Role of Cerebral Oximetry in Reducing Postoperative End-Organ Dysfunction After Major Non-Cardiac Surgery: A Randomised Controlled Trial
Abstract
1. Introduction
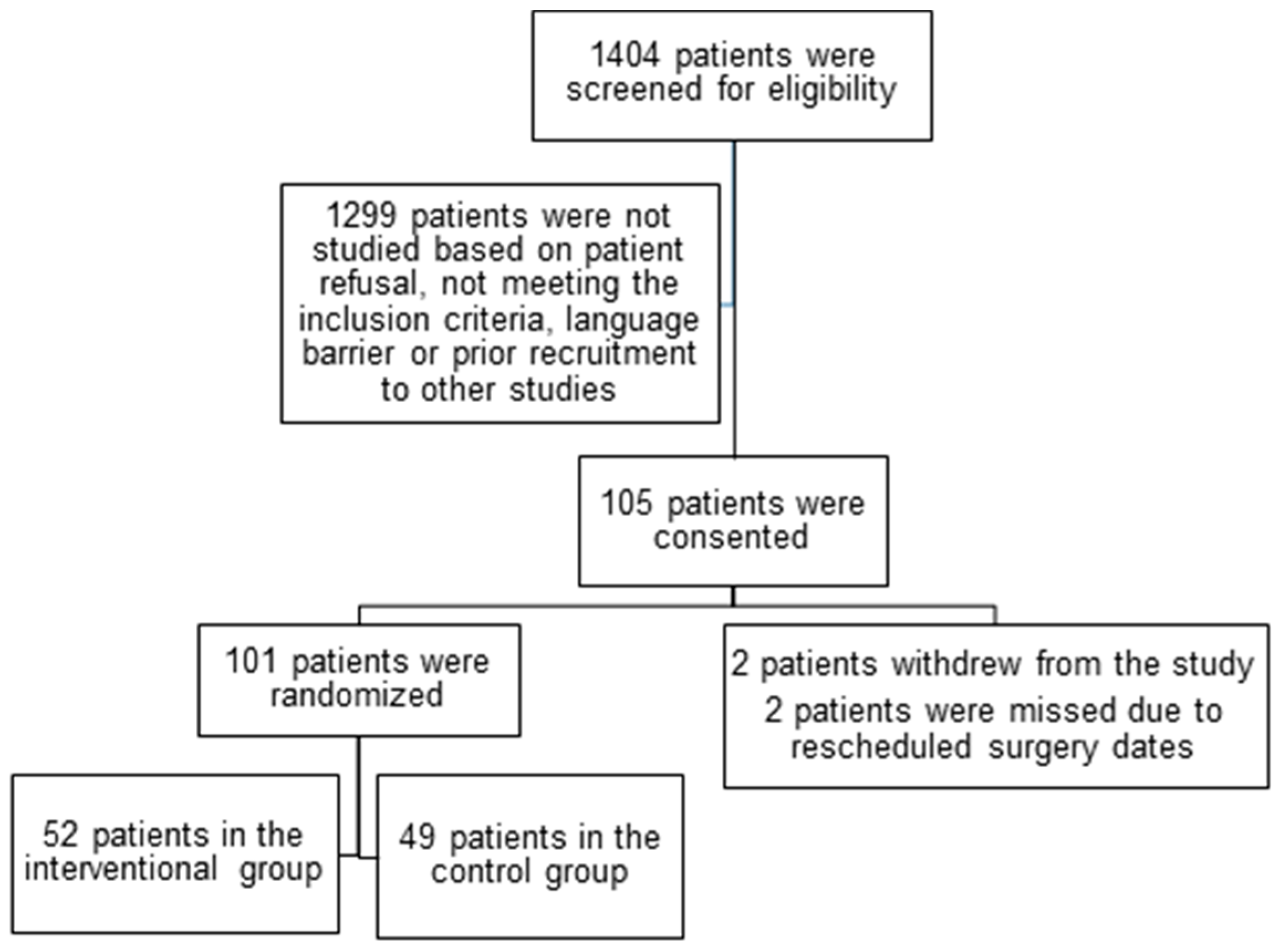
2. Materials and Methods
3. Results
Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| rSO2 | Regional cerebral oxygen saturation |
| RCT | Randomised controlled trial |
| QoR15 | Quality of Recovery-15 |
| DFS | Disability Free Survival |
| WHODAS | World Health Organization Disability Assessment |
References
- Story, D.A.; Leslie, K.; Myles, P.S.; Fink, M.; Poustie, S.J.; Forbes, A.; REASON Investigators, Australian and New Zealand College of Anaesthetists Trials Group. Complications and mortality in older surgical patients in Australia and New Zealand (the REASON study): A multicentre, prospective, observational study. Anaesthesia 2010, 65, 1022–1030. [Google Scholar] [CrossRef]
- Murkin, J.M.; Adams, S.J.; Novick, R.J.; Quantz, M.; Bainbridge, D.; Iglesias, I.; Fox, S. Monitoring brain oxygen saturation during coronary bypass surgery: A randomized, prospective study. Anesth. Analg. 2007, 104, 51–58. [Google Scholar] [CrossRef]
- Scott, J.P.; Hoffman, G.M. Near-infrared spectroscopy: Exposing the dark (venous) side of the circulation. Paediatr. Anaesth. 2014, 24, 74–88. [Google Scholar] [CrossRef]
- Paarmann, H.; Heringlake, M.; Heinze, H.; Hanke, T.; Sier, H.; Karsten, J.; Schön, J. Non-invasive cerebral oxygenation reflects mixed venous oxygen saturation during the varying haemodynamic conditions in patients undergoing transapical transcatheter aortic valve implantation. Interact. Cardiovasc. Thorac. Surg. 2012, 14, 268–272. [Google Scholar] [CrossRef] [PubMed]
- Oh, C.; Baek, S.; Lee, S.; Shim, M.S.; Han, S.J.; Kim, Y.H.; Hong, B. Noninvasive tracking of mixed venous oxygen saturation via near-infrared spectroscopy cerebral oximetry: A retrospective observational study. Sci. Rep. 2023, 13, 21704. [Google Scholar] [CrossRef] [PubMed]
- Murkin, J.M. Cerebral oximetry: Monitoring the brain as the index organ. Anesthesiology 2011, 114, 12–13. [Google Scholar] [CrossRef]
- Green, D.W. A retrospective study of changes in cerebral oxygenation using a cerebral oximeter in older patients undergoing prolonged major abdominal surgery. Eur. J. Anaesthesiol. 2007, 24, 230–234. [Google Scholar] [CrossRef]
- Casati, A.; Fanelli, G.; Pietropaoli, P.; Proietti, R.; Tufano, R.; Montanini, S. Monitoring cerebral oxygen saturation in elderly patients undergoing general abdominal surgery: A prospective cohort study. Eur. J. Anaesthesiol. 2007, 24, 59–65. [Google Scholar] [CrossRef]
- Yao, F.S.; Tseng, C.C.; Ho, C.Y.; Levin, S.K.; Illner, P. Cerebral oxygen desaturation is associated with early postoperative neuropsychological dysfunction in patients undergoing cardiac surgery. J. Cardiothorac. Vasc. Anesth. 2004, 18, 552–558. [Google Scholar] [CrossRef]
- Slater, J.P.; Guarino, T.; Stack, J.; Vinod, K.; Bustami, R.T.; Brown, J.M., III; Rodriguez, A.L.; Magovern, C.J.; Zaubler, T.; Freundlich, K.; et al. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann. Thorac. Surg. 2009, 87, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.; Kazan, R.; Taddei, R.; Zaouter, C.; Cyr, S.; Hemmerling, T.M. Reduced cerebral oxygen saturation during thoracic surgery predicts early postoperative cognitive dysfunction. Br. J. Anaesth. 2012, 108, 623–629. [Google Scholar] [CrossRef]
- Goldman, S.; Sutter, F.; Ferdinand, F.; Trace, C. Optimizing intraoperative cerebral oxygen delivery using noninvasive cerebral oximetry decreases the incidence of stroke for cardiac surgical patients. Heart Surg. Forum 2004, 7, E376–E381. [Google Scholar] [CrossRef]
- Heringlake, M.; Garbers, C.; Käbler, J.H.; Anderson, I.; Heinze, H.; Schön, J.; Hanke, T. Preoperative cerebral oxygen saturation and clinical outcomes in cardiac surgery. Anesthesiology 2011, 114, 58–69. [Google Scholar] [CrossRef]
- Schoen, J.; Meyerrose, J.; Paarmann, H.; Heringlake, M.; Hueppe, M.; Berger, K.U. Preoperative regional cerebral oxygen saturation is a predictor of postoperative delirium in on-pump cardiac surgery patients: A prospective observational trial. Crit. Care 2011, 15, R218. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, Y.; Yoshimura, M.; Utada, K.; Setoyama, K.; Matsumoto, M.; Sakabe, T. Prediction of postoperative delirium after abdominal surgery in the elderly. J. Anesth. 2009, 23, 51–56. [Google Scholar] [CrossRef]
- Casati, A.; Fanelli, G.; Pietropaoli, P.; Proietti, R.; Tufano, R.; Danelli, G.; Servillo, G. Continuous monitoring of cerebral oxygen saturation in elderly patients undergoing major abdominal surgery minimizes brain exposure to potential hypoxia. Anesth. Analg. 2005, 101, 740–747. [Google Scholar] [CrossRef] [PubMed]
- Deschamps, A.; Hall, R.; Grocott, H.; Mazer, C.D.; Choi, P.T.; Turgeon, A.F.; Mckay, W. Cerebral oximetry monitoring to maintain normal cerebral oxygen saturation during high-risk cardiac surgery: A randomized controlled feasibility trial. Anesthesiology 2016, 124, 826–836. [Google Scholar] [CrossRef]
- Subramanian, B.; Nyman, C.; Fritock, M.; Klinger, R.Y.; Sniecinski, R.; Roman, P.; Hogue, C.W. A multicenter pilot study assessing regional cerebral oxygen desaturation frequency during cardiopulmonary bypass and responsiveness to an intervention algorithm. Anesth. Analg. 2016, 122, 1786–1793. [Google Scholar] [CrossRef] [PubMed]
- Lei, L.; Katznelson, R.; Fedorko, L.; Carroll, J.; Poonawala, H.; Machina, M.; Djaiani, G. Cerebral oximetry and postoperative delirium after cardiac surgery: A randomised, controlled trial. Anaesthesia 2017, 72, 1456–1466. [Google Scholar] [CrossRef]
- Thiele, R.H.; Shaw, A.D.; Bartels, K.; Brown, C.H., IV; Grocott, H.; Heringlake, M.; Perioperative Quality, Initative. American society for enhanced recovery and perioperative quality initiative joint consensus statement on the role of neuromonitoring in perioperative outcomes: Cerebral near-infrared spectroscopy. Anesth. Analg. 2020, 131, 1444–1455. [Google Scholar] [CrossRef]
- Raghunathan, K.; Kerr, D.; Xian, Y.; McCarthy, G.; Habib, R.; Nicoara, A.; Shaw, A.D. Cerebral oximetry during adult cardiac surgery is associated with improved postoperative outcomes. J. Cardiothorac. Vasc. Anesth. 2022, 36, 3529–3542. [Google Scholar] [CrossRef] [PubMed]
- Baehner, T.; Perlewitz, O.; Ellerkmann, R.K.; Menzenbach, J.; Brand, G.; Thudium, M.; Velten, M. Preoperative cerebral oxygenation in high-risk noncardiac surgical patients: An observational study on postoperative mortality and complications. J. Clin. Monit. Comput. 2023, 37, 743–752. [Google Scholar] [CrossRef]
- Kahl, U.; Rademacher, C.; Harler, U.; Juilfs, N.; Pinnschmidt, H.O.; Beck, S.; Fischer, M. Intraoperative impaired cerebrovascular autoregulation and delayed neurocognitive recovery after major oncologic surgery: A secondary analysis of pooled data. J. Clin. Monit. Comput. 2022, 36, 765–773. [Google Scholar] [CrossRef]
- Chuan, A.; Short, T.G.; Peng, A.Z.; Wen, S.Y.; Sun, A.X.; Ting, T.H.; Aneman, A. Is cerebrovascular autoregulation associated with outcomes after major noncardiac surgery? a prospective observational pilot study. Acta Anaesthesiol. Scand. 2019, 63, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Ono, M.; Brady, K.; Easley, R.B.; Brown, C.; Kraut, M.; Gottesman, R.F.; Hogue, C.W., Jr. Duration and magnitude of blood pressure below cerebral autoregulation threshold during cardiopulmonary bypass is associated with major morbidity and operative mortality. J. Thorac. Cardiovasc. Surg. 2014, 147, 483–489. [Google Scholar] [CrossRef] [PubMed]
| Variable | Intervention Group | Control Group |
|---|---|---|
| (n = 52) | (n = 49) | |
| Age, mean ± SD, years | 70 ± 5 | 69 ± 6 |
| Male gender, n (%) | 25 (48) | 27 (55) |
| Height, cm | 164 ± 17 | 167 ± 12 |
| Weight, kg | 73 ± 23 | 77 ± 19 |
| Creatinine, mean ± SD, μM | 82 ± 27 | 86 ± 37 |
| Haemoglobin, mean ± SD, g/dL | 134 ± 19 | 135 ± 17 |
| Type of surgery, n (%) | ||
| Gynaecology | 10 (19) | 8 (17) |
| Urology | 10 (19) | 12 (25) |
| General Surgery | 7 (14) | 5 (10) |
| Orthopaedics | 6 (11.5) | 6 (12) |
| Plastics | 1 (2) | 4 (8) |
| Vascular | 10 (19) | 7 (14) |
| Head and Neck | 2 (4) | 2 (4) |
| Liver | 6 (11.5) | 5 (10) |
| Duration of surgery, mean ± SD, min | 362 ± 148 | 328 ± 117 |
| Blood product transfusion, n (%) | 5 (10) | 4 (8) |
| Fluid balance, mean ± SD, ml | 2229 ± 1352 | 1913 ± 895 |
| Vasoactive drugs, n (%) | 13 (25) | 12 (24) |
| Past Medical History, n (%) | ||
| Diabetes mellitus | 12 (23) | 10 (20) |
| Coronary artery disease | 7 (14) | 6 (12) |
| Hypertension | 34 (65) | 29 (59) |
| Cerebrovascular accident/transient | ||
| Ischemic attack | 3 (6) | 4 (8) |
| Peripheral vascular disease | 8 (15) | 6 (12) |
| Chronic obstructive pulmonary disease | 5 (10) | 4 (8) |
| Chronic renal disease | 4 (8) | 3 (6) |
| Myocardial infarction | 4 (8) | 4 (8) |
| Thyroid disease | 5 (10) | 5 (10) |
| Atrial fibrillation | 1 (2) | 2 (4) |
| Alcohol > 20 units per week | 5 (10) | 5 (10) |
| Smoking history | 18 (35) | 15 (30) |
| Medications, n (%) | ||
| Beta-blockers | 10 (19) | 9 (18) |
| Angiotensin-converting enzyme inhibitors | 15 (29) | 13 (26) |
| Calcium channel blockers | 9 (17) | 10 (20) |
| Aspirin | 18 (35) | 18 (37) |
| Statins | 30 (58) | 25 (51) |
| Antidepressants | 2 (4) | 3 (6) |
| Functional scores, median [range] Frailty scale | 2.5 [1, 5] | 3 [1, 7] |
| Duke Activity Status Index | 24 [5, 51] | 21 [7, 58] |
| Interventional Group (n = 52) | Control Group (n = 49) | |||
|---|---|---|---|---|
| Left Side | Right Side | Left Side | Right Side | |
| Baseline rSO2 (%) | 62.5 [52, 84] | 63 [56, 73] | 64 [52, 82] | 63 [43, 79] |
| Number of patients with rSO2 reduction ≥ 10% from baseline, n (%) | 34 (65) | 32 (62) | 35 (71) | 34 (69) |
| Bilateral | 30 (58) | 31 (63) | ||
| Maximum reduction of rSO2 (%) | 12 [0, 35] | 12 [0, 61] | 15 [0, 65] | 12 [0, 85] |
| Number of episodes of rSO2 reduction ≥ 10% from baseline | 1 [0, 7] | 1 [0, 6] | 2 [0, 8] | 2 [0, 7] |
| Bilateral | 2.5 [0, 10] | 4 [0, 15] | ||
| Duration of rSO2 reduction ≥ 10% from baseline, min | 5.5 [0, 128] | 4 [0, 30] | 12 [0, 240] | 7 [0, 364] |
| Bilateral | 5 [0, 128] * | 9 [0, 364] | ||
| Variable, n % | Intervention Group (n = 52) | Control Group (n = 49) |
|---|---|---|
| Myocardial infarction | 4 (8) | 3 (6) |
| Atrial fibrillation | 2 (4) | 2 (4) |
| Delirium | 1 (2) | 2 (4) |
| Stroke/transient ischemic attack | 1 (2) | 0 |
| Renal failure | 2 (4) | 2 (4) |
| Pulmonary embolism | 1 (2) | 0 |
| Sepsis | 1 (2) | 1 (2) |
| Pneumonia | 1 (2) | 2 (4) |
| Wound infection | 2 (4) | 2 (4) |
| Reintubation | 1 (2) | 1 (2) |
| Return to operating room within 24 h | 1 (2) | 1 (2) |
| Length of hospital stay, days [range] | 3 [1, 16] | 3 [1, 14] |
| 30-day mortality | 0 | 0 |
| Quality of Recovery-15, n [range] | ||
| At baseline | 127 [99, 150] | 124 [48, 148] |
| At postoperative day 1 | 105 [54, 145] * | 108 [64, 127] * |
| At hospital discharge | 110 [44, 145] * | 111 [64, 135] * |
| World Health Organization Disability Assessment Schedule, n [range] | 4 [1, 23] | 4 [1, 34] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bieze, M.; Foley, K.; Beattie, W.S.; Carroll, J.; Poonawala, H.; Ti, L.-K.; Djaiani, G. Role of Cerebral Oximetry in Reducing Postoperative End-Organ Dysfunction After Major Non-Cardiac Surgery: A Randomised Controlled Trial. Clin. Pract. 2025, 15, 213. https://doi.org/10.3390/clinpract15110213
Bieze M, Foley K, Beattie WS, Carroll J, Poonawala H, Ti L-K, Djaiani G. Role of Cerebral Oximetry in Reducing Postoperative End-Organ Dysfunction After Major Non-Cardiac Surgery: A Randomised Controlled Trial. Clinics and Practice. 2025; 15(11):213. https://doi.org/10.3390/clinpract15110213
Chicago/Turabian StyleBieze, Matthanja, Karen Foley, W. Scott Beattie, Jo Carroll, Humara Poonawala, Lian-Kah Ti, and George Djaiani. 2025. "Role of Cerebral Oximetry in Reducing Postoperative End-Organ Dysfunction After Major Non-Cardiac Surgery: A Randomised Controlled Trial" Clinics and Practice 15, no. 11: 213. https://doi.org/10.3390/clinpract15110213
APA StyleBieze, M., Foley, K., Beattie, W. S., Carroll, J., Poonawala, H., Ti, L.-K., & Djaiani, G. (2025). Role of Cerebral Oximetry in Reducing Postoperative End-Organ Dysfunction After Major Non-Cardiac Surgery: A Randomised Controlled Trial. Clinics and Practice, 15(11), 213. https://doi.org/10.3390/clinpract15110213






