Zinner Syndrome—A Rare Cause of Recurrent Epididymitis and Infertility
Abstract
:1. Introduction
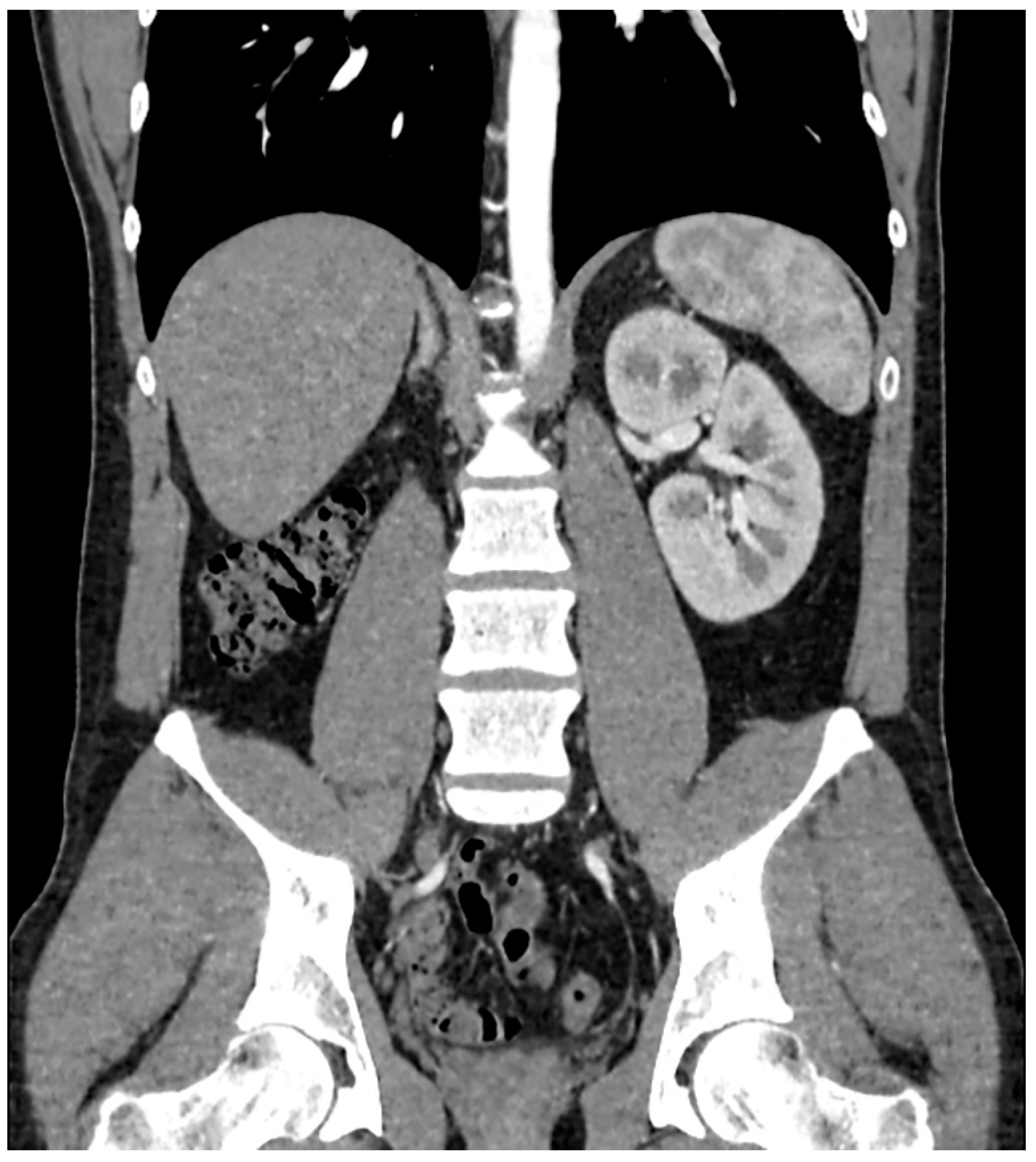
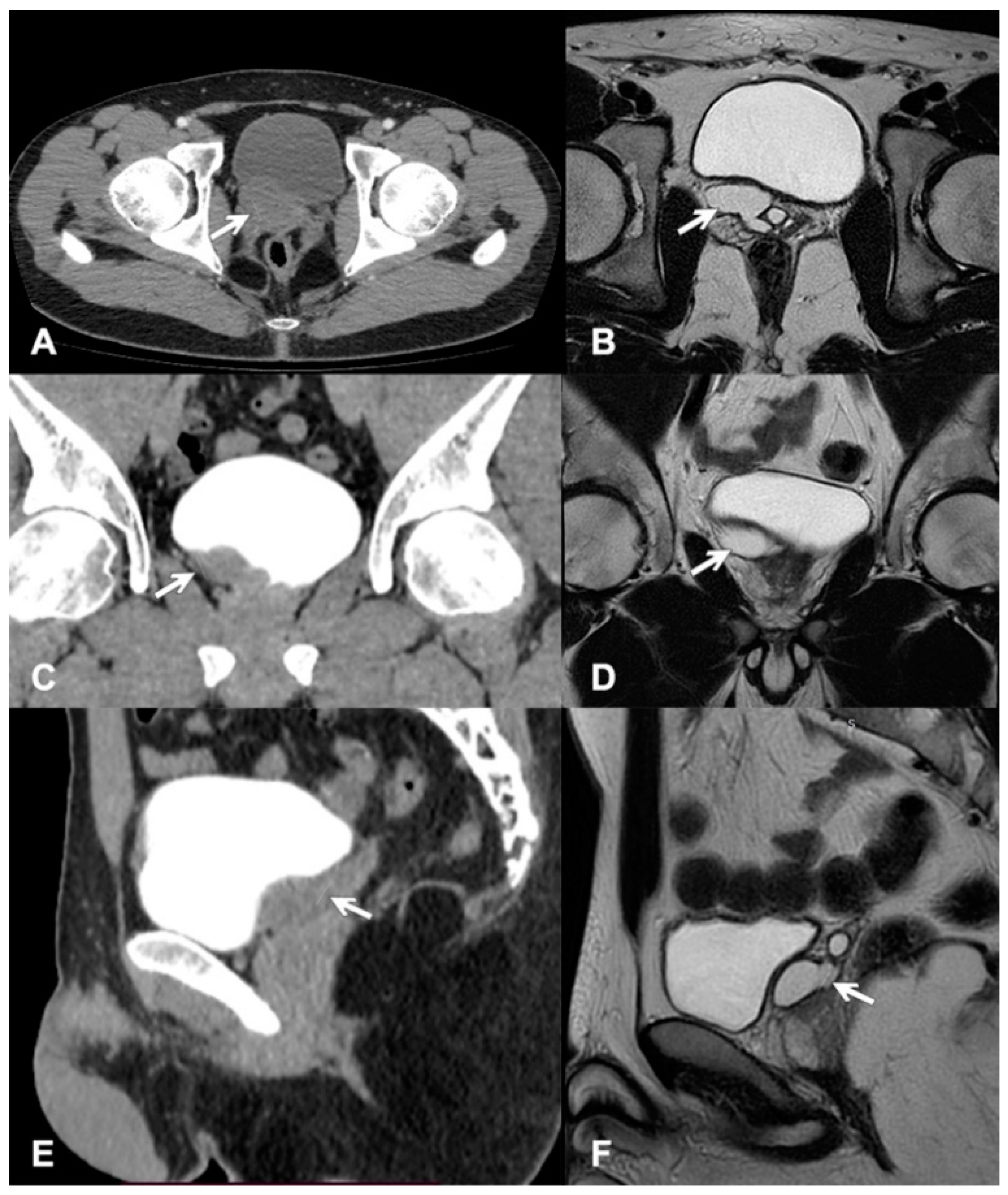
2. Case Report
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Slaoui, A.; Regragui, S.; Lasri, A.; Karmouni, T.; El Khader, K.; Koutani, A.; Ibn Attya, A. Zinner’s syndrome: Report of two cases and review of the literature. Basic Clin. Androl. 2016, 26, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Militaru, V.; Mihaly, Z.A.; Ilea, C.; Coman, M.; Stanciu, M.; Crisan, N.; Coman, I. Zinner syndrome—Case report. Med. Pharm. Rep. 2021, 94, S47–S50. [Google Scholar] [CrossRef] [PubMed]
- Karki, P.; Manandhar, S.; Kharel, A. A rare case of Zinner syndrome: Triad of unilateral renal agenesis, ipsilateral seminal vesicle cyst and ejaculatory duct obstruction. Radiol. Case Rep. 2021, 16, 3380–3382. [Google Scholar] [CrossRef] [PubMed]
- Kori, R.; Bains, L.; Lal, P.; Gupta, S. Zinner syndrome mimicking bladder outlet obstruction managed with aspiration. Urol. Ann. 2019, 11, 449–452. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Li, X.; Huang, L.; Li, H.; Cai, K.; Jiang, J.; Chen, N.; Zhang, W.; Tang, J.; Zhang, M.; et al. Zinner syndrome: An updated pooled analysis based on 214 cases from 1999 to 2020: Systematic review. Ann. Palliat. Med. 2021, 10, 2271–2282. [Google Scholar] [CrossRef] [PubMed]
- Di Paola, V.; Gigli, R.; Totaro, A.; Manfredi, R. Zinner syndrome: Two cases and review of the literature. BMJ Case Rep. 2021, 14, e243002. [Google Scholar] [CrossRef] [PubMed]
- Cito, G.; Sforza, S.; Gemma, L.; Cocci, A.; Di Maida, F.; Dabizzi, S.; Natali, A.; Minervini, A.; Carini, M.; Masieri, L. Infertility case presentation in Zinner syndrome: Can a long-lasting seminal tract obstruction cause secretory testicular injury? Andrologia 2019, 51, 2–7. [Google Scholar] [CrossRef] [PubMed]
- Galosi, A.B.; Montironi, R.; Fabiani, A.; Lacetera, V.; Gallé, G.; Muzzonigro, G. Cystic Lesions of the Prostate Gland: An Ultrasound Classification With Pathological Correlation. J. Urol. 2009, 181, 647–657. [Google Scholar] [CrossRef] [PubMed]
- Demaeyer, L.; Holz, S.; Pamart, D.; Taylor, S.; Naudin, M. Robotic management of painful Zinner syndrome, case report and review of literature. Int. J. Surg. Case Rep. 2020, 73, 61–64. [Google Scholar] [CrossRef] [PubMed]
| Variable | Patient Value | Cut-Off Value |
|---|---|---|
| Sperm volume | 4.0 mL | >1.5 mL |
| Sperm concentration | 3.8 milion/mL | >15 milion/mL |
| Total number | 15.4 milion/mL | >39 milion/mL |
| Sperm total movement | 5.9% | ≥40% |
| Sperm progressive motility (A + B) | 4.7% | >32% |
| Sperm morphology (correct) | 1% | >4% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ostrowska, M.; Grześk, M.; Kaczyński, S.; Skwara, D.; Kulik, K.; Kowalski, F.; Ostrowski, A.; Drewa, T. Zinner Syndrome—A Rare Cause of Recurrent Epididymitis and Infertility. Clin. Pract. 2021, 11, 942-946. https://doi.org/10.3390/clinpract11040108
Ostrowska M, Grześk M, Kaczyński S, Skwara D, Kulik K, Kowalski F, Ostrowski A, Drewa T. Zinner Syndrome—A Rare Cause of Recurrent Epididymitis and Infertility. Clinics and Practice. 2021; 11(4):942-946. https://doi.org/10.3390/clinpract11040108
Chicago/Turabian StyleOstrowska, Magdalena, Magdalena Grześk, Szymon Kaczyński, Dominika Skwara, Kacper Kulik, Filip Kowalski, Adam Ostrowski, and Tomasz Drewa. 2021. "Zinner Syndrome—A Rare Cause of Recurrent Epididymitis and Infertility" Clinics and Practice 11, no. 4: 942-946. https://doi.org/10.3390/clinpract11040108
APA StyleOstrowska, M., Grześk, M., Kaczyński, S., Skwara, D., Kulik, K., Kowalski, F., Ostrowski, A., & Drewa, T. (2021). Zinner Syndrome—A Rare Cause of Recurrent Epididymitis and Infertility. Clinics and Practice, 11(4), 942-946. https://doi.org/10.3390/clinpract11040108





