Understanding Out-of-Home Food Environment, Family Restaurant Choices, and Childhood Obesity with an Agent-Based Huff Model
Abstract
1. Introduction
2. Materials and Methods
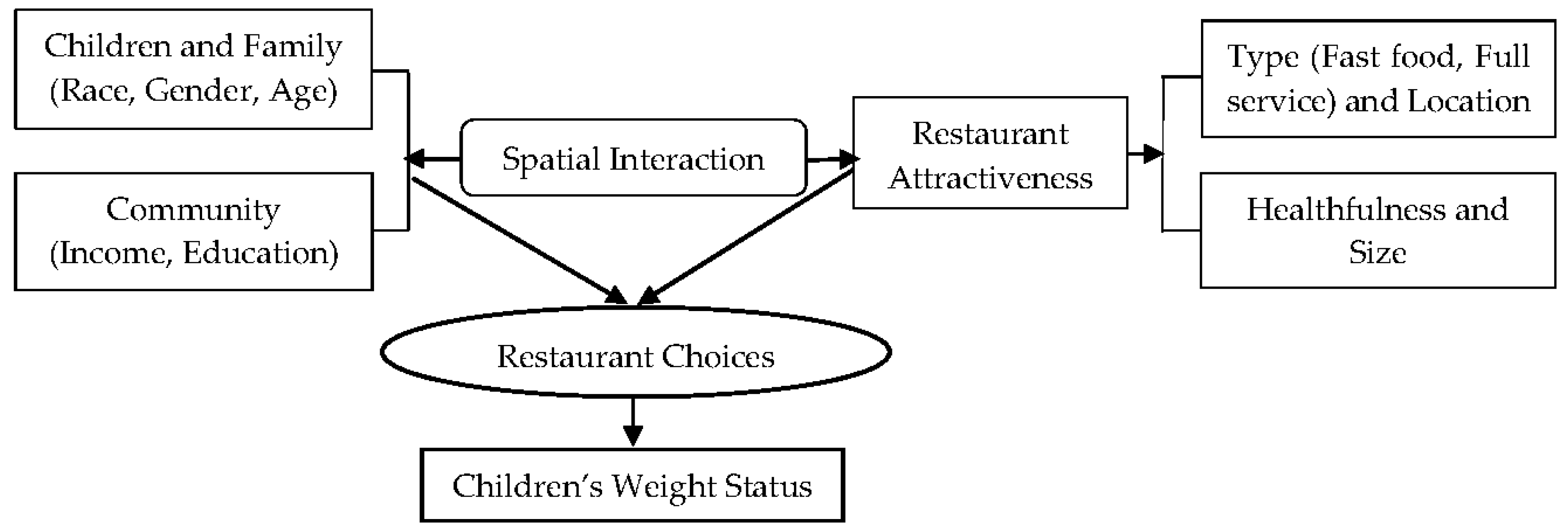
2.1. Analytical Framework
2.2. Study Area
2.3. Survey Assessment of African American Children
2.4. Assessment of Restaurants
2.5. Agent-Based Huff Model
2.6. Statistical Analysis
3. Results
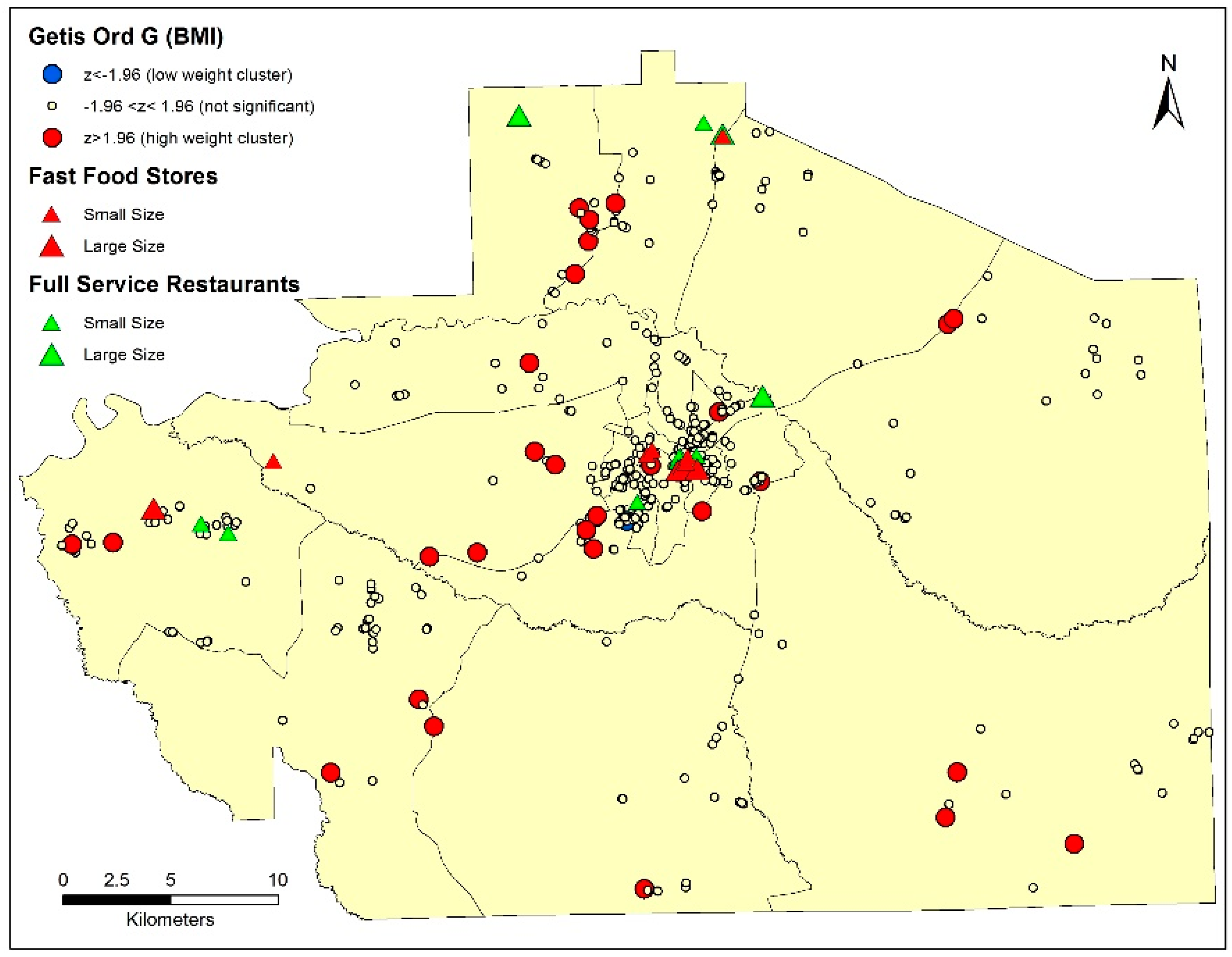
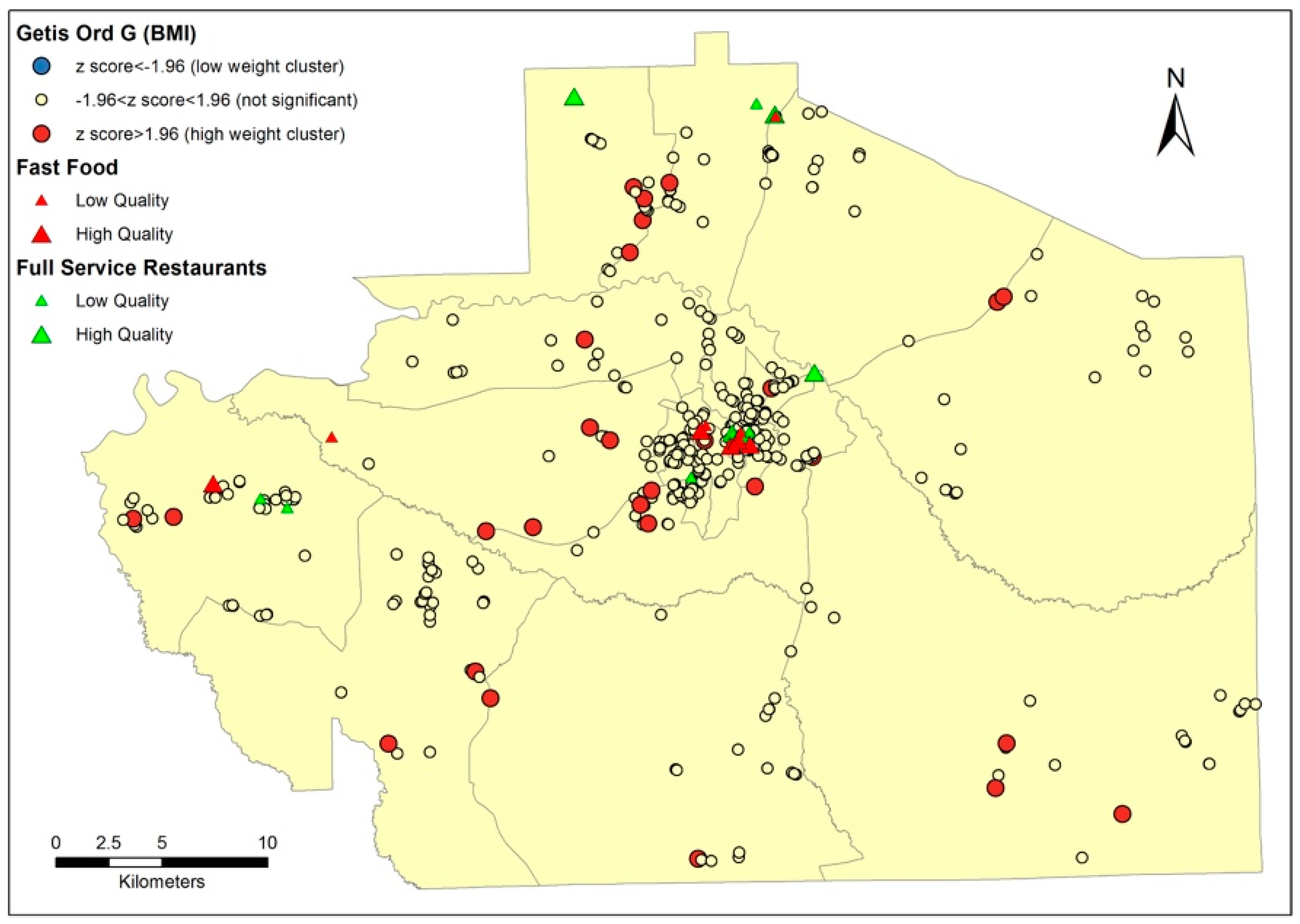
3.1. Children’s Weight Status and Restaurants’ Attractiveness
3.2. Agent-Based Huff Model Validation
3.3. Family Restaurant Choices and Children’s Weight Status
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Zhang, J.; Tong, L.; Lamberson, P.J.; Durazo-Arvizu, R.A.; Luke, A.; Shoham, D.A. Leveraging social influence to address overweight and obesity using agent-based models: The role of adolescent social networks. Soc. Sci. Med. 2015, 125, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Lachat, C.; Nago, E.; Verstraeten, R.; Roberfroid, D.; Van Camp, J.; Kolsteren, P. Eating out of home and its association with dietary intake: A systematic review of the evidence. Obes. Rev. 2012, 13, 329–346. [Google Scholar] [CrossRef] [PubMed]
- Powell, L.M.; Nguyen, B.T.; Han, E. Energy intake from restaurants: Demographics and socioeconomics, 2003–2008. Am. J. Prev. Med. 2012, 43, 498–504. [Google Scholar] [CrossRef] [PubMed]
- United States Department of Agricultural, Economic Research Service. Food Consumption & Demand: Food-Away-from-Home. Available online: http://www.ers.usda.gov/topics/food-choices-health/foodconsumption-demand/food-away-from-home.aspx (accessed on 23 August 2016).
- Josiam, B.M.; Kalldin, A.C.; Duncan, J.L. Using the involvement construct to understand the motivations of customers of casual dining restaurants in the USA. Hosp. Rev. 2015, 31, 9. [Google Scholar]
- National Restaurant Association. Facts at a Glance. Available online: http://www.restaurant.org/research/facts/ (accessed on 29 November 2012).
- An, R. Fast-food and full-service restaurant consumption and daily energy and nutrient intakes in US adults. Eur. J. Clin. Nutr. 2016, 70, 97. [Google Scholar] [CrossRef] [PubMed]
- Goffe, L.; Rushton, S.; White, M.; Adamson, A.; Adams, J. Relationship between mean daily energy intake and frequency of consumption of out-of-home meals in the UK National Diet and Nutrition Survey. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 131. [Google Scholar] [CrossRef] [PubMed]
- Taillie, L.S.; Afeiche, M.C.; Eldridge, A.L.; Popkin, B.M. The contribution of at-home and away-from-home food to dietary intake among 2–13-year-old Mexican children. Public Health Nutr. 2017, 20, 2559–2568. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kasparian, M.; Mann, G.; Serrano, E.L.; Farris, A.R. Parenting practices toward food and children’s behavior: Eating away from home versus at home. Appetite 2017, 114, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Harrington, J.; Fitzgerald, A.P.; Layte, R.; Lutomski, J.; Molcho, M.; Perry, I.J. Sociodemographic, health and lifestyle predictors of poor diets. Public Health Nutr. 2011, 14, 2166–2175. [Google Scholar] [CrossRef] [PubMed]
- Njite, D.; Njoroge, J.; Parsa, H.; Parsa, R.; van der Rest, J.P. Consumer patronage and willingness-to-pay at different levels of restaurant attributes: A study from Kenya. Res. Hosp. Manag. 2015, 5, 171–180. [Google Scholar] [CrossRef]
- Lin, W.L.; Wu, C.C. The Concerns about Choice Attributes and Behavior Intentions of Consumers toward Food Safety Restaurant. Int. Bus. Res. 2016, 9, 11. [Google Scholar] [CrossRef]
- Kim, C.O.; Lee, K.R. Preventive effect of protein-energy supplementation on the functional decline of frail older adults with low socioeconomic status: A community-based randomized controlled study. J. Gerontol. A Biol. Sci. Med. Sci. 2012, 68, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Cruwys, T.; Bevelander, K.E.; Hermans, R.C. Social modeling of eating: A review of when and why social influence affects food intake and choice. Appetite 2015, 86, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Robinson, L.E.; Carter, W.M.; Gupta, R. Childhood obesity and community food environments in Alabama’s Black Belt region. Child Care Health Dev. 2015, 41, 668–676. [Google Scholar] [CrossRef] [PubMed]
- Gordon-Larsen, P.; Nelson, M.C.; Page, P.; Popkin, B.M. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics 2006, 117, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Draxten, M.; Fulkerson, J.A.; Friend, S.; Flattum, C.F.; Schow, R. Parental role modeling of fruits and vegetables at meals and snacks is associated with children’s adequate consumption. Appetite 2014, 78, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ward, D.S.; Vaughn, A.E.; Bangdiwala, S.I.; Campbell, M.; Jones, D.J.; Panter, A.T.; Stevens, J. Integrating a family-focused approach into child obesity prevention: Rationale and design for the My Parenting SOS study randomized control trial. BMC Public Health 2011, 11, 431. [Google Scholar] [CrossRef] [PubMed]
- Oreskovic, N.M.; Kuhlthau, K.A.; Romm, D.; Perrin, J.M. Built environment and weight disparities among children in high-and low-income towns. Acad. Pediatr. 2009, 9, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Powell, L.M.; Nguyen, B.T. Fast-food and full-service restaurant consumption among children and adolescents: Effect on energy, beverage, and nutrient intake. JAMA Pediatr. 2013, 167, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Robson, S.M.; Crosby, L.E.; Stark, L.J. Eating dinner away from home: Perspectives of middle-to high-income parents. Appetite 2016, 96, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Zhang, D. Agent-based simulation of consumer purchase decision-making and the decoy effect. J. Bus. Res. 2007, 60, 912–922. [Google Scholar] [CrossRef]
- Li, Y.; Liu, L. Assessing the impact of retail location on store performance: A comparison of Wal-Mart and Kmart stores in Cincinnati. Appl. Geogr. 2012, 32, 591–600. [Google Scholar] [CrossRef]
- Chasco Yrigoyen, C.; Otero, J.V. Spatial interaction models applied to the design of retail trade areas. In Proceedings of the 38th European Regional Science Association, Vienna, Austria, 23–26 August 1998. [Google Scholar]
- Brown, S. Retail location theory: Evolution and evaluation. Int. Rev. Retail Distrib. Consum. Res. 1993, 3, 185–229. [Google Scholar] [CrossRef]
- Huff, D.L. A probabilistic analysis of shopping center trade areas. Land Econ. 1963, 39, 81–90. [Google Scholar] [CrossRef]
- Vandell, K.; Carter, C. Retail store location and market analysis: A review of the research. JREL 1994, 2, 13–45. [Google Scholar] [CrossRef]
- Dock, J.P.; Song, W.; Lu, J. Evaluation of dine-in restaurant location and competitiveness: Applications of gravity modeling in Jefferson County, Kentucky. Appl. Geogr. 2015, 60, 204–209. [Google Scholar] [CrossRef]
- Thang, D.C.L.; Tan, B.L.B. Linking consumer perception to preference of retail stores: An empirical assessment of the multi-attributes of store image. J. Retail. Consum. Serv. 2003, 10, 193–200. [Google Scholar] [CrossRef]
- Li, Y.; Berenson, J.; Gutiérrez, A.; Pagán, J.A. Leveraging the food environment in obesity prevention: The promise of systems science and agent-based modeling. Curr. Nutr. Rep. 2016, 5, 245–254. [Google Scholar] [CrossRef]
- Page, S.E. Agent-based models. NPDE 2008, 47–52. [Google Scholar] [CrossRef]
- Yang, Y.; Diez-Roux, A.V. Using an agent-based model to simulate children’s active travel to school. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 67. [Google Scholar] [CrossRef] [PubMed]
- Steeves, E.A.; Martins, P.A.; Gittelsohn, J. Changing the food environment for obesity prevention: Key gaps and future directions. Curr. Obes. Rep. 2014, 3, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Schenk, T.A.; Löffler, G.; Rauh, J. Agent-based simulation of consumer behavior in grocery shopping on a regional level. J. Bus. Res. 2007, 60, 894–903. [Google Scholar] [CrossRef]
- Auchincloss, A.H.; Riolo, R.L.; Brown, D.G.; Cook, J.; Roux, A.V.D. An agent-based model of income inequalities in diet in the context of residential segregation. Am. J. Prev. Med. 2011, 40, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Balaraman, V.; Athle, D.; Singh, M. An agent-based exploration of a relationship between daily routines and convenience store footfalls. In Proceedings of the Conference on Summer Computer Simulation, Chicago, IL, USA, 26–29 July 2015. [Google Scholar]
- Richardson, A.S.; Boone-Heinonen, J.; Popkin, B.M.; Gordon-Larsen, P. Are neighbourhood food resources distributed inequitably by income and race in the USA? Epidemiological findings across the urban spectrum. BMJ Open 2012, 2. [Google Scholar] [CrossRef] [PubMed]
- Yeager, C.D.; Gatrell, J.D. Rural food accessibility: An analysis of travel impedance and the risk of potential grocery closures. Appl. Geogr. 2014, 53, 1–10. [Google Scholar] [CrossRef]
- Brofenbrenner, U. The Ecology of Human Development: Experiments by Nature and Design; Harvard University Press: Cambridge, MA, USA; London, UK, 1979. [Google Scholar]
- Huff, D.L. Parameter estimation in the Huff model. ESRI ArcUser. 2003. Available online: http://uat.esri.com/news/arcuser/1003/files/huff.pdf (accessed on 15 May 2017).
- Sallis, J.F.; Owen, N.; Fisher, E. Ecological models of health behavior. In Health Behavior: Theory, Research, and Practice; Glanz, K., Rimer, B.K., Eds.; Josey-Bass: San Francisco, CA, USA, 2008; Volume 5, pp. 43–64. [Google Scholar]
- Bukatko, D.; Daehler, M.W. Child Development: A Thematic Approach; Houghton, Mifflin and Company: Boston, MA, USA, 1995. [Google Scholar]
- Glanz, K. Measuring food environments: A historical perspective. Am. J. Prev. Med. 2009, 36, S93–S98. [Google Scholar] [CrossRef] [PubMed]
- Morland, K.B.; Evenson, K.R. Obesity prevalence and the local food environment. Health Place 2009, 15, 491–495. [Google Scholar] [CrossRef] [PubMed]
- Yun, D.; Silk, K.J. Social norms, self-identity, and attention to social comparison information in the context of exercise and healthy diet behavior. J. Health Commun. 2011, 26, 275–285. [Google Scholar] [CrossRef] [PubMed]
- Grow, H.M.G.; Cook, A.J.; Arterburn, D.E.; Saelens, B.E.; Drewnowski, A.; Lozano, P. Child obesity associated with social disadvantage of children’s neighborhoods. Soc. Sci. Med. 2010, 71, 584–591. [Google Scholar] [CrossRef] [PubMed]
- Hotelling, H. Stability in Competition. Econ. J. 1929, 39, 41–57. [Google Scholar] [CrossRef]
- Nelson, R.L. The Selection of Retail Locations; FW Dodge Corporation: New York, NY, USA, 1958. [Google Scholar]
- Ghosh, A.; Rushton, G. Spatial Analysis and Location-Allocation Models; Van Nostrand Reinhold Company: New York, NY, USA, 1987; ISBN 0-442-22803-1. [Google Scholar]
- Ghosh, A.; McLafferty, S.; Craig, C.S. Multifacility retail networks. In Facility Location: A Survey of Applications and Methods; Springer: New York, NY, USA, 1995; pp. 301–330. [Google Scholar]
- Serra, D.; ReVelle, C. Competitive location in discrete space. J. Econ. Lit. Classif. 1995, 367–386. [Google Scholar] [CrossRef]
- Drezner, T.; Drezner, Z. Lost demand in a competitive environment. J. Oper. Res. Soc. 2008, 59, 362–371. [Google Scholar] [CrossRef]
- Davy, B.M.; Harrell, K.; Stewart, J.; King, D.S. Body weight status, dietary habits, and physical activity levels of middle school-aged children in rural Mississippi. South. Med. J. 2004, 97, 571–578. [Google Scholar] [CrossRef] [PubMed]
- United States Census Bureau. 2010 Census Data. Available online: http://www.census.gov/2010census/data/ (accessed on 20 November 2016).
- Kowalski, K.C.; Crocker, P.R.; Donen, R.M. The Physical Activity Questionnaire for Older Children (PAQ-C) and Adolescents (PAQ-A) Manual; College of Kinesiology, University of Saskatchewan: Saskatoon, SK, Canada, 2004; pp. 1–38. [Google Scholar]
- Centers for Disease Control and Prevention. Defining Childhood Obesity. Available online: https://www.cdc.gov/obesity/childhood/defining.html (accessed on 3 August 2017).
- Glanz, K.; Sallis, J.F.; Saelens, B.E.; Frank, L.D. Nutrition Environment Measures Survey in stores (NEMS-S): Development and evaluation. Am. J. Prev. Med. 2007, 32, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Huddleston, P.; Whipple, J.; Nye Mattick, R.; Jung Lee, S. Customer satisfaction in food retailing: Comparing specialty and conventional grocery stores. Int. J. Retail Distrib. Manag. 2009, 37, 63–80. [Google Scholar] [CrossRef]
- Lukermann, F.; Porter, P.W. Gravity and potential models in economic geography. Ann. Assoc. Am. Geogr. 1960, 50, 493–504. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey 2013–2014. Available online: https://wwwn.cdc.gov/Nchs/Nhanes/Search/nhanes13_14.aspx (accessed on 23 August 2016).
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012, 307, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Jenks, G.F. The Data Model Concept in Statistical Mapping. Int. Yearb. Cartogr. 1967, 7, 186–190. [Google Scholar]
- Hirsch, J.A.; Hillier, A. Exploring the role of the food environment on food shopping patterns in Philadelphia, PA, USA: A semiquantitative comparison of two matched neighborhood groups. Int. J. Environ. Res. Public Health 2013, 10, 295–313. [Google Scholar] [CrossRef] [PubMed]
- Fotheringham, A.S. Spatial structure and distance-decay parameters. Ann. Assoc. Am. Geogr. 1981, 71, 425–436. [Google Scholar] [CrossRef]
- Bao, K.Y.; Tong, D. The effects of spatial scale and aggregation on food access assessment: A case study of Tucson, Arizona. Prof. Geogr. 2017, 69, 337–347. [Google Scholar] [CrossRef]
- Shannon, J. Beyond the supermarket solution: Linking food deserts, neighborhood context, and everyday mobility. Ann. Assoc. Am. Geogr. 2016, 106, 186–202. [Google Scholar] [CrossRef]
- Widener, M.J.; Minaker, L.; Farber, S.; Allen, J.; Vitali, B.; Coleman, P.C.; Cook, B. How do changes in the daily food and transportation environments affect grocery store accessibility? Appl. Geogr. 2017, 83, 46–62. [Google Scholar] [CrossRef]
- Farley, T.A.; Rice, J.; Bodor, J.N.; Cohen, D.A.; Bluthenthal, R.N.; Rose, D. Measuring the food environment: Shelf space of fruits, vegetables, and snack foods in stores. J. Urban Health 2009, 86, 672–682. [Google Scholar] [CrossRef] [PubMed]
- Shier, V.; Nicosia, N.; Datar, A. Neighborhood and home food environment and children’s diet and obesity: Evidence from military personnel’s installation assignment. Soc. Sci. Med. 2016, 158, 122–131. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Kawachi, I. Diets and health: How food decisions are shaped by biology, economics, geography, and social interactions. Big Data 2015, 3, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Larson, N.; Neumark-Sztainer, D.; Laska, M.N.; Story, M. Young adults and eating away from home: Associations with dietary intake patterns and weight status differ by choice of restaurant. J. Am. Diet. Assoc. 2011, 111, 1696–1703. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Yuan, N.J.; Zheng, K.; Lian, D.; Xie, X.; Rui, Y. Exploiting dining preference for restaurant recommendation. In Proceedings of the 25th International Conference on World Wide Web, Montreal, QC, Canada, 11–15 April 2016. [Google Scholar]
- Burdette, H.L.; Whitaker, R.C. Neighborhood playgrounds, fast food restaurants, and crime: Relationships to overweight in low-income preschool children. Prev. Med. 2004, 38, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Crawford, D.A.; Timperio, A.F.; Salmon, J.A.; Baur, L.; Giles-Corti, B.; Roberts, R.J.; Jackson, M.L.; Andrianopoulos, N.; Ball, K. Neighbourhood fast food outlets and obesity in children and adults: The CLAN Study. Pediatr. Obes. 2008, 3, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Fleischhacker, S.E.; Evenson, K.R.; Rodriguez, D.A.; Ammerman, A.S. A systematic review of fast food access studies. Obes. Rev. 2011, 12. [Google Scholar] [CrossRef] [PubMed]
- Lee, H. The role of local food availability in explaining obesity risk among young school-aged children. Soc. Sci. Med. 2012, 74, 1193–1203. [Google Scholar] [CrossRef] [PubMed]
- Powell, L.M.; Han, E.; Chaloupka, F.J. Economic Contextual Factors, Food Consumption, and Obesity among US Adolescents. J. Nutr. 2010, 140, 1175–1180. [Google Scholar] [CrossRef] [PubMed]
- Alviola, P.A., IV; Nayga, R.M., Jr.; Thomsen, M.R.; Danforth, D.; Smartt, J. The effect of fast-food restaurants on childhood obesity: A school level analysis. Econ. Hum. Biol. 2014, 12, 110–119. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.C.; Wilson, J.S.; Qi, R.; Ying, J. Green neighborhoods, food retail and childhood overweight: Differences by population density. Am. J. Health Promot. 2007, 21, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Mehta, N.K.; Chang, V.W. Weight status and restaurant availability: A multilevel analysis. Am. J. Prev. Med. 2008, 34, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Nicklas, T.; Johnson, R. Position of the American Dietetic Association: Dietary guidance for healthy children ages 2 to 11 years. J. Am. Diet. Assoc. ISO 2004, 104, 660–677. [Google Scholar] [CrossRef]
- Wootan, M.G. Children’s meals in restaurants: Families need more help to make healthy choices. Child. Obes. 2012, 8, 31–33. [Google Scholar] [CrossRef] [PubMed]
- Cohen, D.A.; Story, M. Mitigating the health risks of dining out: The need for standardized portion sizes in restaurants. Am. J. Public Health 2014, 104, 586–590. [Google Scholar] [CrossRef] [PubMed]
- Wansink, B.; Hanks, A.S. Calorie reductions and within-meal calorie compensation in children’s meal combos. Obesity 2014, 22, 630–632. [Google Scholar] [CrossRef] [PubMed]
- Anzman-Frasca, S.; Mueller, M.P.; Sliwa, S.; Dolan, P.R.; Harelick, L.; Roberts, S.B.; Washburn, K.; Economos, C.D. Changes in children’s meal orders following healthy menu modifications at a regional US restaurant chain. Obesity 2015, 23, 1055–1062. [Google Scholar] [CrossRef] [PubMed]
- Lee-Kwan, S.H.; Bleich, S.N.; Kim, H.; Colantuoni, E.; Gittelsohn, J. Environmental intervention in carryout restaurants increases sales of healthy menu items in a low-income urban setting. Am. J. Health Promot. 2015, 29, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, M.B.; Puhl, R. Childhood obesity: A societal problem to solve. Obes. Rev. 2003, 4, 57–71. [Google Scholar] [CrossRef] [PubMed]
- Larsen, J.K.; Hermans, R.C.J.; Sleddens, E.F.C.; Vink, J.M.; Kremers, S.P.J.; Ruiter, E.L.M.; Fisher, J.O. How to bridge the intention-behavior gap in food parenting: Automatic constructs and underlying techniques. Appetite 2018, 123, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Alderson, T.S.J.; Ogden, J. What do mothers feed their children and why? Health Educ. Res. 1999, 14, 717–727. [Google Scholar] [CrossRef][Green Version]
| Survey Questions | Scoring (p-Point) |
|---|---|
| Availability of Healthful Options | |
| # of healthy dishes/entrees | 1 = 1 p; 2–4 = 2 ps; 5 or more = 3 ps. |
| # of healthy main-dish salads | 1 = 1 p; 2–4 = 2 ps; 5 or more = 3 ps. |
| Facilitators of healthy eating | |
| Nutrition information on menu or healthy entrees identified on menu | Yes for EITHER = 1 p |
| Highlighting healthy options or healthy eating encouraged | Yes for EITHER = 1 p |
| Barriers to healthful eating | |
| Large portions encouraged | Yes = −1 |
| “All you can eat” or “unlimited” available | Yes = −1 |
| Kid’s menu | |
| 1% or nonfat milk availability | Yes = 1 |
| Unhealthy dessert automatic | Yes = −1 |
| Categories | Probability to Fast Food | Probability to Full Service | |
|---|---|---|---|
| Children | Boys | 70.7% | 29.3% |
| Girls | 69.9% | 30.1% | |
| Community (block group) | Education | % of population without high school degree × 71.2% + % of population with high school degree or above × 62.3% | % of population without high school degree × 28.8% + % of population with high school degree or above × 37.7% |
| MHHI < Poverty line | 75.6% | 24.4% | |
| MHHI > Poverty line | 68.5% | 31.5% | |
| Restaurants | Fast Food | Probability that a family chooses each restaurant estimated by Huff’s model | |
| Full-Service | |||
| Category | Type | Students | Overweight | Obese | Overweight and Obese |
|---|---|---|---|---|---|
| All | 613 | 15.6% | 26.4% | 42.1% | |
| Age | 4–6 | 130 | 15.4% | 18.4% | 33.8% |
| 7–9 | 300 | 17.3% | 27.0% | 44.3% | |
| 10–13 | 183 | 13.1% | 31.2% | 44.3% | |
| Gender | Male | 301 | 16.6% | 24.9% | 41.5% |
| Female | 312 | 14.7% | 28.2% | 42.9% |
| ID | Type | Size (sq. ft.) | Healthfulness Score | Average Distance to Family (Meters) | ||||
|---|---|---|---|---|---|---|---|---|
| AHO | FHE | BHE | KM | Total | ||||
| 0 | FS | 280 | 3 | 1 | −1 | 0 | 3 | 8615.77 |
| 1 | FS | 168 | 4 | 2 | 0 | 2 | 8 | 8590.27 |
| 2 | FS | 75 | 5 | 2 | −1 | 2 | 8 | 8590.26 |
| 3 | FS | 595 | 7 | 3 | −1 | 0 | 9 | 8654.06 |
| 4 | FS | 766 | 7 | 0 | 0 | 4 | 11 | 11,305.4 |
| 5 | FS | 172 | 3 | 0 | 0 | 0 | 3 | 8880.14 |
| 6 | FS | 345 | 9 | 3 | 0 | 3 | 15 | 19,900.39 |
| 7 | FS | 256 | 8 | 2 | −1 | 0 | 9 | 19,093.55 |
| 8 | FS | 328 | 6 | 1 | 0 | 3 | 10 | 8738.92 |
| 9 | FS | 189 | 5 | 2 | 0 | 3 | 10 | 8760.47 |
| 10 | FS | 350 | 9 | 1 | 1 | 2 | 13 | 18,815.11 |
| 11 | FS | 133 | 4 | 2 | 0 | 2 | 8 | 21,099.52 |
| 12 | FS | 110 | 4 | 2 | 0 | 2 | 8 | 20,081.69 |
| 13 | FS | 322 | 6 | 1 | 0 | 3 | 10 | 8721.51 |
| 14 | FS | 169 | 9 | 1 | 0 | 0 | 10 | 8653.13 |
| 0 | FF | 203 | 6 | 3 | −1 | 5 | 13 | 8617.82 |
| 1 | FF | 306 | 5 | 3 | −2 | 7 | 13 | 8872.48 |
| 2 | FF | 186 | 5 | 3 | −2 | 0 | 6 | 8531.85 |
| 3 | FF | 198 | 0 | 3 | −2 | 0 | 1 | 8708.51 |
| 4 | FF | 155 | 0 | 0 | −1 | 0 | −1 | 8745.36 |
| 5 | FF | 119 | 0 | 0 | −1 | −1 | −2 | 18,453.77 |
| 6 | FF | 312 | 7 | 4 | −3 | 0 | 8 | 8687.59 |
| 7 | FF | 240 | 1 | 0 | 0 | 1 | 1 | 18,744.39 |
| 8 | FF | 286 | 7 | 4 | −3 | 0 | 8 | 23,007.61 |
| 9 | FF | 142 | 1 | 0 | 0 | 0 | 1 | 8578.25 |
| 10 | FF | 217 | 0 | 3 | −2 | 0 | 1 | 8644.40 |
| Distance Beta | Size | Healthfulness | ||
|---|---|---|---|---|
| Fast Food | Full-Service | Fast Food | Full-Service | |
| Beta = 0 | 0.76 | 0.57 | 0.81 | 0.55 |
| Beta = 0.5 | 0.56 | 0.56 | 0.71 | 0.60 |
| Beta = 1 | 0.63 | 0.58 | 0.65 | 0.59 |
| Beta = 1.5 | 0.63 | 0.57 | 0.79 | 0.57 |
| Beta = 2 | 0.64 | 0.57 | 0.65 | 0.59 |
| Beta = 2.5 | 0.66 | 0.54 | 0.78 | 0.60 |
| Beta = 3 | 0.71 | 0.60 | 0.76 | 0.57 |
| Beta = 3.5 | 0.74 | 0.56 | 0.57 | 0.57 |
| Beta = 4 | 0.94 | 0.54 | 0.96 | 0.59 |
| Distance Beta | Size | Healthfulness | ||
|---|---|---|---|---|
| Fast Food | Full-Service | Fast Food | Full-Service | |
| Beta = 0 | <0.01 | <0.01 | <0.01 | <0.01 |
| Beta = 0.5 | <0.01 | <0.01 | <0.01 | <0.01 |
| Beta = 1 | <0.01 | <0.01 | <0.01 | <0.01 |
| Beta = 1.5 | <0.01 | <0.01 | <0.01 | <0.01 |
| Beta = 2 | <0.01 | <0.01 | <0.01 | <0.01 |
| Beta = 2.5 | <0.01 | <0.01 | <0.01 | <0.01 |
| Beta = 3 | <0.01 | <0.01 | <0.01 | <0.01 |
| Beta = 3.5 | <0.01 | <0.01 | <0.01 | <0.01 |
| Beta = 4 | <0.01 | <0.01 | <0.01 | <0.01 |
| Fast Food | High Quality FF | Low Quality FF | Full Service | High Quality FS | Low Quality FS | ||
|---|---|---|---|---|---|---|---|
| Aj = size (β = 3) | Weight | −0.034 | −0.077 * | −0.033 | 0.072 * | 0.028 | 0.084 ** |
| Aj = healthfulness (β = 2.5) | Weight | 0.013 | −0.004 | −0.010 | 0.050 | −0.023 | 0.034 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; Du, T.; Peng, J. Understanding Out-of-Home Food Environment, Family Restaurant Choices, and Childhood Obesity with an Agent-Based Huff Model. Sustainability 2018, 10, 1575. https://doi.org/10.3390/su10051575
Li Y, Du T, Peng J. Understanding Out-of-Home Food Environment, Family Restaurant Choices, and Childhood Obesity with an Agent-Based Huff Model. Sustainability. 2018; 10(5):1575. https://doi.org/10.3390/su10051575
Chicago/Turabian StyleLi, Yingru, Ting Du, and Jian Peng. 2018. "Understanding Out-of-Home Food Environment, Family Restaurant Choices, and Childhood Obesity with an Agent-Based Huff Model" Sustainability 10, no. 5: 1575. https://doi.org/10.3390/su10051575
APA StyleLi, Y., Du, T., & Peng, J. (2018). Understanding Out-of-Home Food Environment, Family Restaurant Choices, and Childhood Obesity with an Agent-Based Huff Model. Sustainability, 10(5), 1575. https://doi.org/10.3390/su10051575




