Analysis of the Risk and Protective Roles of Work-Related and Individual Variables in Burnout Syndrome in Nurses
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instruments
2.3. Procedure
2.4. Data Analysis
3. Results
3.1. Burnout, Sociodemographic Variables, and Workplace Characteristics
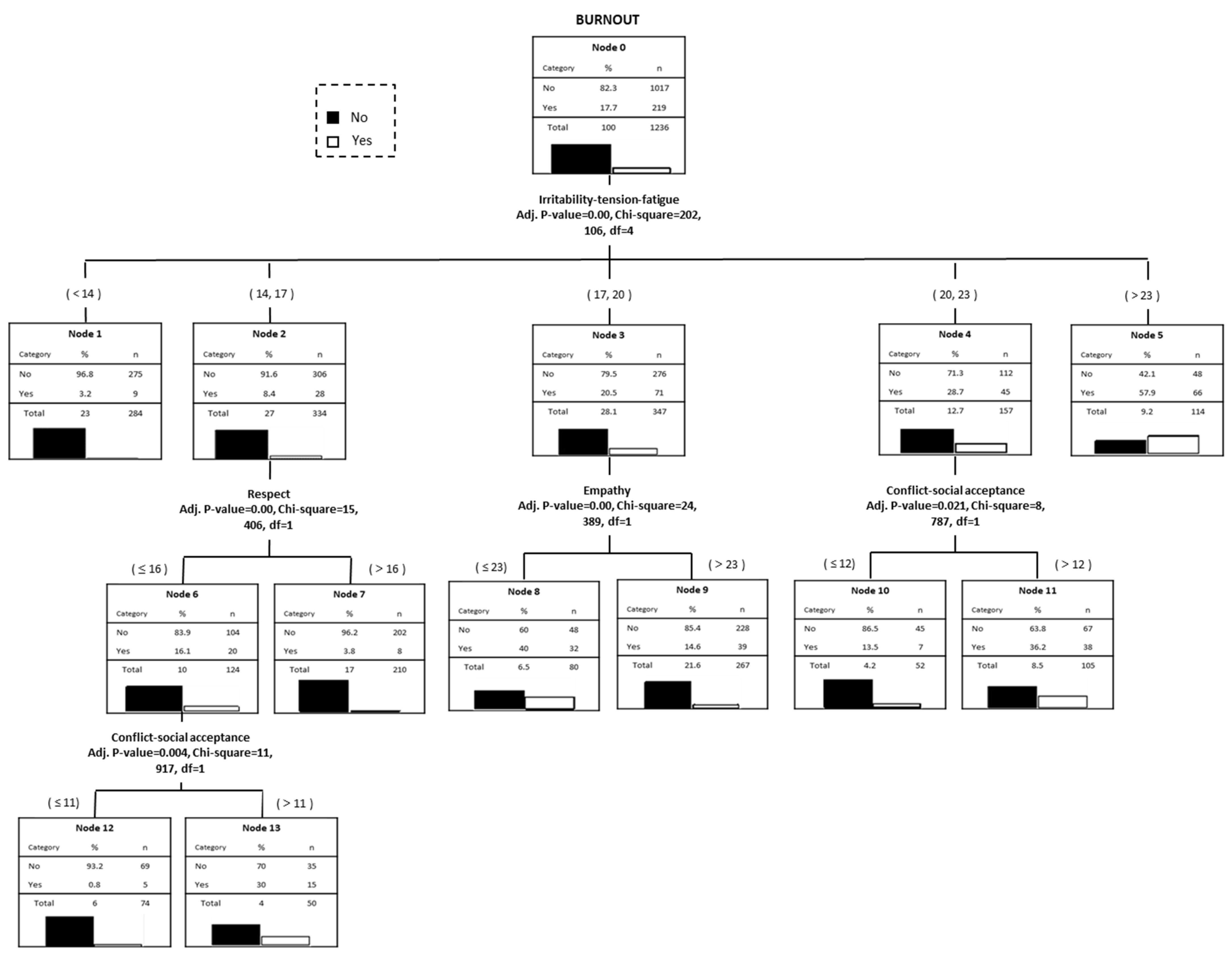
3.2. Psychological Variables and Burnout
3.3. Logistic Regression Model for the Presence of Burnout: Risk and Protective Factors
3.4. Multiple Linear Regression Model of Burnout according to Employment Situation
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Navarro-Abal, Y.; López-López, M.J.; Climent-Rodríguez, J.A. Engagement, resilience and empathy in nursing assistants. Enferm. Clin. 2018, 28, 77–148. [Google Scholar] [CrossRef]
- Maslach, C.; Leiter, M.P. Burnout. In Encyclopedia of Mental Health, 2nd ed.; Friedman, H., Ed.; Elsevier: Oxford, UK, 2016; pp. 222–227. [Google Scholar]
- Maslach, C. Psychology of Burnout’s. In International Encyclopedia of the Social & Behavioral Sciences, 2nd ed.; Wright, J.D., Ed.; Elsevier: Oxford, UK, 2015; pp. 929–932. [Google Scholar]
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry 2016, 15, 103–111. [Google Scholar] [CrossRef]
- Pérez-Fuentes, M.C.; Gázquez, J.J.; Ruiz, M.D.; Molero, M.M. Inventory of Overburden in Alzheimer’s Patient Family Caregivers with no Specialized Training. Int. J. Clin. Health Psychol. 2017, 17, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Juliá-Sachís, R.; Richart-Martínez, M.; García-Aracil, N.; José-Alcaide, L.; Pirque-Donat, T.; Castejón-de la Encina, M.E. Measuring the levels of burnout syndrome and empathy of Spanish emergency medical service professionals. Australas. Emerg. Care 2019, 22, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Setyomati, S.; Rusca, K.; Putra, P. Prevalence of burnout syndrome among nurses in general hospitals in provincial East Java: Cross-sectional study. Enferm. Clin. 2019, 29, 362–366. [Google Scholar] [CrossRef]
- Kim, H.S.; Yeom, H.A. The association between spiritual well-being and burnout in intensive care unit nurses: A descriptive study. Intensive Crit. Care Nurs. 2018, 46, 92–97. [Google Scholar] [CrossRef]
- Martín, R.A. Burnout in nursing: Prevalence and related factors in a hospital environment. Rev. Cient. Soc. Esp. Enferm. Neurol. 2015, 41, 9–14. [Google Scholar] [CrossRef]
- Maslach, C.; Leiter, M.P. Burnout. In Stress: Concepts, Cognition, Emotion, and Behavior; Fink, G., Ed.; Academic Press: Cambridge, MA, USA, 2016; pp. 351–357. [Google Scholar]
- Suñer-Soler, R.; Grau-Martín, A.; Dlichtentrei, D.; Prats, M.; Braga, F.; Font-Mayolas, S.; Gras, M.E. The consequences of burnout syndrome among healthcare professionals in Spain and Spanish speaking Latin American countries. Burn. Res. 2014, 1, 82–89. [Google Scholar] [CrossRef] [Green Version]
- Konstantinou, A.K.; Bonotis, K.; Sokratous, M.; Siokas, V.; Dardiotis, E. Burnout Evaluation and Potential Predictors in a Greek Cohort of Mental Health Nurses. Arch. Psychiatr. Nurs. 2018, 32, 449–456. [Google Scholar] [CrossRef]
- Bagnall, A.M.; Jones, R.; Akter, H.; Woodall, J. Interventions to Prevent Burnout in High Risk Individuals: Evidence Review; Public Health England: London, UK, 2016. [Google Scholar]
- Gómez-Perdomo, G.E.; Meneses-Higuita, A.C.; Montes-Palacio, M.C. La satisfacción laboral y el capital psicológico: Factores que influyen en el síndrome de burnout. Ansiedad Estrés 2017, 23, 71–75. [Google Scholar] [CrossRef]
- Purvanova, R.K.; Muros, J.P. Gender differences in burnout: A meta-analysis. J. Vocat. Behav. 2010, 77, 168–185. [Google Scholar] [CrossRef]
- Martos, Á.; Pérez-Fuentes, M.C.; Molero, M.M.; Gázquez, J.J.; Simón, M.M.; Barragán, A.B. Burnouty engagement en estudiantes de Ciencias de la Salud. Eur. J. Investig. Health Psychol. Educ. 2018, 8, 23–36. [Google Scholar] [CrossRef]
- Sanfilippo, F.; Noo, A.; Foresta, G.; Santonocito, C.; Palumbo, G.J.; Arcadipane, A.; Maybauer, D.; Maybauer, M.O. Incidence and Factors Associated with Burnout in Anesthesiology: A Systematic Review. Biomed. Res. Int. 2017, 2017, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yuguero, O.; Melnick, E.R.; Marsal, J.R.; Esquerda, M.; Soler-González, J. Cross-sectional study of the association between healthcare professionals’ empathy and burnout and the number of annual primary care visits per patient under their care in Spain. BMJ Open 2018, 8, e020949. [Google Scholar] [CrossRef]
- Torre, M.; Popper, S.; Math, B. Burnout prevalence in intensive care nurses in Argentina. Enferm. Intensiva 2019, 30, 108–115. [Google Scholar] [CrossRef]
- Arrogante, O.; Aparicio-Zaldivar, E.G. Burnout syndrome in intensive care professionals: Relationships with health status and wellbeing. Enferm. Intensiva 2019. [Google Scholar] [CrossRef]
- Carrillo-García, C.; Ríos-Rísquez, M.I.; Martínez-Hurtado, R.; Noguera-Villaescusa, P. Stress level assessment of the nursing staff in the Intensive Care Unit of a university hospital. Enferm. Intensiva 2016, 27, 89–95. [Google Scholar] [CrossRef]
- Chuang, C.H.; Tseng, P.C.; Lin, C.Y.; Lin, K.H.; Chen, Y.Y. Burnout in the intensive care unit professionals: A systematic review. Medicine 2016, 95, e5629. [Google Scholar] [CrossRef]
- Qu, H.Y.; Wang, C.M. Study on the relationships between nurses’job burnout and subjetive well-being. Chin. Nurs. Res. 2015, 2, 61–66. [Google Scholar] [CrossRef]
- Jensen, M.T. A two wave cross-lagged study of work-role conflict: Work-family conflict and emotional exhaustion. Scand. J. Psychol. 2016, 57, 591–600. [Google Scholar] [CrossRef]
- Fang, Y. Burnout and work family-conflict among nurses during the preparation for reevaluation of a grade A tertiary hospital. Chin. Nurs. Res. 2017, 4, 51–55. [Google Scholar] [CrossRef]
- Dhaini, S.R.; Denhaerynck, K.; Bachnick, S.; Schwendimann, R.; Schubert, M.; De Geest, S.; Simon, M. Work schedule flexibility is associated with emotional exhaustion among registered nurses in Swiss hospitals: A cross-sectional study. Int. J. Nurs. Stud. 2018, 82, 99–105. [Google Scholar] [CrossRef]
- Teng, C.I.; Shyu, Y.I.L.; Chiou, W.K.; Fan, H.C.; Lam, S.M. Interactive effects of nurse-experienced time pressure and burnout on patient safety: A cross-sectional survey. Int. J. Nurs. Stud. 2010, 47, 1442–1450. [Google Scholar] [CrossRef] [PubMed]
- De Vliegeher, K.; Milisen, K.; Wouters, R.; Scheepmans, K.; Paquay, L.; Debaillie, R.; Greys, L.; Okerman, F.; Van Deuren, I.; Dierckx de Casterlé, B. The professional self-image of registered home nurses in Flanders (Belgium): A cross-sectional questionnaire survey. Appl. Nurs. Res. 2011, 24, 29–36. [Google Scholar] [CrossRef]
- Alférez, A.D. La comunicación en la relación de ayuda al paciente en enfermería: Saber qué decir y qué hacer. Rev. Esp. C Sal. 2012, 3, 147–157. [Google Scholar]
- Sánchez-Romero, S. Prevalencia del Síndrome de Burnout en profesionales de Enfermería de las Unidades de Cuidados Críticos y Urgencias del Hospital Médico-Quirúrgico de Jaén. Enferm. Trab. 2014, 4, 115–125. [Google Scholar]
- Frögéli, E.; Rudman, A.; Gustavsson, P. The relationship between task mastery, role clarity, social acceptance, and stress: An intensive longitudinal study with a sample of newly registered nurses. Int. J. Nurs. Stud. 2019, 91, 60–69. [Google Scholar] [CrossRef]
- Macías, A.J.; Gutiérrez-Castañeda, C.; Carmona, F.J.; Crespillo, D. Relación de la inteligencia emocional y la calidad de vida profesional con la consecución de objetivos laborales en el distrito de atención primaria Costa del Sol. Aten. Primaria 2016, 48, 301–307. [Google Scholar] [CrossRef]
- Molero, M.M.; Pérez-Fuentes, M.C.; Gázquez, J.J.; Barragán, A.B. Burnout in Health Professionals According to Their Self-Esteem, Social Support and Empathy Profile. Front. Psychol. 2018, 9, 1–6. [Google Scholar] [CrossRef]
- Liu, H.; Zhang, X.; Chang, R.; Wang, W. A research regarding the relationship among intensive care nurses’ self-esteem, job satisfaction and subjective well-being. Int. J. Nurs. Stud. 2017, 4, 291–295. [Google Scholar] [CrossRef]
- Nwafor, C.E.; Immanel, E.U.; Obi-Nwosu, H. Does nurses’ self-concept mediate the relationship between job satisfaction and burnout among Nigerian nurses. Int. J. Afr. Nurs. Sci. 2015, 3, 71–75. [Google Scholar] [CrossRef]
- Smeds, M.R.; Janko, M.R.; Allen, S.; Amankwah, K.; Arnell, T.; Ansari, P.; Yoo, P. El agotamiento y su relación con el estrés percibido, la autoeficacia, la depresión, el apoyo social y los factores programáticos en los residentes de cirugía general. Am. J. Surg. 2019, in press. [Google Scholar] [CrossRef]
- MacPhee, M.; Dahinten, V.S.; Havei, F. The impact of Heavy Perceived Nurse Workloads on Patient and Nurse Outcomes. Adm. Sci. 2017, 7, 7. [Google Scholar] [CrossRef]
- Rodríguez-Mantilla, J.M.; Fernández-Díaz, M.J. The effect of interpersonal relationships on burnout syndrome in Secondary Education teachers. Psicothema 2017, 29, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Önler, E.; Yildiz, T.; Bahar, S. Evaluation of the communication skills of operating room staff. J. Interprof. Educ. Pract. 2018, 10, 44–46. [Google Scholar] [CrossRef]
- Shin, S.; Park, J.H.; Bae, S.H. Nurse staffing and nurse outcomes: A systematic review and meta-analysis. Nurs. Outlook 2018, 66, 273–282. [Google Scholar] [CrossRef]
- Leal-Costa, C.; Díaz-Agea, J.L.; Tirado-González, S.; Rodríguez-Marín, J.; van der Hofstadt, C.J. Las habilidades de comunicación como factor preventivo del síndrome de Burnout en los profesionales de la salud. An. Sist. Sanit. Navar. 2015, 38, 213–223. [Google Scholar] [CrossRef]
- Vermir, P.; Blot, S.; Degoote, S.; Vandijck, D.; Mariman, A.; Vanacker, T.; Peleman, R.; Verhaeghe, R.; Vogelaers, D. Communication satisfaction and job satisfaction among critical care nurses and their impact on burnout and intention to leave: A questionnaire study. Intensive Crit. Care Nurs. 2018, 48, 21–27. [Google Scholar] [CrossRef]
- Chang, B.P.; Carter, E.; Ng, N.; Flynn, C.; Tan, T. Association of clinician burnout and perceived clinician-patient communication. Am. J. Emerg. Med. 2018, 36, 156–158. [Google Scholar] [CrossRef]
- Cherry, M.G.; Fletcher, I.; O’Sullivan, H. Exploring the relationships among attachment, emotional intelligence and communication. Med. Educ. 2013, 47, 317–325. [Google Scholar] [CrossRef]
- Borg, E.; Hyman, S.A.; Wells, N.; Shi, Y.; Shotwell, M.S.; Weinger, M.B. Burnout and Resiliency in Perianesthesia Nurses: Findings and Recommendations From a National Study of Members of the American Society of PeriAnesthesia Nurses. J. PeriAnesth Nurs. 2019. [Google Scholar] [CrossRef]
- Van der Heijden, B.; Brown, C.; Xu, Y. Impact of Job Demands and Resources on Nurses’ Burnout and Occupational Turnover Intention Towards an Age-Moderated Mediation Model for the Nursing Profession. Int. J. Environ. Res. Public Health 2019, 16, 2011. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.K.; Ji, E.J. The Moderating Role of Leader–Member Exchange in the Relationships Between Emotional Labor and Burnout in Clinical Nurses. Asian Nurs. Res. 2018, 12, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Minamizono, S.; Nomura, K.; Inoue, Y.; Hiraike, H.; Tsuchiya, A.; Okinaga, H.; Illing, J. Gender Division of Labor, Burnout, and Intention to Leave Work Among Young Female Nurses in Japan: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 2201. [Google Scholar] [CrossRef] [PubMed]
- García-Arroyo, J.; Osca, A. Coping with burnout: Analysis of linear, non-linear and interaction relationships. An. Psicol. 2017, 33, 722–731. [Google Scholar] [CrossRef]
- Vicente-Galindo, M.P.; López-Herrera, H.; Pedrosa, I.; Suárez-Álvarez, J.; Galindo-Villardón, M.P.; García-Cueto, E. Estimating the effect of emotional intelligence in wellbeing among priests. Int. J. Clin. Health Psychol. 2017, 17, 46–55. [Google Scholar] [CrossRef]
- Smith, K.B.; Profetto-McGrath, J.; Cummings, G.G. Emotional intelligence and nursing: An integrative literature review. Int. J. Nurs. Stud. 2009, 46, 1624–1636. [Google Scholar] [CrossRef]
- Lee, K.R.; Kim, J.M. Effects of emotional labor on burnout in nurses: Focusing on the moderating effects of social intelligence and emotional intelligence. J. Korean Acad. Nurs. 2016, 22, 22–32. [Google Scholar] [CrossRef]
- Vilelas, J.M.S.; Diogo, P.M.J. Emotional labor in nursing praxis. Rev. Gaucha Enferm. 2014, 35, 145–149. [Google Scholar] [CrossRef]
- Raghubir, A.E. Emotional intelligence in professional nursing practice: A concept review using Rodgers’s evolutionary analysis approach. Int. J. Nurs. Stud. 2018, 5, 126–130. [Google Scholar] [CrossRef]
- Nightingale, S.; Spiby, H.; Sheen, K.; Slade, P. The impact of emotional intelligence in health care professionals on caring behaviour towards patients in clinical and long-term care settings: Findings from an integrative review. Int. J. Nurs. Stud. 2018, 80, 106–117. [Google Scholar] [CrossRef] [PubMed]
- Başoğul, C.; Özgür, G. Role of Emotional Intelligence in Conflict Management Strategies of Nurses. Asian Nurs. Res. 2016, 10, 228–233. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boyle, D.A.; Bush, N.J. Reflections on the Emotional Hazards of Pediatric Oncology Nursing: Four Decades of Perspectives and Potential. J. Pediatr. Nurs. 2018, 40, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Jaracz, M.; Rosiak, I.; Bertrand-Bucińska, A.; Jaskulski, M.; Nieżurawska, J.; Borkowska, A. Affective temperament, job stress and professional burnout in nurses and civil servants. PLoS ONE 2017, 12, e0176698. [Google Scholar] [CrossRef]
- Fernández-Castro, J.; Martínez-Zaragoza, F.; Rovira, T.; Edo, S.; Solanes-Puchol, A.; Martín-del Río, B.; García-Sierra, R.; Benavides-Gil, G.; Doval, E. How does emotional exhaustion influence work stress? Relationships between stressor appraisals, hedonic tone, and fatigue in nurses’ daily tasks: A longitudinal cohort study. Int. J. Nurs. Stud. 2017, 75, 43–50. [Google Scholar] [CrossRef]
- Morales, F.M. Relaciones entre afrontamiento del estrés cotidiano, autoconcepto, habilidades sociales e inteligencia emocional. Eur. J. Educ. Psychol. 2017, 10, 41–48. [Google Scholar] [CrossRef]
- García-Sierra, R.; Fernández-Castro, J.; Martínez-Zaragoza, F. Engagement of nurses in their profession. Qualitative study on engagement. Enferm. Clin. 2017, 27, 153–162. [Google Scholar] [CrossRef]
- Ye, Y.; Hu, R.; Ni, Z.; Jiang, N.; Jiang, X. Effects of perceived stress and professional values on clinical performance in practice nursing students: A structural equation modeling approach. Nurse Educ. Today 2018, 71, 157–162. [Google Scholar] [CrossRef]
- Elshaer, N.S.M.; Moustafa, M.S.A.; Aiad, M.W.; Ramadán, I.E. Job Stress and Burnout Syndrome among Critical Care Healthcare Workers. Alex. J. Med. 2017, 54, 273–277. [Google Scholar] [CrossRef]
- Kind, N.; Eckert, A.; Steinlin, C.; Ferget, J.M.; Schmid, M. Verbal and physical client aggression—A longitudinal analysis of professional caregivers’ psychophysiological stress response and burnout. Psychoneuroendocrino 2018, 94, 11–16. [Google Scholar] [CrossRef]
- Chang, H.E.; Cho, S.H. Workplace Violence and Job Outcomes of Newly Licensed Nurses. Asian Nurs. Res. 2016, 10, 271–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marsollier, R.; Aparicio, M. Burnout and engagement: Complementary or opposed perspectives? An analysis on university staff. Rev. Orientac. Educ. 2013, 27, 63–74. [Google Scholar]
- Moreno, B.; Bustos, R.; Matallana, A.; Miralles, T. La evaluación del burnout. Problemas y alternativas. El CBB como evaluación de los elementos del proceso. Rev. Psicol. Trab. Organ. 1997, 13, 185–207. [Google Scholar]
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Baessler, J.; Schwarcer, R. Evaluación de la autoeficacia: Adaptación española de la escala de Autoeficacia General. Ansiedad Estrés 1996, 2, 1–8. [Google Scholar]
- Rosenberg, M. Sociedad y Autoimagen Adolescente; Princeton University Press: Princeton, NJ, USA, 1965. [Google Scholar]
- Calvo, F.; Díaz-Palarea, M.D. Apoyo social percibido: Características psicométricas del cuestionario CASPE en una población urbana geriátrica. Psicothema 2004, 16, 570–575. [Google Scholar]
- Pérez-Fuentes, M.C.; Gázquez, J.J.; Mercader, I. Brief Emotional Intelligence Inventory for Senior Citizens (EQ-i-M20). Psicothema 2014, 26, 524–530. [Google Scholar] [CrossRef]
- Leal, C.; Tirado, S.; van-der Hofstadt, C.; Rodríguez-Marín, J. Creación de la Escala sobre Habilidades de Comunicación en Profesionales de la Salud, EHC-PS. An. Psicol. 2016, 32, 49–59. [Google Scholar] [CrossRef]
- Sanz-Carrillo, C.; García-Campayo, J.; Rubio, A.; Santed, M.A.; Montoro, M. Validation of the Spanish version of the Perceived Stress Questionnaire. J. Psychosom. Res. 2002, 53, 167–172. [Google Scholar] [CrossRef]
- Livingston, S.A. Criterion-referenced applications of Classical Test Theory. J. Educ. Meas. 1972, 9, 13–26. [Google Scholar] [CrossRef]
- Livingston, S.A. A note on the interpretation of the criterion-referenced reliability coefficient. J. Educ. Meas. 1973, 10, 311. [Google Scholar] [CrossRef]
- Gempp, R.; Saiz, J.L. El coeficiente K2 de Livingston y la fiabilidad de una decisión dicotómica en un test psicológico. Univ. Psychol. 2014, 13, 217–226. [Google Scholar] [CrossRef]
| Burnout Syndrome | ||
|---|---|---|
| Emotional intelligence | Intrapersonal | −0.10 *** |
| Interpersonal | −0.15 *** | |
| Stress management | −0.26 *** | |
| Adaptability | −0.16*** | |
| General mood | −0.26 *** | |
| Perceived stress | Conflict-social acceptance | 0.46 *** |
| Overburden | 0.36 *** | |
| Irritability-tension-fatigue | 0.49 *** | |
| Energy-joy | −0.47 *** | |
| Fear-anxiety | −0.36 *** | |
| Self-realization-satisfaction | 0.18 *** | |
| Communication skills | Empathy | −0.28 *** |
| Informative communication | −0.15 *** | |
| Respect | −0.23 *** | |
| Social skills | 0.01 | |
| General self-efficacy | −0.19 *** | |
| Overall self-esteem | −0.34 *** | |
| Perceived social support | −0.27 *** | |
| Burnout | t | p | ||||||
|---|---|---|---|---|---|---|---|---|
| <25 points | ≥25 points | |||||||
| N | Mean | SD | N | Mean | SD | |||
| Intrapersonal | 1017 | 10.66 | 1.93 | 219 | 10.29 | 2.65 | 1.85 | 0.065 |
| Interpersonal | 1017 | 12.40 | 1.85 | 219 | 11.88 | 2.08 | 3.66 *** | 0.000 |
| Stress management | 1017 | 13.36 | 2.23 | 219 | 12.25 | 2.40 | 6.56 *** | 0.000 |
| Adaptability | 1017 | 11.77 | 2.05 | 219 | 11.19 | 2.13 | 3.77 *** | 0.000 |
| General mood | 1017 | 12.73 | 2.22 | 219 | 11.47 | 2.32 | 7.57 *** | 0.000 |
| Conflict-social acceptance | 1017 | 11.78 | 2.49 | 219 | 14.73 | 3.40 | −12.10 *** | 0.000 |
| Overburden | 1017 | 9.37 | 2.35 | 219 | 10.77 | 2.40 | −7.94 *** | 0.000 |
| Irritability-tension-fatigue | 1017 | 17.04 | 3.57 | 219 | 21.14 | 4.25 | −13.28 *** | 0.000 |
| Energy-joy | 1017 | 15.05 | 2.82 | 219 | 12.28 | 2.87 | 13.10 *** | 0.000 |
| Fear-anxiety | 1017 | 3.66 | 1.30 | 219 | 4.51 | 1.47 | −7.82 *** | 0.000 |
| Self-realization-satisfaction | 1017 | 6.88 | 1.19 | 219 | 7.32 | 1.29 | −4.62 *** | 0.000 |
| Empathy | 1017 | 26.51 | 3.33 | 219 | 24.29 | 4.29 | 7.21 *** | 0.000 |
| Informative communication | 1017 | 28.88 | 3.39 | 219 | 27.63 | 4.30 | 4.03 *** | 0.000 |
| Respect | 1017 | 16.45 | 1.98 | 219 | 15.31 | 2.55 | 6.23 *** | 0.000 |
| Social skills | 1017 | 16.84 | 3.01 | 219 | 16.71 | 3.21 | 0.54 | 0.587 |
| General self-efficacy | 1017 | 32.35 | 4.21 | 219 | 30.84 | 4.46 | 4.76 *** | 0.000 |
| Overall self-esteem | 1017 | 33.39 | 4.22 | 219 | 30.48 | 4.34 | 9.19 *** | 0.000 |
| Perceived social support | 1017 | 24.72 | 2.97 | 219 | 22.77 | 3.58 | 7.52 *** | 0.000 |
| Variables | β | Std. Err | Wald | df | Sig | Exp(β) | 95% CI |
|---|---|---|---|---|---|---|---|
| Intrapersonal | 0.02 | 0.03 | 0.38 | 1 | 0.538 | 1.02 | 0.95–1.10 |
| Interpersonal | 0.03 | 0.06 | 0.29 | 1 | 0.586 | 1.03 | 0.91–1.16 |
| Stress management | 0.05 | 0.04 | 1.91 | 1 | 0.166 | 1.06 | 0.97–1.15 |
| Adaptability | −0.03 | 0.06 | 0.26 | 1 | 0.610 | 0.96 | 0.86–1.09 |
| General mood | 0.02 | 0.06 | 0.13 | 1 | 0.718 | 1.02 | 0.90–1.15 |
| Conflict-social acceptance | 0.17 | 0.04 | 18.74 | 1 | 0.000 | 1.19 | 1.10–1.29 |
| Overburden | −0.01 | 0.05 | 0.08 | 1 | 0.768 | 0.98 | 0.88–1.09 |
| Irritability-tension-fatigue | 0.15 | 0.03 | 16.25 | 1 | 0.000 | 1.16 | 1.08–1.26 |
| Energy-joy | −0.19 | 0.03 | 24.75 | 1 | 0.000 | 0.82 | 0.76–0.88 |
| Fear-anxiety | −0.11 | 0.08 | 1.58 | 1 | 0.209 | 0.89 | 0.75–1.06 |
| Self-realization-satisfaction | −0.08 | 0.08 | 0.99 | 1 | 0.319 | 0.91 | 0.77–1.08 |
| Empathy | −0.19 | 0.05 | 13.74 | 1 | 0.000 | 0.82 | 0.74–.91 |
| Informative communication | 0.09 | 0.04 | 3.95 | 1 | 0.047 | 1.10 | 1.00–1.21 |
| Respect | −0.03 | 0.07 | 0.22 | 1 | 0.632 | 0.96 | 0.83–1.12 |
| Social skills | 0.03 | 0.03 | 0.77 | 1 | 0.379 | 1.03 | 0.95–1.11 |
| General self-efficacy | 0.01 | 0.02 | 0.36 | 1 | 0.544 | 1.01 | 0.96–1.06 |
| Overall self-esteem | −0.01 | 0.02 | 0.14 | 1 | 0.707 | 0.98 | 0.93–1.04 |
| Perceived social support | −0.01 | 0.03 | 0.23 | 1 | 0.628 | 0.98 | 0.92–1.04 |
| Constant | −1.74 | 1.30 | 1.78 | 1 | 0.182 | 0.17 |
| DISCONTINUOUS WORK | Model | R | R2 | Corrected R2 | Change Statistics | Durbin–Watson | ||||
| Standard Error of Estimation | Change in R2 | Change in F | Sig. of Change in F | |||||||
| 1 | 0.47 | 0.22 | 0.22 | 4.12 | 0.22 | 247.85 | 0.000 | 2.02 | ||
| 2 | 0.55 | 0.30 | 0.30 | 3.91 | 0.08 | 97.83 | 0.000 | |||
| 3 | 0.57 | 0.33 | 0.33 | 3.83 | 0.02 | 36.93 | 0.000 | |||
| 4 | 0.58 | 0.34 | 0.34 | 3.79 | 0.01 | 17.32 | 0.000 | |||
| 5 | 0.59 | 0.35 | 0.35 | 3.77 | 0.00 | 8.98 | 0.003 | |||
| Model 5 | Non-Standardized Coefficients | Standardized Coefficients | t | Sig. | Collinearity | |||||
| B | Std. Error | Beta | Tol. | VIF | ||||||
| (Constant) | 23.97 | 1.47 | 16.26 | 0.000 | ||||||
| Energy-joy | −0.39 | 0.05 | −0.25 | −7.61 | 0.000 | 0.66 | 1.49 | |||
| Conflict-soc. accpt. | 0.28 | 0.06 | 0.17 | 4.40 | 0.000 | 0.48 | 2.05 | |||
| Empathy | −0.29 | 0.04 | −0.22 | −6.95 | 0.000 | 0.70 | 1.41 | |||
| Irrita.-tens.-fatigue | 0.19 | 0.04 | 0.17 | 4.05 | 0.000 | 0.42 | 2.37 | |||
| Social skills | 0.14 | 0.04 | 0.09 | 2.99 | 0.003 | 0.77 | 1.29 | |||
| PERMANENT WORK | Model | R | R2 | Corrected R2 | Change statistics | Durbin Watson | ||||
| Standard Error of Estimation | Change in R2 | Change in F | Sig. of Change in F | |||||||
| 1 | 0.54 | 0.29 | 0.29 | 4.24 | 0.29 | 157.20 | 0.000 | 1.91 | ||
| 2 | 0.59 | 0.34 | 0.34 | 4.08 | 0.05 | 30.94 | 0.000 | |||
| 3 | 0.61 | 0.38 | 0.37 | 3.98 | 0.03 | 20.14 | 0.000 | |||
| 4 | 0.62 | 0.39 | 0.38 | 3.95 | 0.01 | 6.63 | 0.010 | |||
| 5 | 0.63 | 0.40 | 0.39 | 3.93 | 0.00 | 5.56 | 0.019 | |||
| 6 | 0.64 | 0.40 | 0.40 | 3.90 | 0.00 | 5.17 | 0.023 | |||
| Model 6 | Non-Standardized Coefficients | Standardized Coefficients | t | Sig. | Collinearity | |||||
| B | Std. Error | Beta | Tol. | VIF | ||||||
| (Constant) | 15.67 | 2.27 | 6.89 | 0.000 | ||||||
| Irrita.-tens.-fatigue | 0.30 | 0.07 | 0.23 | 4.18 | 0.000 | 0.48 | 2.05 | |||
| Conflict-soc. accpt. | 0.47 | 0.09 | 0.27 | 5.17 | 0.000 | 0.56 | 1.76 | |||
| Energy-joy | −0.31 | 0.08 | −0.18 | −3.78 | 0.000 | 0.66 | 1.50 | |||
| Empathy | −0.40 | 0.10 | −0.29 | −3.90 | 0.000 | 0.27 | 3.58 | |||
| Social skills | 0.17 | 0.07 | 0.10 | 2.38 | 0.018 | 0.75 | 1.32 | |||
| Respect | 0.38 | 0.16 | 0.16 | 2.27 | 0.023 | 0.30 | 3.25 | |||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez-Fuentes, M.d.C.; Molero Jurado, M.d.M.; Martos Martínez, Á.; Gázquez Linares, J.J. Analysis of the Risk and Protective Roles of Work-Related and Individual Variables in Burnout Syndrome in Nurses. Sustainability 2019, 11, 5745. https://doi.org/10.3390/su11205745
Pérez-Fuentes MdC, Molero Jurado MdM, Martos Martínez Á, Gázquez Linares JJ. Analysis of the Risk and Protective Roles of Work-Related and Individual Variables in Burnout Syndrome in Nurses. Sustainability. 2019; 11(20):5745. https://doi.org/10.3390/su11205745
Chicago/Turabian StylePérez-Fuentes, María del Carmen, María del Mar Molero Jurado, África Martos Martínez, and José Jesús Gázquez Linares. 2019. "Analysis of the Risk and Protective Roles of Work-Related and Individual Variables in Burnout Syndrome in Nurses" Sustainability 11, no. 20: 5745. https://doi.org/10.3390/su11205745






