Abstract
The COVID-19 pandemic due to the SARS-CoV-2 coronavirus showed acute and prolonged effects on human health. In addition, over the past four years, there has been a tremendous surge in COVID-19-related scientific publications, as shown by bibliometric and scientometric studies. However, such analysis of the scientific literature is lacking in the area of male reproduction. The current scientometric study analyzes publication characteristics of articles related to male reproduction and COVID-19 infection. We used the Scopus database to analyze scientometric data (the number of publications, journals, countries, type of documents, and subject area) related to COVID-19 and male reproductive research. Our literature search identified 345 articles related to COVID-19 and male reproductive research. Most of the articles were published in the USA (n = 72), Italy (n = 55), and China (n = 51). Such research was mainly focused around medicine (57.1%), followed by biochemistry, genetics, and molecular biology (25.7%). Also, in the area of male reproduction, only 37.1% (n = 128) of the articles contributed towards original research, whereas 52.8% (n = 182) were review articles and editorials focusing more on sexual dysfunction than infertility. Such a small number of studies published on COVID-19-related effects on male reproduction warrants a significant increase in research, which is required to decipher the mechanism(s) underlying SARS-CoV-2 infection-associated impairment of male reproductive function.
1. Introduction
The coronavirus disease (COVID-19), caused by the SARS-CoV-2 virus, has resulted in nearly 15 million deaths worldwide [1]. The COVID-19 pandemic has also resulted in significant public health, social, and economic impacts worldwide [2,3]. SARS-CoV-2 infection mainly causes respiratory, digestive, cardiovascular, urinary, and nervous system complications [4,5]. The virus gains entry into cells by attaching itself to specific angiotensin-converting enzyme 2 (ACE2) receptors that are present on the surface of the cells [6] of various tissues (such as the respiratory tract, blood vessels, heart, intestines, and kidneys), including the reproductive system [7]. Male reproductive organs contain a substantially greater number of ACE2 receptors than female reproductive system organs [8,9]. Because of the ample expression of ACE2 receptors in the penis (especially corpus cavernosum) and testis, the male reproductive system is vulnerable to the effects of COVID-19 infection, thus affecting the sexual health and fertility of men [10,11,12].
Globally, infertility impacts more than 80 million couples (i.e., 15%) in the reproductive age group. The male factor is responsible for 50% of such infertile cases [13,14]. In general, laboratory evaluation of male infertility typically involves semen analysis mainly to assess sperm count, total motility, and morphology, in addition to a detailed physical, medical, and sexual history evaluation, including examination of the testes [13,14,15]. Combined, these can provide accurate information on a man’s fertility potential [16]. On the other hand, male sexual dysfunction includes difficulties with sexual desire, arousal, erection, orgasm, or ejaculation [17]. Both male infertility and sexual dysfunction can significantly impact not only a man’s but a couple’s quality of life and emotional well-being [18,19]. Research on male infertility and sexual dysfunction is continuously evolving to understand better the causes, risk factors, and treatment options for these conditions. Recent reports revealed that the male reproductive system is directly and indirectly affected by SARS-CoV-2, thus compromising its fertility potential [7,20]. The latest research trends in male infertility and sexual health have been analyzed and reported using bibliometric and scientometric tools [21,22,23,24]. However, there is scant information and publications on research trends on how COVID-19 is linked to male reproductive health.
Scientometrics is an interdisciplinary field involving quantitative analysis of science and scientific research [25]. It uses various bibliometric and statistical methods to study different aspects of scientific publications, such as journals, articles, authors, citations, research institutions, and scholarly communication [25,26]. These are essential tools used to evaluate and assess research productivity and scientific impact. It also provides valuable insights into the dissemination of knowledge, research trends, and the impact of scholarly work. Researchers frequently make efforts to quantify the development of a scientific field, the significance of peer-reviewed academic publications, and authorship patterns. Scientometrics is an important tool that has been widely used to study and analyze the scientific literature [27,28,29,30,31,32]. Since the onset of the COVID-19 pandemic and frequent occurrences of new variants along with “long COVID” effects, such scientometric tools are providing meaningful insight and gaining importance for current and future research in the medical field. However, no scientometric analysis studies are available to date that specifically focus on COVID-19 research in the area of male reproduction. The current scientometric study identifies and analyzes publication characteristics of articles on male reproduction and COVID-19.
2. Materials and Methods
2.1. Data Source
Scopus is a thorough bibliographic database that covers 17.6 million author profiles, and more than 87 million documents with 1.8 billion cited references [33]. Scopus provides details such as the type of document, number of citations, number of documents per year, authors and their affiliation, journal, country, and subject area, as required for scientometric analysis. In the current study, we used this Scopus database to identify the publications associated with male reproduction and COVID-19.
2.2. Data Retrieval Strategy
For a search of the literature in the Scopus database, we used a specific set of keywords (Table 1) to retrieve the articles published on male reproduction and COVID-19 (Figure 1). We limited our search to scientific articles published only on human subjects. Using the asterisk ‘*’ mark after a word, we included all possible variants of the term along with multiple Boolean operators such as ‘AND’, ‘OR’, ‘NOT’, and ‘AND NOT’ to invalidate false positive results. Also, functions such as ‘TITLE-ABSTRACT’ and ‘TITLE-ABSTRACT-KEYWORDS’ were used to retrieve a maximum number of relevant articles. Animal studies, non-English articles, and publications unrelated to male reproduction and COVID-19 were excluded from this analysis.

Table 1.
Search terms or keywords used to identify relevant articles related to male reproduction and COVID-19.
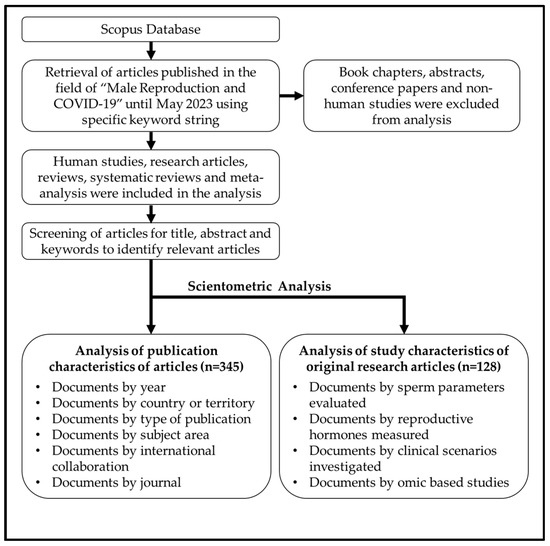
Figure 1.
The f low diagram signifiesthe data retrieval strategy for our scientometric analysis.
Any relevant article was categorized based on publication type (research or review article), subject area, and journal type. Further, we have sorted the original research articles according to clinical scenarios linked to male reproductive disorders or dysfunction, i.e., we classified the original studies that reported sperm parameters and reproductive hormone levels in SRAS-CoV-2 infected men in this analysis.
2.3. Scientometric and Statistical Analysis
The scientometric data that we retrieved from Scopus as comma-separated value (CSV) files was converted to Microsoft Excel data files for the purpose of descriptive statistical analysis. Such CSV files related to COVID-19 and male reproductive research were then used for geographical mapping. Further, we generated network maps based upon international collaboration in the area of COVID-19 and male reproductive research by using the software “VOSviewer” (downloaded from http://vosviewer.com, accessed on 11 June 2023) [34]. The number of documents co-authored by investigators from different countries was used to measure the relatedness between the countries. Whereas the size of the node was determined by the number of articles published by each country.
3. Results
3.1. COVID-19 and Male Reproductive Research
Our search of the literature showed 345 research articles that were directly related to COVID-19 and male reproduction (Figure 2). The majority of these articles were published in the USA (n = 72), then Italy (n = 55), and China (n = 51) (Figure 3). The majority of these publications were in the form of review articles (n = 182, 52.8%), and fewer were original articles (n = 128, 37.1%) (Figure 4A). The main research was in the fields of medicine, genetics and molecular biology, biochemistry, and microbiology/ immunology (Figure 4B). The network map shown in Figure 5 suggests collaboration between the countries. The major journals that published articles in this area were Andrology (n = 29), Andrologia (n = 16), and the Journal of Endocrinological Investigation (n = 13) (Figure 6).
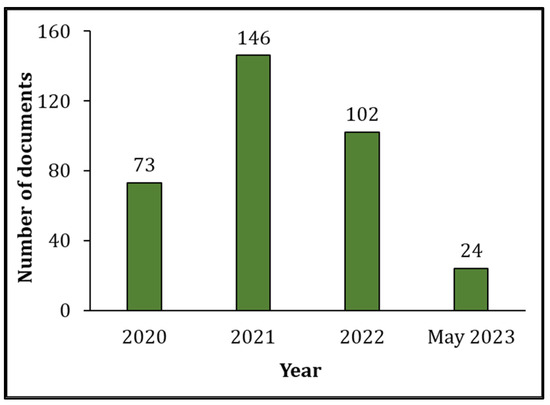
Figure 2.
Number of publications per year since the COVID-19 pandemic (2020 to May 2023) related to COVID-19 and male reproductive research.
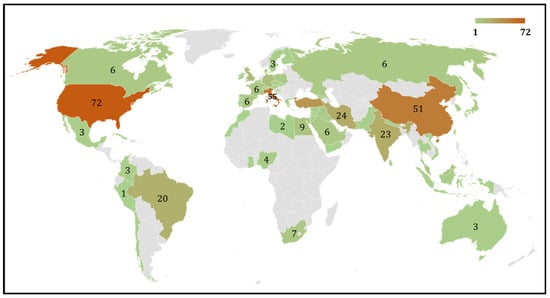
Figure 3.
Geomap depicting the distribution of number of publications from various countries that contributed to this research related to COVID-19 and male reproduction.
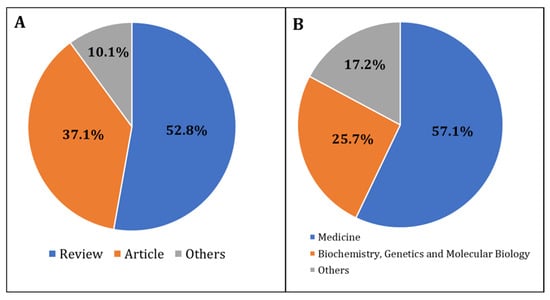
Figure 4.
Research trends based on the (A) type of publications, and (B) study areas that were related to COVID-19 and male reproduction during the period 2020 to May 2023.
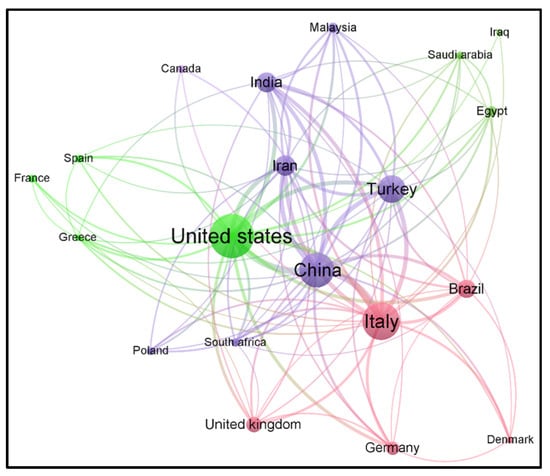
Figure 5.
Network map showing various countries that published such articles in the field of research related to COVID-19 and male reproduction from 2020 to May 2023.
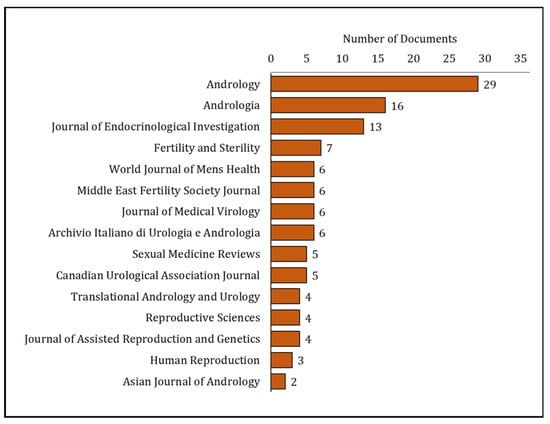
Figure 6.
Various journals that published research on COVID-19 and male reproduction from 2020 to May 2023.
3.2. The Scientometrics of COVID-19: Semen Parameters, Reproductive Hormones, and Viral Tropism Studies
Our publication trend analysis revealed that among the 128 research articles, 38 studies assessed male reproductive hormones (such as testosterone, luteinizing hormone, follicle-stimulating hormone, prolactin, estradiol, and inhibin) in COVID-19 patients with reproductive issues. In addition, 37 studies evaluated the effect of COVID-19 on semen parameters.
Scientometric analysis revealed that semen (n = 24) was the most common male reproductive system biospecimen to detect SARS-CoV-2 from COVID-19 patients. Other specimens, such as testis (n = 3) and penile tissue (n = 1), were also evaluated for the SARS-CoV-2 virus. Further, publication trend analysis revealed that 16.4% of studies (n = 21) investigated the expression of ACE receptors in sperm or testicular tissues.
3.3. COVID-19 Pandemic: Clinical Scenarios Associated with Men’s Sexual Health and Infertility
We investigated research publications on COVID-19 and male reproduction under different clinical situations related to male reproduction (Table 2). Our results showed that most of the COVID-19-related studies were focused on the area of erectile dysfunction (n = 21) followed by evaluation of semen characteristics (n = 6), varicocele (n = 5), idiopathic infertility (n = 2) and orchiepididymitis (n = 1). Our analysis revealed that erectile dysfunction was the leading area that gained more attention in COVID-19 and male reproduction research. Furthermore, we also noticed that 23 studies (18%) investigated the histopathology and pathophysiology of the male reproductive system associated with COVID-19 infection. In addition, only three studies investigated seminal oxidative stress-induced sperm DNA fragmentation in SARS-CoV-2-infected men.

Table 2.
Clinical scenarios coupled with men’s sexual health and infertility investigating the effect of COVID-19 on male reproduction during the years 2020 to May 2023.
3.4. Publication Trends in Omics-Based Male Reproductive Research during COVID-19 Infection
Finally, we evaluated publication trends on the impact of SARS-CoV-2 on molecular changes in male reproductive organs. Scientometric analysis revealed that ten studies (7.8%) used omics platforms to study the transcriptome and proteome of male reproductive organs.
4. Discussion
The COVID-19 pandemic, on a global scale, negatively affected the wellness of human beings, including their reproductive health [7]. Several scientometric, bibliometric, and publication pattern studies were published on COVID-19 in various fields of biomedical research [32,35,36,37,38,39,40]. Scientometric studies provide a global evaluation report of scientific publications on a specific topic. This study is the first methodical evaluation of COVID-19 and male reproductive health based on a scientometric approach. The literature analysis identified the extent of publications on COVID-19 related to male reproductive research, with a maximum number of studies in 2021. Interestingly, publications on COVID-19 and male reproduction were mostly review articles compared to original research articles. Geo-mapping and network analysis clearly illustrated the USA as the top publishing country studying the impact of this virus on men’s sexual health and infertility, along with its international collaboration with other countries.
SARS-CoV-2 enters the cells via the ACE2 receptor, which is also present in different organs, including the testes [6]. Further, SARS-CoV-2 can activate the ACE2 receptor in seminal plasma components, making semen a transmission route to COVID-19 infection [41]. Our scientometric results indicated that 16.4% of studies investigating the consequences of COVID-19 on male reproduction measured the expression of the ACE2 receptor in sperm or testicular tissues. Mainly, the ACE2 receptors are expressed in the sperm midpiece and distributed in the acrosomal region of the sperm head. Whereas in human testis, ACE2 receptors are highly expressed in spermatogonia, Leydig, and Sertoli cells [42]. Interestingly, SARS-CoV-2 was also detected in the penile tissue of infected patients, even those who recovered from this infection [43,44]. In addition, SARS-CoV-2 has been identified in other body fluids such as saliva, blood, urine, and cerebrospinal fluid [45,46]. We noticed that about 18.8% of studies published on the effects of COVID-19 on male reproduction screened semen samples for the presence of the virus. Several studies have documented the shedding of SARS-CoV-2 in the semen of men with symptomatic and asymptomatic phases [47,48]. In contrast, other investigators were unable to detect virus particles in the semen of men infected with SARS-CoV-2 [49,50,51]. Hence, the detection of viruses in semen samples remains debatable. It may be possible that the strain or variant and virulence factor of the virus may have a crucial role in causing damage to the blood–testis barrier (BTB) and other accessory reproductive glands, such as seminal vesicles and the prostate, and thus infiltrate into semen. Additional studies are required to draw a meaningful conclusion to validate the transmission of SARS-CoV-2 through semen.
COVID-19 infection has been linked to male infertility [7], and molecular findings revealed defective spermatogenesis and an impaired BTB in infected men [52,53]. The scientometric analysis indicated that nearly 28.9% of studies focused on reproductive health investigated the semen parameters of SARS-CoV-2-infected men. Also, recent meta-analysis results reported a negative association between semen quality and SARS-CoV-2 infection [54,55,56,57]. However, till now, none of the studies investigated the long-term impact of this virus on semen quality and reproductive function. Few studies have focused on male infertility associated with semen abnormalities (4.7%), varicocele (3.9%), and idiopathic infertility (1.6%), evaluating the repercussions of this disease on sperm parameters. Systemic viral infection negatively impacts sperm production and the quality of semen [58]. Further, such viral infections may induce damage to sperm DNA, impairing their ability to fertilize oocytes [59,60]. Based on our current analysis in this area, very few studies (n = 3) reported seminal oxidative stress and damage to sperm DNA induced by SARS-CoV-2 infection. Seminal oxidative stress was evaluated based on the increased levels of reactive oxygen species (ROS) or decreased antioxidant levels in the semen or seminal plasma, whereas sperm DNA fragmentation is commonly measured based on the extent of chromatin dispersion (halos) observed under the microscope. A positive correlation exists between oxidative stress and sperm DNA damage [61]. However, the literature still lacks mechanistic studies that can delineate the negative influence of SARS-CoV-2 infection on sperm DNA and fertility.
Scientometric analysis indicated nearly 29.7% of research articles reported reproductive hormone levels in SARS-CoV-2-infected men. The hypothalamus-pituitary-gonad (HPG) axis maintains the balance of male sex hormones and gonadal function [62,63]. SARS-CoV-2 infection negatively impacts the HPG axis, affecting male reproductive hormone levels and testicular physiology [64,65]. Endocrine disturbances linked to the male reproductive system decrease testosterone levels in patients with COVID-19, resulting in hypogonadism, which may result in erectile dysfunction (ED) [66,67]. In addition, other hormones, such as LH and FSH levels, were significantly lower, and estradiol levels were higher in COVID-19 patients [68,69]. Whereas no such change was reported in the prolactin levels. Our analysis also shows that research on male reproductive health is focused more on ED. Men infected or recovered from SARS-CoV-2 infection are more prone to ED issues than uninfected men [70,71]. However, additional research is required to establish a causal link between COVID-19, hypogonadism, and ED. Further, the exact mechanisms and the extent of this impact are not yet fully understood.
Omics platforms, such as genomics, transcriptomics, and proteomics, including single-cell RNA sequencing techniques, are widely employed to understand the changes at the subcellular level due to infection [72]. Most of the omics studies on SARS-CoV-2 infection and its consequence on testis focused on understanding the expression pattern of ACE2 in various types of cells. Transcriptomic analysis revealed the negative impact of COVID-19 on spermatogenesis and the dysregulation of molecular pathways linked to the immune response, which in turn may alter spermatogenesis by inducing testicular cell senescence through the MAPK signaling pathway [73]. Further, impaired spermatogenesis was supported by histopathological changes such as the presence of degenerated germ cells (GCs) in the lumen of seminiferous tubules that indicated negative a impact of SARS-CoV-2 infection on GC development [74]. In addition, proteomic analysis revealed downregulation of proteins involved in reproductive function in the seminal plasma of COVID-19-recovered patients, indicating that the fertility potential of these men was compromised post-SARS-CoV-2 infection [75]. However, further studies are needed to understand the impact of long COVID-19 on spermatogenesis, semen quality, and overall impact on male reproduction, especially since many new variants are frequently evolving.
In the present study, we have analyzed the data of the last four years, thus including the most recent publications (2019–May 2023) since COVID-19 was declared a pandemic. Thus, it represents all the publications available on COVID-19 and male reproductive research. However, we have only used bibliometric information retrieved from the Scopus database, and therefore, a few publications not indexed in Scopus could have been omitted from the analysis.
5. Conclusions
To our knowledge, this is the first scientometric analysis showing a detailed assessment of published studies focused on COVID-19 and male reproduction. Our analysis was focused on both male infertility and sexual dysfunction studies. This information is useful to researchers interested in the latest developments in this area and looking forward to evidence-based research concerning the COVID-19 pandemic. A small number of studies have been published on male reproduction compared to other fields related to the health sciences. A significant increase in COVID-based reproductive research is required to ascertain the mechanism(s) underlying SARS-CoV-2 infection-associated impairment of male reproduction and the impact of long COVID-19.
Author Contributions
Conceptualization, M.K.P.S. and S.C.S.; methodology, M.K.P.S., A.K. and S.B.; software, M.K.P.S.; validation, M.K.P.S., A.K. and S.B.; formal analysis, M.K.P.S. and S.B.; data curation, M.K.P.S., A.K., A.K.M. and S.B.; writing—original draft preparation, M.K.P.S., S.B. and A.K.; writing—review and editing, M.K.P.S., S.B., A.K., A.K.M. and S.C.S.; supervision, M.K.P.S. and S.C.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded and supported by Department of Urology, Tulane University School of Medicine.
Institutional Review Board Statement
This study was conducted using the scientometric data retrieved from the SCOPUS database and did not involve the participation of human or animal subjects. Hence, it is exempted from review by the Institutional Review Board.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
We are thankful to the Department of Urology, Tulane University School of Medicine for supporting this research.
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO. 14.9 Million Excess Deaths Associated with the COVID-19 Pandemic in 2020 and 2021. 2022. Available online: https://www.who.int/news/item/05-05-2022-14.9-million-excess-deaths-were-associated-with-the-covid-19-pandemic-in-2020-and-2021 (accessed on 30 July 2023).
- Miyah, Y.; Benjelloun, M.; Lairini, S.; Lahrichi, A. COVID-19 Impact on Public Health, Environment, Human Psychology, Global Socioeconomy, and Education. Sci. World J. 2022, 2022, 5578284. [Google Scholar] [CrossRef] [PubMed]
- Osterrieder, A.; Cuman, G.; Pan-Ngum, W.; Cheah, P.K.; Cheah, P.K.; Peerawaranun, P.; Silan, M.; Orazem, M.; Perkovic, K.; Groselj, U.; et al. Economic and social impacts of COVID-19 and public health measures: Results from an anonymous online survey in Thailand, Malaysia, the UK, Italy and Slovenia. BMJ Open 2021, 11, e046863. [Google Scholar] [CrossRef] [PubMed]
- Kopańska, M.; Barnaś, E.; Błajda, J.; Kuduk, B.; Łagowska, A.; Banaś-Ząbczyk, A. Effects of SARS-CoV-2 Inflammation on Selected Organ Systems of the Human Body. Int. J. Mol. Sci. 2022, 23, 4178. [Google Scholar] [CrossRef] [PubMed]
- Connelly, Z.M.; Whitaker, D.; Dullea, A.; Ramasamy, R. SARS-CoV-2 Effects on the Male Genitourinary System. Am. J. Clin. Exp. Urol. 2022, 10, 199–209. [Google Scholar] [PubMed]
- Gheblawi, M.; Wang, K.; Viveiros, A.; Nguyen, Q.; Zhong, J.C.; Turner, A.J.; Raizada, M.K.; Grant, M.B.; Oudit, G.Y. Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System: Celebrating the 20th Anniversary of the Discovery of ACE2. Circ. Res. 2020, 126, 1456–1474. [Google Scholar] [CrossRef] [PubMed]
- Khalili, M.A.; Leisegang, K.; Majzoub, A.; Finelli, R.; Panner Selvam, M.K.; Henkel, R.; Mojgan, M.; Agarwal, A. Male Fertility and the COVID-19 Pandemic: Systematic Review of the Literature. World J. Men’s Health 2020, 38, 506–520. [Google Scholar] [CrossRef] [PubMed]
- Hikmet, F.; Méar, L.; Edvinsson, Å.; Micke, P.; Uhlén, M.; Lindskog, C. The protein expression profile of ACE2 in human tissues. Mol. Syst. Biol. 2020, 16, e9610. [Google Scholar] [CrossRef]
- Zangeneh, F.Z. Interaction of SARS-CoV-2 with RAS/ACE2 in the Female Reproductive System. J. Fam. Reprod. Health 2022, 16, 1–8. [Google Scholar] [CrossRef]
- Li, X.; Lu, H.; Li, F.; Zhang, Q.; Wang, T.; Qiang, L.; Yang, Q. Impacts of COVID-19 and SARS-CoV-2 on male reproductive function: A systematic review and meta-analysis protocol. BMJ Open 2022, 12, e053051. [Google Scholar] [CrossRef]
- He, Y.; Wang, J.; Ren, J.; Zhao, Y.; Chen, J.; Chen, X. Effect of COVID-19 on Male Reproductive System—A Systematic Review. Front. Endocrinol. 2021, 12, 677701. [Google Scholar] [CrossRef]
- Rainer, Q.; Molina, M.; Ibrahim, E.; Saltzman, R.; Masterson, T.; Ramasamy, R. Peyronie’s disease in a patient after COVID-19 infection: A case report. Andrologia 2021, 53, e14219. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Baskaran, S.; Parekh, N.; Cho, C.L.; Henkel, R.; Vij, S.; Arafa, M.; Panner Selvam, M.K.; Shah, R. Male infertility. Lancet 2021, 397, 319–333. [Google Scholar] [CrossRef] [PubMed]
- Sikka, S.C.; Hellstrom, W.J. Current updates on laboratory techniques for the diagnosis of male reproductive failure. Asian J. Androl. 2016, 18, 392–401. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Sharma, R.; Gupta, S.; Finelli, R.; Parekh, N.; Selvam, M.K.P.; Pompeu, C.P.; Madani, S.; Belo, A.; Darbandi, M.; et al. Standardized Laboratory Procedures, Quality Control and Quality Assurance Are Key Requirements for Accurate Semen Analysis in the Evaluation of Infertile Male. World J. Men’s Health 2022, 40, 52–65. [Google Scholar] [CrossRef]
- Barratt, C.L. Semen analysis is the cornerstone of investigation for male infertility. Practitioner 2007, 251, 8–10, 12, 15–17. [Google Scholar]
- Anderson, D.; Laforge, J.; Ross, M.M.; Vanlangendonck, R.; Hasoon, J.; Viswanath, O.; Kaye, A.D.; Urits, I. Male Sexual Dysfunction. Health Psychol. Res. 2022, 10, 37533. [Google Scholar] [CrossRef]
- Fisher, J.R.; Hammarberg, K. Psychological and social aspects of infertility in men: An overview of the evidence and implications for psychologically informed clinical care and future research. Asian J. Androl. 2012, 14, 121–129. [Google Scholar] [CrossRef]
- Sánchez-Cruz, J.J.; Cabrera-León, A.; Martín-Morales, A.; Fernández, A.; Burgos, R.; Rejas, J. Male erectile dysfunction and health-related quality of life. Eur. Urol. 2003, 44, 245–253. [Google Scholar] [CrossRef]
- Ardestani Zadeh, A.; Arab, D. COVID-19 and male reproductive system: Pathogenic features and possible mechanisms. J. Mol. Histol. 2021, 52, 869–878. [Google Scholar] [CrossRef]
- Hui, J.; He, S.; Liu, R.; Zeng, Q.; Zhang, H.; Wei, A. Trends in erectile dysfunction research from 2008 to 2018: A bibliometric analysis. Int. J. Impot. Res. 2020, 32, 409–419. [Google Scholar] [CrossRef]
- Baskaran, S.; Agarwal, A.; Leisegang, K.; Pushparaj, P.N.; Panner Selvam, M.K.; Henkel, R. An In-Depth Bibliometric Analysis and Current Perspective on Male infertility Research. World J. Men’s Health 2021, 39, 302–314. [Google Scholar] [CrossRef] [PubMed]
- Rezaee, M.E.; Johnson, H.A.; Munarriz, R.M.; Gross, M.S. Bibliometric Analysis of Erectile Dysfunction Publications in Urology and Sexual Medicine Journals. J. Sex. Med. 2018, 15, 1426–1433. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Xiao, F.; Lu, S.; Song, J.; Zhang, C.; Li, J.; Gu, K.; Lan, A.; Lv, B.; Zhang, R.; et al. Research trends and perspectives of male infertility: A bibliometric analysis of 20 years of scientific literature. Andrology 2016, 4, 990–1001. [Google Scholar] [CrossRef] [PubMed]
- Klaić, B. The use of scientometric parameters for the evaluation of scientific contributions. Coll. Antropol. 1999, 23, 751–770. [Google Scholar] [PubMed]
- de Oliveira, O.J.; da Silva, F.F.; Juliani, F.; Barbosa, L.C.F.M.; Nunhes, T.V. Bibliometric method for mapping the state-of-the-art and identifying research gaps and trends in literature: An essential instrument to support the development of scientific projects. In Scientometrics Recent Advances; IntechOpen: London, UK, 2019. [Google Scholar]
- Ginting, B.; Chiari, W.; Duta, T.F.; Hudaa, S.; Purnama, A.; Harapan, H.; Rizki, D.R.; Puspita, K.; Idroes, R.; Meriatna, M.; et al. COVID-19 pandemic sheds a new research spotlight on antiviral potential of essential oils—A bibliometric study. Heliyon 2023, 9, e17703. [Google Scholar] [CrossRef] [PubMed]
- Lai, P.; Xu, S.; Xue, J.H.; Zhang, H.Z.; Zhong, Y.M.; Liao, Y.L. Current hotspot and study trend of innate immunity in COVID-19: A bibliometric analysis from 2020 to 2022. Front. Immunol. 2023, 14, 1135334. [Google Scholar] [CrossRef]
- Yeung, A.W.K.; Parvanov, E.D.; Nawaz, F.A.; Rayan, R.A.; Kletecka-Pulker, M.; Willschke, H.; Atanasov, A.G. COVID-19 Rapid Antigen Tests: Bibliometric Analysis of the Scientific Literature. Int. J. Environ. Res. Public Health 2022, 19, 12493. [Google Scholar] [CrossRef]
- Wen, R.; Zhang, M.; Xu, R.; Gao, Y.; Liu, L.; Chen, H.; Wang, X.; Zhu, W.; Lin, H.; Liu, C.; et al. COVID-19 imaging, where do we go from here? Bibliometric analysis of medical imaging in COVID-19. Eur. Radiol. 2023, 33, 3133–3143. [Google Scholar] [CrossRef]
- Wang, H.; Le, Z. Expert recommendations based on link prediction during the COVID-19 outbreak. Scientometrics 2021, 126, 4639–4658. [Google Scholar] [CrossRef]
- Noruzi, A.; Gholampour, B.; Gholampour, S.; Jafari, S.; Farshid, R.; Stanek, A.; Saboury, A.A. Current and Future Perspectives on the COVID-19 Vaccine: A Scientometric Review. J. Clin. Med. 2022, 11, 750. [Google Scholar] [CrossRef]
- Scopus. Scopus Provides Unmatched Content and Data Quality, with Superior Search and Analytical Tools. 2023. Available online: https://www.elsevier.com/solutions/scopus/how-scopus-works (accessed on 30 July 2023).
- van Eck, N.J.; Waltman, L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics 2010, 84, 523–538. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.X.; Ha, G.H.; Nguyen, L.H.; Vu, G.T.; Hoang, M.T.; Le, H.T.; Latkin, C.A.; Ho, C.S.H.; Ho, R.C.M. Studies of Novel Coronavirus Disease 19 (COVID-19) Pandemic: A Global Analysis of Literature. Int. J. Environ. Res. Public Health 2020, 17, 4095. [Google Scholar] [CrossRef] [PubMed]
- Şenel, E.; Topal, F.E. Holistic Analysis of Coronavirus Literature: A Scientometric Study of the Global Publications Relevant to SARS-CoV-2 (COVID-19), MERS-CoV (MERS) and SARS-CoV (SARS). Disaster Med. Public Health Prep. 2021, 15, e12–e19. [Google Scholar] [CrossRef] [PubMed]
- Wei, N.; Xu, Y.; Wang, H.; Jia, Q.; Shou, X.; Zhang, X.; Zhang, N.; Li, Y.; Zhai, H.; Hu, Y. Bibliometric and visual analysis of cardiovascular diseases and COVID-19 research. Front. Public Health 2022, 10, 1022810. [Google Scholar] [CrossRef] [PubMed]
- Hamidi, A.; Khosravi, A.; Hejazi, R.; FatemehTorabi; Abtin, A. A scientometric approach to psychological research during the COVID-19 pandemic. Curr. Psychol. 2023, 1–10. [Google Scholar] [CrossRef]
- Zhou, R.; Lin, X.; Xu, J.; Lin, X.; Wu, Z. Knowledge mapping analysis of mental health research on COVID-19. Front. Psychiatry 2022, 13, 931575. [Google Scholar] [CrossRef]
- Kalra, G.; Kaur, R.; Ichhpujani, P.; Chahal, R.; Kumar, S. COVID-19 and ophthalmology: A scientometric analysis. Indian J. Ophthalmol. 2021, 69, 1234–1240. [Google Scholar] [CrossRef]
- Hajizadeh Maleki, B.; Tartibian, B. COVID-19 and male reproductive function: A prospective, longitudinal cohort study. Reproduction 2021, 161, 319–331. [Google Scholar] [CrossRef]
- Wang, Z.; Xu, X. scRNA-seq Profiling of Human Testes Reveals the Presence of the ACE2 Receptor, A Target for SARS-CoV-2 Infection in Spermatogonia, Leydig and Sertoli Cells. Cells 2020, 9, 920. [Google Scholar] [CrossRef]
- Kervancioglu Demirci, E.; Dursun, M.; Seviç, E.; Ergül, R.B.; Önel, M.; Ağaçfidan, A.; Kadıoğlu, A. Evidence for residual SARS-CoV-2 in corpus cavernosum of patients who recovered from COVID-19 infection. Andrology 2022, 11, 1016–1022. [Google Scholar] [CrossRef]
- Kresch, E.; Achua, J.; Saltzman, R.; Khodamoradi, K.; Arora, H.; Ibrahim, E.; Kryvenko, O.N.; Almeida, V.W.; Firdaus, F.; Hare, J.M.; et al. COVID-19 Endothelial Dysfunction Can Cause Erectile Dysfunction: Histopathological, Immunohistochemical, and Ultrastructural Study of the Human Penis. World J. Men’s Health 2021, 39, 466–469. [Google Scholar] [CrossRef] [PubMed]
- Mumm, J.N.; Ledderose, S.; Ostermann, A.; Rudelius, M.; Hellmuth, J.C.; Münchhoff, M.; Munker, D.; Scherer, C.; Volz, Y.; Ebner, B.; et al. Dynamics of urinary and respiratory shedding of Severe acute respiratory syndrome virus 2 (SARS-CoV-2) RNA excludes urine as a relevant source of viral transmission. Infection 2022, 50, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.W.L.; Klinkhammer, B.M.; Djudjaj, S.; Villwock, S.; Timm, M.C.; Buhl, E.M.; Wucherpfennig, S.; Cacchi, C.; Braunschweig, T.; Knüchel-Clarke, R.; et al. Multisystemic Cellular Tropism of SARS-CoV-2 in Autopsies of COVID-19 Patients. Cells 2021, 10, 1900. [Google Scholar] [CrossRef] [PubMed]
- Saylam, B.; Uguz, M.; Yarpuzlu, M.; Efesoy, O.; Akbay, E.; Çayan, S. The presence of SARS-CoV-2 virus in semen samples of patients with COVID-19 pneumonia. Andrologia 2021, 53, e14145. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Jin, M.; Bao, P.; Zhao, W.; Zhang, S. Clinical Characteristics and Results of Semen Tests Among Men with Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e208292. [Google Scholar] [CrossRef]
- Pavone, C.; Giammanco, G.M.; Cascino, A.P.; Baiamonte, D.; Pinelli, M.; Cangelosi, E.; Filizzolo, C.; Sciortino, G.; Grazia, S.; Bonura, F. Assessment of SARS-CoV-2 RNA shedding in semen of 36 males with symptomatic, asymptomatic, and convalescent infection during the first and second wave of COVID-19 pandemic in Italy. Asian J. Androl. 2022, 24, 135–138. [Google Scholar] [CrossRef]
- Burke, C.A.; Skytte, A.B.; Kasiri, S.; Howell, D.; Patel, Z.P.; Trolice, M.P.; Parekattil, S.J.; Michael, S.F.; Paul, L.M. A cohort study of men infected with COVID-19 for presence of SARS-CoV-2 virus in their semen. J. Assist. Reprod. Genet. 2021, 38, 785–789. [Google Scholar] [CrossRef]
- Holtmann, N.; Edimiris, P.; Andree, M.; Doehmen, C.; Baston-Buest, D.; Adams, O.; Kruessel, J.S.; Bielfeld, A.P. Assessment of SARS-CoV-2 in human semen-a cohort study. Fertil. Steril. 2020, 114, 233–238. [Google Scholar] [CrossRef]
- Peirouvi, T.; Aliaghaei, A.; Eslami Farsani, B.; Ziaeipour, S.; Ebrahimi, V.; Forozesh, M.; Ghadipasha, M.; Mahmoudiasl, G.R.; Aryan, A.; Moghimi, N.; et al. COVID-19 disrupts the blood-testis barrier through the induction of inflammatory cytokines and disruption of junctional proteins. Inflamm. Res. 2021, 70, 1165–1175. [Google Scholar] [CrossRef]
- Selvam, M.K.P.; Pushparaj, P.N.; Baskaran, S.; Sikka, S. PD36-01 Bioinformatic Analysis of RNA Sequencing Data of Testis from SARS-CoV-2 Infected Men Reveals Molecular Alteration of Germ Cell-Sertoli cell Junction Signaling Pathway. J. Urol. 2022, 207, e633. [Google Scholar] [CrossRef]
- Xie, Y.; Mirzaei, M.; Kahrizi, M.S.; Shabestari, A.M.; Riahi, S.M.; Farsimadan, M.; Roviello, G. SARS-CoV-2 effects on sperm parameters: A meta-analysis study. J. Assist. Reprod. Genet. 2022, 39, 1555–1563. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, S.; Kc, N.; Thapa, S.; Ghimire, A.; Bijukchhe, S.; Sah, G.S.; Isnuwardana, R. Semen parameters in men recovered from COVID-19: A systematic review and meta-analysis. Middle East Fertil. Soc. J. 2021, 26, 44. [Google Scholar] [CrossRef] [PubMed]
- Corona, G.; Vena, W.; Pizzocaro, A.; Pallotti, F.; Paoli, D.; Rastrelli, G.; Baldi, E.; Cilloni, N.; Gacci, M.; Semeraro, F.; et al. Andrological effects of SARS-Cov-2 infection: A systematic review and meta-analysis. J. Endocrinol. Investig. 2022, 45, 2207–2219. [Google Scholar] [CrossRef]
- Lan, X.; Wang, M.; Yu, X.; Dong, L.; Li, J.; Chang, D.; Yang, F. A systematic review of the effect of COVID-19 on semen parameters. Heliyon 2023, 9, e14776. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, T.A.; Oliveira, Y.C.; Bernardes, F.S.; Kallas, E.G.; Duarte-Neto, A.N.; Esteves, S.C.; Drevet, J.R.; Hallak, J. Viral infections and implications for male reproductive health. Asian J. Androl. 2021, 23, 335–347. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Sun, P.; Xie, X.; Sun, D.; Zhou, Q.; Yang, S.; Xie, Q.; Zhou, X. Hepatitis B virus surface protein induces oxidative stress by increasing peroxides and inhibiting antioxidant defences in human spermatozoa. Reprod. Fertil. Dev. 2020, 32, 1180–1189. [Google Scholar] [CrossRef] [PubMed]
- Akhigbe, R.E.; Dutta, S.; Hamed, M.A.; Ajayi, A.F.; Sengupta, P.; Ahmad, G. Viral Infections and Male Infertility: A Comprehensive Review of the Role of Oxidative Stress. Front. Reprod. Health 2022, 4, 782915. [Google Scholar] [CrossRef] [PubMed]
- Panner Selvam, M.K.; Baskaran, S.; O’Connell, S.; Almajed, W.; Hellstrom, W.J.G.; Sikka, S.C. Association between Seminal Oxidation-Reduction Potential and Sperm DNA Fragmentation-A Meta-Analysis. Antioxidants 2022, 11, 1563. [Google Scholar] [CrossRef] [PubMed]
- Plant, T.M. 60 Years of Neuroendocrinology: The hypothalamo-pituitary-gonadal axis. J. Endocrinol. 2015, 226, T41–T54. [Google Scholar] [CrossRef]
- Caroppo, E. Male hypothalamic–pituitary–gonadal axis. In Infertility in the Male, 4th ed.; Niederberger, C.S., Lipshultz, L.I., Howards, S.S., Eds.; Cambridge University Press: Cambridge, UK, 2009; pp. 14–28. [Google Scholar] [CrossRef]
- Dai, P.; Qiao, F.; Chen, Y.; Chan, D.Y.L.; Yim, H.C.H.; Fok, K.L.; Chen, H. SARS-CoV-2 and male infertility: From short- to long-term impacts. J. Endocrinol. Investig. 2023, 46, 1491–1507. [Google Scholar] [CrossRef]
- Moreno-Perez, O.; Merino, E.; Alfayate, R.; Torregrosa, M.E.; Andres, M.; Leon-Ramirez, J.M.; Boix, V.; Gil, J.; Pico, A. Male pituitary-gonadal axis dysfunction in post-acute COVID-19 syndrome-Prevalence and associated factors: A Mediterranean case series. Clin. Endocrinol. 2022, 96, 353–362. [Google Scholar] [CrossRef] [PubMed]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Alarfaj, S.J.; Al-Akeel, R.K.; Faidah, H.; El-Bouseary, M.M.; Sabatier, J.M.; De Waard, M.; El-Masry, T.A.; Batiha, G.E. Long COVID and risk of erectile dysfunction in recovered patients from mild to moderate COVID-19. Sci. Rep. 2023, 13, 5977. [Google Scholar] [CrossRef] [PubMed]
- Adeyemi, D.H.; Odetayo, A.F.; Hamed, M.A.; Akhigbe, R.E. Impact of COVID-19 on erectile function. Aging Male 2022, 25, 202–216. [Google Scholar] [CrossRef] [PubMed]
- Temiz, M.Z.; Dincer, M.M.; Hacibey, I.; Yazar, R.O.; Celik, C.; Kucuk, S.H.; Alkurt, G.; Doganay, L.; Yuruk, E.; Muslumanoglu, A.Y. Investigation of SARS-CoV-2 in semen samples and the effects of COVID-19 on male sexual health by using semen analysis and serum male hormone profile: A cross-sectional, pilot study. Andrologia 2021, 53, e13912. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Wang, Z.; Feng, C.; Yu, W.; Chen, Y.; Zeng, X.; Liu, C. Effects of SARS-CoV-2 infection on male sex-related hormones in recovering patients. Andrology 2021, 9, 107–114. [Google Scholar] [CrossRef]
- Harirugsakul, K.; Wainipitapong, S.; Phannajit, J.; Paitoonpong, L.; Tantiwongse, K. Erectile dysfunction after COVID-19 recovery: A follow-up study. PLoS ONE 2022, 17, e0276429. [Google Scholar] [CrossRef]
- Gök, A.; Altan, M.; Doğan, A.E.; Eraslan, A.; Uysal, F.; Öztürk, U.; Saguner, A.M.; İmamoğlu, M.A. Does Post-COVID-19 Erectile Dysfunction Improve over Time? J. Clin. Med. 2023, 12, 1241. [Google Scholar] [CrossRef]
- Li, Y.; Hou, G.; Zhou, H.; Wang, Y.; Tun, H.M.; Zhu, A.; Zhao, J.; Xiao, F.; Lin, S.; Liu, D.; et al. Multi-platform omics analysis reveals molecular signature for COVID-19 pathogenesis, prognosis and drug target discovery. Signal Transduct. Target. Ther. 2021, 6, 155. [Google Scholar] [CrossRef]
- Wang, Z.; Ma, Y.; Chen, Z.; Yang, R.; Liu, Q.; Pan, J.; Wang, J.; Liu, Y.; Zhou, M.; Zhang, Y.; et al. COVID-19 inhibits spermatogenesis in the testes by inducing cellular senescence. Front. Genet. 2022, 13, 981471. [Google Scholar] [CrossRef]
- Ma, X.; Guan, C.; Chen, R.; Wang, Y.; Feng, S.; Wang, R.; Qu, G.; Zhao, S.; Wang, F.; Wang, X.; et al. Pathological and molecular examinations of postmortem testis biopsies reveal SARS-CoV-2 infection in the testis and spermatogenesis damage in COVID-19 patients. Cell. Mol. Immunol. 2021, 18, 487–489. [Google Scholar] [CrossRef]
- Ghosh, S.; Parikh, S.; Nissa, M.U.; Acharjee, A.; Singh, A.; Patwa, D.; Makwana, P.; Athalye, A.; Barpanda, A.; Laloraya, M.; et al. Semen Proteomics of COVID-19 Convalescent Men Reveals Disruption of Key Biological Pathways Relevant to Male Reproductive Function. ACS Omega 2022, 7, 8601–8612. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).