Doubly Blinded: An Uncommon Cause of Acute Visual Loss Due to Orbital Compartment Syndrome
Abstract
:1. Introduction
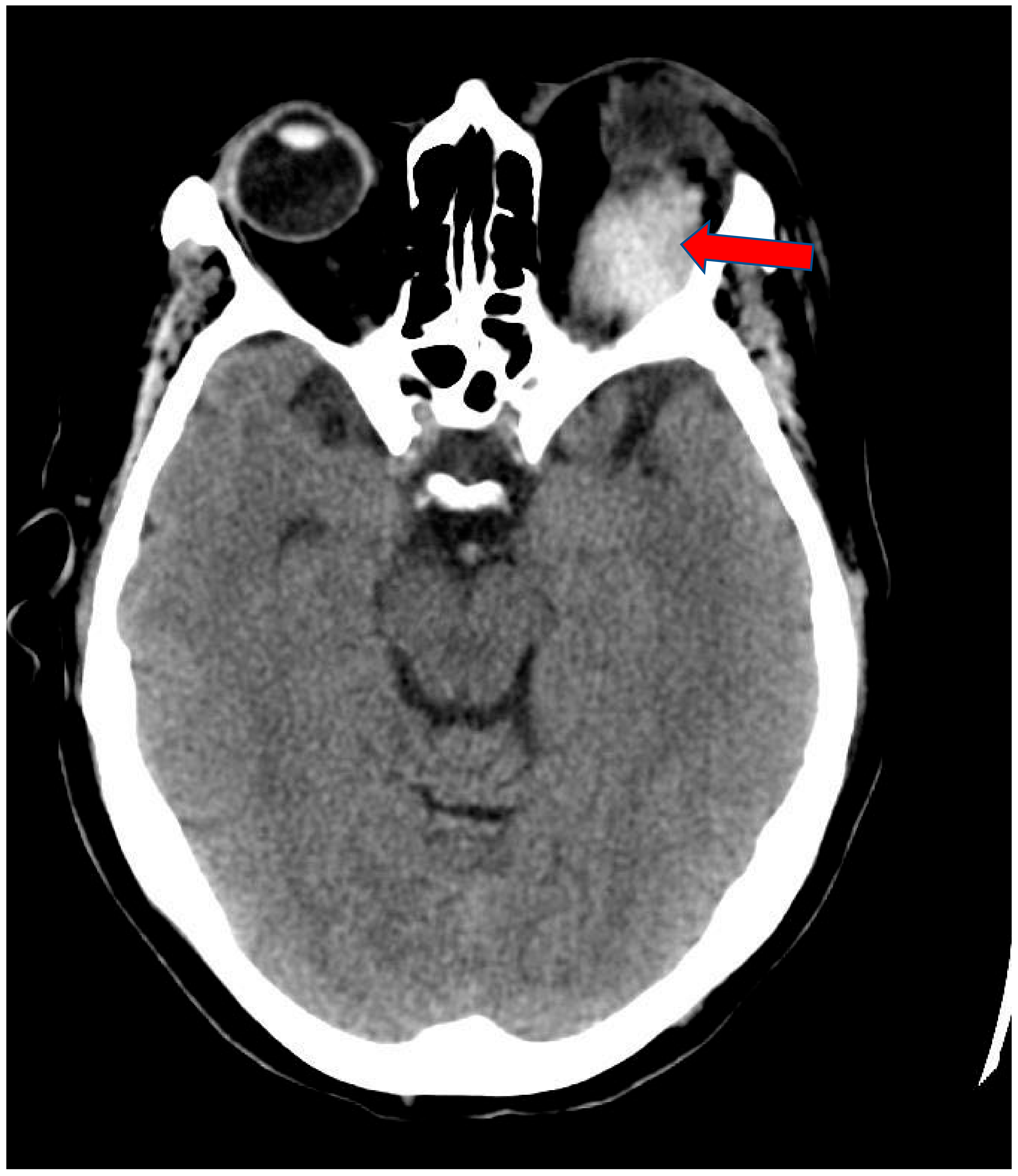
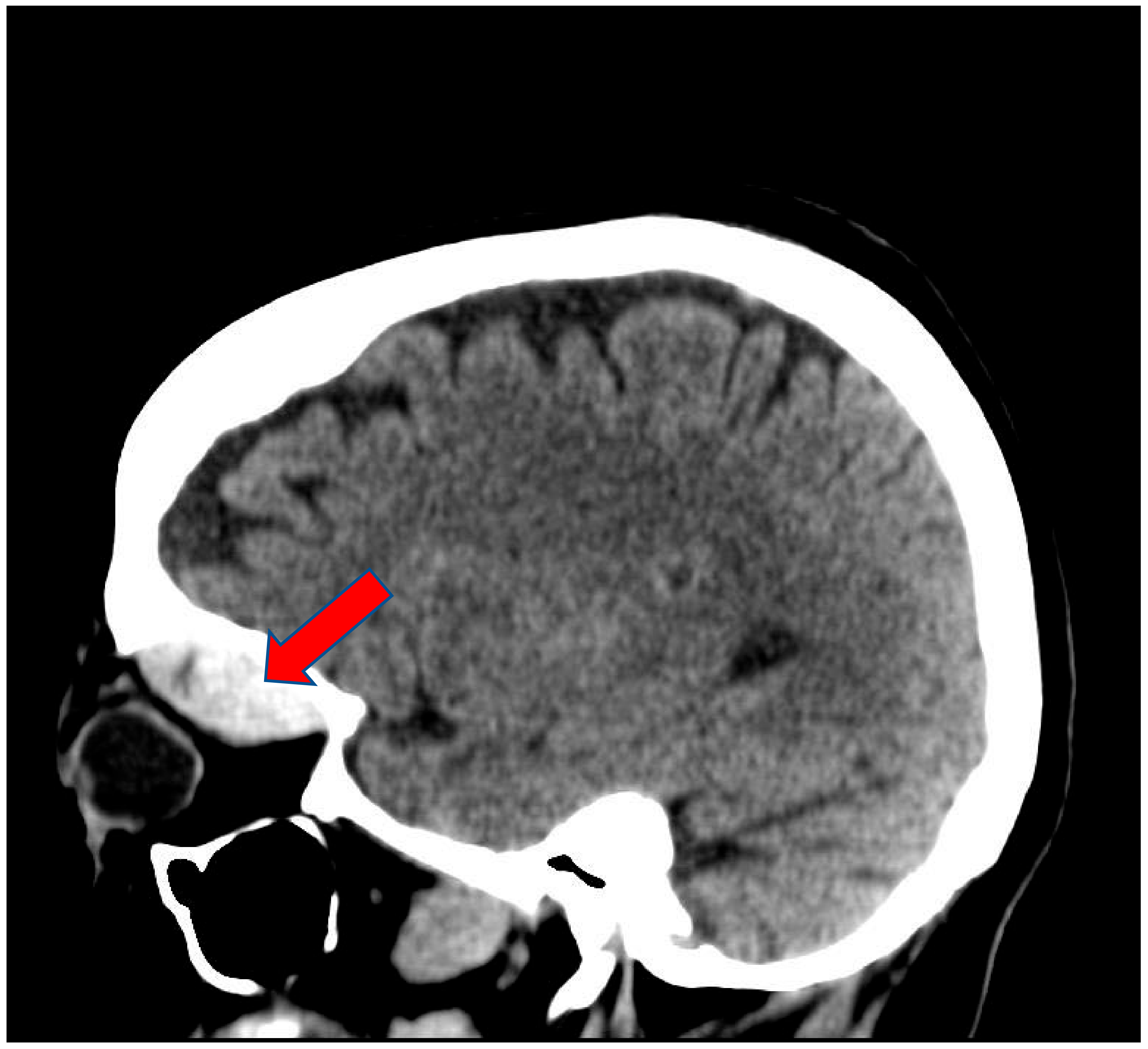
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fattahi, T.; Brewer, K.; Retana, A.; Ogledzki, M. Incidence of retrobulbar hemorrhage in the emergency department. J. Oral Maxillofac. Surg. 2014, 72, 2500–2502. [Google Scholar] [CrossRef] [PubMed]
- Lima, V.; Burt, B.; Leibovitch, I.; Prabhakaran, V.; Goldberg, R.A.; Selva-Nayagam, D. Orbital compartment syndrome: The ophthalmic surgical emergency. Surv. Ophthalmol. 2009, 54, 441–449. [Google Scholar] [CrossRef] [PubMed]
- DeMere, M.; Wood, T.; Austin, W. Eye complications with blepharoplasty or other eyelid surgery. A national survey. Plast. Reconstr. Surg. 1974, 53, 634–637. [Google Scholar] [CrossRef] [PubMed]
- Stankiewicz, J.A.; Chow, J.M. Two faces of orbital hematoma in intranasal (endoscopic) sinus surgery. Otolaryngol. Head Neck Surg. 1999, 120, 841–847. [Google Scholar] [CrossRef]
- Gosau, M.; Schöneich, M.; Draenert, F.G.; Ettl, T.; Driemel, O.; Reichert, T.E. Retrospective analysis of orbital floor fractures--complications, outcome, and review of literature. Clin. Oral Investig. 2011, 15, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Hass, A.N.; Penne, R.B.; Stefanyszyn, M.A.; Flanagan, J.C. Incidence of postblepharoplasty orbital hemorrhage and associated visual loss. Ophthalmic Plast. Reconstr. Surg. 2004, 20, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Teng, C.C.; Reddy, S.; Wong, J.J.; Lisman, R.D. Retrobulbar hemorrhage nine days after cosmetic blepharoplasty resulting in permanent visual loss. Ophthalmic Plast. Reconstr. Surg. 2006, 22, 388–389. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.A.; Roth, S.; Posner, K.L.; Cheney, F.W.; Caplan, R.A.; Newman, N.J.; Domino, K.B. The American Society of Anesthesiologists Postoperative Visual Loss Registry: Analysis of 93 spine surgery cases with postoperative visual loss. Anesthesiology 2006, 105, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Rettinger, G.; Christ, P.; Meythaler, F.H. Erblindung durch Zentralarterienverschluss nach Septumkorrektur [Blindness caused by central artery occlusion following nasal septum correction]. HNO 1990, 38, 105–109. [Google Scholar] [PubMed]
- Whiteman, D.W.; Rosen, D.A.; Pinkerton, R.M. Retinal and choroidal microvascular embolism after intranasal corticosteroid injection. Am. J. Ophthalmol. 1980, 89, 851–853. [Google Scholar] [CrossRef]
- Fu, A.D.; McDonald, H.R.; Eliott, D.; Fuller, D.G.; Halperin, L.S.; Ramsay, R.C.; Johnson, R.N.; Ai, E. Complications of general anesthesia using nitrous oxide in eyes with preexisting gas bubbles. Retina 2002, 22, 569–574. [Google Scholar] [CrossRef] [PubMed]
- Silvanus, M.T.; Moldzio, P.; Bornfeld, N.; Peters, J. Visual loss following intraocular gas injection. Dtsch. Arztebl Int. 2008, 105, 108–112. [Google Scholar] [PubMed]
- Deveer, M.; Cullu, N.; Beydilli, H.; Sozen, H.; Yeniceri, O.; Parlak, S. Spontaneous retrobulbar haematoma. Case Rep. Radiol. 2015, 2015, 796834. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sawalha, K.; Nair, D. Doubly Blinded: An Uncommon Cause of Acute Visual Loss Due to Orbital Compartment Syndrome. Clin. Pract. 2021, 11, 327-331. https://doi.org/10.3390/clinpract11020046
Sawalha K, Nair D. Doubly Blinded: An Uncommon Cause of Acute Visual Loss Due to Orbital Compartment Syndrome. Clinics and Practice. 2021; 11(2):327-331. https://doi.org/10.3390/clinpract11020046
Chicago/Turabian StyleSawalha, Khalid, and Devi Nair. 2021. "Doubly Blinded: An Uncommon Cause of Acute Visual Loss Due to Orbital Compartment Syndrome" Clinics and Practice 11, no. 2: 327-331. https://doi.org/10.3390/clinpract11020046
APA StyleSawalha, K., & Nair, D. (2021). Doubly Blinded: An Uncommon Cause of Acute Visual Loss Due to Orbital Compartment Syndrome. Clinics and Practice, 11(2), 327-331. https://doi.org/10.3390/clinpract11020046




