Running Cadence and the Influence on Frontal Plane Knee Deviations
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
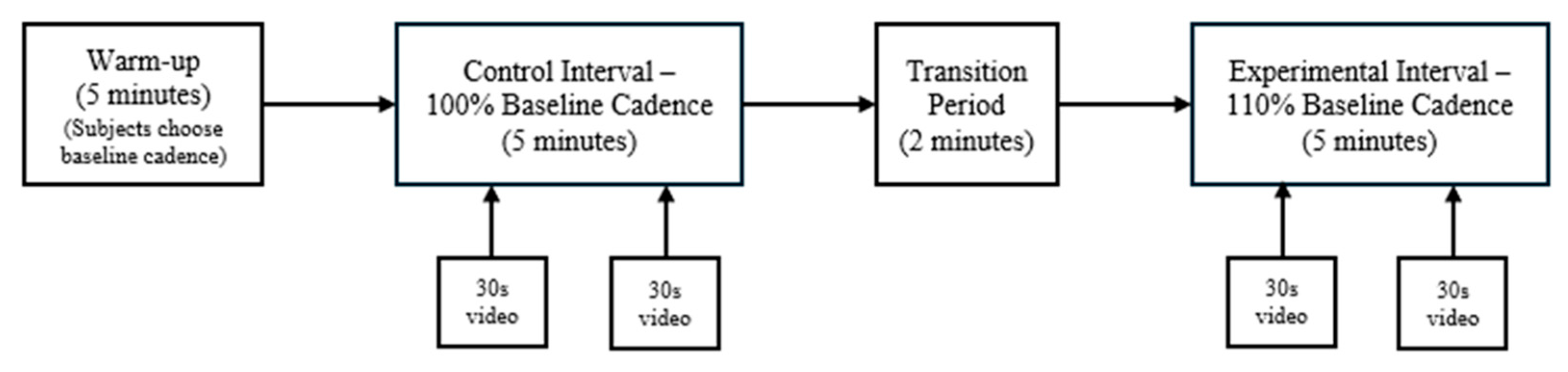
2.2. Procedure
2.3. Data Acquisition
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gaitonde, D.Y.; Ericksen, A.; Robbins, R.C. Patellofemoral Pain Syndrome. Am. Fam. Physician 2019, 99, 88–94. [Google Scholar] [PubMed]
- Willy, R.W.; Hoglund, L.T.; Barton, C.J.; Bolgla, L.A.; Scalzitti, D.A.; Logerstedt, D.S.; Lynch, A.D.; Snyder-Mackler, L.; McDonough, C.M. Patellofemoral Pain. J. Orthop. Sports Phys. Ther. 2019, 49, CPG1–CPG95. [Google Scholar] [CrossRef] [PubMed]
- Capin, J.J.; Snyder-Mackler, L. The current management of patients with patellofemoral pain from the physical therapist’s perspective. Ann. Jt. 2018, 3, 40. [Google Scholar] [CrossRef] [PubMed]
- Barber Foss, K.D.; Myer, G.D.; Chen, S.S.; Hewett, T.E. Expected prevalence from the differential diagnosis of anterior knee pain in adolescent female athletes during preparticipation screening. J. Athl. Train. 2012, 47, 519–524. [Google Scholar] [CrossRef] [PubMed]
- Collins, N.J.; Bierma-Zeinstra, S.M.A.; Crossley, K.M.; van Linschoten, R.L.; Vicenzino, B.; van Middelkoop, M. Prognostic factors for patellofemoral pain: A multicentre observational analysis. Br. J. Sports Med. 2013, 47, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Nimon, G.; Murray, D.; Sandow, M.; Goodfellow, J. Natural history of anterior knee pain: A 14- to 20-year follow-up of nonoperative management. J. Pediatr. Orthop. 1998, 18, 118–122. [Google Scholar] [CrossRef]
- Rathleff, M.S.; Skuldbøl, S.K.; Rasch, M.N.B.; Roos, E.M.; Rasmussen, S.; Olesen, J.L. Care-seeking behaviour of adolescents with knee pain: A population-based study among 504 adolescents. BMC Musculoskelet. Disord. 2013, 14, 225. [Google Scholar] [CrossRef]
- Ferber, R.; Kendall, K.D.; Farr, L. Changes in knee biomechanics after a hip-abductor strengthening protocol for runners with patellofemoral pain syndrome. J. Athl. Train. 2011, 46, 142–149. [Google Scholar] [CrossRef]
- Petersen, W.; Ellermann, A.; Gösele-Koppenburg, A.; Best, R.; Rembitzki, I.V.; Brüggemann, G.P.; Liebau, C. Patellofemoral pain syndrome. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 2264–2274. [Google Scholar] [CrossRef]
- Cashman, G.E. The effect of weak hip abductors or external rotators on knee valgus kinematics in healthy subjects: A systematic review. J. Sport Rehabil. 2012, 21, 273–284. [Google Scholar] [CrossRef]
- Dierks, T.A.; Manal, K.T.; Hamill, J.; Davis, I. Lower extremity kinematics in runners with patellofemoral pain during a prolonged run. Med. Sci. Sports Exerc. 2011, 43, 693–700. [Google Scholar] [CrossRef] [PubMed]
- Stefanyshyn, D.J.; Stergiou, P.; Lun, V.M.Y.; Meeuwisse, W.H.; Worobets, J.T. Knee angular impulse as a predictor of patellofemoral pain in runners. Am. J. Sports Med. 2006, 34, 1844–1851. [Google Scholar] [CrossRef]
- Dierks, T.A.; Manal, K.T.; Hamill, J.; Davis, I.S. Proximal and distal influences on hip and knee kinematics in runners with patellofemoral pain during a prolonged run. J. Orthop. Sports Phys. Ther. 2008, 38, 448–456. [Google Scholar] [CrossRef]
- Powers, C.M. The influence of abnormal hip mechanics on knee injury: A biomechanical perspective. J. Orthop. Sports Phys. Ther. 2010, 40, 42–51. [Google Scholar] [CrossRef]
- Heiderscheit, B.C.; Chumanov, E.S.; Michalski, M.P.; Wille, C.M.; Ryan, M.B. Effects of step rate manipulation on joint mechanics during running. Med. Sci. Sports Exerc. 2011, 43, 296–302. [Google Scholar] [CrossRef] [PubMed]
- De Souza, J.R., Jr.; Rabelo, P.H.R.; Lemos, T.V.; Esculier, J.F.; Barbosa, G.M.P.; Matheus, J.P.C. Effects of two gait retraining programs on pain, function, and lower limb kinematics in runners with patellofemoral pain: A randomized controlled trial. PLoS ONE 2024, 19, e0295645. [Google Scholar] [CrossRef] [PubMed]
- Chumanov, E.S.; Wille, C.M.; Michalski, M.P.; Heiderscheit, B.C. Changes in muscle activation patterns when running step rate is increased. Gait Posture 2012, 36, 231–235. [Google Scholar] [CrossRef]
- Hafer, J.F.; Brown, A.M.; deMille, P.; Hillstrom, H.J.; Garber, C.E. The effect of a cadence retraining protocol on running biomechanics and efficiency: A pilot study. J. Sports Sci. 2015, 33, 724–731. [Google Scholar] [CrossRef] [PubMed]
- Lenhart, R.; Thelen, D.; Heiderscheit, B. Hip muscle loads during running at various step rates. J. Orthop. Sports Phys. Ther. 2014, 44, 766-A4. [Google Scholar] [CrossRef]
- Wellenkotter, J.; Kernozek, T.W.; Meardon, S.; Suchomel, T. The effects of running cadence manipulation on plantar loading in healthy runners. Int. J. Sports Med. 2014, 35, 779–784. [Google Scholar] [CrossRef]
- Schubert, A.G.; Kempf, J.; Heiderscheit, B.C. Influence of stride frequency and length on running mechanics: A systematic review. Sports Health 2014, 6, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Lenhart, R.L.; Smith, C.R.; Vignos, M.F.; Kaiser, J.; Heiderscheit, B.C.; Thelen, D.G. Influence of step rate and quadriceps load distribution on patellofemoral cartilage contact pressures during running. J. Biomech. 2015, 48, 2871–2878. [Google Scholar] [CrossRef] [PubMed]
- Willy, R.W.; Willson, J.D.; Clowers, K.; Baggaley, M.; Murray, N. The effects of body-borne loads and cadence manipulation on patellofemoral and tibiofemoral joint kinetics during running. J. Biomech. 2016, 49, 4028–4033. [Google Scholar] [CrossRef]
- Souza, R.B. An Evidence-Based Videotaped Running Biomechanics Analysis. Phys. Med. Rehabil. Clin. N. Am. 2016, 27, 217–236. [Google Scholar] [CrossRef]
- Eltoukhy, M.; Asfour, S.; Thompson, C.; Latta, L. Evaluation of the Performance of Digital Video Analysis of Human Motion: Dartfish Tracking System. Int. J. Sci. Eng. Res. 2012, 3, 1–6. [Google Scholar]
- Maykut, J.N.; Taylor-Haas, J.A.; Paterno, M.V.; DiCesare, C.A.; Ford, K.R. Concurrent validity and reliability of 2d kinematic analysis of frontal plane motion during running. Int. J. Sports Phys. Ther. 2015, 10, 136–146. [Google Scholar] [PubMed]
- Parks, M.T.; Wang, Z.; Siu, K.-C. Current Low-Cost Video-Based Motion Analysis Options for Clinical Rehabilitation: A Systematic Review. Phys. Ther. 2019, 99, 1405–1425. [Google Scholar] [CrossRef]
- Foch, E.; Aubol, K.; Milner, C.E. Relationship between iliotibial band syndrome and hip neuromechanics in women runners. Gait Posture 2020, 77, 64–68. [Google Scholar] [CrossRef]
- Tateuchi, H.; Shiratori, S.; Ichihashi, N. The effect of angle and moment of the hip and knee joint on iliotibial band hardness. Gait Posture 2015, 41, 522–528. [Google Scholar] [CrossRef]
- Pohl, M.B.; Mullineaux, D.R.; Milner, C.E.; Hamill, J.; Davis, I.S. Biomechanical predictors of retrospective tibial stress fractures in runners. J. Biomech. 2008, 41, 1160–1165. [Google Scholar] [CrossRef]
- Willson, J.D.; Davis, I.S. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clin. Biomech. 2008, 23, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Werner, D.M.; Di Stasi, S.; Lewis, C.; Barrios, J.A. Test-retest reliability and minimum detectable change for various frontal plane projection angles during dynamic tasks. Phys. Ther. Sport. 2019, 40, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, M.; Negrete, R.; Hanney, W.J.; Kolber, M.J. Quantifying Frontal Plane Knee Kinematics in Subjects with Anterior Knee Pain: The Reliability and Concurrent Validity of 2d Motion Analysis. Int. J. Sports Phys. Ther. 2018, 13, 86–93. [Google Scholar] [CrossRef] [PubMed]
- De Ruiter, C.J.; Verdijk, P.W.; Werker, W.; Zuidema, M.J.; de Haan, A. Stride frequency in relation to oxygen consumption in experienced and novice runners. Eur. J. Sport Sci. 2014, 14, 251–258. [Google Scholar] [CrossRef]
- Van Oeveren, B.T.; de Ruiter, C.J.; Beek, P.J.; van Dieën, J.H. Optimal stride frequencies in running at different speeds. PLoS ONE 2017, 12, e0184273. [Google Scholar] [CrossRef]
- Meinerz, C.; Fritz, J.; Cross, J.A.; Dziuk, C.; Kipp, K.; Vetter, C. Running to the beat: Does listening to music affect running cadence and lower extremity biomechanics? Gait Posture 2023, 103, 62–66. [Google Scholar] [CrossRef]
- Sakaguchi, M.; Shimizu, N.; Yanai, T.; Stefanyshyn, D.J.; Kawakami, Y. Hip rotation angle is associated with frontal plane knee joint mechanics during running. Gait Posture 2015, 41, 557–561. [Google Scholar] [CrossRef]
- Lopes, T.J.A.; Ferrari, D.; Ioannidis, J.; Simic, M.; Mícolis de Azevedo, F.; Pappas, E. Reliability and Validity of Frontal Plane Kinematics of the Trunk and Lower Extremity Measured with 2-Dimensional Cameras During Athletic Tasks: A Systematic Review with Meta-analysis. J. Orthop. Sports Phys. Ther. 2018, 48, 812–822. [Google Scholar] [CrossRef]
- Yong, J.R.; Silder, A.; Montgomery, K.L.; Fredericson, M.; Delp, S.L. Acute changes in foot strike pattern and cadence affect running parameters associated with tibial stress fractures. J. Biomech. 2018, 76, 1–7. [Google Scholar] [CrossRef]
- Futrell, E.E.; Jamison, S.T.; Tenforde, A.S.; Davis, I.S. Relationships between Habitual Cadence, Footstrike, and Vertical Load Rates in Runners. Med. Sci. Sports Exerc. 2018, 50, 1837–1841. [Google Scholar] [CrossRef]
- Chan, Z.Y.; Zhang, J.H.; Au, I.P.; An, W.W.; Shum, G.L.; Ng, G.Y.; Cheung, R.T. Gait Retraining for the Reduction of Injury Occurrence in Novice Distance Runners: 1-Year Follow-up of a Randomized Controlled Trial. Am. J. Sports Med. 2018, 46, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.M.; Vincent, H.K. Manipulating Cadence for Gait Re-training in Runners. Curr. Sports Med. Rep. 2017, 16, 381. [Google Scholar] [CrossRef] [PubMed]
| df | T-Value | 95% CI | Difference in Knee Angle Control vs. Experimental Intervals | |
|---|---|---|---|---|
| Right Knee Valgus | 9 | 10.13 | 2.72–1.73 | 2.23 |
| Left Knee Valgus | 9 | 6.49 | 2.74–1.34 | 2.05 |
| Combined Knee Valgus | 19 | 11.35 | 2.53–1.74 | 2.14 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peterson, J.R.; Sanders, C.R.; Reynolds, N.S.; Alford, C.A.; Platt, M.J.; Parr, J.J.; Twum, F.; Burns, J.R.; Dolbow, D.R. Running Cadence and the Influence on Frontal Plane Knee Deviations. Clin. Pract. 2024, 14, 2491-2498. https://doi.org/10.3390/clinpract14060195
Peterson JR, Sanders CR, Reynolds NS, Alford CA, Platt MJ, Parr JJ, Twum F, Burns JR, Dolbow DR. Running Cadence and the Influence on Frontal Plane Knee Deviations. Clinics and Practice. 2024; 14(6):2491-2498. https://doi.org/10.3390/clinpract14060195
Chicago/Turabian StylePeterson, Jacob R., Collin R. Sanders, Nathan S. Reynolds, Conner A. Alford, Michael J. Platt, Jeffrey J. Parr, Felix Twum, James R. Burns, and David R. Dolbow. 2024. "Running Cadence and the Influence on Frontal Plane Knee Deviations" Clinics and Practice 14, no. 6: 2491-2498. https://doi.org/10.3390/clinpract14060195
APA StylePeterson, J. R., Sanders, C. R., Reynolds, N. S., Alford, C. A., Platt, M. J., Parr, J. J., Twum, F., Burns, J. R., & Dolbow, D. R. (2024). Running Cadence and the Influence on Frontal Plane Knee Deviations. Clinics and Practice, 14(6), 2491-2498. https://doi.org/10.3390/clinpract14060195





