Diagnostic Algorithm in Patients with Flexion Instability after Cruciate-Retaining Total Knee Arthroplasty: A Case Report
Abstract
:1. Introduction
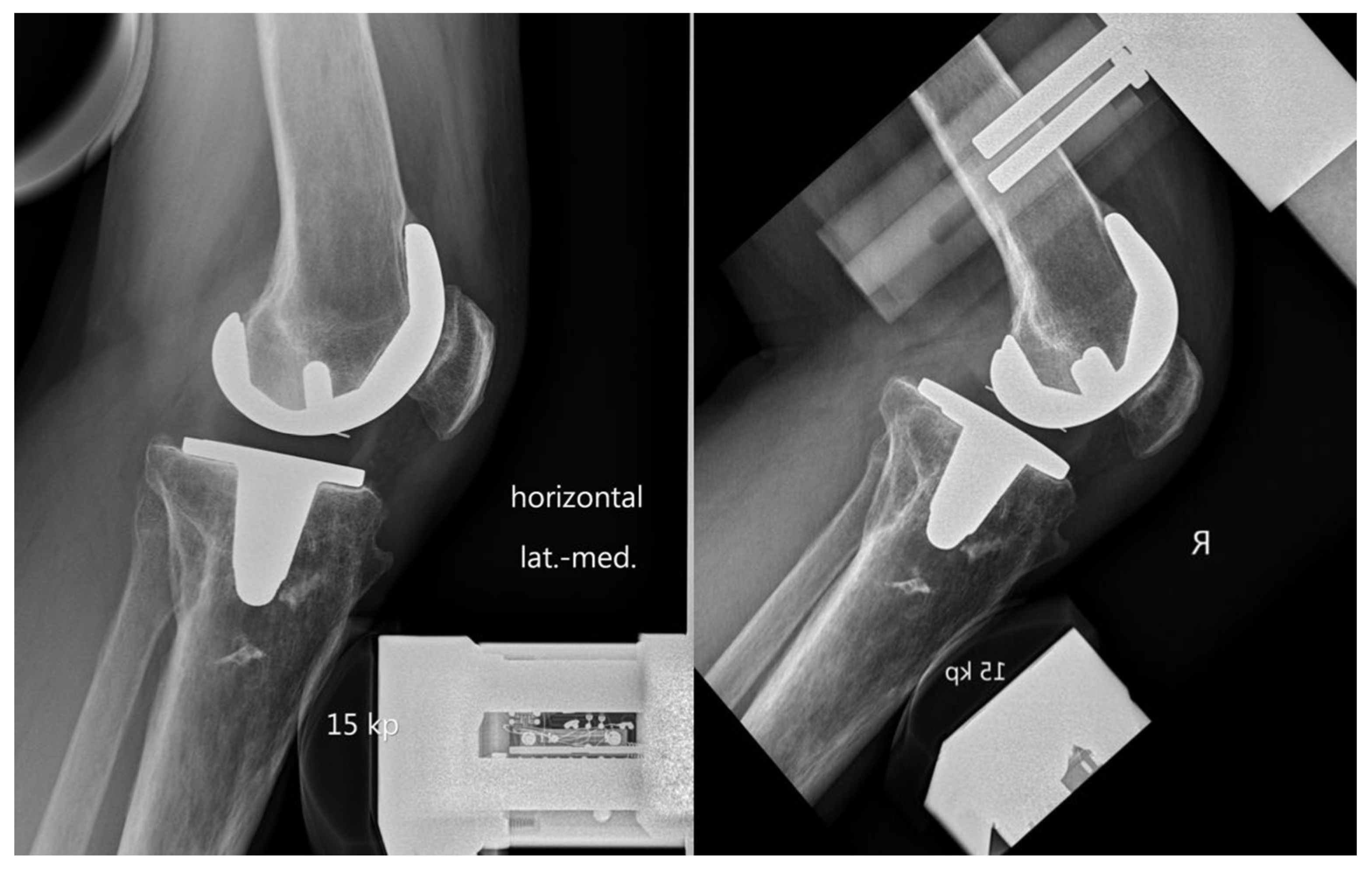
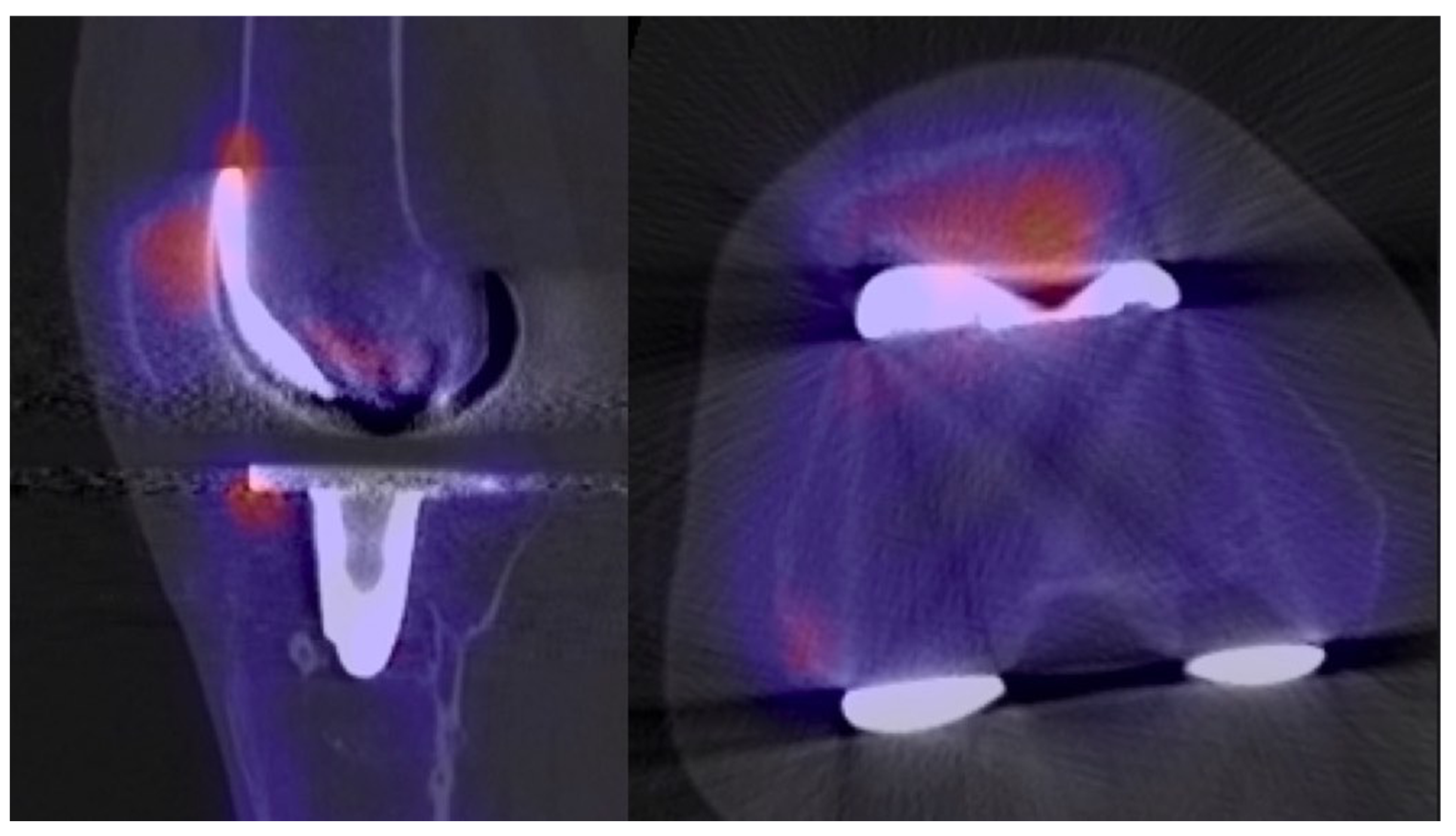
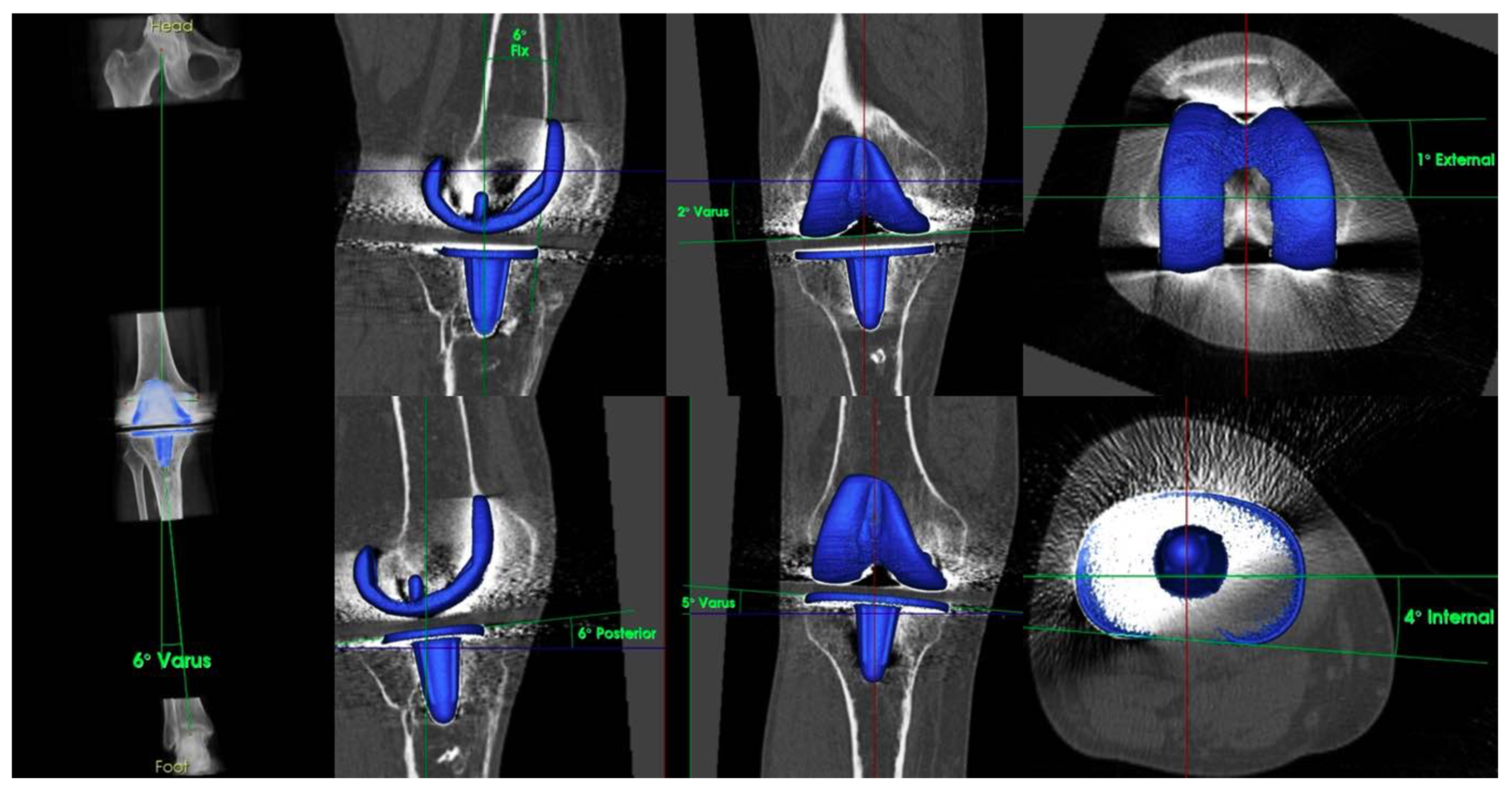
2. Case Report
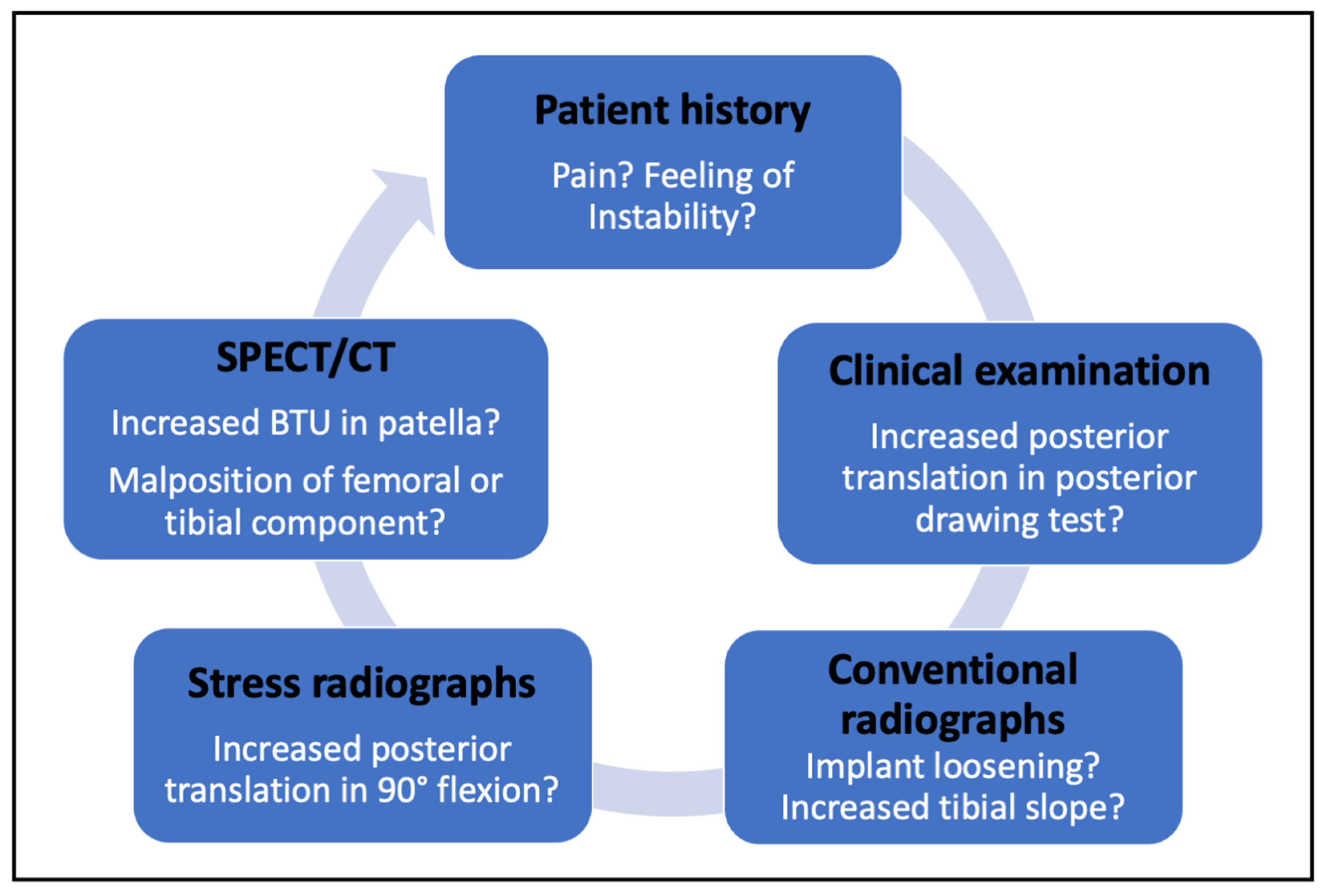
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Becker, R.; Bonnin, M.; Hofmann, S. The Painful Knee after Total Knee Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1409–1410. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonzalez, M.H.; Mekhail, A.O. The Failed Total Knee Arthroplasty: Evaluation and Etiology. J. Am. Acad. Orthop. Surg. 2004, 12, 436–446. [Google Scholar] [CrossRef] [PubMed]
- Parratte, S.; Pagnano, M.W. Instability after Total Knee Arthroplasty. J. Bone Jt. Surg. Am. 2008, 90, 184–194. [Google Scholar]
- Wood, A.R.; Rabbani, T.A.; Sheffer, B.; Wagner, R.A.; Sanchez, H.B. Protecting the PCL During Total Knee Arthroplasty Using a Bone Island Technique. J. Arthroplast. 2018, 33, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Hirschmann, M.T.; Konala, P.; Iranpour, F.; Kerner, A.; Rasch, H.; Friederich, N.F. Clinical Value of SPECT/CT for Evaluation of Patients with Painful Knees after Total Knee Arthroplasty—A New Dimension of Diagnostics? BMC Musculoskelet. Disord. 2011, 12, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montgomery, R.L.; Goodman, S.B.; Csongradi, J. Late Rupture of the Posterior Cruciate Ligament after Total Knee Replacement. Iowa Orthop. J. 1993, 13, 167–170. [Google Scholar] [PubMed]
- Pagnano, M.W.; Hanssen, A.D.; Lewallen, D.G.; Stuart, M.J. Flexion Instability after Primary Posterior Cruciate Retaining Total Knee Arthroplasty. Clin. Orthop. Relat. Res. 1998, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Waslewski, G.L.; Marson, B.M.; Benjamin, J.B. Early, Incapacitating Instability of Posterior Cruciate Ligament-Retaining Total Knee Arthroplasty. J. Arthroplast. 1998, 13, 763–767. [Google Scholar] [CrossRef]
- Murer, M.; Falkowski, A.L.; Hirschmann, A.; Amsler, F.; Hirschmann, M.T. Threshold Values for Stress Radiographs in Unstable Knees after Total Knee Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2020, 29, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Pagnano, M.W.; Cushner, F.D.; Scott, W.N. Role of the Posterior Cruciate Ligament in Total Knee Arthroplasty. J. Am. Acad. Orthop. Surg 1998, 6, 176–187. [Google Scholar] [CrossRef] [PubMed]
- Israel, O.; Pellet, O.; Biassoni, L.; De Palma, D.; Estrada-Lobato, E.; Gnanasegaran, G.; Kuwert, T.; la Fougère, C.; Mariani, G.; Massalha, S.; et al. Two Decades of SPECT/CT—the Coming of Age of a Technology: An Updated Review of Literature Evidence. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 1990–2012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirschmann, M.T.; Schön, S.; Afifi, F.K.; Amsler, F.; Rasch, H.; Friederich, N.F.; Arnold, M.P. Assessment of Loading History of Compartments in the Knee Using Bone SPECT/CT: A Study Combining Alignment and 99mTc-HDP Tracer Uptake/Distribution Patterns. J. Orthop. Res. 2013, 31, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Mucha, A.; Dordevic, M.; Hirschmann, A.; Rasch, H.; Amsler, F.; Arnold, M.P.; Hirschmann, M.T. Effect of High Tibial Osteotomy on Joint Loading in Symptomatic Patients with Varus Aligned Knees: A Study Using SPECT/CT. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 2315–2323. [Google Scholar] [CrossRef] [PubMed]
- Mathis, D.T.; Hirschmann, A.; Falkowski, A.L.; Kiekara, T.; Amsler, F.; Rasch, H.; Hirschmann, M.T. Increased Bone Tracer Uptake in Symptomatic Patients with ACL Graft Insufficiency: A Correlation of MRI and SPECT/CT Findings. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 563–573. [Google Scholar] [CrossRef] [PubMed]
- Slevin, O.; Schmid, F.A.; Schiapparelli, F.-F.; Rasch, H.; Amsler, F.; Hirschmann, M.T. Coronal Femoral TKA Position Significantly Influences in Vivo Patellar Loading in Unresurfaced Patellae after Primary Total Knee Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3605–3610. [Google Scholar] [CrossRef] [PubMed]
- Moser, L.B.; Mandegaran, R.; Hess, S.; Amsler, F.; Rasch, H.; Hirschmann, M.T. Increased Focal Bone Tracer Uptake at the Popliteus Muscle Origin in Primary TKA Compared with Revision TKA. Skelet. Radiol. 2020, 49, 1127–1133. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moser, L.B.; Prabhakar, P.; Hess, S.; Hirschmann, M.T. Diagnostic Algorithm in Patients with Flexion Instability after Cruciate-Retaining Total Knee Arthroplasty: A Case Report. Clin. Pract. 2021, 11, 687-693. https://doi.org/10.3390/clinpract11030084
Moser LB, Prabhakar P, Hess S, Hirschmann MT. Diagnostic Algorithm in Patients with Flexion Instability after Cruciate-Retaining Total Knee Arthroplasty: A Case Report. Clinics and Practice. 2021; 11(3):687-693. https://doi.org/10.3390/clinpract11030084
Chicago/Turabian StyleMoser, Lukas B., Ponnaian Prabhakar, Silvan Hess, and Michael T. Hirschmann. 2021. "Diagnostic Algorithm in Patients with Flexion Instability after Cruciate-Retaining Total Knee Arthroplasty: A Case Report" Clinics and Practice 11, no. 3: 687-693. https://doi.org/10.3390/clinpract11030084
APA StyleMoser, L. B., Prabhakar, P., Hess, S., & Hirschmann, M. T. (2021). Diagnostic Algorithm in Patients with Flexion Instability after Cruciate-Retaining Total Knee Arthroplasty: A Case Report. Clinics and Practice, 11(3), 687-693. https://doi.org/10.3390/clinpract11030084




