Primary Fallopian Tube Carcinoma: An Extremely Rare Gynecological Cancer Misdiagnosed Intraoperatively as Benign Ovarian Neoplasm: A Case Report
Abstract
:1. Introduction
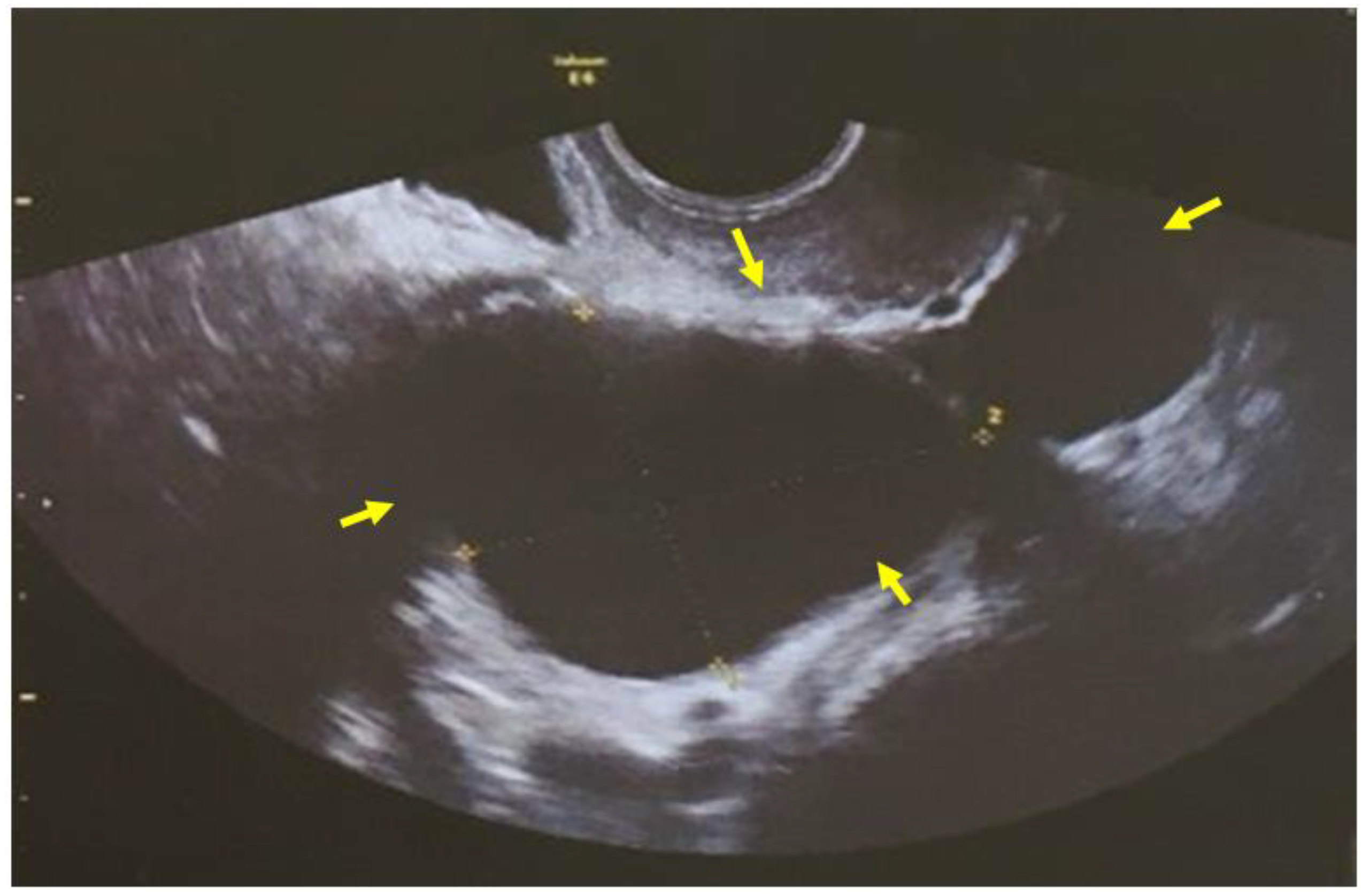
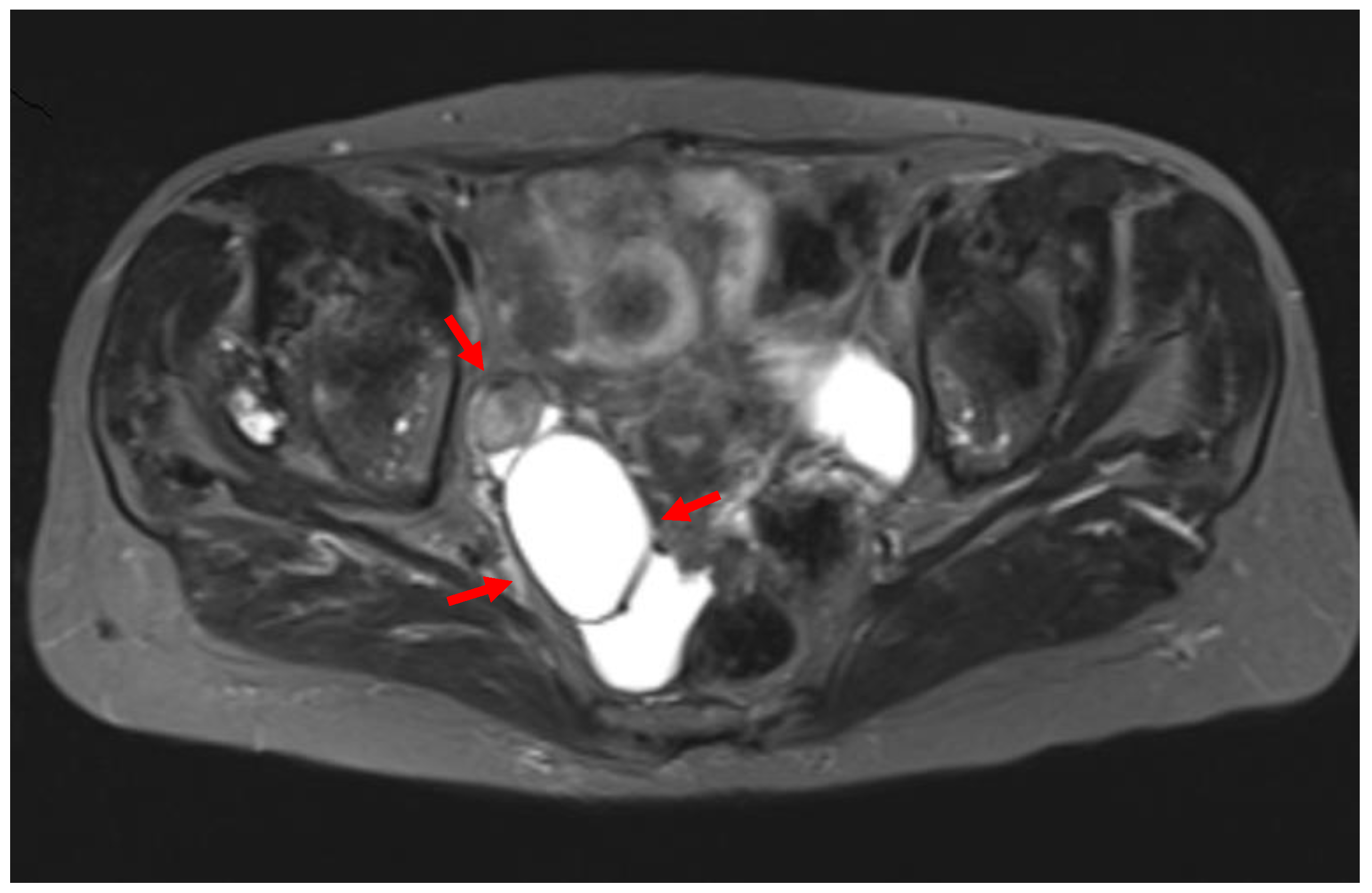
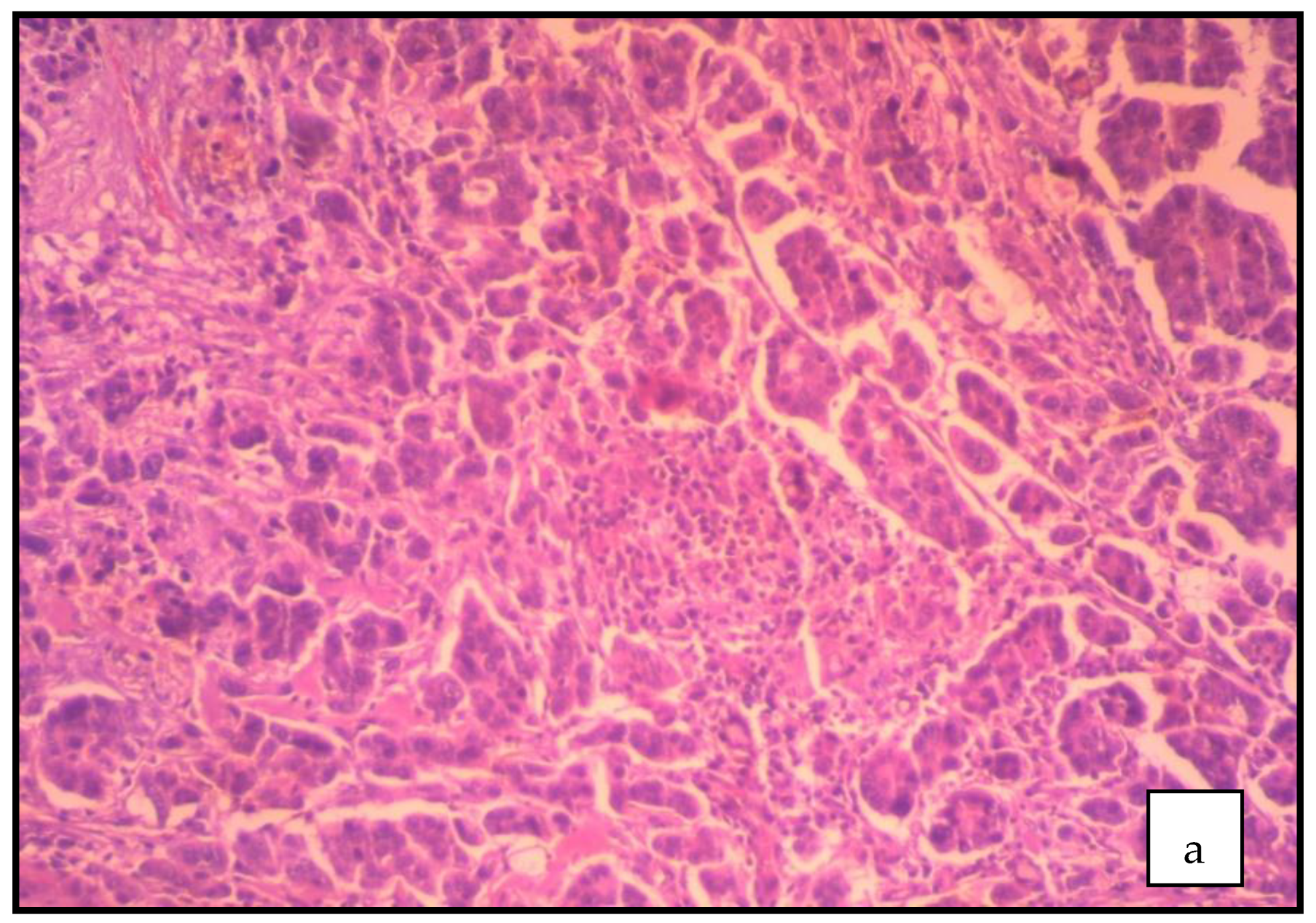
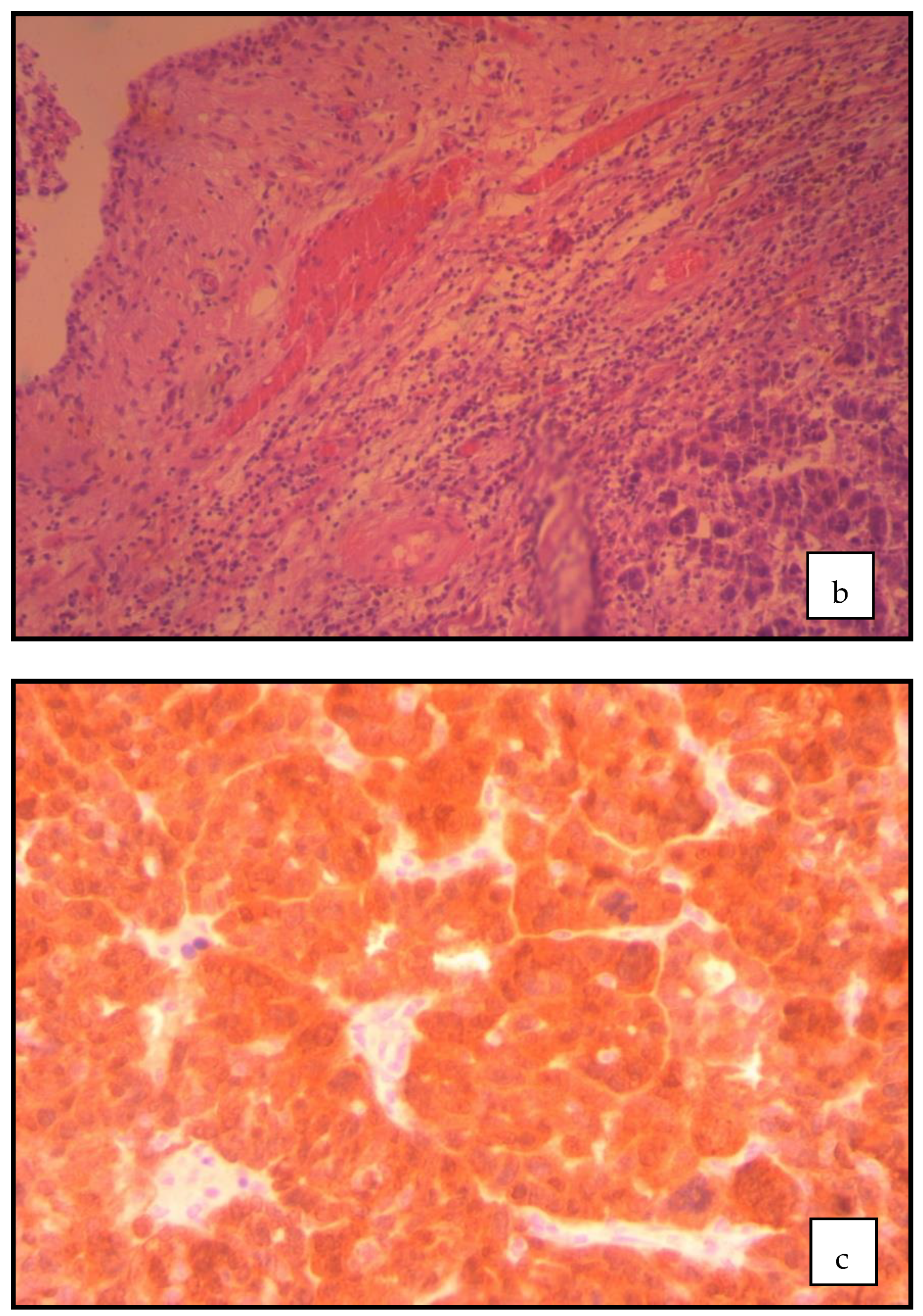
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eken, M.; Temizkan, O.; Kaygusuz, E.I.; Herkiloğlu, D.; Çöğendez, E.; Karateke, A. Primarycarcinoma of the fallopian tubes: Analysis of sixteen patients. Turk. J. Obstet. Gynecol. 2015, 12, 83–88. [Google Scholar] [CrossRef]
- Jeung, I.C.; Lee, Y.S.; Lee, H.N.; Park, E.K. Primary carcinoma of the fallopian tube: Report of two cases with literature review. Cancer Res. Treat. 2009, 41, 113–116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riska, A.; Leminen, A.; Pukkala, E. Sociodemographic determinants of incidence of primary fallopian tube carcinoma, Finland 1953–1997. Int. J. Cancer 2003, 104, 643–645. [Google Scholar] [CrossRef] [PubMed]
- Shaaban, A.M.; Rezvani, M. Imaging of primary fallopian tube carcinoma. Abdom. Imaging 2013, 38, 608–618. [Google Scholar] [CrossRef] [PubMed]
- Nanaiah, S.P.; Rathod, P.S.; Rajkumar, N.N.; Kundargi, R.; Subbian, A.; Ramachandra, P.V.; Krishnappa, S.; Narayan, A.; Devi, U.K.; Uttamchand, B.D. Primary carcinoma of the fallopian tube: A review of a single institution experience of 8 cases. Sci. World J. 2014, 2014, 630731. [Google Scholar] [CrossRef] [Green Version]
- Trabert, B.; Coburn, S.B.; Mariani, A.; Yang, H.P.; Rosenberg, P.S.; Gierach, G.L.; Wentzensen, N.; Cronin, K.A.; Sherman, M.E. Reported Incidence and Survival of FallopianTube Carcinomas: A Population-Based Analysis from the North American Association of Central Cancer Registries. J. Natl. Cancer Inst. 2018, 110, 750–757. [Google Scholar] [CrossRef]
- Berek, J.S.; Renz, M.; Kehoe, S.; Kumar, L.; Friedlander, M. Cancer of the ovary, fallopiantube, and peritoneum: 2021 update. Int. J. Gynaecol. Obstet. 2021, 155, 61–85. [Google Scholar] [CrossRef]
- Rai, S.; Maheshwari, A. Management of Fallopian Tube Cancer. Rev. Recent Clin. Trials. 2015, 10, 276–281. [Google Scholar] [CrossRef]
- Mladenović–Segedi, L. Primary fallopian tube carcinoma. Med. Pregl. 2009, 62, 31–36. [Google Scholar] [CrossRef] [Green Version]
- Pectasides, D.; Pectasides, E.; Economopoulos, T. Fallopian tube carcinoma: A review. Oncologist 2006, 11, 902–912. [Google Scholar] [CrossRef]
- Nishith, N.; Monappa, V.; Kudva, R. Fallopian Tube Carcinoma In–situ in Endometrial Curettage. Iran. J. Pathol. 2018, 13, 363–367. [Google Scholar] [PubMed]
- Ajithkumar, T.V.; Minimole, A.L.; John, M.M.; Ashokkumar, O.S. Primary fallopian tube carcinoma. Obstet. Gynecol. Surv. 2005, 60, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Kalampokas, E.; Kalampokas, T.; Tourountous, I. Primary fallopian tube carcinoma. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 169, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Ludovisi, M.; De Blasis, I.; Virgilio, B.; Fischerova, D.; Franchi, D.; Pascual, M.A.; Savelli, L.; Epstein, E.; Van Holsbeke, C.; Guerriero, S.; et al. Imaging in gynecological disease (9): Clinical and ultrasound characteristics of tubal cancer. Ultrasound Obstet. Gynecol. 2014, 43, 328–335. [Google Scholar] [CrossRef] [PubMed]
- Balaya, V.; Metzger, U.; Lecuru, F. Ultrasonographic features in the preoperative diagnosis of primitive fallopian tube carcinoma. J. Gynecol. Obstet. Biol. Reprod. 2016, 45, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Haratz–Rubinstein, N.; Russell, B.; Gal, D. Sonographic diagnosis of Fallopian tube carcinoma. Ultrasound Obstet. Gynecol. 2004, 24, 86–88. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Xiao, Z.; Liu, Z.; Lv, F. MRI can be used to differentiate between primary fallopian tube carcinoma and epithelial ovarian cancer. Clin. Radiol. 2020, 75, 457–465. [Google Scholar] [CrossRef]
- Koo, Y.J.; Im, K.S.; Kwon, Y.S.; Lee, I.H.; Kim, T.J.; Lim, K.T.; Lee, K.H.; Shim, J.U.; Mok, J.E. Primary fallopian tube carcinoma: A clinicopathological analysis of a rare entity. Int. J. Clin. Oncol. 2011, 16, 45–49. [Google Scholar] [CrossRef]
- Seong, S.J.; Kim, D.H.; Kim, M.K.; Song, T. Controversies in borderline ovarian tumors. J. Gynecol. Oncol. 2015, 26, 343–349. [Google Scholar] [CrossRef] [Green Version]
- Veloso Gomes, F.; Dias, J.L.; Lucas, R.; Cunha, T.M. Primary fallopian tube carcinoma: Review of MR imaging findings. Insights Imaging 2015, 6, 431–4399. [Google Scholar] [CrossRef] [Green Version]
- Hu, C.Y.; Taymor, M.L.; Hertig, A.T. Primary carcinoma of the fallopian tube. Am. J. Obstet. Gynecol. 1950, 59, 58–67. [Google Scholar] [CrossRef]
- Sedlis, A. Primary carcinoma of the fallopian tube. Obstet. Gynecol. Surv. 1961, 16, 209–222. [Google Scholar] [CrossRef] [PubMed]
- Sedlis, A. Carcinoma of the fallopian tube. Surg. Clin. N. Am. 1978, 58, 121–129. [Google Scholar] [CrossRef]
- Horng, H.C.; Teng, S.W.; Huang, B.S.; Sun, H.D.; Yen, M.S.; Wang, P.H.; Tsui, K.H.; Wen, K.C.; Chen, Y.J.; Chuang, C.M.; et al. Primary fallopian tube cancer: Domestic data and up–to–date review. Taiwan J. Obstet. Gynecol. 2014, 53, 287–292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roze, J.F.; Hoogendam, J.P.; van de Wetering, F.T.; Spijker, R.; Verleye, L.; Vlayen, J.; Veldhuis, W.B.; Scholten, R.J.; Zweemer, R.P. Positron emission tomography (PET) and magnetic resonance imaging (MRI) for assessing tumourresectability in advanced epithelial ovarian/fallopian tube/primary peritoneal cancer. Cochrane Database Syst. Rev. 2018, 10, CD012567. [Google Scholar]
- Sumtsov, D.H.; Gladchuk, I.Z.; Kashtalian, N.M.; Sumtsov, G.O. Practical means of preoperative diagnostics of primaryfallopiantube cancer. Wiad. Lek. 2021, 74, 282–287. [Google Scholar] [CrossRef]
- Zeppernick, F.; Meinhold-Heerlein, I. The new FIGO staging system for ovarian, fallopian tube, and primary peritoneal cancer. Arch. Gynecol. Obstet. 2014, 290, 839–842. [Google Scholar] [CrossRef]
- Jereczek, B.; Jassem, J.; Kobierska, A. Primary cancer of the fallopian tube. Report of 26 patients. Acta Obstet. Gynecol. Scand. 1996, 75, 281–286. [Google Scholar] [CrossRef]
- Stier, E.A.; Barakat, R.R.; Curtin, J.P.; Brown, C.L.; Jones, W.B.; Hoskins, W.J. Laparotomy to complete staging of presumed early ovarian cancer. Obstet. Gynecol. 1996, 87, 737–740. [Google Scholar] [CrossRef]
- Sun, M.; Bao, L.; Shen, H.; Ji, M.; Yao, L.; Yi, X.; Jiang, W. Unexpected primary fallopian tube carcinoma during gynecological operations: Clinicopathological and prognostic factors analyses of 67 cases. Taiwan J. Obstet. Gynecol. 2019, 58, 626–632. [Google Scholar] [CrossRef]
- Bao, L.; Ding, Y.; Cai, Q.; Ning, Y.; Hu, W.; Xue, X.; Sun, H.; Hua, K.; Zhou, X.; Yi, X. Primary Fallopian Tube Carcinoma: A Single–Institution Experience of 101 Cases: A Retrospective Study. Int. J. Gynecol. Cancer 2016, 26, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Cao, L.; Chen, W.; Wang, J.; Wang, W.; Liang, Z. Feasibility of neoadjuvant and adjuvant intraperitoneal chemotherapy in patients with advanced epithelial ovarian cancer: A single-center experience. Medicine 2020, 99, e22100. [Google Scholar] [CrossRef] [PubMed]
- Horng, H.C.; Teng, S.W.; Lai, C.R.; Chang, W.H.; Chang, Y.H.; Yen, M.S.; Wang, P.H.P. Prognostic factors of primary fallopian tube cancer in a single institute in Taiwan. Int. J. Gynaecol. Obstet. 2014, 127, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Manning-Geist, B.; Gockley, A.; Ramos, A.; Sisodia, R.C.; Del Carmen, M.; Growdon, W.B.; Horowitz, N.; Berkowitz, R.; Worley, M., Jr. Use of ablation and ultrasonic aspiration at primary debulking surgery in advanced stage ovarian, fallopiantube, and primary peritoneal cancer. Int. J. Gynecol. Cancer 2020, 30, 1052–1057. [Google Scholar] [CrossRef]
- van Driel, W.J.; Koole, S.N.; Sikorska, K.; van Schagen Leeuwen, J.H.; Schreuder, H.W.R.; Hermans, R.H.M.; de Hingh, I.H.J.T.; van der Velden, J.; Arts, H.J.; Massuger, L.F.A.G.; et al. Hyperthermic Intraperitoneal Chemotherapy in Ovarian Cancer. N. Engl. J. Med. 2018, 378, 230–240. [Google Scholar] [CrossRef]
- Stasenko, M.; Fillipova, O.; Tew, W.P. Fallopian Tube Carcinoma. J. Oncol. Pract. 2019, 15, 375–382. [Google Scholar] [CrossRef]
- Dowson, C.B.; Stewart, C.; O’Sullivan, S.; Pachter, N.; Schofield, L.; Cohen, P.A. Incidence of germline BRCA1/2 mutations in women with tubo-ovarian high-grade serous carcinomas with and without serous tubal intra-epithelial carcinomas. Int. J. Gynecol. Cancer 2020, 30, 94–99. [Google Scholar] [CrossRef]
- Stearnes, G.; Nichols, C.B.; Schofield, L.; O’Sullivan, S.; Pachter, N.; Cohen, P.A. Uptake of testing for germline BRCA mutations in patients with non-mucinous epithelial ovarian cancers in Western Australia: A comparison of different genetic counseling methods. Int. J. Gynecol. Cancer 2019, 29, 1038–1042. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thanasa, E.; Stamouli, D.; Gerokostas, E.-E.; Balafa, K.; Koutalia, N.; Thanasas, I. Primary Fallopian Tube Carcinoma: An Extremely Rare Gynecological Cancer Misdiagnosed Intraoperatively as Benign Ovarian Neoplasm: A Case Report. Clin. Pract. 2022, 12, 253-260. https://doi.org/10.3390/clinpract12030030
Thanasa E, Stamouli D, Gerokostas E-E, Balafa K, Koutalia N, Thanasas I. Primary Fallopian Tube Carcinoma: An Extremely Rare Gynecological Cancer Misdiagnosed Intraoperatively as Benign Ovarian Neoplasm: A Case Report. Clinics and Practice. 2022; 12(3):253-260. https://doi.org/10.3390/clinpract12030030
Chicago/Turabian StyleThanasa, Efthymia, Dimitra Stamouli, Ektoras-Evangelos Gerokostas, Konstantina Balafa, Nikoleta Koutalia, and Ioannis Thanasas. 2022. "Primary Fallopian Tube Carcinoma: An Extremely Rare Gynecological Cancer Misdiagnosed Intraoperatively as Benign Ovarian Neoplasm: A Case Report" Clinics and Practice 12, no. 3: 253-260. https://doi.org/10.3390/clinpract12030030
APA StyleThanasa, E., Stamouli, D., Gerokostas, E.-E., Balafa, K., Koutalia, N., & Thanasas, I. (2022). Primary Fallopian Tube Carcinoma: An Extremely Rare Gynecological Cancer Misdiagnosed Intraoperatively as Benign Ovarian Neoplasm: A Case Report. Clinics and Practice, 12(3), 253-260. https://doi.org/10.3390/clinpract12030030





