Smoking and Hypertriglyceridemia Predict ST-Segment Elevation Myocardial Infarction in Kosovo Patients with Acute Myocardial Infarction
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
3.1. General Data of Patients with AMI
3.2. Patients with STEMI Versus NSTEMI
3.3. Risk Factors and Predictors of STEMI
3.4. Age and Gender in Patients with Acute AMI
Comparison between Acute MI Patients in Kosovo and Northern and Southern Europe
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ralapanawa, U.; Sivakanesan, R. Epidemiology and the Magnitude of Coronary Artery Disease and Acute Coronary Syndrome: A Narrative Review. J. Epidemiol. Glob. Health 2021, 11, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Dawson, L.P.; Lum, M.; Nerleker, N.; Nicholls, S.J.; Layland, J. Coronary Atherosclerotic Plaque Regression: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2022, 79, 66–82. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Mortality Collaborators. Global, regional, and national age-sex-specific mortality and life expectancy, 1950–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1684–1735. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.B.; Hashim, M.J.; Mustafa, H.; Baniyas, M.Y.; Khalid, S.; Suwaidi, B.M.A.; AlKatheer, R.; Alblooshi, F.M.K.; Ali, M.E.; Almatrooshi, H.; et al. Global Epidemiology of Ischemic Heart Disease: Results from the Global Burden of Disease Study. Cureus 2020, 12, e9349. [Google Scholar] [CrossRef] [PubMed]
- Timmis, A.; Vardas, P.; Townsend, N.; Torbica, A.; Katus, H.; De Smedt, D.; Gale, C.P.; Maggioni, A.P.; Petersen, S.E.; Atlas Writing Group; et al. European Society of Cardiology: Cardiovascular disease statistics 2021. Eur. Heart J. 2022, 43, 716–799. [Google Scholar] [CrossRef] [PubMed]
- Nowbar, A.N.; Gitto, M.; Howard, J.P.; Francis, D.P.; Al-Lamee, R. Mortality from Ischemic Heart Disease. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005375. [Google Scholar] [CrossRef] [PubMed]
- Beza, L.; Leslie, S.L.; Alemayehu, B.; Gary, R. Acute coronary syndrome treatment delay in low to middle-income countries: A systematic review. Int. J. Cardiol. Heart Vasc. 2021, 35, 100823. [Google Scholar] [CrossRef] [PubMed]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update from the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Zeymer, U.; Ludman, P.; Danchin, N.; Kala, P.; Laroche, C.; Sadeghi, M.; Caporale, R.; Shaheen, S.M.; Legutko, J.; Iakobsishvili, Z.; et al. Reperfusion therapies and in-hospital outcomes for ST-elevation myocardial infarction in Europe: The ACVC-EAPCI EORP STEMI Registry of the European Society of Cardiology. Eur. Heart J. 2021, 42, 4536–4549. [Google Scholar] [CrossRef]
- Poloński, L.; Gasior, M.; Gierlotka, M.; Kalarus, Z.; Cieśliński, A.; Dubiel, J.S.; Gil, R.J.; Ruzyłło, W.; Trusz-Gluza, M.; Zembala, M.; et al. Polish Registry of Acute Coronary Syndromes (PL-ACS). Characteristics, treatments and outcomes of patients with acute coronary syndromes in Poland. Kardiol. Pol. 2007, 65, 861–872. [Google Scholar]
- Sidhu, N.S.; Rangaiah, S.K.K.; Ramesh, D.; Veerappa, K.; Manjunath, C.N. Clinical Characteristics, Management Strategies, and In-Hospital Outcomes of Acute Coronary Syndrome in a Low Socioeconomic Status Cohort: An Observational Study From Urban India. Clin. Med. Insights Cardiol. 2020, 14, 1179546820918897. [Google Scholar] [CrossRef] [PubMed]
- Caughey, M.C.; Arora, S.; Qamar, A.; Chunawala, Z.; Gupta, M.D.; Gupta, P.; Vaduganathan, M.; Pandey, A.; Dai, X.; Smith, S.C.; et al. Trends, Management, and Outcomes of Acute Myocardial Infarction Hospitalizations With In-Hospital-Onset Versus Out-of-Hospital Onset: The ARIC Study. J. Am. Heart Assoc. 2021, 10, e018414. [Google Scholar] [CrossRef] [PubMed]
- Ederhy, S.; Cohen, A.; Boccara, F.; Puymirat, E.; Aissaoui, N.; Elbaz, M.B.; Bonnefoy-Cudraz, E.; Druelles, P.; Andrieu, S.; FAST-MI Investigators; et al. In-hospital outcomes and 5-year mortality following an acute myocardial infarction in patients with a history of cancer: Results from the French registry on Acute ST-elevation or non-ST-elevation myocardial infarction (FAST-MI) 2005 cohort. Arch. Cardiovasc. Dis. 2019, 112, 657–669. [Google Scholar] [CrossRef] [PubMed]
- Sanchis Gomar, F.; Perez Quilis, C.; Leischik, R.; Lucia, A. Epidemiology of coronary heart disease and acute coronary syndrome. Ann. Transl. Med. 2016, 4, 256. [Google Scholar] [CrossRef] [PubMed]
- Ferreira-González, I. The epidemiology of coronary heart disease. Rev. Esp. Cardiol. (Engl. Ed.) 2014, 67, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, A.; Lamichhane, P.; Eghbali, M.; Xavier, R.; Cook, D.E.; Elsherbiny, R.M.; Jhajj, L.K.; Khanal, R. Risk factors, lab parameters, angiographic characteristics and outcomes of coronary artery disease in young South Asian patients: A systematic review. J. Int. Med. Res. 2023, 51, 3000605231187806. [Google Scholar] [CrossRef] [PubMed]
- Okrainec, K.; Banerjee, D.K.; Eisenberg, M.J. Coronary artery disease in the developing world. Am. Heart J. 2004, 148, 7–15. [Google Scholar] [CrossRef]
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef]
- Ludman, P.; Zeymer, U.; Danchin, N.; Kala, P.; Laroche, C.; Sadeghi, M.; Caporale, R.; Shaheen, S.M.; Legutko, J.; Iakobishvili, Z.; et al. Care of patients with ST-elevation myocardial infarction: An international analysis of quality indicators in the acute coronary syndrome STEMI Registry of the EURObservational Research Programme and ACVC and EAPCI Associations of the European Society of Cardiology in 11 462 patients. Eur. Heart J. Acute Cardiovasc. Care 2023, 12, 22–37. [Google Scholar]
- McManus, D.D.; Gore, J.; Yarzebski, J.; Spencer, F.; Lessard, D.; Goldberg, R.J. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am. J. Med. 2011, 124, 40–47. [Google Scholar] [CrossRef]
- Meyers, H.P.; Bracey, A.; Lee, D.; Lichtenheld, A.; Li, W.J.; Singer, D.D.; Kane, J.A.; Dodd, K.W.; MEn, K.E.M.; Thode, H.C.; et al. Comparison of the ST-Elevation Myocardial Infarction (STEMI) vs. NSTEMI and Occlusion MI (OMI) vs. NOMI Paradigms of Acute MI. J. Emerg. Med. 2021, 60, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Rogers, W.J.; Frederick, P.D.; Stoehr, E.; Canto, J.G.; Ornato, J.P.; Gibson, C.M.; Pollack, C.V., Jr.; Gore, J.M.; Chandra-Strobos, N.; Peterson, E.D.; et al. Trends in presenting characteristics and hospital mortality among patients with ST elevation and non-ST elevation myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am. Heart J. 2008, 156, 1026–1034. [Google Scholar] [CrossRef] [PubMed]
- Bajraktari, G.; Thaqi, K.; Pacolli, S.; Gjoka, S.; Rexhepaj, N.; Daullxhiu, I.; Sylejmani, X.; Elezi, S. In-hospital mortality following acute myocardial infarction in Kosovo: A single center study. Ann. Saudi Med. 2008, 28, 430–434. [Google Scholar] [PubMed]
- André, R.; Bongard, V.; Elosua, R.; Kirchberger, I.; Farmakis, D.; Häkkinen, U.; Fusco, D.; Torre, M.; Garel, P.; Araújo, G.; et al. International differences in acute coronary syndrome patients’ baseline characteristics, clinical management and outcomes in Western Europe: The EURHOBOP study. Heart 2014, 100, 1201–1207. [Google Scholar] [CrossRef] [PubMed]
- Bradley, M.S.; Borgerding, J.A.; Wood, G.B.; Maynard, C.; Fihn, S.D. Incidence, Risk Factors, and Outcomes Associated with In-Hospital Acute Myocardial Infarction. JAMA Netw. Open 2019, 2, e187348. [Google Scholar] [CrossRef] [PubMed]
- Bahall, M.; Seemungal, T.; Legall, G. Risk factors for first-time acute myocardial infarction patients in Trinidad. BMC Public Health 2018, 18, 161. [Google Scholar] [CrossRef]
- Nicoll, R.; Wiklund, U.; Zhao, Y.; Diederichsen, A.; Mickley, H.; Ovrehus, K.; Zamorano, J.; Gueret, P.; Schmermund, A.; Maffei, E.; et al. Gender and age effects on risk factor-based prediction of coronary artery calcium in symptomatic patients: A Euro-CCAD study. Atherosclerosis 2016, 252, 32–39. [Google Scholar] [CrossRef]
- Price, J.F.; Mowbray, P.I.; Lee, A.J.; Rumley, A.; Lowe, G.D.; Fowkes, F.G. Relationship between smoking and cardiovascular risk factors in the development of peripheral arterial disease and coronary artery disease: Edinburgh artery study. Eur. Heart J. 1999, 20, 344–353. [Google Scholar] [CrossRef]
- Larsson, S.C.; Carter, P.; Kar, S.; Vithayathil, M.; Mason, A.M.; Michaëlsson, K.; Burgess, S. Smoking, alcohol consumption, and cancer: A mendelian randomisation study in UK Biobank and international genetic consortia participants. PLoS Med. 2020, 17, e1003178. [Google Scholar] [CrossRef]
- Farnier, M.; Zeller, M.; Masson, D.; Cottin, Y. Triglycerides and risk of atherosclerotic cardiovascular disease: An update. Arch. Cardiovasc. Dis. 2021, 114, 132–139. [Google Scholar] [CrossRef]
- Prakash, V.; Jaker, S.; Burgan, A.; Jacques, A.; Fluck, D.; Sharma, P.; Fry, C.H.; Han, T.S. The smoking-dyslipidaemia dyad: A potent synergistic risk for atherosclerotic coronary artery disease. JRSM Cardiovasc. Dis. 2021, 10, 2048004020980945. [Google Scholar] [CrossRef] [PubMed]
- Song, W.; Guan, J.; He, P.; Fan, S.; Zhi, H.; Wang, L. Mediating effects of lipids on the association between smoking and coronary artery disease risk among Chinese. Lipids Health Dis. 2020, 19, 149. [Google Scholar] [CrossRef] [PubMed]
- Banach, M.; Lewek, J.; Surma, S.; Penson, P.E.; Sahebkar, A.; Martin, S.S.; Bajraktari, G.; Henein, M.Y.; Reiner, Ž.; Bielecka-Dąbrowa, A.; et al. The association between daily step count and all-cause and cardiovascular mortality: A meta-analysis. Eur. J. Prev. Cardiol. 2023, 30, 1975–1985. [Google Scholar] [CrossRef]
- Delabays, B.; de La Harpe, R.; Vollenweider, P.; Fournier, S.; Müller, O.; Strambo, D.; Graham, I.; Visseren, F.L.J.; Nanchen, D.; Marques-Vidal, P.; et al. Comparison of the European and US guidelines for lipid-lowering therapy in primary prevention of cardiovascular disease. Eur. J. Prev. Cardiol. 2023, 30, 1856–1864. [Google Scholar] [CrossRef] [PubMed]
- Wong, N.D.; Budoff, M.J.; Ferdinand, K.; Graham, I.M.; Michos, E.D.; Reddy, T.; Shapiro, M.D.; Toth, P.P. Atherosclerotic cardiovascular disease risk assessment: An American Society for Preventive Cardiology clinical practice statement. Am. J. Prev. Cardiol. 2022, 10, 100335. [Google Scholar] [CrossRef]
- Masrouri, S.; Tamehri Zadeh, S.S.; Shapiro, M.D.; Khalili, D.; Hadaegh, F. Impact of optimal cholesterol levels on subclinical atherosclerosis in the absence of risk factors in young adults. Atherosclerosis 2024, 393, 117520. [Google Scholar] [CrossRef]



| Variable | All Included Patients | Patients with NSTEMI | Patients with STEMI | p-Value |
|---|---|---|---|---|
| (n = 7353) | (n = 2987) | (n = 4366) | ||
| Age (years) | 63 ± 12 | 63 ± 11 | 64 ± 12 | 0.077 |
| Female (%) | 28.7 | 31.7 | 26.6 | ˂0.001 |
| Smoking (%) | 51.7 | 48.3 | 54 | ˂0.001 |
| Diabetes (%) | 35.3 | 37.8 | 33.6 | ˂0.001 |
| Hypercholesterolemia (%) | 40.1 | 39.4 | 40.1 | 0.099 |
| Arterial hypertension (%) | 65.6 | 69.6 | 63 | <0.001 |
| Family history of CAD (%) | 38.1 | 39.9 | 36.9 | 0.009 |
| Atrial fibrillation (%) | 4.4 | 3.9 | 5.0 | 0.036 |
| Left bundle branch block (%) | 3.7 | 2.6 | 5.3 | <0.001 |
| Cardiogenic shock (%) | 3.7 | 2.1 | 4.9 | <0.001 |
| Fasting glucose (mmol/L) | 9.5 ± 5.5 | 9.2 ± 5 | 9.8 ± 6 | <0.001 |
| Total cholesterol (mmol/L) | 4.8 ± 1.6 | 4.8 ± 1.6 | 4.5 ± 1.5 | 0.939 |
| Triglycerides (mmol/L) | 1.9 ± 1.3 | 2.0 ± 1.3 | 1.88 ± 1.2 | 0.001 |
| Creatinine (μmol/L) | 118 ± 74 | 118 ± 74 | 117 ± 73 | 0.632 |
| Urea (mg/dL) | 9.2 ± 6 | 9.2 ± 6 | 9.1 ± 6 | 0.652 |
| Hemoglobin (g/dL) | 13.7 ± 3.2 | 13.7 ± 3.4 | 13.7 ± 3 | 0.942 |
| Heart rate at admission (beats/min) | 82.6 ± 23 | 82.5 ± 26 | 82.6 ± 20 | 0.822 |
| Left ventricular ejection fraction (%) | 50.6 ± 9 | 51.6 ± 9 | 49.8 ± 9 | <0.001 |
| Variable | All Included Patients | Patients with NSTEMI | Patients with STEMI | p-Value |
|---|---|---|---|---|
| (n = 7353) | (n = 2987) | (n = 4366) | ||
| Coronary Angiography (%) | 67.3 | 66.8 | 67.8 | 0.396 |
| Primary Percutaneous Intervention (%) | 50.1 | 43.6 | 55.2 | <0.001 |
| Univariate Associates | Multivariate Associates | |||||
|---|---|---|---|---|---|---|
| Variable | OR | (CI 95%) | p-Value | OR | (CI 95%) | p-Value |
| Age | 0.993 | (0.989–1.997) | 0.001 | |||
| Female gender | 0.782 | (0.706–0.876) | <0.001 | |||
| Smoking | 0.796 | (0.725–0.874) | <0.001 | 0.783 | (0.685–0.895) | <0.001 |
| Diabetes | 1.202 | (1.090–1.324) | <0.001 | |||
| Arterial hypertension | 1.347 | (1.220–1.488) | <0.001 | |||
| Family anamnesis for CAD | 1.135 | (1.032–1.249) | 0.009 | |||
| Triglycerides | 0.943 | (0.901–0.987) | 0.012 | 0.946 | (0.902–0.991) | 0.020 |
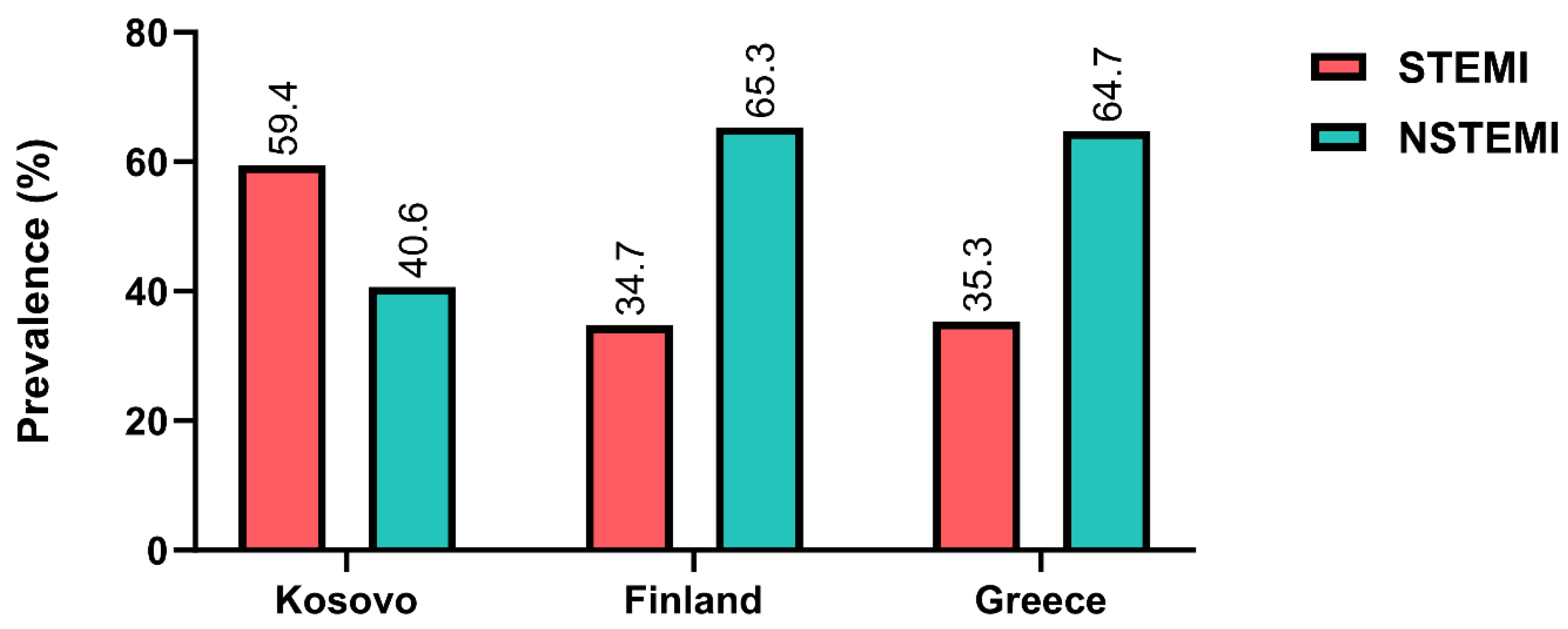
| Variable | Kosovo | Finland | Kosovo | Greece | ||
|---|---|---|---|---|---|---|
| (n = 7353) | (n = 1813) | p-Value | (n = 7353) | (n = 1185) | p-Value | |
| Age (years) Female (%) | 63 ± 12 28.7 | 71 ± 13 34.6 | <0.000 <0.001 | 63 ± 12 28.7 | 67 ± 13 26.2 | <0.001 <0.001 |
| Smoking (%) Diabetes (%) | 51.7 35.3 | 20.4 24.8 | <0.001 <0.001 | 51.7 35.3 | 41.4 27.6 | <0.001 <0.001 |
| Arterial hypertension (%) STEMI (%) | 65.6 59.4 | 53.4 34.7 | <0.001 <0.001 | 65.6 59.4 | 52.6 35.3 | <0.001 <0.001 |
| NSTEMI (%) | 40.6 | 65.3 | <0.001 | 40.6 | 64.7 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poniku, A.; Batalli, A.; Shita, D.; Rexhaj, Z.; Ferati, A.; Leka, R.; Bajraktari, A.; Abdyli, G.; Haliti, E.; Ibrahimi, P.; et al. Smoking and Hypertriglyceridemia Predict ST-Segment Elevation Myocardial Infarction in Kosovo Patients with Acute Myocardial Infarction. Clin. Pract. 2024, 14, 1149-1158. https://doi.org/10.3390/clinpract14030091
Poniku A, Batalli A, Shita D, Rexhaj Z, Ferati A, Leka R, Bajraktari A, Abdyli G, Haliti E, Ibrahimi P, et al. Smoking and Hypertriglyceridemia Predict ST-Segment Elevation Myocardial Infarction in Kosovo Patients with Acute Myocardial Infarction. Clinics and Practice. 2024; 14(3):1149-1158. https://doi.org/10.3390/clinpract14030091
Chicago/Turabian StylePoniku, Afrim, Arlind Batalli, Dua Shita, Zarife Rexhaj, Arlind Ferati, Rita Leka, Artan Bajraktari, Genc Abdyli, Edmond Haliti, Pranvera Ibrahimi, and et al. 2024. "Smoking and Hypertriglyceridemia Predict ST-Segment Elevation Myocardial Infarction in Kosovo Patients with Acute Myocardial Infarction" Clinics and Practice 14, no. 3: 1149-1158. https://doi.org/10.3390/clinpract14030091
APA StylePoniku, A., Batalli, A., Shita, D., Rexhaj, Z., Ferati, A., Leka, R., Bajraktari, A., Abdyli, G., Haliti, E., Ibrahimi, P., Karahoda, R., Elezi, S., Shatri, F., Bytyçi, I., Henein, M., & Bajraktari, G. (2024). Smoking and Hypertriglyceridemia Predict ST-Segment Elevation Myocardial Infarction in Kosovo Patients with Acute Myocardial Infarction. Clinics and Practice, 14(3), 1149-1158. https://doi.org/10.3390/clinpract14030091








