Quality of Life among Pediatric Neurocognitive, Speech, and Psychomotor Rehabilitation Professionals during the COVID-19 Pandemic: A Longitudinal Study on an Italian Sample
Abstract
:1. Introduction
2. Materials and Methods
- (i).
- Working in public or accredited private rehabilitation centers for neuropsychiatric disorders of childhood;
- (ii).
- Giving the informed consent.
- (i).
- No informed consent;
- (ii).
- Not working in public or accredited private rehabilitation centers for neuropsychiatric disorders of childhood.
2.1. Measures
- I.
- How is your health in general? (Excellent, Very good, Good, Fair, or Poor).
- II.
- Now, thinking about your physical health, which includes physical illness and injury, how many days during the past 30 days was your physical health not good?
- III.
- Now, thinking about your mental health, which includes stress, depression, and problems with emotions, how many days during the past 30 days was your mental health not good?
- IV.
- Now, thinking about your usual activities. During the past 30 days, approximately how many days did poor physical or mental health keep you from doing your usual activities, such as self-care, work, or recreation?
2.2. Outcomes
2.3. Statistical Analysis
3. Results
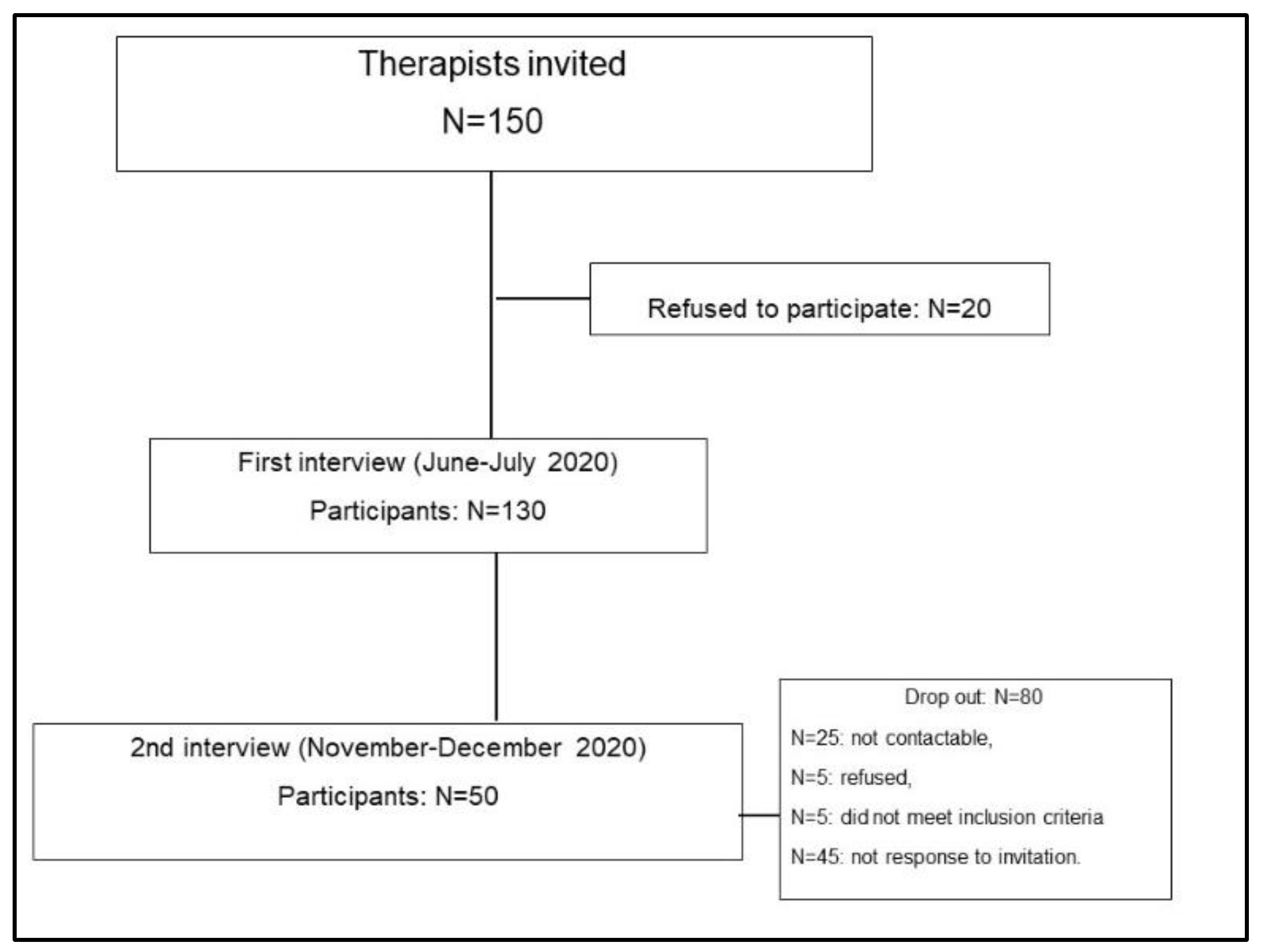
3.1. Inclusion/Exclusion Results
3.2. Characteristics of Participants
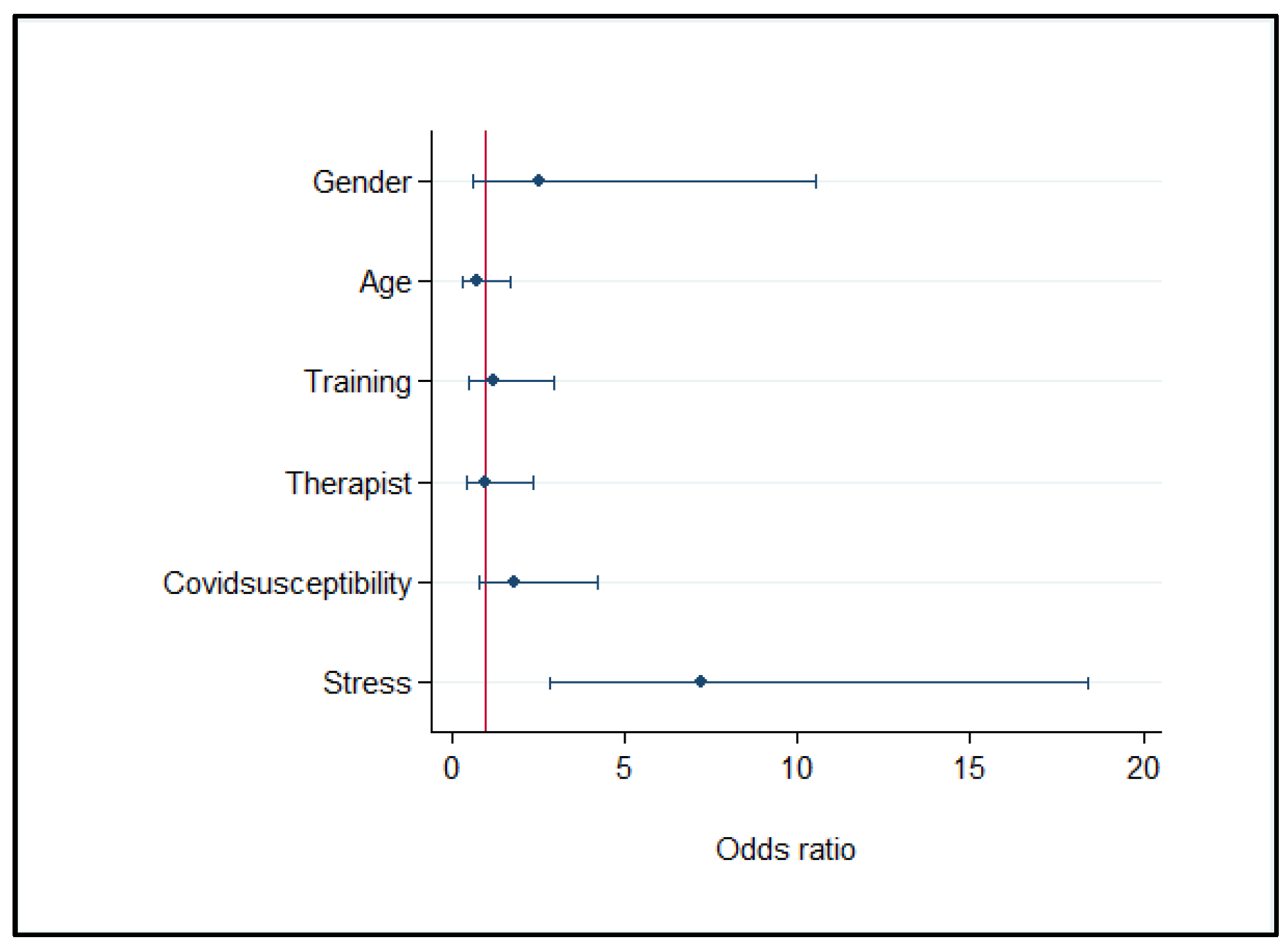
3.3. Survey Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Muselli, M.; Cofini, V.; Desideri, G.; Necozione, S. Coronavirus (COVID-19) pandemic: How may communication strategies influence our behaviours? Int. J. Disaster Risk Reduct. 2021, 53, 101982. [Google Scholar] [CrossRef]
- Muselli, M.; Cofini, V.; Mammarella, L.; Carmignani, C.; Fabiani, L.; Desideri, G.; Necozione, S. The impact of COVID-19 pandemic on emergency services. Ann. Ig. Med. Prev. Comunita 2021. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Manuli, A.; Naro, A.; Rao, G. How COVID 19 has changed Neurorehabilitation in Italy: A critical appraisal. Acta Biomed. 2020, 91, e2020143. [Google Scholar] [CrossRef]
- Documento Tecnico Sulla Possibile Rimodulazione Delle Misure di Contenimento del Contagio da COVID-19 nei Luoghi di Lavoro e Strategie di Prevenzione. 2020. Available online: https://www.inail.it/cs/internet/comunicazione/pubblicazioni/catalogo-generale/pubbl-rimodulazione-contenimento-COVID19-sicurezza-lavoro.html (accessed on 21 April 2021).
- Reilly, S.E.; Soulliard, Z.A.; McCuddy, W.T.; Mahoney, J.J. Frequency and perceived effectiveness of mental health providers’ coping strategies during COVID-19. Curr. Psychol. 2021, 1–10. [Google Scholar] [CrossRef]
- Labrague, L.J.; de los Santos, J.A.A. COVID-19 anxiety among front-line nurses: Predictive role of organisational support, per-sonal resilience and social support. J. Nurs. Manag. 2020, 28, 1653–1661. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.; Goldberg, S.B.; Lin, D.; Qiao, S.; Operario, D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. Glob. Health 2021, 17, 15. [Google Scholar] [CrossRef] [PubMed]
- Dolić, M.; Antičević, V.; Dolić, K.; Pogorelić, Z. Questionnaire for Assessing Social Contacts of Nurses Who Worked with Coronavirus Patients during the First Wave of the COVID-19 Pandemic. Health 2021, 9, 930, PMCID:PMC8391600. [Google Scholar] [CrossRef] [PubMed]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatry 2020, 52, 102066. [Google Scholar] [CrossRef]
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef] [Green Version]
- Pfefferbaum, B.; North, C.S. Mental Health and the COVID-19 Pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Feng, X.L.; Wang, X.H.; Van Ijzendoorn, M.H. Coping with COVID-19: Exposure to COVID-19 and Negative Impact on Livelihood Predict Elevated Mental Health Problems in Chinese Adults. Int. J. Environ. Res. Public Health 2020, 17, 3857. [Google Scholar] [CrossRef]
- Pearman, A.; Hughes, M.; Smith, E.L.; Neupert, S.D. Mental Health Challenges of United States Healthcare Professionals During COVID-19. Front. Psychol. 2020, 11, 2065, PMCID:PMC7438566. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, N.; Docherty, M.; Gnanapragasam, S.; Wessely, S. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ 2020, 368, m1211. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Yang, L.; Zhang, C.; Xiang, Y.-T.; Liu, Z.; Hu, S.; Zhang, B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e17–e18. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, C.; Pan, W.; Zheng, J.; Gao, J.; Huang, X.; Cai, S.; Zhai, Y.; Latour, J.M.; Zhu, C. Stress, Burnout, and Coping Strategies of Frontline Nurses During the COVID-19 Epidemic in Wuhan and Shanghai, China. Front. Psychiatry 2020, 11, 565520. [Google Scholar] [CrossRef]
- Rivas, N.; López, M.; Castro, M.-J.; Luis-Vian, S.; Fernández-Castro, M.; Cao, M.-J.; García, S.; Velasco-Gonzalez, V.; Jiménez, J.-M. Analysis of Burnout Syndrome and Resilience in Nurses throughout the COVID-19 Pandemic: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 10470, PMCID:PMC8508575. [Google Scholar] [CrossRef] [PubMed]
- Bruschini, M.; Carli, A.; Burla, F. Burnout and Work-related Stress in Italian Rehabilitation Professionals: A Comparison of Physiotherapists, Speech Therapists and Occupational Therapists. Work 2018, 59, 121–129. [Google Scholar] [CrossRef]
- Farì, G.; de Sire, A.; Giorgio, V.; Rizzo, L.; Bruni, A.; Bianchi, F.P.; Zonno, A.; Pierucci, P.; Ranieri, M.; Megna, M. Impact of COVID-19 on the mental health in a cohort of Italian rehabilitation healthcare workers. J. Med. Virol. 2021, 1–9. [Google Scholar] [CrossRef]
- Taddei, M.; Bulgheroni, S. Facing the real time challenges of the COVID-19 emergency for child neuropsychology service in Milan. Res. Dev. Disabil. 2020, 107, 103786, PMCID:PMC7510541. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, R.; Dubey, M.J.; Chatterjee, S.; Dubey, S. Impact of COVID-19 on children: Special focus on the psychosocial aspect. Minerva Pediatr. 2020, 72, 226–235. [Google Scholar] [CrossRef]
- Bova, S.M.; Basso, M.; Bianchi, M.F.; Savaré, L.; Ferrara, G.; Mura, E.; Redaelli, M.G.; Olivieri, I.; Veggiotti, P.; Milan COVID-19; et al. Impact of COVID-19 lockdown in children with neurological disorders in Italy. Disabil. Health J. 2021, 14, 101053. [Google Scholar] [CrossRef]
- Gigantesco, A.; D’Argenio, P.; Cofini, V.; Mancini, C.; Minardi, V. Health-Related Quality of Life in the Aftermath of the L’Aquila Earthquake in Italy. Disaster Med. Public Health Prep. 2016, 10, 11–15. [Google Scholar] [CrossRef]
- Minardi, V.; Gigantesco, A.; Mancini, C.; Quarchioni, E.; D’Argenio, P.; Cofini, V. Fattori di rischio comportamentali all’Aquila 3-5 anni dopo il terremoto del 2009. Epidemiol. Prev. 2016, 40, 34–41. [Google Scholar]
- Gigantesco, A.; Mirante, N.; Granchelli, C.; Diodati, G.; Cofini, V.; Mancini, C.; Carbonelli, A.; Tarolla, E.; Minardi, V.; Salmaso, S.; et al. Psychopathological chronic sequelae of the 2009 earthquake in L’Aquila, Italy. J. Affect. Disord. 2013, 148, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Measuring Healthy Days; CDC: Atlanta, GA, USA, 2000. Available online: https://www.cdc.gov/hrqol/pdfs/mhd.pdf (accessed on 9 November 2021).
- ECOM Project. Available online: http://ecomeu.info/ecom-project/ (accessed on 2 March 2020).
- Goldberg, D.P.; Williams, P. A User’s Guide to the General Health Questionnaire; NFER-Nelson: Windsor, ON, Canada, 1998. [Google Scholar]
- Ryali, S.; Kumar, A.; Bhat, P.S. Study of quality of life among health workers and psychosocial factors influencing it. Ind. Psychiatry J. 2018, 27, 96–102, PMCID:PMC6198596. [Google Scholar] [CrossRef] [PubMed]
- L’epidemiologia per la Sanità Pubblica. Available online: https://www.epicentro.iss.it/passi/dati/PercezioneSalute (accessed on 28 July 2021).
- Ruiz-Fernández, M.D.; Ortega-Galán, Á.M.; Fernández-Sola, C.; Hernández-Padilla, J.M.; Granero-Molina, J.; Ramos-Pichardo, J.D. Occupational Factors Associated with Health-Related Quality of Life in Nursing Professionals: A Multi-Centre Study. Int. J. Environ. Res. Public Health 2020, 17, 982, PMCID:PMC7038014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romero-Ayuso, D.; Alcántara-Vázquez, P.; Almenara-García, A.; Nuñez-Camarero, I.; Triviño-Juárez, J.M.; Ariza-Vega, P.; Molina, J.-P.; González, P. Self-Regulation in Children with Neurodevelopmental Disorders “SR-MRehab: Un Colegio Emocionante”: A Protocol Study. Int. J. Environ. Res. Public Health 2020, 17, 4198. [Google Scholar] [CrossRef]
- Chiang, Y.-M.; Kuo, M.-L.; Wang, S.-H.; Huang, S.; Lee, I.-C. The Association of the Disturbed Degree of Job Stressful Events, Physical Data and Quality of Life in Allied Personnel of Outpatient Department. Hu Li Za Zhi J. Nurs. 2016, 63, 68–77. [Google Scholar]
- Lan, Y.L.; Lin, Y.C.; Yan, Y.H.; Tang, Y.P. Relationship between Work Stress, Workload, and Quality of Life among Rehabilitation Professionals. Int. J. Healthc. Med. Sci. 2018, 4, 105–110. [Google Scholar]
- Man, M.A.; Toma, C.; Motoc, N.S.; Necrelescu, O.L.; Bondor, C.I.; Chis, A.F.; Lesan, A.; Pop, C.M.; Todea, D.A.; Dantes, E.; et al. Disease Perception and Coping with Emotional Distress During COVID-19 Pandemic: A Survey Among Medical Staff. Int. J. Environ. Res. Public Health 2020, 17, 4899, PMCID:PMC7369835. [Google Scholar] [CrossRef] [PubMed]
- Danet, A.D. Psychological impact of COVID-19 pandemic in Western frontline healthcare professionals. A systematic review. Med. Clínica 2021, 156, 449–458, PMCID:PMC7972644. [Google Scholar] [CrossRef] [PubMed]
- Buzzi, N. Rapporto Sanità 2019—Il Personale Dipendente Delle Aziende Sanitarie Pubbliche; Nebo Ricerche PA: Rome, Italy, 2019. [Google Scholar]
- Trumello, C.; Bramanti, S.M.; Ballarotto, G.; Candelori, C.; Cerniglia, L.; Cimino, S.; Crudele, M.; Lombardi, L.; Pignataro, S.; Viceconti, M.L.; et al. Psychological Adjustment of Healthcare Workers in Italy during the COVID-19 Pandemic: Differences in Stress, Anxiety, Depression, Burnout, Secondary Trauma, and Compassion Satisfaction between Frontline and Non-Frontline Professionals. Int. J. Environ. Res. Public Health 2020, 17, 8358, PMCID:PMC7696387. [Google Scholar] [CrossRef] [PubMed]
- de Leeuw, E.D.; Lugtig, P. Dropouts in Longitudinal Surveys. Wiley StatsRef Stat. Ref. Online 2015, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Cai, C.Z.; Lin, Y.-L.; Hu, Z.-J.; Wong, L.P. Psychological and mental health impacts of COVID-19 pandemic on healthcare workers in China: A review. World J. Psychiatry 2021, 11, 337–346, PMCID:PMC8311517. [Google Scholar] [CrossRef] [PubMed]
- Marinaccio, A.; Boccuni, F.; Rondinone, B.M.; Brusco, A.; D’Amario, S.; Iavicoli, S. Occupational factors in the COVID-19 pandemic in Italy: Compensation claims applications support establishing an occupational surveillance system. Occup. Environ. Med. 2020, 77, 818–821. [Google Scholar] [CrossRef]
| Characteristics | 1st Interview (June–July 2020) n = 130 | 2nd Interview (November to December 2020) n = 50 |
|---|---|---|
| Mean (SD) or n (%) | Mean (SD) or n (%) | |
| Age (years) | 36 (10.5) | 41 (10.8) |
| Gender | - | - |
| Female | 116 (89%) | 37 (74%) |
| Male | 14 (11%) | 13 (26%) |
| Residence | - | - |
| Northern Italy | 35 (27%) | 4 (8%) |
| Central Italy | 59 (45%) | 24 (48%) |
| Southern Italy | 36 (28%) | 22 (44%) |
| Civil status | - | - |
| Married | 50 (38%) | 23 (46%) |
| Civil partner | 17 (13%) | 9 (18%) |
| Divorced | 6 (5%) | 2 (4%) |
| Single | 57 (44%) | 16 (32%) |
| Health rehabilitation category | - | - |
| Speech therapy | 31 (22%) | 7 (14%) |
| Psychology | 47 (36%) | 33 (66%) |
| Neuro-psychomotricity | 82 (42%) | 10 (20%) |
| Training on COVID-19 | - | - |
| Yes | 93 (71%) | 42 (84%) |
| No | 37 (29%) | 8 (16%) |
| Variables | 1st Interview n = 130 | 2nd Interview n = 50 |
|---|---|---|
| Mean (SD) or n (%) (95% CI) | Mean (SD) or n (%) (95% CI) | |
| How is your health in general? | ||
| Excellent | 53 (41) (33–50) | 16 (32) (20–46) |
| Good or very good | 76 (58) (49–67) | 33 (66) (51–78) |
| Fair or Poor | 1 (1) (0.1–5) | 1 (2) (0.2–13.7) |
| Physical unhealthy days | 2.4 (5) (1.7–3.1) | 1.5 (2) (0.4–2.7) |
| Mental unhealthy days | 6 (5) (4.7–7.3) | 4.3 (1) (2.2–6.3) |
| Unhealthy days with activity limitation | 2 (3) (1.7–2.8) | 1 (2) (1.0–2.4) |
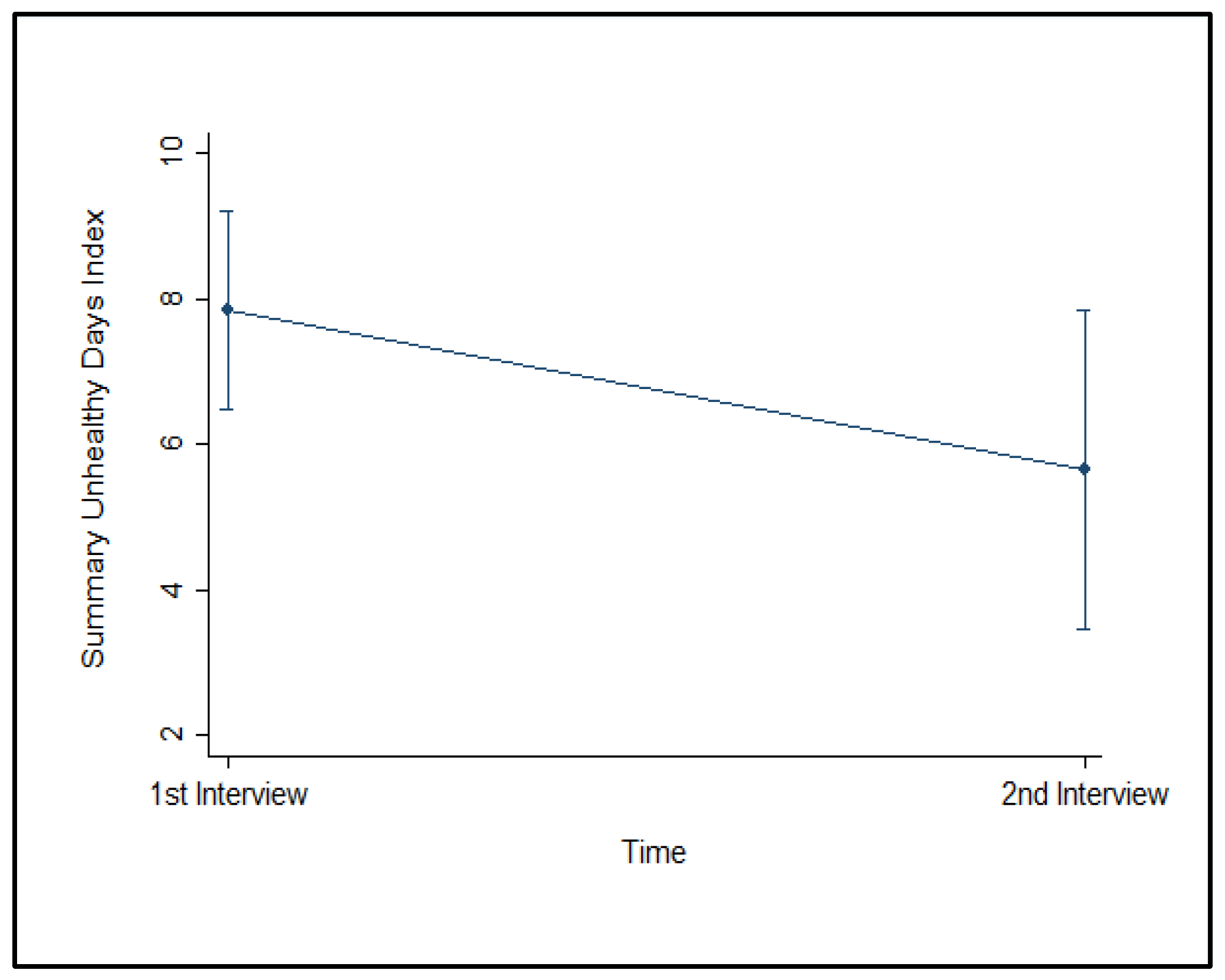
| Summary Unhealthy Days Index | 8 (9) (7–10) | 6 (6) (4–8) |
| Perception of susceptibility to COVID-19 | 4 (0.9) (3.9–4.2) | 4.3 (0.7) (4–4.5) |
| Perceived stress (GH-12 score) | 18.7 (3.6) (18.1–19.3) | 19.8 (3.2) (18.1–20.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cofini, V.; Bianchini, V.; Muselli, M.; Budroni, D.; Tobia, L.; Calò, G.L.; Fabiani, L.; Necozione, S. Quality of Life among Pediatric Neurocognitive, Speech, and Psychomotor Rehabilitation Professionals during the COVID-19 Pandemic: A Longitudinal Study on an Italian Sample. Clin. Pract. 2021, 11, 860-869. https://doi.org/10.3390/clinpract11040101
Cofini V, Bianchini V, Muselli M, Budroni D, Tobia L, Calò GL, Fabiani L, Necozione S. Quality of Life among Pediatric Neurocognitive, Speech, and Psychomotor Rehabilitation Professionals during the COVID-19 Pandemic: A Longitudinal Study on an Italian Sample. Clinics and Practice. 2021; 11(4):860-869. https://doi.org/10.3390/clinpract11040101
Chicago/Turabian StyleCofini, Vincenza, Valeria Bianchini, Mario Muselli, Danila Budroni, Loreta Tobia, Giovanna Letizia Calò, Leila Fabiani, and Stefano Necozione. 2021. "Quality of Life among Pediatric Neurocognitive, Speech, and Psychomotor Rehabilitation Professionals during the COVID-19 Pandemic: A Longitudinal Study on an Italian Sample" Clinics and Practice 11, no. 4: 860-869. https://doi.org/10.3390/clinpract11040101
APA StyleCofini, V., Bianchini, V., Muselli, M., Budroni, D., Tobia, L., Calò, G. L., Fabiani, L., & Necozione, S. (2021). Quality of Life among Pediatric Neurocognitive, Speech, and Psychomotor Rehabilitation Professionals during the COVID-19 Pandemic: A Longitudinal Study on an Italian Sample. Clinics and Practice, 11(4), 860-869. https://doi.org/10.3390/clinpract11040101






