Full Familiarisation Is Not Required for the Self-Paced 1 km Treadmill Walk to Predict Peak Oxygen Uptake in Phase IV Cardiac Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Ethical Approval
2.2. Experimental Visits
2.3. Statistical Analysis
3. Results
3.1. Baseline Observations at Rest
3.2. Walking Observations: Self-Selected Walking Speed and Walking Time
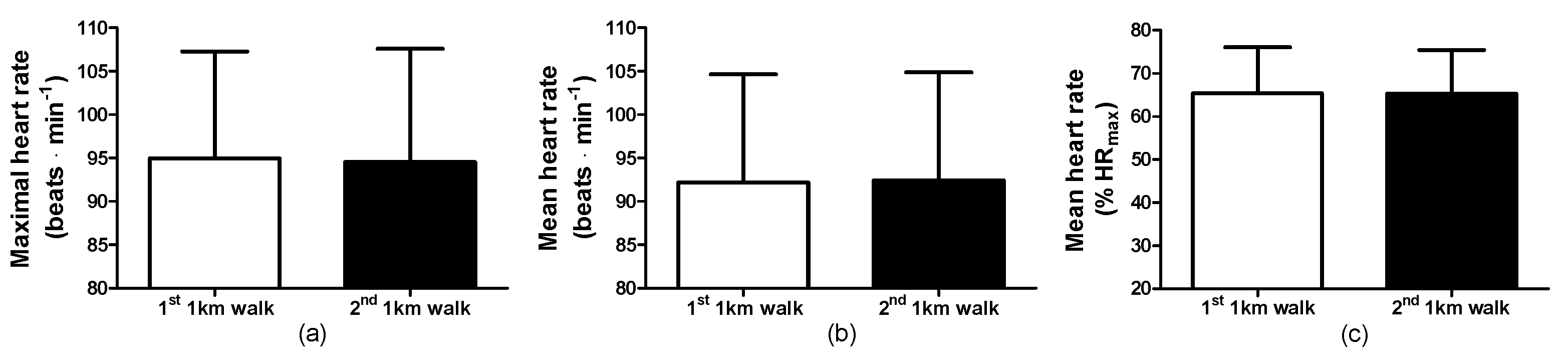
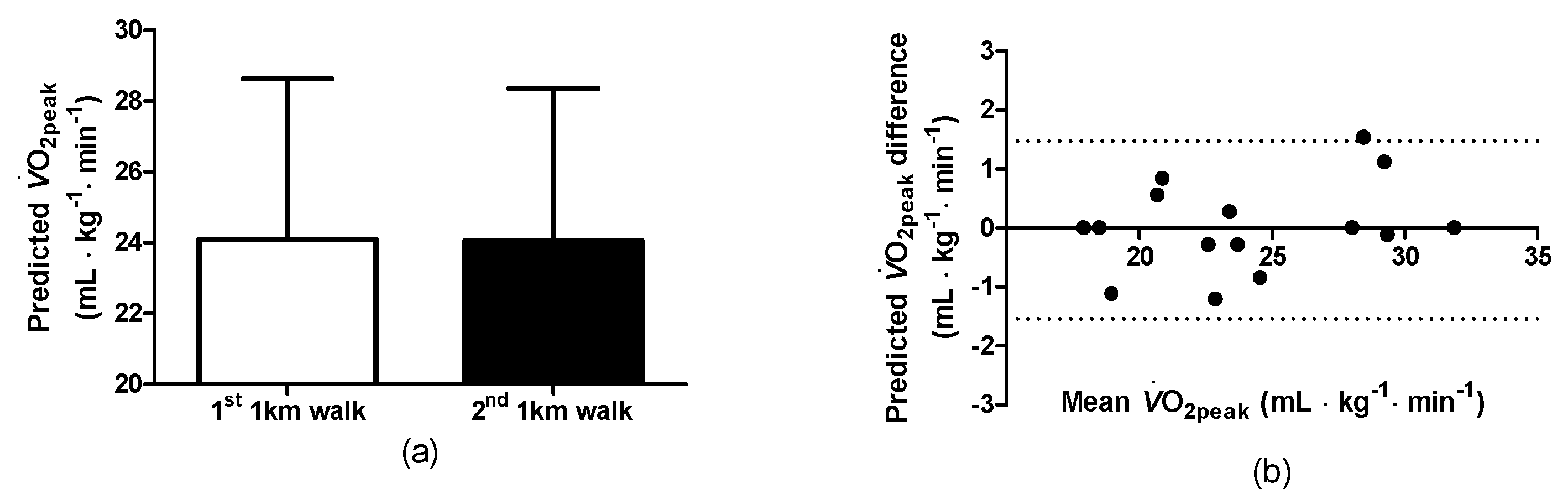
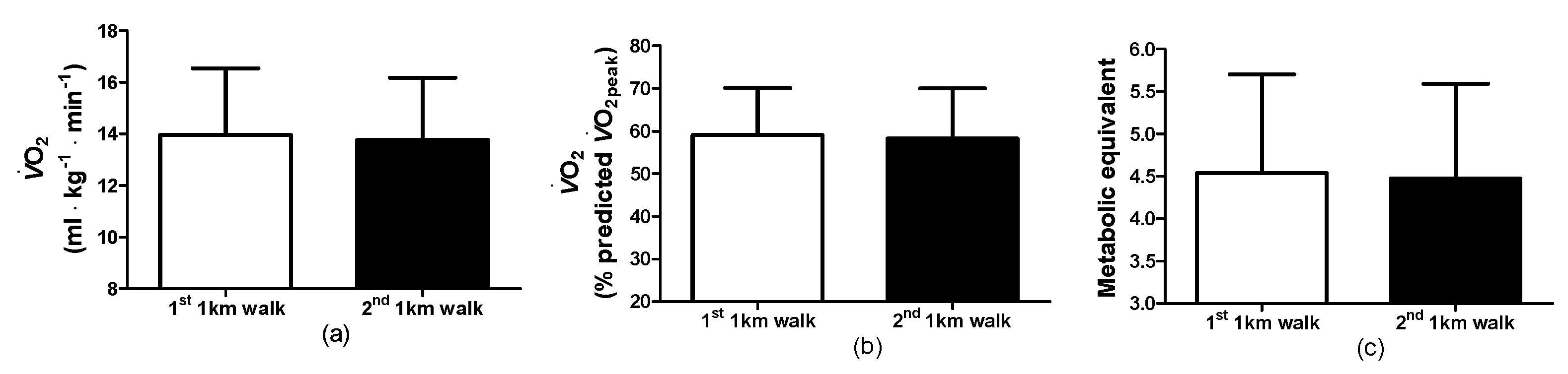
3.3. Walking Observations: Physiological and Cardiovascular Responses
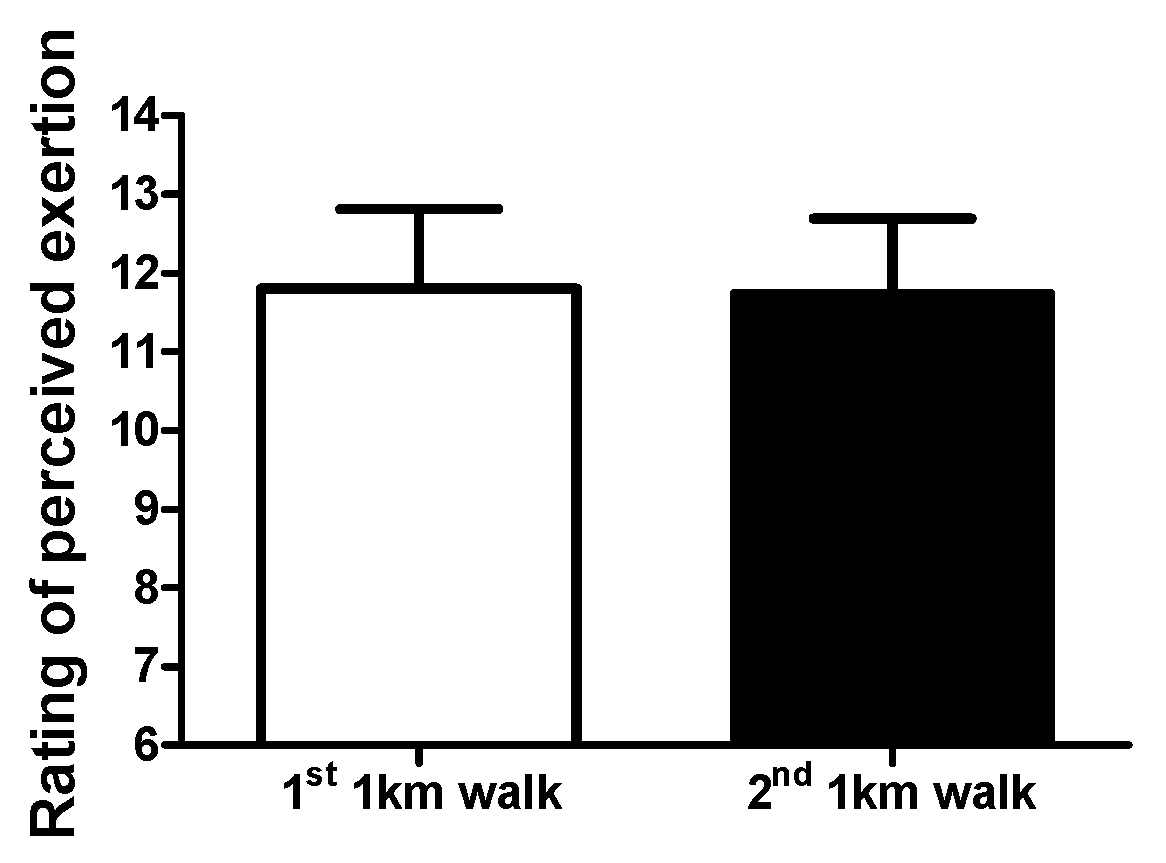
3.4. Walking Observations: Rating of Perceived Exertion
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jones, J.; Furze, G.; Buckley, J. Cardiovascular Disease Prevention and Rehabilitation. In Cardiovascular Prevention and Rehabilitation in Practice, 2nd ed.; Jones, J., Furze, G., Buckley, J., Sheppard, G., Eds.; John Wiley & Sons Ltd.: Hoboken, NJ, USA, 2020; pp. 1–19. [Google Scholar]
- National Audit of Cardiac Rehabilitation. Annual Statistical Report 2017. Available online: https://www.bhf.org.uk/ (accessed on 6 December 2016).
- Heran, B.S.; Chen, J.M.; Ebrahim, S.; Moxham, T.; Oldridge, N.; Rees, K.; Thompson, D.R.; Taylor, R.S. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst. Rev. 2011, 7, CD001800. [Google Scholar] [CrossRef]
- Dibben, G.; Faulkner, J.; Oldridge, N.; Rees, K.; Thompson, D.R.; Zwisler, A.; Taylor, R.S. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst. Rev. 2021, 11, CD001800. [Google Scholar] [CrossRef]
- Lim, C.; Dunford, E.C.; Valentino, S.E.; Oikawa, S.Y.; McGlory, C.; Baker, S.K.; Macdonald, M.J.; Phillips, S.M. Both Traditional and Stair Climbing-based HIIT Cardiac Rehabilitation Induce Beneficial Muscle Adaptations. Med. Sci. Sports Exerc. 2021, 53, 1114–1124. [Google Scholar] [CrossRef] [PubMed]
- Dunford, E.C.; Valentino, S.E.; Dubberley, J.; Oikawa, S.Y.; McGlory, C.; Lonn, E.; Jung, M.E.; Gibala, M.J.; Phillips, S.M.; MacDonald, M.J. Brief Vigorous Stair Climbing Effectively Improves Cardiorespiratory Fitness in Patients with Coronary Artery Disease: A Randomized Trial. Front. Sports Act. Living 2021, 3, 630912. [Google Scholar] [CrossRef] [PubMed]
- Ross, R.; Blair, S.N.; Arena, R.; Church, T.S.; Després, J.P.; Franklin, B.A.; Haskell, W.L.; Kaminsky, L.A.; Levine, B.D.; Lavie, C.J.; et al. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement from the American Heart Association. Circulation 2016, 134, e653–e699. [Google Scholar] [CrossRef] [PubMed]
- Wenger, H.A.; Bell, G.J. The interactions of intensity, frequency and duration of exercise training in altering cardiorespiratory fitness. Sports Med. 1986, 3, 346–356. [Google Scholar] [CrossRef]
- Bruce, R.A.; Kusumi, F.; Hosmer, D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am. Heart J. 1973, 85, 546–562. [Google Scholar] [CrossRef]
- Chiaranda, G.; Myers, J.; Mazzoni, G.; Terranova, F.; Bernardi, E.; Grossi, G.; Codecà, L.; Conconi, F.; Grazzi, G. Peak oxygen uptake prediction from a moderate, perceptually regulated, 1-km treadmill walk in male cardiac patients. J. Cardiopulm. Rehabil. Prev. 2012, 32, 262–269. [Google Scholar] [CrossRef]
- Weber, K.T.; Kinasewitz, G.T.; Janicki, J.S.; Fishman, A.P. Oxygen utilization and ventilation during exercise in patients with chronic cardiac failure. Circulation 1982, 65, 1213–1223. [Google Scholar] [CrossRef]
- Wass, E.; Taylor, N.F.; Matsas, A. Familiarisation to treadmill walking in unimpaired older people. Gait Posture 2005, 21, 72–79. [Google Scholar] [CrossRef]
- Franklin, B.A.; Eijsvogels, T.M.H.; Pandey, A.; Quindry, J.; Toth, P.P. Physical activity, cardiorespiratory fitness, and cardiovascular health: A clinical practice statement of the American Society for Preventive Cardiology Part II: Physical activity, cardiorespiratory fitness, minimum and goal intensities for exercise training, prescriptive methods, and special patient populations. Am. J. Prev. Cardiol. 2022, 12, 100425. [Google Scholar] [CrossRef]
- Franklin, B.A.; Eijsvogels, T.M.H.; Pandey, A.; Quindry, J.; Toth, P.P. Physical activity, cardiorespiratory fitness, and cardiovascular health: A clinical practice statement of the ASPC Part I: Bioenergetics, contemporary physical activity recommendations, benefits, risks, extreme exercise regimens, potential maladaptations. Am. J. Prev. Cardiol. 2022, 12, 100424. [Google Scholar] [CrossRef]
- Spelman, C.C.; Pate, R.R.; Macera, C.A.; Ward, D.S. Self-selected exercise intensity of habitual walkers. Med. Sci. Sports Exerc. 1993, 25, 1174–1179. [Google Scholar] [CrossRef] [PubMed]
- Pintar, J.A.; Robertson, R.J.; Kriska, A.M.; Nagle, E.; Goss, F.L. The influence of fitness and body weight on preferred exercise intensity. Med. Sci. Sports Exerc. 2006, 38, 981–988. [Google Scholar] [CrossRef]
- Dishman, R.K.; Farquhar, R.P.; Cureton, K.J. Responses to preferred intensities of exertion in men differing in activity levels. Med. Sci. Sports Exerc. 1994, 26, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Kravitz, L.; Robergs, R.A.; Heyward, V.H.; Wagner, D.R.; Powers, K. Exercise mode and gender comparisons of energy expenditure at self-selected intensities. Med. Sci. Sports Exerc. 1997, 29, 1028–1035. [Google Scholar] [CrossRef] [PubMed]
- Kanegusuku, H.; Cucato, G.G.; Longano, P.; Okamoto, E.; Piemonte, M.E.P.; Correia, M.A.; Ritti-Dias, R.M. Acute Cardiovascular Responses to Self-selected Intensity Exercise in Parkinson’s Disease. Int. J. Sports Med. 2022, 43, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Barros, T.A.R.; do Prado, W.L.; Tenório, T.R.S.; Ritti-Dias, R.M.; Germano-Soares, A.H.; Balagopal, B.P.; Hill, J.O.; Freitas-Dias, R. Cardiovascular Effects of Aerobic Exercise with Self-Selected or Predetermined Intensity in Adolescents with Obesity. Pediatr. Exerc. Sci. 2021, 33, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Costa, I.B.B.; Schwade, D.; Macêdo, G.A.D.; Browne, R.A.V.; Farias-Junior, L.F.; Freire, Y.A.; Sócrates, J.; Boreskie, K.F.; Duhamel, T.A.; Caldas Costa, E. Acute antihypertensive effect of self-selected exercise intensity in older women with hypertension: A crossover trial. Clin. Interv. Aging 2019, 14, 1407–1418. [Google Scholar] [CrossRef] [PubMed]
- Bethell, H.J.N. Exercise-based cardiac rehabilitation. Medicine 2006, 34, 195–196. [Google Scholar] [CrossRef]
- Gordon, N.F.; Duncan, J.J. Effect of beta-blockers on exercise physiology: Implications for exercise training. Med. Sci. Sports Exerc. 1991, 23, 668–676. [Google Scholar] [CrossRef]
- Resnick, B.; Jenkins, L.S. Testing the reliability and validity of the Self-Efficacy for Exercise scale. Nurs. Res. 2000, 49, 154–159. [Google Scholar] [CrossRef]
- McInnis, K.J.; Balady, G.J. Comparison of submaximal exercise responses using the Bruce vs modified Bruce protocols. Med. Sci. Sports Exerc. 1994, 26, 103–107. [Google Scholar] [CrossRef]
- Byrne, N.M.; Hills, A.P.; Hunter, G.R.; Weinsier, R.L.; Schutz, Y. Metabolic equivalent: One size does not fit all. J. Appl. Physiol. 2005, 99, 1112–1119. [Google Scholar] [CrossRef]
- Gault, M.L.; Clements, R.E.; Willems, M.E.T. Functional mobility of older adults after concentric and eccentric endurance exercise. Eur. J. Appl. Physiol. 2012, 112, 3699–3707. [Google Scholar] [CrossRef]
- Rossignol, S.; Dubuc, R.; Gossard, J.P. Dynamic sensorimotor interactions in locomotion. Physiol. Rev. 2006, 86, 89–154. [Google Scholar] [CrossRef] [PubMed]
- Van de Putte, M.; Hagemeister, N.; St-Onge, N.; Parent, G.; de Guise, J.A. Habituation to treadmill walking. Biomed. Mater. Eng. 2006, 16, 43–52. [Google Scholar] [PubMed]
- Meyer, C.; Killeen, T.; Easthope, C.S.; Curt, A.; Bolliger, M.; Linnebank, M.; Zörner, B.; Filli, L. Familiarization with treadmill walking: How much is enough? Sci. Rep. 2019, 9, 5232. [Google Scholar] [CrossRef] [PubMed]
- Malatesta, D.; Canepa, M.; Menendez Fernandez, A. The effect of treadmill and overground walking on preferred walking speed and gait kinematics in healthy, physically active older adults. Eur. J. Appl. Physiol. 2017, 117, 1833–1843. [Google Scholar] [CrossRef] [PubMed]
- Faulkner, J.; Gerhard, J.; Stoner, L.; Lambrick, D. Self-Paced Walking within a Diverse Topographical Environment Elicits an Appropriate Training Stimulus for Cardiac Rehabilitation Patients. Rehabil. Res. Pract. 2012, 2012, 140871. [Google Scholar] [CrossRef] [PubMed]
- Grazzi, G.; Mazzoni, G.; Myers, J.; Codecà, L.; Pasanisi, G.; Mandini, S.; Piepoli, M.; Volpato, S.; Conconi, F.; Chiaranda, G. Determining the best percent-predicted equation for estimated VO2 peak by a 1-km moderate perceptually-regulated treadmill walk to predict mortality in outpatients with cardiovascular disease. J. Sci. Med. Sport. 2018, 21, 307–311. [Google Scholar] [CrossRef]
- Chiaranda, G.; Myers, J.; Arena, R.; Kaminsky, L.; Sassone, B.; Pasanisi, G.; Mandini, S.; Mazzoni, G.; Grazzi, G. Prognostic comparison of the FRIEND and Wasserman/Hansen peak VO2 equations applied to a submaximal walking test in outpatients with cardiovascular disease. Eur. J. Prev. Cardiol. 2021, 28, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Raisi, A.; Bernardi, E.; Myers, J.; Piva, T.; Zerbini, V.; Massotti, S.; Menegatti, E.; Caruso, L.; Mazzoni, G.; Grazzi, G.; et al. Change in Peak Oxygen Uptake Predicted by the Moderate 1-km Treadmill Walking Test After Walking Training in Outpatients with Cardiovascular Disease. J. Cardiopulm. Rehabil. Prev. 2023, in press. [Google Scholar] [CrossRef] [PubMed]
- Raisi, A.; Piva, T.; Myers, J.; Lordi, R.; Zerbini, V.; Massotti, S.; Chiaranda, G.; Grazzi, G.; Mazzoni, G.; Mandini, S. A Moderate Walking Test Predicts Survival in Women with Cardiovascular Diseases. Am. J. Prev. Med. 2023, 65, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Zerbini, V.; Raisi, A.; Myers, J.; Piva, T.; Lordi, R.; Chiaranda, G.; Mazzoni, G.; Grazzi, G.; Mandini, S. Peak Oxygen Uptake Estimation From A Moderate 1-KM Treadmill Walk in Women with Cardiovascular Disease. J. Cardiopulm. Rehabil. Prev. 2021, 41, 432–434. [Google Scholar] [CrossRef] [PubMed]
- Savage, P.D.; Toth, M.J.; Ades, P.A. A re-examination of the metabolic equivalent concept in individuals with coronary heart disease. J. Cardiopulm. Rehabil. Prev. 2007, 27, 143–148. [Google Scholar] [CrossRef]
- Williams, P.T.; Thompson, P.D. Increased cardiovascular disease mortality associated with excessive exercise in heart attack survivors. Mayo Clin. Proc. 2014, 89, 1187–1194. [Google Scholar] [CrossRef]

| Cardiac Condition/Intervention | n |
|---|---|
| Myocardial infarction and percutaneous intervention | 6 |
| Angina and percutaneous intervention | 1 |
| Valve replacement surgery | 3 |
| Myocardial infarction and coronary artery bypass graph surgery | 3 |
| Pacemaker | 1 |
| Heart failure (class I/II) | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gault, M.L.; Willems, M.E.T. Full Familiarisation Is Not Required for the Self-Paced 1 km Treadmill Walk to Predict Peak Oxygen Uptake in Phase IV Cardiac Patients. Clin. Pract. 2024, 14, 327-336. https://doi.org/10.3390/clinpract14010025
Gault ML, Willems MET. Full Familiarisation Is Not Required for the Self-Paced 1 km Treadmill Walk to Predict Peak Oxygen Uptake in Phase IV Cardiac Patients. Clinics and Practice. 2024; 14(1):327-336. https://doi.org/10.3390/clinpract14010025
Chicago/Turabian StyleGault, Mandy L., and Mark E. T. Willems. 2024. "Full Familiarisation Is Not Required for the Self-Paced 1 km Treadmill Walk to Predict Peak Oxygen Uptake in Phase IV Cardiac Patients" Clinics and Practice 14, no. 1: 327-336. https://doi.org/10.3390/clinpract14010025
APA StyleGault, M. L., & Willems, M. E. T. (2024). Full Familiarisation Is Not Required for the Self-Paced 1 km Treadmill Walk to Predict Peak Oxygen Uptake in Phase IV Cardiac Patients. Clinics and Practice, 14(1), 327-336. https://doi.org/10.3390/clinpract14010025







