Changes in Perceived Tinnitus Sound Qualities Following Internet-Based Cognitive Behavioral Therapy for Tinnitus
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participants
2.3. Intervention
2.4. Data Collection
- Tinnitus severity: Tinnitus Functional Index (TFI; [16]);
- Anxiety symptoms: Generalized Anxiety Disorder-7 (GAD-7; [17]);
- Depressive symptoms: Patient Health Questionnaire-9 (PHQ-9; [18]);
- Sleep disturbance: Insomnia Severity Index (ISI; [19]);
- Health-related quality of life (HRQoL): EQ-5D-5L Visual Analog Scale (VAS; [20]).
2.5. Data Analysis
3. Results
3.1. Study Population
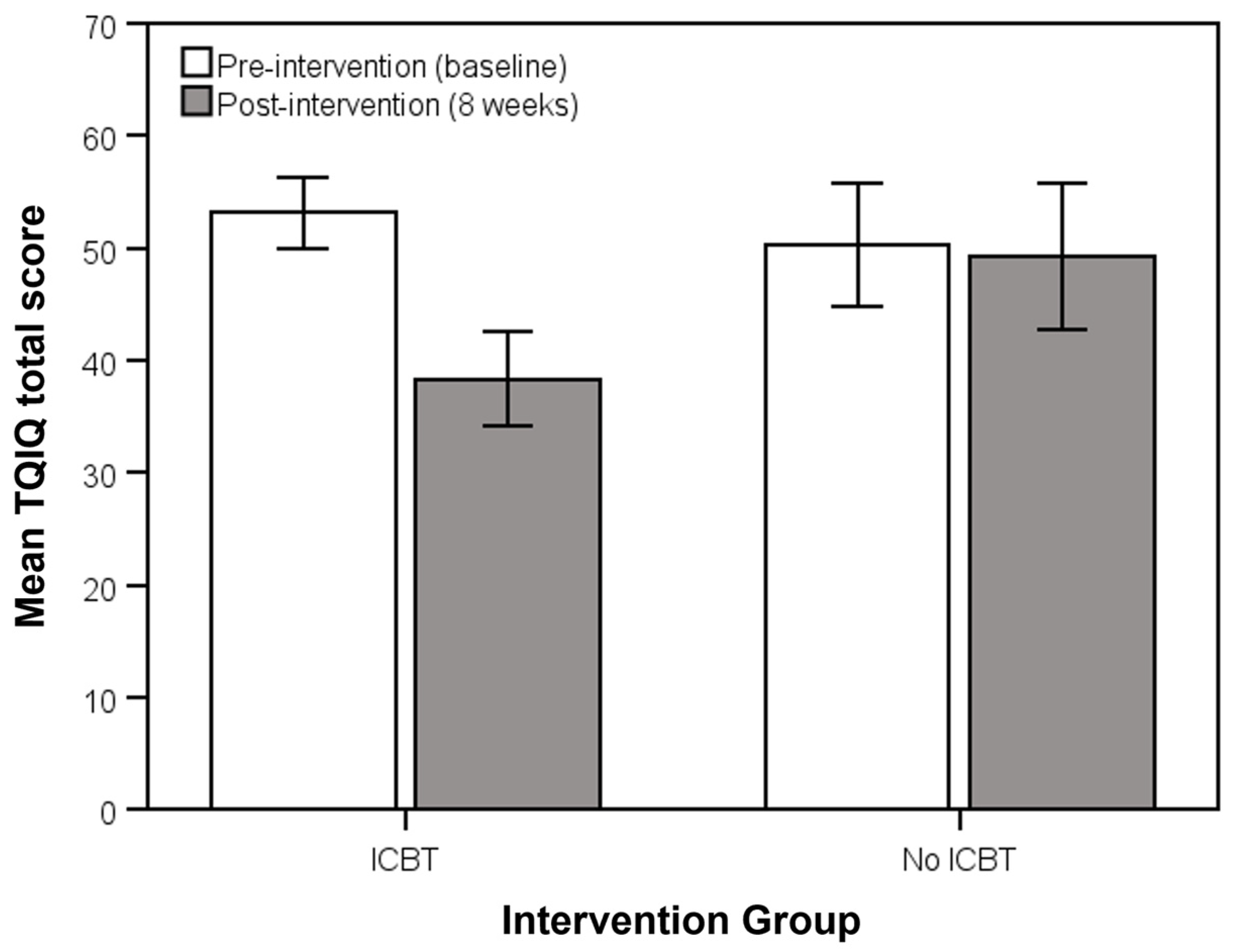
3.2. Change from Pre- (Baseline) to Post-Intervention (8 Weeks)
3.3. TQIQ Minimum Clinical Important Difference (MCID)
4. Discussion
4.1. Change in Tinnitus Sound Qualities Following ICBT Intervention
4.2. Importance of Measuring Tinnitus Sound Qualities
4.3. Study Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baguley, D.; McFerran, D.; Hall, D. Tinnitus. Lancet 2013, 382, 1600–1607. [Google Scholar] [CrossRef]
- Cederroth, C.R.; Gallus, S.; Hall, D.A.; Kleinjung, T.; Langguth, B.; Maruotti, A.; Meyer, M.; Norena, A.; Probst, T.; Pryss, R.; et al. Editorial: Towards an Understanding of Tinnitus Heterogeneity. Front. Aging Neurosci. 2019, 11, 53. [Google Scholar] [CrossRef]
- Yang, D.; Zhang, D.; Zhang, X.; Li, X. Tinnitus-associated cognitive and psychological impairments: A comprehensive review meta-analysis. Front. Neurosci. 2024, 18, 1275560. [Google Scholar] [CrossRef]
- Molnár, A.; Mavrogeni, P.; Tamás, L.; Maihoub, S. Correlation Between Tinnitus Handicap and Depression and Anxiety Scores. Ear Nose Throat J. 2022, 1455613221139211. [Google Scholar] [CrossRef]
- Mavrogeni, P.; Molnár, A.; Molnár, V.; Tamás, L.; Maihoub, S. Correlation Between the Pitch and Loudness of Tinnitus, Hearing Levels, and Tinnitus Handicap Inventory Scores in Patients with Chronic Subjective Tinnitus. J. Clin. Med. 2024, 13, 7261. [Google Scholar] [CrossRef] [PubMed]
- Landgrebe, M.; Azevedo, A.; Baguley, D.; Bauer, C.; Cacace, A.; Coelho, C.; Dornhoffer, J.; Figueiredo, R.; Flor, H.; Hajak, G.; et al. Methodological aspects of clinical trials in tinnitus: A proposal for an international standard. J. Psychosom. Res. 2012, 73, 112–121. [Google Scholar] [CrossRef]
- Henry, J.A.; Manning, C. Clinical Protocol to Promote Standardization of Basic Tinnitus Services by Audiologists. Am. J. Audiol. 2019, 28, 152–161. [Google Scholar] [CrossRef] [PubMed]
- Manchaiah, V.; Andersson, G.; Beukes, E.W.; Fagelson, M.; Swanepoel, D.W.; Heffernan, E.; Maidment, D.W. Development and psychometric validation of Tinnitus Qualities and Impact Questionnaire. Under review 2025.
- Han, B.I.; Lee, H.W.; Kim, T.Y.; Lim, J.S.; Shin, K.S. Tinnitus: Characteristics, causes, mechanisms, and treatments. J. Clin. Neurol. 2009, 5, 11–19. [Google Scholar] [CrossRef]
- Beukes, E.W.; Manchaiah, V.; Andersson, G.A.; Allen, P.A.; Baguley, D.M. Participants experiences of an Internet-based cognitive-behavioral therapy for tinnitus. Int. J. Audiol. 2018, 57, 947–954. [Google Scholar] [CrossRef]
- Beukes, E.W.; Andersson, G.; Fagelson, M.; Manchaiah, V. Audiologist-Supported Internet-Based Cognitive Behavioral Therapy for Tinnitus in the United States: A Pilot Trial. Am. J. Audiol. 2021, 30, 717–729. [Google Scholar] [CrossRef] [PubMed]
- Beukes, E.W.; Andersson, G.; Fagelson, M.A.; Manchaiah, V. Dismantling internet-based cognitive behavioral therapy for tinnitus. The contribution of applied relaxation: A randomized controlled trial. Internet Interv. 2021, 25, 100402. [Google Scholar] [CrossRef] [PubMed]
- Beukes, E.W.; Andersson, G.; Fagelson, M.; Manchaiah, V. Internet-Based Audiologist-Guided Cognitive Behavioral Therapy for Tinnitus: Randomized Controlled Trial. J. Med. Internet Res. 2022, 24, e27584. [Google Scholar] [CrossRef]
- Beukes, E.W.; Manchaiah, V.; Allen, P.M.; Baguley, D.M.; Andersson, G. Internet-Based Interventions for Adults With Hearing Loss, Tinnitus, and Vestibular Disorders: A Systematic Review and Meta-Analysis. Trends Hear. 2019, 23, 2331216519851749. [Google Scholar] [CrossRef]
- Beukes, E.W.; Andersson, G.; Manchaiah, V.; Kaldo, V. Cognitive Behavioral Therapy for Tinnitus; Plural Publishing: San Diego, CA, USA, 2021. [Google Scholar]
- Meikle, M.B.; Henry, J.A.; Griest, S.E.; Stewart, B.J.; Abrams, H.B.; McArdle, R.; Myers, P.J.; Newman, C.W.; Sandridge, S.; Turk, D.C.; et al. The tinnitus functional index: Development of a new clinical measure for chronic, intrusive tinnitus. Ear Hear. 2012, 33, 153–176. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Rabin, R.; de Charro, F. EQ-5D: A measure of health status from the EuroQol Group. Ann. Med. 2001, 33, 337–343. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Hillsdale, N.J., Ed.; Lawrence Erlbaum Associates, Publishers: Mahwah, NJ, USA, 1988. [Google Scholar]
- Beukes, E.W.; Baguley, D.M.; Allen, P.M.; Manchaiah, V.; Andersson, G. Audiologist-Guided Internet-Based Cognitive Behavior Therapy for Adults With Tinnitus in the United Kingdom: A Randomized Controlled Trial. Ear Hear. 2018, 39, 423–433. [Google Scholar] [CrossRef]
- Andersson, G. Tinnitus loudness matchings in relation to annoyance and grading of severity. Auris Nasus Larynx 2003, 30, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Vasudevan, H.; Palaniswamy, H.P.; Balakrishnan, R.; Rajashekhar, B. Cortical Reorganization Following Psychoeducational Counselling and Residual Inhibition Therapy (RIT) in Individuals with Tinnitus. Int. Arch. Otorhinolaryngol. 2022, 26, e701–e711. [Google Scholar] [CrossRef] [PubMed]
- McFerran, D.J.; Stockdale, D.; Holme, R.; Large, C.H.; Baguley, D.M. Why Is There No Cure for Tinnitus? Front. Neurosci. 2019, 13, 802. [Google Scholar] [CrossRef] [PubMed]
- Manchaiah, V.; Londero, A.; Deshpande, A.K.; Revel, M.; Palacios, G.; Boyd, R.L.; Ratinaud, P. Online Discussions About Tinnitus: What Can We Learn From Natural Language Processing of Reddit Posts? Am. J. Audiol. 2022, 31, 993–1002. [Google Scholar] [CrossRef]

| Socio-Demographic Variable | Overall N = 152 | ICBT n = 107 | No Intervention n = 45 | p-Value |
|---|---|---|---|---|
| Age (years), mean (SD) | 57.3 (11.8) | 56.5 (12.3) | 59.3 (10.3) | 0.179 |
| Gender (n) | ||||
| Male | 59 (38.8%) | 37 (34.6%) | 22 (48.9%) | 0.098 |
| Female | 93 (61.2%) | 70 (65.4%) | 23 (51.1%) | |
| Employment status (n) | ||||
| Entry level/unskilled work | 2 (1.3%) | 2 (1.9%) | 0 (0.0%) | 0.141 |
| Skilled/professional work | 85 (55.9%) | 64 (59.8%) | 21 (46.7%) | |
| Retired | 54 (35.5%) | 36 (33.6%) | 18 (40.0%) | |
| Not working/unemployed | 11 (7.2%) | 5 (4.7%) | 6 (13.3%) | |
| Education (n) | ||||
| <High School | 1 (0.7) | 1 (0.9%) | 0 (0.0%) | 0.110 |
| High School | 16 (10.5) | 10 (9.3%) | 6 (13.3%) | |
| Some college but not degree | 43 (28.3) | 25 (23.4%) | 18 (40.0%) | |
| >University degree | 92 (60.5) | 71 (66.4%) | 21 (46.7%) | |
| Tinnitus duration (years), mean (SD) | 13.2 (14.9) | 12.8 (15.9) | 14.0 (12.0) | 0.293 |
| Frequency of tinnitus awareness, mean (SD) | ||||
| Morning | 2.6 (0.7) | 2.6 (0.6) | 2.6 (0.7) | 0.949 |
| Afternoon | 2.3 (0.7) | 2.2 (0.7) | 2.5 (0.7) | 0.064 |
| Evening | 2.6 (0.6) | 2.6 (0.6) | 2.7 (0.5) | 0.219 |
| Night | 2.3 (0.9) | 2.2 (0.9) | 2.4 (0.8) | 0.322 |
| Outcome Measures | Overall N = 152 | ICBT n = 107 | No Intervention n = 45 | p-Value | Adjusted p-Value |
|---|---|---|---|---|---|
| TFI Total | 54.54 (21.69) | 54.74 (22.19) | 54.07 (19.12) | 0.860 | 1.00 |
| GAD-7 | 6.97 (5.57) | 7.67 (5.81) | 5.31 (4.57) | 0.009 | 0.009 |
| PHQ-9 | 7.44 (5.85) | 8.09 (6.17) | 5.89 (4.74) | 0.019 | 0.019 |
| ISI | 11.31 (6.34) | 11.85 (6.42) | 10.02 (6.02) | 0.105 | 0.105 |
| EQ-5D-5L VAS | 75.80 (15.74) | 75.55 (15.91) | 76.40 (15.49) | 0.763 | 0.763 |
| TQIQ Total | 52.29 (17.33) | 53.12 (16.89) | 50.31 (18.37) | 0.363 | 1.00 |
| TQIQ Loudness | 7.20 (2.20) | 7.15 (2.18) | 7.33 (2.27) | 0.639 | 1.00 |
| TQIQ Pitch | 6.95 (2.65) | 6.90 (2.67) | 7.09 (2.64) | 0.685 | 1.00 |
| TQIQ Complexity | 1.78 (2.40) | 1.80 (2.43) | 1.73 (2.34) | 0.869 | 1.00 |
| TQIQ Frequency | 7.13 (2.39) | 7.04 (2.67) | 7.33 (2.67) | 0.517 | 1.00 |
| TQIQ Coexisting | 5.39 (2.59) | 5.67 (2.61) | 4.73 (2.43) | 0.041 | 0.451 |
| TQIQ Distractibility | 4.09 (2.80) | 4.06 (2.75) | 4.16 (2.94) | 0.842 | 1.00 |
| TQIQ Maskability | 4.66 (2.80) | 4.64 (2.74) | 4.71 (2.97) | 0.880 | 1.00 |
| TQIQ Mood | 3.98 (3.13) | 4.38 (3.05) | 3.02 (3.12) | 0.014 | 0.154 |
| TQIQ Loud sounds | 5.41 (3.38) | 5.50 (3.34) | 5.18 (3.49) | 0.588 | 1.00 |
| TQIQ Sensitivity | 5.70 (2.88) | 5.98 (2.71) | 5.02 (3.17) | 0.060 | 0.660 |
| TQIQ Internal qualities * | 5.90 (2.08) | 5.91 (2.06) | 5.89 (2.14) | 0.967 | 1.00 |
| TQIQ External qualities ** | 5.03 (2.42) | 5.29 (2.34) | 4.41 (2.53) | 0.040 | 0.080 |
| TQIQ Mild (score 0–37) | 26.08 (7.52) | 25.53 (6.60) | 26.82 (8.91) | 0.676 | 1.00 |
| TQIQ Significant (score 38–51) | 44.90 (3.60) | 44.92 (3.52) | 44.85 (3.95) | 0.953 | 1.00 |
| TQIQ Severe (score ≥ 52) | 65.84 (10.64) | 65.79 (10.76) | 66.00 (10.58) | 0.938 | 1.00 |
| Outcome Measures | ICBT Mean ∆ (95% CI) | No Intervention Mean ∆ (95% CI) | Difference Between Groups | ||
|---|---|---|---|---|---|
| Mean ∆ (95% CI) | ES | p-Value | |||
| TFI Total | 26.03 (21.83,30.23) | 15.79 (10.06,21.53) | 10.24 (−17.99,−2.49) | 0.50 | 0.010 |
| GAD-7 | 3.59 (2.63,4.55) | 0.97 (−0.27,2.21) | 2.62 (0.86,4.38) | 0.55 | 0.002 |
| PHQ-9 | 4.04 (2.92,5.16) | 1.56 (0.15,2.96) | 2.48 (0.45,4.52) | 0.47 | 0.007 |
| ISI | 4.91 (93.82,6.00) | 2.28 (0.95,3.61) | 2.63 (0.65,4.61) | 0.51 | 0.003 |
| EQ-5D-5L VAS | −4.26 (−6.84,−1.67) | −0.75 (−3.58,2.08) | −3.51 (−8.13,1.12) | −0.29 | 0.136 |
| TQIQ Total | 14.82 (11.83,17.82) | 1.04 (−2.31,4.40) | 13.78 (8.70,18.86) | 0.95 | <0.001 |
| TQIQ Loudness | 2.05 (1.60,2.49) | 0.66 (0.11,1.23) | 1.38 (0.61,2.15) | 0.63 | <0.001 |
| TQIQ Pitch | 2.53 (2.04,3.00) | 0.93 (0.43,1.44) | 1.59 (0.79,2.39) | 0.69 | <0.001 |
| TQIQ Complexity | 0.49 (0.22,0.77) | −0.14 (−0.67,0.40) | 0.63 (0.09,1.17) | 0.41 | 0.024 |
| TQIQ Frequency | 2.10 (1.62,2.56) | 0.20 (−0.28,0.68) | 1.89 (1.11,2.68) | 0.85 | <0.001 |
| TQIQ Coexisting | 1.69 (1.25,2.14) | 0.38 (−0.17,0.93) | 1.31 (0.55,2.08) | 0.60 | <0.001 |
| TQIQ Distractibility | 0.96 (0.52,1.40) | −0.76 (−1.36,−0.15) | 1.72 (0.94,2.50) | 0.77 | <0.001 |
| TQIQ Maskability | 1.22 (0.78,1.67) | −0.64 (−1.29,0.00) | 1.87 (1.07,2.67) | 0.82 | <0.001 |
| TQIQ Mood | 1.04 (0.46,1.61) | −0.56 (−1.34,0.23) | 1.59 (0.58,2.61) | 0.55 | 0.002 |
| TQIQ Loud sounds | 1.49 (0.94,2.03) | 0.73 (−0.10,1.56) | 0.75 (−0.24,1.75) | 0.27 | 0.136 |
| TQIQ Sensitivity | 1.26 (0.75,1.77) | 0.22 (−0.55,1.00) | 1.04 (0.12,1.96) | 0.40 | 0.028 |
| TQIQ Internal qualities * | 1.76 (1.41,2.11) | 0.13 (−0.22,0.48) | 1.63 (1.14,2.12) | 0.98 | <0.001 |
| TQIQ External qualities ** | 1.26 (0.86,1.67) | 0.13 (−0.44,0.71) | 1.13 (0.41,1.85) | 0.55 | 0.002 |
| TQIQ Mild (score 0–37) | 8.67 (1.75,15.58) | 2.27 (−5.16,9.71) | 6.39 (−3.37,16.15) | 0.54 | 0.189 |
| TQIQ Significant (score 38–51) | 15.00 (10.37,19.63) | −1.92 (−9.52,5.67) | 16.92 (8.20,25.64) | 1.26 | <0.001 |
| TQIQ Severe (score ≥52) | 16.36 (11.72,21.00) | 2.24 (−2.55,7.03) | 14.12 (7.60,20.64) | 0.89 | <0.001 |
| TQIQ MCID Category | ICBT | No Intervention | ||||
|---|---|---|---|---|---|---|
| N | Mean Diff. (SD) | 95% CI | N | Mean Diff. (SD) | 95% CI | |
| Overall difference score < 19 | 66 (61.7%) | 4.94 (9.08) | 2.71, 7.17 | 41 (91%) | −0.95 (9.55) | −3.97, 2.06 |
| Overall difference score ≥ 19 | 41 (38.3%) | 30.73 (9.67) | 27.68, 33.78 | 4 (9%) | 21.50 (1.73) | 18.74, 24.26 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manchaiah, V.; Andersson, G.; Beukes, E.W.; Fagelson, M.A.; Swanepoel, D.W.; Maidment, D. Changes in Perceived Tinnitus Sound Qualities Following Internet-Based Cognitive Behavioral Therapy for Tinnitus. Clin. Pract. 2025, 15, 69. https://doi.org/10.3390/clinpract15040069
Manchaiah V, Andersson G, Beukes EW, Fagelson MA, Swanepoel DW, Maidment D. Changes in Perceived Tinnitus Sound Qualities Following Internet-Based Cognitive Behavioral Therapy for Tinnitus. Clinics and Practice. 2025; 15(4):69. https://doi.org/10.3390/clinpract15040069
Chicago/Turabian StyleManchaiah, Vinaya, Gerhard Andersson, Eldré W. Beukes, Marc A. Fagelson, De Wet Swanepoel, and David Maidment. 2025. "Changes in Perceived Tinnitus Sound Qualities Following Internet-Based Cognitive Behavioral Therapy for Tinnitus" Clinics and Practice 15, no. 4: 69. https://doi.org/10.3390/clinpract15040069
APA StyleManchaiah, V., Andersson, G., Beukes, E. W., Fagelson, M. A., Swanepoel, D. W., & Maidment, D. (2025). Changes in Perceived Tinnitus Sound Qualities Following Internet-Based Cognitive Behavioral Therapy for Tinnitus. Clinics and Practice, 15(4), 69. https://doi.org/10.3390/clinpract15040069









