1. Introduction
Human activities, such as irresponsible depletion of limited natural resources and pollution, push our planet towards its boundaries [
1,
2] and foster the debate over environmental protection measures and the necessity of corporate environmental management [
3,
4]. Several researchers have discussed mandatory and voluntary environmental management initiatives in order to reduce negative corporate environmental impacts [
5,
6,
7,
8,
9]. Among the voluntary initiatives that should improve organizational environmental performance beyond the legal requirements is the implementation of an environmental management system (EMS) [
9,
10].
EMSs can be defined as “part of the general management system which includes the organizational structure, planning of activities, responsibilities, practices, procedures, processes and resources for developing, implementing, carrying out, reviewing and maintaining the organization’s environmental policy” [
11]. The internal and external benefits of such structured management approaches—which systematize existing processes within the organizations—are various (e.g., see [
12]). With the help of this management approach, it is possible to reveal potential for optimization of environmental inputs and outputs (for example, see [
13], who researched the question of how EMSs impact environmental performance). Furthermore, the implementation of a formal EMS can increase organizational and management efficiency [
10,
14], and ensure legal compliance [
14]. Further, it can impact economic performance [
15,
16], corporate performance [
17], and competitiveness [
18].
It is popular to certify or validate EMSs according to the international standard ISO 14001 or according to the European EMAS Regulation (Eco-Management and Audit Scheme). Despite many similarities in the elements, EMAS has some additional demands, such as external verification, the preparation of an environmental statement, or stricter requirements to publish information ([
19]; for detailed information on EMAS see [
20]). EMAS and ISO 14001 are said to have different foci: whereas ISO 14001 shall improve management, EMAS shall improve environmental performance [
19]. Organizations being validated according to EMAS are listed in a publicly available register. Information on ISO 14001 certified organizations is not centrally available.
Originally designed for the industrial sector, EMAS can be applied in all organizations following its revision in the year 2001 (Regulation (EC) No. 761/2001). For organizations, several potential benefits are connected to EMAS implementation. Literature demonstrates that EMAS can increase environmental performance [
10,
21,
22,
23], or is at least perceived to improve it [
19,
24,
25]. EMAS also represents a potential source for innovation [
26,
27]. Furthermore, external verification through EMAS can be communicated to corporate stakeholders and can have an impact on competitive performance [
10,
27]. Despite the offered advantages, EMAS diffusion lags behind expectations in this field and a trend can actually be seen that suggests fewer new registrations and increasing numbers of withdrawals [
28,
29]. It is important to understand the critical factors that are leading to decreasing numbers of registered organizations [
29]. To understand the reasons behind the withdrawals, the barriers encountered in EMAS implementation can provide valuable insights [
29].
The critical factors regarding EMS adoption have been addressed by previous research for EMS in general or, more specifically, for ISO 14001 or EMAS. Hillary [
12] describes the internal and external barriers for EMS adoption. The internal barriers are connected to human resources, lack of understanding and perception, problems with implementation, negative attitudes, and culture. The external barriers include problems with the certifier or verifier, economics, institutional weakness, lacking support, and guidance. In their systematic literature review on ISO 14001 implementation, Boiral et al. [
30] list the following obstacles: costs, superficial adoption, paperwork, time constraints, resistance to change, and lack of capabilities. Regarding EMAS, Strachan et al. [
31] and Strachan [
32] researched problems encountered for UK EMAS registered companies regarding the EMAS elements of environmental policy, review, program, management system, audit, statement, and validation. Daddi et al. [
28] list lack of resources, lack of stakeholder recognition, and uncertainty about the value of EMAS as reasons for withdrawal in Spain (see also [
33] for EMAS withdrawal in Italy).
EMS implementation has been researched in, for example, the Chinese hotel industry [
34], the Lebanese food industry [
35], industries along the coast of Cameroon [
36], and small and medium-sized enterprises (SMEs) [
12,
14]. Regarding ISO 14001, research has been conducted in, for example, industrial companies [
37], the Turkish construction industry [
38], and the Spanish automotive industry [
39]. Merli et al. [
40] reviewed and surveyed critical factors that EMAS registered companies experience in Italy (see also [
41]). Álvarez-García and del RíoRama [
42] researched barriers regarding EMAS implementation in Spain. Despite the existing research on EMS in general and, more specifically, on EMAS and ISO 14001, current information is limited regarding EMS in the healthcare sector or hospitals. So far, only two papers have researched EMS implementation in the healthcare sector (see the literature review conducted by Tourais and Videira [
43]). Two studies by Dettenkofer et al. [
44,
45] investigated EMAS implementation in a university hospital. They focused on initial implementation in a single hospital and did not reveal broader insights regarding barriers. Furthermore, Lizzi et al. [
46] described an initial environmental analysis in an Oncology Reference Center in Italy. This can be seen as a basis for EMS implementation in hospitals. However, they focused on the environmental operational indicator “waste” and did not describe problems connected to EMS certification. Ryan-Fogarty et al. [
47] described the adaptation of voluntary measures and initiatives according to the national Green Campus Programme in an Irish university hospital. Again, the study did not look at the obstacles for implementation of such initiatives.
Hospitals are important societal actors that require substantial public financial resources. Their core mission encompasses the safe treatment of patients and ensuring high standards of living. In the sustainability debate, they have long been overlooked [
48]. The sustainability challenge for hospitals is said to encompass three key factors that need to be balanced: the needs of patients, economic issues, and environmental issues [
49]. However, when talking about sustainability, the focus in the healthcare sector has long been on financial issues [
50,
51,
52], with environmental influences and responsibilities of hospitals given a lower priority [
53]. As the literature demonstrates, hospitals consume materials, energy, and water and release various forms of waste and emissions into the water, soil, and air through their clinical activities [
54,
55,
56,
57,
58,
59,
60]. Accompanying services—such as transportation (e.g., of patients, staff, and visitors, but also of purchased goods and wastes), laundry, and food delivery—contribute to their environmental footprint. All activities connected to medical services contribute to environmental harm. They pose environmental risks that can lead to health burdens [
61,
62] and more demand for medical treatment. However, hospitals are slow in adopting proactive environmental strategies [
48].
This study enriches existing research by shedding light on the under-researched area of EMS implementation in hospitals. In total, more than 2000 hospitals are listed in the Krankenhausverzeichnis (a register for all German hospitals) in Germany, of which 22 hospitals are validated according to EMAS. Expert interviews with responsible environmental managers in German EMAS hospitals have been conducted, asking for their experiences with EMAS and especially for any encountered problems. Thus, the aim of this paper is to reveal existing barriers regarding EMS adoption according to EMAS. The focus is on internal problems, as they are found to impede progress quite significantly at the beginning of the implementation process [
12]. Fields of action are deduced in order to reduce existing problems or prevent them from occurring in the future.
The contribution of this paper is of practical and scientific nature. First, this paper is aimed at hospitals and other organizations that want to successfully operate their EMS according to EMAS, prevent its failure, and save resources that might become necessary to overcome problems. Second, consultants, reviewers, and political actors can gain a better understanding of the problems regarding EMS implementation in organizational practice. Thus, this paper, with its systematization of the barriers in a model, helps to build knowledge and creates awareness of the challenges surrounding the implementation of voluntary environmental management measures in practice in the respective organization, as well as being relevant for other important stakeholders. This paper represents a starting point to discuss measures to either avoid, mitigate, or more actively manage future problematic issues and assists in successful implementation and revalidation of an EMS. Third, researchers from several fields, such as environmental and sustainability management or healthcare and hospital management, are provided with insights into the interesting and so far under-researched area of hospital environmental management. Thus, the scientific community can develop and test theoretical concepts and solutions in future research.
The paper is structured as follows. The subsequent section provides information on the data collection. In the third section, the results from the expert interviews are described. These results are discussed and synthesized in a model in
Section 4.
Section 5 presents conclusions, limitations, and implications.
2. Materials and Methods
In this study, the barriers for EMAS in the context of German hospitals were empirically researched with the following research question in mind: Which barriers do hospitals experience within EMAS adoption? In order to answer this research question, expert interviews were conducted with responsible environmental managers. The EMAS hospitals are in a publicly accessible list, which can be found online (
www.emas-register.de). In the year 2016, 22 hospitals were registered. We contacted and asked all registered hospital to participate in the study. After several inquiries, 14 telephone interviews were arranged. The interviewees were guaranteed anonymity.
Table 1 displays some aggregated background information on the hospitals participating in the study.
The interviewees were the responsible environmental manager or the environmental management representative of their organization and had functions such as Technical Director or their representatives, Quality Management Officer, Head of the Departments of Administration, Economy, Ecology, or Team Manager Care/Logistics. The majority of the interviewees accompanied the system from the very beginning in the hospitals and, thus, are very experienced in the field of environmental management and EMAS.
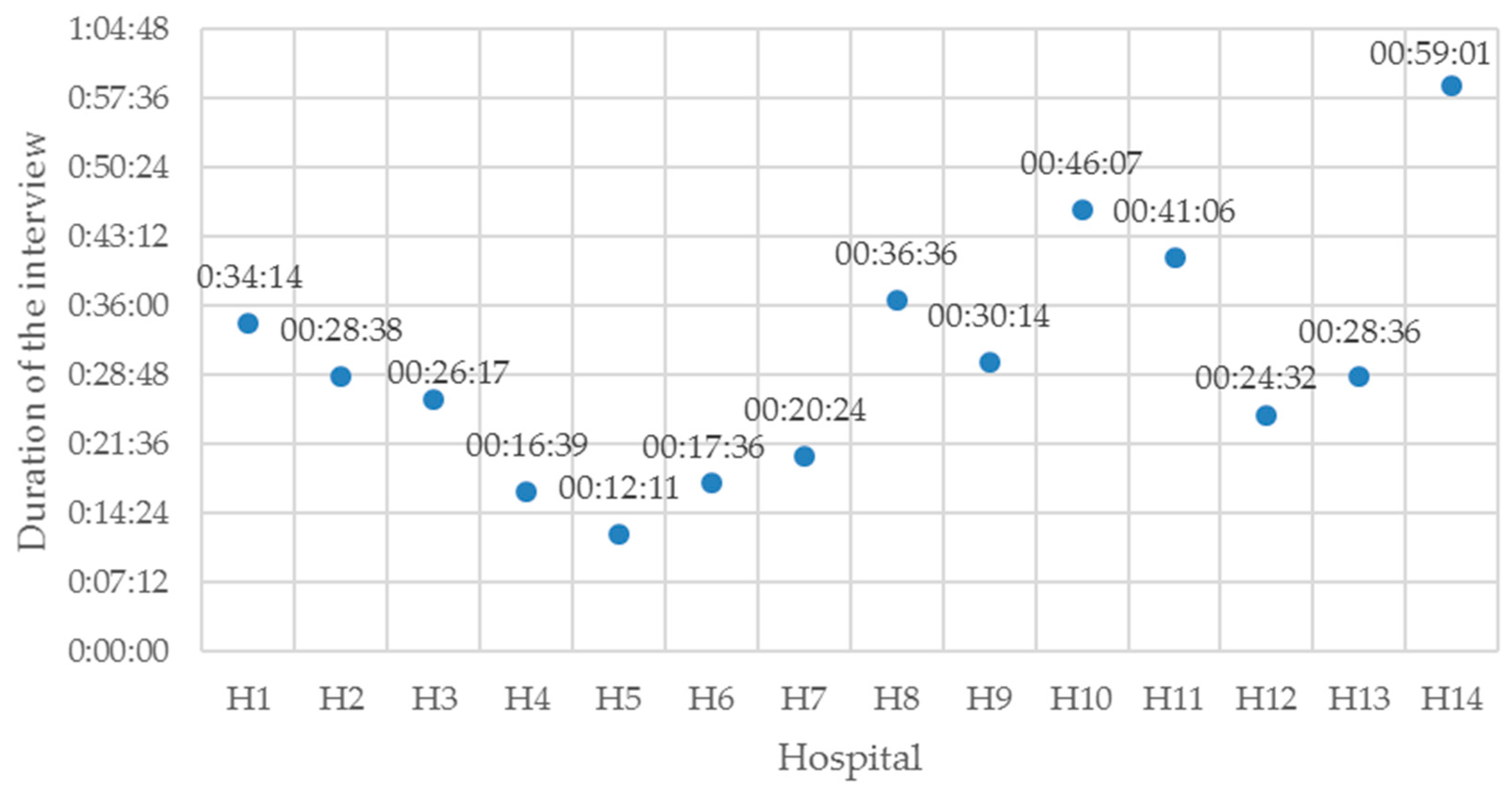
The results presented in this paper are part of a larger interview study on EMAS implementation in German hospitals addressing issues beyond barriers for adoption. A handbook was developed for these interviews; thus, the interviews were structured in advance. The answers were open-ended. The guide included questions on, for example, the interviewee, the registered hospital, the environmental management in the hospital, EMAS implementation in the hospital, and stages that have been problematic within EMAS implementation and reasons for the problems. The interviewer encouraged the hospital environmental managers to name additional information and comment on issues whenever they felt it was necessary. The duration of the 14 interviews in sum was 7 h and 49 min. The single interviews lasted between 12 and 59 min (mean value: 29 min). The duration of the interviews with the hospitals (H1–H14) can be seen in
Figure 1. The variance in the duration of the interviews is mainly due to personal time constraints of the interviewees (e.g., H5) or their willingness to provide deeper insights (e.g., H14).
The interviews were recorded and transcribed, with the transcripts being used for anonymous analysis. These documents were then coded, and content was analyzed by means of the coding software MAXQDA12. The language of the coded material is German.
3. Results
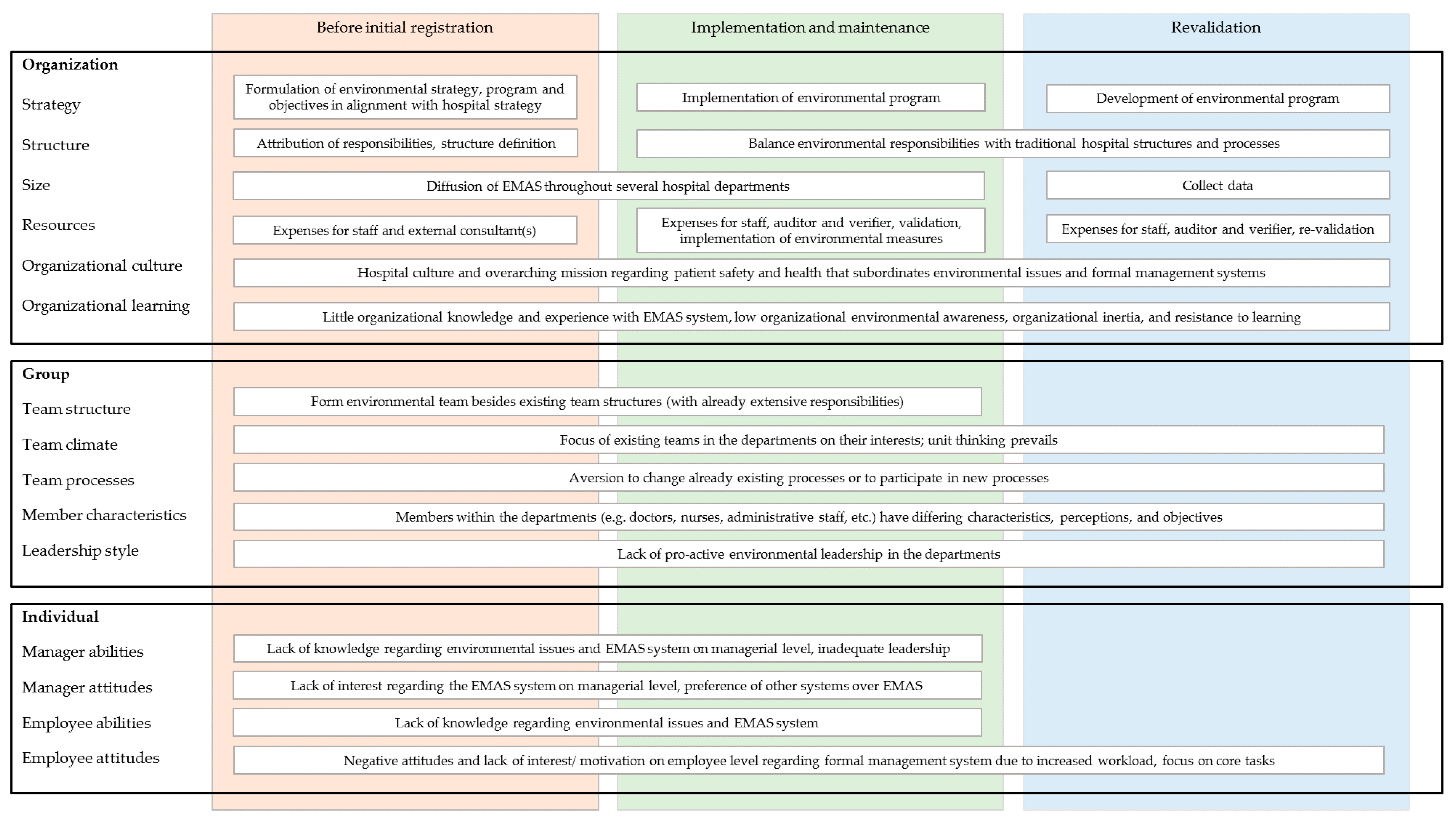
In this section, the barriers the hospital environmental managers mentioned regarding EMAS are described. The results are grouped chronologically, starting with concerns before the initial EMAS registration. Subsequently, problems that arose at the time of EMAS implementation, maintenance, and revalidation of the system are presented. Some illustrative quotes from the interviews are presented alongside the results as supporting evidence. Finally, the barriers are synthesized in a model combining this chronological perspective with the level of analysis, i.e., the organizational, group, and individual level.
3.1. Barriers on the Way towards Initial EMAS Registration
As described by the interviewees, one of the biggest problems facing the hospitals was that they could not estimate in advance how much effort the decision for EMAS would mean for them (e.g., H4, H6, H8, H10, H13). Since there was no experience regarding the introduction of EMAS in hospitals, the area was a black box for them (e.g., H1, H8, H14). They simply had too little knowledge on environmental management systems. The majority reported that it took them around 2 years from initial decision and implementation until the first validation took place (e.g., H5, H6, H7, H8, H12). Some hospitals reported that they already considered some environmental issues before they strived for EMAS validation, for example, they already had an environmental policy (H1), collected data on consumption (H2, H10), had been active in environmental protection in some fields (H5, H8, H11), had other certifications (H6, H7), or thought about environmental issues (H13). Others did not have a detailed concept (H3, H9, H12, H14) and introduced the environmental management with EMAS.
Some hospitals reported that they relied on professional advice from external consultants to support EMAS implementation in order to overcome the lack of knowledge barrier (e.g., H1, H6, H14). However, experience in the field of hospital environmental management and EMAS validation was not only limited early on in the hospitals, but also in the consultancy (H1). The difficulty for hospitals was the choice of a suitable consultant (i.e., finding someone who was familiar with the hospital setting and related environmental issues (e.g., H6, H8)). A further challenge for the hospitals was to balance environmental protection with the primary task of hospitals, the treatment of patients (H8, H9). The institutions’ primary goals limit the time they can devote to EMAS, which is seen as a secondary goal within the organizational strategy (H6, H9). Eventually, this distinctive characteristic of hospital culture also had to be recognized by the consultants (H8). Another practical problem was finding a consultant with the resources and time to commit to the task at hand (H6).
“One problem was that this implementation was uncharted territory, also for our consultants or even for an external consultant. And that at the beginning, a thick pamphlet was created with all the rules and standards according to the motto ‘the more extensive, the better’.”
(H1)
After having decided for EMAS, several interviewees described this bureaucracy as a main barrier they had experienced (H1, H3, H6, H11). Especially for the early adopters of EMAS, putting together all the necessary paperwork to formulate an environmental policy, program, and realistic objectives proved to be quite challenging (e.g., H1, H2, H3, H5, H8, H11). Setting up the legal register was also a challenge for the hospitals (H9, H12).
“So, the most problematic, I think, was the very first step ever to say, I choose EMAS. Well, that was by far the highest hurdle. And I believe … the second hurdle is when a hospital decides to write the environmental policy. Then also to create the environmental management handbook, completely without any external support, either from a consultant or from another hospital (...) to look at what they are doing, to investigate. This is very difficult.”
(H8)
The first hospitals could not benefit much from experience in the field of EMAS implementation. For many hospitals, environmental management systems and their auditing were very theoretical (H2, H11). Companies that started later with EMAS were said to have benefited from certain experiences (H1). For some hospitals, it was very difficult to estimate in advance how much effort would really be required for documents needed for a successful EMAS registration and validation (e.g., H1).
Another issue was to create awareness and acceptance among the employees (H3, H5). The employees feared that lot more work would be required in addition to their current tasks (e.g., H6, H8, H10, H13). For example, one interviewee mentioned problems in convincing employees to contribute to writing the environmental manual (H5). An additional task, like EMAS validation, did not garner much enthusiasm, as other tasks have to be fulfilled in parallel, which put the employees already under pressure (H8).
“So, in particular, the therapeutic and nursing staff were not enthusiastic, so to speak, when, in addition to their other difficult issues with which they have to deal with every day, now the environmental issue comes around the corner.”
(H8)
Therefore, defining structures and responsibilities was a problem for some hospitals (e.g., H4). Finding employees who were interested in performing the tasks required by EMAS (e.g., participating in the environmental commission) was difficult, especially finding someone who was really committed to environmental issues and was not just there because he was obliged to (e.g., H3).
“Maybe, in principle, to create the structure and the environmental commission… to familiarize with the whole issue. That in fact might have been the main problem.”
(H4)
“… of course the manpower that you have to put in there. Taking along the staff, the working groups, the committees that meet… that are obstacles where I would say one can quickly reach the limits.”
(H12)
One problem reported in H2 was that too many people were involved in the environmental management working group at the beginning. The meetings were very frequent in the preparatory phase. Some participants felt that this was lost time because they were unable to contribute anything to the meetings. There were often negative attitudes in these meetings. A positive change could be realized by replacement of the environmental management consultant. The new one built up a more compact core group of participants and reduced the number of meetings.
3.2. Barriers for Validation, Maintenance, and Revalidation
3.2.1. Barriers for Validation
For many hospitals, the procedure of an environmental audit was new to them (e.g., H3, H6, H8). They had difficulties predicting which topics auditors and verifiers might focus on. It was not always understood that the reviewers would go to each department and question the reports (H8). For some employees, the audit was an unfamiliar and stressful situation (e.g., H6). They had to prepare mentally for a survey situation and face critical questions by the auditor on figures and processes. Information and explanations that had not been previously requested had to be provided by the employees on-site (H3).
“Then, to deal with it mentally… these are the things that I do and numbers that I deliver, which are then also questioned again. That was new for some employees. That sometimes led to some difficulties at the beginning, but eventually it worked out, as they say.”
(H8)
It was reported that the audits themselves cost a lot of time (e.g., H10). This is working time that is taken away from other topics in the respective departments. Furthermore, conducting the audit creates costs for the hospital, for example, for the services of the auditor who assesses the hospital. This is a financial burden for the hospitals (H10).
3.2.2. Barriers for Maintenance
After becoming registered, the hospital managers reported several problems. The interviewees stated that it is difficult to reach the entire workforce and communicate the importance of EMAS and environmental issues in the various departments of the hospital (e.g., H2, H9, H14).
“Of course you have to try to communicate well internally. You can not only say that you have an environmental management system now.”
(H8)
To motivate employees and keep them motivated was very often named as being problematic (e.g., H1, H2, H5, H8, H9, H11).
“Through various media, be it the intranet or employee newspaper, we try to address such topics again and again, but realize that this often goes in one ear and out the other.”
(H2)
For the responsible EMAS managers, the challenge is, on the one hand, to meet the theoretical requirements of EMAS, but, on the other hand, to see these brought into action in the individual areas of the hospital by making the application practical and uncomplicated (H11).
“…so it does not degenerate into simply writing stuff (...) and the actual practice comes up short. That’s what the employees do not want. They do not want additional documents and procedures and work instructions.”
(H11)
According to the interviews, different groups in hospitals respond differently to EMAS (H9, H10, H14). Doctors and nurses feel less committed to the EMAS goals than, for example, employees in the technical department, the economic department, or the nursery. Chief physicians were said to be more critical of management systems than normal doctors (H10). Our interviewees emphasized that, in the approach to the employees, one has to keep in mind that the departments have different levels of access to the topic. The closer the employees are to the patients, the less environmental aspects matter because the health of the patient takes priority (H9). In addition, the link between individual behavior in the department and environmental performance of the hospital is not always seen. It was also reported by H2 that influencing and changing the attitudes and behavior of employees is difficult. Bad practices in their private lives are said to be continued at work.
“When they separate the waste at home sloppily, then that employee separates the waste here in the clinic sloppily was well. In my eyes, it’s hard change this.”
(H2)
When implementing measures to improve environmental performance, cost aspects also play a critical role (e.g., H1, H2, H3, H6). Measures may not be implemented due to budget constraints (H2, H3, H6) and are dependent upon board decisions.
“The problem which you have to address at these annual meetings is simply that a financial framework is made available, especially for the implementation of the measures.”
(H1)
If EMAS had been in place for a very long time, in some cases the enthusiasm for the system declined among employees (e.g., H1, H8, H11). Fewer suggestions were being made by employees for the continuous improvement of environmental performance. Therefore, keeping the system alive over extended periods of time represents a challenge.
“…you always have to keep this system alive. However, this actually happens through the internal audits, where it becomes clear that we have a system here that really exists, there is someone here who manages it, who also gathers ideas and suggestions. If you do not, then such a system is actually forgotten very quickly.”
(H11)
The role of the environmental management officer was emphasized in our interviews (e.g., H5, H7). This person was described by H11 as someone who manages the EMAS systems, ensures that the system is not forgotten, and pursues and encourages ideas. This person ensures that the employees do not just hear the explanations of the experts and see the environmental statement in the hallway, but notice much more regarding corporate environmental management. It has been reported that the board of the hospitals was important for the EMAS decision. However, it was also said that it does not “live” the system. While the board represents the environmental management representative, the system depends on the commitment of the environmental management officer, who carries out the operational business.
3.2.3. Barriers for Revalidation
Some challenges were mentioned by the hospitals regarding the required revalidation every three years. An increased workload occurs before the audits (H3, H6, H7, H13). All documents must be updated and prepared and agreed upon with the relevant committees and the Executive Board (H3, H10). For example, many key figures from different areas have to be collected (H6). Furthermore, finding reliable and comparable data for the needed years is considered a problem (H7, H13, H14). Changing staff or data collection software make this even more difficult (H7).
As EMAS strives for continuous environmental improvement, the hospitals need to set new environmental targets for the environmental program and revalidation. It was reported that this becomes more difficult the longer the hospital has EMAS, especially when the hospital is already environmentally well-positioned and has achieved many changes and savings (e.g., H1, H3, H6, H10, H11, H14).
“So you have to set goals for the main consumptions of electricity, gas, water, etc. If you have been doing this for a very long time, you really only have a small ability to influence the overall savings.”
(H1)
For example, one interviewee mentioned that, in case of limited possibilities to influence additional savings in their hospital, then more individual projects are proposed, which can bring about minor changes. The problem then is to get a commitment from the management or other agencies regarding funding (H1).
Furthermore, the more familiar some interviewees became with environmental issues, the more critical questions they asked themselves. For example, the question emerged as to which parts of the value chain should be included in goal setting. As outsourcing is relevant for hospital management, so too is it for the environmental management. Areas such as laundries or laboratories are often outsourced, and this raises the question of whom to assign the responsibility for the environmental impacts and their reduction.
“One thing that causes great difficulties not only for us, but probably for all companies on the road to EMAS, are the indirect environmental aspects.”
(H8)
Indirect impacts challenge environmental managers, for example, in supplier and product assessments (e.g., H7, H8, H12). It is often the case that pertinent information is not available for such reviews. In addition, other criteria—such as patient safety, medical necessity, or employee preferences—are prioritized over environmental issues within procurement.
“Well, if you were to do a product evaluation in America with pacemakers (...) or heart valves coming from America. How do you assess this? Environmental issues are not known there. Because those devices are needed, they have to be used. Or implants that need to be used somewhere. You cannot rate that. You may be able to rate when you have some bulk goods, for example, dressing materials. Or perhaps the packaging. But, of course, there are also hygiene regulations that are always given priority over environmental protection to ensure patient safety. And that’s a huge problem, this product review, that does not work here in the hospital.”
(H12)
In general, it is difficult for hospital managers to set influenceable and realistic environmental goals (e.g., H6, H14). Factors such as changes in patient numbers, environmentally unfriendly patient behavior, structural changes in the facility, or even the weather complicate realistic planning and achievement of environmental goals for hospitals (e.g., H1, H2, H12, H14). Changing external requirements can even reduce already achieved savings by EMAS (e.g., H1). For example, in H1, flow restrictors were installed as part of environmental management in order to reduce water consumption. These had to be uninstalled to meet increased hygiene requirements. Thereby, the previously reduced water consumption increased again.
Our interviewees complained about the annual interim audits that check on the progress of the set goals (e.g., H6, H10). They state that often there is not enough time to actually implement the goals (H3). In addition, these interim audits are also associated with additional staff time and costs (e.g., for auditor), especially when several locations must be certified (H4, H10).
“Every year an interim audit. That’s not only time that gets lost, but that’s also costs (...) the interim audits are at least two days, more like three days, and every three years the validation takes a whole week. That’s five working days.”
(H10)
3.3. Synthesizing the Barriers in a Model
In the previous sections, the barriers the hospitals experienced are presented chronologically. Problems can arise in the preparatory phase before the initial registration and validation, in the maintenance, and the revalidation of the system. This temporal analysis provides a logical overview of problems organizations might face.
In order to address innovation barriers in a multilevel analysis that goes beyond a mere summary [
63,
64], the barriers were analyzed from an additional perspective: the levels in the hospitals where the problems relate to, such as organizational conditions in general, teams, or individuals. A categorization of barriers according to the levels of analysis can be found in Hueske and Guenther [
64]. The authors proposed a barrier model that is based on an exhaustive systematic literature review of 188 empirical studies on innovation barriers, which are then related to theory. Hueske and Guenther grouped the factors that hamper, delay, or block innovation according to the following levels of analysis: external environment, organizational, group, and individual levels. The external environment comprises stakeholders, i.e., investor, potential employee, supplier, competitor, customer, state, society. The organizational level comprises the categories of strategy, structure, size, resources, organizational learning, and organizational culture. At the group level, team structure, climate, processes, member characteristics, and leadership style are categorized. On the individual level, attitudes and abilities of managers and employees represent the categories of the model. For more information on this
External environment
Organization
Group
Individual (EOGI) barrier model, see [
64].
The barriers revealed in the interviews in this paper can be categorized according to three of these four levels: the organizational level, the group level, and the individual level. The environmental level of the EOGI model—which reveals barriers from external stakeholders—is not relevant for this paper, as it focuses on internal barriers. The other three levels and their categories are helpful to expand the chronological view of the EMAS barriers. Thus, the results of this empirical research were analyzed from several perspectives. The results are systemized in
Figure 2. This figure structures the barriers chronologically and according to the level of analysis.
At the organizational level, barriers were identified in implementing the environmental strategy across the whole organization, setting up the EMAS structure and the documents (e.g., H1, H2, H4, H12), and integrating environmental issues into existing structures (e.g., H3, H5, H13). EMAS and the connected environmental issues are shown to compete with hospitals’ existing strategies and structures (e.g., H1, H4, H6, H9). Furthermore, the diffusion of environmental thinking and acting throughout the hospital and the different departments represents a challenge that might increase with the size of the hospital (e.g., H2, H14). To collect data for EMAS revalidation represents another challenge (e.g., H7, H13). Limited resources for staff (e.g., H6, H12, H13), consultants, auditors/verifiers (e.g., H6, H10), and the implementation of measures (e.g., H1, H2, H6) were mentioned as problematic. The time effort of staff to prepare for the EMAS registration and (re)validation and to implement the measures were mentioned very often (e.g., H3, H10, H14). The hospital culture that strongly focuses on routines to deliver high quality care for patients can hamper EMAS adoption, and so can resistance to environmental issues and learning progress due to organizational inertia (e.g., H12). However, learning is fostered by cooperation and information exchange with other hospitals (e.g., H6).
At the group level, problems became apparent that can be related to the different work areas (e.g., care and administration) and therefore reflect different member characteristics and team climate within hospitals (e.g., H5, H6, H8, H9, H14). It has been reported that different hierarchical levels also react differently to environmental issues and the implementation of a formal management system (e.g., H8, H9, H10). Members of different groups in hospitals have different goals and skills, which can create problems (e.g., H10, H14). Furthermore, problems regarding existing team structures and the environmental team-building process were reported (e.g., H5). However, such problems on the group level are highly connected to the organizational level (e.g., structure definition or resource allocation), as well as to the individual team member characteristics and leadership (e.g., H7, H10, H11, H14).
At the individual level, negative attitudes, as well as lack of expertise among employees with regard to environmental issues and a formal EMS, have been identified as problems. It was not so much individual resistance that was reported, but instead negative attitudes and a lack of interest regarding EMAS and environmental issues (depending on the responsibility) (e.g., H2, H3, H10) or the fear that more work would be required (e.g., H6, H8, H10, H13). The lack of knowledge of individuals was mentioned specifically as a problematic issue during the early phases of EMAS implementation (e.g., H1, H4, H8, H14).
4. Discussion
In the previous section, barriers were identified that hospitals have experienced in implementing and maintaining EMAS. Now, these barriers are discussed at the organizational, team, and individual levels in the hospitals and at the EMAS system level. Furthermore, measures to prevent or respond to these problems are elucidated.
An important issue at the organizational level for hospitals is the need for resources, i.e., costs associated with the implementation, validation, maintenance of the system, and the actual implementation of concrete environmental measures. These unavoidable expenditures are widely discussed in the literature, for example, for EMAS [
25,
32,
40] and ISO 14001 [
34,
37,
65,
66,
67,
68]. Daddi et al. [
28] list a lack of financial resources as a factor that can lead to withdrawal from the EMAS system. It is not surprising that these organizational resource problems were mentioned by our interviewees, as hospitals are generally said to be under high quality, cost, and competitive pressure [
69,
70]. Undoubtedly, choosing EMAS is a financial challenge for hospitals. The literature considers top management commitment to be a key factor in the successful implementation of EMS [
25,
37,
66,
68,
71,
72]. In hospitals, the board makes the final decisions, especially on larger expenses. Since this study researched already registered hospitals, it can be assumed that the Executive Board has already made the fundamental decision for EMAS and sees its relevance. It can be assumed that the top management commitment to EMAS resulted in support in the form of personnel and financial resources for the principal implementation of the system. In spite of the initial costs associated with EMAS, which were repeatedly mentioned as a problematic issue, the boards of the hospitals interviewed for this paper have already decided in favor of EMAS implementation, so that the cost issues, at least in the initial stages, should not represent an insurmountable barrier to entry (i.e., EMAS adoption).
The implementation of environmental goals in concrete environmental protection measures costs money and time and was addressed as a barrier. As revealed, not all measures were able to be implemented. It is probably safe to assume that if a potential for financial savings can be displayed, the directors will have a closer look at the proposed environmental measure. This should also apply if non-implementation of the measure threatens legal compliance. However, spending on environmental measures will be balanced against other primary goals of the hospital and its overall strategy. Environmental protection will compete with other sustainability criteria, such as patient safety or hygiene requirements [
49].
Closely related to the directly required financial resources is the effort (time) required for the formal management system EMAS. On the one hand, this results from the minimum requirements imposed by the system, such as for collecting environmental data and conducting reviews or creating documents. This bureaucratic and documentary effort is also discussed in the literature (see, for EMAS, e.g., [
32]; for ISO 14001, e.g., [
73,
74]). The hospitals cannot avoid this effort completely. However, they can try to minimize it in the hospital through the actual design and implementation. For example, required documents can be deliberately kept simple and concise. Concerning the public environmental statement, this can also have the positive side effect of increasing the number of readers both internally and externally. The long-term construction of clear structures and responsibilities, as well as reporting requirements, can reduce the time required for validation. This also applies to the careful planning of audits through the preparation of employees in the individual departments.
Over time, it may become evident that the planning was not realistic and the implementation, despite all efforts, has become more costly and time consuming. At this point, the board and other leaders should control and regulate (e.g., by releasing additional funds or restructuring responsibilities). Thus, it should also be ensured that the additional environmental measures do not result in reduced performance in the regular everyday tasks of the hospital employees.
The perceived effort is certainly partly due to inexperience with the EMAS system and environmental issues. The problem of lack of experience of users with EMAS or EMS in general is also a problem discussed in the literature [
14]. Understanding the scheme and the language used is problematic and applies to EMS in general [
12,
14] and also specifically to EMAS [
31,
32] and ISO 14001 [
34,
75]. For example, due to a lack of competence and knowledge, there may be problems in identifying environmental aspects [
12,
14]. In principle, it can certainly be assumed that there are learning effects on the organizational and individual levels, whereby the perceived effort with increasing familiarity with the system and the validation process can be reduced over time.
Often hospitals will have to rely on external consultants due to a lack of their own expertise. These consultants are intended to compensate for the lack of specialist knowledge in the organization and on the individual level, but are again associated with costs. As this study demonstrates, the consultants did not always provide good advice initially. The lack of experience of some consultants is also referred to in the literature as a problem (e.g., [
34] for ISO 14001 in the hotel industry). This may be less true today than it was a few years ago for the healthcare sector because some consultants and reviewers have already validated hospitals. However, the challenge for hospitals remains finding a suitable advisor.
Another important problem area is the individual employee (see [
40] on EMAS or [
68] on EMS). Their low level of knowledge and skills regarding environmental issues and possible negative attitudes towards a bureaucratic management system—which is introduced in a top-down approach and is not directly related to or even competes with their core business—can, according to our interviewees, cause problems at the beginning as well as during the implementation of EMAS. Pinzone et al. [
48] showed that the lack of environmental commitment is among the more significant barriers for adoption of proactive environmental strategies in healthcare organizations in Italy. They attribute this to the specific nature of this sector (i.e., having different key decision makers from different professional groups on several organizational levels). It is understandable that the thoughts of the employees are usually focused mainly on their field of activity [
44], especially on the well-being of their patients, and not on environmental issues or the implementation of a formal EMS. However, these problems are also present in other industries and with other EMSs, such as ISO 14001 (see, e.g., US industrial companies [
37]; Chinese hotel industry [
34,
72]). The employees have a focus on their day-to-day operations and own needs and less on strategic goals that top management is pursuing with the EMAS decision for the organization. In order not to jeopardize long-term and overarching goals and to reduce resistance and better involve the staff, the awareness of and skills for environmental issues and the management system should be increased among employees. Trainings can be carried out (e.g., see [
68,
76]). Care should be taken to ensure that these training sessions in the hospital are tailored to different target groups and their characteristics. In addition, regular training is advisable, as staff turnover is to be expected [
44]. In addition, employee feedback should be included [
68]. By sensitizing and training employees, environmentally friendly thinking and acting can be anchored as part of the corporate culture for the long term (see also [
77] for the contribution of human resource factors to EMS or [
78] for contribution of EMS to organizational learning).
Increasing awareness regarding EMAS and environmental issues can be achieved through regular communication [
68] via various media within the hospital (e.g., on the achievements of EMAS). Here, team leaders in the departments can influence their teams with their leadership style and their attitudes. However, the communication is largely the responsibility of the environmental manager. The selection of the EMAS officer, who is in a key position, should be done carefully. This person is responsible for planning and implementing measures under EMAS. He is at the interface between top management, which has made the decision for EMAS, and the employees, who have to implement this decision in their day-to-day operations. On the one hand, this means being open to new topics and employee ideas and understanding oneself as a multiplier and motivator. On the other hand, this person must also justify measures to the management, deal with existing restrictions (e.g., budget limitations), and provide decision templates. This person needs the abilities to understand and shape the existing structures and processes, as well as the culture and thinking of the hospitals’ individual members in the different departments. The demands on the abilities and attitudes of this key person, who should influence the organizational culture with regard to environmental issues, are high. Zutshi and Sohal [
68] call this responsible manager a “champion”.
Overall, for managers, understanding the factors that motivate employees and impact employee and organizational performance is important in order to implement measures that address and influence them [
79,
80]. It is not only training or communication, but instead the careful composition of several human resource measure—such as recruitment, performance assessment, training, and communication that is discussed in the literature—that shall increase corporate performance [
81,
82,
83]. Within comprehensive human resources management, the environmental concept can be embedded and aligned with the traditional work environment in a hospital. This can contribute to remedy some of the problems connected to EMAS implementation.
In the interviews, the hospitals identified some issues they generally have regarding the EMAS system. As our hospitals cannot actively manage them, they pose the risk of leading to an exit. In the literature, there are ongoing calls and discussions regarding EMS simplification measures and regulatory relief in order to increase incentives for organizations to adopt or stay within the system (for EMAS see [
84]; for EMS see [
85]; for SMEs and EMS see [
12]; for simplification measures for EMAS and ISO 14001 see [
86]). Daddi et al. [
86] classified and evaluated simplification measures that should increase registration numbers. Among the measures are simplifications for obtaining or renewing a permit, simplification of inspections, and tax breaks. As already mentioned, costs and expenses for EMAS play a critical role for hospitals. From the perspective of the hospitals, the introduction of interim audits is problematic. Our interviewees agreed that audits are useful, as they attribute more internal power to the environmental officer, and the external assessment can legitimize their organization-wide calls for action and, thus, lead to more relevance for the employees. However, the interviewees disagreed in their evaluation of the optimal time intervals. On the one hand, short time intervals ensure progress and innovation. On the other hand, they are not perceived as a simplification measure and are associated with further additional costs and effort. Daddi et al. [
28] demonstrated that cost and effort are factors that can lead to drop outs from the EMAS system.
5. Conclusions
EMAS is a comprehensive voluntary management approach designed to continuously improve the environmental performance of organizations. In Germany, only a few hospitals have implemented and maintained EMAS to date. Concrete numbers regarding EMS certification according to ISO 14001 cannot be established, as no national or international register exists. In this paper, the critical aspects of introducing, implementing, and maintaining a formal EMS according to EMAS in hospitals are examined. Problems which the hospitals experience occur at different stages and at different levels of analysis. It is important to identify problematic issues and actively take countermeasures to avoid a failure of the organizational innovation or a withdrawal from the system. In addition, knowledge of potential problems can lead to preventive action so that the problems do not arise. In the long term, this can save resources that would be needed to overcome problems.
Some limitations are associated with the present study. EMAS hospitals in Germany were researched for this paper. Although this represents the German EMAS hospitals very well, investigating hospitals in other countries or hospitals and their environmental management according to other certifications or standards should be considered in future research. In this study, interviews with the responsible environmental managers were conducted. On the one hand, they are the experts in the organization on this topic. On the other hand, it is possible that they have a distorted picture of environmental management in their hospital based on their respective position in the organization. In the future, more detailed research on the different organizational levels in hospitals and with several actors—such as physicians, nurses, or administrative staff—can provide additional information regarding barriers and how to overcome them. In addition, barriers should be researched at different points throughout the lifetime of EMAS (e.g., when implementing the system or just before a revalidation), as they can prove to be more pronounced at some stages than others. Managers of hospitals that are still registered, and therefore represent cases that have overcome barriers successfully, were interviewed. Examinations of hospitals that have left EMAS can provide further fruitful insights on how to improve the EMAS system. As the EMAS diffusion rate in the healthcare sector is quite low, research can investigate entry barriers for hospitals.
What conclusions can be drawn for hospitals? It is to be expected that the majority of hospitals in Germany are not familiar with formal environmental management systems or environmental issues in general. The perception of problematic issues surrounding EMAS adoption can be understood as entry barriers for hospitals. Today, interested hospitals find slightly more specific and helpful information on the implementation of EMAS in hospitals, as, for example, the environmental statements of EMAS hospitals are publicly available. Moreover, consultants are also more experienced. However, inexperience with the EMAS system and environmental issues increases the costs for hospitals, as they either have to inform themselves independently or engage a professional consultant. In order to promote the diffusion of EMAS, specific information for hospitals should be provided on EMAS and best practices. Support from associations can be helpful. In addition, an exchange of experience with other hospitals can be sought before implementation (for more on advantages of cooperations see [
12,
14,
21]). For example, already validated hospitals recommend gaining initial experience with other certifications (see also [
71]) in order to better understand and implement EMAS. In their opinion, the validation and certification of comprehensive EMS according to EMAS or ISO 14001 is more successful when the hospital already acknowledges some environmental issues or has already operated the environmental management for a while without certification or validation, or according to simpler systems (such as Ökoprofit). The latter can have the additional advantage that subsidies and active networks might exist [
34].
Hospitals have a sense of high social responsibility towards their patients. The research presented here affirms the fact that some hospitals in Germany consider environmental sustainability issues by means of EMS implementation. However, these pioneers experience some barriers on several levels. The perception of barriers influences how organizations perceive benefits [
42], and for that reason it is important to manage them. This study suggests that finding the balance between a sound environmental management, on the one hand, and the feasibility in everyday clinical life, on the other, will remain a challenge. As long as the assessment of the merits of an EMS (see also [
87]) by the Board of Directors is positive, and thus its support through the provision of financial and human resources is assured, it is expected that the hospital will continue with EMAS. This remains a challenge against the background of the primary goal of hospitals, which is providing high quality health services, but these hospitals demonstrate that they can care for both the patients and the environment.