]
- Dewasmes, G.; Loos, N.; Candas, V.; Muzet, A. Effects of a moderate nocturnal cold stress on daytime sleep in humans. Eur. J. Appl. Physiol. 2003, 89, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.; Lian, Z.; Lan, L. Investigation of sleep quality under different temperatures based on subjective and physiological measurements. HVACR Res. 2012, 18, 1030–1043. [Google Scholar]
- Tsuzuki, K.; Okamoto-Mizuno, K.; Mizuno, K.; Iwaki, T. Effects of airflow on body temperatures and sleep stages in a warm humid climate. Int. J. Biometeorol. 2008, 52, 261–270. [Google Scholar] [CrossRef] [PubMed]
- Kräuchi, K. The human sleep–wake cycle reconsidered from a thermoregulatory point of view. Physiol. Behav. 2007, 90, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Kräuchi, K.; Deboer, T. Body temperatures, sleep, and hibernation. In Principles and Practice of Sleep Medicine; Saunders: Philadelphia, PA, USA, 2011; pp. 323–334. [Google Scholar]
- Van Someren, E.J. Mechanisms and functions of coupling between sleep and temperature rhythms. Prog. Brain Res. 2006, 153, 309–324. [Google Scholar] [PubMed]
- Murphy, P.J.; Campbell, S.S. Nighttime drop in body temperature: A physiological trigger for sleep onset? Sleep 1997, 20, 505–511. [Google Scholar] [CrossRef]
- Wakamura, T.; Tokura, H. Circadian rhythm of rectal temperature in humans under different ambient temperature cycles. J. Therm. Biol. 2002, 27, 439–447. [Google Scholar] [CrossRef]
- Lan, L.; Lian, Z.W.; Lin, Y.B. Comfortably cool bedroom environment during the initial phase of the sleeping period delays the onset of sleep in summer. Build. Environ. 2016, 103, 36–43. [Google Scholar] [CrossRef]
- Raymann, R.J.; Swaab, D.F.; Van Someren, E.J. Skin temperature and sleep-onset latency: Changes with age and insomnia. Physiol. Behav. 2007, 90, 257–266. [Google Scholar] [CrossRef] [PubMed]
- VanSomeren, E.J. More than a marker: Interaction between the circadian regulation of temperature and sleep, age-related changes, and treatment possibilities. Chronobiol. Int. 2000, 17, 313–354. [Google Scholar] [CrossRef]
- Okamoto-Mizuno, K.; Tsuzuki, K. Effects of season on sleep and skin temperature in the elderly. Int. J. Biometeorol. 2010, 54, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Raymann, R.J.; Swaab, D.F.; Van Someren, E.J. Skin deep: Enhanced sleep depth by cutaneous temperature manipulation. Brain 2008, 131, 500–513. [Google Scholar] [CrossRef] [PubMed]
- Bach, V.; Telliez, F.; Libert, J.P. The interaction between sleep and thermoregulation in adults and neonates. Sleep Med. Rev. 2002, 6, 481–492. [Google Scholar] [CrossRef] [PubMed]
- Kräuchi, K. How Is the Circadian Rhythm of Core Body Temperature Regulated? Springer: Berlin/Heidelberg, Germany, 2002; pp. 147–149. [Google Scholar]
- Zulley, J.; Wever, R.; Aschoff, J. The dependence of onset and duration of sleep on the circadian rhythm of rectal temperature. Pflügers Arch. 1981, 391, 314–318. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Kavuru, M. Sleep and metabolism: An overview. Int. J. Endocrinol. 2010, 2010, 270832. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Krystal, A.D.; Edinger, J.D. Measuring sleep quality. Sleep Med. 2008, 9, S10–S17. [Google Scholar] [CrossRef]
- Woolson, R.F. Wilcoxon signed-rank test. In Wiley Encyclopedia of Clinical Trials; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2007; pp. 1–3. [Google Scholar]
- Howell, W.H. A contribution to the physiology of sleep, based upon plethysmographic experiments. J. Exp. Med. 1897, 2, 313. [Google Scholar] [CrossRef] [PubMed]
- Roussel, B.; Turrillot, P.; Kitahama, K. Effect of ambient temperature on the sleep-waking cycle in two strains of mice. Brain Res. 1984, 294, 67–73. [Google Scholar] [CrossRef]
- Morairty, S.R.; Szymusiak, R.; Thomson, D.; McGinty, D.J. Selective increases in non-rapid eye movement sleep following whole body heating in rats. Brain Res. 1993, 617, 10–16. [Google Scholar] [CrossRef]
- Djongyang, N.; Tchinda, R.; Njomo, D. Thermal comfort: A review paper. Renew. Sustain. Energy Rev. 2010, 14, 2626–2640. [Google Scholar] [CrossRef]
- Lan, L.; Lian, Z.W.; Qian, X.L.; Dai, C.Z. The effects of programmed air temperature changes on sleep quality and energy saving in bedroom. Energy Build. 2016, 129, 207–214. [Google Scholar] [CrossRef]
- Wang, Z.; de Dear, R.; Luo, M.; Lin, B.; He, Y.; Ghahramani, A.; Zhu, Y. Individual difference in thermal comfort: A literature review. Build. Environ. 2018, 138, 181–193. [Google Scholar] [CrossRef]


| Literature | Neutral Temperature [°C] | Insulation Level | Season | Parameter |
|---|---|---|---|---|
| Karacan et al., 1978 [25] | 22.2 | Light sheet, sleeping apparel, blanket | NA | Air temperature |
| Dewasmes et al., 1996 [29] | 29 | Naked | NA | Air temperature |
| Palca, 1986 [30] | 29 | Naked | NA | Air temperature |
| Dewasmes et al., 2003 [31] | 25 | Cotton t-shirt, pajama pants, cotton sheet and wool blanket | NA | Air temperature |
| Pan et al., 2012 [32] | 23 | Long sleeved sleep wear, quilt | Winter | Air temperature |
| Tzuzuki et al., 2008 [33] | 26 | Short pajamas, cotton sheet and cotton blanket | Summer | Air temperature |
| Lan et al., 2014 [23] | 26 | Short sleeved sleep wear, blanket | Summer | Air temperature |
| Questions | Score | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. How well did you sleep? | 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||||
| Poor | Very good | ||||||||||
| 2. Did you sleep well? | 1 | 2 | 3 | 4 | |||||||
| Not at all | Very much | ||||||||||
| 3. Did you have deep sleep? | 1 | 2 | 3 | 4 | |||||||
| Not at all | Very much | ||||||||||
| 4. Did you have difficulty in falling asleep? | 1 | 2 | 3 | 4 | |||||||
| Not at all | Very much | ||||||||||
| 5. Did you have difficulty staying asleep? | 1 | 2 | 3 | 4 | |||||||
| Not at all | Very much | ||||||||||
| 6. Do you feel refreshed after sleeping? | 1 | 2 | 3 | 4 | |||||||
| Not at all | Very much | ||||||||||
| 7. How many times did you wake up during the night? | 0 | 1 | 2 | 3 | 4 | 5 | |||||
| Never | 5 times | ||||||||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ngarambe, J.; Yun, G.Y.; Lee, K.; Hwang, Y. Effects of Changing Air Temperature at Different Sleep Stages on the Subjective Evaluation of Sleep Quality. Sustainability 2019, 11, 1417. https://doi.org/10.3390/su11051417
Ngarambe J, Yun GY, Lee K, Hwang Y. Effects of Changing Air Temperature at Different Sleep Stages on the Subjective Evaluation of Sleep Quality. Sustainability. 2019; 11(5):1417. https://doi.org/10.3390/su11051417
Chicago/Turabian StyleNgarambe, Jack, Geun Young Yun, Kisup Lee, and Yeona Hwang. 2019. "Effects of Changing Air Temperature at Different Sleep Stages on the Subjective Evaluation of Sleep Quality" Sustainability 11, no. 5: 1417. https://doi.org/10.3390/su11051417
APA StyleNgarambe, J., Yun, G. Y., Lee, K., & Hwang, Y. (2019). Effects of Changing Air Temperature at Different Sleep Stages on the Subjective Evaluation of Sleep Quality. Sustainability, 11(5), 1417. https://doi.org/10.3390/su11051417






