Responders to Cervical Facet Platelet-Rich Plasma Demonstrate Synergistic Improvements in Pain and Isometric Strength in Chronic Whiplash-Associated Disorders: A Series of Mediation Analyses
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
- (a)
- Aged 18 or older.
- (b)
- Presented with a whiplash-associated disorder (WAD) grade II classification (presence of neck complaint and musculoskeletal signs such as reduced cervical ROM and point tenderness).
- (c)
- Received a single autologous injection of ultrasound and fluoroscopically guided PRP into the cervical facet joints and peri-articular joint margins (1) after demonstrating a positive response (greater than 80% relief of index pain or greater than 50% relief of pain AND significant improvement in performing a previously limited activity of daily living) to a single diagnostic medial branch block, as previously reported [1].
- (d)
- Attended rehabilitation (self-reported) in the 3 months post-PRP and a 3-month review, which included repeat patient-reported outcomes and physical measures being collected.
- (e)
- A successful outcome was reported after 3 months, defined as a greater than 15% reduction in pain intensity, which has been demonstrated to be the minimal clinically important change for chronic musculoskeletal pain intensity, when measured on a numerical rating scale, as was instituted in this study [10].
2.3. Conservative Rehabilitation
2.4. Outcomes
2.5. Data Analysis
3. Results
3.1. Association Between Pain, Disability, and Physical Measures
3.2. Tests of Mediation
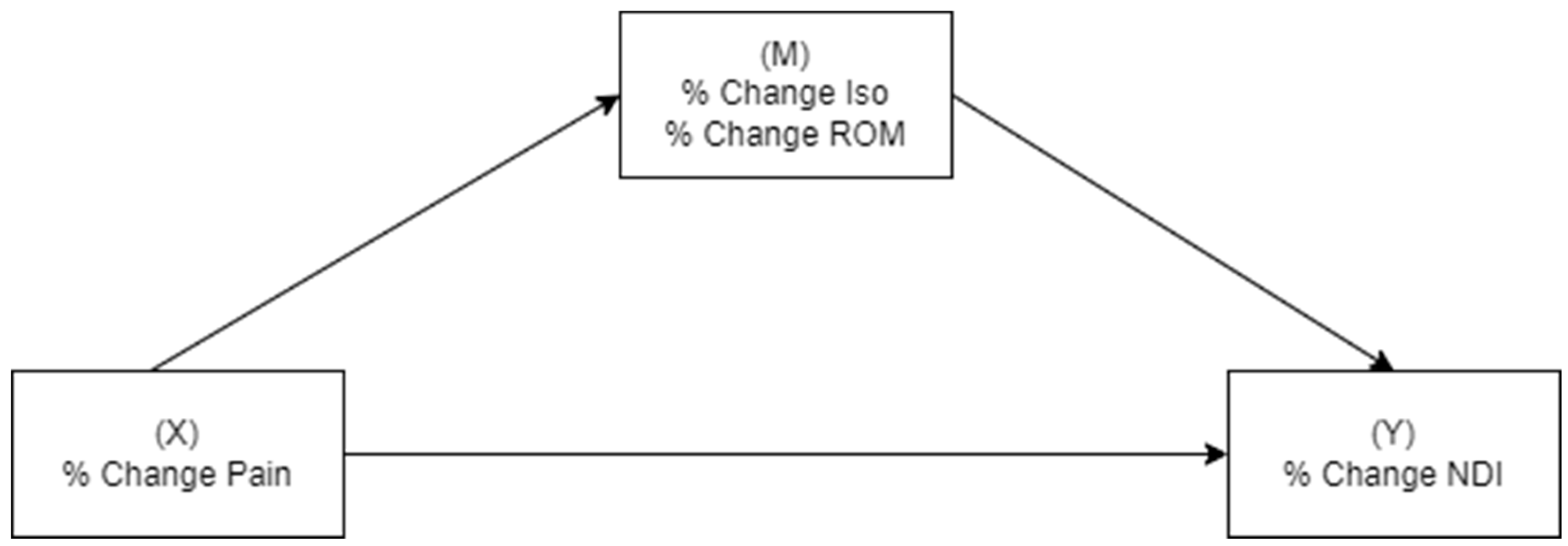
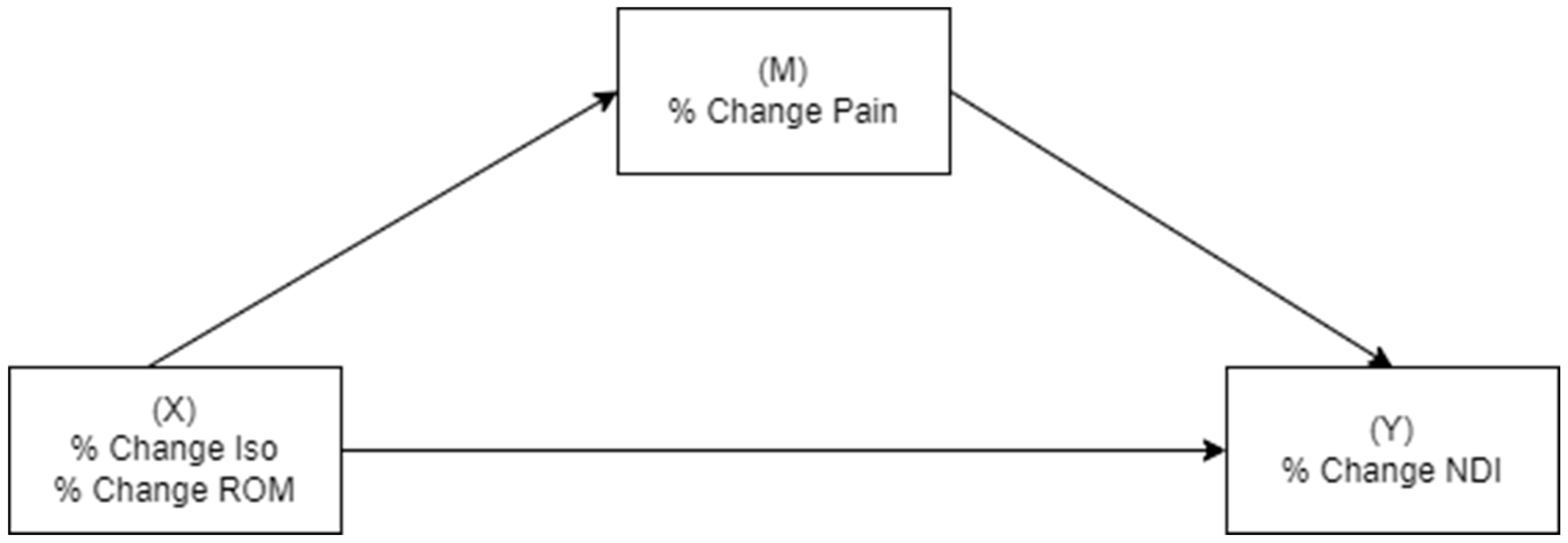
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Smith, A.; Andruski, B.; Deng, G.; Burnham, R. Cervical Facet Joint Platelet-Rich Plasma in People With Chronic Whiplash-Assocated Disorders: A Prospective Case Series of Short-Term Outcomes. Int. Pain Med. 2022, 1, 100078. [Google Scholar]
- Smith, A.; Andruski, B.; Deng, G.; Burnham, R. Cervical facet joint platelet-rich plasma in people with chronic whiplash-associated disorders: A prospective case series of longer term 6- and 12-month outcomes. Interv. Pain Med. 2023, 2, 100237. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Zhou, J.; Liu, C.; Zhang, J.; Xiong, W.; Lv, Y.; Liu, R.; Wang, R.; Du, Z.; Zhang, G.; et al. A Prospective Study Comparing Platelet-Rich Plasma and Local Anesthetic (LA)/Corticosteroid in Intra-Articular Injection for the Treatment of Lumbar Facet Joint Syndrome. Pain. Pract. 2017, 17, 914–924. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Du, Z.; Lv, Y.; Zhang, J.; Xiong, W.; Wang, R.; Liu, R.; Zhang, G.; Liu, Q. A New Technique for the Treatment of Lumbar Facet Joint Syndrome Using Intra-articular Injection with Autologous Platelet Rich Plasma. Pain. Physician 2016, 19, 617–625. [Google Scholar] [PubMed]
- Zhang, J.; Middleton, K.K.; Fu, F.H.; Im, H.-J.; Wang, J.H.-C. HGF mediates the anti-inflammatory effects of PRP on injured tendons. PLoS ONE 2013, 8, e67303. [Google Scholar] [CrossRef] [PubMed]
- Wasterlain, A.S.; Braun, H.J.; Harris, A.H.; Kim, H.J.; Dragoo, J.L. The systemic effects of platelet-rich plasma injection. Am. J. Sports Med. 2013, 41, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Collins, T.; Alexander, D.; Barkatali, B. Platelet-rich plasma: A narrative review. EFORT Open Rev. 2021, 6, 225–235. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.; Gupta, A.; Stone, J.; Habberfield, J.; Schneider, G. The efficacy of multimodal physiotherapy and usual care in chronic whiplash-associated disorders with facet-mediated pain undergoing platelet rich plasma (PRP) treatment: A series of single case experimental designs (SCEDs). Eur. J. Physiother. 2024, 27, 38–47. [Google Scholar] [CrossRef]
- Schneider, G.M.; Jull, G.; Thomas, K.; Smith, A.; Emery, C.; Faris, P.; Cook, C.; Frizzell, B.; Salo, P. Derivation of a clinical decision guide in the diagnosis of cervical facet joint pain. Arch. Phys. Med. Rehabil. 2014, 95, 1695–1701. [Google Scholar] [CrossRef] [PubMed]
- Salaffi, F.; Stancati, A.; Silvestri, C.A.; Ciapetti, A.; Grassi, W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur. J. Pain. 2004, 8, 283–291. [Google Scholar] [CrossRef] [PubMed]
- MacDermid, J.C.; Walton, D.M.; Avery, S.; Blanchard, A.; Etruw, E.; McAlpine, C.; Goldsmith, C.H. Measurement properties of the neck disability index: A systematic review. J. Orthop. Sports Phys. Ther. 2009, 39, 400–417. [Google Scholar] [CrossRef] [PubMed]
- Westaway, M.D.; Stratford, P.W.; Binkley, J.M. The patient-specific functional scale: Validation of its use in persons with neck dysfunction. J. Orthop. Sports Phys. Ther. 1998, 27, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Stratford, P.; Riddle, D.; Binkley, J.; Spadoni, G.; Westaway, M.D.; Padfield, B. Using the Neck Disability Index to make decisions concerning individual patients. Physiother Can. 1999, 51, 107–112. [Google Scholar]
- Vernon, H. The neck disability index: Patient assessment and outcome monitoring in whiplash. J. Musculoskelet Pain. 1996, 4, 95–104. [Google Scholar] [CrossRef]
- Cleland, J.A.; Childs, J.D.; Whitman, J.M. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch. Phys. Med. Rehabil. 2008, 89, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Krebs, E.E.; Lorenz, K.A.; Bair, M.J.; Damush, T.M.; Wu, J.; Sutherland, J.M.; Asch, S.M.; Kroenke, K. Development and initial validation of the PEG, a three-item scale assessing pain intensity and interference. J. Gen. Intern. Med. 2009, 24, 733–738. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, A.M.; Stewart, R.E.; Köke, A.J.A.; Oosterwijk, R.F.A.; Swaan, J.L.; Schreurs, K.M.G.; Preuper, H.R.S. Cut-Off Points for Mild, Moderate, and Severe Pain on the Numeric Rating Scale for Pain in Patients with Chronic Musculoskeletal Pain: Variability and Influence of Sex and Catastrophizing. Front. Psychol. 2016, 7, 1466. [Google Scholar] [CrossRef] [PubMed]
- Bush, K.W.; Collins, N.; Portman, L.; Tillett, N. Validity and intertester reliability of cervical range of motion using inclinometer measurements. J. Man. Manip. Ther. 2000, 8, 52–61. [Google Scholar] [CrossRef]
- Youdas, J.W.; Carey, J.R.; Garrett, T.R. Reliability of measurements of cervical spine range of motion—comparison of three methods. Phys. Ther. 1991, 71, 98–104; discussion 105–106. [Google Scholar] [CrossRef] [PubMed]
- Jørgensen, R.; Ris, I.; Juhl, C.; Falla, D.; Juul-Kristensen, B. Responsiveness of clinical tests for people with neck pain. BMC Musculoskelet. Disord. 2017, 18, 548. [Google Scholar] [CrossRef] [PubMed]
- Versteegh, T.; Beaudet, D.; Greenbaum, M.; Hellyer, L.; Tritton, A.; Walton, D. Evaluating the reliability of a novel neck-strength assessment protocol for healthy adults using self-generated resistance with a hand-held dynamometer. Physiother. Can. 2015, 67, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Preacher, K.J.; Hayes, A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 2004, 36, 717–731. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 3rd ed.; Methodology in the Social Sciences Series; Little, T.D., Ed.; Guilford Press: New York, NY, USA, 2022. [Google Scholar]
- Fritz, M.S.; MacKinnon, D.P. Required sample size to detect the mediated effect. Psychol Sci. 2007, 18, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsson, M.L.; Peterson, G.; O’Leary, S.; Dedering, Å.; Peolsson, A. The effect of neck-specific exercise with, or without a behavioral approach, on pain, disability, and self-efficacy in chronic whiplash-associated disorders: A randomized clinical trial. Clin. J. Pain. 2015, 31, 294–303. [Google Scholar] [CrossRef] [PubMed]
- Jull, G.; Sterling, M.; Kenardy, J.; Beller, E. Does the presence of sensory hypersensitivity influence outcomes of physical rehabilitation for chronic whiplash?—A preliminary RCT. Pain 2007, 129, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.J.; Maher, C.G.; Refshauge, K.M.; Herbert, R.D.; Bogduk, N.; Nicholas, M. Randomized controlled trial of exercise for chronic whiplash-associated disorders. Pain 2007, 128, 59–68. [Google Scholar] [CrossRef] [PubMed]
- A Michaleff, Z.; Maher, C.G.; Lin, C.-W.C.; Rebbeck, T.; Jull, G.; Latimer, J.; Connelly, L.; Sterling, M. Comprehensive physiotherapy exercise programme or advice for chronic whiplash (PROMISE): A pragmatic randomised controlled trial. Lancet 2014, 384, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Chiu, T.T.; Lam, T.H.; Hedley, A.J. Maximal isometric muscle strength of the cervical spine in healthy volunteers. Clin. Rehabil. 2002, 16, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Prushansky, T.; Gepstein, R.; Gordon, C.; Dvir, Z. Cervical muscles weakness in chronic whiplash patients. Clin. Biomech. 2005, 20, 794–798. [Google Scholar] [CrossRef] [PubMed]
- Prushansky, T.; Pevzner, E.; Gordon, C.; Dvir, Z. Performance of cervical motion in chronic whiplash patients and healthy subjects: The case of atypical patients. Spine 2006, 31, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Farrell, S.F.; de Zoete, R.M.J.; Cabot, P.J.; Sterling, M. Systemic inflammatory markers in neck pain: A systematic review with meta-analysis. Eur. J. Pain. 2020, 24, 1666–1686. [Google Scholar] [CrossRef] [PubMed]
- Farrell, S.F.; Armfield, N.R.; Cabot, P.J.; Elphinston, R.A.; Gray, P.; Minhas, G.; Collyer, M.R.; Sterling, M. C-Reactive Protein (CRP) is Associated with Chronic Pain Independently of Biopsychosocial Factors. J. Pain. 2024, 25, 476–496. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.; Hua, S.; Yang, T.; Ma, J.; Yu, W.; Chen, X. Platelet-rich plasma shows beneficial effects for patients with knee osteoarthritis by suppressing inflammatory factors. Exp. Ther. Med. 2018, 15, 3096–3102. [Google Scholar] [CrossRef] [PubMed]
- Lacko, M.; Harvanová, D.; Slovinská, L.; Matuška, M.; Balog, M.; Lacková, A.; Špaková, T.; Rosocha, J. Effect of intra-articular injection of platelet-rich plasma on the serum levels of osteoarthritic biomarkers in patients with unilateral knee osteoarthritis. J. Clin. Med. 2021, 10, 5801. [Google Scholar] [CrossRef] [PubMed]
- Graaf, M.T.-D.; Thoomes, E.; Fernández-De-Las-Peñas, C.; Plaza-Manzano, G.; Cleland, J.A. Normative values of cervical range of motion for both children and adults: A systematic review. Musculoskelet. Sci. Pract. 2020, 49, 102182. [Google Scholar] [CrossRef] [PubMed]
- Siegmund, G.P.; Myers, B.S.; Davis, M.B.; Bohnet, H.F.; Winkelstein, B.A. Mechanical evidence of cervical facet joint capsule injury during whiplash: A cadaveric study using combined shear, compression, and extension loading. Spine 2001, 26, 2095–2101. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kaneoka, K.; Ono, K.; Inami, S.; Hayashi, K. Motion analysis of cervical vertebrae during whiplash loading. Spine 1999, 24, 763–769; discussion 770. [Google Scholar] [CrossRef] [PubMed]
- Stemper, B.D.; Yoganandan, N.; Pintar, F.A. Effects of abnormal posture on capsular ligament elongations in a computational model subjected to whiplash loading. J. Biomech. 2005, 38, 1313–1323. [Google Scholar] [CrossRef] [PubMed]
- Quinn, K.P.; Winkelstein, B.A. Detection of altered collagen fiber alignment in the cervical facet capsule after whiplash-like joint retraction. Ann. Biomed. Eng. 2011, 39, 2163–2173. [Google Scholar] [CrossRef] [PubMed]
- Winkelstein, B.A.; Santos, D.G. An intact facet capsular ligament modulates behavioral sensitivity and spinal glial activation produced by cervical facet joint tension. Spine 2008, 33, 856–862. [Google Scholar] [CrossRef] [PubMed]
- Dong, L.; Quindlen, J.C.; Lipschutz, D.E.; Winkelstein, B.A. Whiplash-like facet joint loading initiates glutamatergic responses in the DRG and spinal cord associated with behavioral hypersensitivity. Brain Res. 2012, 1461, 51–63. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.E.; Davis, M.B.; Winkelstein, B.A. Capsular ligament involvement in the development of mechanical hyperalgesia after facet joint loading: Behavioral and inflammatory outcomes in a rodent model of pain. J. Neurotrauma 2008, 25, 1383–1393. [Google Scholar] [CrossRef] [PubMed]
- Kallakuri, S.; Singh, A.; Lu, Y.; Chen, C.; Patwardhan, A.; Cavanaugh, J.M. Tensile stretching of cervical facet joint capsule and related axonal changes. Eur. Spine J. 2008, 17, 556–563. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Smith, A.D.; Jull, G.; Schneider, G.; Frizzell, B.; Hooper, R.A.; Sterling, M. Cervical Radiofrequency Neurotomy Reduces Central Hyperexcitability and Improves Neck Movement in Individuals with Chronic Whiplash. Pain. Med. 2014, 15, 128–141. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.M.; Barnsley, L.; Wallis, B.J.; McDonald, G.J.; Bogduk, N. Percutaneous radio-frequency neurotomy for chronic cervical zygapophyseal-joint pain. N. Engl. J. Med. 1996, 335, 1721–1726. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.D.; Jull, G.; Schneider, G.M.; Frizzell, B.; Hooper, R.A.; Sterling, M. Modulation of Cervical Facet Joint Nociception and Pain Attenuates Physical and Psychological Features of Chronic Whiplash: A Prospective Study. PMR 2015, 7, 913–921. [Google Scholar] [CrossRef] [PubMed]
- Spine Intervention Society. Practice Guidelines for Spinal Diagnostic and Treatment Procedures, 2nd ed.; International Spine Intervention Society: New York, NY, USA, 2013. [Google Scholar]
- Braveman, P.A.; Cubbin, C.; Egerter, S.; Williams, D.R.; Pamuk, E. Socioeconomic disparities in health in the United States: What the patterns tell us. Am. J. Public Health 2010, 100 (Suppl. S1), S186–S196. [Google Scholar] [CrossRef] [PubMed]
- Habberfield, J.; Schneider, G.; Schneider, K.; Katuli, S.; Olson, L. A clinical test to assess isometric cervical strength in chronic whiplash associated disorder (WAD): A reliability study. BMC Musculoskelet. Disord. 2022, 23, 736. [Google Scholar] [CrossRef] [PubMed]
| Pre-PRP | 3 Months Post-PRP | 95%CI of the Difference | Significance | |
|---|---|---|---|---|
| NRS (/10) | 6.5 (±1.8) | 3.5 (±2.0) | [−3.6, −2.5] | <0.001 |
| NDI (%) | 43 (15) | 29 (15) | [−17, −10] | <0.001 |
| ROM (0) | 276 (54) | 302 (55) | [9, 48] | 0.006 |
| Iso (N) | 180 (100) | 258 (123) | [38, 135] | 0.001 |
| Level Injected | C2/3 | C3/4 | C4/5 | C5/6 | C6/7 | C7/T1 |
|---|---|---|---|---|---|---|
| Number | 19 | 24 | 30 | 32 | 15 | 1 |
| Total Levels | 1 | 2 | 3 | 4 | 5 | Uni/Bilateral |
| Number | 3 | 11 | 17 | 10 | 1 | 22/20 |
| % Change NRS | % Change NDI | % Change Iso | % Change ROM | |
|---|---|---|---|---|
| % change NRS | - | 0.70 ** | 0.08 | −0.23 |
| % change NDI | - | 0.53 ** | 0.14 | |
| % change Iso | - | 0.52 |
| Outcome | Mediator | Direct Effect of Pain | Direct Effect | Indirect Effect | Total Effect |
|---|---|---|---|---|---|
| Disability | Isometric Strength | p< 0.001 | 0.83 (0.53, 1.13) | 0.05 (−0.12, 0.32) | 0.88 (0.49, 1.27) |
| Range of Motion | p< 0.001 | 1.10 (0.70, 1.51) | −0.10 (−0.22, 0.08) | 1.00 (0.56, 1.44) |
| IV | Mediator | Direct Effect of IV | Direct Effect | Indirect Effect | Total Effect |
|---|---|---|---|---|---|
| Isometric Strength | Pain Intensity | p< 0.001 | 0.16 (0.08, 0.24) | 0.02 (−0.06, 0.11) | 0.17 (0.05, 0.30) |
| Range of Motion | Pain Intensity | p= 0.03 | 0.48 (0.14, 0.92) | −0.28 (−1.02, 0.16) | 0.20 (−0.53, 0.93) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smith, A.D.; Andruski, B.; Deng, G.; Bouma, C.; Pesant, M.; Magill, F.; Burnham, R. Responders to Cervical Facet Platelet-Rich Plasma Demonstrate Synergistic Improvements in Pain and Isometric Strength in Chronic Whiplash-Associated Disorders: A Series of Mediation Analyses. Clin. Pract. 2025, 15, 135. https://doi.org/10.3390/clinpract15080135
Smith AD, Andruski B, Deng G, Bouma C, Pesant M, Magill F, Burnham R. Responders to Cervical Facet Platelet-Rich Plasma Demonstrate Synergistic Improvements in Pain and Isometric Strength in Chronic Whiplash-Associated Disorders: A Series of Mediation Analyses. Clinics and Practice. 2025; 15(8):135. https://doi.org/10.3390/clinpract15080135
Chicago/Turabian StyleSmith, Ashley D., Benjamin Andruski, George Deng, Colin Bouma, Marc Pesant, Fiona Magill, and Robert Burnham. 2025. "Responders to Cervical Facet Platelet-Rich Plasma Demonstrate Synergistic Improvements in Pain and Isometric Strength in Chronic Whiplash-Associated Disorders: A Series of Mediation Analyses" Clinics and Practice 15, no. 8: 135. https://doi.org/10.3390/clinpract15080135
APA StyleSmith, A. D., Andruski, B., Deng, G., Bouma, C., Pesant, M., Magill, F., & Burnham, R. (2025). Responders to Cervical Facet Platelet-Rich Plasma Demonstrate Synergistic Improvements in Pain and Isometric Strength in Chronic Whiplash-Associated Disorders: A Series of Mediation Analyses. Clinics and Practice, 15(8), 135. https://doi.org/10.3390/clinpract15080135







