Disciplinary Imbalances in Urology and Gynecology Research Publications within Functional Urology
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Overview of Analyzed Abstracts and Publication Patterns
3.2. Discrepancy Scores Analysis
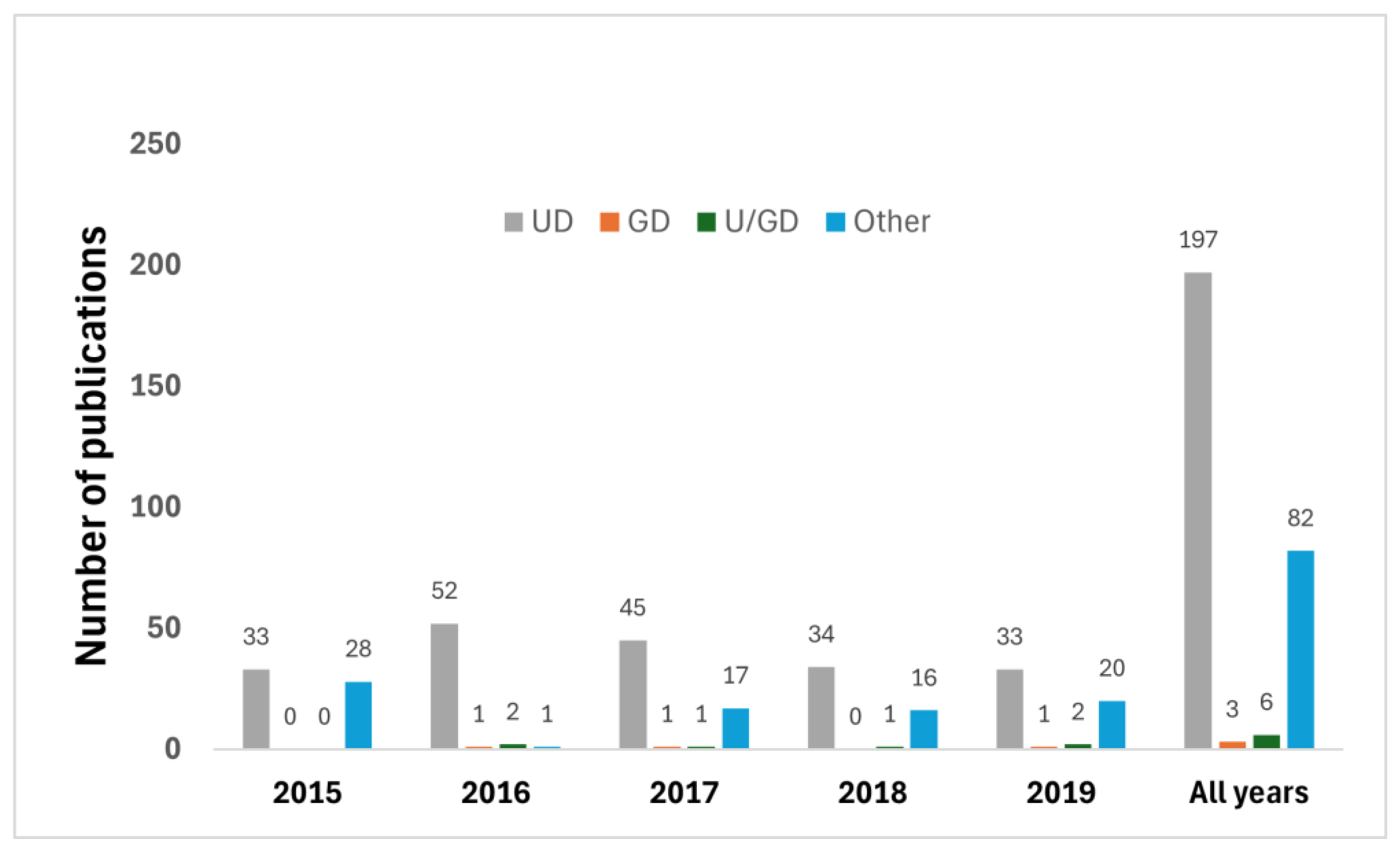
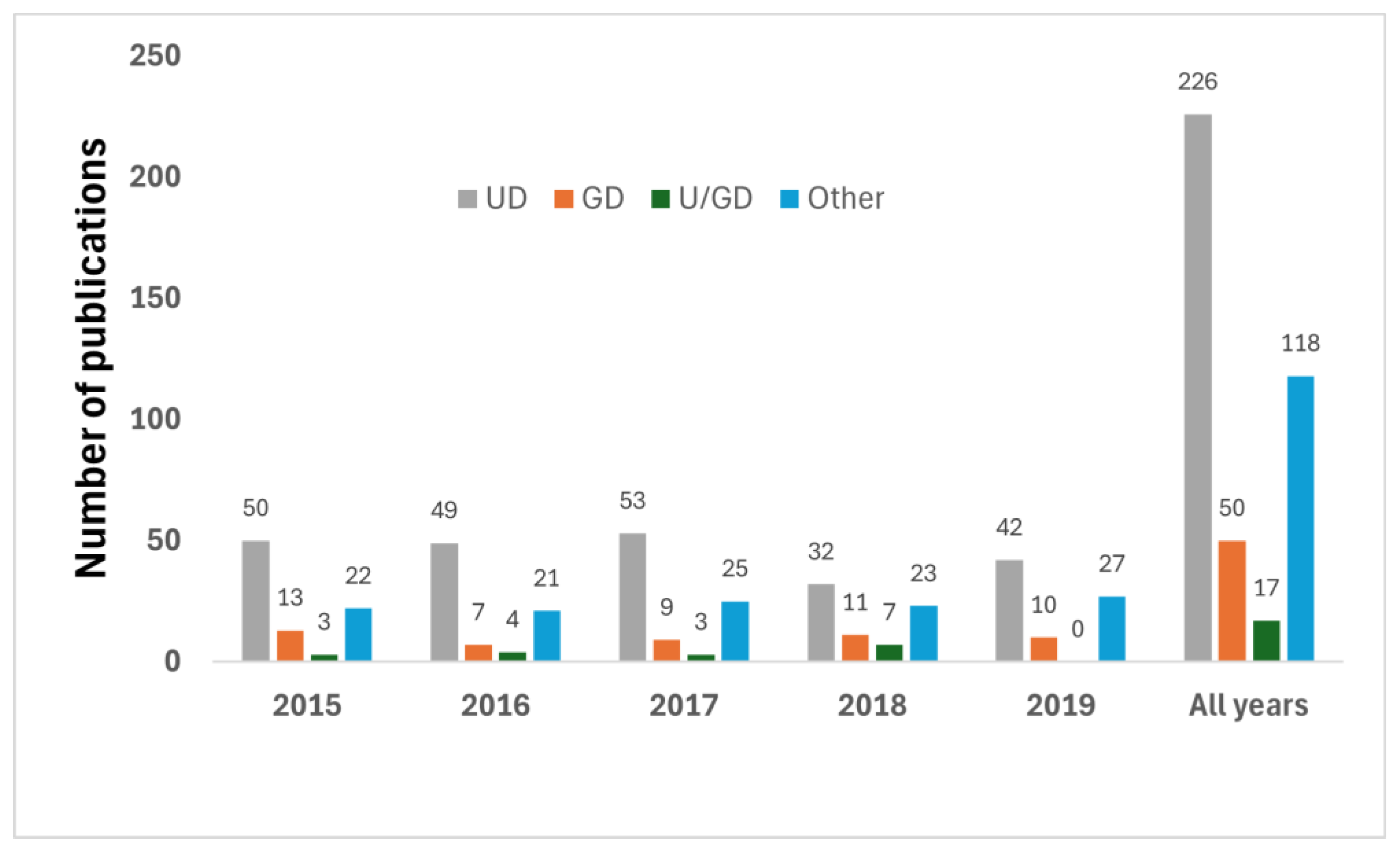
3.3. Origin of Publications by Speciality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kinsey, D.; Pretorius, S.; Glover, L.; Alexander, T. The Psychological Impact of Overactive Bladder: A Systematic Review. J. Health Psychol. 2016, 21, 69–81. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.D.; Amrute, K.V.; Badlani, G.H. Pelvic Organ Prolapse and Stress Urinary Incontinence: A Review of Etiological Factors. Indian. J. Urol. 2007, 23, 135–141. [Google Scholar] [PubMed]
- Bardsley, A. An Overview of Urinary Incontinence. Br. J. Nurs. 2016, 25, S14–S21. [Google Scholar] [CrossRef]
- Leśniczak, B.; Krasomski, G.; Stelmach, W.; Kowalska, A. Urinary Incontinence in Women as a Health and Social Problem. Adv. Med. Sci. 2007, 52 (Suppl. S1), 93–96. [Google Scholar]
- Palmer, S.J. Overview of Urinary Incontinence. Br. J. Community Nurs. 2023, 28, 410–412. [Google Scholar] [CrossRef]
- Chapple, C.R.; Fu, Q.; Xu, C. Functional and Reconstructive Urology (Part One). Asian J. Urol. 2018, 5, 55. [Google Scholar] [CrossRef] [PubMed]
- Chartier-Kastler, E.; Zimmern, P. Functional Urology 2015. World J. Urol. 2015, 33, 1213–1214. [Google Scholar] [CrossRef]
- Hoeritzauer, I.; Phé, V.; Panicker, J.N. Urologic Symptoms and Functional Neurologic Disorders. Handb. Clin. Neurol. 2016, 139, 469–481. [Google Scholar]
- Wein, A.J. Functional Urology in the BJUI. BJU Int. 2013, 112, 277. [Google Scholar] [CrossRef]
- Klingele, C.J. Advances in Urogynecology. Int. J. Fertil. Women’s Med. 2005, 50, 18–23. [Google Scholar]
- Lowenstein, L.; Rosenblatt, P.L.; Dietz, H.P.; Bitzer, J.; Kenton, K. New Advances in Urogynecology. Obstet. Gynecol. Int. 2012, 2012, 453059. [Google Scholar] [CrossRef] [PubMed]
- Umoh, U.E.; Arya, L.A. Surgery in Urogynecology. Minerva Med. 2012, 103, 23–36. [Google Scholar] [PubMed]
- Jackson, S.L.; Weber, A.M.; Hull, T.L.; Mitchinson, A.R.; Walters, M.D. Fecal Incontinence in Women with Urinary Incontinence and Pelvic Organ Prolapse. Obstet. Gynecol. 1997, 89, 423–427. [Google Scholar] [CrossRef]
- Salonia, A.; Zanni, G.; Briganti, A.; Fabbri, F.; Rigatti, P.; Montorsi, F. The Role of the Urologist in the Management of Female Sexual Dysfunctions. Curr. Opin. Urol. 2004, 14, 389–393. [Google Scholar] [CrossRef]
- Cao, C.D.; Teefey, P. Collaborative Efforts between Interventional Radiology and Obstetrics/Gynecology. Technol. Vasc. Interv. Radiol. 2021, 24, 100729. [Google Scholar] [CrossRef]
- Eke, N.; Eke, F.U. Collaboration in Urological Practice in the New Millennium. Niger. Postgrad. Med. J. 2002, 9, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Albertine, K.H. Stewardship of Integrity in Scientific Communication. Anat. Rec. 2018, 301, 1481–1487. [Google Scholar] [CrossRef]
- Buckwalter, J.A.; Tolo, V.T.; O’Keefe, R.J. How Do You Know It Is True? Integrity in Research and Publications: AOA Critical Issues. J. Bone Jt. Surg. 2015, 97, e2. [Google Scholar] [CrossRef][Green Version]
- Mogull, S. Ethics and Practice of Knowledge Integrity in Communicating Health and Medical Research. Rhetor. Health Med. 2021, 4. [Google Scholar] [CrossRef]
- Ratzan, S.C. More Evidence of Communication for Patients—Time for Action. J. Health Commun. 2007, 12, 605–606. [Google Scholar] [CrossRef]
- Ajuwon, A.J. The Relevance of Integrity in Research and Publication. Malawi Med. J. 2018, 30, 218. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.J.; Moher, D. Promote Scientific Integrity via Journal Peer Review Data. Science 2017, 357, 256–257. [Google Scholar] [CrossRef]
- Li, G.; Abbade, L.P.F.; Nwosu, I.; Jin, Y.; Leenus, A.; Maaz, M.; Wang, M.; Bhatt, M.; Zielinski, L.; Sanger, N.; et al. A Scoping Review of Comparisons between Abstracts and Full Reports in Primary Biomedical Research. BMC Med. Res. Methodol. 2017, 17, 181. [Google Scholar] [CrossRef] [PubMed]
- Jarvis, M.F.; Williams, M. Irreproducibility in Preclinical Biomedical Research: Perceptions, Uncertainties, and Knowledge Gaps. Trends Pharmacol. Sci. 2016, 37, 290–302. [Google Scholar] [CrossRef]
- Shakiba, S.; Shakiba, B.; Irani, S. Unpublished Abstracts Can Be Invaluable. Can. Urol. Assoc. J. 2014, 8, e60. [Google Scholar] [CrossRef][Green Version]
- Costa, E.; Inbar, Y.; Tannenbaum, D. Do Registered Reports Make Scientific Findings More Believable to the Public? Collabra Psychol. 2022, 8, 32607. [Google Scholar] [CrossRef]
- Falagas, M.E.; Rosmarakis, E.S. Clinical Decision-Making Based on Findings Presented in Conference Abstracts: Is It Safe for Our Patients? Eur. Heart J. 2006, 27, 2038–2039. [Google Scholar] [CrossRef][Green Version]
- Choudhri, A.F.; Siddiqui, A.; Khan, N.R.; Cohen, H.L. Understanding Bibliometric Parameters and Analysis. Radiographics 2015, 35, 736–746. [Google Scholar] [CrossRef]
- Garner, R.M.; Hirsch, J.A.; Albuquerque, F.C.; Fargen, K.M. Bibliometric Indices: Defining Academic Productivity and Citation Rates of Researchers, Departments and Journals. J. Neurointerv. Surg. 2018, 10, 102–106. [Google Scholar] [CrossRef]
- Yan, L.; Zhiping, W. Mapping the Literature on Academic Publishing: A Bibliometric Analysis on WOS. SAGE Open 2023, 13, 215824402311585. [Google Scholar] [CrossRef]
- Autorino, R.; Quarto, G.; Di Lorenzo, G.; De Sio, M.; Damiano, R. Are Abstracts Presented at the EAU Meeting Followed by Publication in Peer-Reviewed Journals?: A Critical Analysis. Eur. Urol. 2007, 51, 833–840. [Google Scholar] [CrossRef]
- Ataei, J.; Bach, C.; Javan, A.; Vögeli, T.-A.; Grafe, C.; Rahnama’i, M.S. The Scientific Value of Abstracts on Prostate Cancer Presented at the European Association of Urology Congresses. Front. Surg. 2021, 8, 683359. [Google Scholar] [CrossRef] [PubMed]
- Beyar-Katz, O.; Rowe, J.M.; Townsend, L.E.; Tallman, M.S.; Hadomi, R.; Horowitz, N.A. Published Abstracts at International Meetings Often Over-or Underestimate the Initial Response Rate. Blood J. Am. Soc. Hematol. 2017, 129, 2326–2328. [Google Scholar] [CrossRef]
- Nascimento, D.P.; Ostelo, R.W.; van Tulder, M.W.; Gonzalez, G.Z.; Araujo, A.C.; Vanin, A.A.; Costa, L.O. Do Not Make Clinical Decisions Based on Abstracts of Healthcare Research: A Systematic Review. J. Clin. Epidemiol. 2021, 135, 136–157. [Google Scholar] [CrossRef] [PubMed]
- Neymeyer, J.; Moldovan, D.E.; Miller, K.; Weinberger, S. Female Urology: Review of the Development in the Past 5 Decades. Aktuelle Urol. 2019, 50, 39–55. [Google Scholar] [PubMed]
- Colaco, M.; Svider, P.F.; Mauro, K.M.; Eloy, J.A.; Jackson-Rosario, I. Is There a Relationship between National Institutes of Health Funding and Research Impact on Academic Urology? J. Urol. 2013, 190, 999–1003. [Google Scholar] [CrossRef]
- Silvestre, J.; Agarwal, D.; Lee, D.I. Analysis of National Institutes of Health Funding to Departments of Urology. Urology 2016, 91, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Madjar, S.; Evans, D.; Duncan, R.C.; Gousse, A.E. Collaboration and Practice Patterns among Urologists and Gynecologists in the Treatment of Urinary Incontinence and Pelvic Floor Prolapse: A Survey of the International Continence Society Members. Neurourol. Urodyn. 2001, 20, 3–11. [Google Scholar] [CrossRef]
- Pereira, G.M.V.; Driusso, P.; Ferreira, C.H.J.; Brito, L.G.O. Multidisciplinary Approach between Physicians and Physiotherapists in Urogynecology: How Can We Make It Stronger? Int. Urogynecol. J. 2020, 31, 2187–2188. [Google Scholar] [CrossRef]
- Sungur, U.; Polat, H.; Yılmaz, H.; Güner, E. Multidisciplinary Collaborative Operations of Urology and Other Surgical Specialties: Thirteen Years of Experience at a Single Center. J. Urol. Surg. 2022, 9, 253–259. [Google Scholar] [CrossRef]
- Di Mattina, J.W.; Pronovost, P.J.; Holzmueller, C.G. Transdisciplinary Teams Spur Innovation for Patient Safety and Quality Improvement. Qual. Manag. Healthc. 2017, 26, 124–125. [Google Scholar] [CrossRef] [PubMed]
- Fox-Wasylyshyn, S.M.; Oldfield, P.; Muscedere, J.; El-Masri, M.M. Enhancing Health-Care Research: An Interdisciplinary Collaborative Approach. Can. J. Nurs. Res. Arch. 2005, 37, 34–46. [Google Scholar]
- Lewin, J.S. Interdisciplinary Teams and the Road to Discovery. Radiology 2010, 254, 26–30. [Google Scholar] [CrossRef]
| 2015 | 2016 | 2017 | 2018 | 2019 | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EAU | ICS | EAU | ICS | EAU | ICS | EAU | ICS | EAU | ICS | EAU | ICS | |
| FU-related abstracts, N | 88 | 142 | 100 | 150 | 113 | 159 | 117 | 136 | 128 | 135 | 546 | 722 |
| Abstracts published as full-text paper n (%) | 61 (69) | 88 (62) | 56 (56) | 81 (54) | 64 (57) | 90 (57) | 51 (44) | 73 (54) | 56 (44) | 79 (59) | 288 (53) | 411 (57) |
| Score | 0 | 1 | 2 | 3 |
|---|---|---|---|---|
| EAU (n = 288) | 108 (38%) | 73 (25%) | 59 (20%) | 48 (17%) |
| ICS (n = 411) | 201 (49%) | 80 (19%) | 62 (15%) | 68 (17%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kozan, S.; Rahnamai, M.S.; Ataei, J.; Dombrowski, J.; Najjari, L. Disciplinary Imbalances in Urology and Gynecology Research Publications within Functional Urology. Clin. Pract. 2024, 14, 1744-1752. https://doi.org/10.3390/clinpract14050139
Kozan S, Rahnamai MS, Ataei J, Dombrowski J, Najjari L. Disciplinary Imbalances in Urology and Gynecology Research Publications within Functional Urology. Clinics and Practice. 2024; 14(5):1744-1752. https://doi.org/10.3390/clinpract14050139
Chicago/Turabian StyleKozan, Sümeyye, Mohammad Sajjad Rahnamai, Jasmin Ataei, Janina Dombrowski, and Laila Najjari. 2024. "Disciplinary Imbalances in Urology and Gynecology Research Publications within Functional Urology" Clinics and Practice 14, no. 5: 1744-1752. https://doi.org/10.3390/clinpract14050139
APA StyleKozan, S., Rahnamai, M. S., Ataei, J., Dombrowski, J., & Najjari, L. (2024). Disciplinary Imbalances in Urology and Gynecology Research Publications within Functional Urology. Clinics and Practice, 14(5), 1744-1752. https://doi.org/10.3390/clinpract14050139







