Developing Sustainable Healthcare Systems in Developing Countries: Examining the Role of Barriers, Enablers and Drivers on Knowledge Management Adoption
Abstract
1. Introduction
2. Literature Review
2.1. Knowledge Management
2.2. The Need for KM in the Healthcare of Pakistan
2.3. Knowledge Management Barriers to Healthcare
2.4. Knowledge Management Enablers of Healthcare
2.5. Knowledge Management Drivers of Healthcare
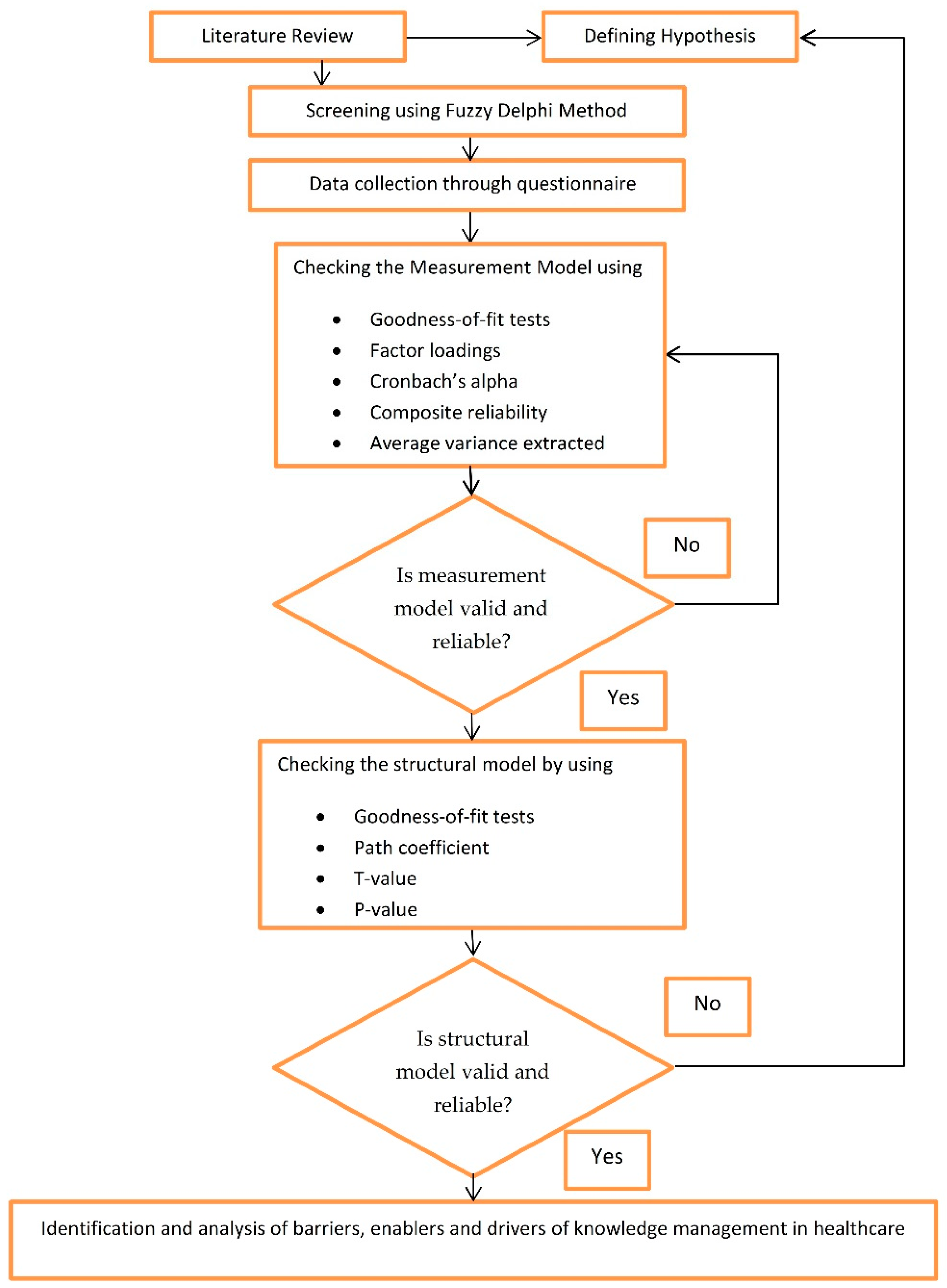
3. Research Methodology
3.1. Fuzzy Delphi Method (FDM)
- (1)
- Distribute the questionnaire and obtain response and preference for each barrier, enabler or driver through TFNs.
- (2)
- At the second step, fuzzy weights obtained through TFNs were transformed into one single value by utilizing the center of gravity technique:(Where is the threshold criteria for rejection or selection of the appropriate item, represent the minimum value of TFNs, shows the geometric mean, and represent the maximum value of TFNs).
- (3)
- After two rounds, facilitator adopted the questions according to the threshold criteria that were the part of final questionnaires distributed in respondents.
3.2. Data Collection
3.3. Structural Equation Modeling (SEM)
4. Results
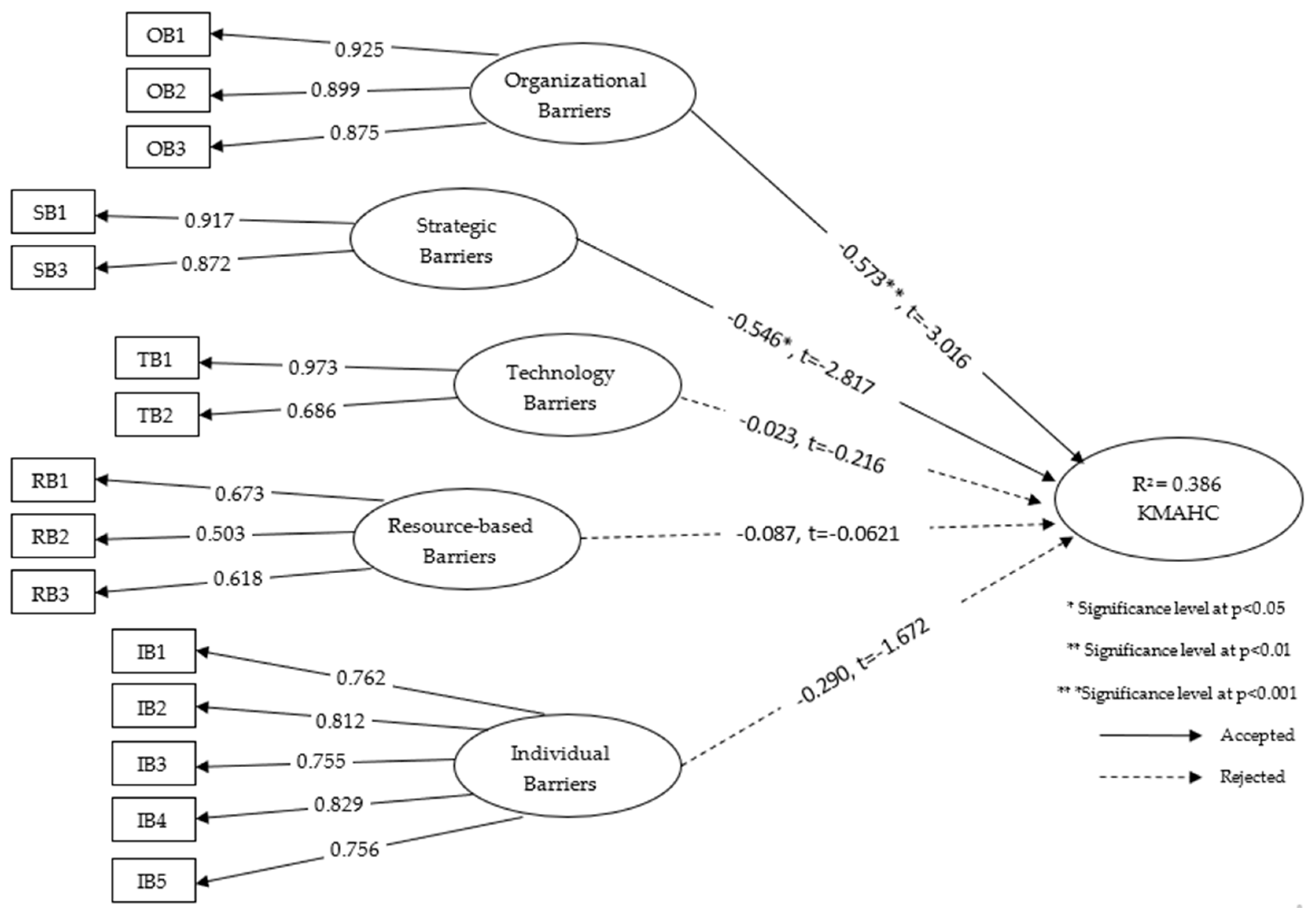
4.1. Barriers
4.1.1. Validation and Reliability of Measurement Model
4.1.2. The Structural Model Validation and Reliability
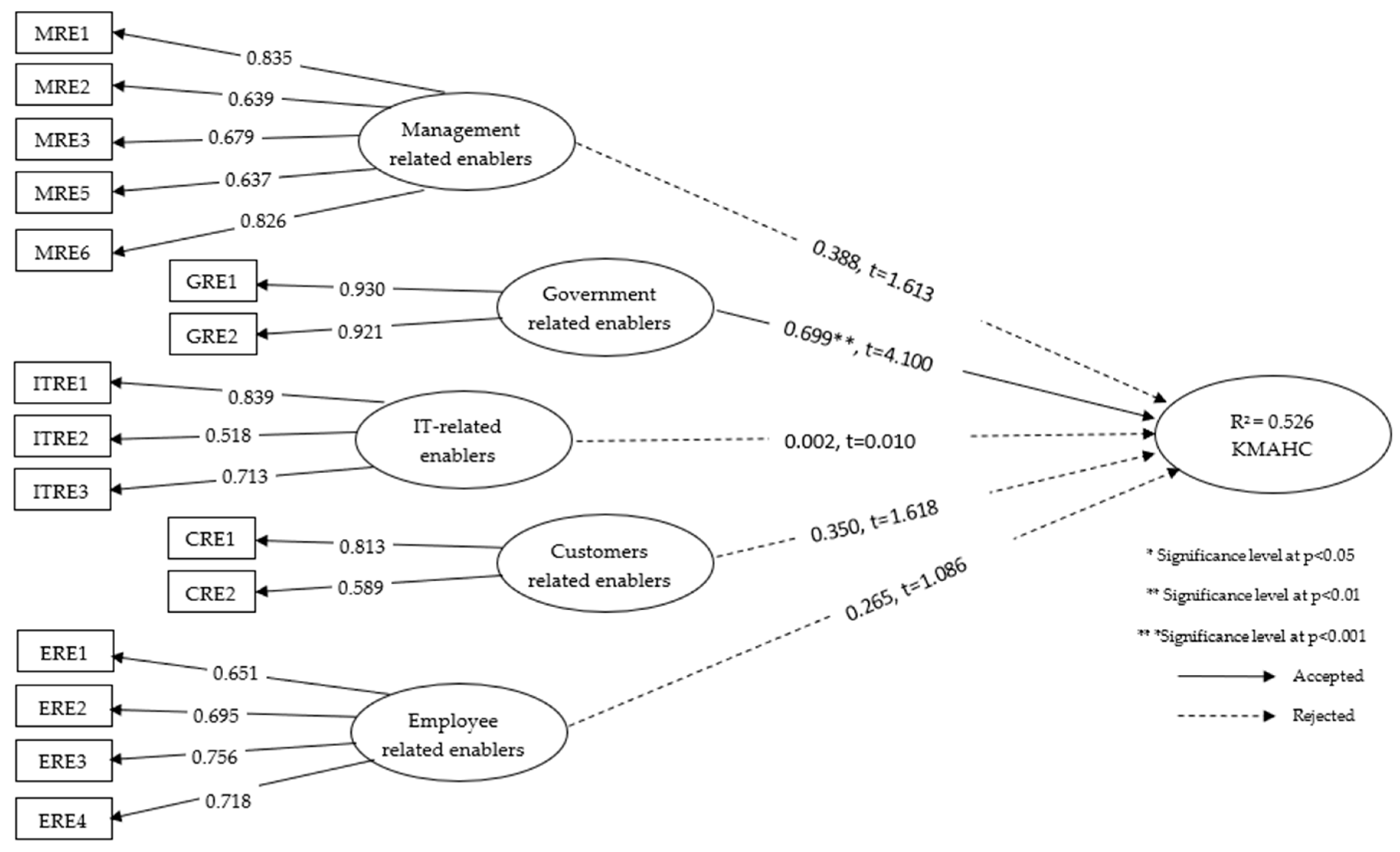
4.2. Enablers
4.2.1. Validation and Reliability of the Measurement Model
4.2.2. The structural Model Validation and Reliability
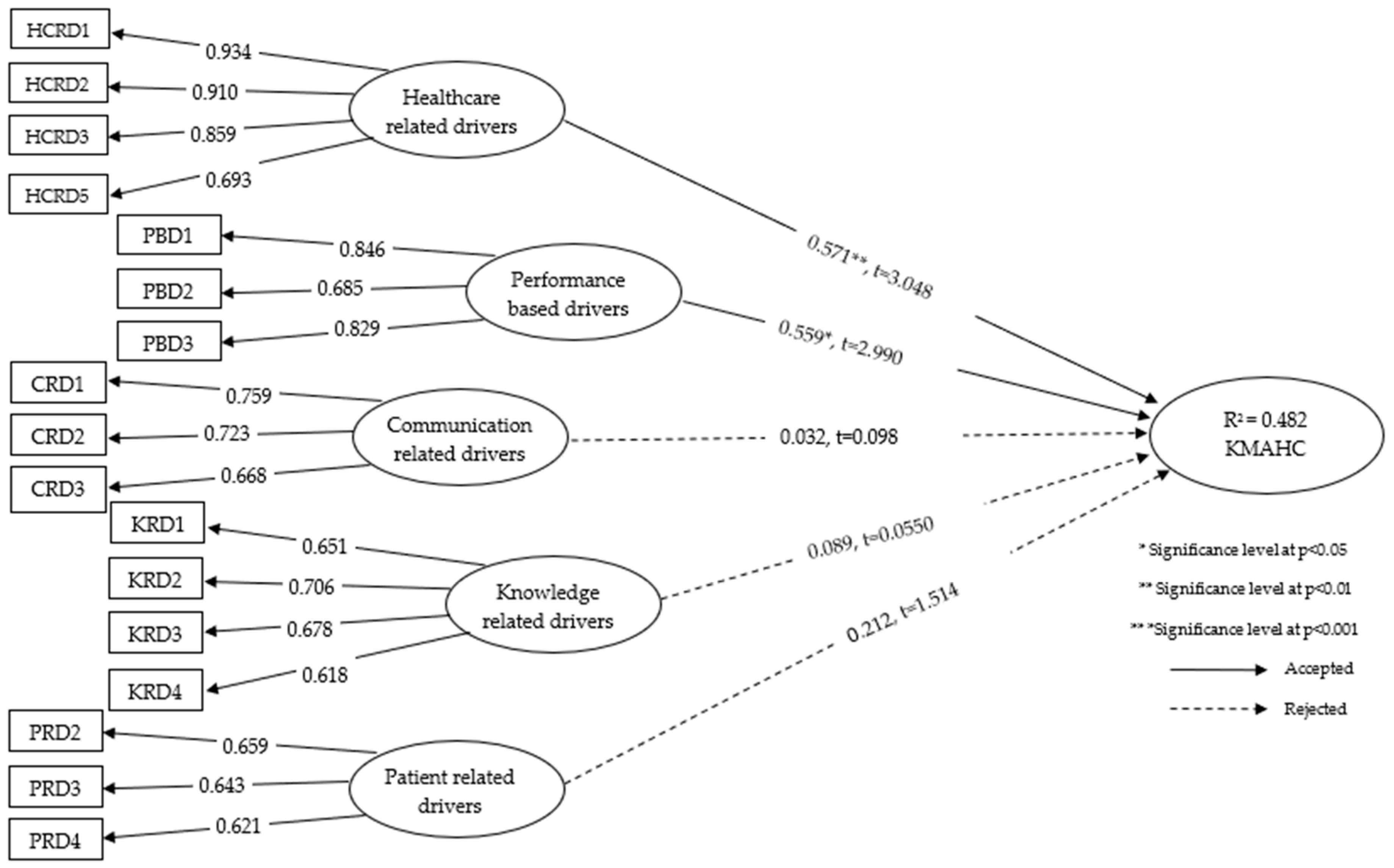
4.3 Drivers
4.3.1. Validation and Reliability of the Measurement Model
4.3.2. The Structural Model Validation and Reliability
5. Discussion
5.1. Barriers
5.2. Enablers
5.3. Drivers
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Varabyova, Y.; Müller, J.-M. The efficiency of health care production in OECD countries: A systematic review and meta-analysis of cross-country comparisons. Health Policy 2016, 120, 252–263. [Google Scholar] [CrossRef] [PubMed]
- Edwards, J.S.; Hall, M.; Shaw, D. Proposing a Systems Vision of Knowledge Management in Emergency Care. In Operational Research for Emergency Planning in Healthcare: Volume 2; Springer: Berlin, Germany, 2016; pp. 203–228. [Google Scholar]
- El Morr, C.; Subercaze, J. Knowledge management in healthcare. In Handbook of Research on Developments in e-Health and Telemedicine: Technological and Social Perspectives; IGI Global: Hershey, PA, USA, 2010; pp. 490–510. [Google Scholar]
- WBCSD (World Business Council on Sustainable Development). 2014. Available online: http://www.wbcsd.org/ (accessed on 23 December 2017).
- Guptill, J. Knowledge management in health care. J. Health Care Financ. 2005, 31, 10–14. [Google Scholar]
- lo Storto, C.; Goncharuk, A.G. Efficiency vs effectiveness: A benchmarking study on European healthcare systems. Econ. Sociol. 2017, 10, 102–115. [Google Scholar] [CrossRef] [PubMed]
- Sackett, D.L.; Rosenberg, W.M.; Gray, J.M.; Haynes, R.B.; Richardson, W.S. Evidence Based Medicine: What It Is and What It Isn’t; British Medical Journal Publishing Group: London, UK, 1996; Volume 312, pp. 71–72. [Google Scholar]
- Sharma, S.K.; Wickramasinghe, N.; Gupta, J.N. Knowledge management in healthcare. In Creating Knowledge-Based Healthcare Organizations; IGI Global: Hershey, PA, USA, 2005; pp. 1–13. [Google Scholar]
- Sharma, B.; Singh, M. Modeling the knowledge sharing barriers: An ISM approach. Int. J. Knowl.-Based Organ. (IJKBO) 2015, 5, 16–33. [Google Scholar] [CrossRef]
- Martini, A.; Pellegrini, L. Barriers and levers towards knowledge management configurations: A case study-based approach. J. Manuf. Technol. Manag. 2005, 16, 670–681. [Google Scholar] [CrossRef]
- Singh, M.; Shankar, R.; Narain, R.; Agarwal, A. An interpretive structural modeling of knowledge management in engineering industries. J. Adv. Manag. Res. 2003, 1, 28–40. [Google Scholar] [CrossRef]
- Ichijo, K.; von Krogh, G.; Nonaka, I. Knowledge enablers. In Knowing in Firms: Understanding, Managing and Measuring Knowledge; SAGE Publications Ltd.: Thousand Oaks, CA, USA, 1998; pp. 173–203. [Google Scholar]
- Yeh, Y.-J.; Lai, S.-Q.; Ho, C.-T. Knowledge management enablers: A case study. Ind. Manag. Data Syst. 2006, 106, 793–810. [Google Scholar] [CrossRef]
- Lee, H.; Choi, B. Knowledge management enablers, processes, and organizational performance: An integrative view and empirical examination. J. Manag. Inf. Syst. 2003, 20, 179–228. [Google Scholar]
- Shabbir, S.; Kaufmann, H.R.; Shehzad, M. Service quality, word of mouth and trust: Drivers to achieve patient satisfaction. Sci. Res. Essays 2010, 5, 2457–2462. [Google Scholar]
- Du Plessis, M. Drivers of knowledge management in the corporate environment. Int. J. Inf. Manag. 2005, 25, 193–202. [Google Scholar] [CrossRef]
- Jafari, M.; Akhavan, P.; Fesharaki, M.N.; Fathian, M. Iran aerospace industries’ KM approach based on a comparative study: A benchmarking on successful practices. Aircr. Eng. Aerosp. Technol. 2007, 79, 69–78. [Google Scholar] [CrossRef]
- Hojabri, R.; Eftekhar, F.; Sharifi, M.; Hatamian, A. Knowledge Management in an Iranian Health organization: Investigation of Critical Success Factors. J. Ind. Distrib. Bus. Vol. 2014, 5, 31–42. [Google Scholar] [CrossRef]
- Borousan, E.; Sharifian, N.; Hajiabolhassani, A.; Hazrati, S. Evaluating effect of knowledge management in sales forecasting: Evidence from Iran’s food retail industry. Int. J. Bus. Manag. 2011, 6, 213. [Google Scholar] [CrossRef]
- Karamat, J.; Shurong, T.; Ahmad, N.; Waheed, A.; Khan, S. Barriers to Knowledge Management in the Health Sector of Pakistan. Sustainability 2018, 10, 4155. [Google Scholar] [CrossRef]
- Karamat, J.; Shurong, T.; Ahmad, N.; Afridi, S.; Khan, S.; Mahmood, K. Enablers Supporting the Implementation of Knowledge Management in the Healthcare of Pakistan. Int. J. Environ. Res. Public Health 2018, 15, 2816. [Google Scholar] [CrossRef] [PubMed]
- Khan, A. Pakistan Economic Survey 2013–14, Health & Nutrition. 2013. Available online: http://www.finance.gov.pk/survey/chapters_14/11_Health_and_Nutrition.pdf (accessed on 1 December 2018).
- Aibinu, A.A.; Al-Lawati, A.M. Using PLS-SEM technique to model construction organizations’ willingness to participate in e-bidding. Autom. Constr. 2010, 19, 714–724. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming; Routledge: Abingdon-on-Thames, UK, 2016. [Google Scholar]
- Avkiran, N.K. An in-depth discussion and illustration of partial least squares structural equation modeling in health care. Health Care Manag. Sci. 2018, 21, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, B.; Anderson, M.; Ferguson, J. A predictive model of days from infection to discharge in patients with healthcare-associated urinary tract infections: A structural equation modelling approach. J. Hosp. Infect. 2017, 97, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Guo, R.; Berkshire, S.D.; Fulton, L.V.; Hermanson, P.M. Predicting intention to use evidence-based management among US healthcare administrators: Application of the theory of planned behavior and structural equation modeling. Int. J. Healthc. Manag. 2019, 12, 25–32. [Google Scholar] [CrossRef]
- Debata, B.R.; Patnaik, B.; Mahapatra, S.S.; Sree, K. Interrelations of service quality and service loyalty dimensions in medical tourism: A structural equation modelling approach. Benchmarking 2015, 22, 18–55. [Google Scholar] [CrossRef]
- Jacobs, S.R.; Weiner, B.J.; Reeve, B.B.; Hofmann, D.A.; Christian, M.; Weinberger, M. Determining the predictors of innovation implementation in healthcare: A quantitative analysis of implementation effectiveness. BMC Health Serv. Res. 2015, 15, 6. [Google Scholar] [CrossRef] [PubMed]
- Desouza, K.C. Managing Knowledge with Artificial Intelligence: An Introduction with Guidelines for Nonspecialists; Greenwood Publishing Group: Santa Barbara, CA, USA, 2002. [Google Scholar]
- Popadiuk, S.; Choo, C.W. Innovation and knowledge creation: How are these concepts related? Int. J. Inf. Manag. 2006, 26, 302–312. [Google Scholar] [CrossRef]
- Nonaka, I. A dynamic theory of organizational knowledge creation. Organ. Sci. 1994, 5, 14–37. [Google Scholar] [CrossRef]
- Beveridge, R. Creating value-focused healthcare delivery systems: Part three—Core competencies. J. Oncol. Manag. 1997, 6, 16–23. [Google Scholar] [PubMed]
- Anderson, J.G.; Aydin, C.E. Evaluating the impact of health care information systems. Int. J. Technol. Assess. Health Care 1997, 13, 380–393. [Google Scholar] [CrossRef] [PubMed]
- Pakistan Bureau of Statistics. 6th Population and Housing Census. 2017. Available online: www.pbscensus.gov.pk (accessed on 1 November 2018).
- Government of Pakistan, Ministry of Finance. Budget in Brief. Available online: http://www.finance.gov.pk/budget/Budget_in_Brief_2018_19.pdf (accessed on 20 November 2018).
- Amin Tabish, S. Towards development of professional management in Indian hospitals. J. Manag. Med. 1998, 12, 109–119. [Google Scholar] [CrossRef]
- Eiriz, V.; António Figueiredo, J. Quality evaluation in health care services based on customer-provider relationships. Int. J. Health Care Qual. Assur. 2005, 18, 404–412. [Google Scholar] [CrossRef]
- Ilyas, F. Pakistan ranked 149th in UN health goals. Dawn, 23 September 2016. [Google Scholar]
- Saad Andaleeb, S. Determinants of customer satisfaction with hospitals: A managerial model. Int. J. Health Care Qual. Assur. 1998, 11, 181–187. [Google Scholar] [CrossRef]
- Institute for Health Metrics and Evaluation. Pakistan Diseases. 2017. Available online: https://vizhub.healthdata.org/gbd-compare/ (accessed on 4 November 2018).
- Khan, S. The Kashmir Earthquake of October 8, 2005: Impacts in Pakistan. 28 Feburary 2006. Available online: https://reliefweb.int/report/pakistan/kashmir-earthquake-october-8-2005-impacts-pakistan (accessed on 29 November 2018 ).
- Hersch, W.R.; Lunin, L.F. Perspectives on medical informatics: Information technology in health care. Introduction and overview. J. Am. Soc. Infrastruct. Sci. 1995, 44, 726–727. [Google Scholar]
- Karamitri, I.; Talias, M.A.; Bellali, T. Knowledge management practices in healthcare settings: A systematic review. Int. J. Health Plan. Manag. 2017, 32, 4–18. [Google Scholar] [CrossRef]
- Kothari, A.; Hovanec, N.; Hastie, R.; Sibbald, S. Lessons from the business sector for successful knowledge management in health care: A systematic review. BMC Health Serv. Res. 2011, 11, 173. [Google Scholar] [CrossRef] [PubMed]
- Nicolini, D.; Powell, J.; Conville, P.; Martinez-Solano, L. Managing knowledge in the healthcare sector. A review. Int. J. Manag. Rev. 2008, 10, 245–263. [Google Scholar] [CrossRef]
- Hung, Y.-C.; Huang, S.-M.; Lin, Q.-P.; Tsai, M.-L. Critical factors in adopting a knowledge management system for the pharmaceutical industry. Ind. Manag. Data Syst. 2005, 105, 164–183. [Google Scholar] [CrossRef]
- Akhavan, P.; Jafari, M.; Fathian, M. Critical success factors of knowledge management systems: A multi-case analysis. Eur. Bus. Rev. 2006, 18, 97–113. [Google Scholar] [CrossRef]
- Chua, A.Y. The rise and fall of a community of practice: A descriptive case study. Knowl. Process Manag. 2006, 13, 120–128. [Google Scholar] [CrossRef]
- Robinson, H.; Carrillo, P.; Anumba, C.; Al-Ghassani, A. Developing a business case for knowledge management: The IMPaKT approach. Constr. Manag. Econ. 2004, 22, 733–743. [Google Scholar] [CrossRef]
- Patil, S.K.; Kant, R. A fuzzy AHP-TOPSIS framework for ranking the solutions of Knowledge Management adoption in Supply Chain to overcome its barriers. Expert Syst. Appl. 2014, 41, 679–693. [Google Scholar] [CrossRef]
- Seidler-de Alwis, R.; Hartmann, E. The use of tacit knowledge within innovative companies: Knowledge management in innovative enterprises. J. Knowl. Manag. 2008, 12, 133–147. [Google Scholar] [CrossRef]
- Cervigon, V.G.; Romero, N. A Knowledge Management experience in the energy sector. In Proceedings of the Engineering Management Conference (IEMC Europe 2008), Estoril, Portugal, 28–30 June 2008; pp. 1–4. [Google Scholar]
- Hsiao, J.-L.; Chen, R.-F. Critical factors influencing physicians’ intention to use computerized clinical practice guidelines: An integrative model of activity theory and the technology acceptance model. BMC Med. Inform. Decis. Mak. 2015, 16, 3. [Google Scholar] [CrossRef]
- Blumenberg, S.; Wagner, H.-T.; Beimborn, D. Knowledge transfer processes in IT outsourcing relationships and their impact on shared knowledge and outsourcing performance. Int. J. Inf. Manag. 2009, 29, 342–352. [Google Scholar] [CrossRef]
- Raisinghani, M.S.; Meade, L.L. Strategic decisions in supply-chain intelligence using knowledge management: An analytic-network-process framework. Supply Chain Manag. 2005, 10, 114–121. [Google Scholar] [CrossRef]
- Alavi, M.; Leidner, D.E. Knowledge management and knowledge management systems: Conceptual foundations and research issues. MIS Q. 2001, 107–136. [Google Scholar] [CrossRef]
- Wilson, T.D. The nonsense of knowledge management. Inf. Res. 2002, 8, 1–33. [Google Scholar]
- Lien, B.Y.H.; Hung, R.Y.; McLean, G.N. Organizational learning as an organization development intervention in six high-technology firms in Taiwan: An exploratory case study. Hum. Resour. Dev. Q. 2007, 18, 211–228. [Google Scholar] [CrossRef]
- Flottorp, S.A.; Oxman, A.D.; Krause, J.; Musila, N.R.; Wensing, M.; Godycki-Cwirko, M.; Baker, R.; Eccles, M.P. A checklist for identifying determinants of practice: A systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implement. Sci. 2013, 8, 35. [Google Scholar] [CrossRef] [PubMed]
- Kortteisto, T.; Kaila, M.; Komulainen, J.; Mäntyranta, T.; Rissanen, P. Healthcare professionals’ intentions to use clinical guidelines: A survey using the theory of planned behaviour. Implement. Sci. 2010, 5, 51. [Google Scholar] [CrossRef] [PubMed]
- Castillo, V.H.; Martínez-García, A.I.; Pulido, J. A knowledge-based taxonomy of critical factors for adopting electronic health record systems by physicians: A systematic literature review. BMC Med. Inf. Decis. Mak. 2010, 10, 60. [Google Scholar] [CrossRef]
- Hahn, T.; Schmiedinger, B.; Stephan, E. Supporting Research and Development Processes Using Knowledge Management Methods. In Knowledge Management: Concepts, Methodologies, Tools, and Applications; IGI Global: Hershey, PA, USA, 2008; pp. 490–508. [Google Scholar]
- Bartczak, S.E.; England, E.C. Challenges in Developing a Knowledge Management Strategy for the Air Force Materiel Command. In Knowledge Management and Business Strategies: Theoretical Frameworks and Empirical Research; IGI Global: Hershey, PA, USA, 2008; pp. 314–340. [Google Scholar]
- Larsen, M.H.; Pedersen, M.K. Distributed knowledge management in health care administration. In Proceedings of the 34th Annual Hawaii International Conference on System Sciences, Maui, HI, USA, 3–6 January 2001; p. 10. [Google Scholar]
- Rich, E.; Duchessi, P. Keeping the Flame Alive: Sustaining a Successful Knowledge Management Program. In Knowledge Management: Concepts, Methodologies, Tools, and Applications; IGI Global: Hershey, PA, USA, 2008; pp. 112–122. [Google Scholar]
- del-Rey-Chamorro, F.M.; Roy, R.; van Wegen, B.; Steele, A. A framework to create key performance indicators for knowledge management solutions. J. Knowl. Manag. 2003, 7, 46–62. [Google Scholar] [CrossRef]
- Hamaideh, S.H. Sources of Knowledge and Barriers of Implementing Evidence-Based Practice Among Mental Health Nurses in Saudi Arabia. Perspect. Psychiatr. Care 2017, 53, 190–198. [Google Scholar] [CrossRef] [PubMed]
- Aziz, N.; Sparrow, J. Patterns of gaining and sharing of knowledge about customers: A study of an Express Parcel Delivery Company. Knowl. Manag. Res. Pract. 2011, 9, 29–47. [Google Scholar] [CrossRef]
- Lowe, A.; McIntosh, A. Knowledge management in a New Zealand tree farming company: Ambiguity and resistance to the “technology solution”. J. Organ. Chang. Manag. 2007, 20, 539–558. [Google Scholar] [CrossRef]
- Samuel, K.E.; Goury, M.-L.; Gunasekaran, A.; Spalanzani, A. Knowledge management in supply chain: An empirical study from France. J. Strateg. Inf. Syst. 2011, 20, 283–306. [Google Scholar] [CrossRef]
- Burley, D.L.; Pandit, G. Lesson learned: Organizational realities influence KMS implementation. Vine 2008, 38, 476–489. [Google Scholar] [CrossRef]
- Franco, M.; Mariano, S. Information technology repositories and knowledge management processes: A qualitative analysis. Vine 2007, 37, 440–451. [Google Scholar] [CrossRef]
- Davenport, E. Mundane knowledge management and microlevel organizational learning: An ethological approach. J. Assoc. Inf. Sci. Technol. 2002, 53, 1038–1046. [Google Scholar] [CrossRef]
- Downing, J.R. “It’s Easier to Ask Someone I Know” Call Center Technicians’ Adoption of Knowledge Management Tools. J. Bus. Commun. (1973) 2004, 41, 166–191. [Google Scholar] [CrossRef]
- Cheng, J.-H.; Yeh, C.-H.; Tu, C.-W. Trust and knowledge sharing in green supply chains. Supply Chain Manag. 2008, 13, 283–295. [Google Scholar] [CrossRef]
- Pillai, K.G.; Min, S. A firm’s capability to calibrate supply chain knowledge—Antecedents and consequences. Ind. Mark. Manag. 2010, 39, 1365–1375. [Google Scholar] [CrossRef]
- Willem, A.; Buelens, M. Knowledge sharing in public sector organizations: The effect of organizational characteristics on interdepartmental knowledge sharing. J. Public Adm. Res. Theory 2007, 17, 581–606. [Google Scholar] [CrossRef]
- Pee, L.G.; Kankanhalli, A. Interactions among factors influencing knowledge management in public-sector organizations: A resource-based view. Gov. Inf. Q. 2016, 33, 188–199. [Google Scholar] [CrossRef]
- Sánchez-Polo, M.T.; Cegarra-Navarro, J.G. Implementing knowledge management practices in hospital-in-the-home units. J. Nurs. Care Q. 2008, 23, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-Y.; Hsu, P.-F.; Li, M.-H.; Chang, C.-C. Performance evaluation of knowledge management among hospital employees. Int. J. Health Care Q. Assur. 2011, 24, 348–365. [Google Scholar] [CrossRef] [PubMed]
- Ash, J.S.; Sittig, D.F.; Guappone, K.P.; Dykstra, R.H.; Richardson, J.; Wright, A.; Carpenter, J.; McMullen, C.; Shapiro, M.; Bunce, A. Recommended practices for computerized clinical decision support and knowledge management in community settings: A qualitative study. BMC Med. Inform. Decis. Mak. 2012, 12, 6. [Google Scholar] [CrossRef] [PubMed]
- Kümpers, S.; Mur, I.; Hardy, B.; Maarse, H.; Raak, A.V. The importance of knowledge transfer between specialist and generic services in improving health care: A cross-national study of dementia care in England and The Netherlands. Int. J. Health Plan. Manag. 2006, 21, 151–167. [Google Scholar] [CrossRef]
- Armstrong, R.; Waters, E.; Crockett, B.; Keleher, H. The nature of evidence resources and knowledge translation for health promotion practitioners. Health Promot. Int. 2007, 22, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, U.R.; Ravindran, S.; Freeze, R. A knowledge management success model: Theoretical development and empirical validation. J. Manag. Inf. Syst. 2006, 23, 309–347. [Google Scholar] [CrossRef]
- Quaddus, M.; Xu, J. Adoption and diffusion of knowledge management systems: Field studies of factors and variables. Knowl.-Based Syst. 2005, 18, 107–115. [Google Scholar] [CrossRef]
- Chang, S.-F.; Hsieh, P.-J.; Chen, H.-F. Key success factors for clinical knowledge management systems: Comparing physician and hospital manager viewpoints. Technol. Health Care 2016, 24, S297–S306. [Google Scholar] [CrossRef] [PubMed]
- Sunassee, N.N.; Sewry, D.A. A theoretical framework for knowledge management implementation. In Proceedings of the 2002 Annual Research Conference of the South African Institute of Computer Scientists and Information Technologists on Enablement through Technology, Port Elizabeth, South Africa, 16–18 September 2002; pp. 235–245. [Google Scholar]
- Ein-Dor, P.; Myers, M.D.; Raman, K. Information technology in three small developed countries. J. Manag. Inf. Syst. 1997, 13, 61–89. [Google Scholar] [CrossRef]
- Gibbs, J.; Kraemer, K.L.; Dedrick, J. Environment and policy factors shaping global e-commerce diffusion: A cross-country comparison. Inf. Soc. 2003, 19, 5–18. [Google Scholar] [CrossRef]
- Zhu, K.; Kraemer, K.L.; Dedrick, J. Information technology payoff in e-business environments: An international perspective on value creation of e-business in the financial services industry. J. Manag. Inf. Syst. 2004, 21, 17–54. [Google Scholar] [CrossRef]
- Liebowitz, J.; Wright, K. Does measuring knowledge make “cents”? Expert Syst. Appl. 1999, 17, 99–103. [Google Scholar] [CrossRef]
- Holtshouse, D.K. Information Technology for Knowledge Management; Springer Science & Business Media: New York, NY, USA, 2013. [Google Scholar]
- Van de Walle, S.; Van Dooren, W. How is information used to improve performance in the public sector? Exploring the dynamics of performance information. In Connecting Knowledge and Performance in Public Services: From Knowing to Doing; Cambridge University Press: Cambridge, UK, 2010; pp. 33–45. [Google Scholar]
- Godbout, A.J.; Godbout, G.M. Filtering knowledge: Changing information into knowledge assets. J. Syst. Knowl. Manag. 1999, 1, 1–5. [Google Scholar]
- Dobbins, M.; DeCorby, K.; Twiddy, T. A knowledge transfer strategy for public health decision makers. Worldviews Evid.-Based Nurs. 2004, 1, 120–128. [Google Scholar] [CrossRef]
- Lee, M.-C. Customer Relationship management and knowledge Management enhancing on innovation Competence: Case Study. Int. J. Inf. Technol. Manag. 2014, 10, 1784–1800. [Google Scholar]
- Kankanhalli, A.; Tan, B.C.; Wei, K.-K. Contributing knowledge to electronic knowledge repositories: An empirical investigation. MIS Q. 2005, 29, 113–143. [Google Scholar] [CrossRef]
- Chourides, P.; Longbottom, D.; Murphy, W. Excellence in knowledge management: An empirical study to identify critical factors and performance measures. Meas. Bus. Excell. 2003, 7, 29–45. [Google Scholar] [CrossRef]
- Davenport, T.H.; De Long, D.W.; Beers, M.C. Successful knowledge management projects. Sloan Manag. Rev. 1998, 39, 43–57. [Google Scholar]
- Darko, A.; Chan, A.P.C.; Yang, Y.; Shan, M.; He, B.-J.; Gou, Z. Influences of barriers, drivers, and promotion strategies on green building technologies adoption in developing countries: The Ghanaian case. J. Clean. Prod. 2018, 200, 687–703. [Google Scholar] [CrossRef]
- Lee, J.-H.; Kim, Y.-G.; Kim, M.-Y. Effects of managerial drivers and climate maturity on knowledge-management performance: Empirical validation. Inf. Resour. Manag. J. (IRMJ) 2006, 19, 48–60. [Google Scholar] [CrossRef]
- Yu, D. Building the Knowledge Advantage. 1999. Available online: http://www.pwcglobal.com/extweb/newcolth.nsf/DocID/D68D5EE66EDBFE828525679F0050D362 (accessed on 20 November 2018).
- Du Plessis, M. The role of knowledge management in innovation. J. Knowl. Manag. 2007, 11, 20–29. [Google Scholar] [CrossRef]
- Parlby, D.; Taylor, R. The Power of Knowledge: A Business Guide to Knowledge Management. 2000. Available online: http://www.kpmgconsulting.com/index.html (accessed on 28 November 2018).
- Bontis, N. There’s a price on your head: Managing intellectual capital strategically. Bus. Q. 1996, 60, 40–78. [Google Scholar]
- Yu, S.-H.; Kim, Y.-G.; Kim, M.-Y. Linking organizational knowledge management drivers to knowledge management performance: An exploratory study. In Proceedings of the 37th Annual Hawaii International Conference on System Sciences, Big Island, HI, USA, 5–8 January 2004; p. 10. [Google Scholar]
- Luxford, K.; Safran, D.G.; Delbanco, T. Promoting patient-centered care: A qualitative study of facilitators and barriers in healthcare organizations with a reputation for improving the patient experience. Int. J. Qual. Health Care 2011, 23, 510–515. [Google Scholar] [CrossRef]
- Bjørnson, F.O.; Dingsøyr, T. Knowledge management in software engineering: A systematic review of studied concepts, findings and research methods used. Inf. Softw. Technol. 2008, 50, 1055–1068. [Google Scholar] [CrossRef]
- Du Plessis, M. The strategic drivers and objectives of communities of practice as vehicles for knowledge management in small and medium enterprises. Int. J. Inf. Manag. 2008, 28, 61–67. [Google Scholar] [CrossRef]
- Zack, M.H. Managing codified knowledge. Sloan Manag. Rev. 1999, 40, 45–58. [Google Scholar]
- Martiny, M. Knowledge management at HP consulting. Organ. Dyn. 1998, 27, 71–78. [Google Scholar] [CrossRef]
- Ernst, Y. A Blueprint for Success: How to Put Knowledge to Work in Your Organization. 1999. Available online: http://www.ey.com (accessed on 21 November 2018).
- Mudge, A. Knowledge Management: Do we know that we know? Commun. World 1999, 16, 24–27. [Google Scholar]
- Caldwell, F. Knowledge Management Risk Analysis Framework. 1999. Available online: http://gartner4.gartnerweb.com:80/gg/purchase/0/00/853/52/doc/00085352/ (accessed on 19 November 2018).
- Hargadon, A.; Sutton, R.I. Building an innovation factory. Harv. Bus. Rev. 2000, 78, 157–166, 217. [Google Scholar]
- Andaleeb, S.S. Service quality perceptions and patient satisfaction: A study of hospitals in a developing country. Soc. Sci. Med. 2001, 52, 1359–1370. [Google Scholar] [CrossRef]
- Greco, J. Knowledge Is Power. Available online: http://web7.infotrac.london.galegroup.com/itw/infomark/482/356/72858976w3/purl=rcl_GBI-M_0_A54293713&dyn=30!xrn_10_0_A54293713?sw_aep=up_itw (accessed on 16 November 2018).
- Okoli, C.; Pawlowski, S.D. The Delphi method as a research tool: An example, design considerations and applications. Inf. Manag. 2004, 42, 15–29. [Google Scholar] [CrossRef]
- Dalkey, N.; Helmer, O. An experimental application of the Delphi method to the use of experts. Manag. Sci. 1963, 9, 458–467. [Google Scholar] [CrossRef]
- Murray, T.J.; Pipino, L.L.; van Gigch, J.P. A pilot study of fuzzy set modification of Delphi. Hum. Syst. Manag. 1985, 5, 76–80. [Google Scholar]
- Ahmad, N.; Zhu, Y.; Gebreslase, M.; Han, Q. Establishing standard definition and guidelines for brownfields in Pakistan; a stakeholder perspective. In Proceedings of the International Conference on Management Sciences and Engineering, Kanazawa, Japan, 28–31 July 2017. [Google Scholar]
- Ahmad, N.; Zhu, Y.; Ibrahim, M.; Waqas, M.; Waheed, A. Development of a standard brownfield definition, guidelines, and evaluation index system for brownfield redevelopment in developing countries: The case of Pakistan. Sustainability 2018, 10, 4347. [Google Scholar] [CrossRef]
- Hsu, T.; Yang, T. Application of fuzzy analytic hierarchy process in the selection of advertising media. J. Manag. Syst. 2000, 7, 19–39. [Google Scholar]
- Mao, C.; Shen, Q.; Pan, W.; Ye, K. Major barriers to off-site construction: The developer’s perspective in China. J. Manag. Eng. 2013, 31, 04014043. [Google Scholar] [CrossRef]
- Ekanayake, L.L.; Ofori, G. Building waste assessment score: Design-based tool. Build. Environ. 2004, 39, 851–861. [Google Scholar] [CrossRef]
- Wolf, E.J.; Harrington, K.M.; Clark, S.L.; Miller, M.W. Sample size requirements for structural equation models: An evaluation of power, bias, and solution propriety. Educ. Psychol. Meas. 2013, 73, 913–934. [Google Scholar] [CrossRef]
- Wu, J.-H.; Wang, S.-C.; Lin, L.-M. Mobile computing acceptance factors in the healthcare industry: A structural equation model. Int. J. Med. Inform. 2007, 76, 66–77. [Google Scholar] [CrossRef]
- Mercer, S.W.; Neumann, M.; Wirtz, M.; Fitzpatrick, B.; Vojt, G. General practitioner empathy, patient enablement, and patient-reported outcomes in primary care in an area of high socio-economic deprivation in Scotland—a pilot prospective study using structural equation modeling. Patient Educ. Couns. 2008, 73, 240–245. [Google Scholar] [CrossRef]
- Bagozzi, R.P.; Yi, Y. Specification, evaluation, and interpretation of structural equation models. J. Acad. Mark. Sci. 2012, 40, 8–34. [Google Scholar] [CrossRef]
- Ahmad, N.; Zhu, Y.; Shafait, Z.; Sahibzada, U.F.; Waheed, A. Critical barriers to brownfield redevelopment in developing countries: The case of Pakistan. J. Clean. Prod. 2019, 212, 1193–1209. [Google Scholar] [CrossRef]
- Hair, J.F.; Ringle, C.M.; Sarstedt, M. PLS-SEM: Indeed a silver bullet. J. Mark. Theory Pract. 2011, 19, 139–152. [Google Scholar] [CrossRef]
- Hair, J.F.; Sarstedt, M.; Ringle, C.M.; Mena, J.A. An assessment of the use of partial least squares structural equation modeling in marketing research. J. Acad. Mark. Sci. 2012, 40, 414–433. [Google Scholar] [CrossRef]
- Hair, J.F.; Sarstedt, M.; Hopkins, L.; Kuppelwieser, V.G. Partial least squares structural equation modeling (PLS-SEM) An emerging tool in business research. Eur. Bus. Rev. 2014, 26, 106–121. [Google Scholar] [CrossRef]
- Anderson, J.C.; Gerbing, D.W. Structural equation modeling in practice: A review and recommended two-step approach. Psychol. Bull. 1988, 103, 411. [Google Scholar] [CrossRef]
- Jöreskog, K.G.; Sörbom, D. LISREL 8: Structural Equation Modeling with the SIMPLIS Command Language; Scientific Software International: Skokie, IL, USA, 1993. [Google Scholar]
- Hu, L.-T.; Bentler, P.M. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychol. Methods 1998, 3, 424. [Google Scholar] [CrossRef]
- Schermelleh-Engel, K.; Moosbrugger, H.; Müller, H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods Psychol. Res. Online 2003, 8, 23–74. [Google Scholar]
- Bagozzi, R.P.; Yi, Y. On the evaluation of structural equation models. J. Acad. Mark. Sci. 1988, 16, 74–94. [Google Scholar] [CrossRef]
- Lim, M.; Griffiths, G.; Sambrook, S. Orgarnizational Structure for the 21st Century. In Annual Meeting of the Institute for Operations Research and Management Sciences; The Institute of Operations Research and Mananagemen: Austin, TX, USA, 2010. [Google Scholar]
- Ashkanasy, N.M.; Broadfoot, L.E.; Falkus, S.A. Questionnaire Measures of Organizational Culture; Sage Publications, Inc.: Thousand Oaks, CA, USA, 2000. [Google Scholar]
- Borousan, E.; Hajiabolhasani, A.; Hojabri, R. Evaluating factors that cause problem in implementation of knowledge management in Irans oil and gas industry. Afr. J. Bus. Manag. 2012, 6, 9589–9596. [Google Scholar] [CrossRef]
- Akram, M.; Khan, F.J. Health Care Services and Government Spending in Pakistan. 2007. Available online: www.pide.org.pk/pdf/Working%20Paper/WorkingPaper-32.pdf (accessed on 1 September 2018).
- Government of Pakistan. National Health Vision 2016–2025. 2016. Available online: http://www.nationalplanningcycles.org/sites/default/files/planning_cycle_repository/pakistan/national_health_vision_2016-25_30-08-2016.pdf (accessed on 25 September 2018).
- export.gov. Pakistan—Healthcare and Medical Equipment. Available online: https://www.export.gov/article?id=Pakistan-Healthcare-and-Medical-Equipment (accessed on 1 November 2018).
- Organization, W.H. Health Systems Profile—Pakistan. 2017. Available online: http://www.emro.who.int/human-resources-observatory/countries/country-profile.html (accessed on 15 September 2018).
- Rodríguez Perera Fde, P.; Peiró, M. Strategic planning in healthcare organizations. Rev. Esp. Cardiol. 2012, 65, 749–754. [Google Scholar]
- Islam, A. Health-related millennium development goals: Policy challenges for Pakistan. JPMA J. Pak. Med. Assoc. 2004, 54, 175–181. [Google Scholar]
- Ali, S. Pakistan: Achieving the SDGs. Daily Times, 17 April 2018. [Google Scholar]
- Ranjan Debata, B.; Sree, K.; Patnaik, B.; Sankar Mahapatra, S. Evaluating medical tourism enablers with interpretive structural modeling. Benchmarking 2013, 20, 716–743. [Google Scholar] [CrossRef]
- Layne-Farrar, A. Business Models and the Standard Setting Process. 2010. Available online: http://www.konkurrensverket.se/globalassets/english/publications-and-decisions/the-pros-and-cons-of-standard-setting.pdf (accessed on 30 November 2018).
- Egan, M. Setting standards: Strategic advantages in international trade. Bus. Strategy Rev. 2002, 13, 51–64. [Google Scholar] [CrossRef]
- WHO. Country Cooperation Strategy at a Glance, Pakistan. 2017. Available online: http://apps.who.int/iris/bitstream/handle/10665/136607/ccsbrief_pak_en.pdf?sequence=1 (accessed on 25 August 2018).
- Blake, W. Hospitals Are Learning from Industry How to Cut Medical Errors. Available online: https://www.economist.com/international/2018/06/28/hospitals-are-learning-from-industry-how-to-cut-medical-errors (accessed on 19 November 2018).
| Category | Code | Barrier | Reference |
|---|---|---|---|
| Organizational barriers | OB1 | Lack of top management commitment | [45,46,47,48,49,50,51] |
| OB2 | Unsupportive organization structure | [2,13,45,50,51,52,53,54] | |
| OB3 | Unsupportive organizational culture | [2,13,45,50,51,52,53,54] | |
| OB4 | Learning from previous mistakes | [44] | |
| Strategic barriers | SB1 | Insufficient strategic planning | [51,55,56] |
| SB2 | No common definition of knowledge management | [57,58] | |
| SB3 | Fear of inefective knowledge management implementaiton | [45,59] | |
| Technology barriers | TB1 | Implementation of complex knowledge managenent system | [54,60,61,62] |
| TB2 | Difficulty of integrating knowledge management with existing system | [13,45,51,63] | |
| Resource barriers | RB1 | Implementation cost of knowledge management | [45,48,51,64,65,66,67] |
| RB2 | Unavailability of resources | [51,68,69] | |
| RB3 | Questionable information quality | [44] | |
| Individual barriers | IB1 | Conflict between employees | [51,54,60,61] |
| IB2 | Resistance to change | [45,68] | |
| IB3 | Unwilling to work in a team | [68,70,71] | |
| IB4 | Unmotivated employee | [2,45,52,72,73,74,75] | |
| IB5 | Resistance to information sharing | [51,76] | |
| IB6 | Fear of sharing incorrect information | [51,77,78] |
| Category | Code | Enabler | Reference |
|---|---|---|---|
| Management related enablers | MRE1 | Management support | [44,79,80] |
| MRE2 | Proper well defined transparent workflow | [44,81,82] | |
| MRE3 | Creation of trust among employees | [18,44,79,83] | |
| MRE4 | Identification of the knowledge champion | [44,45,84] | |
| MRE5 | Creating a learning environment | [18,68,85,86,87] | |
| MRE6 | Alignment of organization and knowledge management goals | [18,19,88] | |
| Government related enablers | GRE1 | Government policies | [89,90,91] |
| GRE2 | Strategic planning | [18,19,92] | |
| Information Technology related enablers | ITRE1 | Information Technology for knowledge management | [44,79,81,87,93] |
| ITRE2 | Avoiding information overflow | [18,57] | |
| ITRE3 | Knowledge filtering | [44,87,94,95] | |
| ITRE4 | E-data promotion | [44,96] | |
| Customer related enablers | CRE1 | Taking constant feedback from customers | [85,86,87] |
| CRE2 | Establishing customer relationship management (CRM) | [81,97] | |
| Employee related enablers | ERE1 | Motivated employee | [44,79,80] |
| ERE2 | Empowerment of employee | [44] | |
| ERE3 | Recruitment of skilled professionals with knowledge management experience | [79,85,98] | |
| ERE4 | Training and education | [18,19,48,99] |
| Category | Code | Drivers | References |
|---|---|---|---|
| Healthcare related drivers | HCRD1 | Attaining competitive advantage | [16,104,105,106] |
| HCRD2 | Setting a standard for other organizations | [107] | |
| HCRD3 | Improved reputation of healthcare | [101,108] | |
| HCRD4 | More job openings | [100,101,109] | |
| HCRD5 | Rapid adjustment to change | [110,111,112] | |
| Performance-based drivers | PBD1 | Efficient decision making | [16,100,103,113] |
| PBD2 | Less resources used | [101,109] | |
| PBD3 | Improved administrative healthcare performance | [16,100,101] | |
| Communication related drivers | CRD1 | Improved interdepartmental communication | [16,104,107] |
| CRD2 | Communication with other healthcare organizations | [14,16,104,110,114] | |
| CRD3 | Improved knowledge quality | [16,107,112] | |
| Knowledge related drivers | KRD1 | Reduced knowledge loss | [16,110,115] |
| KRD2 | Elimination of distrust | [14,101,107] | |
| KRD3 | Increased innovation | [100,104,110,116] | |
| KRD4 | Creation of learning organization | [14,100,107] | |
| Patient related drivers | PRD1 | Reduced deaths due to error | Recommended by Group of Experts |
| PRD2 | Improvement in patient service | [15,100,101,117] | |
| PRD3 | Reduction in administrative cost | [100,101,103,118] | |
| PRD4 | Less costly service | [100,103,118] |
| Category | Frequency | Percentage |
|---|---|---|
| Age | ||
| <20 | 9 | 4% |
| 21–30 | 74 | 33% |
| 31–40 | 81 | 36.2% |
| 41–50 | 55 | 24.6% |
| >50 | 5 | 2.2% |
| Gender | ||
| Male | 128 | 57.1% |
| Female | 96 | 42.9% |
| Organization | ||
| Government hospital | 27 | 12.1% |
| Government teaching hospital | 32 | 14.3% |
| Private hospital | 24 | 10.7% |
| Private Teaching hospital | 31 | 13.8% |
| Medical centers | 18 | 8% |
| Pharmaceutical employees | 14 | 6.3% |
| N/A1 | 78 | 34.8% |
| Ownership | ||
| Privately owned | 87 | 38.8% |
| Government owned | 59 | 26.3% |
| N/A1 | 78 | 34.8% |
| Occupation | ||
| Federal Ministry of Health employee | 19 | 8.5% |
| Provincial Ministry of Health employee | 29 | 12.9% |
| Doctor | 25 | 11.2% |
| Dentist | 20 | 8.9% |
| Nurse | 29 | 12.9% |
| Administration | 35 | 15.6% |
| Patient | 30 | 13.4% |
| Technicians | 37 | 16.5% |
| Experience | ||
| <5 | 65 | 29% |
| 6–9 | 73 | 32.6% |
| 10-19 | 51 | 22.8% |
| >20 | 5 | 2.2% |
| N/A2 | 30 | 13.4% |
| Goodness-of-Fit | Recommended Value * | Result |
|---|---|---|
| The Chi Square (χ²) | N/A | 70 |
| Degree of freedom (df) | N/A | 32 |
| χ²/df | ≤3 | 2.180 |
| Standardized root mean square (SRMR) | ≤0.1 | 0.053 |
| Goodness-of-fit index (GFI) | ≥0.9 | 0.985 |
| Adjusted goodness-of-fit index (AGFI) | ≥0.85 | 0.950 |
| Normed fit index (NFI) | ≥0.9 | 0.980 |
| Comparative fit index (CFI) | ≥0.95 | 0.983 |
| Root mean square error of approximation (RMSEA) | ≤ 0.08 | 0.06 |
| Category | Code | Factor Loading | Cronbach’s Alpha | Composite Realiability | AVE |
|---|---|---|---|---|---|
| Organizational barriers | OB1 | 0.925 | 0.856 | 0.879 | 0.605 |
| OB2 | 0.899 | ||||
| OB3 | 0.875 | ||||
| Strategic barriers | SB1 | 0.917 | 0.839 | 0.871 | 0.583 |
| SB3 | 0.872 | ||||
| Technology barrier | TB1 | 0.973 | 0.733 | 0.761 | 0.529 |
| TB2 | 0.686 | ||||
| Resource barrier | RB1 | 0.673 | 0.762 | 0.785 | 0.540 |
| RB2 | 0.505 | ||||
| RB3 | 0.618 | ||||
| Individual barrier | IB1 | 0.762 | 0.715 | 0.736 | 0.527 |
| IB2 | 0.812 | ||||
| IB3 | 0.755 | ||||
| IB4 | 0.829 | ||||
| IB5 | 0.756 | ||||
| Category | OB | SB | TB | RB | IB |
|---|---|---|---|---|---|
| Organizational barriers (OB) | 0.852 | ||||
| Strategic barriers (SB) | 0.537 | 0.759 | |||
| Technology barriers (TB) | 0.482 | 0.479 | 0.739 | ||
| Resource barriers (RB) | 0.358 | 0.384 | 0.520 | 0.763 | |
| Individual barriers (IB) | 0.438 | 0.258 | 0.347 | 0.428 | 0.628 |
| Code | OB | SB | TB | RB | IB |
|---|---|---|---|---|---|
| OB1 | 0.925 | 0.475 | 0.394 | 0.398 | 0.413 |
| OB2 | 0.899 | 0.463 | 0.248 | 0.285 | 0.311 |
| OB3 | 0.875 | 0.418 | 0.267 | 0.375 | 0.479 |
| SB1 | 0.278 | 0.917 | 0.236 | 0.349 | 0.408 |
| SB3 | 0.234 | 0.872 | 0.346 | 0.429 | 0.016 |
| TB1 | 0.473 | 0.394 | 0.973 | 0.246 | 0.279 |
| TB2 | 0.213 | 0.386 | 0.686 | 0.379 | 0.197 |
| RB1 | 0.364 | 0.349 | 0.175 | 0.673 | 0.264 |
| RB2 | 0.326 | 0.149 | 0.196 | 0.505 | 0.151 |
| RB3 | 0.418 | 0.285 | 0.259 | 0.618 | 0.230 |
| IB1 | 0.427 | 0.349 | 0.200 | 0.186 | 0.762 |
| IB2 | 0.253 | 0.259 | 0.349 | 0.267 | 0.812 |
| IB3 | 0.053 | 0.281 | 0.255 | 0.112 | 0.755 |
| IB4 | 0.212 | 0.351 | 0.351 | 0.058 | 0.829 |
| IB5 | 0.369 | 0.247 | 0.188 | 0.192 | 0.756 |
| Goodness-of-Fit | Recommended Value * | Result |
|---|---|---|
| The Chi Square (χ²) | N/A | 76.51 |
| degree of freedom (df) | N/A | 40 |
| χ²/df | ≤3 | 1.913 |
| Standardized root mean square (SRMR) | ≤0.1 | 0.052 |
| Goodness-of-fit index (GFI) | ≥0.9 | 0.975 |
| Adjusted goodness-of-fit index (AGFI) | ≥0.85 | 0.955 |
| Normed fit index (NFI) | ≥0.9 | 0.981 |
| Comparative fit index (CFI) | ≥0.95 | 0.99 |
| Root mean square error of approximation (RMSEA) | ≤0.08 | 0.058 |
| Hypothesis | Path Coefficient | t-Value | p-Value | Result |
|---|---|---|---|---|
| H1a: OB→KMAHC | −0.573 | −3.016 | 0.009 ** | Supported |
| H1b: SB→ KMAHC | −0.546 | −2.817 | 0.087 * | Supported |
| H1c: TB→ KMAHC | −0.023 | −0.216 | 0.903 | Not Supported |
| H1d: RB→ KMAHC | −0.087 | −0.621 | 0.627 | Not Supported |
| H1e: IB→ KMAHC | −0.290 | −1.672 | 0.146 | Not Supported |
| Goodness-of-Fit | Recommended Value * | Result |
|---|---|---|
| The Chi Square (χ²) | N/A | 75 |
| degree of freedom (df) | N/A | 38 |
| χ²/df | ≤3 | 1.974 |
| Standardized root mean square (SRMR) | ≤0.1 | 0.052 |
| Goodness-of-fit index (GFI) | ≥0.9 | 0.965 |
| Adjusted goodness-of-fit index (AGFI) | ≥0.85 | 0.931 |
| Normed fit index (NFI) | ≥0.9 | 0.960 |
| Comparative fit index (CFI) | ≥0.95 | 0.963 |
| Root mean square error of approximation (RMSEA) | ≤0.08 | 0.059 |
| Category | Code | Factor Loading | Cronbach’s Alpha | Composite Realiability | AVE |
|---|---|---|---|---|---|
| Management related enablers (MRE) | MRE1 | 0.835 | 0.752 | 0.758 | 0.627 |
| MRE2 | 0.639 | ||||
| MRE3 | 0.679 | ||||
| MRE5 | 0.637 | ||||
| MRE6 | 0.826 | ||||
| Government related enablers (GRE) | GRE1 | 0.930 | 0.803 | 0.880 | 0.713 |
| GRE2 | 0.921 | ||||
| Information Technology related enablers (ITRE) | ITRE1 | 0.839 | 0.718 | 0.729 | 0.697 |
| ITRE2 | 0.518 | ||||
| ITRE3 | 0.713 | ||||
| Customer related enabler (CRE) | CRE1 | 0.813 | 0.805 | 0.815 | 0.559 |
| CRE2 | 0.589 | ||||
| ERE1 | 0.651 | 0.755 | 0.763 | 0.516 | |
| Employee related enablers (ERE) | ERE2 | 0.695 | |||
| ERE3 | 0.756 | ||||
| ERE4 | 0.718 |
| Category | MRE | GRE | ITRE | CRE | ERE |
|---|---|---|---|---|---|
| Management related enablers (MRE) | 0.765 | ||||
| Government related enablers (GRE) | 0.475 | 0.863 | |||
| Information Technology related enablers (ITRE) | 0.084 | 0.388 | 0.715 | ||
| Customer related enabler (CRE) | 0.395 | 0.265 | 0.285 | 0.706 | |
| Employee related enablers (ERE) | 0.092 | 0.397 | 0.056 | 0.349 | 0.649 |
| Code | MRE | GRE | ITRE | CRE | ERE |
|---|---|---|---|---|---|
| MRE1 | 0.835 | 0.214 | 0.288 | 0.022 | 0.012 |
| MRE2 | 0.639 | 0.168 | 0.358 | 0.061 | 0.084 |
| MRE3 | 0.679 | 0.311 | 0.447 | 0.059 | 0.361 |
| MRE5 | 0.637 | 0.335 | 0.197 | 0.007 | 0.199 |
| MRE6 | 0.826 | 0.182 | 0.418 | 0.018 | 0.164 |
| GRE1 | 0.486 | 0.930 | 0.265 | 0.191 | 0.179 |
| GRE2 | 0.438 | 0.921 | 0.319 | 0.252 | 0.298 |
| ITRE1 | 0.283 | 0.053 | 0.839 | 0.189 | 0.249 |
| ITRE2 | 0.255 | 0.372 | 0.518 | 0.259 | 0.294 |
| ITRE3 | 0.187 | 0.290 | 0.713 | 0.184 | 0.130 |
| CRE1 | 0.121 | 0.354 | 0.189 | 0.813 | 0.085 |
| CRE2 | 0.043 | 0.097 | 0.165 | 0.589 | 0.058 |
| ERE1 | 0.553 | 0.079 | 0.056 | 0.354 | 0.651 |
| ERE2 | 0.450 | 0.297 | 0.268 | 0.299 | 0.695 |
| ERE3 | 0.433 | 0.198 | 0.199 | 0.219 | 0.756 |
| ERE4 | 0.005 | 0.354 | 0.319 | 0.149 | 0.718 |
| Goodness-of-fit | Recommended Value* | Result |
|---|---|---|
| The Chi Square (χ²) | N/A | 79 |
| degree of freedom (df) | N/A | 43 |
| χ²/df | ≤3 | 1.837 |
| Standardized root mean square (SRMR) | ≤0.1 | 0.051 |
| Goodness-of-fit index (GFI) | ≥0.9 | 0.965 |
| Adjusted goodness-of-fit index (AGFI) | ≥0.85 | 0.945 |
| Normed fit index (NFI) | ≥0.9 | 0.971 |
| Comparative fit index (CFI) | ≥0.95 | 0.980 |
| Root mean square error of approximation (RMSEA) | ≤0.08 | 0.057 |
| Hypothesis | Path Coefficient | t-Value | p-Value | Result |
|---|---|---|---|---|
| H2a: MRE→KMAHC | 0.388 | 1.613 | 0.148 | Not Supported |
| H2b: GRE→ KMAHC | 0.699 | 4.100 | 0.000 ** | Supported |
| H2c: ITRE→ KMAHC | 0.002 | 0.010 | 0.887 | Not Supported |
| H2d: CRE→ KMAHC | 0.350 | 1.618 | 0.221 | Not Supported |
| H2e: ERE→ KMAHC | 0.265 | 1.086 | 0.460 | Not Supported |
| Goodness-of-Fit | Recommended Value * | Result |
|---|---|---|
| The Chi Square (χ²) | N/A | 132.83 |
| degree of freedom (df) | N/A | 73 |
| χ²/df | ≤3 | 1.820 |
| Standardized root mean square (SRMR) | ≤0.1 | 0.052 |
| Goodness-of-fit index (GFI) | ≥0.9 | 0.960 |
| Adjusted goodness-of-fit index (AGFI) | ≥0.85 | 0.926 |
| Normed fit index (NFI) | ≥0.9 | 0.956 |
| Comparative fit index (CFI) | ≥0.95 | 0.958 |
| Root mean square error of approximation (RMSEA) | ≤0.08 | 0.059 |
| Category | Code | Factor Loading | Cronbach’s Alpha | Composite Realiability | AVE |
|---|---|---|---|---|---|
| Healthcare related drivers | HCRD1 | 0.934 | 0.825 | 0.869 | 0.596 |
| HCRD2 | 0.910 | ||||
| HCRD3 | 0.859 | ||||
| HCRD5 | 0.693 | ||||
| Performance-based drivers | PBD1 | 0.846 | 0.779 | 0.806 | 0.654 |
| PBD2 | 0.685 | ||||
| PBD3 | 0.829 | ||||
| Communication related drivers | CRD1 | 0.759 | 0.756 | 0.813 | 0.643 |
| CRD2 | 0.723 | ||||
| CRD3 | 0.668 | ||||
| Knowledge related drivers | KRD1 | 0.651 | 0.758 | 0.856 | 0.513 |
| KRD2 | 0.706 | ||||
| KRD3 | 0.678 | ||||
| KRD4 | 0.618 | ||||
| Patient related drivers | |||||
| PRD2 | 0.659 | 0.635 | 0.746 | 0.649 | |
| PRD3 | 0.643 | ||||
| PRD4 | 0.621 |
| Category | HCRD | PBD | CRD | KRD | PRD |
|---|---|---|---|---|---|
| Healthcare related drivers (HCRD) | 0.754 | ||||
| Performance-based drivers (PBD) | 0.617 | 0.775 | |||
| Communication related drivers (CRD) | 0.513 | 0.562 | 0.616 | ||
| Knowledge related drivers (KRD) | 0.492 | 0.486 | 0.466 | 0.603 | |
| Patient related drivers (PRD) | 0.335 | 0.354 | 0.361 | 0.442 | 0.698 |
| Code | HCRD | PBD | CRD | KRD | PRD |
|---|---|---|---|---|---|
| HCRD1 | 0.934 | 0.280 | 0.215 | 0.335 | 0.160 |
| HCRD2 | 0.910 | 0.523 | 0.384 | 0.253 | 0.218 |
| HCRD3 | 0.859 | 0.416 | 0.522 | 0.366 | 0.021 |
| HCRD5 | 0.693 | 0.610 | 0.277 | 0.150 | 0.516 |
| PBD1 | 0.434 | 0.846 | 0.223 | 0.336 | 0.513 |
| PBD2 | 0.553 | 0.685 | 0.254 | 0.234 | 0.463 |
| PBD3 | 0.489 | 0.829 | 0.166 | 0.315 | 0.246 |
| CRD1 | 0.432 | 0.298 | 0.759 | 0.299 | 0.326 |
| CRD2 | 0.398 | 0.317 | 0.723 | 0.352 | 0.142 |
| CRD3 | 0.580 | 0.456 | 0.668 | 0.250 | 0.156 |
| KRD1 | 0.386 | 0.533 | 0.286 | 0.651 | 0.166 |
| KRD2 | 0.366 | 0.357 | 0.646 | 0.706 | 0.059 |
| KRD3 | 0.339 | 0.168 | 0.246 | 0.678 | 0.441 |
| KRD4 | 0.311 | 0.258 | 0.054 | 0.618 | 0.493 |
| PRD2 | 0.274 | 0.156 | 0.462 | 0.395 | 0.659 |
| PRD3 | 0.190 | 0.502 | 0.180 | 0.373 | 0.643 |
| PRD4 | 0.200 | 0.611 | 0.513 | 0.486 | 0.621 |
| Goodness-of-Fit | Recommended Value * | Result |
|---|---|---|
| The Chi Square (χ²) | N/A | 139.7 |
| degree of freedom (df) | N/A | 79 |
| χ²/df | ≤3 | 1.768 |
| Standardized root mean square (SRMR) | ≤0.1 | 0.051 |
| Goodness-of-fit index (GFI) | ≥0.9 | 0.956 |
| Adjusted goodness-of-fit index (AGFI) | ≥0.85 | 0.936 |
| Normed fit index (NFI) | ≥0.9 | 0.961 |
| Comparative fit index (CFI) | ≥0.95 | 0.970 |
| Root mean square error of approximation (RMSEA) | ≤0.08 | 0.057 |
| Hypothesis | Path Coefficient | t-Value | p-Value | Result |
|---|---|---|---|---|
| H3a: HCRD→KMAHC | 0.571 | 3.048 | 0.004 ** | Supported |
| H3b: PBD→ KMAHC | 0.559 | 2.990 | 0.031 * | Supported |
| H3c: CRD→ KMAHC | 0.032 | 0.098 | 0.928 | Not Supported |
| H3d: KRD→ KMAHC | 0.089 | 0.550 | 0.625 | Not Supported |
| H3e: PRD→ KMAHC | 0.212 | 1.514 | 0.169 | Not Supported |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karamat, J.; Shurong, T.; Ahmad, N.; Afridi, S.; Khan, S.; Khan, N. Developing Sustainable Healthcare Systems in Developing Countries: Examining the Role of Barriers, Enablers and Drivers on Knowledge Management Adoption. Sustainability 2019, 11, 954. https://doi.org/10.3390/su11040954
Karamat J, Shurong T, Ahmad N, Afridi S, Khan S, Khan N. Developing Sustainable Healthcare Systems in Developing Countries: Examining the Role of Barriers, Enablers and Drivers on Knowledge Management Adoption. Sustainability. 2019; 11(4):954. https://doi.org/10.3390/su11040954
Chicago/Turabian StyleKaramat, Jawad, Tong Shurong, Naveed Ahmad, Sana Afridi, Shahbaz Khan, and Nidha Khan. 2019. "Developing Sustainable Healthcare Systems in Developing Countries: Examining the Role of Barriers, Enablers and Drivers on Knowledge Management Adoption" Sustainability 11, no. 4: 954. https://doi.org/10.3390/su11040954
APA StyleKaramat, J., Shurong, T., Ahmad, N., Afridi, S., Khan, S., & Khan, N. (2019). Developing Sustainable Healthcare Systems in Developing Countries: Examining the Role of Barriers, Enablers and Drivers on Knowledge Management Adoption. Sustainability, 11(4), 954. https://doi.org/10.3390/su11040954






